Submitted:
01 November 2025
Posted:
04 November 2025
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
2.1. Animals
2.2. Recombinant Adeno-Associated Virus (rAAV) Vector Production
2.3. Intra-SDH Injection of rAAV Vectors
2.4. Intra-S1 Injection of rAAV Vectors
2.5. Immunohistochemistry
2.6. Neuropathic Pain Model and Behavioral Assays
2.7. Chemogenetic Manipulation of S1→SDH Neurons
2.8. Whole-Cell Patch-Clamp Recordings
2.9. Administration of Diphtheria Toxin (DTX)
2.10. Statistical Analysis
3. Results
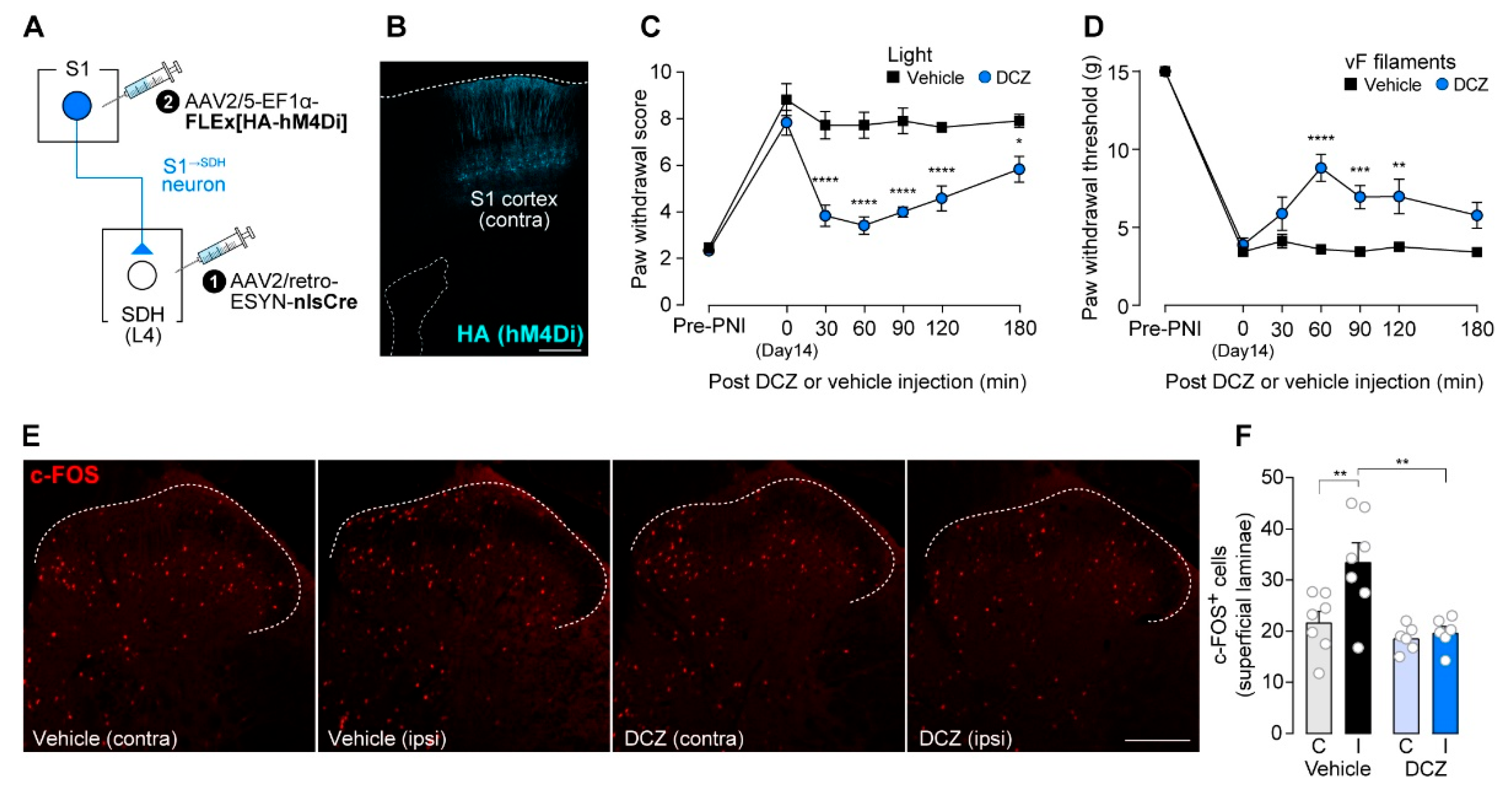
3.1. S1→SDH Neurons Contribute to Aβ Fiber-Derived Neuropathic Allodynia in Rats
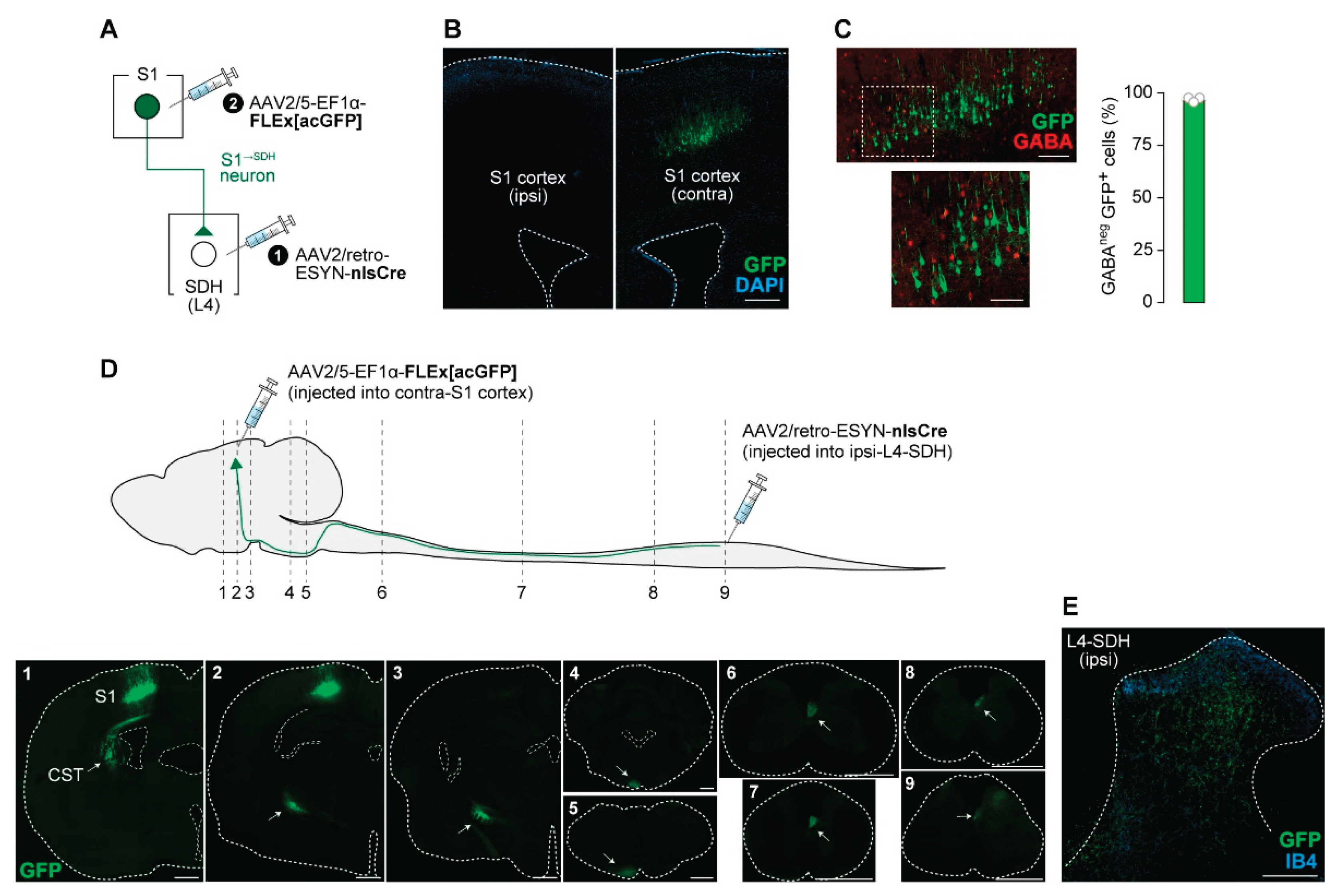
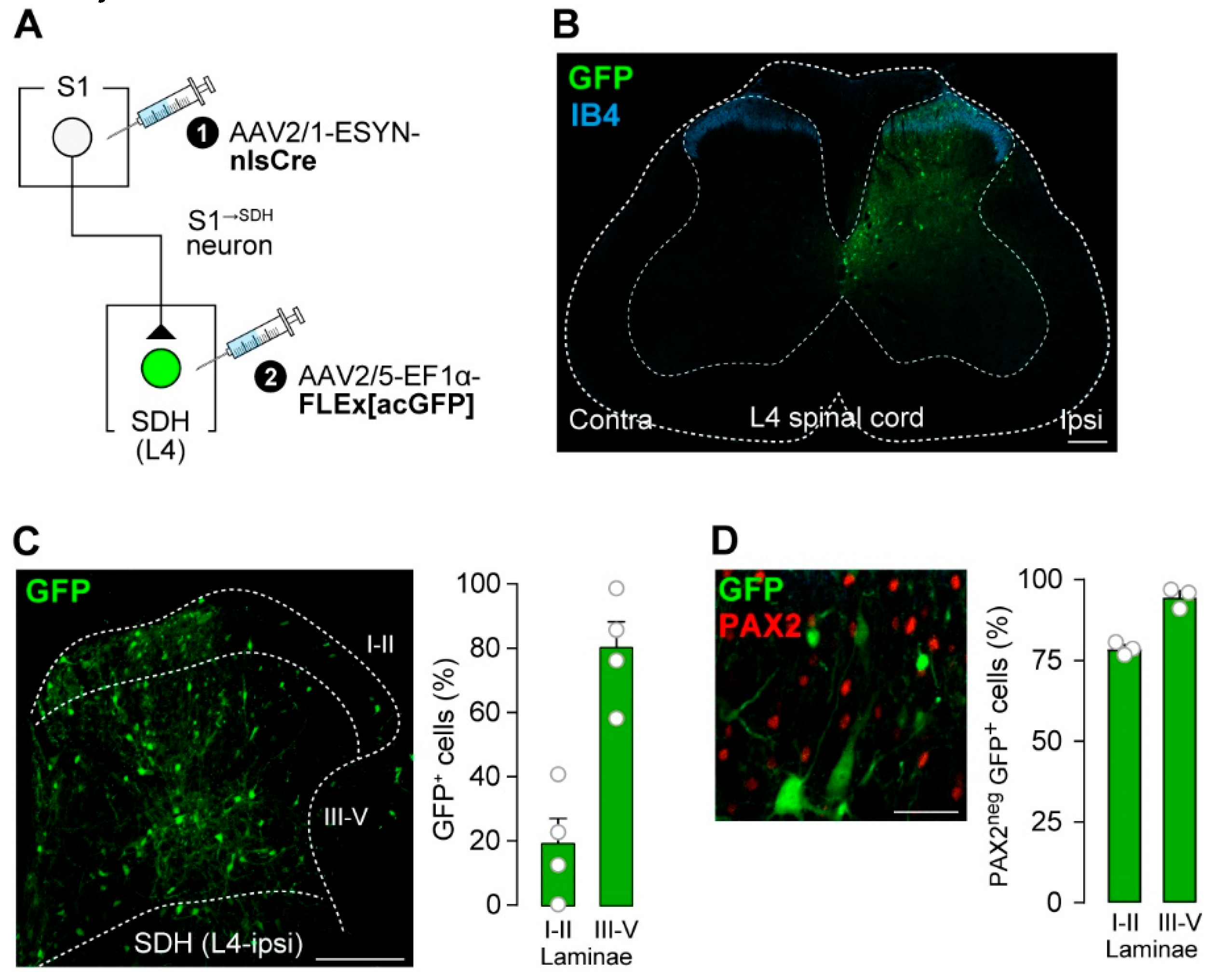
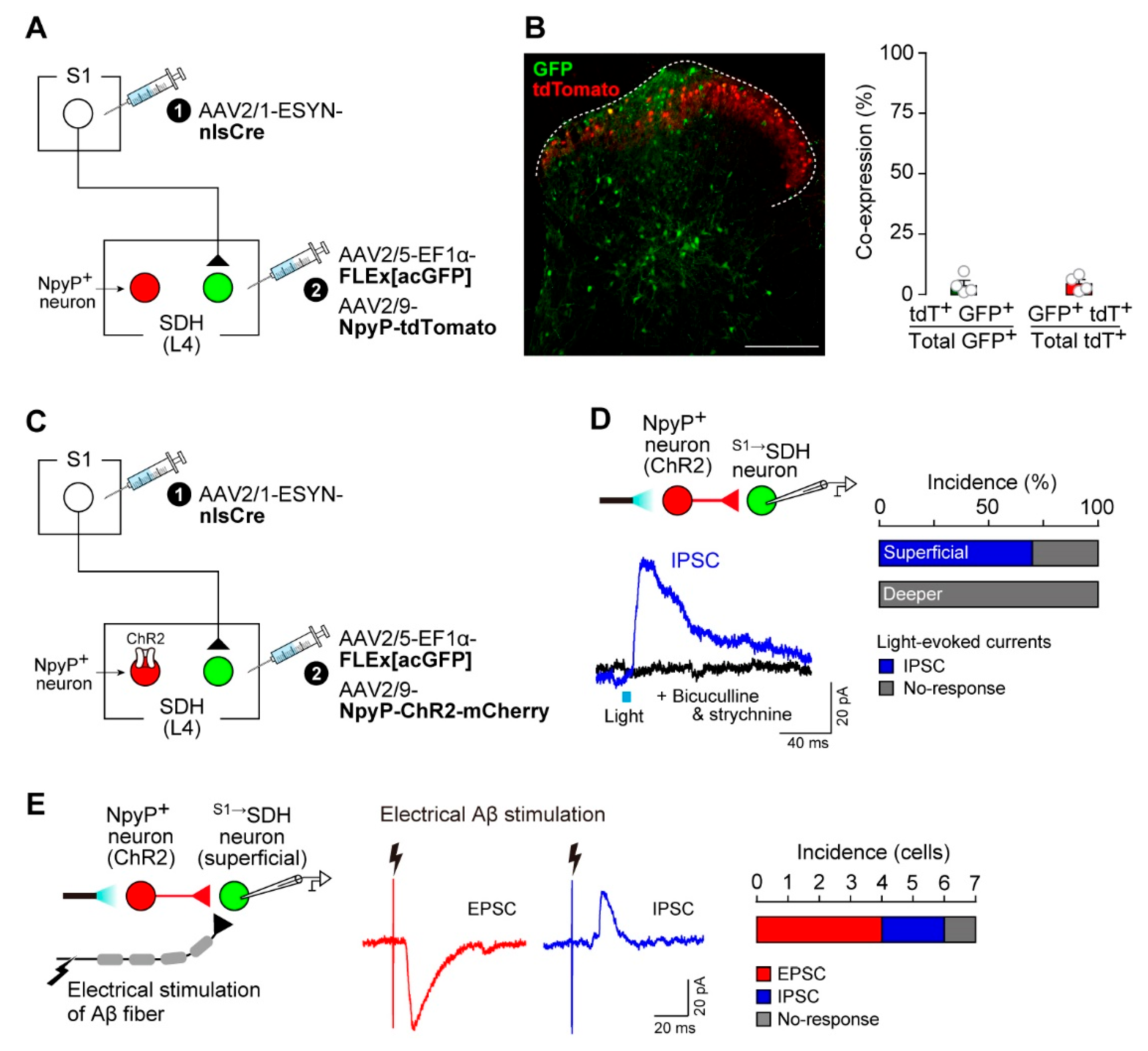
3.2. S1→SDH Neurons Form Synaptic Connections with SDH Neurons That Receive Aβ Fiber Input

3.3. Impact of S1→SDH Neuron Signaling on Allodynia Is Unmasked Under Pathological Conditions
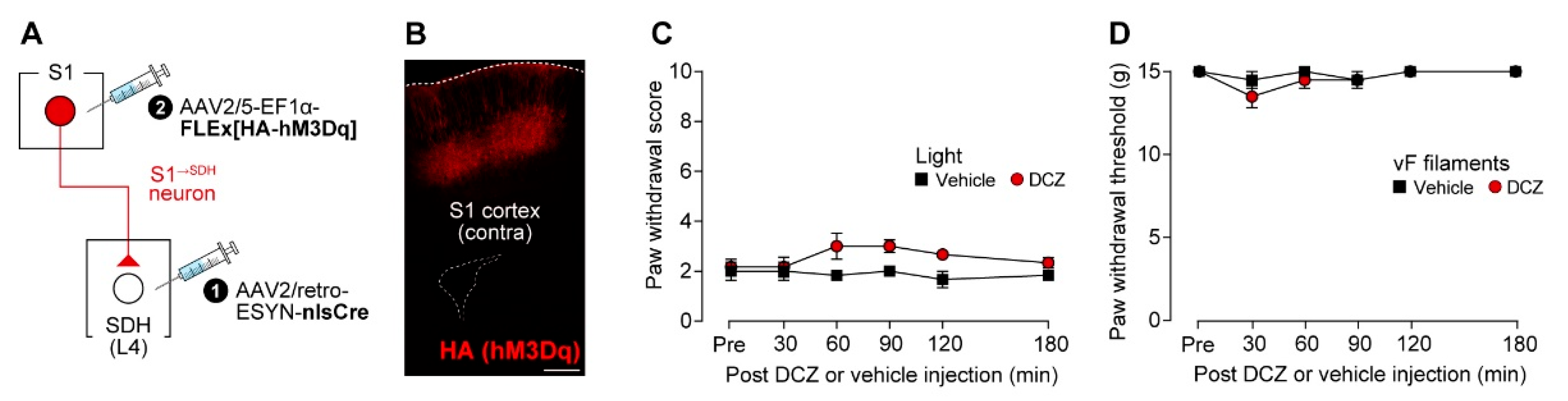

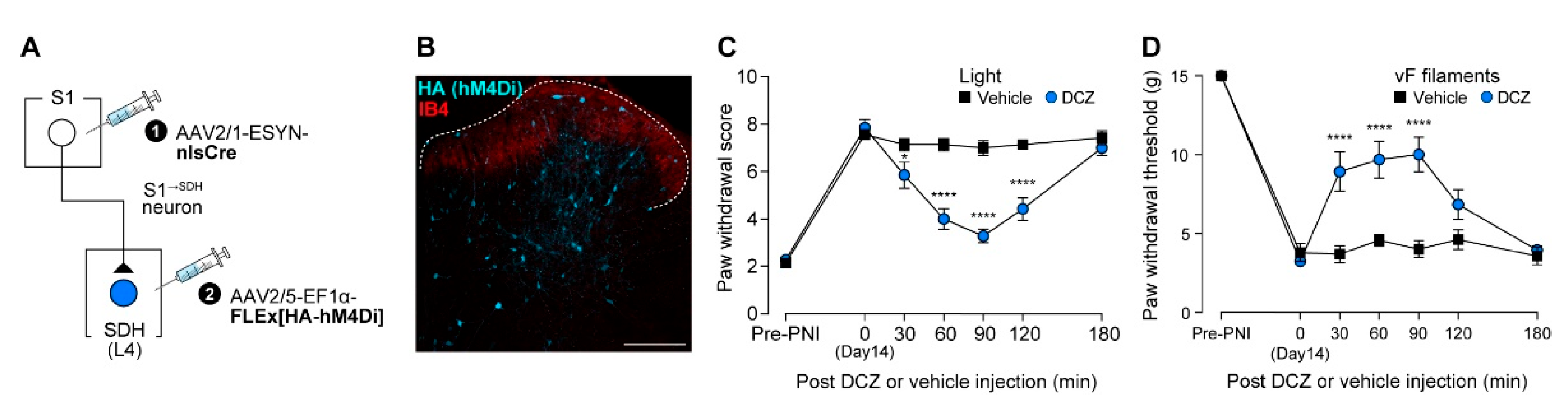
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| PNI | Peripheral nerve injury |
| SDH | Spinal dorsal horn |
| S1 | Primary somatosensory |
| S1→SDH neurons | Descending neurons projecting directly from the S1 cortex to the SDH |
| S1→SDH neurons | SDH neurons directly receiving projections from S1 |
| NpyP | Neuropeptide Y promoter |
| LTMRs | Low-threshold mechanoreceptors |
| ChR2 | Channelrhodopsin-2 |
| AAV | Adeno-associated virus |
| ACC | Anterior cingulate cortex |
| IC | Insular cortex |
| TRECK | Toxin receptor–mediated cell knockout |
| rAAV | Recombinant adeno-associated virus |
| DTR | Diphtheria toxin receptor |
| HA | Hemagglutinin |
| hM4Di | Human muscarinic Gi-coupled receptor |
| hM3Dq | Human muscarinic Gq-coupled receptor |
