Submitted:
08 April 2025
Posted:
11 April 2025
You are already at the latest version
Abstract
Keywords:
1. Introduction
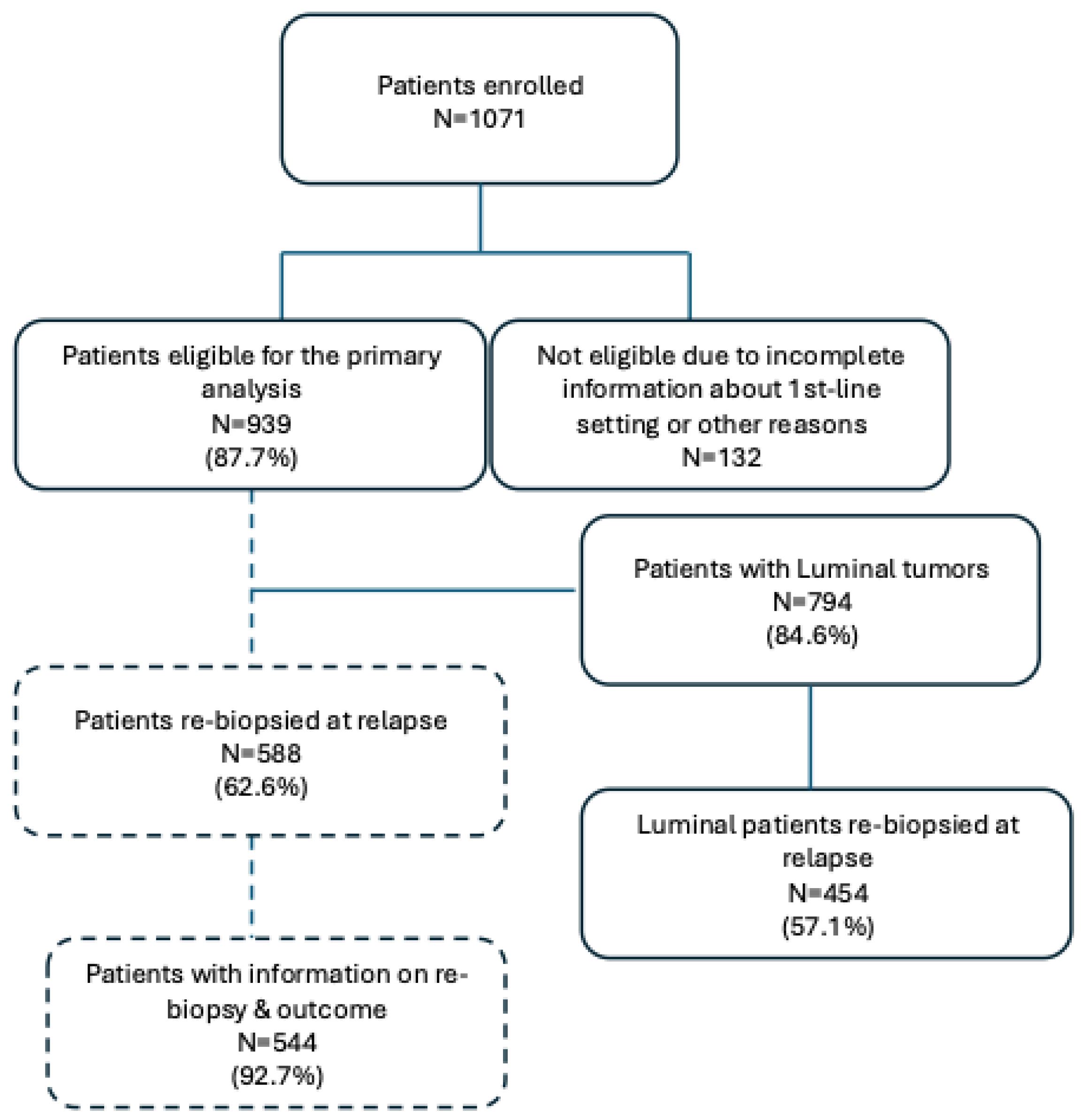
2. Patients and Methods
2.1. Study Design
2.2. Objectives
2.3. Statistical Analysis
3. Results
3.1. Patients’ and Tumor Characteristics at First Relapse
4. Discussion
Declaration of Interest
Supplementary Materials
Acknowledgments
References
- H. Sung et al., “Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries,” CA Cancer J Clin, vol. 71, no. 3, pp. 209–249, May 2021. [CrossRef]
- “Cos’è il Cancro | AIRC.” Accessed: Apr. 04, 2025. [Online]. Available: https://www.airc.it/cancro/informazioni-tumori/cose-il-cancro/numeri-del-cancro.
