1. Introduction
Anomalous Head Position (AHP) is a postural deviation of the head from its physiological alignment with the body's axis [
1]. It can manifest as lateral tilting, horizontal rotation, or alterations in chin elevation and depression, and it may present as combinations of these variations. AHP is a frequently observed clinical sign, with an estimated prevalence of approximately 3% in pediatric populations [
2,
3]. While not a diagnosis in itself, AHP often reflects compensatory mechanisms for ocular, orthopaedic, or neurological dysfunctions. These deviations can alter cervical spine mechanics and create muscle imbalances, which, over time, may lead to chronic pain, postural abnormalities, and other complications [
3,
4,
5,
6,
7].
The causes of AHP can be broadly categorized into ocular and non-ocular causes [
8,
9,
10,
11]. Non-ocular causes are often associated with musculoskeletal abnormalities, including congenital muscular torticollis and facial asymmetry [
12,
13], the third most common congenital musculoskeletal condition in neonates [
14,
15,
16,
17], while ocular causes typically involve the misalignment of the visual axes, prompting affected individuals to adopt compensatory head postures to optimize visual function. These include conditions such as strabismus [
18,
19,
20], nystagmus [
21,
22,
23], congenital syndromes like Duane syndrome [
24,
25], uncorrected refractive errors [
26,
27], and pathologies preventing foveal fixation, such as palpebral ptosis [
28]. Patients with ocular AHP adopt compensatory head positions to enhance visual acuity, achieve single binocular vision, or eliminate diplopia. For example, in cases of superior oblique muscle palsy, patients tend to tilt their head towards the side opposite the affected eye to minimize vertical deviation and stabilize vision [
29]. Understanding the etiology of AHP is essential for accurate diagnosis, as early intervention can prevent secondary complications like facial asymmetry and long-term musculoskeletal issues [
30].
Quantitative measurement of AHP plays a key role in diagnosing its underlying causes and planning surgical or corrective treatments, particularly in pediatric patients where early intervention can significantly improve outcomes in terms of visual function and reduced risk of long-term postural alterations [
31,
32]. In early clinical practice, direct visual observation was a common method for evaluating AHP. However, this approach was found to produce significant measurement errors, with a tendency to overestimate the extent of AHP. Additionally, the accuracy of visual assessments diminished as the severity of AHP increased, with examiner estimates varying by as much as several dozen degrees in cases of more pronounced postural deviations [
33]. Nowadays, various tools are used to measure AHP, ranging from traditional mechanical devices to advanced solutions based on electronic, magnetic, and ultrasound technologies, whose reliability and validity have been studied over the past decades.
Traditionally, mechanical goniometers have been widely used to assess head inclination, rotation, and elevation/depression. While these tools are valued for their affordability and simplicity, their accuracy can be influenced by the operator’s experience, leading to variability in results [
34]. The Cervical Range of Motion (CROM) system represents a significant advancement in the measurement of head posture, combining both gravitational and magnetic inclinometers to allow for accurate measurements of head inclination, rotation, and elevation [
35]. While highly reliable and validated for clinical use, the CROM device can be challenging to adapt for pediatric patients and may cause discomfort during prolonged use [
36,
37,
38].
Innovative technologies originally designed for entertainment, have recently been adapted for AHP measurement. The WiiMote system (Nintendo, Kyoto, Japan), for example, uses infrared sensors and a head-mounted transmitter to capture three-dimensional head posture data. Although affordable, further refinement is needed to ensure its reliability in clinical settings [
39]. The Microsoft Kinect® (Microsoft, Redmond, Washington, United States) sensor, employing depth camera technology, offers a more robust alternative able to reliably track head movements across various angles [
40,
41], and support real-time, non-invasive three-dimensional pose estimation [
42].
Smartphone applications have also emerged as promising tools for measuring AHP, including forward head posture. Leveraging built-in sensors like accelerometers and gyroscopes, these applications deliver reliable assessments of craniovertebral angles and other postural parameters, also providing real-time visual feedback can significantly improve craniovertebral alignment and reduce muscle fatigue [
43].
Validation studies demonstrate the clinical utility of smartphone-based tools, showing high sensitivity and specificity for accurately measuring craniovertebral angles [
44]. Their affordability, ease of use, and potential for integration into telemedicine platforms make smartphone applications a valuable addition to the array of tools for assessing and managing AHP. Finally, 3D optoelectronic motion capture (MoCap) systems represent the gold standard in terms of precision and accuracy to assess the movement kinematics [
45,
46,
47].
A MoCap system uses multiple infrared cameras to detect the position of reflective markers attached to a subject’s body. These markers reflect infrared light emitted by the cameras, allowing the system to track their precise three-dimensional position in space. The cameras capture the markers' movements from different views, and specialized software triangulates the data to calculate the exact location of each marker. By tracking multiple markers, the system can capture the full motion of the subject, reconstructing it into a digital model. However, the technical complexity and high costs make these tools more suitable for research settings than for routine clinical use.
Despite the availability of various measurement instruments, each presents distinct advantages and limitations. Many of these tools are hindered by unresolved issues, such as inadequate precision or the requirement for expensive equipment that may not be accessible in many clinical settings.
In this context, the aim of this study was twofold. First, it evaluated the accuracy of tools commonly used by ophthalmologists to measure AHP by comparing their measurements with those obtained from a gold-standard MoCap system in a pediatric population with AHP. Second, it aimed to detect and quantify the presence of potential limitations in head movements in children with AHP, comparing their motion profiles to those of a control group in terms of range of motion (ROM).
2. Materials and Methods
2.1. Participants
A total of 15 participants (M: 7/F: 8; age: 10.67 ± 2.89 years; weight: 40.61 ± 14.49 kg; height: 149.5 ± 17.33 cm) were voluntarily enrolled in the study at the Pediatric Ophthalmology Clinic at San Giuseppe Hospital in Milan. The main inclusion criteria were: (i) a confirmed diagnosis of AHP of ocular origin, associated with conditions such as strabismus, essential infantile esotropia, nystagmus, refractive errors (e.g., hyperopia, astigmatism, or myopia), eyelid ptosis or visual field defect; (ii) age between 6 and 17 years; and (iii) normal neuropsychological development. Conversely, exclusion criteria included: (i) AHP due to orthopaedic conditions, such as muscular torticollis, spastic torticollis, or cervical spine abnormalities; (ii) neurological disorders such as neoplasms, post-inflammatory central nervous system lesions, psychomotor delays, or syringomyelic malformations; (iii) otolaryngologic conditions, including hearing loss or vestibular pathologies; (iv) rare syndromes such as Sandifer syndrome or functional torticollis; (v) impaired neuropsychological development; and (vi) insufficient compliance during assessments.
