Submitted:
03 April 2025
Posted:
04 April 2025
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Methods
2.1. Limitations
2.2. Justification of Method
3. Literary Review
3.1. Health in the Context of Emergencies and Disasters
3.2. Psychological First Aid: Concept, Principles, and Relevance
3.3. Disaster Psychology and Community Resilience
3.4. Institutional Framework for Emergency Health and Psychosocial Support
3.5. The Role of the Red Cross in Delivering Psychological Support
3.6. Gaps and Challenges in the Integration of Psychosocial Support
4. Findings from Expert Interview
4.1. Interconnectedness of Medical and Psychosocial First Aid
4.2. Institutional Capacity and Team Preparedness
4.3. Clarifying the Distinction Between PFA and Clinical Intervention
4.4. Adherence to Core PFA Guidelines
4.5. The Role of Volunteers in Providing Psychological Support
4.6. Gaps in Education and Perception of PFA
4.7. Lack of Empirical Data and the Importance of Experience-Based Knowledge
4.8. Impact of First Aid on Community Health
5. Conclusions
Funding
Acknowledgments
Conflicts of Interest
References
- Adams, R. (2018). Disabilities and Disasters: How Social Cognitive and Community Factors Influence Preparedness among People with Disabilities. Retrieved from https://consensus.app/papers/disabilities-and-disasters-how-social-cognitive-and-adams/3201c03ffba6507db9a53fd8c53e8df5/.
- Anđelić, M., Lazić, M., & Detki, R. (2015). Uloga javnog zdravlja u vanrednim situacijama [The role of public health in emergencies]. Novi Sad: Institut za javno zdravlje Vojvodine.
- Arambašić, L. (2000). Psihološka pomoć u kriznim situacijama [Psychological assistance in crisis situations]. Zagreb: Društvo za psihološku pomoć.
- Andric, I. (1977). The bridge on the Drina. University of Chicago press.
- Australian Psychological Society. (2013). Psychological first aid: An Australian guide to supporting people affected by disaster. Melbourne: APS.
- Babaii, A., Mohammadi, E., & Sadooghiasl, A. (2021). The Meaning of the Empathetic Nurse–Patient Communication: A Qualitative Study. Journal of Patient Experience, 8. [CrossRef]
- Babić, D. (2011). Zdravstvena zaštita u vanrednim situacijama [Health care in emergencies]. Beograd: Zdravstvena zaštita.
- Babić, D. (2012). Organizacija zdravstvene službe u kriznim situacijama [Organization of the health service in crisis situations]. Beograd: Vojnomedicinska akademija.
- Baek, J. S., & Hong, S. (2022). A Study on the Risk of Terrorism by Simulated Guns and Homemade Explosives. Forum of Public Safety and Culture. [CrossRef]
- Bangpan, M., Felix, L., & Dickson, K. (2019). Mental health and psychosocial support programmes for adults in humanitarian emergencies: a systematic review and meta-analysis in low and middle-income countries. BMJ Global Health, 4. [CrossRef]
- Banyard, V., Edwards, V., & Kendall-Tackett, K. (2009). Trauma and physical health : understanding the effects of extreme stress and of psychological harm.
- Batut – Institut za javno zdravlje Srbije. (2013). Plan pripravnosti za vanredne situacije [Preparedness plan for emergencies]. Beograd.
- Betz, L., Penzel, N., Rosen, M., & Kambeitz, J. (2020). Relationships between childhood trauma and perceived stress in the general population: a network perspective. Psychological Medicine, 51, 2696-2706. [CrossRef]
- Breckner, M., & Sunde, U. (2019). Temperature extremes, global warming, and armed conflict: new insights from high resolution data. World Development.
- Bretton, O. M. (2024). Mapping the Psychosocial: Introducing a Standardised System to Improve Psychosocial Understanding within Mental Health. Archives of Psychiatry and Mental Health. [CrossRef]
- Brooks, S., Dunn, R., Amlȏt, R., Greenberg, N., & Rubin, J. (2018). Training and post-disaster interventions for the psychological impacts on disaster-exposed employees: a systematic review. Journal of mental health, 1-25. [CrossRef]
- Brooks, S., Rubin, G., & Greenberg, N. (2018). Traumatic stress within disaster-exposed occupations: overview of the literature and suggestions for the management of traumatic stress in the workplace. British Medical Bulletin, 129, 25. [CrossRef]
- Burke, T., Sticca, F., & Perren, S. (2017). Everything’s Gonna be Alright! The Longitudinal Interplay among Social Support, Peer Victimization, and Depressive Symptoms. Journal of Youth and Adolescence, 46, 1999-2014. [CrossRef]
- Chan, E., & Shi, P. (2017). Health and Risks: Integrating Health into Disaster Risk Reduction, Risk Communication, and Building Resilient Communities. International Journal of Disaster Risk Science, 8, 107-108. [CrossRef]
- Chan, S., Khong, P., & Wang, W. (2017). Psychological responses, coping and supporting needs of healthcare professionals as second victims. International Nursing Review, 64, 242.
- Chen, L., Li, H., & Zhao, L. (2024). Pathway Selection for Enhancing the Efficiency of Psychological Crisis Intervention Resource Integration during Major Emergencies: Evidence from China. Applied Sciences. [CrossRef]
- Chesler, A. (2024). Environmental displacement and political instability: Evidence from Africa. Journal of Peace Research. [CrossRef]
- Chrousos, G. (2009). Stress and disorders of the stress system. Nature Reviews Endocrinology, 5, 374-381. [CrossRef]
- Colvonen, P., Straus, L., Acheson, D., & Gehrman, P. (2019). A Review of the Relationship Between Emotional Learning and Memory, Sleep, and PTSD. Current Psychiatry Reports, 21, 1-11. [CrossRef]
- Cvetkovic, V. (2021). Earthquake Risk Perception in Belgrade: Implications for Disaster Risk Management. International Journal of Disaster Risk Management.
- Cvetkovic, V. M., & Martinović, J. (2020). Innovative solutions for flood risk management. International Journal of Disaster Risk Management, 2(2), 71-100.
- Cvetković, V. (2013). Possibilities of biological weapons abuse for terrorist purposes. Bezbednost, Beograd, 55(1), 122-139.
- Cvetković, M. (2016). Citizens preparedness for responding to natural disaster caused by flood in Serbia (Doctoral dissertation, PhD Thesis, University of Belgrade, Serbia, 2016. https://eteze. bg. ac. rs/application/showtheses).
- Cvetković, V. (2016). Strah i poplave u Srbiji: spremnost građana za reagovanje na prirodne katastrofe (Fear and Floods in Serbia: Citizens’ Preparedness for Responding to Natural Disasters). Zbornik matice srpske za društvena istraživanja, 155(2), 2016.
- Cvetković, V. (2016). The relationship between educational level and citizen preparedness for responding to natural disasters. Journal of the Geographical Institute “Jovan Cvijić” SASA, 66(2), 237-253.
- Cvetković, V. (2019). First aid disaster kit for a family: a case study of Serbia. Paper presented at the IX International scientic conference Archibald Reiss days November 6-7, 2019. University of Criminal Investigation and Police Studies, Belgrade.
- Cvetković, V. (2023). A Predictive Model of Community Disaster Resilience based on Social Identity Influences (MODERSI). International Journal of Disaster Risk Management, 5(2), 57-80.