| GFP | Green fluorescent protein |
| acGFP | Aequorea coerulescens GFP |
| ESYN | Enhanced synapsin |
| EF1α | Elongation factor 1α |
| WPRE | Woodchuck hepatitis virus post-transcriptional response element |
| HEK293T | Human embryonic kidney 293T |
| PBS | Phosphate-buffered saline |
| i.p. | Intraperitoneal |
| Th12 | The twelfth thoracic |
| L4 | The fourth lumbar |
| GC | Genome copy |
| AP | Anteroposterior |
| ML | Mediolateral |
| DV | Dorsoventral |
| PFA | Paraformaldehyde |
| IB4 | Isolectin B4 |
| GABA | γ-aminobutyric acid |
| PAX2 | Paired box 2 |
| DAPI | 4′,6-diamidino-2-phenylindole |
| DCZ | Deschloroclozapine |
| DMSO | Dimethyl sulfoxide |
| NMDG | N-Methyl-D-glucamine |
| aCSF | Artificial cerebrospinal fluid |
| EPSCs | Excitatory postsynaptic currents |
| IPSCs | Inhibitory postsynaptic currents |
| DTX | Diphtheria toxin |
| SEM | Standard error of the mean |
| CST | Corticospinal tract |
| DREADD | Designer receptors exclusively activated by designer drugs |
| E/I | Excitatory/Inhibitory |
References
- Colloca, L.; Ludman, T.; Bouhassira, D.; Baron, R.; Dickenson, A.H.; Yarnitsky, D.; Freeman, R.; Truini, A.; Attal, N.; Finnerup, N.B.; et al. Neuropathic pain. Nature reviews. Disease primers 2017, 3, 17002. [CrossRef]
- Soliman, N.; Moisset, X.; Ferraro, M.C.; de Andrade, D.C.; Baron, R.; Belton, J.; Bennett, D.L.H.; Calvo, M.; Dougherty, P.; Gilron, I.; et al. Pharmacotherapy and non-invasive neuromodulation for neuropathic pain: a systematic review and meta-analysis. The Lancet. Neurology 2025, 24, 413-428. [CrossRef]
- Todd, A.J. Neuronal circuitry for pain processing in the dorsal horn. Nature reviews. Neuroscience 2010, 11, 823-836. [CrossRef]
- Peirs, C.; Seal, R.P. Neural circuits for pain: Recent advances and current views. Science (New York, N.Y.) 2016, 354, 578-584. [CrossRef]