A control group (CG) was also included, consisting of 20 individuals (8 males and 12 females) without any visual impairments.
This study was performed in accordance with the ethics standards of the University of Milan with the approval of the study by the ethics committee on 2nd April 2020 (protocol n. 29/20) and with the Declaration of Helsinki 1964 and its latest amendments. As the participants were minors, written informed consent was obtained from their parents or legal representatives prior to enrolment in the study.
2.2. Study Design and Instrumentation
The study was conducted at the “L. Divieti” Posture and Movement Laboratory at Politecnico di Milano (Milan, Italy). The data collection process focused on tracking head position during static and dynamic tests, using different tools. Specifically, measurements were taken using a digital goniometer (DG), an iOS mobile application (eyeTilt, SeeVision, LLC), and a MoCap system (SMART DX 400, BTSBioengineering SpA, Milano, Italy).
2.2.1. Digital Goniometer
The digital goniometer (Figure 1) is an electronic device designed to measure the rotational angle of the head, particularly in ophthalmology, where it plays a key role in the assessment of abnormal head posture. Equipped with high-precision sensors and a digital display, this tool allows for accurate measurement of head rotation relative to a reference axis. During testing, the participant is asked to focus on a fixed point, enabling clinicians to assess eye alignment and detect deviations from the normal head posture. Compared to traditional goniometers, the digital version offers improved accuracy, minimizes manual errors, and facilitates longitudinal monitoring of postural changes.
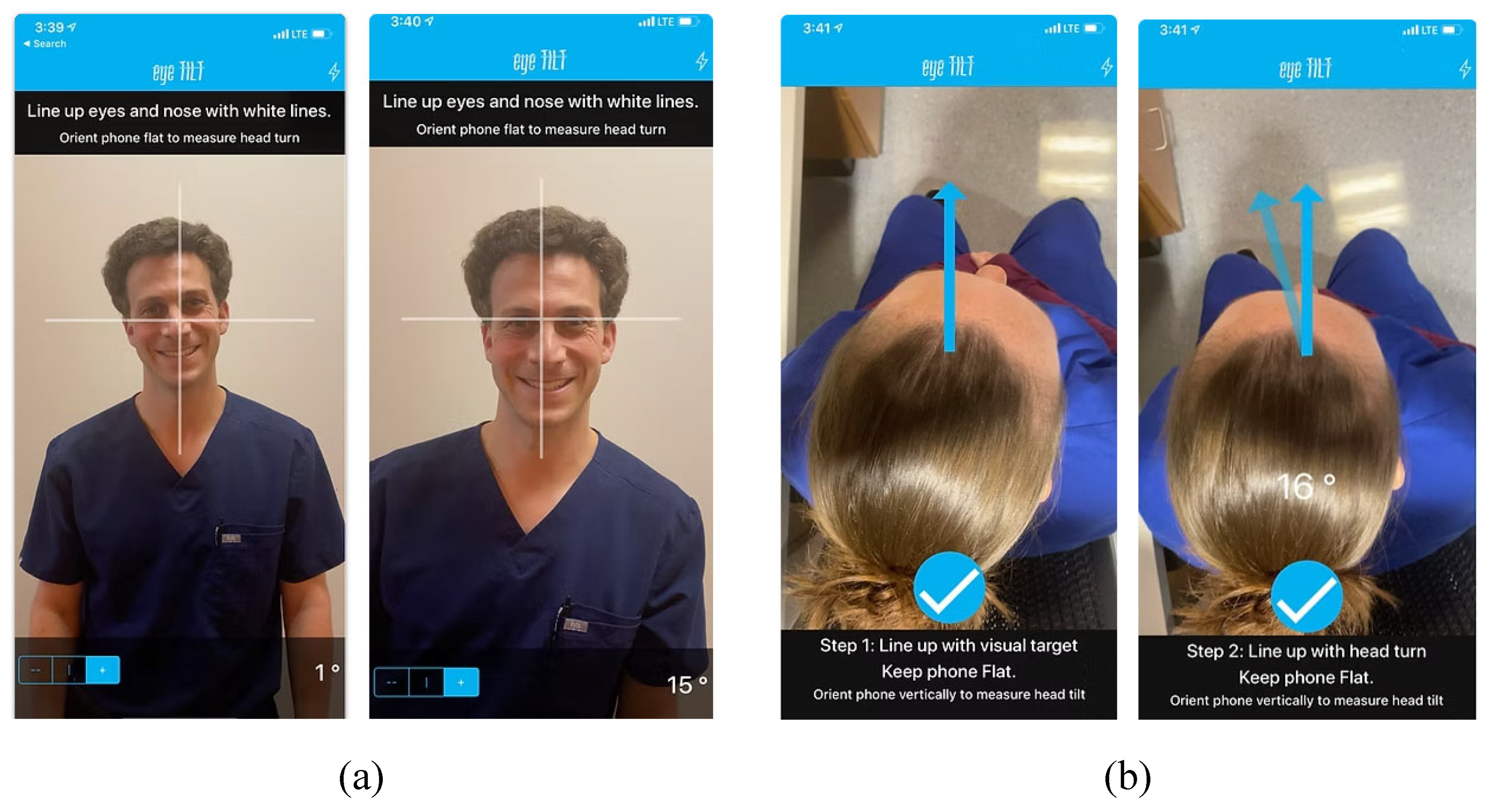
2.2.2. iOS Application
eyeTilt (See Vision, LCC) is an iOS-based mobile application designed for the measurement of head tilt and rotational angles (
Figure 2). Serving as a digital goniometer, the application utilizes the built-in sensors of the iOS device to measure head position relative to a reference axis. The user aligns the device with specific anatomical landmarks, and the apps provides real-time feedback by displaying the angular measurement of head rotation and inclination in degrees. This tool offers an accessible and user-friendly method for postural assessment, making it a valuable resource for tracking and evaluating postural deviations associated with conditions such as torticollis, nystagmus, and strabismus.