- Cvetković, V. (2024a). Disaster Resilience: Guide for Prevention, Response and Recovery. In: Scientific-Professional Society for Disaster Risk Management, Belgrade.
- Cvetković, V. (2024b). Disaster Risk Management. Scientific-Professional Society for Disaster Risk Management, Belgrade.
- Cvetković, V. (2024c). Essential Tactics for Disaster Protection and Rescue. Scientific-Professional Society for Disaster Risk Management, Belgrade.
- Cvetković, V. M., Dragašević, A., Protić, D., Janković, B., Nikolić, N., & Milošević, P. (2022). Fire safety behavior model for residential buildings: Implications for disaster risk reduction. International Journal of Disaster Risk Reduction, 76, 102981.
- Cvetković, V. M., Gačić, J., & Jakovljević, V. (2016). Geospatial and temporal distribution of forest fires as natural disasters. Vojno delo, 68(2), 108-127.
- Cvetković, V. M., Renner, R., & Jakovljević, V. (2024). Industrial Disasters and Hazards: From Causes to Conse-quences—A Holistic Approach to Resilience. International Journal of Disaster Risk Management, 6(2), 149-168.
- Cvetković, V. M., Tanasić, J., Ocal, A., Kešetović, Ž., Nikolić, N., & Dragašević, A. (2021). Capacity Development of Local Self-Governments for Disaster Risk Management. International Journal of Environmental Research and Public Health, 18(19), 10406.
- Cvetković, V., & Janković, B. (2020). Private security preparedness for disasters caused by natural and anthropogenic hazards. International Journal of Disaster Risk Management, 2(1), 23-33.
- Cvetković, V., & Popović, M. (2011). Possibilities of weapon of mass destruction abuse for terrorist purposes. Bezbednost, Beograd, 53(2), 149-167.
- Cvetković, V., & Renner, R. (2024). Comprehensive Databases on Natural and Man-Made (Technological) Hazards and Disasters: Mapping Risks and Challenges. Belgrade: Scientific-Professional Society for Disaster Risk Management.
- Cvetković, V., & Stojković, D. (2015). Analysis of geospatial and temporal distribution of storms as a natural disaster. Paper presented at the International scientific conference - Criminalistic education, situation and perspectives 20 years after Vodinelic.
- Cvetković, V., & Stojković, D. (2015). Analysis of geospatial and temporal distribution of storms as a natural disaster. In International scientific conference - Criminalistic education, situation and perspectives 20 years after Vodinelic. Skopje: Faculty of security, University St. Kliment Ohridski - Bitola in collaboration with Faculty of detectives and security, FON University.
- Cvetković, V., Noji, E., Filipović, M., Marija, M. P., Želimir, K., & Nenad, R. (2018). Public Risk Perspectives Regarding the Threat of Terrorism in Belgrade: Implications for Risk Management Decision-Making for Individuals, Communities and Public Authorities. Journal of Criminal Investigation and Criminology/, 69(4), 279-298.
- Cvetković, V., Öcal, A., & Ivanov, A. (2019). Young adults’ fear of disasters: A case study of residents from Turkey, Serbia and Macedonia. International Journal of Disaster Risk Reduction, 101095. [CrossRef]
- Cvetković, V., Renner, R., Aleksova, B., & Lukić, T. (2024). Geospatial and Temporal Patterns of Natural and Man-Made (Technological) Disasters (1900–2024): Insights from Different Socio-Economic and Demographic Perspectives. Applied Sciences, 14(18), 8129.
- Cvetković, V., Tanasić, J., Ocal, A., Živković-Šulović, M., Ćurić, N., Milojević, S., & Knežević, S. (2023). The Assessment of Public Health Capacities at Local Self-Governments in Serbia. Lex localis - Journal of Local Self Government, 21(4), 1201-1234.
- Cvetković, V., Tanasić, J., Renner, R., Rokvić, V., & Beriša, H. (2024b). Comprehensive Risk Analysis of Emergency Medical Response Systems in Serbian Healthcare: Assessing Systemic Vulnerabilities in Disaster Preparedness and Response. 12, 1962.
- De Munter, L., Polinder, S., Havermans, R., Steyerberg, E., & De Jongh, M. (2021). Prognostic factors for recovery of health status after injury: a prospective multicentre cohort study. BMJ Open, 11. [CrossRef]
- Désilets, L., Fernet, M., Otis, J., Cousineau, M.-M., Massie, L., De Pokomandy, A., & Mensah, M. N. (2020). Trauma-Informed Practices to Address Intersections Between HIV and Intimate Partner Violence Among Women: Perspective of Community Service Providers. Journal of the Association of Nurses in AIDS Care. [CrossRef]
- Devlin, M., Waterhouse, J., Taylor, J., & Brodie, J. (2001). Flood plumes in the Great Barrier Reef: spatial and temporal patterns in composition and distribution: Great Barrier Reef Marine Park Authority.
- Djordjević, I., & Gačić, J. (2024). Sustainable Recovery: the Link Between Development and Response to Disasters. International Journal of Disaster Risk Management, 6(2), 223-244.
- Downing, M., Hicks, A., Braaf, S., Myles, D., Gabbe, B., Cameron, P., Ponsford, J. (2020). Factors facilitating recovery following severe traumatic brain injury: A qualitative study. Neuropsychological Rehabilitation, 31, 889-913. [CrossRef]
- Drury, J., Carter, H., Cocking, C., Ntontis, E., Guven, S. T., & Amlȏt, R. (2019). Facilitating Collective Psychosocial Resilience in the Public in Emergencies: Twelve Recommendations Based on the Social Identity Approach. Frontiers in public health, 7. [CrossRef]
- Ellis, C., & Knight, K. (2018). Advancing a Model of Secondary Trauma: Consequences for Victim Service Providers. Journal of Interpersonal Violence, 36, 3557-3583.
- El-Mougher, M. M. (2022). Level of coordination between the humanitarian and governmental organizations in Gaza Strip and its impact on the humanitarian interventions to the Internally Displaced People (IDPs) following May escalation 2021. International Journal of Disaster Risk Management, 4(2), 15-45.
- Engel, S., Berkowitz, G., Wolff, M., & Yehuda, R. (2005). Psychological trauma associated with the World Trade Center attacks and its effect on pregnancy outcome. Paediatric and perinatal epidemiology, 19 5, 334-341. [CrossRef]
- Fahey, S., LaFree, G., Dugan, L., & Piquero, A. (2012). A Situational Model for Distinguishing Terrorist and Non-Terrorist Aerial Hijackings, 1948–2007. Justice Quarterly, 29, 573-595.