- Tsuda, M. New approach for investigating neuropathic allodynia by optogenetics. Pain 2019, 160 Suppl 1, S53-s58. [CrossRef]
- Koch, S.C.; Acton, D.; Goulding, M. Spinal Circuits for Touch, Pain, and Itch. Annual review of physiology 2018, 80, 189-217. [CrossRef]
- Moehring, F.; Halder, P.; Seal, R.P.; Stucky, C.L. Uncovering the Cells and Circuits of Touch in Normal and Pathological Settings. Neuron 2018, 100, 349-360. [CrossRef]
- Peirs, C.; Dallel, R.; Todd, A.J. Recent advances in our understanding of the organization of dorsal horn neuron populations and their contribution to cutaneous mechanical allodynia. Journal of neural transmission (Vienna, Austria : 1996) 2020, 127, 505-525. [CrossRef]
- Kuner, R.; Flor, H. Structural plasticity and reorganisation in chronic pain. Nature reviews. Neuroscience 2016, 18, 20-30. [CrossRef]
- Hughes, D.I.; Todd, A.J. Central Nervous System Targets: Inhibitory Interneurons in the Spinal Cord. Neurotherapeutics : the journal of the American Society for Experimental NeuroTherapeutics 2020, 17, 874-885. [CrossRef]
- Tashima, R.; Koga, K.; Sekine, M.; Kanehisa, K.; Kohro, Y.; Tominaga, K.; Matsushita, K.; Tozaki-Saitoh, H.; Fukazawa, Y.; Inoue, K.; et al. Optogenetic Activation of Non-Nociceptive Aβ Fibers Induces Neuropathic Pain-Like Sensory and Emotional Behaviors after Nerve Injury in Rats. eNeuro 2018, 5. [CrossRef]
- Tashima, R.; Koga, K.; Yoshikawa, Y.; Sekine, M.; Watanabe, M.; Tozaki-Saitoh, H.; Furue, H.; Yasaka, T.; Tsuda, M. A subset of spinal dorsal horn interneurons crucial for gating touch-evoked pain-like behavior. Proceedings of the National Academy of Sciences of the United States of America 2021, 118. [CrossRef]