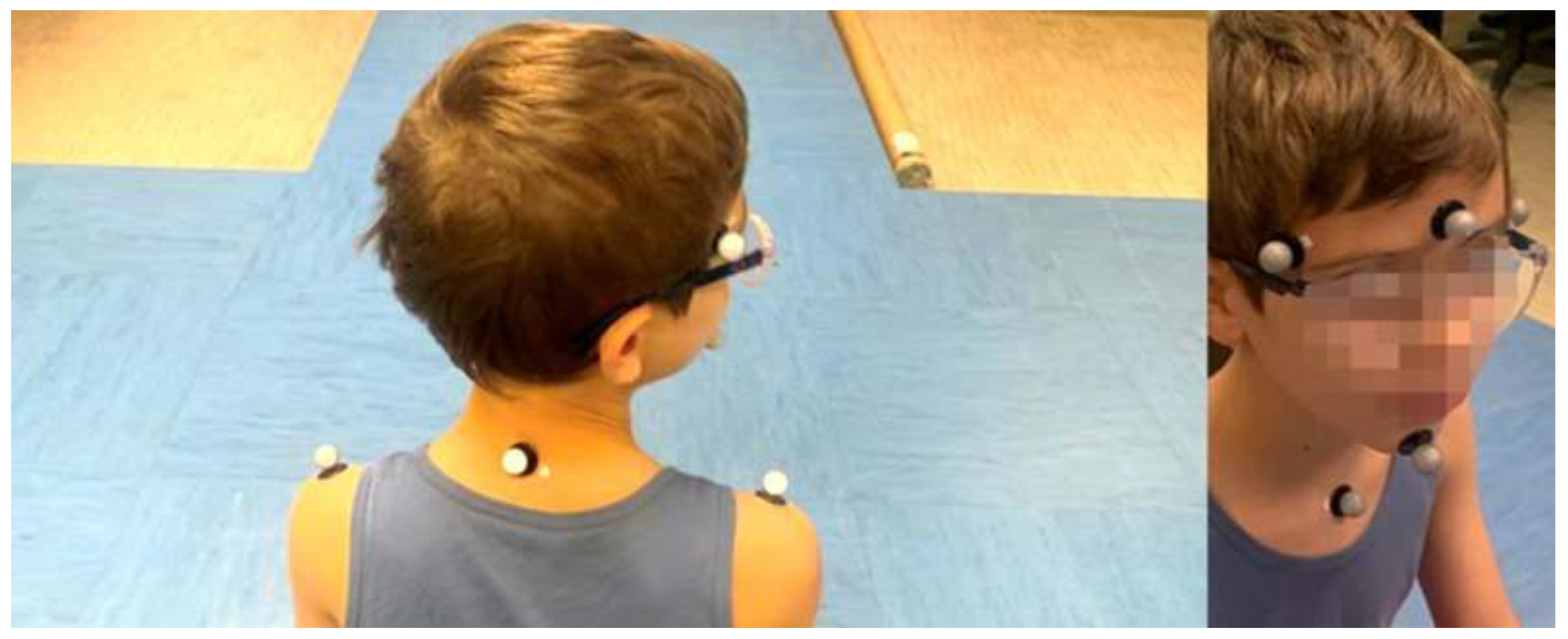
2.2.3. MoCap system
The MoCap system used for optical data collection was the SMART DX 400 system (BTSBioengineering SpA, Milano, Italy), which features eight cameras and operates at a sampling frequency of 100 Hz. A set of eight passive markers was placed on participants’ bodies at the following anatomical landmarks: the right and left temples, glabella, chin, right and left acromion, seventh cerebral vertebra (C7) and jugular notch
(Figure 3) [
49].
2.2.4. Experimental Procedures
Participants from both groups underwent static and dynamic measurements using the previously described tools. All testing sessions were conducted with participants sitting on a chair with their back straight and feet flat on the ground to minimize unwanted trunk movement.
The first set of measurements involved static assessments of AHP. Head rotation was quantified using DG, with participants instructed to gaze at an object placed 5 meters away. Following this, head inclination was measured using the eyeTilt application on an iOS smartphone. Lastly, a 5-second static measurement was performed with the MoCap to obtain quantitative data on both head rotation and inclination. The three-dimensional positions of the markers were used to calculate these angles, employing the same conventions applied during goniometer measurements. Specifically, angles of head rotation and inclination to the subject’s right were considered positive, while angles to the left were assigned negative values. This convention was consistently applied across all measurements to ensure uniformity in data collection.
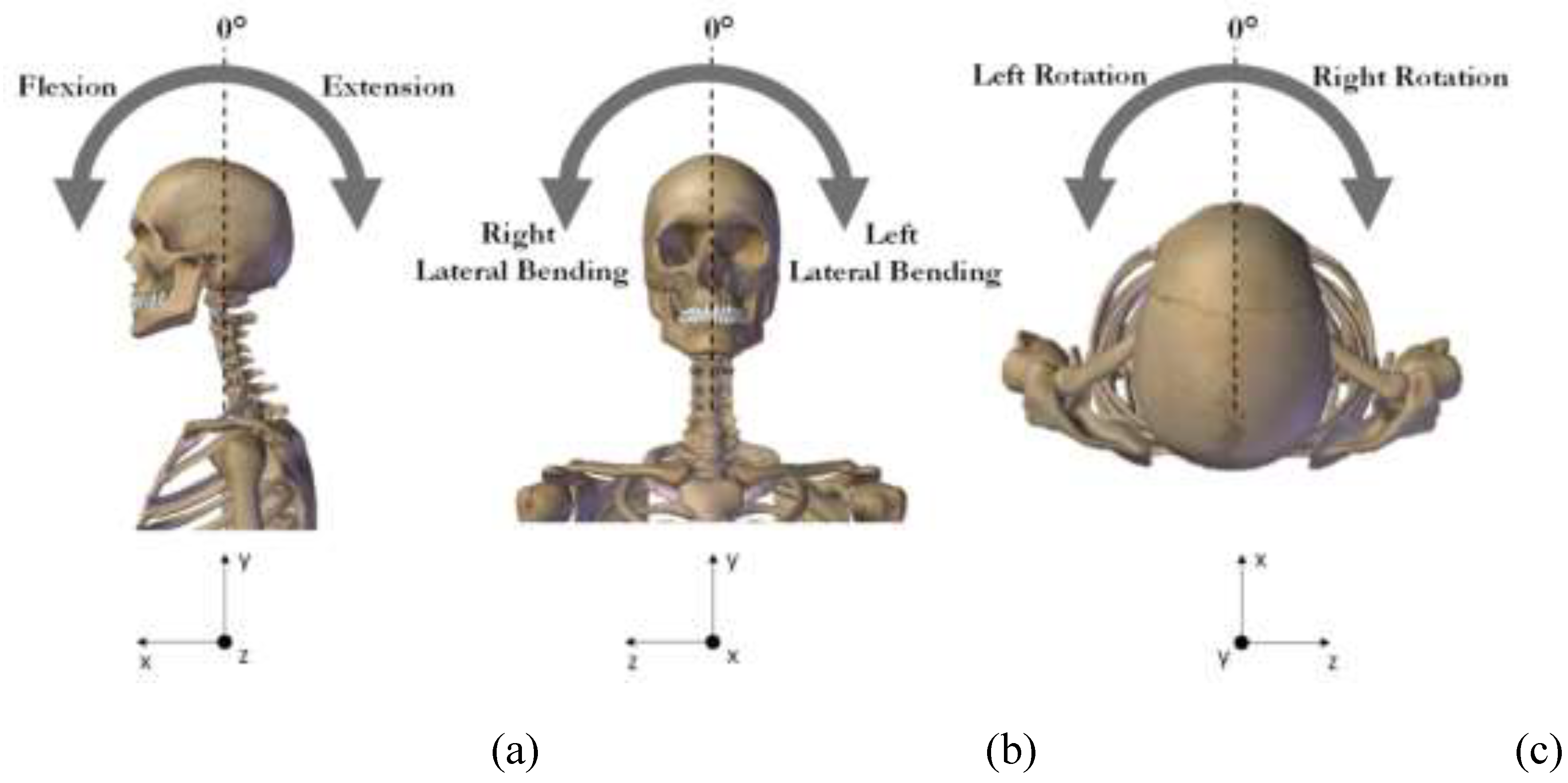
To assess the cervical ROM in participants and compare the measurements with both static head rotation and inclination angles, as well as with the CROM from healthy subjects, participants were instructed to perform specific dynamic movements. Each movement was repeated twice for consistency. The following tasks were performed
(Figure 4):
In addition, an orthodontic evaluation was conducted, by means of intraoral and extraoral photographs for each patient using occlusal mirrors and cheek retractors. Only patients with no prior orthodontic treatment were assessed, as previous treatments may have already compensated for possible anomalies. Furthermore, the absence of permanent first molars, which are considered key teeth for occlusion analysis, is considered exclusion criteria. According to these considerations, only 9 patients were available and thus these data were not included in this study.
2.3. Data Analysis and Parameters
