Submitted:
07 November 2025
Posted:
12 November 2025
Read the latest preprint version here
Abstract
Keywords:
1. Introduction
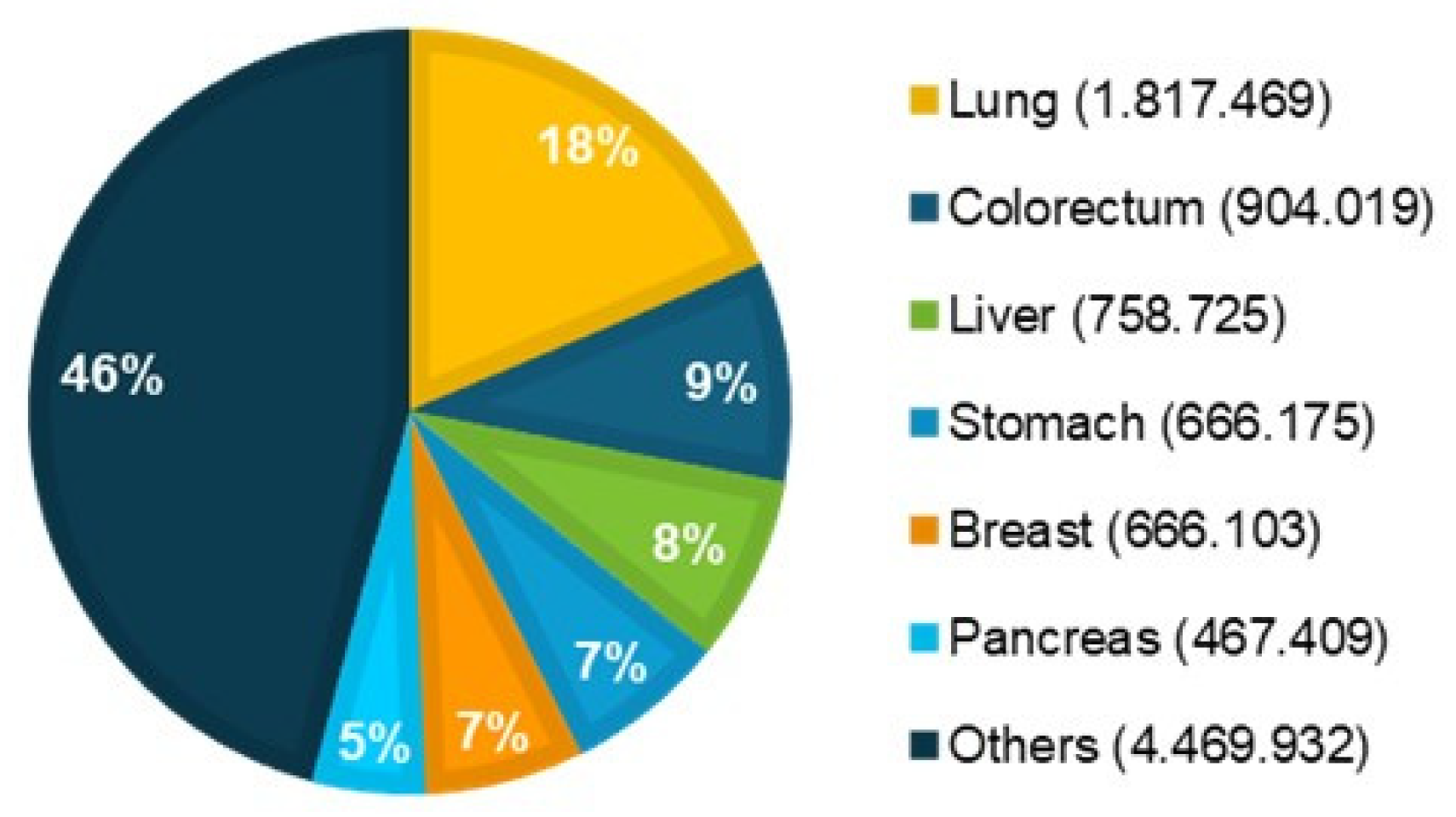
1.1. Global Cancer Epidemiology Overview
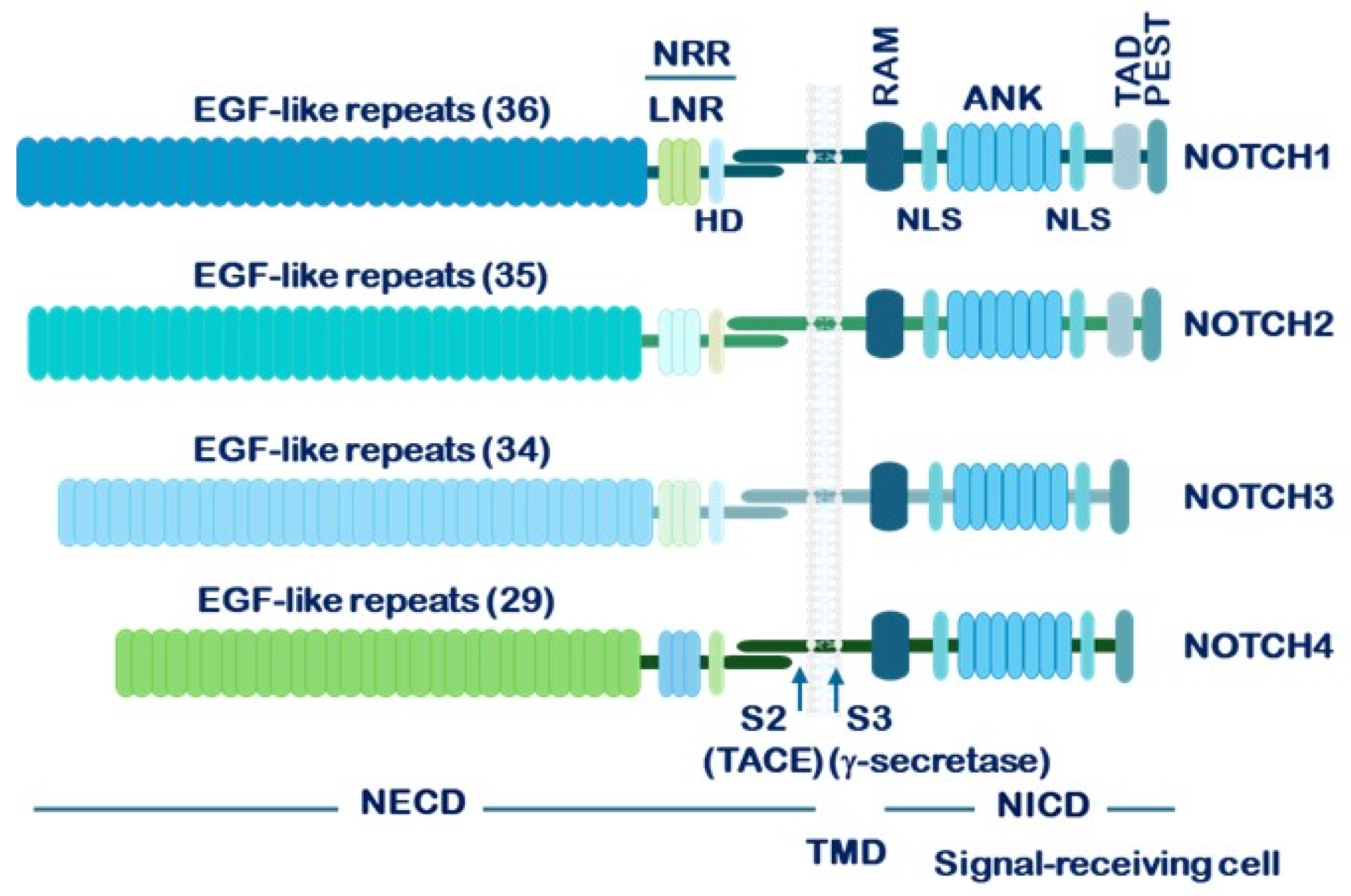
1.2. Structure of NOTCH Receptors and Their Ligands
1.3. Mechanism of NOTCH Receptor Activation and Downstream Signaling
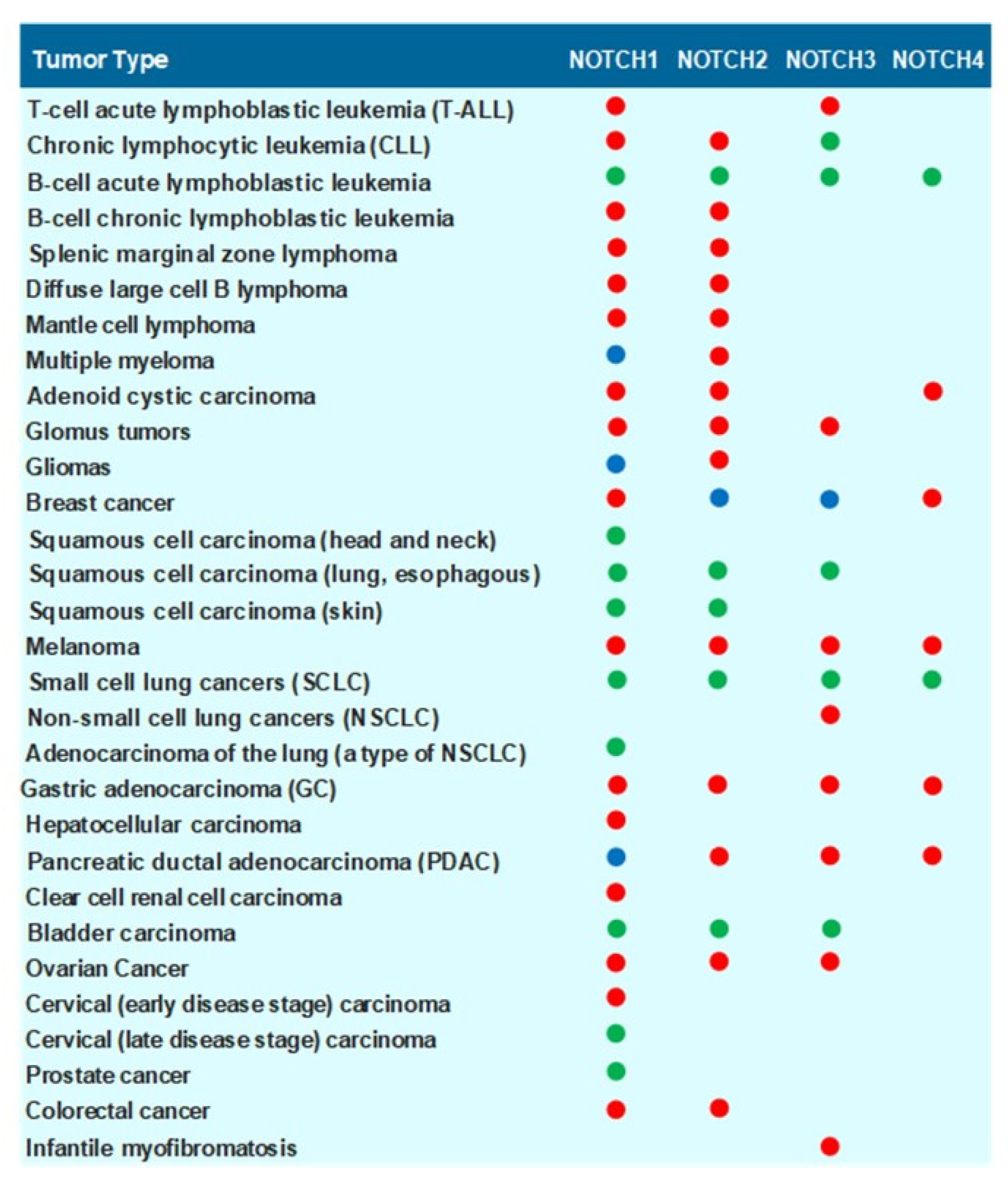
1.4. Role of NOTCH Receptors and NOTCH Ligands in Carcinogenesis
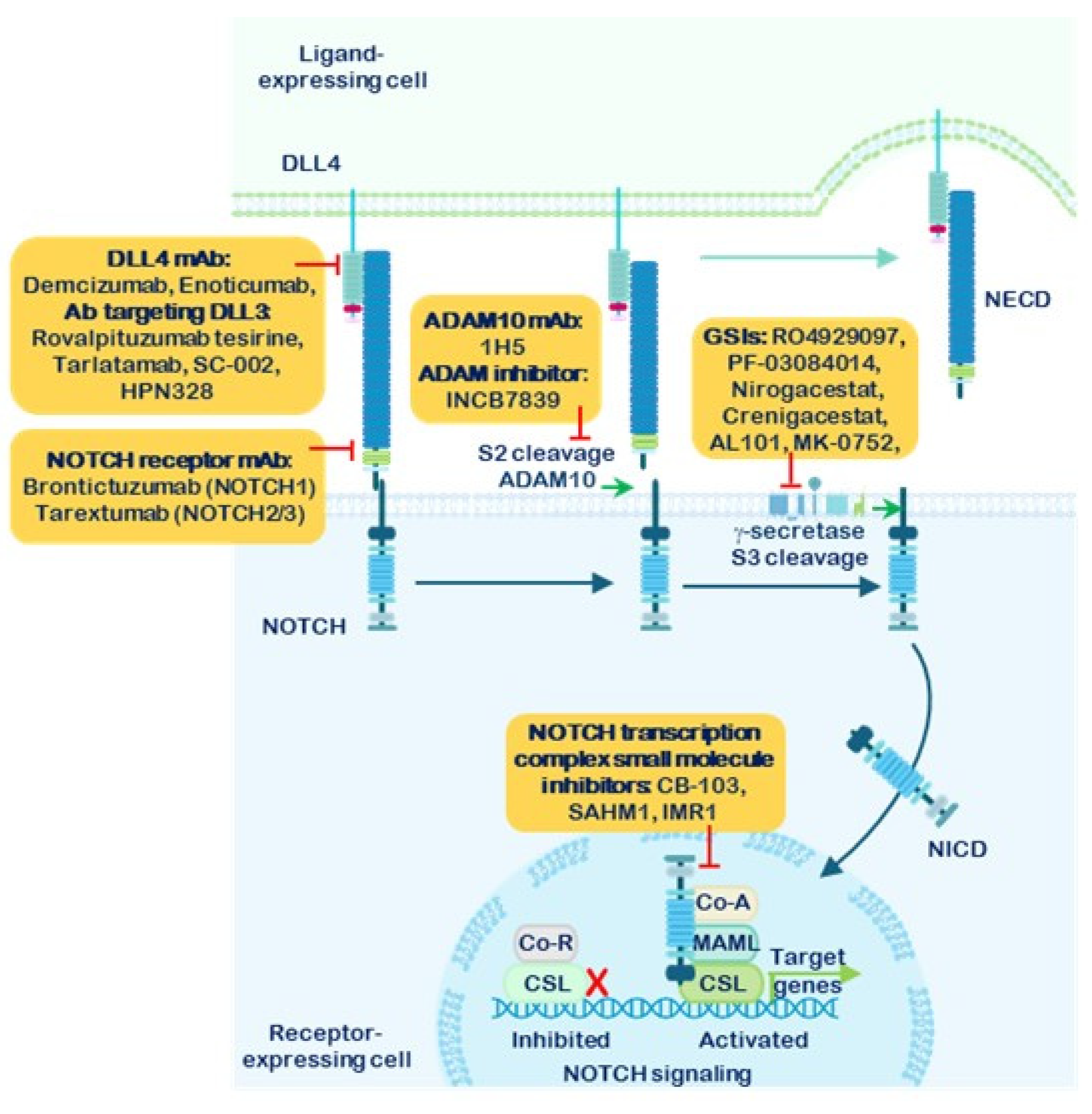
1.5. Strategies for the Inhibition of NOTCH Receptor Signaling
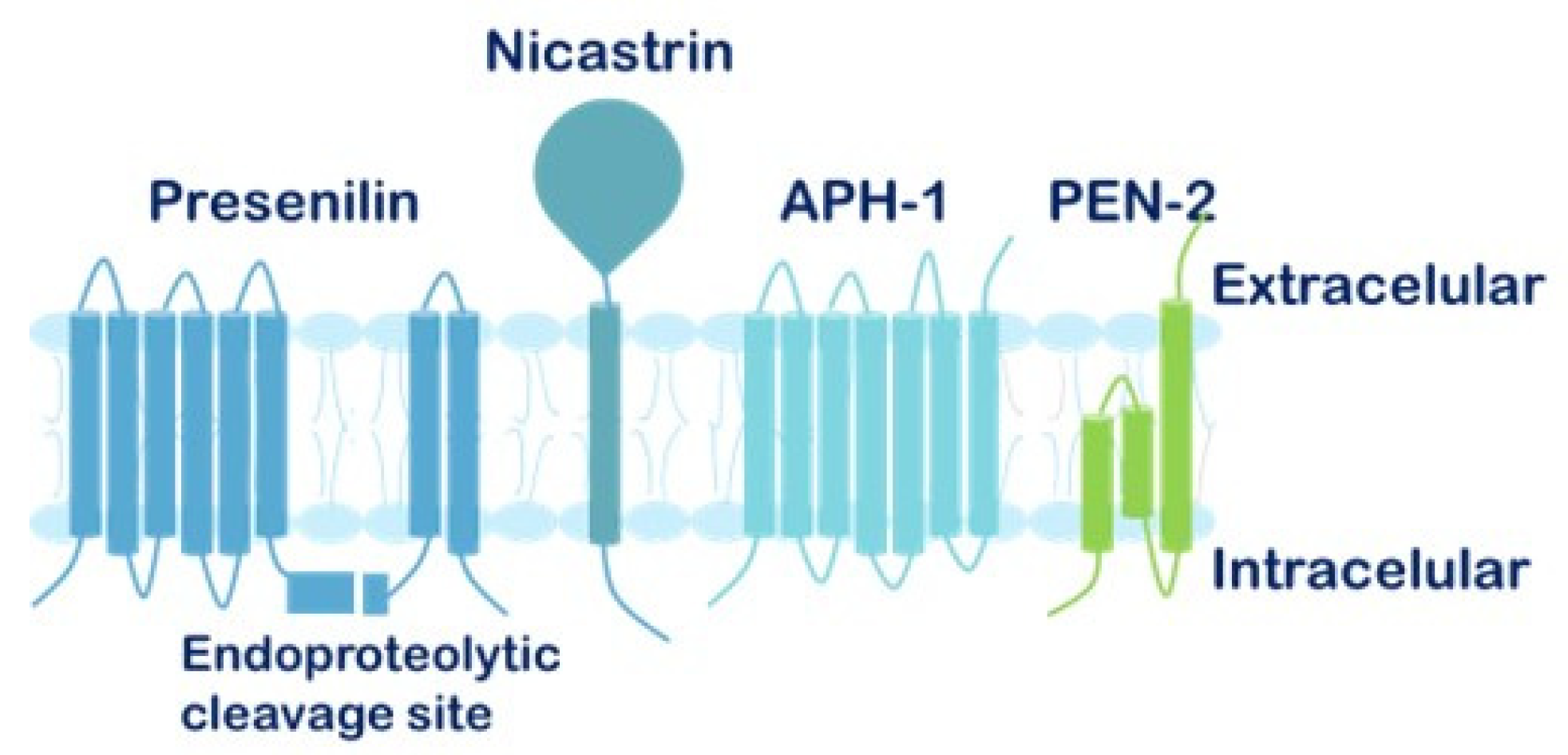
1.6. The γ-Secretase Complex and γ-Secretase Complex Inhibitors (GSIs)
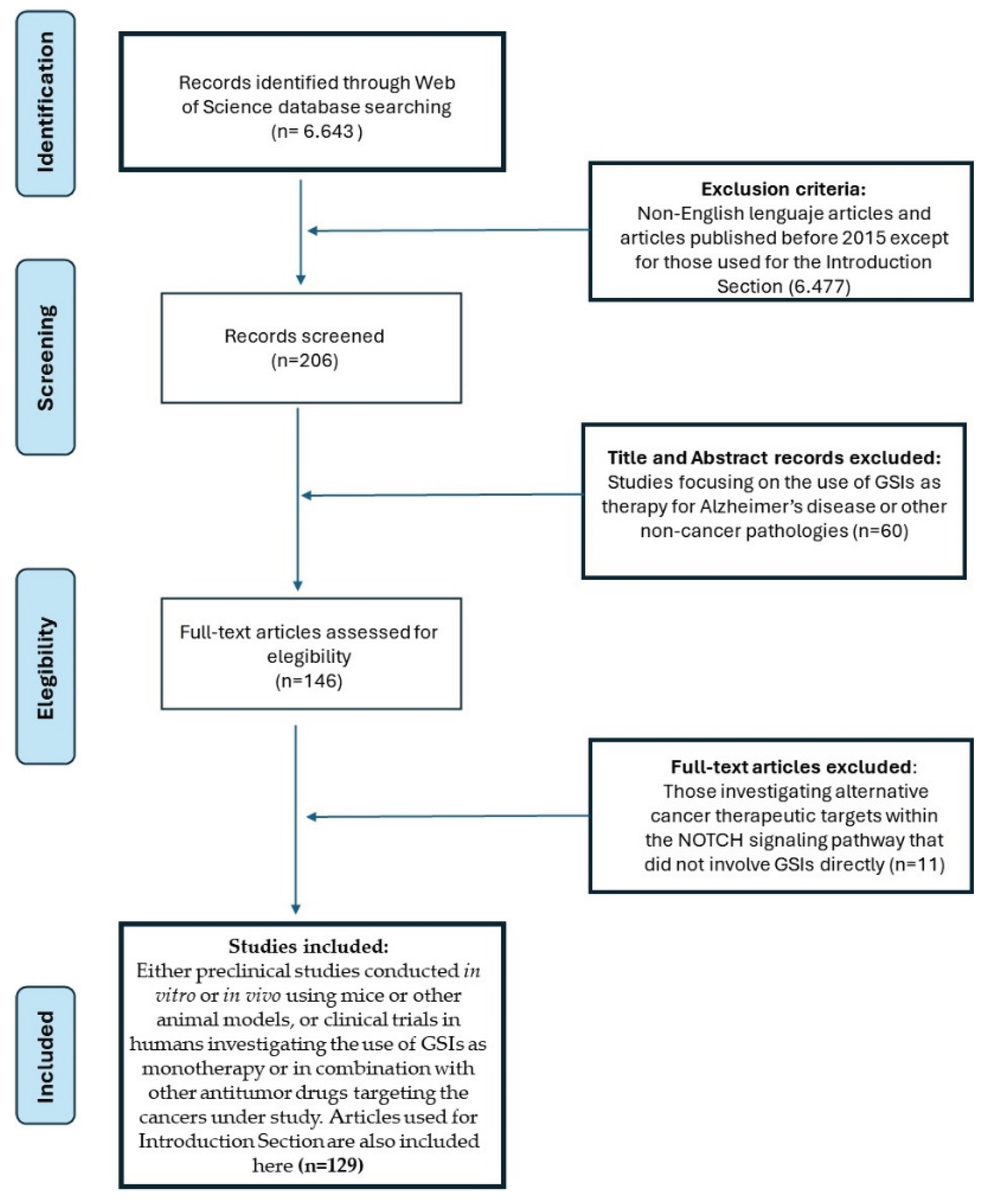
2. Methods
3. Results
3.1. The Combination of GSIs with Other Therapeutic Agents Has Demonstrated Efficacy in Reducing Pancreatic Ductal Adenocarcinoma (PDAC) Progression in Preclinical Studies
3.2. Treatment Resistance in Non-Small Cell Lung Cancer (NSCLC) Can Be Mitigated Through the Application of γ-Secretase Inhibitors Alone and Combined with Other Drugs
3.3. The Use of GSIs, ADAM Inhibitors and Other Combined Therapies Have Contributed to Elucidating the Role of NOTCH Signaling in Gastric Cancer (GC)
3.4. GSIs Enhance the Efficacy of Targeted Therapies in Phase II Clinical Trials for Metastatic Melanoma