- Fap, B. (2025). Navigating Complex Cases With Empathetic Communication. Journal of the Advanced Practitioner in Oncology. [CrossRef]
- Farchi, M., Bathish, L., Hayut, N., Alexander, S., & Gidron, Y. (2024). Effects of a psychological first aid (PFA) based on the SIX Cs model on acute stress responses in a simulated emergency. Psychological trauma : theory, research, practice and policy. [CrossRef]
- Ferguson, A., Ward, K., & Parke, R. (2024). What is known about resilient healthcare systems in the context of natural disasters? A scoping review. Collegian. [CrossRef]
- Feuer, B. (2021). First Responder Peer Support: An Evidence-Informed Approach. Journal of Police and Criminal Psychology, 1-7. [CrossRef]
- Freeman, G., & McDaniel, J. (2004). An observational study to identify predictors of acute stress disorder and depressive symptoms in adult female victims of sexual assault. Annals of emergency medicine, 44. [CrossRef]
- Gaiser, M., Buche, J., Baum, N., & Grazier, K. (2023). Mental Health Needs Due to Disasters: Implications for Behavioral Health Workforce Planning During the COVID-19 Pandemic. Public Health Reports, 138, 48-55. [CrossRef]
- Guilaran, J., De Terte, I., Kaniasty, K., & Stephens, C. (2018). Psychological Outcomes in Disaster Responders: A Systematic Review and Meta-Analysis on the Effect of Social Support. International Journal of Disaster Risk Science, 9, 344-358. [CrossRef]
- Han, R., Schmidt, M., Waits, W., Bell, A., & Miller, T. (2020). Planning for Mental Health Needs During COVID-19. Current Psychiatry Reports, 22. [CrossRef]
- Hanspal, M. S., & Behera, B. (2024). Role of Emerging Technology in Disaster Management in India: An Overview. International Journal of Disaster Risk Management, 6(2), 133-148.
- Haribhai-Thompson, J., McBride-Henry, K., Hales, C., & Rook, H. (2022). Understanding of empathetic communication in acute hospital settings: a scoping review. BMJ Open, 12.
- Hsieh, H.-F., Chen, Y.-M., Wang, H.-H., Chang, S.-C., & Shu, C. (2016). Association among components of resilience and workplace violence-related depression among emergency department nurses in Taiwan: a cross-sectional study. Journal of clinical nursing, 25 17-18, 2639-2647. [CrossRef]
- Hunt, D., Bailey, J., Lennox, B., Crofts, M., & Vincent, C. (2021). Enhancing psychological safety in mental health services. International Journal of Mental Health Systems, 15. [CrossRef]
- Ide, T. (2023). Rise or Recede? How Climate Disasters Affect Armed Conflict Intensity. International Security, 47, 50-78. [CrossRef]
- IFRC – International Federation of Red Cross and Red Crescent Societies. (2018). Psychosocial Centre Manual. Geneva.
- Institute of Public Health of Serbia. (2013). Annual Report on the Health Status of the Population of Serbia. Belgrade.
- Inter-Agency Standing Committee (IASC). (2007). IASC Guidelines on Mental Health and Psychosocial Support in Emergency Settings. Geneva: IASC.
- Ivanović, S. (2014). Zdravstvena zaštita u kriznim situacijama [Health care in crisis situations]. Beograd: Institut za javno zdravlje Srbije.
- Jacobs, G., Gray, B., Erickson, S., Gonzalez, E., & Quevillon, R. (2016). Disaster Mental Health and Community-Based Psychological First Aid: Concepts and Education/Training. Journal of clinical psychology, 72 12, 1307-1317. [CrossRef]
- Jehoshaphat, J. D., & Oghenah, B. (2021). Building resilience through local and international partnerships, Nigeria experiences. International Journal of Disaster Risk Management (IJDRM), 3(2), 11-24.
- Jevtić, M. (2011). Katastrofe i zdravlje [Disasters and health]. Novi Sad: Medicinski fakultet.
- Jevtić, M., & Jevtić, G. (2017). Javno zdravlje u kriznim situacijama [Public health in crisis situations]. Novi Sad: Medicinski fakultet.
- Kabir, M. H., Tanvir, H., & Haque, M. W. (2022). Resilience to natural disasters: A case study on southwestern region of coastal Bangladesh. International Journal of Disaster Risk Management, 4(2), 91-105.
- Kachanov, S. (2021). Methodology for Building Automated Systems for Monitoring Engineering (Load-Bearing) Structures, and Natural Hazards to Ensure Comprehensive Safety of Buildings and Constructions. International Journal of Disaster Risk Management (IJDRM), 3(2), 1-10.
- Kantor, V., Knefel, M., & Lueger-Schuster, B. (2017). Perceived barriers and facilitators of mental health service utilization in adult trauma survivors: A systematic review. Clinical psychology review, 52, 52-68. [CrossRef]
- Kaur, B. (2020). Disasters and exemplified vulnerabilities in a cramped Public Health Infrastructure in India. International Journal of Disaster Risk Management, 2(1), 15-22.
- Kelly-Hope, L., Harding-Esch, E., Willems, J., Ahmed, F., & Sanders, A. (2023). Conflict-climate-displacement: a cross-sectional ecological study determining the burden, risk and need for strategies for neglected tropical disease programmes in Africa. BMJ Open, 13. [CrossRef]
- Khan, Y., O’Sullivan, T., Brown, A., Tracey, S., Gibson, J., Généreux, M., Schwartz, B. (2018). Public health emergency preparedness: a framework to promote resilience. BMC Public Health, 18. [CrossRef]
- Khedr, M. A., Al-Ahmed, N. A., Mattar, F. K., Alshammari, M., & Ali, E. A. (2024). The feasibility of a psychological first aid intervention as a supportive tactic for feelings of psychological distress and mental health recovery outcomes among earthquake survivors in Northern Syria. International journal of nursing practice. [CrossRef]
- Kordić, B. (2018). Psihološka prva pomoć: Priručnik za terenski rad [Psychological first aid: Field guide]. Beograd: Crveni krst Srbije.
- Kordić, B., & Babić, D. (2015). Psihološka pomoć u kriznim situacijama [Psychological support in crisis situations]. Beograd: Crveni krst Srbije.
- Kouhirostamkolaei, M. (2023). Integrating Mental Health Support in Emergency Planning and Disaster Risk Mitigation Strategies. Qeios. [CrossRef]
- Krstić, D. (2009). Psihologija katastrofa [Disaster psychology]. Psihologija, 42(4), 411–424.
- Kruk, M., Myers, M., Varpilah, T., & Dahn, B. (2015). What is a resilient health system? Lessons from Ebola. The Lancet, 385, 1910-1912. [CrossRef]
- Levy, B. (2019). Increasing Risks for Armed Conflict: Climate Change, Food and Water Insecurity, and Forced Displacement. International Journal of Health Services, 49, 682-691. [CrossRef]
- Limone, P., & Toto, G. (2022). Protocols and strategies to use emergency psychology in the face of an emergency: A systematic review. Acta psychologica, 229, 103697.
- Lotzin, A., De Pommereau, A. F., & Laskowsky, I. (2023). Promoting Recovery from Disasters, Pandemics, and Trauma: A Systematic Review of Brief Psychological Interventions to Reduce Distress in Adults, Children, and Adolescents. International Journal of Environmental Research and Public Health, 20. [CrossRef]
- Loukas, A., & Quick, M. C. (1996). Spatial and temporal distribution of storm precipitation in southwestern British Columbia. Journal of Hydrology, 174(1), 37-56.
- Lowe, A., Neligan, A., & Greenwood, R. (2020). Sleep disturbance and recovery during rehabilitation after traumatic brain injury: a systematic review. Disability and Rehabilitation, 42, 1041-1054. [CrossRef]
- Mach, K., Kraan, C., Adger, W., Buhaug, H., Burke, M., Fearon, J., Uexkull, N. (2019). Climate as a risk factor for armed conflict. Nature, 571, 193-197. [CrossRef]
- Marceta, Ž., & Jurišic, D. (2024). Psychological Preparedness of the Rescuers and Volunteers: A Case Study of 2023 Türkiye Earthquake. International Journal of Disaster Risk Management, 6(1), 27-40.