The static measures of head rotation and inclination, taken with DG and the eyeTilt application respectively, were automatically displayed during the assessment and recorded by the operator. Data collected with MoCap were firstly processed using SMARTTracker (BTSBioengineering SpA, Milano, Italy) software. In this step, each marker was manually assigned to its corresponding anatomical landmark. Reconstructed data were then imported into SMARTAnalyzer software (BTSBioengineering SpA, Milano, Italy) for further analysis. Custom routines within the software were employed to compute quantitative measurements. For the static trials, head inclination and rotation angles were calculated. For the dynamic trials, the computed outputs included angles during head flexion/extension, lateral bending, and rotation. The dynamic ROM was subsequently calculated as the difference between the maximum angular displacement achieved during each movement and the neutral head position.
2.4. Statistical Analysis
Statistical analysis was performed with Minitab Statistical Software (2023 Minitab, LLC, State College, Pennsylvania, USA). The data were assessed for normality using the Kolmogorov-Smirnov test, which confirmed a normal distribution. As a result, variables were reported as mean values with their corresponding standard deviations.
For the first objective of the study, measurements obtained using DG and the eyeTilt application were compared to those from the MoCap system during static trials. A paired t-test was performed to identify any statistically significant differences (p < 0.05). To evaluate the relationship between measurements, Pearson’s Correlation Coefficient (PCC) was calculated, describing the level of agreement between the compared systems (i.e., MoCap vs. DG and MoCap vs. eyeTilt). The strength of the correlation was classified as follows: |r| ≤ 0.4, weak; 0.4 < |r| ≤ 0.6, moderate; 0.6 < |r| ≤ 0.8, strong; and |r| > 0.8, very strong [
50].
Additionally, Bland-Altman plots were used to visually assess the level of agreement (LoA) between the paired measurements. The accuracy of the static angular measurements was then computed according to the following equation (Eq. 1):
Additionally, the Root Mean Square Error (RMSE) was computed according to the following equation (Eq.2):
where ŷ
1... ŷ
n represent the head rotation or inclination angles measured using the digital goniometer or the eyeTilt application, while y
1…y
n correspond to the measurements obtained using the MoCap system. The differences between these values, e
1…e
n, denote the errors, and n represents the number of observations (i.e., the number of participants). Low RMSE values, approaching zero, indicate a high level of agreement between the MoCap system and the other measurement tools.
For the second aim of the study, potential limitations in head movements in individuals with AHP were analyzed during dynamic head movements. Unpaired t-tests were conducted to compare the ROM values for individuals with AHP with those of the control group. All statistical tests were performed with a significance level set at α = 0.05.