- Ji, Z.G.; Ito, S.; Honjoh, T.; Ohta, H.; Ishizuka, T.; Fukazawa, Y.; Yawo, H. Light-evoked somatosensory perception of transgenic rats that express channelrhodopsin-2 in dorsal root ganglion cells. PloS one 2012, 7, e32699. [CrossRef]
- Koga, K.; Descalzi, G.; Chen, T.; Ko, H.G.; Lu, J.; Li, S.; Son, J.; Kim, T.; Kwak, C.; Huganir, R.L.; et al. Coexistence of two forms of LTP in ACC provides a synaptic mechanism for the interactions between anxiety and chronic pain. Neuron 2015, 85, 377-389. [CrossRef]
- Chen, T.; Taniguchi, W.; Chen, Q.Y.; Tozaki-Saitoh, H.; Song, Q.; Liu, R.H.; Koga, K.; Matsuda, T.; Kaito-Sugimura, Y.; Wang, J.; et al. Top-down descending facilitation of spinal sensory excitatory transmission from the anterior cingulate cortex. Nature communications 2018, 9, 1886. [CrossRef]
- Song, Q.; Wei, A.; Xu, H.; Gu, Y.; Jiang, Y.; Dong, N.; Zheng, C.; Wang, Q.; Gao, M.; Sun, S.; et al. An ACC-VTA-ACC positive-feedback loop mediates the persistence of neuropathic pain and emotional consequences. Nature neuroscience 2024, 27, 272-285. [CrossRef]
- Chen, J.; Gao, Y.; Bao, S.T.; Wang, Y.D.; Jia, T.; Yin, C.; Xiao, C.; Zhou, C. Insula→Amygdala and Insula→Thalamus Pathways Are Involved in Comorbid Chronic Pain and Depression-Like Behavior in Mice. The Journal of neuroscience : the official journal of the Society for Neuroscience 2024, 44. [CrossRef]
- Liu, Y.; Latremoliere, A.; Li, X.; Zhang, Z.; Chen, M.; Wang, X.; Fang, C.; Zhu, J.; Alexandre, C.; Gao, Z.; et al. Touch and tactile neuropathic pain sensitivity are set by corticospinal projections. Nature 2018, 561, 547-550. [CrossRef]
- Danjo, Y.; Shigetomi, E.; Hirayama, Y.J.; Kobayashi, K.; Ishikawa, T.; Fukazawa, Y.; Shibata, K.; Takanashi, K.; Parajuli, B.; Shinozaki, Y.; et al. Transient astrocytic mGluR5 expression drives synaptic plasticity and subsequent chronic pain in mice. The Journal of experimental medicine 2022, 219. [CrossRef]
