Submitted:
09 July 2023
Posted:
11 July 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
2.1. Outcome measures
2.1.1. Posture measurement
2.1.2. Gait and jump paramters
- A-Walking
- Cadence (steps/min): number of steps taken by the participant in one minute.
- Speed (m/s): average walking speed.
- Stride length (m): average value of distances between each initial contact and the next one of the same sides.
- %Stride length (%height): Stride length normalized over the height of the subject.
- This includes all the steps taken by the patient during the trial showcased by initial contact and foot off (thus showcasing the symmetry between right and left steps, and the symmetry between steps taken on each side respectively.
- Different graphs representing left and right gait cycles starting with stance phase, shown via initial contact (0%), and the next initial contact on the same foot (100%), in addition to toe off (represented using a dotted line) to signal the start of the stride phase
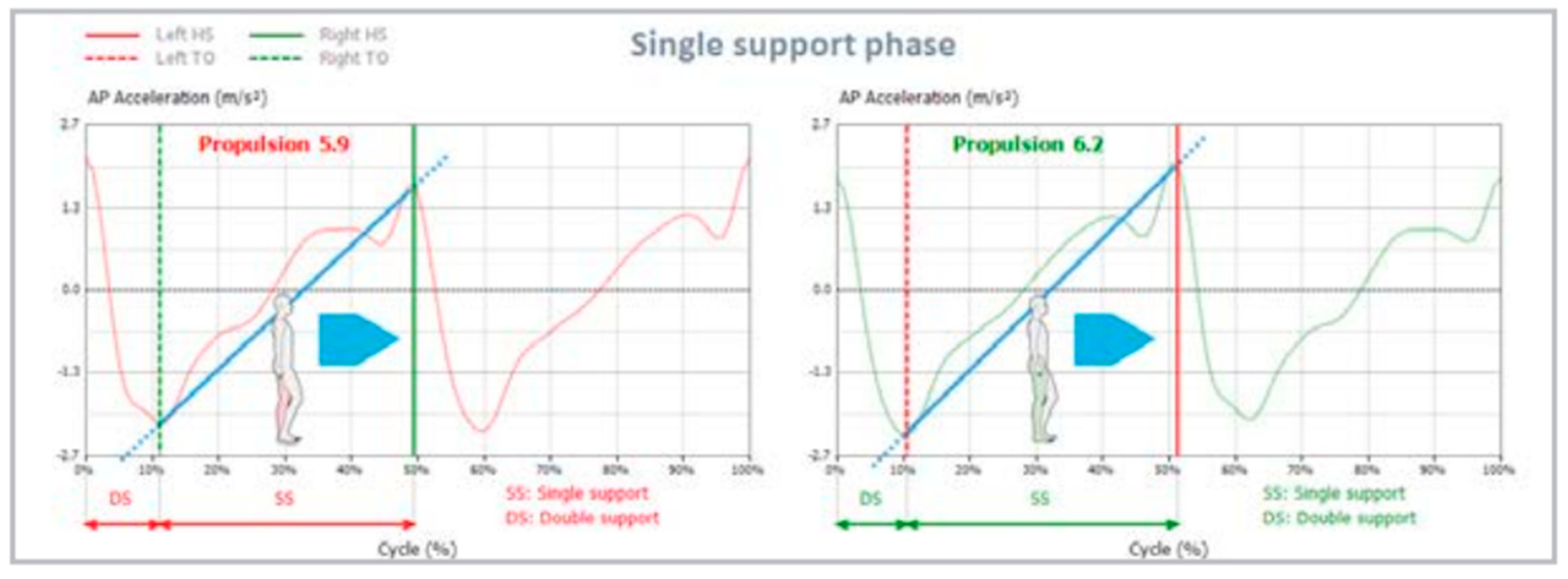
- Symmetry index, which is the percentage of symmetry between the curve of anterior/posterior acceleration during left and right gait cycles, the maximum value of 100 represents ideal symmetry throughout walking.