3.5. Various Clinical Studies Explore the Use of GSIs as Monotherapy and in Combination Therapies for Triple-Negative Breast Cancer (TNBC)
4. Discussion and Conclusions
5. Challenges and Future Directions
Supplementary Materials
Author Contributions
Funding
Declaration of Generative AI in Scientific Writing
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
- ADAM: A Disintegrin And Metalloproteinase
- ALDH: aldehyde dehydrogenase
- ATRA: All-trans retinoic acid.
- BCL2i: BLC-2 inhibitors.
- BCSCs: Breast cancer stem cells.
- BRAFi: BRAF inhibitor.
- CD44: Cell Surface Glycoprotein CD44
- CD133: Transmembrane glycoprotein CD133
- CSCs: cancer stem cells
- CSL: CBF1/Suppressor of Hairless/LAG-1, also known as RBP-Jκ
- DAPT: GSI-IX
- DLK1: Delta like homolog 1.
- DLK2: Delta like homolog 2.
- DLL1: Canonical Delta-Like1 ligand.
- DLL3: Canonical Delta-Like3 ligand.
- DLL4: Canonical Delta-Like4 ligand.
- DOS: Delta and OSM-11 Motif.
- DSL: Delta/Serrate/LAG-2 domain
- EGF: Epidermal growth factor.
- EMT: Epithelial-Mesenchymal Transition.
- EPBCm: Estrogen receptor-positive metastatic breast cancer.
- ERK: Extracellular Signal-Regulated Kinase
- ERKi: ERK MAPK inhibitor.
- EVO: Evodiamine.
- 5-FU: 5-fluorouracil
- GC: Gastric cancer.