- Basbaum, A.I.; Clanton, C.H.; Fields, H.L. Opiate and stimulus-produced analgesia: functional anatomy of a medullospinal pathway. Proceedings of the National Academy of Sciences of the United States of America 1976, 73, 4685-4688. [CrossRef]
- Basbaum, A.I.; Fields, H.L. The origin of descending pathways in the dorsolateral funiculus of the spinal cord of the cat and rat: further studies on the anatomy of pain modulation. The Journal of comparative neurology 1979, 187, 513-531. [CrossRef]
- Leong, S.K.; Shieh, J.Y.; Wong, W.C. Localizing spinal-cord-projecting neurons in adult albino rats. The Journal of comparative neurology 1984, 228, 1-17. [CrossRef]
- Nudo, R.J.; Masterton, R.B. Descending pathways to the spinal cord: a comparative study of 22 mammals. The Journal of comparative neurology 1988, 277, 53-79. [CrossRef]
- Liang, H.; Paxinos, G.; Watson, C. Projections from the brain to the spinal cord in the mouse. Brain structure & function 2011, 215, 159-186. [CrossRef]
- Wang, Z.; Maunze, B.; Wang, Y.; Tsoulfas, P.; Blackmore, M.G. Global Connectivity and Function of Descending Spinal Input Revealed by 3D Microscopy and Retrograde Transduction. The Journal of neuroscience : the official journal of the Society for Neuroscience 2018, 38, 10566-10581. [CrossRef]
- Winter, C.C.; Jacobi, A.; Su, J.; Chung, L.; van Velthoven, C.T.J.; Yao, Z.; Lee, C.; Zhang, Z.; Yu, S.; Gao, K.; et al. A transcriptomic taxonomy of mouse brain-wide spinal projecting neurons. Nature 2023, 624, 403-414. [CrossRef]
- Xie, J.; Feng, R.; Chen, Y.; Gao, L. Morphological analysis of descending tracts in mouse spinal cord using tissue clearing, tissue expansion and tiling light sheet microscopy techniques. Scientific reports 2023, 13, 16445. [CrossRef]