- Propulsion (represented using a blue line), in addition to propulsion index (represented using the slope of the blue line) where more “vertical” lines indicate higher propulsion indices, thus, better propulsion symmetry between both sides.
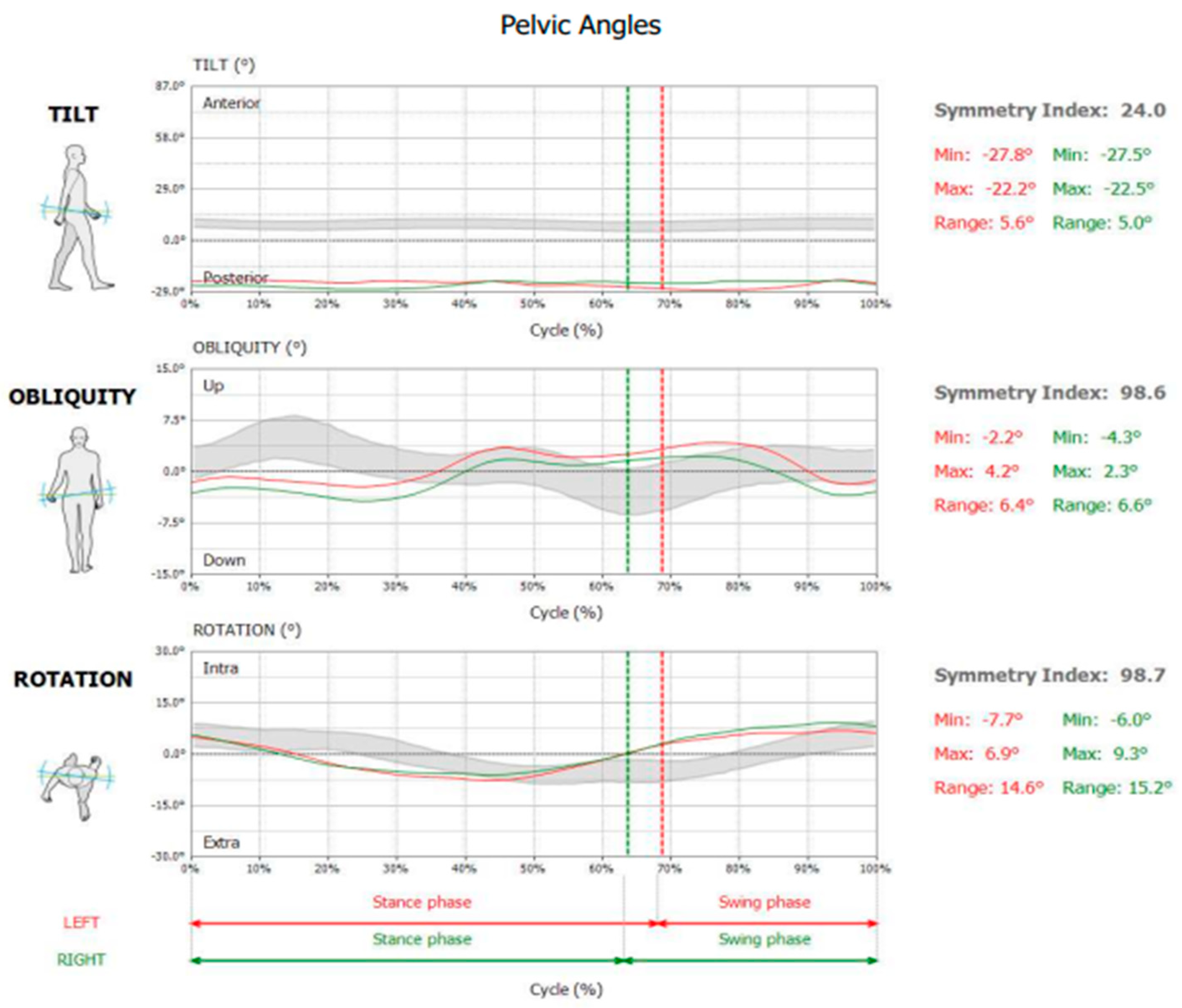
- Tilt: positive angular values indicate an anterior tilt of the pelvis, while negative angular values indicate a posterior tilt of the pelvis (sagittal plane movement).
- Obliquity: negative angular values indicate DOWN condition, while positive angular values indicate UP position for the considered side (frontal plane movement).
- Rotation: negative angular values indicate pelvis internally rotated, while positive angular values indicate a pelvis externally rotated (transverse plane movement).
- Relative symmetry index, minimum and maximum angles were shown for each of the 3 pelvic parameters mentioned above.
- B-Jumping
- 1-
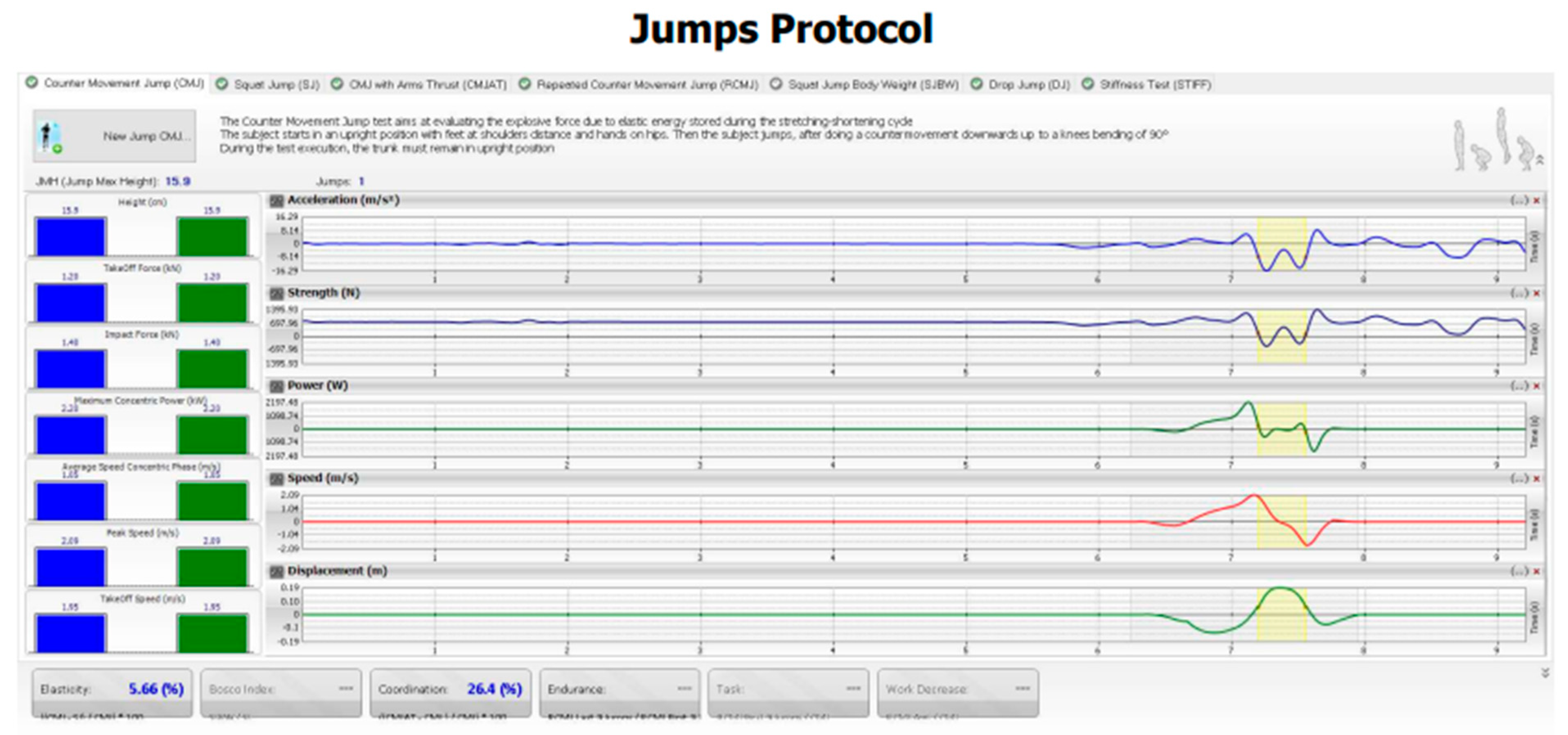
- Counter Movement Jump (CMJ)
- The participant begins the test in upright position with their hands on the hips and their feet placed in line with the shoulders. They are then instructed to jump by performing a countermovement towards the downward direction and bending their knees by 90°. During the entire course of the test, the trunk should remain upright with hands near the hips (Figure 5).