- GCSCs: Gastric cancer stem cells.
- GSC: γ-Secretase complex
- GSI: γ-Secretase inhibitor.
- JAG1: Canonical Jagged 1 ligand.
- JAG2: Canonical Jagged 2 ligand.
- KRAS: Kirsten rat Sarcoma
- LCSCs: Lung cancer stem cells.
- mAb: monoclonal antibodies
- MAML: Mastermind-like protein.
- MAPK: Mitogen-Activated Protein Kinase
- MEK: Mitogen-Activated Protein Kinase 1 (MAP2K1)
- MEKi: MEK inhibitor.
- MET: Mesenchymal Epithelial Transition receptor tyrosine kinase
- METi: MET inhibitor.
- MTD: maximum tolerated dose
- MSC: Melanoma stem cells.
- NECD: NOTCH extracellular domain
- NICD: NOTCH intracellular domain.
- NRR: Negative regulatory region.
- NSCLC: Non-small cell lung cancer.
- PDAC: Pancreatic ductal adenocarcinoma.
- PEST: proline, glutamic acid, serine, and threonine domain
- PFS: Progression-free survival.
- RBP-Jκ: Recombination signal binding protein for immunoglobulin kappa J region
- RECK: Reversion-inducing cysteine-rich protein with Kazal motifs.
- RT: Radiotherapy.
- SAHA: Suberoylanilide hydroxamic acid.
- SS: Sulindac sulfide.
- TACE: Tumor necrosis factor (TNF)-converting enzyme
- TMD: transmembrane domain.
- TNBC: Triple-negative breast cancer.
- WNT: Wingless and Int-1.
- 2D: Two dimensions.
- 3D: Three dimensions.
- WHO: World Health Organization.