- Fujimori, K.; Sekine, M.; Watanabe, M.; Tashima, R.; Tozaki-Saitoh, H.; Tsuda, M. Chemogenetic silencing of spinal cord-projecting cortical neurons attenuates Aβ fiber-derived neuropathic allodynia in mice. Neuroscience research 2022, 181, 115-119. [CrossRef]
- Saito, M.; Iwawaki, T.; Taya, C.; Yonekawa, H.; Noda, M.; Inui, Y.; Mekada, E.; Kimata, Y.; Tsuru, A.; Kohno, K. Diphtheria toxin receptor-mediated conditional and targeted cell ablation in transgenic mice. Nature biotechnology 2001, 19, 746-750. [CrossRef]
- Tomita, H.; Sugano, E.; Fukazawa, Y.; Isago, H.; Sugiyama, Y.; Hiroi, T.; Ishizuka, T.; Mushiake, H.; Kato, M.; Hirabayashi, M.; et al. Visual properties of transgenic rats harboring the channelrhodopsin-2 gene regulated by the thy-1.2 promoter. PloS one 2009, 4, e7679. [CrossRef]
- Kohro, Y.; Sakaguchi, E.; Tashima, R.; Tozaki-Saitoh, H.; Okano, H.; Inoue, K.; Tsuda, M. A new minimally-invasive method for microinjection into the mouse spinal dorsal horn. Scientific reports 2015, 5, 14306. [CrossRef]
- Kawanabe-Kobayashi, R.; Uchiyama, S.; Yoshihara, K.; Koga, K.; Kojima, D.; McHugh, T.; Hatada, I.; Matsui, K.; Tanaka, K.F.; Tsuda, M. Descending locus coeruleus noradrenergic signaling to spinal astrocyte subset is required for stress-induced mechanical pain hypersensitivity. bioRxiv 2025, 10.1101/2024.11.14.623627, 2024.2011.2014.623627. [CrossRef]
- Ho Kim, S.; Mo Chung, J. An experimental model for peripheral neuropathy produced by segmental spinal nerve ligation in the rat. Pain 1992, 50, 355-363. [CrossRef]
- Tsuda, M.; Shigemoto-Mogami, Y.; Koizumi, S.; Mizokoshi, A.; Kohsaka, S.; Salter, M.W.; Inoue, K. P2X4 receptors induced in spinal microglia gate tactile allodynia after nerve injury. Nature 2003, 424, 778-783. [CrossRef]