- 2-
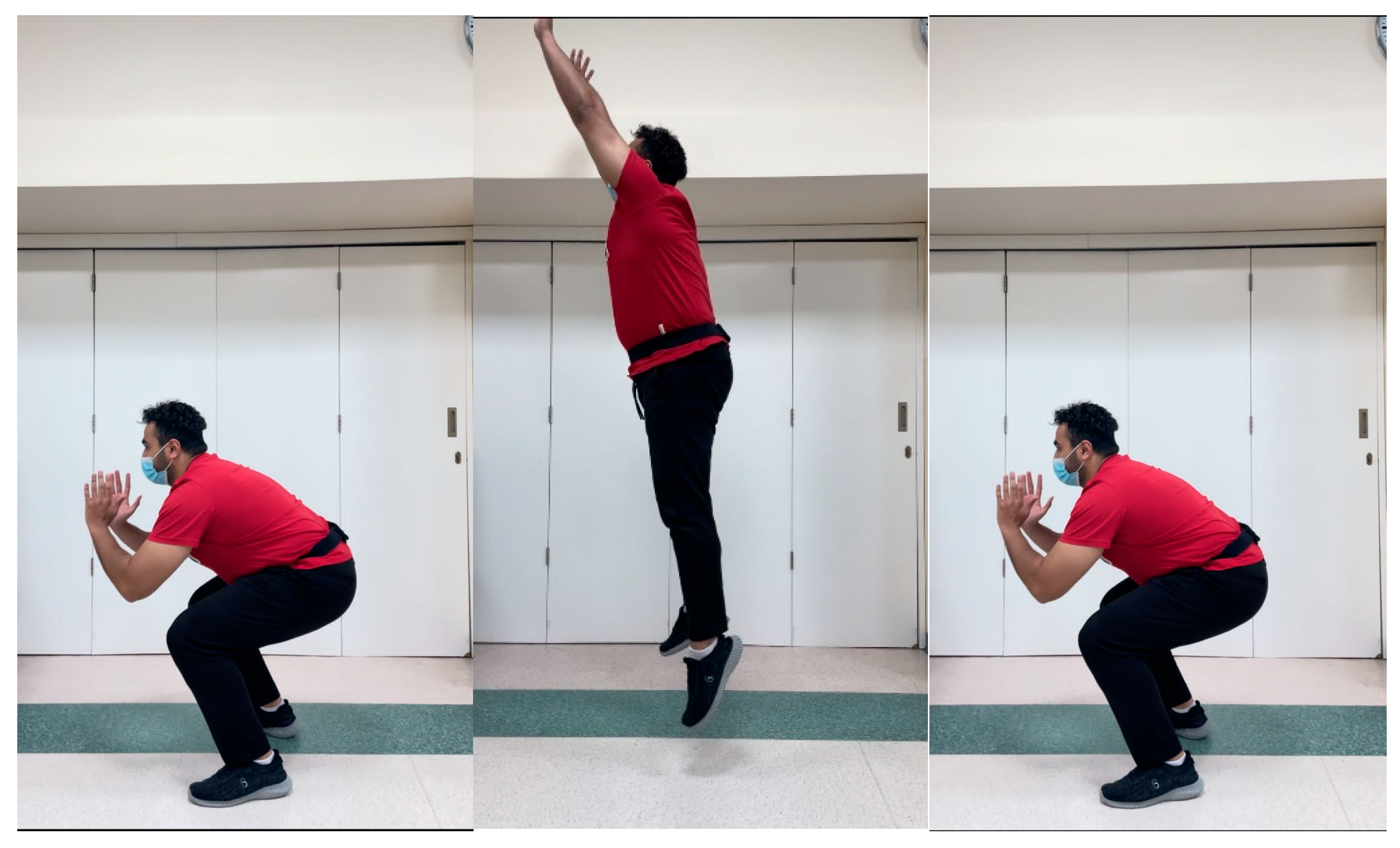
- CMJ with Arms Thrust (CMJAT)
- The participant begins the test in upright position with their hands on the sides and their feet placed in line with the shoulders. They are then instructed to jump by performing a countermovement towards the downward direction and bending their knees by 90°, with the help of using their arms as they extended them upwards. During the entire course of the test, the trunk should remain upright with arms and hands extending upwards in a thrust maneuver (Figure 6).