References
- Zhou, B.; Lin, W.; Long, Y.; Yang, Y.; Zhang, H.; Wu, K.; Chu, Q. Notch signaling pathway: architecture, disease, and therapeutics. Signal Transduct. Target. Ther. 2022, 7, 1–33. [Google Scholar] [CrossRef]
- Siebel, C.; Lendahl, U. Notch Signaling in Development, Tissue Homeostasis, and Disease. Physiol. Rev. 2017, 97, 1235–1294. [Google Scholar] [CrossRef] [PubMed]
- Aster, J.C.; Pear, W.S.; Blacklow, S.C. The Varied Roles of Notch in Cancer. Annu. Rev. Pathol. Mech. Dis. 2017, 12, 245–275. [Google Scholar] [CrossRef] [PubMed]
- Kopan, R.; Ilagan, M.X.G. The Canonical Notch Signaling Pathway: Unfolding the Activation Mechanism. Cell 2009, 137, 216–233. [Google Scholar] [CrossRef] [PubMed]
- Artavanis-Tsakonas, S.; Rand, M.D.; Lake, R.J. Notch Signaling: Cell Fate Control and Signal Integration in Development. Science 1999, 284, 770–776. [Google Scholar] [CrossRef]
- Weinmaster, G. Notch signal transduction: a real Rip and more. Curr. Opin. Genet. Dev. 2000, 10, 363–369. [Google Scholar] [CrossRef]
- Mumm, J.S.; Kopan, R. Notch signaling: from the outside in. Dev. Biol. 2000, 228, 151–165. [Google Scholar] [CrossRef]
- Lai, E.C. Notch signaling: control of cell communication and cell fate. Development 2004, 131, 965–973. [Google Scholar] [CrossRef]
- Artavanis-Tsakonas, S.; Muskavitch, M.A. Notch: the past, the present, and the future. Curr. Top. Dev. Biol. 2010, 92, 1–29. [Google Scholar]
- Dexter, J.S. The Analysis of a Case of Continuous Variation in Drosophila by a Study of Its Linkage Relations. Am. Nat. 1914, 48, 712–758. [Google Scholar] [CrossRef]
- Blaumueller, C.M.; Qi, H.; Zagouras, P.; Artavanis-Tsakonas, S. Intracellular Cleavage of Notch Leads to a Heterodimeric Receptor on the Plasma Membrane. Cell 1997, 90, 281–291. [Google Scholar] [CrossRef] [PubMed]
- Logeat, F.; Bessia, C.; Brou, C.; LeBail, O.; Jarriault, S.; Seidah, N.G.; Israël, A. The Notch1 receptor is cleaved constitutively by a furin-like convertase. Proc. Natl. Acad. Sci. 1998, 95, 8108–8112. [Google Scholar] [CrossRef]
- Czerwonka, A.; Kałafut, J.; Nees, M. Modulation of Notch Signaling by Small-Molecular Compounds and Its Potential in Anticancer Studies. Cancers 2023, 15, 4563. [Google Scholar] [CrossRef]
- Lubman, O.Y.; Ilagan, M.X.G.; Kopan, R.; Barrick, D. Quantitative Dissection of the Notch:CSL Interaction: Insights into the Notch-mediated Transcriptional Switch. J. Mol. Biol. 2007, 365, 577–589. [Google Scholar] [CrossRef]
- Kopan, R.; Schroeter, E.H.; Weintraub, H.; Nye, J.S. Signal transduction by activated mNotch: importance of proteolytic processing and its regulation by the extracellular domain. Proc. Natl. Acad. Sci. 1996, 93, 1683–1688. [Google Scholar] [CrossRef]
- Kopan, R.; Cagan, R. Notch on the cutting edge. Trends Genet. 1997, 13, 465–467. [Google Scholar] [CrossRef] [PubMed]
- Krebs, L.T.; Xue, Y.; Norton, C.R.; Shutter, J.R.; Maguire, M.; Sundberg, J.P.; Gallahan, D.; Closson, V.; Kitajewski, J.; Callahan, R.; et al. Notch signaling is essential for vascular morphogenesis in mice. Genome Res. 2000, 14, 1343–1352. [Google Scholar] [CrossRef]
- D’Souza, B.; Meloty-Kapella, L.; Weinmaster, G. Canonical and Non-Canonical Notch Ligands. Curr. Top. Dev. Biol. 2010, 92, 73–129. [Google Scholar] [PubMed]
- D’Souza, B.; Miyamoto, A.; Weinmaster, G. The many facets of Notch ligands. Oncogene 2008, 27, 5148–5167. [Google Scholar] [CrossRef]
- Hozumi, K. Distinctive properties of the interactions between Notch and Notch ligands. Dev. Growth Differ. 2019, 62, 49–58. [Google Scholar] [CrossRef]
- Kuintzle, R.; Santat, A.; Elowitz, M.B. Diversity in Notch ligand-receptor signaling interactions. bioRxiv 2024. [Google Scholar] [CrossRef]
- Laborda, J.; Sausville, E.; Hoffman, T.; Notario, V. dlk, a putative mammalian homeotic gene differentially expressed in small cell lung carcinoma and neuroendocrine tumor cell line. J. Biol. Chem. 1993, 268, 3817–3820. [Google Scholar] [CrossRef]
- Baladrón, V.; Ruiz-Hidalgo, M.J.; Nueda, M.L.; Díaz-Guerra, M.J.M.; García-Ramírez, J.J.; Bonvini, E.; Gubina, E.; Laborda, J. dlk acts as a negative regulator of Notch1 activation through interactions with specific EGF-like repeats. Exp. Cell Res. 2005, 303, 343–359. [Google Scholar] [CrossRef]
- Nueda, M.-L.; Baladrón, V.; García-Ramírez, J.-J.; Sánchez-Solana, B.; Ruvira, M.-D.; Rivero, S.; Ballesteros, M.; Monsalve, E.-M.; Díaz-Guerra, M.-J.M.; Ruiz-Hidalgo, M.-J.; et al. The Novel Gene EGFL9/Dlk2, Highly Homologous to Dlk1, Functions as a Modulator of Adipogenesis. J. Mol. Biol. 2007, 367, 1270–1280. [Google Scholar] [CrossRef] [PubMed]
- Nueda, M.-L.; Baladrón, V.; Sánchez-Solana, B.; Ballesteros, M.-A.; Laborda, J. The EGF-like Protein dlk1 Inhibits Notch Signaling and Potentiates Adipogenesis of Mesenchymal Cells. J. Mol. Biol. 2007, 367, 1281–1293. [Google Scholar] [CrossRef] [PubMed]
- Sánchez-Solana, B.; Nueda, M.L.; Ruvira, M.D.; Ruiz-Hidalgo, M.J.; Monsalve, E.M.; Rivero, S.; García-Ramírez, J.J.; Díaz-Guerra, M.J.M.; Baladrón, V.; Laborda, J. The EGF-like proteins DLK1 and DLK2 function as inhibitory non-canonical ligands of NOTCH1 receptor that modulate each other’s activities. Biochim. et Biophys. Acta (BBA) - Mol. Cell Res. 2011, 1813, 1153–1164. [Google Scholar] [CrossRef]
- Schmidt, M.H.; Bicker, F.; Nikolic, I.; Meister, J.; Babuke, T.; Picuric, S.; Müller-Esterl, W.; Plate, K.H.; Dikic, I. Epidermal growth factor-like domain 7 (EGFL7) modulates Notch signalling and affects neural stem cell renewal. Nat. Cell Biol. 2019, 11, 873–880. [Google Scholar] [CrossRef]
- Greene, M.; Lai, Y.; Pajcini, K.; Bailis, W.; Pear, W.S.; Lancaster, E. Delta/Notch-Like EGF-Related Receptor (DNER) Is Not a Notch Ligand. PLOS ONE 2016, 11, e0161157. [Google Scholar] [CrossRef]
- Nueda, M.-L.; Baladrón, V.; García-Ramírez, J.-J.; Sánchez-Solana, B.; Ruvira, M.-D.; Rivero, S.; Ballesteros, M.; Monsalve, E.-M.; Díaz-Guerra, M.-J.M.; Ruiz-Hidalgo, M.-J.; et al. The Novel Gene EGFL9/Dlk2, Highly Homologous to Dlk1, Functions as a Modulator of Adipogenesis. J. Mol. Biol. 2007, 367, 1270–1280. [Google Scholar] [CrossRef]
- Lee, Y.L.; Helman, L.; Hoffman, T.; Laborda, J. dlk, pG2 and Pref-1 mRNAs encode similar proteins belonging to the EGF-like superfamily. Identification of polymorphic variants of this RNA. Biochim. et Biophys. Acta (BBA) - Gene Struct. Expr. 1995, 1261, 223–232. [Google Scholar] [CrossRef]
- Wang, Y.; Kim, K.A.; Kim, J.H.; Sul, H. S. Pref-1, a preadipocyte secreted factor that inhibits adipogenesis. J. Nutr. 2006, 136, 2953–2956. [Google Scholar] [CrossRef]
- Smas, C.M.; Chen, L.; Sul, H.S. Cleavage of Membrane-Associated pref-1 Generates a Soluble Inhibitor of Adipocyte Differentiation. Mol. Cell. Biol. 1997, 17, 977–988. [Google Scholar] [CrossRef]
- Smas, C.M.; Green, D.; Sul, H.S. Structural characterization and alternate splicing of the gene encoding the preadipocyte EGF-like protein Pref-1. Biochemistry 1994, 33, 9257–9265. [Google Scholar] [CrossRef] [PubMed]
- Sánchez-Solana, B.; Nueda, M.L.; Ruvira, M.D.; Ruiz-Hidalgo, M.J.; Monsalve, E.M.; Rivero, S.; García-Ramírez, J.J.; Díaz-Guerra, M.J.M.; Baladrón, V.; Laborda, J. The EGF-like proteins DLK1 and DLK2 function as inhibitory non-canonical ligands of NOTCH1 receptor that modulate each other’s activities. Biochim. et Biophys. Acta (BBA) - Mol. Cell Res. 2011, 1813, 1153–1164. [Google Scholar] [CrossRef] [PubMed]