- T. Sørlie et al., “Gene expression patterns of breast carcinomas distinguish tumor subclasses with clinical implications,” Proc Natl Acad Sci U S A, vol. 98, no. 19, pp. 10869–10874, Sep. 2001. [CrossRef]
- K. H. Allison, “Prognostic and predictive parameters in breast pathology: a pathologist’s primer,” Modern Pathology, vol. 34, pp. 94–106, Jan. 2021. [CrossRef]
- G. Curigliano et al., “De-escalating and escalating treatments for early-stage breast cancer: the St. Gallen International Expert Consensus Conference on the Primary Therapy of Early Breast Cancer 2017,” Ann Oncol, vol. 28, no. 8, pp. 1700–1712, Aug. 2017. [CrossRef]
- Gennari et al., “ESMO Clinical Practice Guideline for the diagnosis, staging and treatment of patients with metastatic breast cancer 5 behalf of the ESMO Guidelines Committee,” Annals of Oncology, vol. 32, pp. 1475–1495, 2021. [CrossRef]
- D. J. Slamon et al., “Overall Survival With Palbociclib Plus Letrozole in Advanced Breast Cancer,” J Clin Oncol, vol. 42, no. 9, pp. 994–1000, Mar. 2024. [CrossRef]
- G. N. Hortobagyi et al., “Overall Survival with Ribociclib plus Letrozole in Advanced Breast Cancer,” N Engl J Med, vol. 386, no. 10, pp. 942–950, Mar. 2022. [CrossRef]
- M. P. Goetz et al., “Abemaciclib plus a nonsteroidal aromatase inhibitor as initial therapy for HR+, HER2- advanced breast cancer: final overall survival results of MONARCH 3,” Ann Oncol, vol. 35, no. 8, pp. 718–727, Aug. 2024. [CrossRef]
- Y. S. Lu et al., “Updated Overall Survival of Ribociclib plus Endocrine Therapy versus Endocrine Therapy Alone in Pre- and Perimenopausal Patients with HR+/HER2- Advanced Breast Cancer in MONALEESA-7: A Phase III Randomized Clinical Trial,” Clin Cancer Res, vol. 28, no. 5, pp. 851–859, Mar. 2022. [CrossRef]
- M. Robson et al., “Olaparib for Metastatic Breast Cancer in Patients with a Germline BRCA Mutation,” N Engl J Med, vol. 377, no. 6, pp. 523–533, Aug. 2017. [CrossRef]
- M. E. Robson et al., “OlympiAD final overall survival and tolerability results: Olaparib versus chemotherapy treatment of physician’s choice in patients with a germline BRCA mutation and HER2-negative metastatic breast cancer,” Annals of Oncology, vol. 30, no. 4, pp. 558–566, Apr. 2019. [CrossRef]
- P. Schmid et al., “Pembrolizumab for Early Triple-Negative Breast Cancer,” New England Journal of Medicine, vol. 382, no. 9, pp. 810–821, Feb. 2020. [CrossRef]
- W. A. M. E. Schrijver, K. P. M. Suijkerbuijk, C. H. Van Gils, E. Van Der Wall, C. B. Moelans, and P. J. Van Diest, “Receptor Conversion in Distant Breast Cancer Metastases: A Systematic Review and Meta-analysis,” J Natl Cancer Inst, vol. 110, no. 6, pp. 568–580, Jun. 2018. [CrossRef]
- Kolberg-Liedtke et al., “Phenotype Discordance between Primary Tumor and Metastasis Impacts Metastasis Site and Outcome: Results of WSG-DETECT-PriMet,” Breast Care (Basel), vol. 16, no. 5, pp. 475–483, Oct. 2021. [CrossRef]
- M. E. Cazzaniga et al., “Clinical Outcomes of HER2-Negative Metastatic Breast Cancer Patients in Italy in the Last Decade: Results of the GIM 13-AMBRA Study,” Cancers (Basel), vol. 16, no. 1, 2024. [CrossRef]
- Prat, B. Adamo, M. C. U. Cheang, C. K. Anders, L. A. Carey, and C. M. Perou, “Molecular characterization of basal-like and non-basal-like triple-negative breast cancer,” Oncologist, vol. 18, no. 2, pp. 123–133, Feb. 2013. [CrossRef]
- M. Meegdes et al., “The initial hormone receptor/HER2 subtype is the main determinator of subtype discordance in advanced breast cancer: a study of the SONABRE registry,” Breast Cancer Res Treat, vol. 192, no. 2, pp. 331–342, Apr. 2022. [CrossRef]
- M. Mellouli et al., “Discordance in receptor status between primary and metastatic breast cancer and overall survival: A single-center analysis,” Ann Diagn Pathol, vol. 61, Dec. 2022. [CrossRef]
- T. Grinda et al., “Phenotypic discordance between primary and metastatic breast cancer in the large-scale real-life multicenter French ESME cohort,” NPJ Breast Cancer, vol. 7, no. 1, Dec. 2021. [CrossRef]
- L. Peng, Z. Zhang, D. Zhao, J. Zhao, F. Mao, and Q. Sun, “Discordance in ER, PR, HER2, and Ki-67 Expression Between Primary and Recurrent/Metastatic Lesions in Patients with Primary Early Stage Breast Cancer and the Clinical Significance: Retrospective Analysis of 75 Cases,” Pathology and Oncology Research, vol. 27, Apr. 2021. [CrossRef]
| Luminal A | Luminal B | TNBC |
| 233/38660.4% | 257/40862.9% | 100/14568.9% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