- Flight Height (cm)
- Take-Off Force (kN)
- Impact Force (kN)
- Take-Off Speed (m/s)
- Peak Speed (m/s)
- Average Speed Concentric Phase (m/s)
- Maximum Concentric Power (kW)
- Average Concentric Power (kW)
2.2. Data analysis
2.2.1. Sample size determination
2.2.2. Statistical analysis
3. Results
3.1. Participant demographics and characteristics
3.2. Correlations between variables
| CMJAT | CVA | Lateral translationhead | AHT | Lateral angulation head | ||||
|---|---|---|---|---|---|---|---|---|
| r | p | r | p | r | p | r | p | |
| CMJAT - flight height (cm) | 0.55* | < 0.001 | -0.39* | < 0.001 | -0.70* | < 0.001 | -0.39* | < 0.001 |
| CMJAT – take-off force (kN) | 0.43* | < 0.001 | -0.40* | < 0.001 | -0.65* | < 0.001 | -0.38* | < 0.001 |
| CMJAT - impact force (kN) | 0.39* | < 0.001 | -0.48* | < 0.001 | -0.55* | < 0.001 | -0.40* | < 0.001 |
| CMJAT – take-off Speed (m/s) | 0.44* | < 0.001 | -0.43* | < 0.001 | -0.50* | < 0.001 | -0.40* | < 0.001 |
| CMJAT - peak speed (m/s) | 0.48* | < 0.001 | -0.42* | < 0.001 | -0.55* | < 0.001 | -0.39* | < 0.001 |
| CMJAT - average Speed concentric phase (m/s) | 0.39* | < 0.001 | -0.42* | < 0.001 | -0.60* | < 0.001 | -0.40* | < 0.001 |
| CMJAT - maximum concentric power (kW) | 0.27* | 0.03 | -0.31* | 0.003 | -0.48* | < 0.001 | -0.31* | 0.003 |
| CMJAT - average concentric power (kW) | 0.52* | < 0.001 | -0.54* | < 0.001 | -0.60* | < 0.001 | -0.31* | 0.003 |
4. Discussion
4.1. Posture and Athletic Skills
4.2. Posture and Gait Asymmetries
4.3. Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Menz, H.B.; Lord, S.R.; Fitzpatrick, R.C. Age-related differences in walking stability. Age Ageing 2003, 32, 137–142. [Google Scholar] [CrossRef]
- Promsri, A.; Cholamjiak, P.; Federolf, P. Walking Stability and Risk of Falls. Bioengineering 2023, 10, 471. [Google Scholar] [CrossRef]
- Biewener, A.A.; Farley, C.T.; Roberts, T.J.; Temaner, M.; Ludlow, L.W.; Weyand, P.G.; Beck, O.N.; Taboga, P.; Grabowski, A.M.; Giovanelli, N.; et al. Muscle mechanical advantage of human walking and running: implications for energy cost. J. Appl. Physiol. 2004, 97, 2266–2274. [Google Scholar] [CrossRef]
- Kwak, S.T.; Chang, Y.-H. Fascicle dynamics of the tibialis anterior muscle reflect whole-body walking economy. Sci. Rep. 2023, 13, 4660. [Google Scholar] [CrossRef] [PubMed]
- Graci, V.; Salsich, G.B. Trunk and lower extremity segment kinematics and their relationship to pain following movement instruction during a single-leg squat in females with dynamic knee valgus and patellofemoral pain. J. Sci. Med. Sport 2014, 18, 343–347. [Google Scholar] [CrossRef]
- Nunes, G.S.; de Moraes, W.S.L.A.; Sampaio, V.d.S.; Seda, N.R.; Mouta, G.d.S.; Dangui, A.J.M.; Petersen, R.d.S.; Nakagawa, T.H. Are Changes in Dynamic Knee Movement Control Related to Changes in Pain or Function in People With Knee Disorders? A Systematic Review and Meta-analysis. J. Orthop. Sports Phys. Ther. 2023, 53, 388–401. [Google Scholar] [CrossRef] [PubMed]
- Myer, G.D.; Ford, K.R.; Hewett, T.E. Tuck Jump Assessment for Reducing Anterior Cruciate Ligament Injury Risk. Athl. Ther. Today 2008, 13, 39–44. [Google Scholar] [CrossRef] [PubMed]
- Kang, J.-H.; Park, R.-Y.; Lee, S.-J.; Kim, J.-Y.; Yoon, S.-R.; Jung, K.-I. The Effect of The Forward Head Posture on Postural Balance in Long Time Computer Based Worker. Ann. Rehabilitation Med. 2012, 36, 98–104. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.-H. Effects of forward head posture on static and dynamic balance control. J. Phys. Ther. Sci. 2016, 28, 274–277. [Google Scholar] [CrossRef] [PubMed]
- Ruivo, R.M.; Pezarat-Correia, P.; Carita, A.I. Effects of a Resistance and Stretching Training Program on Forward Head and Protracted Shoulder Posture in Adolescents. J. Manip. Physiol. Ther. 2016, 40, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Muyor, J.M.; López-Miñarro, P.A.; Casimiro, A.J. Effect of stretching program in an industrial workplace on hamstring flexibility and sagittal spinal posture of adult women workers: A randomized controlled trial. J. Back Musculoskelet. Rehabilitation 2012, 25, 161–169. [Google Scholar] [CrossRef]