- Nueda, M.-L.; González-Gómez, M.-J.; Rodríguez-Cano, M.-M.; Monsalve, E.-M.; Díaz-Guerra, M.J.M.; Sánchez-Solana, B.; Laborda, J.; Baladrón, V. DLK proteins modulate NOTCH signaling to influence a brown or white 3T3-L1 adipocyte fate. Sci. Rep. 2018, 8, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Pittaway, J.F.H.; Lipsos, C.; Mariniello, K.; Guasti, L. The role of delta-like non-canonical Notch ligand 1 (DLK1) in cancer. Endocrine-Related Cancer 2021, 28, R271–R287. [Google Scholar] [CrossRef]
- Yevtodiyenko, A.; Schmidt, J.V. Dlk1 expression marks developing endothelium and sites of branching morphogenesis in the mouse embryo and placenta. Dev. Dyn. 2006, 235, 1115–1123. [Google Scholar] [CrossRef]
- Garcia-Gallastegi, P.; Ruiz-García, A.; Ibarretxe, G.; Rivero-Hinojosa, S.; González-Siccha, A.D.; Laborda, J.; Crende, O.; Unda, F.; García-Ramírez, J.J. Similarities and differences in tissue distribution of DLK1 and DLK2 during E16.5 mouse embryogenesis. Histochem. 2019, 152, 47–60. [Google Scholar] [CrossRef]
- Christopoulos, P.F.; Gjølberg, T.T.; Krüger, S.; Haraldsen, G.; Andersen, J.T.; Sundlisæter, E. Targeting the Notch Signaling Pathway in Chronic Inflammatory Diseases. Front. Immunol. 2021, 12. [Google Scholar] [CrossRef]
- Bray, S.J. Notch signalling: a simple pathway becomes complex. Nat. Rev. Mol. Cell Biol. 2006, 7, 678–689. [Google Scholar] [CrossRef]
- Miele, L. Notch signaling. Clin. Cancer Res. 2006, 12, 1074–1079. [Google Scholar] [CrossRef]
- Mumm, J.S.; Schroeter, E.H.; Saxena, M.T.; Griesemer, A.; Tian, X.; Pan, D.; Ray, W.J.; Kopan, R. A Ligand-Induced Extracellular Cleavage Regulates γ-Secretase-like Proteolytic Activation of Notch1. Mol. Cell 2000, 5, 197–206. [Google Scholar] [CrossRef]
- Brou, C.; Logeat, F.; Gupta, N.; Bessia, C.; LeBail, O.; Doedens, J.R.; Cumano, A.; Roux, P.; Black, R.A.; Israël, A. A novel proteolytic cleavage involved in Notch signaling: the role of the disintegrin-metalloprotease TACE. Mol. Cell 2000, 5, 207–216. [Google Scholar] [CrossRef]
- Lai, E.C. Notch Cleavage: Nicastrin Helps Presenilin Make the Final Cut. Curr. Biol. 2002, 12, R200–R202. [Google Scholar] [CrossRef] [PubMed]
- Wolfe, M.S. Substrate recognition and processing by γ-secretase. Biochim. et Biophys. Acta (BBA) - Biomembr. 2020, 1862, 183016. [Google Scholar] [CrossRef]
- Kimberly, W.T.; Esler, W.P.; Ye, W.; Ostaszewski, B.L.; Gao, J.; Diehl, T.; Selkoe, D.J.; Wolfe, M.S. Notch and the Amyloid Precursor Protein Are Cleaved by Similar γ-Secretase(s). Biochemistry 2002, 42, 137–144. [Google Scholar] [CrossRef]
- Wong, E.; Frost, G.R.; Li, Y.-M. γ-Secretase Modulatory Proteins: The Guiding Hand Behind the Running Scissors. Front. Aging Neurosci. 2020, 12. [Google Scholar] [CrossRef] [PubMed]
- Schroeter, E.H.; Kisslinger, J.A.; Kopan, R. Notch-1 signalling requires ligand-induced proteolytic release of intracellular domain. Nature 1998, 393, 382–386. [Google Scholar] [CrossRef]
- Barrick, D.; Kopan, R. The Notch Transcription Activation Complex Makes Its Move. Cell 2006, 124, 883–885. [Google Scholar] [CrossRef]
- Previs, R.A.; Coleman, R.L.; Harris, A.L.; Sood, A.K. Molecular Pathways: Translational and Therapeutic Implications of the Notch Signaling Pathway in Cancer. Clin. Cancer Res. 2015, 21, 955–961. [Google Scholar] [CrossRef]
- Katoh, M.; Katoh, M. Precision medicine for human cancers with Notch signaling dysregulation (Review). Int. J. Mol. Med. 2020, 45, 279–297. [Google Scholar] [CrossRef]
- Aster, J.C.; Pear, W.S.; Blacklow, S.C. The Varied Roles of Notch in Cancer. Annu. Rev. Pathol. Mech. Dis. 2017, 12, 245–275. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, A.; Aster, J.C. Notch signaling in cancer: Complexity and challenges on the path to clinical translation. Semin. Cancer Biol. 2022, 85, 95–106. [Google Scholar] [CrossRef] [PubMed]
- Aster, J.C.; Blacklow, S.C. Targeting the Notch Pathway: Twists and Turns on the Road to Rational Therapeutics. J. Clin. Oncol. 2012, 30, 2418–2420. [Google Scholar] [CrossRef] [PubMed]
- Chimento, A.; D’amico, M.; Pezzi, V.; De Amicis, F. Notch Signaling in Breast Tumor Microenvironment as Mediator of Drug Resistance. Int. J. Mol. Sci. 2022, 23, 6296. [Google Scholar] [CrossRef]
- Gallahan, D.; Callahan, R. The mouse mammary tumor associated gene INT3 is a unique member of the NOTCH gene family (NOTCH4). Oncogene 1997, 14, 1883–1890. [Google Scholar] [CrossRef]
- Demitrack, E.S.; Samuelson, L.C. Notch as a Driver of Gastric Epithelial Cell Proliferation. Cell. Mol. Gastroenterol. Hepatol. 2017, 3, 323–330. [Google Scholar] [CrossRef]
- Gupta, S.; Kumar, P.; Das, B.C. HPV: Molecular pathways and targets. Curr. Probl. Cancer 2018, 42, 161–174. [Google Scholar] [CrossRef]
- Cook, N.; Frese, K.K.; Bapiro, T.E.; Jacobetz, M.A.; Gopinathan, A.; Miller, J.L.; Rao, S.S.; Demuth, T.; Howat, W.J.; Jodrell, D.I.; et al. Gamma secretase inhibition promotes hypoxic necrosis in mouse pancreatic ductal adenocarcinoma. J. Exp. Med. 2012, 209, 437–444. [Google Scholar] [CrossRef]
- Grochowski, C.M.; Loomes, K.M.; Spinner, N.B. Jagged1 (JAG1): Structure, expression, and disease associations. Gene 2016, 576, 381–384. [Google Scholar] [CrossRef]
- Grassi, E.S.; Pietras, A. Emerging Roles of DLK1 in the Stem Cell Niche and Cancer Stemness. J. Histochem. Cytochem. 2021, 70, 17–28. [Google Scholar] [CrossRef]
- Nueda, M.-L.; Naranjo, A.-I.; Baladrón, V.; Laborda, J. The proteins DLK1 and DLK2 modulate NOTCH1-dependent proliferation and oncogenic potential of human SK-MEL-2 melanoma cells. Biochim. et Biophys. Acta (BBA) - Mol. Cell Res. 2014, 1843, 2674–2684. [Google Scholar] [CrossRef]
- Naranjo, A.-I.; González-Gómez, M.-J.; Baladrón, V.; Laborda, J.; Nueda, M.-L. Different Expression Levels of DLK2 Inhibit NOTCH Signaling and Inversely Modulate MDA-MB-231 Breast Cancer Tumor Growth In Vivo. Int. J. Mol. Sci. 2022, 23, 1554. [Google Scholar] [CrossRef]
- Nueda, M.; Naranjo, A.; Baladrón, V.; Laborda, J. Different expression levels of DLK1 inversely modulate the oncogenic potential of human MDA-MB-231 breast cancer cells through inhibition of NOTCH1 signaling. FASEB J. 2017, 31, 3484–3496. [Google Scholar] [CrossRef] [PubMed]
- Lundkvist, J.; Naslund, J. Gamma-secretase: a complex target for Alzheimer’s disease. Curr. Opin. Pharmacol. 2007, 7, 112–118. [Google Scholar] [CrossRef] [PubMed]
- Moore, G.; Annett, S.; McClements, L.; Robson, T. Top Notch Targeting Strategies in Cancer: A Detailed Overview of Recent Insights and Current Perspectives. Cells 2020, 9, 1503. [Google Scholar] [CrossRef] [PubMed]
- Groth, C.; Fortini, M.E. Therapeutic approaches to modulating Notch signaling: Current challenges and future prospects. Semin. Cell Dev. Biol. 2012, 23, 465–472. [Google Scholar] [CrossRef]
- Panelos, J.; Batistatou, A.; Paglierani, M.; Zioga, A.; Maio, V.; Santi, R.; Pimpinelli, N.; De Giorgi, V.; Santucci, M.; Massi, D. Expression of Notch-1 and alteration of the E-cadherin/β-catenin cell adhesion complex are observed in primary cutaneous neuroendocrine carcinoma (Merkel cell carcinoma). Mod. Pathol. 2009, 22, 959–968. [Google Scholar] [CrossRef]
- Zhang, X.; Li, Y.; Xu, H.; Zhang, Y.W. The gamma-secretase complex: from structure to function. Front. Cell. Neurosci. 2014, 8, 427. [Google Scholar] [CrossRef]
- Wolfe, M.S. Structure and Function of the gamma-Secretase Complex Biochemistry. Biochemistry 2019, 58, 2953–2966. [Google Scholar] [CrossRef]
- Kimberly, W.T.; Wolfe, M.S. Identity and function of gamma-secretase. J. Neurosci. Res. 2003, 74, 353–360. [Google Scholar] [CrossRef]
- Ghanbari-Movahed, M.; Ghanbari-Movahed, Z.; Momtaz, S.; Kilpatrick, K.L.; Farzaei, M.H.; Bishayee, A. Unlocking the Secrets of Cancer Stem Cells with γ-Secretase Inhibitors: A Novel Anticancer Strategy. Molecules 2021, 26, 972. [Google Scholar] [CrossRef] [PubMed]