- Tsuda, M.; Kohro, Y.; Yano, T.; Tsujikawa, T.; Kitano, J.; Tozaki-Saitoh, H.; Koyanagi, S.; Ohdo, S.; Ji, R.R.; Salter, M.W.; et al. JAK-STAT3 pathway regulates spinal astrocyte proliferation and neuropathic pain maintenance in rats. Brain : a journal of neurology 2011, 134, 1127-1139. [CrossRef]
- Sueto, D.; I, E.; Onishi, A.; Tsuda, M. Spinal dorsal horn neurons involved in the alleviating effects of cannabinoid receptor agonists on neuropathic allodynia-like behaviors in rats. Journal of pharmacological sciences 2025, 157, 253-260. [CrossRef]
- Petreanu, L.; Huber, D.; Sobczyk, A.; Svoboda, K. Channelrhodopsin-2-assisted circuit mapping of long-range callosal projections. Nature neuroscience 2007, 10, 663-668. [CrossRef]
- Honsek, S.D.; Seal, R.P.; Sandkühler, J. Presynaptic inhibition of optogenetically identified VGluT3+ sensory fibres by opioids and baclofen. Pain 2015, 156, 243-251. [CrossRef]
- Roth, B.L. DREADDs for Neuroscientists. Neuron 2016, 89, 683-694. [CrossRef]
- Ishibashi, T.; Yoshikawa, Y.; Sueto, D.; Tashima, R.; Tozaki-Saitoh, H.; Koga, K.; Yamaura, K.; Tsuda, M. Selective Involvement of a Subset of Spinal Dorsal Horn Neurons Operated by a Prodynorphin Promoter in Aβ Fiber-Mediated Neuropathic Allodynia-Like Behavioral Responses in Rats. Frontiers in molecular neuroscience 2022, 15, 911122. [CrossRef]
- Nagai, Y.; Miyakawa, N.; Takuwa, H.; Hori, Y.; Oyama, K.; Ji, B.; Takahashi, M.; Huang, X.P.; Slocum, S.T.; DiBerto, J.F.; et al. Deschloroclozapine, a potent and selective chemogenetic actuator enables rapid neuronal and behavioral modulations in mice and monkeys. Nature neuroscience 2020, 23, 1157-1167. [CrossRef]