- Martikainen, P., Bartley, M., & Lahelma, E. (2002). Psychosocial determinants of health in social epidemiology. International journal of epidemiology, 31 6, 1091-1093. [CrossRef]
- Martinez, J.-M., & Le Toan, T. (2007). Mapping of flood dynamics and spatial distribution of vegetation in the Amazon floodplain using multitemporal SAR data. Remote sensing of Environment, 108(3), 209-223.
- Mathai, M., Mbwayo, A., Concepcion, T., Mutavi, T., Njeru, M., Waruinge, S., .Collins, P. (2023). Sustainable Partnerships to Ensure Quality in Psychological Support (EQUIP) for Adolescents. Psychiatric services. [CrossRef]
- Maulana, I., Febrianti, S., & Nugraha, B. A. (2023). Intervensi Terapi Dukungan Psikologis pada Korban Terdampak Bencana yang Mengalami PTSD (Literature Review). Malahayati Nursing Journal. [CrossRef]
- McBride, D. (2020). Emergency Department Preparedness for Children Seeking Mental Health Care. Journal of Pediatric Nursing, 54, 106-108. [CrossRef]
- McFarlane, A., & Williams, R. (2012). Mental Health Services Required after Disasters: Learning from the Lasting Effects of Disasters. Depression Research and Treatment, 2012. [CrossRef]
- McNaughton, M. (2024). A Shared Journey: Effective communication tools to successfully navigate the patient-provider relationship. Pain Management Nursing. [CrossRef]
- Merandi, J., Liao, N., Lewe, D., Morvay, S., Stewart, B., Catt, C., & Scott, S. (2017). Deployment of a Second Victim Peer Support Program: A Replication Study. Pediatric Quality & Safety, 2. Milenković, D., Cvetković, V. M., & Renner, R. (2024). A Systematic Literary Review on Community Resilience Indicators: Adaptation and Application of the BRIC Method for Measuring Disasters Resilience. International Journal of Disaster Risk Management, 6(2), 79-104.
- Milošević, G., Cvjetković-Ivetić, C., & Baturan, L. (2024). State Aid in Reconstruction of Natural and Other Disasters’ Consequences Using the Budget Funds of the Republic of Serbia. International Journal of Disaster Risk Management, 6(2), 169-182.
- Ministry of Health, Republic of Serbia. (2013). National Strategy for Health Care Protection. Belgrade.
- Mitrović, S., & Gavrilović, B. (2013). Zdravstvena zaštita u vanrednim situacijama [Health protection in emergencies]. Beograd: Zavod za unapređenje zdravlja.
- Molnár, A. (2024). A Systematic Collaboration of Volunteer and Professional Fire Units in Hungary. International Journal of Disaster Risk Management, 6(1), 1-13.
- Mooney, G., Speed, J., & Sheppard, S. (2005). Factors related to recovery after mild traumatic brain injury. Brain Injury, 19, 975-987. [CrossRef]
- Mora, F., Segovia, G., Arco, A., Blas, M., & Garrido, P. (2012). Stress, neurotransmitters, corticosterone and body–brain integration. Brain Research, 1476, 71-85. [CrossRef]
- Mortelmans, L. J. M., Van Boxstael, S., De Cauwer, H. G., Sabbe, M. B., Emergency, A. B. S. o., & study, D. M. (2014). Preparedness of Belgian civil hospitals for chemical, biological, radiation, and nuclear incidents: are we there yet? , 21(4), 296-300. [CrossRef]
- Nagano, H., Chida, K., & Ozawa, T. (2021). Can We Be at Peace With Unsolvable Suffering? A Qualitative Study Exploring the Effectiveness of Supportive Communication and Resilience Building. Journal of Hospice and Palliative Nursing, 24. [CrossRef]
- Nayani, R., Rajapaksha, U., Khatri, R., Abeysena, C., Supun, M., Wijesinghe, D., Alemu, Y. (2022). Success and challenges of health systems resilience-enhancing strategies for managing Public Health Emergencies of International Concerns (PHEIC): A systematic review protocol. BMJ Open, 12. [CrossRef]
- Neil-Sztramko, S., Belita, E., Hopkins, S., Sherifali, D., Anderson, L., Apatu, E., . . . Dobbins, M. (2023). What are effective strategies to respond to the psychological impacts of working on the frontlines of a public health emergency? Frontiers in public health, 11. [CrossRef]
- Nenadović, M. (2013). Psihosocijalna podrška kao deo humanitarnog odgovora [Psychosocial support as part of humanitarian response]. In M. Nenadović (Ed.), Psihosocijalna podrška u kriznim situacijama [Psychosocial support in crisis situations] (pp. 307–322). Beograd: Crveni krst Srbije.
- Neuner, F. (2022). Physical and social trauma: Towards an integrative transdiagnostic perspective on psychological trauma that involves threats to status and belonging. Clinical psychology review, 99, 102219. [CrossRef]
- Nykonenko, L. (2022). Model of victims’ socio-psychological support in emergency conditions. Scientific Studios on Social and Political Psychology. [CrossRef]
- Öcal, A. (2021). Disaster management in Turkey: a spatial approach. International Journal of Disaster Risk Management, 3(1), 15-22.
- Official Gazette of the Republic of Serbia. (2005–2017). Law on Health Care (No. 107/2005, 72/2009, 88/2010, 119/2012, 113/2017).
- Pace-Schott, E., Seo, J.-H., & Bottary, R. (2022). The influence of sleep on fear extinction in trauma-related disorders. Neurobiology of Stress, 22. [CrossRef]
- Perić, J., & Vladimir, C. M. (2019). Demographic, socio-economic and phycological perspective of risk perception from disasters caused by floods: case study Belgrade. International Journal of Disaster Risk Management, 1(2), 31-43.
- Peter, K., Helfer, T., Golz, C., Halfens, R., & Hahn, S. (2021). Development of an Interrelated Definition of Psychosocial Health for the Health Sciences Using Concept Analysis. Journal of psychosocial nursing and mental health services, 1-8. [CrossRef]
- Plough, A., Fielding, J., Chandra, A., Williams, M., Eisenman, D., Wells, K., . . . Magaña, A. (2013). Building community disaster resilience: perspectives from a large urban county department of public health. American journal of public health, 103 7, 1190-1197. [CrossRef]
- Putwain, D. (2007). Researching academic stress and anxiety in students: some methodological considerations. British Educational Research Journal, 33, 207-219. [CrossRef]
- Rajani, A., Tuhin, R., & Rina, A. (2023). The Challenges of Women in Post-disaster Health Management: A Study in Khulna District. International Journal of Disaster Risk Management, 5(1), 51-66.
- Rawat, A., Hsu, K., Ameha, A., Pun, A., Hassen, K., Simen-Kapeu, A., Rasanathan, K. (2024). Learning From Countries on Measuring and Defining Community-Based Resilience in Health Systems: Voices From Nepal, Sierra Leone, Liberia, and Ethiopia. International Journal of Health Policy and Management, 13. [CrossRef]
- Rebouh, N., Tout, F., Dinar, H., Benzid, Y., & Zouak, Z. (2024). Integrating Multi-Source Geospatial Data and AHP for Flood Susceptibility Mapping in Ain Smara, Constantine, Algeria. International Journal of Disaster Risk Management, 6(2), 245-264.