3. Results
3.1. Comparison between MoCap and Ophthalmologic Tools
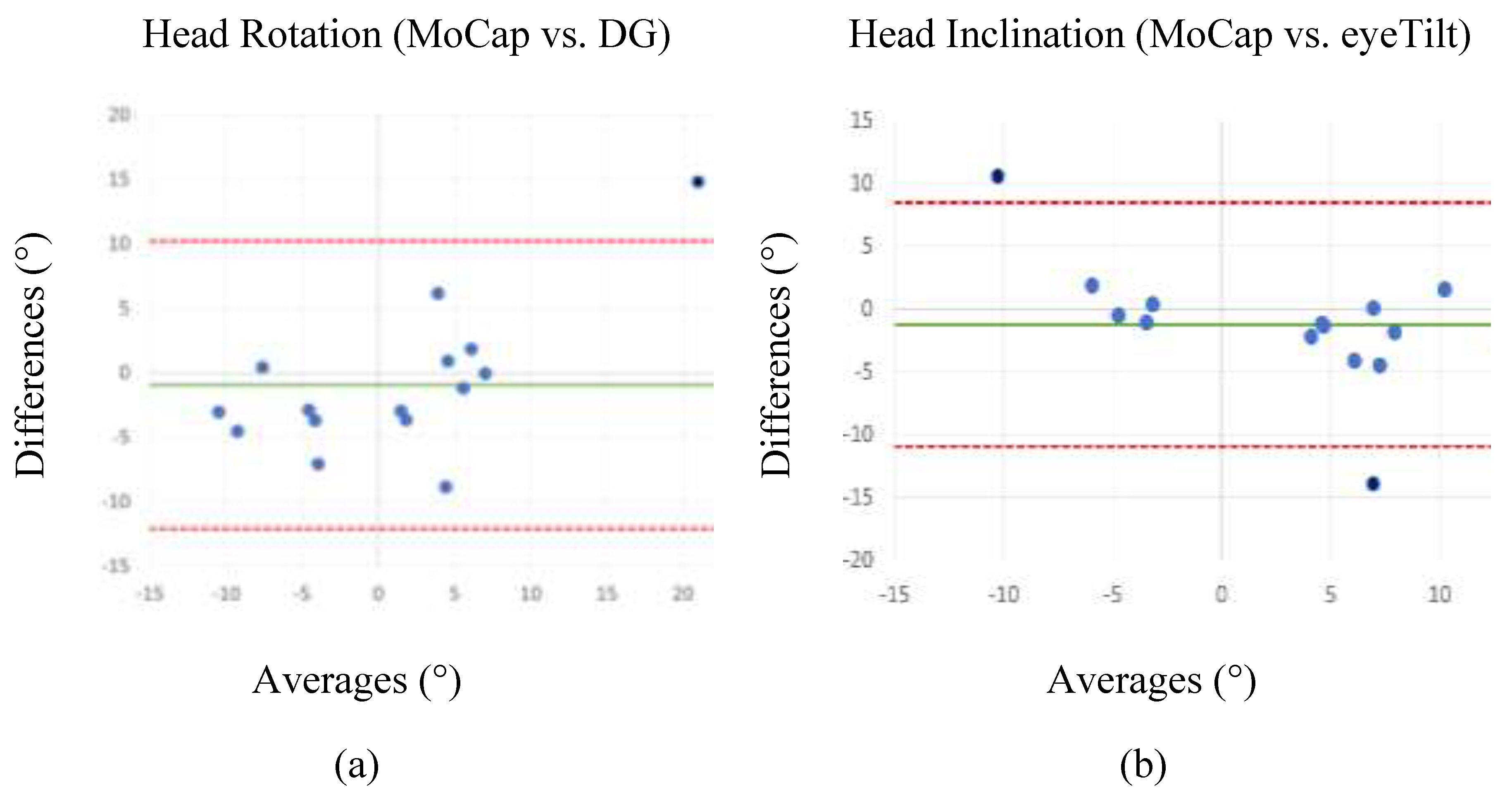
Table 1 provides an overview of the mean values and standard deviations for head rotation and inclination angles in static position, measured using ophthalmologic tools (i.e., digital goniometer for head rotation and eyeTilt application for head inclination) and MoCap system in individuals with AHP. The table also includes PCC, RMSE, and accuracy values for the comparisons between the measurements from the ophthalmological tools and the MoCap system.
Overall, the results highlight a high degree of concordance between ophthalmological tools and the MoCap, supporting their validity for clinical assessment. The measurements demonstrate consistency across the systems, as reflected by the accuracy and RMSE values, and by the absence of statistically significant inter-system differences (p > 0.05) at paired t-test. This consistency is further supported by PCC values, which indicate very strong, statistically significant correlations (PCC > 0.8; p < 0.05) between MoCap and the other tools.
Figure 5 presents the Bland-Altman plots comparing the head rotation and inclination angles obtained from the digital goniometer and the eyeTilt application, respectively, and the MoCap system. The horizontal lines in the plots represent the mean difference and the LoA, defined as the mean difference ± 1.96 * standard deviation. Conversely, the differences between the two paired values are plotted on the vertical axis, while their mean values are reported on the horizontal axis. Although a few measurements fall outside the LoA, no significant bias was observed, with the 95% of the differences falling within the LoA. This indicates a generally good agreement between the compared systems, consistent with the results presented in
Table 1.
3.2. Assessment of head movement limitations in individuals with AHP
Table 2 presents the mean values and standard deviation of cervical ROM for dynamic head movements acquired with MoCap, measured in both individuals with AHP and CG, together with the results of unpaired t-tests conducted to detect potential differences between the two groups. Statistically significant differences (p < 0.05) were found in the flexion angle while no significant differences (p > 0.05) were found for the other tasks.
4. Discussion
AHP is a compensatory mechanism that helps individuals optimize visual input in response to visual impairments. This phenomenon is evident in conditions such as nystagmus and strabismus, where patients adopt specific head positions to reduce visual disturbances. For example, patients with nystagmus often present abnormal head positions, typically as a head turn, to minimize involuntary eye movements and improve focus [
51,
52]. Understanding and accurately measuring AHP important for evaluating post-treatment changes and planning potential surgical interventions, especially in pediatric population. Timely interventions not only improve visual function but also prevent long-term musculoskeletal issues resulting from untreated ocular torticollis.
Over time, various tools have been developed to measure AHP, ranging from traditional manual goniometer to advanced electronic, magnetic, ultrasound-based systems, and visual-based solutions like Microsoft Kinect and smartphone applications. Despite their availability, these tools are hindered by limitations, such as issues with precision, high costs, and practical challenges in clinical settings which limit their accessibility to a broader population. In response to the need for a practical, efficient, and cost-effective tool capable of delivering clinically valid assessments, the primary objective of this study was to assess the accuracy of more accessible ophthalmological tools—digital goniometer and the iOS-based eyeTilt application—against a gold standard MoCap system.
The results demonstrated that both tools assessed in this study provided accurate measurements comparable to those obtained from the MoCap. High PCC (> 0.7) and p-values exceeding the significance threshold indicated very strong inter-system agreement, further supported by the corresponding RMSE values. Notably, RMSE was lower for head rotation (3.43°) compared to head inclination (5°). Bland-Altman plots also confirmed the general agreement between the measurement tools, with 95% of data points within the confidence interval.
The findings align with existing literature that supports the clinical utility of digital tools for assessing AHP. Although manual goniometers have long been used in clinical practice to effectively measure head posture and in diagnosing of conditions like torticollis or strabismus [
53,
54], advancements in technology have introduced new tools, such as digital devices smartphone applications, as significant steps toward more precise, accessible, and cost-effective solutions for assessing and monitoring AHP. Digital goniometers address many of the limitations of traditional tools by offering enhanced precision with digital readouts, eliminating parallax errors and minimizing user dependency for accurate positioning [
55]. Moreover, they can provide real-time feedback, dynamic angle tracking, and data storage, which improve both accuracy and clinical efficiency.