- Ran, Y.; Hossain, F.; Pannuti, A.; Lessard, C.B.; Ladd, G.Z.; Jung, J.I.; Minter, L.M.; A Osborne, B.; Miele, L.; E Golde, T. γ-Secretase inhibitors in cancer clinical trials are pharmacologically and functionally distinct. EMBO Mol. Med. 2017, 9, 950–966. [Google Scholar] [CrossRef] [PubMed]
- Moher, D. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst. Rev. 2015, 4, 1. [Google Scholar] [CrossRef] [PubMed]
- Avila, J.L.; Kissil, J.L. Notch signaling in pancreatic cancer: oncogene or tumor suppressor? Trends Mol. Med. 2013, 19, 320–327. [Google Scholar] [CrossRef]
- Samore, W.R.; Gondi, C.S. Brief overview of selected approaches in targeting pancreatic adenocarcinoma. Expert Opin. Investig. Drugs 2014, 23, 793–807. [Google Scholar] [CrossRef] [PubMed]
- Yabuuchi, S.; Pai, S.G.; Campbell, N.R.; de Wilde, R.F.; De Oliveira, E.; Korangath, P.; Streppel, M.M.; Rasheed, Z.A.; Hidalgo, M.; Maitra, A.; et al. Notch signaling pathway targeted therapy suppresses tumor progression and metastatic spread in pancreatic cancer. Cancer Lett. 2013, 335, 41–51. [Google Scholar] [CrossRef]
- Mizuma, M.; Rasheed, Z.A.; Yabuuchi, S.; Omura, N.; Campbell, N.R.; de Wilde, R.F.; De Oliveira, E.; Zhang, Q.; Puig, O.; Matsui, W.; et al. The Gamma Secretase Inhibitor MRK-003 Attenuates Pancreatic Cancer Growth in Preclinical Models. Mol. Cancer Ther. 2012, 11, 1999–2009. [Google Scholar] [CrossRef]
- Palagani, V.; Bozko, P.; El Khatib, M.; Belahmer, H.; Giese, N.; Sipos, B.; Malek, N.P.; Plentz, R.R. Combined inhibition of Notch and JAK/STAT is superior to monotherapies and impairs pancreatic cancer progression. Carcinog. 2013, 35, 859–866. [Google Scholar] [CrossRef]
- Gounder, M.; Ratan, R.; Alcindor, T.; Schöffski, P.; van der Graaf, W.T.; Wilky, B.A.; Riedel, R.F.; Lim, A.; Smith, L.M.; Moody, S.; et al. Nirogacestat, a γ-Secretase Inhibitor for Desmoid Tumors. New Engl. J. Med. 2023, 388, 898–912. [Google Scholar] [CrossRef]
- Cook, N.; Basu, B.; Smith, D.-M.; Gopinathan, A.; Evans, J.; Steward, W.P.; Palmer, D.; Propper, D.; Venugopal, B.; Hategan, M.; et al. A phase I trial of the γ-secretase inhibitor MK-0752 in combination with gemcitabine in patients with pancreatic ductal adenocarcinoma. Br. J. Cancer 2018, 118, 793–801. [Google Scholar] [CrossRef] [PubMed]
- De Jesus-Acosta, A.; Laheru, D.; Maitra, A.; Arcaroli, J.; Rudek, M.A.; Dasari, A.; Messersmith, W. A phase II study of the gamma secretase inhibitor RO4929097 in patients with previously treated metastatic pancreatic adenocarcinoma. Invest. New Drugs 2014, 32, 739–745. [Google Scholar] [CrossRef]
- Zhang, Y.; Xu, W.; Guo, H.; Zhang, Y.; He, Y.; Lee, S.H.; Guo, W. NOTCH1 Signaling Regulates Self-Renewal and Platinum Chemoresistance of Cancer Stem-like Cells in Human Non-Small Cell Lung Cancer. Cancer Res. 2017, 77, 3082–3091. [Google Scholar] [CrossRef]
- Morgan, K.M.; Fischer, B.S.; Lee, F.Y.; Shah, J.J.; Bertino, J.R.; Rosenfeld, J.; Singh, A.; Khiabanian, H.; Pine, S.R. Gamma Secretase Inhibition by BMS-906024 Enhances Efficacy of Paclitaxel in Lung Adenocarcinoma. Mol. Cancer Ther. 2017, 16, 2759–2769. [Google Scholar] [CrossRef] [PubMed]
- Iglesias, V.S.; Theys, J.; Groot, A.J.; Barbeau, L.M.O.; Lemmens, A.; Yaromina, A.; Losen, M.; Houben, R.; Dubois, L.; Vooijs, M. Synergistic Effects of NOTCH/γ-Secretase Inhibition and Standard of Care Treatment Modalities in Non-small Cell Lung Cancer Cells. Front. Oncol. 2018, 8, 460. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.P.; Yang, C.J.; Huang, M.S.; Yeh, C.T.; Wu, A.T.; Lee, Y.C.; Hsiao, M. Cisplatin selects for multidrug-resistant CD133+ cells in lung adenocarcinoma by activating Notch signaling. Cancer Res. 2013, 73, 406–416. [Google Scholar] [CrossRef]
- Xie, M.; He, J.; He, C.; Wei, S. γ Secretase Inhibitor BMS-708163 Reverses Resistance to EGFR Inhibitor via the PI3K/Akt Pathway in Lung Cancer. J. Cell. Biochem. 2015, 116, 1019–1027. [Google Scholar] [CrossRef]
- Pine, S.R. Rethinking Gamma-secretase Inhibitors for Treatment of Non-small-Cell Lung Cancer: Is Notch the Target? Clin. Cancer Res. 2018, 24, 6136–6141. [Google Scholar] [CrossRef]
- Mizugaki, H.; Sakakibara-Konishi, J.; Ikezawa, Y.; Kikuchi, J.; Kikuchi, E.; Oizumi, S.; Dang, T.P.; Nishimura, M. γ-Secretase inhibitor enhances antitumour effect of radiation in Notch-expressing lung cancer. Br. J. Cancer 2012, 106, 1953–1959. [Google Scholar] [CrossRef]
- Yang, X.; Zhang, Y.; Huang, Y.; Wang, Y.; Qi, X.; Su, T.; Lu, L. Evodiamine suppresses Notch3 signaling in lung tumorigenesis via direct binding to γ-secretases. Phytomedicine 2020, 68, 153176. [Google Scholar] [CrossRef]
- Demitrack, E.S.; Gifford, G.B.; Keeley, T.M.; Horita, N.; Todisco, A.; Turgeon, D.K.; Siebel, C.W.; Samuelson, L.C. NOTCH1 and NOTCH2 regulate epithelial cell proliferation in mouse and human gastric corpus. Am. J. Physiol. Liver Physiol. 2017, 312, G133–G144. [Google Scholar] [CrossRef]
- Hong, K.; Wu, D.; Cheng, K.; Chen, L.; Hung, W. RECK Inhibits Stemness Gene Expression and Tumorigenicity of Gastric Cancer Cells by Suppressing ADAM-Mediated Notch1 Activation. J. Cell. Physiol. 2013, 229, 191–201. [Google Scholar] [CrossRef]
- Li, L.-C.; Wang, D.-L.; Wu, Y.-Z.; Nian, W.-Q.; Wu, Z.-J.; Li, Y.; Ma, H.-W.; Shao, J.-H. Gastric tumor-initiating CD44+ cells and epithelial-mesenchymal transition are inhibited by γ-secretase inhibitor DAPT. Oncol. Lett. 2015, 10, 3293–3299. [Google Scholar] [CrossRef] [PubMed]
- Barat, S.; Chen, X.; Bui, K.C.; Bozko, P.; Götze, J.; Christgen, M.; Krech, T.; Malek, N.P.; Plentz, R.R. Gamma-Secretase Inhibitor IX (GSI) Impairs Concomitant Activation of Notch and Wnt-Beta-Catenin Pathways in CD44+ Gastric Cancer Stem Cells. STEM CELLS Transl. Med. 2017, 6, 819–829. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.-J.; Lee, H.-W.; Baek, J.-H.; Cho, Y.-H.; Kang, H.G.; Jeong, J.S.; Song, J.; Park, H.-S.; Chun, K.-H. Activation of nuclear PTEN by inhibition of Notch signaling induces G2/M cell cycle arrest in gastric cancer. Oncogene 2015, 35, 251–260. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.-W.; Kim, S.-J.; Choi, I.J.; Song, J.; Chun, K.-H. Targeting Notch signaling by γ-secretase inhibitor I enhances the cytotoxic effect of 5-FU in gastric cancer. Clin. Exp. Metastasis 2015, 32, 593–603. [Google Scholar] [CrossRef]
- Yao, J.; Qian, C.; Shu, T.; Zhang, X.; Zhao, Z.; Liang, Y. Combination treatment of PD98059 and DAPT in gastric cancer through induction of apoptosis and downregulation of WNT/β-catenin. Cancer Biol. Ther. 2013, 14, 833–839. [Google Scholar] [CrossRef]
- Kang, M.; Zhang, Y.; Jin, X.; Chen, G.; Huang, Y.; Wu, D.; Li, G.; Shan, J.; Huang, P.; Chen, J. Concurrent Treatment with Anti-DLL4 Enhances Antitumor and Proapoptotic Efficacy of a γ-Secretase Inhibitor in Gastric Cancer. Transl. Oncol. 2018, 11, 599–608. [Google Scholar] [CrossRef]
- Kumar, D.; Kumar, S.; Gorain, M.; Tomar, D.; Patil, H.S.; Radharani, N.N.; Kumar, T.V.; Patil, T.V.; Thulasiram, H.V.; Kundu, G.C. Notch1-MAPK Signaling Axis Regulates CD133+ Cancer Stem Cell-Mediated Melanoma Growth and Angiogenesis. J. Investig. Dermatol. 2016, 136, 2462–2474. [Google Scholar] [CrossRef]
- Zhu, G.; Yi, X.; Haferkamp, S.; Hesbacher, S.; Li, C.; Goebeler, M.; Gao, T.; Houben, R.; Schrama, D. Combination with γ-secretase inhibitor prolongs treatment efficacy of BRAF inhibitor in BRAF-mutated melanoma cells. Cancer Lett. 2016, 376, 43–52. [Google Scholar] [CrossRef]
- Porcelli, L.; Di Fonte, R.; Pierri, C.L.; Fucci, L.; Saponaro, C.; Armenio, A.; Serratì, S.; Strippoli, S.; Fasano, R.; Volpicella, M.; et al. BRAFV600E;K601Q metastatic melanoma patient-derived organoids and docking analysis to predict the response to targeted therapy. Pharmacol. Res. 2022, 182, 106323. [Google Scholar] [CrossRef]