- Lin, G.; Zhao, X.; Wang, W.; Wilkinson, T. The relationship between forward head posture, postural control and gait: A systematic review. Gait Posture 2022, 98, 316–329. [Google Scholar] [CrossRef]
- Ahmadipoor, A.; Khademi-Kalantari, K.; Rezasoltani, A.; Naimi, S.-S.; Akbarzadeh-Baghban, A. Effect of Forward Head Posture on Dynamic Balance Based on the Biodex Balance System. J. Biomed. Phys. Eng. 2022, 12, 543–548. [Google Scholar] [CrossRef] [PubMed]
- Caneiro, J.P.; O’Sullivan, P.; Burnett, A.; Barach, A.; O’Neil, D.; Tveit, O.; Olafsdottir, K. The influence of different sitting postures on head / neck posture and muscle activity. Man Ther 2010, 15, 54–60. [Google Scholar] [CrossRef]
- Shaghayegh fard, B.; Ahmadi, A.; Maroufi, N.; Sarrafzadeh, J. Evaluation of forward head posture in sitting and standing positions. Eur Spine J 2016, 25, 3577–3582. [Google Scholar] [CrossRef]
- Ruivo, R.M.; Pezarat-Correia, P.; Carita, A.I. Effects of a Resistance and Stretching Training Program on Forward Head and Protracted Shoulder Posture in Adolescents. J. Manip. Physiol. Ther. 2016, 40, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Jain, D. EFFECTS OF FORWARD HEAD POSTURE ON POSTURAL BALANCE IN YOUNG ADULTS. Int. J. Adv. Res. 2019, 7, 136–146. [Google Scholar] [CrossRef] [PubMed]
- Kang, J.-H.; Park, R.-Y.; Lee, S.-J.; Kim, J.-Y.; Yoon, S.-R.; Jung, K.-I. The Effect of The Forward Head Posture on Postural Balance in Long Time Computer Based Worker. Ann. Rehabilitation Med. 2012, 36, 98–104. [Google Scholar] [CrossRef]
- Lau, K.T.; Cheung, K.Y.; Chan, K.B.; Chan, M.H.; Lo, K.Y.; Chiu, T.T.W. Relationships between sagittal postures of thoracic and cervical spine, presence of neck pain, neck pain severity and disability. Man. Ther. 2010, 15, 457–462. [Google Scholar] [CrossRef]
- Kapandji, I.A. The Physiology of the Joints. Volume 3. the trunk and the vertebral column. Postgrad Med J 1975, 51, 682. [Google Scholar]
- Harman, K.; Hubley-Kozey, C.L.; Butler, H. Effectiveness of an Exercise Program to Improve Forward Head Posture in Normal Adults: A Randomized, Controlled 10-Week Trial. J. Man. Manip. Ther. 2005, 13, 163–176. [Google Scholar] [CrossRef]
- Alowa, Z.; Elsayed, W. The impact of forward head posture on the electromyographic activity of the spinal muscles. J. Taibah Univ. Med Sci. 2020, 16, 224–230. [Google Scholar] [CrossRef] [PubMed]
- Panjabi, M.M.; M., M. The Stabilizing System of the Spine. Part I. Function, Dysfunction, Adaptation, and Enhancement. J. Spinal Disord. 1992, 5, 383–389. [CrossRef]
- Cholewicki, J.; IV, J.J.V. Relative contribution of trunk muscles to the stability of the lumbar spine during isometric exertions. Clin. Biomech. 2002, 17, 99–105. [Google Scholar] [CrossRef] [PubMed]
- Panjabi, M.; Abumi, K.; Duranceau, J.; Oxland, T.M. Spinal Stability and Intersegmental Muscle Forces. Spine 1989, 14, 194–200. [Google Scholar] [CrossRef]
- Boynton, A.M.; Carrier, D.R. The Human Neck is Part of the Musculoskeletal Core: Cervical Muscles Help Stabilize the Pelvis During Running and Jumping. Integr. Org. Biol. 2022, 4, obac021. [Google Scholar] [CrossRef] [PubMed]
- Panjabi, M.M.; M., M. The Stabilizing System of the Spine. Part II. Neutral Zone and Instability Hypothesis. J. Spinal Disord. 1992, 5, 390–397. [CrossRef] [PubMed]
- Adams, M.; Dolan, P.; Hutton, W.C. The stages of disc degeneration as revealed by discograms. . 1986, 68, 36–41. [Google Scholar] [CrossRef]
- Harrison, D.E.; Oakley, P.A. An Introduction to Chiropractic BioPhysics® (CBP®) Technique: A Full Spine Rehabilitation Approach to Reducing Spine Deformities. 2022. [Google Scholar] [CrossRef]
- Oakley, P.A.; Ehsani, N.N.; Moustafa, I.M.; Harrison, D.E. Restoring cervical lordosis by cervical extension traction methods in the treatment of cervical spine disorders: a systematic review of controlled trials. J. Phys. Ther. Sci. 2021, 33, 784–794. [Google Scholar] [CrossRef]
- Tao, W.; Liu, T.; Zheng, R.; Feng, H. Gait Analysis Using Wearable Sensors. Sensors 2012, 12, 2255–2283. [Google Scholar] [CrossRef]
- Wang, W.; Adamczyk, P.G. Analyzing Gait in the Real World Using Wearable Movement Sensors and Frequently Repeated Movement Paths. Sensors 2019, 19, 1925. [Google Scholar] [CrossRef] [PubMed]