- Red Cross of Serbia. (2011). Pocket Guide for Field Workers. Beograd: Crveni krst Srbije.
- Red Cross of Serbia. (2018). Organization Overview. Beograd: Crveni krst Srbije.
- Richards, H., Eustace, J., O' Dwyer, A., Wormald, A., Curtin, Y., & Fortune, D. (2022). Healthcare workers use of psychological support resources during COVID-19; a mixed methods approach utilising Pillar Integration Analysis. PloS one, 17. [CrossRef]
- Rigney, G., Jo, J., Williams, K., Terry, D., & Zuckerman, S. (2023). Parental Factors Associated with Recovery after Mild Traumatic Brain Injury: A Systematic Review. Journal of neurotrauma. [CrossRef]
- Ro, E., & Clark, L. (2009). Psychosocial functioning in the context of diagnosis: assessment and theoretical issues. Psychological assessment, 21 3, 313-324. [CrossRef]
- Ryan, B., Kako, R. M., Fink, R., Ek, P. I., BmedSci, M.., Acosta, J., Brooks, B. (2023). Strategies for Strengthening the Resilience of Public Health Systems for Pandemics, Disasters, and Other Emergencies. Disaster Medicine and Public Health Preparedness, 17. [CrossRef]
- Savvoulidou, K., Papageorgiou, A., Kolokotroni, O., Kapreli, P., Tsokani, A., Strimpakos, N., & Kapreli, E. (2024). Facilitators and barriers of empathetic behaviour in physiotherapy clinical practice: A qualitative focus group study. Musculoskeletal science & practice, 70, 102923. [CrossRef]
- Schemitsch, C., & Nauth, A. (2020). Psychological factors and recovery from trauma. Injury. [CrossRef]
- Schippert, A., Grov, E., Dahl-Michelsen, T., Silvola, J., Sparboe-Nilsen, B., Danielsen, S., . . . Bjørnnes, A. (2023). Re-traumatization of torture survivors during treatment in somatic healthcare services: A mapping review and appraisal of literature presenting clinical guidelines and recommendations to prevent re-traumatization. Social science & medicine, 323, 115775. [CrossRef]
- Semerci, M., & Uzun, S. (2023). The effectiveness of post-disaster psychotherapeutic interventions: A systematic review and meta-analysis study. Asian journal of psychiatry, 85, 103615. [CrossRef]
- Silei, G. (2014). Technological Hazards, Disasters and Accidents. 1, 227-253. [CrossRef]
- Sopp, M., Brueckner, A., Schäfer, S., Lass-Hennemann, J., & Michael, T. (2019). Differential effects of sleep on explicit and implicit memory for potential trauma reminders: findings from an analogue study. European Journal of Psychotraumatology, 10.
- Stark, E., Stark, E., Parsons, C., Hartevelt, T., Hartevelt, T., Charquero-Ballester, M., Kringelbach, M. (2015). Post-traumatic stress influences the brain even in the absence of symptoms: A systematic, quantitative meta-analysis of neuroimaging studies. Neuroscience & Biobehavioral Reviews, 56, 207-221. [CrossRef]
- Starosta, D. (2023). Raised Under Bad Stars: Negotiating a culture of disaster preparedness. International Journal of Disaster Risk Management, 5(2), 1-16.
- Stevens, J., & Jovanović, T. (2018). Role of social cognition in post-traumatic stress disorder: A review and meta-analysis. Genes, 18. [CrossRef]
- Stewart, T., & Gonzalez, V. (2023). Associations of historical trauma and racism with health care system distrust and mental health help-seeking propensity among American Indian and Alaska Native college students. Cultural diversity & ethnic minority psychology. [CrossRef]
- Stough, L., & Ducy, E. M. (2014). Disasters and Disabilities. [CrossRef]
- Štrbac, S. (2008). Finansiranje humanitarnih organizacija u Srbiji [Financing humanitarian organizations in Serbia]. Beograd: Pravni fakultet.
- Takhdat, K., Adib, A. E., & Lamtali, S. (2020). Stress and anxiety in nursing simulation. Journal of psychiatric and mental health nursing. [CrossRef]
- Tanasić, J., & Cvetković, V. (2024). The Efficiency of Disaster and Crisis Management Policy at the Local Level: Lessons from Serbia. In: Scientific-Professional Society for Disaster Risk Management, Belgrade.
- Tang, M., Tan, Q., & Yu, K. (2023). Self-Rated Physiological Health and Psychological Intervention among Residents during Major Public Health Emergencies. Journal of Medicine and Health Science. [CrossRef]
- Taylor, S., & McAvoy, J. (2015). Researching the Psychosocial: An Introduction. Qualitative Research in Psychology, 12, 1-7. [CrossRef]
- Thennavan, E., Ganapathy, G., Chandrasekaran, S., & Rajawat, A. J. (2020). Probabilistic rainfall thresholds for shallow landslides initiation – A case study from The Nilgiris district, Western Ghats, India. 2(1).
- Türkeş, M., Sümer, U. J. T., & Climatology, A. (2004). Spatial and temporal patterns of trends and variability in diurnal temperature ranges of Turkey. 77(3-4), 195-227.
- Ursin, H., & Eriksen, H. (2004). The cognitive activation theory of stress. Psychoneuroendocrinology, 29, 567-592. [CrossRef]
- Vico, P., Milošević, Z., Džamić, Z., & Bokan, V. (2013). Zdravstveni aspekti vanrednih situacija [Health aspects of emergencies]. Beograd: Vojnomedicinska akademija.
- Vrućinić, Z. (2018). Stres i strategije suočavanja kod adolescenata [Stress and coping strategies among adolescents]. Beograd: Fakultet za specijalnu edukaciju i rehabilitaciju.
- Walton, A. A., Marr, J., Cahillane, M., & Bush, K. (2021). Building Community Resilience to Disasters: A Review of Interventions to Improve and Measure Public Health Outcomes in the Northeastern United States. Sustainability. [CrossRef]
- Wang, L., Norman, I., Edleston, V., Oyo, C., & Leamy, M. (2024). The Effectiveness and Implementation of Psychological First Aid as a Therapeutic Intervention After Trauma: An Integrative Review. Trauma, Violence & Abuse, 25, 2638-2656. [CrossRef]
- Wang, Z., & Wang, D. (2021). The influence and enlightenment of five public health emergencies on public psychology since new century: A systematic review. International Journal of Social Psychiatry, 67, 878-891. [CrossRef]
- Whetten, K., Reif, S., Whetten, R., & Murphy-McMillan, L. (2008). Trauma, mental health, distrust, and stigma among HIV-positive persons: implications for effective care. Psychosomatic medicine, 70 5, 531-538. [CrossRef]
- Wolff, K., & Larsen, S. (2014). Can terrorism make us feel safer? Risk perceptions and worries before and after the July 22nd attacks. Annals of Tourism Research, 44, 200-209.
- Wood, M. M., Mileti, D. S., Kano, M., Kelley, M. M., Regan, R., & Bourque, L. B. (2012). Communicating actionable risk for terrorism and other hazards. Risk Analysis, 32(4), 601-615.