- Krepler, C.; Xiao, M.; Samanta, M.; Vultur, A.; Chen, H.-Y.; Brafford, P.; Reyes-Uribe, P.I.; Halloran, M.; Chen, T.; He, X.; et al. Targeting Notch enhances the efficacy of ERK inhibitors in BRAF-V600E melanoma. Oncotarget 2016, 7, 71211–71222. [Google Scholar] [CrossRef]
- Mukherjee, N.; Almeida, A.; Partyka, K.A.; Lu, Y.; Schwan, J.V.; Lambert, K.; Rogers, M.; A Robinson, W.; E Robinson, S.; Applegate, A.J.; et al. Combining a GSI and BCL-2 inhibitor to overcome melanoma’s resistance to current treatments. Oncotarget 2016, 7, 84594–84607. [Google Scholar] [CrossRef]
- Nueda, M.-L.; Naranjo, A.-I.; Baladrón, V.; Laborda, J. The proteins DLK1 and DLK2 modulate NOTCH1-dependent proliferation and oncogenic potential of human SK-MEL-2 melanoma cells. Biochim. et Biophys. Acta (BBA) - Mol. Cell Res. 2014, 1843, 2674–2684. [Google Scholar] [CrossRef]
- Keyghobadi, F.; Mehdipour, M.; Nekoukar, V.; Firouzi, J.; Kheimeh, A.; Lahrood, F.N.; Zavareh, V.A.; Azimi, M.; Mohammadi, M.; Sodeifi, N.; et al. Long-Term Inhibition of Notch in A-375 Melanoma Cells Enhances Tumor Growth Through the Enhancement of AXIN1, CSNK2A3, and CEBPA2 as Intermediate Genes in Wnt and Notch Pathways. Front. Oncol. 2020, 10, 531. [Google Scholar] [CrossRef] [PubMed]
- Tolcher, A.W.; Messersmith, W.A.; Mikulski, S.M.; Papadopoulos, K.P.; Kwak, E.L.; Gibbon, D.G.; Patnaik, A.; Falchook, G.S.; Dasari, A.; Shapiro, G.I.; et al. Phase I Study of RO4929097, a Gamma Secretase Inhibitor of Notch Signaling, in Patients With Refractory Metastatic or Locally Advanced Solid Tumors. J. Clin. Oncol. 2012, 30, 2348–2353. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.M.; Moon, J.; Redman, B.G.; Chidiac, T.; Flaherty, L.E.; Zha, Y.; Othus, M.; Ribas, A.; Sondak, V.K.; Gajewski, T.F.; et al. Phase 2 study of RO4929097, a gamma-secretase inhibitor, in metastatic melanoma: SWOG 0933. Cancer 2014, 121, 432–440. [Google Scholar] [CrossRef]
- Jayaprakash, K.T.; Hussein, M.; Shaffer, R.; Michael, A.; Nisbet, A.; Ajaz, M. In Vitro Evaluation of Notch Inhibition to Enhance Efficacy of Radiation Therapy in Melanoma. Adv. Radiat. Oncol. 2020, 6, 100622. [Google Scholar] [CrossRef]
- Azzam, D.J.; Zhao, D.; Sun, J.; Minn, A.J.; Ranganathan, P.; Drews-Elger, K.; Han, X.; Picon-Ruiz, M.; Gilbert, C.A.; Wander, S.A.; et al. Triple negative breast cancer initiating cell subsets differ in functional and molecular characteristics and in γ-secretase inhibitor drug responses. EMBO Mol. Med. 2013, 5, 1502–1522. [Google Scholar] [CrossRef]
- Li, W.; Yang, H.; Li, X.; Han, L.; Xu, N.; Shi, A. Signaling pathway inhibitors target breast cancer stem cells in triple-negative breast cancer. Oncol. Rep. 2018, 41, 437–446. [Google Scholar] [CrossRef]
- Stoeck, A.; Lejnine, S.; Truong, A.; Pan, L.; Wang, H.; Zang, C.; Sathyanarayanan, S. Discovery of biomarkers predictive of GSI response in triple-negative breast cancer and adenoid cystic carcinoma. Cancer Discov. 2014, 4, 1154–1167. [Google Scholar] [CrossRef]
- Zhang, S.; Chung, W.-C.; Miele, L.; Xu, K. Targeting Met and Notch in theLfng-deficient,Met-amplified triple-negative breast cancer. Cancer Biol. Ther. 2014, 15, 633–642. [Google Scholar] [CrossRef]
- Schott, A.F.; Landis, M.D.; Dontu, G.; Griffith, K.A.; Layman, R.M.; Krop, I.; Chang, J.C. Preclinical and clinical studies of gamma secretase inhibitors with docetaxel on human breast tumors. Clin. Cancer Res. 2013, 19, 1512–1524. [Google Scholar] [CrossRef] [PubMed]
- Locatelli, M.A.; Aftimos, P.; Dees, E.C.; LoRusso, P.M.; Pegram, M.D.; Awada, A.; Huang, B.; Cesari, R.; Jiang, Y.; Shaik, M.N.; et al. Phase I study of the gamma secretase inhibitor PF-03084014 in combination with docetaxel in patients with advanced triple-negative breast cancer. Oncotarget 2016, 8, 2320–2328. [Google Scholar] [CrossRef]
- Sardesai, S.; Badawi, M.; Mrozek, E.; Morgan, E.; Phelps, M.; Stephens, J.; Wei, L.; Kassem, M.; Ling, Y.; Lustberg, M.; et al. A phase I study of an oral selective gamma secretase (GS) inhibitor RO4929097 in combination with neoadjuvant paclitaxel and carboplatin in triple negative breast cancer. Investig. New Drugs 2020, 38, 1400–1410. [Google Scholar] [CrossRef]
- Means-Powell, J.A.; Mayer, I.A.; Ismail-Khan, R.; Del Valle, L.; Tonetti, D.; Abramson, V.G.; Sanders, M.S.; Lush, R.M.; Sorrentino, C.; Majumder, S.; et al. A Phase Ib Dose Escalation Trial of RO4929097 (a γ-secretase inhibitor) in Combination with Exemestane in Patients with ER + Metastatic Breast Cancer (MBC). Clin. Breast Cancer 2021, 22, 103–114. [Google Scholar] [CrossRef] [PubMed]
- Wan, X.; Liu, C.; Lin, Y.; Fu, J.; Lu, G.; Lu, Z. pH sensitive peptide functionalized nanoparticles for co-delivery of erlotinib and DAPT to restrict the progress of triple negative breast cancer. Drug Deliv. 2019, 26, 470–480. [Google Scholar] [CrossRef]
- Paroni, G.; Zanetti, A.; Barzago, M.M.; Kurosaki, M.; Guarrera, L.; Fratelli, M.; Troiani, M.; Ubezio, P.; Bolis, M.; Vallerga, A.; et al. Retinoic Acid Sensitivity of Triple-Negative Breast Cancer Cells Characterized by Constitutive Activation of the notch1 Pathway: The Role of Rarβ. Cancers 2020, 12, 3027. [Google Scholar] [CrossRef] [PubMed]
- Sen, P.; Ghosh, S.S. γ-Secretase Inhibitor Potentiates the Activity of Suberoylanilide Hydroxamic Acid by Inhibiting Its Ability to Induce Epithelial to Mesenchymal Transition and Stemness via Notch Pathway Activation in Triple-Negative Breast Cancer Cells. ACS Pharmacol. Transl. Sci. 2023, 6, 1396–1415. [Google Scholar] [CrossRef]
- Sen, P.; Kandasamy, T.; Ghosh, S.S. Multi-targeting TACE/ADAM17 and gamma-secretase of notch signalling pathway in TNBC via drug repurposing approach using Lomitapide. Cell. Signal. 2022, 102, 110529. [Google Scholar] [CrossRef]
- Hossain, F.; Ucar, D.A.; Monticone, G.; Ran, Y.; Majumder, S.; Larter, K.; Luu, H.; Wyczechowska, D.; Heidari, S.; Xu, K.; et al. Sulindac sulfide as a non-immune suppressive γ-secretase modulator to target triple-negative breast cancer. Front. Immunol. 2023, 14, 1244159. [Google Scholar] [CrossRef] [PubMed]
- Yabuuchi, S.; Pai, S.G.; Campbell, N.R.; de Wilde, R.F.; De Oliveira, E.; Korangath, P.; Streppel, M.M.; Rasheed, Z.A.; Hidalgo, M.; Maitra, A.; et al. Notch signaling pathway targeted therapy suppresses tumor progression and metastatic spread in pancreatic cancer. Cancer Lett. 2013, 335, 41–51. [Google Scholar] [CrossRef] [PubMed]
- Palagani, V.; Bozko, P.; El Khatib, M.; Belahmer, H.; Giese, N.; Sipos, B.; Malek, N.P.; Plentz, R.R. Combined inhibition of Notch and JAK/STAT is superior to monotherapies and impairs pancreatic cancer progression. Carcinog. 2013, 35, 859–866. [Google Scholar] [CrossRef]
- Zhu, S.; Zhao, L.; Li, Y.; Hou, P.; Yao, R.; Tan, J.; Liu, D.; Han, L.; Huang, B.; Lu, J.; et al. Suppression of RAD21 Induces Senescence of MDA-MB-231 Human Breast Cancer Cells Through RB1 Pathway Activation Via c-Myc Downregulation. J. Cell. Biochem. 2015, 117, 1359–1369. [Google Scholar] [CrossRef]
- Mukherjee, A.; Kumar, B.; Hatano, K.; Russell, L.M.; Trock, B.J.; Searson, P.C.; Lupold, S.E. Development and Application of a Novel Model System to Study "Active" and "Passive" Tumor Targeting. Mol. Cancer Ther. 2016, 15, 2541–2550. [Google Scholar] [CrossRef]
- Hong, K.; Wu, D.; Cheng, K.; Chen, L.; Hung, W. RECK Inhibits Stemness Gene Expression and Tumorigenicity of Gastric Cancer Cells by Suppressing ADAM-Mediated Notch1 Activation. J. Cell. Physiol. 2013, 229, 191–201. [Google Scholar] [CrossRef]