Smartphone applications, on the other hand, use built-in sensors such as accelerometer and gyroscopes to measure head rotation and inclination. These apps eliminate the need for precise manual positioning and reduce user error, while offering real-time data collection and analysis [
56,
57]. Moreover, smartphone-based applications offer dynamic feedback and facilitate long-term monitoring, capturing variations in head posture across different scenarios. For instance, by integrating features such as data visualization, tele-medicine compatibility, and patient education modules, these tools can support a multidisciplinary approach to AHP management and adjustments to treatment plans, complementing existing methods and expanding access to effective care.
The second aim of this study was to detect and quantify potential limitations in cervical ROM in individuals with AHP compared to age-matched healthy controls. Using the MoCap system, significant differences (p< 0.05) in head flexion angles between individuals with AHP and healthy controls.
AHP of ocular origin is a multifaceted issue involving ocular, musculoskeletal, and neurological factors. Differences in ROM in the frontal plane are likely linked to the compensatory mechanisms adopted by individuals with AHP. For example, children with nystagmus may adopt a "null position" tilting the head to reduce involuntary eye movements and enhance visual focus [
58]. Similarly, patients with superior oblique palsy often tilt their heads toward the affected side to maintain binocular vision [
59]. Research suggests that ocular causes of AHP often allow for greater neck mobility compared to non-ocular causes, which may result in restricted neck movements due to muscular or orthopaedic issues. This distinction is critical, as prolonged AHP can lead to secondary musculoskeletal complications, including cervical muscle imbalances and reduced neck mobility over time [
60,
61,
62]. These findings underscore the importance of a multidisciplinary approach involving ophthalmology, neurology, and physical therapy to address the interplay between ocular conditions and neck posture effectively.
While the study's findings are promising, they should be interpreted cautiously due to the small sample size. Future research should include larger cohorts and categorize patients by specific diagnoses (e.g., strabismus and nystagmus) to better understand variations in AHP. For instance, patients with strabismus often exhibit head rotation, while those with nystagmus show head inclination. Incorporating variables such as chin-up and chin-down angles, and assessing head posture before and after visual correction, could further clarify the impact of AHP on posture and dynamics. Exploring these factors would enhance the development of targeted interventions to improve outcomes for patients with AHP. Furthermore, a larger dataset would provide the opportunity to incorporate orthodontic assessments into the results, allowing for a more thorough analysis of the potential relationship between malocclusions and AHP.
Building on these findings, this study highlights the potential of accessible and cost-effective tools, such as digital goniometers and smartphone applications, to improve the assessment and management of AHP. The dynamic evaluation of AHP offers valuable insights into compensatory mechanisms and their impact on movement and stability, paving the way for targeted interventions and better patient outcomes. Expanding research in this area will enhance the ability to develop effective, multidisciplinary treatment strategies and broaden access to care across diverse populations.
Author Contributions
Conceptualization, G.B., P.N. and V.C.; methodology, G.B., F.B. and E.V.; software, F.A.; formal analysis, S.C.; data curation, S.C.; writing—original draft preparation, S.C.; F.B. and G.B. writing—review and editing, L.D., F.A., M.G., F.N., E.V., P.N. and V.C.; supervision, G.B. and V.C.. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The study was approved by the Ethics Committee of the University of Milan on 2nd April 2020 (protocol n. 29/20).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Dataset available on request from the authors
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| AHP |
Anomalous Head Posture |
| ROM |
Range of Motion |
| DG |
Digital Goniometer |
References
- Akbari, M.R.; Khorrami-Nejad, M.; Kangari, H.; Akbarzadeh Baghban, A.; Ranjbar Pazouki, M. Ocular Abnormal Head Posture: A Literature Review. J. Curr. Ophthalmol. 2021, 33, 379–387. [Google Scholar] [CrossRef]
- Mitchell, P.R. Ocular torticollis. Trans. Am. Ophthalmol. Soc. 1999, 97, 697–769. [Google Scholar] [PubMed]
- Nucci, P.; Kushner, B.J.; Serafino, M.; Orzalesi, N. A multi-disciplinary study of the ocular, orthopedic, and neurologic causes of abnormal head postures in children. Am. J. Ophthalmol. 2005, 140, 65–68. [Google Scholar] [CrossRef]
- Caldeira, J.A. Abnormal head posture: an ophthalmological approach. Binocul. Vis. Strabismus Q. 2000, 15, 237–239. [Google Scholar] [PubMed]
- Campobasso, A.; Di Cosola, M.; Testa, N.F.; Lacarbonara, V.; Dioguardi, M.; Lo Muzio, L.; Lo Muzio, E.; Scarpa, M.; Covelli, M.; Crincoli, V.; et al. The influence of abnormal head posture on facial asymmetry. J. Biol. Regul. \& Homeost. Agents 2022, 36, 325–335. [Google Scholar]
- Yadegari, S. Approach to abnormal head posture. Strabismus 2024, 32, 287–293. [Google Scholar] [CrossRef]
- Davitt, B. V Abnormal Head Postures: A Review. Am. Orthopt. J. 2001, 51, 137–143. [Google Scholar] [CrossRef]
- Amaral, D.M.; Cadilha, R.P.B.S.; Rocha, J.A.G.M.; Silva, A.I.G.; Parada, F. Congenital muscular torticollis: where are we today? A retrospective analysis at a tertiary hospital. Porto Biomed. J. 2019, 4, e36. [Google Scholar] [CrossRef]
- Ballock, R.T.; Song, K.M. The prevalence of nonmuscular causes of torticollis in children. J. Pediatr. Orthop. 1996, 16, 500–504. [Google Scholar] [CrossRef]
- Khorrami-Nejad, M.; Akbari, M.; Kangari, H.; Baghban, A.A.; Pazouki, M.R. Ocular Abnormal Head Posture. J. Curr. Ophthalmol. 2021.