- World Health Organization (WHO). (2003). Mental Health in Emergencies. Geneva: WHO.
- World Health Organization (WHO). (2011). Psychological first aid: Guide for field workers. Geneva: WHO.
- Wulff, K., Donato, D., & Lurie, N. (2015). What is health resilience and how can we build it? Annual review of public health, 36, 361-374. [CrossRef]
- Yang, Y., & Bae, S. (2022). Association between resilience, social support, and institutional trust and post-traumatic stress disorder after natural disasters. Archives of psychiatric nursing, 37, 39-44. [CrossRef]
- Yaribeygi, H., Panahi, Y., Sahraei, H., Johnston, T., & Sahebkar, A. (2017). The impact of stress on body function: A review. EXCLI Journal, 16, 1057-1072. [CrossRef]
- Zahos, H., Crilly, J., & Ranse, J. (2022). Psychosocial problems and support for disaster medical assistance team members in the preparedness, response and recovery phases of natural hazards resulting in disasters: A scoping review. Australasian emergency care. [CrossRef]
- Zgueb, Y., Bourgou, S., Neffeti, A., Amamou, B., Masmoudi, J., Chebbi, H., . . . Bouasker, A. (2020). Psychological crisis intervention response to the COVID 19 pandemic: A Tunisian centralised Protocol. Psychiatry Research, 289, 113042. [CrossRef]
- Zheng, K., Chu, J., Zhang, X., Ding, Z., Song, Q., Liu, Z., . . . Yi, J. (2022). Psychological resilience and daily stress mediate the effect of childhood trauma on depression. Child abuse & neglect, 125, 105485. [CrossRef]
- Zúñiga, R. A., De Lima, G. N., & Suarez-Herrera, J. C. (2024). Tackling Complexity: Integrating Responses to Internal Displacements, Extreme Climate Events, and Pandemics. Climate. [CrossRef]
- 吕, 晓. (2023). Research on Psychological Status and Coping Methods of Medical Staff in Public Health Emergencies. Advances in Psychology. [CrossRef]
| Category | Identified Gap/Challenge | Description |
|---|---|---|
| Legal and strategic framework | Absence of national strategy on psychosocial support | Mental health care is often marginal in legal documents and emergency preparedness plans. |
| Institutional coordination | Poor inter-agency cooperation | Fragmented responsibilities and lack of clear referral protocols between institutions involved. |
| Professional workforce | Shortage of trained professionals | A limited number of psychologists, social workers, and counsellors are trained in emergencies. |