- Cheng, L.; Samad, O.A.; Xu, Y.; Mizuguchi, R.; Luo, P.; Shirasawa, S.; Goulding, M.; Ma, Q. Lbx1 and Tlx3 are opposing switches in determining GABAergic versus glutamatergic transmitter phenotypes. Nature neuroscience 2005, 8, 1510-1515. [CrossRef]
- Koga, K.; Kanehisa, K.; Kohro, Y.; Shiratori-Hayashi, M.; Tozaki-Saitoh, H.; Inoue, K.; Furue, H.; Tsuda, M. Chemogenetic silencing of GABAergic dorsal horn interneurons induces morphine-resistant spontaneous nocifensive behaviours. Scientific reports 2017, 7, 4739. [CrossRef]
- Yasaka, T.; Tiong, S.Y.X.; Hughes, D.I.; Riddell, J.S.; Todd, A.J. Populations of inhibitory and excitatory interneurons in lamina II of the adult rat spinal dorsal horn revealed by a combined electrophysiological and anatomical approach. Pain 2010, 151, 475-488. [CrossRef]
- Mercer Lindsay, N.; Chen, C.; Gilam, G.; Mackey, S.; Scherrer, G. Brain circuits for pain and its treatment. Science translational medicine 2021, 13, eabj7360. [CrossRef]
- Kim, S.K.; Nabekura, J. Rapid synaptic remodeling in the adult somatosensory cortex following peripheral nerve injury and its association with neuropathic pain. The Journal of neuroscience : the official journal of the Society for Neuroscience 2011, 31, 5477-5482. [CrossRef]
- Kim, S.K.; Hayashi, H.; Ishikawa, T.; Shibata, K.; Shigetomi, E.; Shinozaki, Y.; Inada, H.; Roh, S.E.; Kim, S.J.; Lee, G.; et al. Cortical astrocytes rewire somatosensory cortical circuits for peripheral neuropathic pain. The Journal of clinical investigation 2016, 126, 1983-1997. [CrossRef]
- Takeda, I.; Yoshihara, K.; Cheung, D.L.; Kobayashi, T.; Agetsuma, M.; Tsuda, M.; Eto, K.; Koizumi, S.; Wake, H.; Moorhouse, A.J.; et al. Controlled activation of cortical astrocytes modulates neuropathic pain-like behaviour. Nature communications 2022, 13, 4100. [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).