- Kushner, B.J. Ocular causes of abnormal head postures. Ophthalmology 1979, 86, 2115–2125. [Google Scholar] [CrossRef]
- Rao, R.; Morton, G. V; Kushner, B.J. Ocular torticollis and facial asymmetry. Binocul. Vis. Strabismus Q. 1999, 14, 27–32. [Google Scholar] [PubMed]
- Nilesh, K.; Mukherji, S. Congenital muscular torticollis. Ann. Maxillofac. Surg. 2013, 3. [Google Scholar] [CrossRef] [PubMed]
- Kaplan, S.L.; Coulter, C.; Sargent, B. Physical Therapy Management of Congenital Muscular Torticollis: A 2018 Evidence-Based Clinical Practice Guideline From the APTA Academy of Pediatric Physical Therapy. Pediatr. Phys. Ther. Off. Publ. Sect. Pediatr. Am. Phys. Ther. Assoc. 2018, 30, 240–290. [Google Scholar] [CrossRef]
- Sudesh, P.; Bali, K.; Mootha, A.K.; Dhillon, M.S. Results of Bipolar Release in the Treatment of Congenital Muscular Torticolis in Patients Older Than 10 Years of Age. J. Child. S Orthop. 2010. [CrossRef] [PubMed]
- Cheng, J.C.Y.; Au, A.W.Y. Infantile Torticollis: A Review of 624 Cases. J. Pediatr. Orthop. 1994, 14. [Google Scholar] [CrossRef]
- Herman, M.J. Torticollis in infants and children: common and unusual causes. Instr. Course Lect. 2006, 55, 647–653. [Google Scholar]
- Wang, P.; Lou, L.; Song, L.; 2011. Design and Efficacy of Surgery for Horizontal Idiopathic Nystagmus With Abnormal Head Posture and Strabismus. J. Huazhong Univ. Sci. Technol. [Medical Sci. 2011. [Google Scholar]
- Turan, K.E.; Şekeroğlu, H.T.; Koç, İ.; Vural, E.; Karakaya, J.; Şener, E.C.; Sanaç, A.Ş. Ocular Causes of Abnormal Head Position: Strabismus Clinic Data. Turkish J. Ophthalmol. 2017.
- Reddy, A.C.; Portilla, A.; Donahue, S.P. Purely horizontal strabismus associated with head tilt. J. AAPOS Off. Publ. Am. Assoc. Pediatr. Ophthalmol. Strabismus 2018, 22, 69–71. [Google Scholar] [CrossRef]
- Noval, S.; González-Manrique, M.; Valle, J.M.R.-D.; Rodríguez-Sánchez, J.M. Abnormal Head Position in Infantile Nystagmus Syndrome. Isrn Ophthalmol. 2011. [CrossRef]
- Teodorescu, L. ANOMALOUS HEAD POSTURES IN STRABISMUS AND NYSTAGMUS DIAGNOSIS AND MANAGEMENT. Rom. J. Ophthalmol. 2015, 59, 137–140. [Google Scholar] [PubMed]
- Papageorgiou, E.; McLean, R.J.; Gottlob, I. Nystagmus in childhood. Pediatr. Neonatol. 2014, 55, 341–351. [Google Scholar] [CrossRef] [PubMed]
- Zanin, E.; Gambarelli, N.; Denis, D. Distinctive Clinical Features of Bilateral Duane Retraction Syndrome. J. Am. Assoc. Pediatr. Ophthalmol. Strabismus 2010. [CrossRef]
- Akbari, M.R.; Manouchehri, V.; Mirmohammadsadeghi, A. Surgical treatment of Duane retraction syndrome. J. Curr. Ophthalmol. 2017, 29, 248–257. [Google Scholar] [CrossRef]
- Carreira, F.; Pereira, B.; Rodrigues, M.; Borges, M.; Silva, S.; Sá, C. Postural Changes in Adolescents With Refractive Errors. Revsalus - Rev. Científica Da Rede Académica Das Ciências Da Saúde Da Lusofonia, 2024. [Google Scholar]
- Havertape, S.A.; Cruz, O.A. Abnormal head posture associated with high hyperopia. J. AAPOS Off. Publ. Am. Assoc. Pediatr. Ophthalmol. Strabismus 1998, 2, 12–16. [Google Scholar] [CrossRef] [PubMed]
- Wu, P.; Ma, J.; Zhang, T.; Ma, D. Advances in the Genetics of Congenital Ptosis. Ophthalmic Res. 2021. [CrossRef]
- Kushner, B.J. The influence of head tilt on ocular torsion in patients with superior oblique muscle palsy. J. AAPOS Off. Publ. Am. Assoc. Pediatr. Ophthalmol. Strabismus 2009, 13, 132–135. [Google Scholar] [CrossRef]
- Akbari, M.R.; Khorrami Nejad, M.; Askarizadeh, F.; Pour, F.F.; Ranjbar Pazooki, M.; Moeinitabar, M.R. Facial asymmetry in ocular torticollis. J. Curr. Ophthalmol. 2015, 27, 4–11. [Google Scholar] [CrossRef]
- Kraft, S.P.; O’Donoghue, E.P.; Roarty, J.D. Improvement of compensatory head postures after strabismus surgery. Ophthalmology 1992, 99, 1301–1308. [Google Scholar] [CrossRef]
- Kraft, S.P. Oblique Muscle Surgery for Head Tilt Caused by Congenital Motor Nystagmus. Am. Orthopt. J. 1996, 46, 143–149. [Google Scholar] [CrossRef]
- Burchell, V.-J.; Arblaster, G.; Buckley, D.; Wheat, J. Is a Depth Camera in Agreement with an Electromagnetic Tracking Device when Measuring Head Position? Br. Ir. Orthopt. J. 2021, 17, 142–149. [Google Scholar] [CrossRef] [PubMed]
- Raya, R.; Garcia-Carmona, R.; Sanchez, C.; Urendes, E.; Ramirez, O.; Martin, A.; Otero, A. An Inexpensive and Easy to Use Cervical Range of Motion Measurement Solution Using Inertial Sensors. Sensors 2018, 18. [Google Scholar] [CrossRef] [PubMed]
- Kushner, B.J. The usefulness of the cervical range of motion device in the ocular motility examination. Arch. Ophthalmol. (Chicago, Ill. 1960) 2000, 118, 946–950. [Google Scholar]
- Tousignant, M.; Smeesters, C.; Breton, A.-M.; Breton, E.; Corriveau, H. Criterion validity study of the cervical range of motion (CROM) device for rotational range of motion on healthy adults. J. Orthop. Sports Phys. Ther. 2006, 36, 242–248. [Google Scholar] [CrossRef]
- Tousignant, M.; Duclos, E.; Laflèche, S.; Mayer, A.; Tousignant-Laflamme, Y.; Brosseau, L.; O’Sullivan, J.P. Validity study for the cervical range of motion device used for lateral flexion in patients with neck pain. Spine (Phila. Pa. 1976). 2002, 27, 812–817. [Google Scholar] [CrossRef]