| Training and preparedness | Inadequate training in psychosocial first aid | Lack of structured, certified training programs for first responders and volunteers. |
| Community awareness | Low public awareness and mental health literacy | Populations are often unaware of available support or reluctant to seek help due to stigma or distrust. |
| Access to services | Geographic and logistical barriers | Rural and remote areas lack timely access to psychosocial services during and after emergencies. |
| Support to vulnerable groups | Insufficient target-group specific focus on at-risk populations | Children, the elderly, persons with disabilities, and migrants often receive inadequate or generic support. |
| Cultural sensitivity | Lack of culturally appropriate approaches | Psychosocial programs often fail to align with local beliefs, traditions, and values. |
| Resources and funding | Limited and unstable funding | Budget constraints hinder the implementation of long-term psychosocial recovery programs. |
| Monitoring and evaluation | Absence of impact assessment and data collection | No standardised tools for monitoring mental health outcomes or evaluating intervention effectiveness. |
| Continuity of care | Discontinuation of services post-emergency (Missing transfer function) | Psychosocial support ends after an immediate crisis, leaving long-term needs unmet. |
| Support for responders | Lack of mental health care for professionals and volunteers | Frontline workers often face burnout and vicarious trauma with no systemic support in place. |
| Integration with medical care | Weak linkage between psychosocial and medical services | Lack of coordination between mental health providers and emergency medical services. |
| Policy implementation | Gaps between policy and practice | Even when policies exist, they are inconsistently applied or lack enforcement mechanisms. |
| Community resilience building | Neglected role of community in recovery | Insufficient inclusion of local leaders and networks in planning and delivering psychosocial support. |
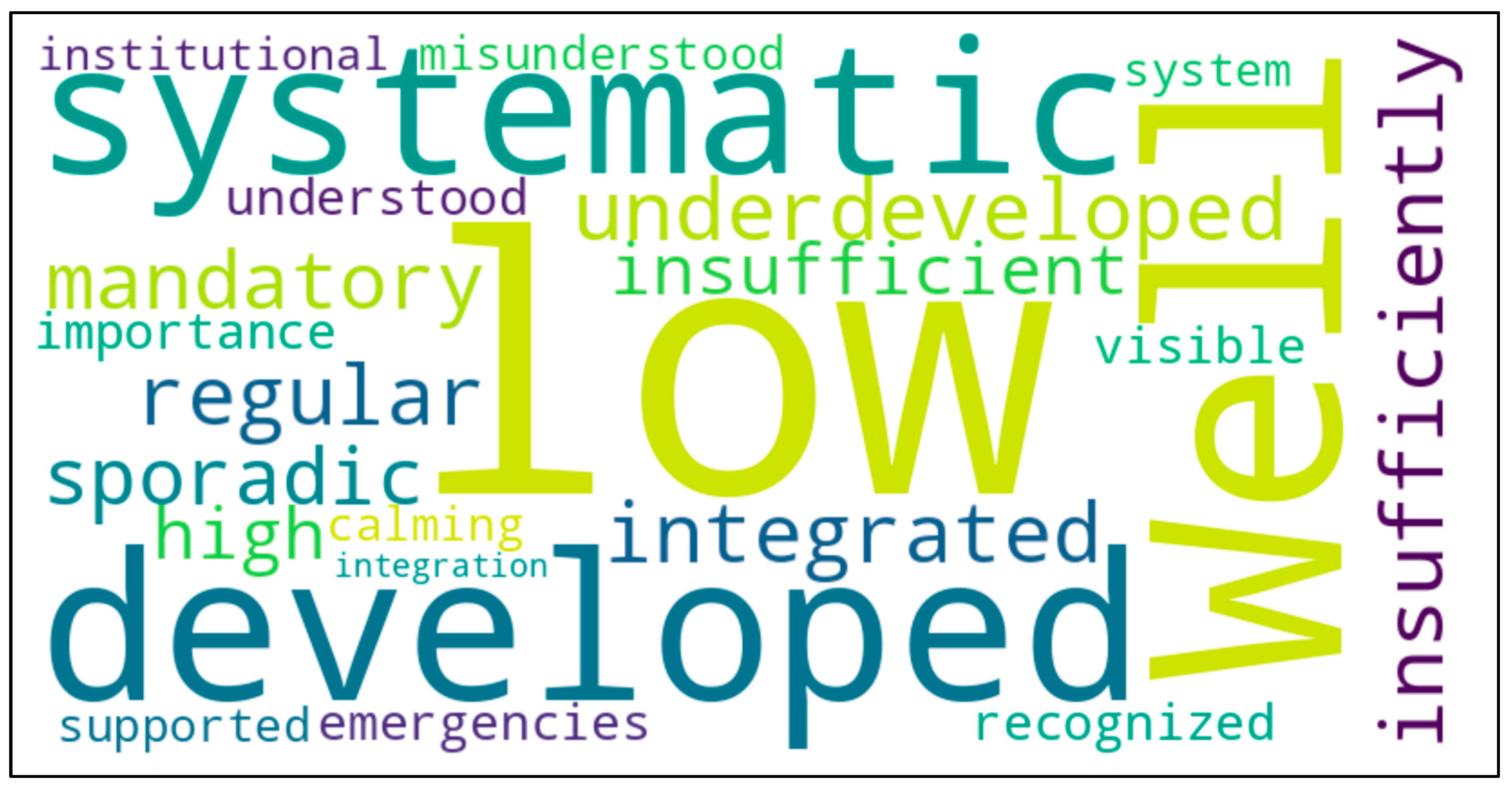
| Aspect | Medical First Aid | Psychosocial First Aid |
| Level of implementation | Well-developed and systematic | Underdeveloped and insufficiently integrated |
| Training | Regular and mandatory | Sporadic and insufficient |
| Prevalence | High, especially in emergencies | Low, despite recognised importance |
| Public perception | Visible and understood | Often misunderstood as simple calming |