- Muro-De-La-Herran, A.; Garcia-Zapirain, B.; Mendez-Zorrilla, A. Gait Analysis Methods: An Overview of Wearable and Non-Wearable Systems, Highlighting Clinical Applications. Sensors 2014, 14, 3362–3394. [Google Scholar] [CrossRef] [PubMed]
- Bisi, M.C.; Stagni, R. Development of gait motor control: What happens after a sudden increase in height during adolescence? Biomed Eng Online 2016, 15. [Google Scholar] [CrossRef] [PubMed]
- Szucs, K.A.; Brown, E.V.D. Rater reliability and construct validity of a mobile application for posture analysis. J. Phys. Ther. Sci. 2018, 30, 31–36. [Google Scholar] [CrossRef]
- Boland, D.M.; Neufeld, E.V.; Ruddell, J.; Dolezal, B.A.; Cooper, C.B. Inter- and intra-rater agreement of static posture analysis using a mobile application. J. Phys. Ther. Sci. 2016, 28, 3398–3402. [Google Scholar] [CrossRef]
- Volkan-Yazici, M.; Çobanoğlu, G.; Yazici, G. Test-retest reliability and minimal detectable change for measures of wearable gait analysis system (G-walk) in children with cerebral palsy. Turk J Med Sci 2022, 52, 658–666. [Google Scholar] [CrossRef] [PubMed]
- De Ridder, R.; Lebleu, J.; Willems, T.; De Blaiser, C.; Detrembleur, C.; Roosen, P. Concurrent Validity of a Commercial Wireless Trunk Triaxial Accelerometer System for Gait Analysis. J. Sport Rehabilitation 2019, 28. [Google Scholar] [CrossRef] [PubMed]
- Randell, R.K.; Clifford, T.; Drust, B.; Moss, S.L.; Unnithan, V.B.; de Ste Croix, M.B.A.; Datson, N.; Martin, D.; Mayho, H.; Carter, J.M.; et al. Physiological Characteristics of Female Soccer Players and Health and Performance Considerations: A Narrative Review. Sports Med. 2021, 51, 1377–1399. [Google Scholar] [CrossRef] [PubMed]
- Park, G.; Woo, Y. Comparison between a center of mass and a foot pressure sensor system for measuring gait parameters in healthy adults. J. Phys. Ther. Sci. 2015, 27, 3199–3202. [Google Scholar] [CrossRef]
- Yazici, G.; Yazici, M.V.; Çobanoğlu, G.; Küpeli, B.; Özkul, Ç.; Oskay, D.; Güzel, N.A. The reliability of a wearable movement analysis system (G-walk) on gait and jump assessment in healthy adults. Journal of Exercise Therapy and Rehabilitation 2020, 7, 159–167. [Google Scholar]
- Pau, M.; Leban, B.; Collu, G.; Migliaccio, G.M. Effect of light and vigorous physical activity on balance and gait of older adults. Arch. Gerontol. Geriatr. 2014, 59, 568–573. [Google Scholar] [CrossRef] [PubMed]
- Mahmoud, N.F.; Hassan, K.A.; Abdelmajeed, S.F.; Moustafa, I.M.; Silva, A.G. The Relationship Between Forward Head Posture and Neck Pain: a Systematic Review and Meta-Analysis. Curr. Rev. Musculoskelet. Med. 2019, 12, 562–577. [Google Scholar] [CrossRef] [PubMed]
- Al Suwaidi, A.S.; Moustafa, I.M.; Kim, M.; Oakley, P.A.; Harrison, D.E. A Comparison of Two Forward Head Posture Corrective Approaches in Elderly with Chronic Non-Specific Neck Pain: A Randomized Controlled Study. J. Clin. Med. 2023, 12, 542. [Google Scholar] [CrossRef] [PubMed]
- Khan, A.; Khan, Z.; Bhati, P.; Hussain, M.E. Influence of Forward Head Posture on Cervicocephalic Kinesthesia and Electromyographic Activity of Neck Musculature in Asymptomatic Individuals. J. Chiropr. Med. 2020, 19, 230–240. [Google Scholar] [CrossRef] [PubMed]
- Martinez-Merinero, P.; Nuñez-Nagy, S.; Achalandabaso-Ochoa, A.; Fernandez-Matias, R.; Pecos-Martin, D.; Gallego-Izquierdo, T. Relationship between Forward Head Posture and Tissue Mechanosensitivity: A Cross-Sectional Study. J. Clin. Med. 2020, 9, 634. [Google Scholar] [CrossRef]
- Pacheco, J.; Raimundo, J.; Santos, F.; Ferreira, M.; Lopes, T.; Ramos, L.; Silva, A.G. Forward head posture is associated with pressure pain threshold and neck pain duration in university students with subclinical neck pain. Somatosens. Mot. Res. 2018, 35, 103–108. [Google Scholar] [CrossRef]
- Naz, A.; Bashir, S.; Noor, R. Prevalence of forward head posture among university students. Rawal Medical Journal 43.
- Singh, S.; Kaushal, K.; Jasrotia, S. Prevalence of forward head posture and its impact on the activity of daily living among students of Adesh University – A cross-sectional study. Adesh Univ. J. Med Sci. Res. 2020, 2, 99–102. [Google Scholar] [CrossRef]