- Fletcher, J.P.; Bandy, W.D. Intrarater reliability of CROM measurement of cervical spine active range of motion in persons with and without neck pain. J. Orthop. Sports Phys. Ther. 2008, 38, 640–645. [Google Scholar] [CrossRef]
- Kim, J.; Nam, K.W.; Jang, I.G.; Yang, H.K.; Kim, K.G.; Hwang, J.-M. Nintendo Wii remote controllers for head posture measurement: accuracy, validity, and reliability of the infrared optical head tracker. Invest. Ophthalmol. Vis. Sci. 2012, 53, 1388–1396. [Google Scholar] [CrossRef]
- Yamamoto, M.; Yagasaki, T.; Ichikawa, S.; Nakamura, T.; Konishi, Y. Accuracy and Correlation of the Kinect-Based Semi-Automatic Scoring Method for Measuring Anomalous Head Posture as Compared to the CROM® Device. Clin. Ophthalmol. 2022. [CrossRef]
- Oh, B.L.; Kim, J.; Kim, J.; Hwang, J.; Lee, J. Validity and Reliability of Head Posture Measurement Using Microsoft Kinect. Br. J. Ophthalmol. 2014. [CrossRef]
- Darby, J.; Sánchez, M.B.G.; Butler, P.B.; Loram, I.D. An Evaluation of 3D Head Pose Estimation Using the Microsoft Kinect V2. Gait \& Posture, 2016. [Google Scholar]
- Kim, S.J.; Jeong, S.H.; Yoon, T.L. The Effect of Visual Feedback of Head Angles With Using a Mobile Posture-Aware System on Craniocervical Angle and Neck and Shoulder Muscles Fatigue During Watching the Smartphone. J. Korean Phys. Ther. 2018. [CrossRef]
- Gallego-Izquierdo, T.; Arroba-Díaz, E.; García-Ascoz, G.; Val-Cano, M.D.A.; Pecos-Martín, D.; Cano-de-la-Cuerda, R. Psychometric Proprieties of a Mobile Application to Measure the Craniovertebral Angle a Validation and Reliability Study. Int. J. Environ. Res. Public Health 2020. [CrossRef]
- Duc, C.; Salvia, P.; Lubansu, A.; Feipel, V.; Aminian, K. A wearable inertial system to assess the cervical spine mobility: Comparison with an optoelectronic-based motion capture evaluation. Med. Eng. Phys. 2014, 36, 49–56. [Google Scholar] [CrossRef] [PubMed]
- Williams, M.A.; McCarthy, C.J.; Chorti, A.; Cooke, M.W.; Gates, S. A Systematic Review of Reliability and Validity Studies of Methods for Measuring Active andPassive Cervical Range of Motion. J. Manipulative Physiol. Ther. 2010, 33, 138–155. [Google Scholar] [CrossRef] [PubMed]
- Ferrario, V.F.; Sforza, C.; Serrao, G.; Grassi, G.; Mossi, E. Active range of motion of the head and cervical spine: a three-dimensional investigation in healthy young adults. J. Orthop. Res. 2002, 20, 122–129. [Google Scholar] [CrossRef]
- Lee, Y.; Park, D.; Kim, Y. The effect of wearing a head-mounted display on the boundaries of the cervical range of motion based on perceived comfort in a static posture. Virtual Real. 2022, 27. [Google Scholar] [CrossRef]
- Palmieri, M.; Donno, L.; Cimolin, V.; Galli, M. Cervical Range of Motion Assessment through Inertial Technology: A Validity and Reliability Study. Sensors (Basel). 2023, 23. [Google Scholar] [CrossRef]
- Akoglu, H. User’s guide to correlation coefficients. Turkish J. Emerg. Med. 2018, 18, 91–93. [Google Scholar] [CrossRef]
- Kang, N.Y.; Isenberg, S.J. Kestenbaum Procedure With Posterior Fixation Suture for Anomalous Head Posture in Infantile Nystagmus. Graefe S Arch. Clin. Exp. Ophthalmol. 2009.
- Porro, G.L.; Linden, D. van der; Nieuwenhuizen, O. van; Wittebol–Post, D. Role of Visual Dysfunction in Postural Control in Children With Cerebral Palsy. Neural Plast. 2005.
- Silverson, O.; Cascia, N.; Hettrich, C.M.; Heebner, N.R.; Uhl, T.L. Reliability and Validity of a Clinical Assessment Tool for Measuring Scapular Motion in All 3 Anatomical Planes. J. Athl. Train. 2020.
- Irving, F.; Russell, J.A.; Smith, T. Reliability of Knee Joint Position Sense Measurement: A Comparison Between Goniometry and Image Capture Methods. Eur. J. Physiother. 2016.
- Szczygieł, E.; Fudacz, N.; Golec, J.; Golec, E. The Impact of the Position of the Head on the Functioning of the Human Body: A Systematic Review. Int. J. Occup. Med. Environ. Health 2020.
- Farah, M. de L.; M, S.; Carvalho, L.E.M.R. de; Uesugui, C.F.; Barcellos, R.B. Using a Smartphone as a Tool to Measure Compensatory and Anomalous Head Positions. Arq. Bras. Oftalmol. 2018. [Google Scholar]
- Keogh, J.W.L.; Cox, A.J.; Anderson, S.L.; Liew, B.X.W.; Olsen, A.; Schram, B.; Furness, J. Reliability and Validity of Clinically Accessible Smartphone Applications to Measure Joint Range of Motion: A Systematic Review. PLoS One 2019.
- Costa, A.C.R.V. da; Lopes, M.C.B.; Nakanami, C.R. Influence of Head Posture on the Visual Acuity of Children With Nystagmus. Arq. Bras. Oftalmol. 2014.
- Qiu, X.; Wang, Z.; Pan, L.; Shen, T.; Deng, D.; Chen, Q.; Yan, J. Use of a Microelectromechanical Systems Sensor for Objective Measurements of Abnormal Head Posture in Congenital Superior Oblique Palsy Patients. Transl. Vis. Sci. \& Technol. 2024. [Google Scholar]
- Narayanappa, D.; Rajani, H.S.; Anita, T.G.; Nagaraj, R. A Case of Ocular Torticollis. Oman Med. J. 2013.
- Nucci, P.; Curiel, B. Abnormal Head Posture due to Ocular Problems- A Review. Curr. Pediatr. Rev. 2009, 5, 105–111. [Google Scholar] [CrossRef]
- Subbarayalu, A. V; Ameer, M.A. Relationships among head posture, pain intensity, disability and deep cervical flexor muscle performance in subjects with postural neck pain. J. Taibah Univ. Med. Sci. 2017, 12, 541–547. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).