| Institutional support | Supported by system | Low institutional integration |
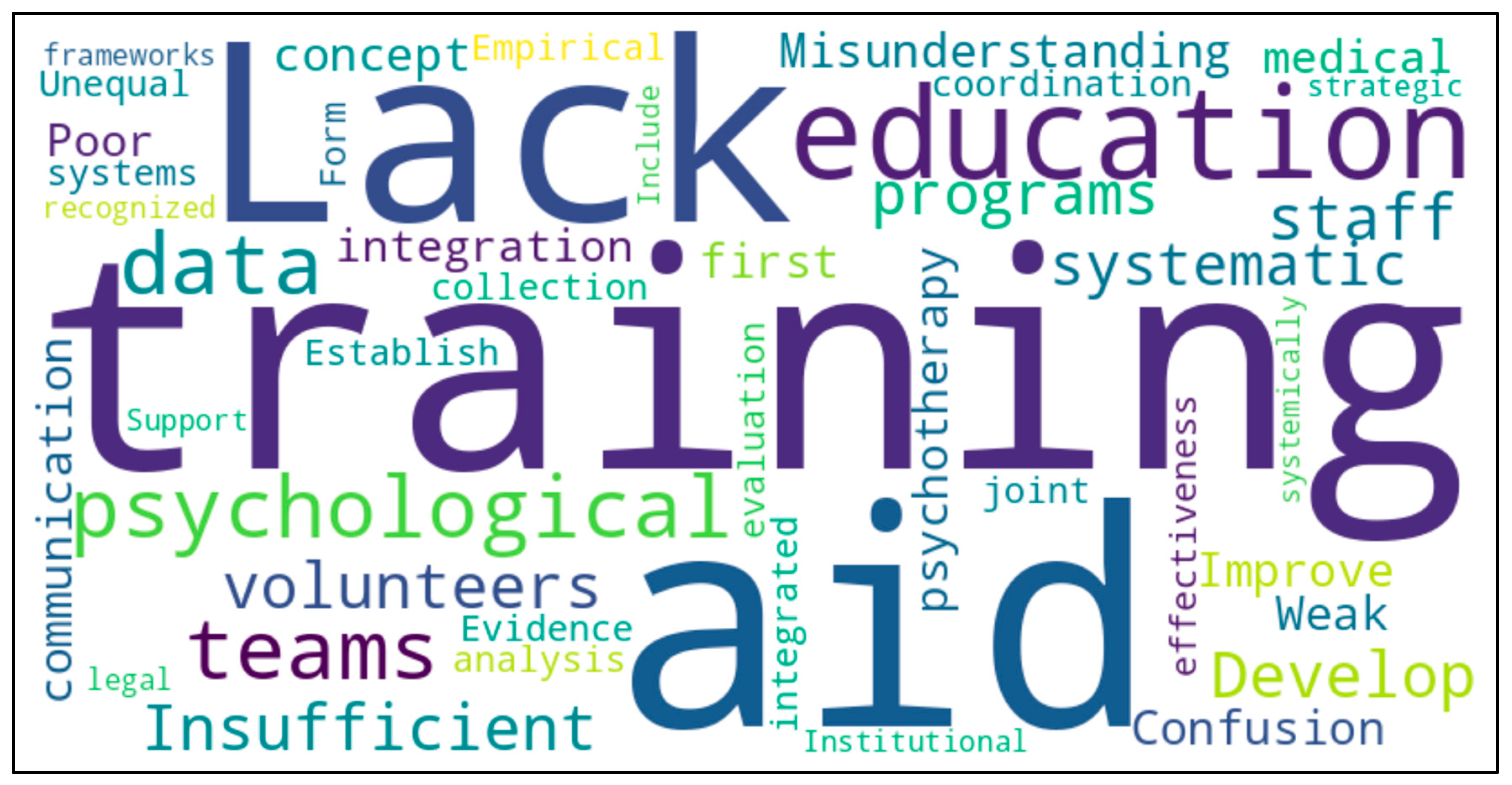
| Identified challenges | Problem description | Suggested improvements |
| Lack of training | Insufficient education for staff and volunteers | Develop systematic training programs |
| Misunderstanding of concept | Confusion between psychosocial first aid and professional support such as psychotherapy | Improve education and communication |
| Weak integration with medical aid | Poor coordination between teams | Form integrated teams and joint training |
| Lack of empirical evidence | No data collection and analysis on effectiveness | Establish data systems and evaluation |
| Unequal institutional support | Psychosocial aid not systemically recognised | Include in legal and strategic frameworks International Networking Insufficient exchange at the international level Learn from existing best practice examples, concepts and experiences through exchange |
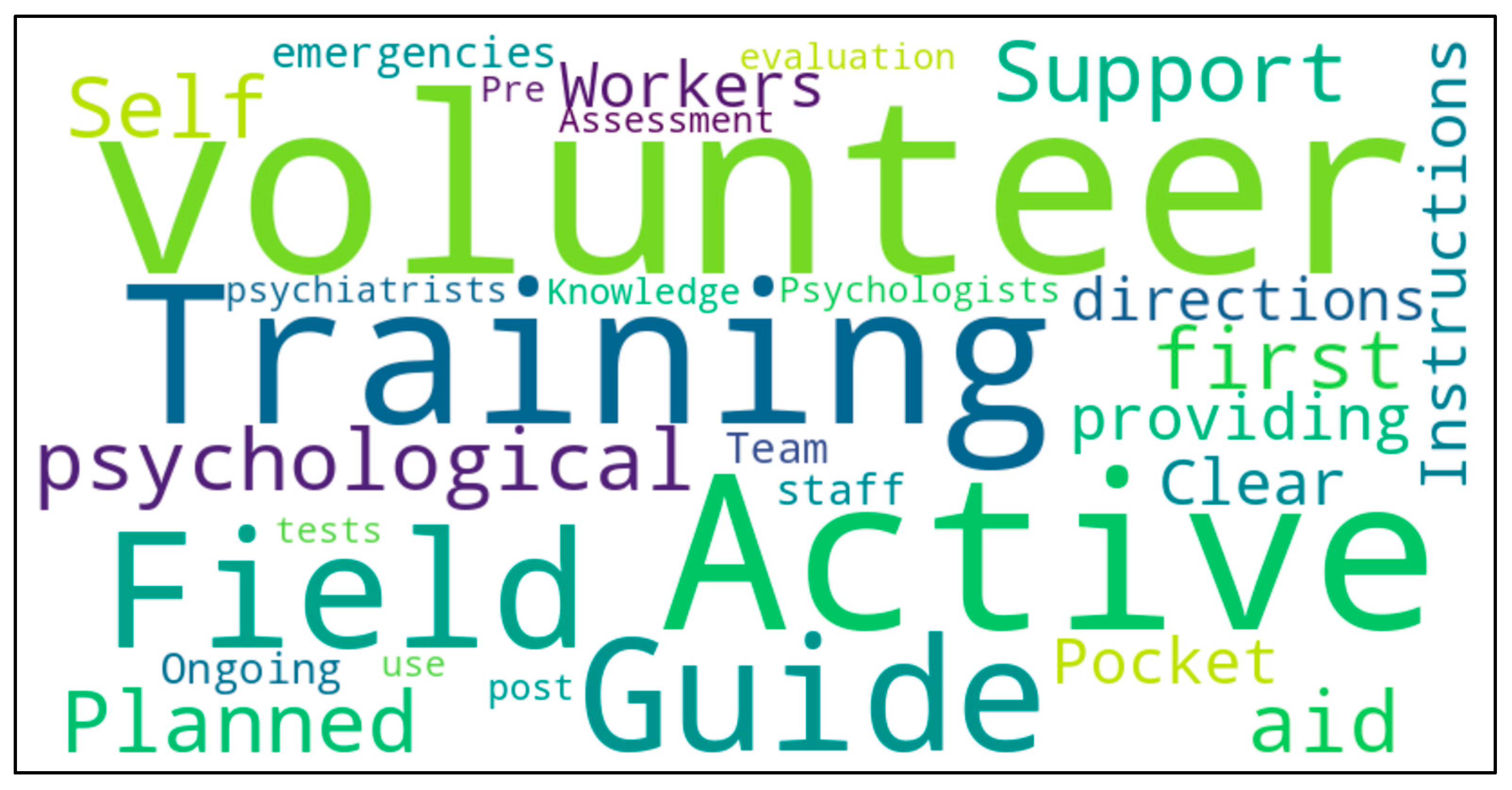
| Initiative/Activity | Description | Implementation Status |
| Field workers’ guide | Instructions for providing psychosocial first aid in the field | Active |
| Pocket guide | Clear directions for volunteers during emergencies | Active |
| Planned trainings | Training in psychosocial first aid for volunteers and staff | Planned/ongoing |
| Volunteer support team | Psychologists and psychiatrists support volunteers | Active |
| Knowledge self-assessment | Pre and post-training tests and self-evaluation | In use |
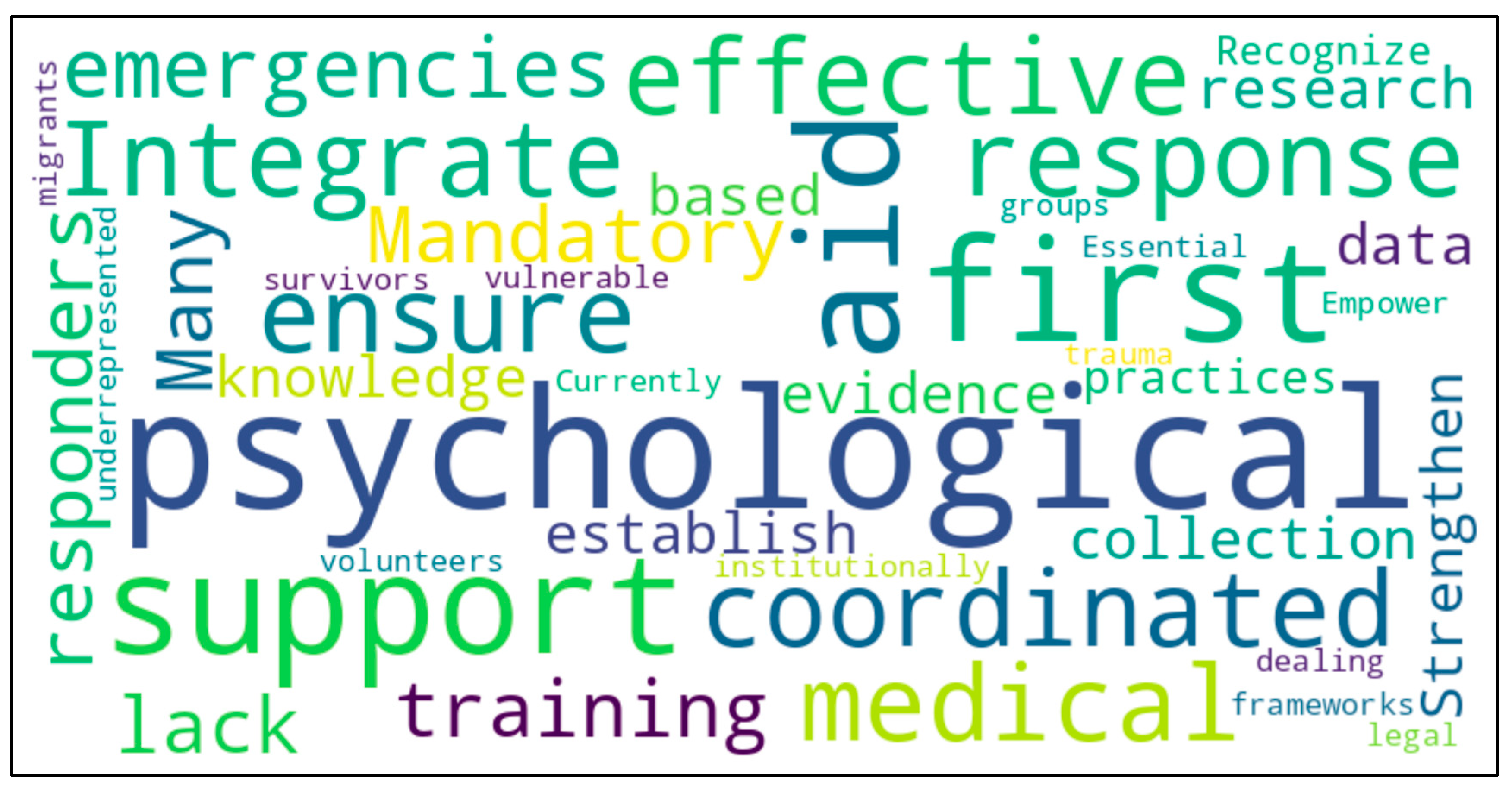
| Recommendation | Rationale |
| Integrate medical and psychosocial first aid | To ensure a coordinated and effective response in emergencies. |
| Mandatory training for all responders | To effectively support victims and to protect themselves |
| Strengthen data collection and research | To establish evidence-based practices |
| Recognise psychosocial support institutionally | Currently underrepresented in legal frameworks |
| Empower volunteers to support vulnerable groups Psychosocial support can be provided by volunteers, but training, coordination and follow-up structures are needed to ensure quality. The mental health of the volunteers must be taken care of. |
Essential in dealing with migrants and trauma survivors The costs for this must be budgeted. Functioning pre- and post-care by professionals and psychosocial peer support should be guaranteed. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