- Sen, P.; Ghosh, S.S. The Intricate Notch Signaling Dynamics in Therapeutic Realms of Cancer. ACS Pharmacol. Transl. Sci. 2023, 6, 651–670. [Google Scholar] [CrossRef]
- Li, S.-Y.; Sun, R.; Wang, H.-X.; Shen, S.; Liu, Y.; Du, X.-J.; Zhu, Y.-H.; Jun, W. Combination therapy with epigenetic-targeted and chemotherapeutic drugs delivered by nanoparticles to enhance the chemotherapy response and overcome resistance by breast cancer stem cells. J. Control. Release 2015, 205, 7–14. [Google Scholar] [CrossRef]
- Nueda, M.; Naranjo, A.; Baladrón, V.; Laborda, J. Different expression levels of DLK1 inversely modulate the oncogenic potential of human MDA-MB-231 breast cancer cells through inhibition of NOTCH1 signaling. FASEB J. 2017, 31, 3484–3496. [Google Scholar] [CrossRef]
- Zhou, Y.; Guan, L.; Li, W.; Jia, R.; Jia, L.; Zhang, Y.; Wen, X.; Meng, S.; Ma, D.; Zhang, N.; et al. DT7 peptide-modified lecithin nanoparticles co-loaded with γ-secretase inhibitor and dexamethasone efficiently inhibit T-cell acute lymphoblastic leukemia and reduce gastrointestinal toxicity. Cancer Lett. 2022, 533, 215608. [Google Scholar] [CrossRef]

| GSI | Type of Cancer | Type of Study | Main Results | Reference |
|---|---|---|---|---|
| MRK003 | PDAC | In vivo (xenograft) +/- gemcitabine | The combination blocked tumor progression | [59,77] |
| TNBC |
In vitro e in vivo + placitaxel |
Greater antitumor activity of the combination in cells with higher NICD levels | [110] | |
| GSI-IX | PDAC |
In vivo (xenograft) + AG-490 |
Mice treated with the combination showed no visible tumors | [78] |
| GC | In vitro, in CD44+ cells | Smaller tumor spheres and increased apoptosis | [93] | |
| In vivo (xenograft) | Reduced tumor growth and increased necrosis | |||
| GSI-X | METASTATIC MELANOMA | In vitro | GSI decreased CD133+ cells (MSCs) | [98] |
| PF-03084014 (Nirogacestat) | PDAC |
In vivo (xenograft) +/- gemcitabine |
Only in combination did it show antiproliferative activity and reduce cancer stem cells | [76,79] |
| METASTATIC MELANOMA | In vitro + MEKi | The combination was more effective in stopping proliferation and migration | [99] | |
| DAPT | NSCLC | In vitro + cisplatin | Decrease in the appearance of CD133+, ALDH+ LCSC cells, with lower resistance to cisplatin | [85] |
| GC | In vitro | Inhibited the formation of GCSC-rich spheres by 25% | 91 | |
| In vitro, in CD44+ and CD44− cells | CD44+ cells, behaving as GCSCs, showed greater antitumor response to GSI | [92] |
||
| In vivo (xenograft) | Significant inhibition of tumor growth and EMT | |||
|
In vitro +/- PD98059 In vivo (xenograft) +/- PD98059 |
Reduced tumor growth and increased apoptosis in combination | [96] | ||
| In vitro +/- anti-DLL4 | Significant increase in apoptosis and reduced invasion and tumor size | [97] | ||
| METASTATIC MELANOMA |
In vivo (xenograft) +/- BRAFi |
Reversal of melanoma cell resistance to BRAFi | [100] | |
|
In vitro +/- DLK1 and/or DLK2 levels |
Dose-dependent effect of DAPT: decreased proliferation at high doses, increased at low doses. The combination reduced cell proliferation | [103] | ||
| In vitro e In vivo (Xenograft) | Long-term use of DAPT increased tumor growth | [104] | ||
| TNBC | In vitro, in BCSCs cells | Reduced proliferation and increased apoptosis | [109] | |
| In vivo (xenograft) | Delay in tumor formation and reduced subsequent growth | |||
|
In vivo (xenograft) + Erlotinib + Director peptide |
The nanoparticle reduced tumor growth and cell migration | [116] | ||
| In vitro + ATRA | The combination was more effective in inhibiting tumor growth | [117] | ||
| GSI-34 | NSCLC |
In vivo (xenograft) with CD166+Lin− LCSC cells +/- cisplatin |
CD166+Lin- showed intrinsic resistance to cisplatin, which was reversed with GSI. The combination effectively reduced tumor size | [82] |
| BMS-708163 | NSCLC |
In vitro, in NSCLC-gefitinb resistant cells + gefitinib |
High doses of GSI reversed resistance to gefitinib and formed smaller colonies | [86] |
|
In vivo (xenograft) + gefitinib |
The combination produced considerable inhibition of tumor growth | |||
| BMS-906024 |
In vitro, in NSCLC cells + RT +/- placitaxel y crizotinib |
Monotherapy + RT did not show significant reduction. It was observed with the combination | [84] | |
|
In vivo (xenograft) + placitaxel |
The combination enhanced the cytotoxic effect of paclitaxel | [83,87] | ||
| GSI-XX |
In vivo (xenograft) + RT |
The combination caused a significant delay in tumor growth | [88] | |
| GSI-I | In vitro + RT | Higher level of apoptosis than isolated RT | [88] | |
| GC |
In vitro and in vivo (xenograft) + placitaxel or 5-FU |
Increased activity of PTEN, a tumor suppressor gene. Both combinations were more effective than monotherapy |
[94] | |
| METASTATIC MELANOMA |
In vivo (xenofraft) and in vitro + BCL2i |
The combination was more effective than monotherapy | [102] | |
| RO4929097 | In vitro + ERKi | Sensitization to ERKi in cell lines that did not respond to it in monotherapy | [101] | |
| In vivo (xenograft) +ERKi | The combination was more effective than monotherapy | |||
| In vitro + RT | Synergism at low doses in combination | [107] | ||
| TNBC | In vitro, in CD24 low and CD24− (BCSCs) cells | Inhibition of CD24low sphere growth | [64,114] | |
| In vivo (xenograft) with CD24 low and CD24− (BCSCs) cells | Halted tumor growth and metastasis in CD24 low models | |||
| MK-0752 |
In vitro. Different levels of NOTCH expression + METi |
The combination showed synergism in halting cell growth | [111] | |
| In vivo (xenograft) | Injecting BCSC cells treated with GSI did not reproduce the tumor | [112] | ||
| LY411575 | In vitro + SAHA | SAHA in monotherapy was seen to promote EMT. The combination reduced EMT and increased apoptosis | [68] | |
|
OTHERS (Evodiamina) |
NSCLC | In vitro | Not a GSI but behaves like one. It reduced cell proliferation and metastasis | [89] |
|
OTHERS (NSAID sulindac (SS)) |
TNBC | In vitro, in vivo and ex vivo | Significantly inhibited nanosphere growth in all human and murine TNBC models. Eliminated NOTCH1 protein expression in tumors | [120] |
|
OTHERS (Lomitapide) |
In vitro | Multi-targeting TACE/ADAM17 and gamma-secretase complex of NOTCH signaling pathway | [119] |
| Type of Cancer | GSI | Phase | Results | Reference |
|---|---|---|---|---|
| PDAC | MK-0752 + gemcitabine |
I | 14 out of 44 patients reached a stable condition, in both monotherapy and combination therapy. Gastrointestinal disorders and anemia were observed | [80] |
| RO4929097 | II | The trial could not be completed because GSI synthesis was discontinued | [81] | |
| METASTATIC MELANOMA | RO4929097 | I | In two groups of 110 patients, 33% and 41% reached a stable condition. Hypophosphatemia was noted | [105] |
| RO4929097 | II | Of 32 evaluated patients, 1 had a partial response and 8 reached a stable condition. Hypophosphatemia was also observed |
[106] |
|
| TNBC | MK-0752 + docetaxel |
I | Among 24 patients, 11 had a partial response, 9 reached a stable condition, and 3 showed tumor progression. There was one case of severe pneumonitis. | [112] |
| PF-03084014 + docetaxel |
I | 29 women showed limited treatment efficacy, with severe hematologic and infectious reactions | [113] | |
| RO4929097 + placitaxel + carboplatin |
I | Of 14 evaluated patients, 5 had a partial response, 4 reached a stable condition, and 5 had residual disease. Neutropenia was reported | [64,114] | |
| EPBCm | RO4929097 + exemestane |
Ib | Among 14 evaluated patients, 7 had a partial response and 7 reached a stable condition | [115] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).