- Hodges, P.W.; Smeets, R.J. Interaction between pain, movement, and physical activity: Short-term benefits, long-term consequences, and targets for treatment. Clin J Pain 2015, 31, 97–107. [Google Scholar] [CrossRef] [PubMed]
- Danna-Dos-Santos, A.; Degani, A.M.; Latash, M.L. Anticipatory control of head posture. Clin. Neurophysiol. 2007, 118, 1802–1814. [Google Scholar] [CrossRef] [PubMed]
- Massion, J. Movement, posture and equilibrium: Interaction and coordination. Prog. Neurobiol. 1992, 38, 35–56. [Google Scholar] [CrossRef] [PubMed]
- Frank, J.S.; Earl, M. Coordination of Posture and Movement. Phys. Ther. 1990, 70, 855–863. [Google Scholar] [CrossRef] [PubMed]
- Moustafa, I.; Kim, M.; Harrison, D.E. Comparison of sensorimotor integration and skill-re-lated physical fitness components between college athletes with and without forward head posture. J. Sport Rehabil. 2022, 32, 53–62. [Google Scholar] [CrossRef]
- Abbruzzese, G.; Berardelli, A. Sensorimotor integration in movement disorders. Mov. Disord. 2002, 18, 231–240. [Google Scholar] [CrossRef] [PubMed]
- Haavik, H.; Murphy, B. The role of spinal manipulation in addressing disordered sensorimotor integration and altered motor control. J. Electromyogr. Kinesiol. 2012, 22, 768–776. [Google Scholar] [CrossRef]
- Haavik-Taylor, H.; Murphy, B. Cervical spine manipulation alters sensorimotor integration: A somatosensory evoked potential study. Clin. Neurophysiol. 2007, 118, 391–402. [Google Scholar] [CrossRef] [PubMed]
- Pickar, J.G. Neurophysiological effects of spinal manipulation. Spine J. 2002, 2, 357–371. [Google Scholar] [CrossRef] [PubMed]
- Taylor, H.H.; Murphy, B. Altered Central Integration of Dual Somatosensory Input After Cervical Spine Manipulation. J. Manip. Physiol. Ther. 2010, 33, 178–188. [Google Scholar] [CrossRef] [PubMed]
- Hishinuma, M.; Yamaguchi, T. Axonal projection of descending pathways responsible for eliciting forelimb stepping into the cat cervical spinal cord. Exp. Brain Res. 1990, 82, 597–605. [Google Scholar] [CrossRef] [PubMed]
- Desmurget, M.; Sirigu, A. A parietal-premotor network for movement intention and motor awareness. Trends Cogn. Sci. 2009, 13, 411–419. [Google Scholar] [CrossRef]
- Azevedo, R.d.A.; Cruz, R.; Couto, P.; Silva-Cavalcante, M.D.; Boari, D.; Lima-Silva, A.E.; Millet, G.Y.; Bertuzzi, R.; Drouin, P.J.; Kohoko, Z.I.N.; et al. Spinal and Supraspinal Factors in Human Muscle Fatigue. Physiol. Rev. 2001, 81, 1725–1789. [Google Scholar] [CrossRef]
- Krakauer, J.W.; Ghazanfar, A.A.; Gomez-Marin, A.; MacIver, M.A.; Poeppel, D. Neuroscience Needs Behavior: Correcting a Reductionist Bias. Neuron 2017, 93, 480–490. [Google Scholar] [CrossRef] [PubMed]
- E Harrison, D.; Harrison, D.D.; Betz, J.J.; Janik, T.J.; Holland, B.; Colloca, C.J.; Haas, J.W. Increasing the cervical lordosis with chiropractic biophysics seated combined extension-compression and transverse load cervical traction with cervical manipulation: nonrandomized clinical control trial. J. Manip. Physiol. Ther. 2003, 26, 139–151. [Google Scholar] [CrossRef]
- Harrison, D.E.; Cailliet, R.; Harrison, D.D.; Janik, T.J.; Holland, B. A new 3-point bending traction method for restoring cervical lordosis and cervical manipulation: A nonrandomized clinical controlled trial. Arch. Phys. Med. Rehabilitation 2002, 83, 447–453. [Google Scholar] [CrossRef]
- Harrison, D.E.; Cailliet, R.; Betz, J.; Haas, J.W.; Harrison, D.D.; Janik, T.J.; Holland, B. Conservative methods for reducing lateral translation postures of the head: a nonrandomized clinical control trial. J. Rehabilitation Res. Dev. 2004, 41, 631. [Google Scholar] [CrossRef]
- Oakley, P.A.; Kallan, S.Z.; Harrison, D.E. Structural rehabilitation of the cervical lordosis and forward head posture: a selective review of Chiropractic BioPhysics® case reports. J. Phys. Ther. Sci. 2022, 34, 759–771. [Google Scholar] [CrossRef] [PubMed]
- Kawkabani, G.; Saliby, R.M.; Mekhael, M.; Rachkidi, R.; Massaad, A.; Ghanem, I.; Kharrat, K.; Kreichati, G.; Saad, E.; Lafage, V.; et al. Gait kinematic alterations in subjects with adult spinal deformity and their radiological determinants. Gait Posture 2021, 88, 203–209. [Google Scholar] [CrossRef]
- Mekhael, E.; El Rachkidi, R.; Saliby, R.M.; Nassim, N.; Semaan, K.; Massaad, A.; Karam, M.; Saade, M.; Ayoub, E.; Rteil, A.; et al. Functional assessment using 3D movement analysis can better predict health-related quality of life outcomes in patients with adult spinal deformity: a machine learning approach. Front. Surg. 2023, 10, 1166734. [Google Scholar] [CrossRef] [PubMed]
- Sato, K.; Tominaga, R.; Endo, T.; Miura, T.; Iwabuchi, M.; Ito, T.; Shirado, O. The association of dynamic spinal alignment on gait endurance of patients with adult spinal deformity: a cross-sectional study. Spine Deform. 2022, 11, 1–7. [Google Scholar] [CrossRef]
- Arima, H.; Yamato, Y.; Hasegawa, T.; Togawa, D.; Kobayashi, S.; Yasuda, T.; Banno, T.; Oe, S.; Matsuyama, Y. Discrepancy Between Standing Posture and Sagittal Balance During Walking in Adult Spinal Deformity Patients. Spine 2017, 42, E25–E30. [Google Scholar] [CrossRef] [PubMed]
- Semaan, K.; Rachkidi, R.; Saad, E.; Massaad, A.; Kawkabani, G.; Saliby, R.M.; Mekhael, M.; Karam, K.A.; Fakhoury, M.; Jaber, E.; et al. Alterations of gait kinematics depend on the deformity type in the setting of adult spinal deformity. Eur. Spine J. 2022, 31, 3069–3080. [Google Scholar] [CrossRef] [PubMed]
- Khamis, S.; Carmeli, E. Relationship and significance of gait deviations associated with limb length discrepancy: A systematic review. Gait Posture 2017, 57, 115–123. [Google Scholar] [CrossRef]
- Shi, Y.; Pang, H.; Xu, H.; Li, X.; Cao, Y.; Merryweather, A.; Zheng, P.; Xiang, J. Effects of orthotic insole on gait patterns in children with mild leg length discrepancy. Gait Posture 2022, 93, 191–197. [Google Scholar] [CrossRef] [PubMed]
- Khamis, S.; Carmeli, E. The effect of simulated leg length discrepancy on lower limb biomechanics during gait. Gait Posture 2018, 61, 73–80. [Google Scholar] [CrossRef]
| Variable | N=100 |
|---|---|
| Age (years) | 21.10 ± 1.70 |
| Weight (kg) | 67.77 ± 17.28 |
| Height (cm) | 166.68 ± 8.72 |
| BMI (kg/m2) | 24.27 ± 5.33 |
| Gender (%) | |
| Male | 27 |
| Female | 73 |
| Race / ethnicity (n) | |
| Arab-Non GCC | 51 |
| Arab-GCC | 31 |
| Non-Arab | 18 |
| Head Posture Parameters | N = 100 Median (IQR) |
|---|---|
| CVA (°) | 51.60 (46.60, 55.30) |
| Lateral translation head (cm) | 3.79 (2.68, 5.03) |
| AHT (cm) | 0.69 (0.18, 1.21) |
| Lateral angulation head (°) | 10.32 (6.67 ,14.3) |
| Gait Spatiotemporal Parameters | N = 100 Median (IQR) |
|---|---|
| Cadence | 109.70 (105.30, 116.30) |
| Speed (m/s) | 1.15 (0.98 ,1.24) |
| Symmetry index | 92.20 (80.90, 95.60) |
| % Left stride length (% height) | 76 (66.70, 83.20) |
| % Right stride length (% height) | 75.40 (67.70, 82.60) |
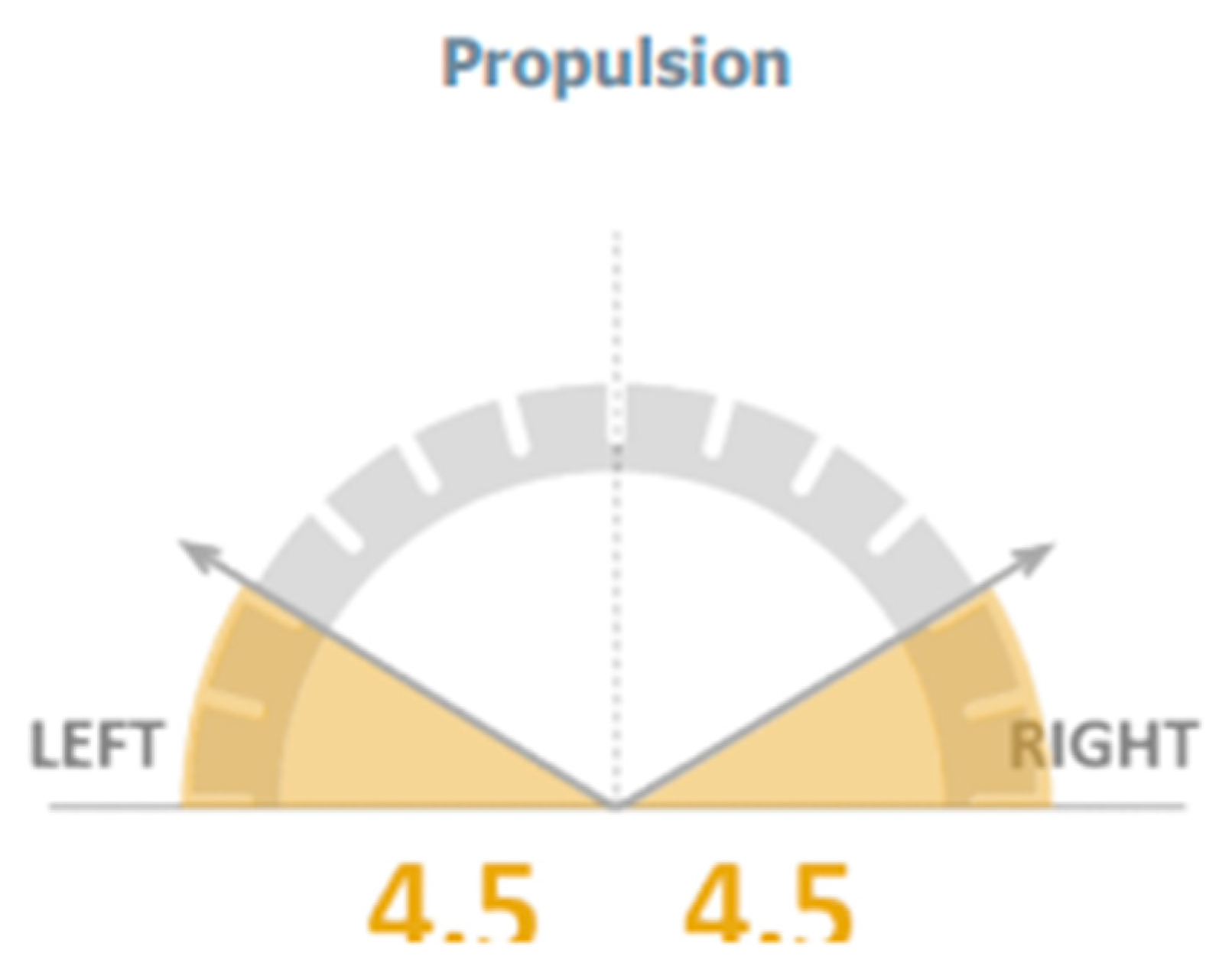
| Left propulsion index | 5.50 (4.20, 7.50) |
| Right Propulsion Index | 4.80 (3.90, 7.60) |
| Tilt - symmetry index | 47.10 (24.30, 77.90) |
| Tilt - left - range | 4.30 (3.30, 5.40) |
| Tilt - right - Range | 8.40 (3.70, 13.20) |
| Obliquity – symmetry index | 95.80 (84.80, 98.10) |
| Obliquity - left - range | 7.50 (5.70, 10.40) |
| Obliquity - right - range | 80.00 (5.80, 10.50) |
| Rotation - symmetry index | 96.70 (85.70, 98.10) |
| Rotation - left - range | 10.30 (6.90, 13.30) |
| Rotation - right - range | 10.50 (6.90, 13.70) |
| CMJ Parameters | N = 100 Median (IQR) |
|---|---|
| CMJ - flight height (cm) | 17.20 (14.20, 24.30) |
| CMJ – take-off force (kN) | 1.11 (0.92, 1.40) |
| CMJ - impact force (kN) | 1.35 (1.05, 1.69) |
| Take-off speed (m/s) | 2.12 (1.85, 2.48) |
| CMJ - peak speed (m/s) | 2.24 (1.99, 2.58) |
| CMJ - average speed concentric phase (m/s) | 1.23 (1.08, 1.41) |
| CMJ - maximum concentric power (kW) | 2.19 (1.67, 2.94) |
| CMJ - average concentric power (kW) | 1.02 (0.85, 1.41) |
| CMJAT Parameters | N = 100 Median (IQR) |
|---|---|
| CMJAT - flight height (cm) | 19.60 (15.90, 27.70) |
| CMJAT – take-off force (kN) | 1.15 (0.95, 1.55) |
| CMJAT - impact force (kN) | 1.45 (1.11, 1.95) |
| CMJAT – take-off speed (m/s) | 2.15 (1.94, 2.45) |
| CMJAT - peak speed (m/s) | 2.27 (2.09, 2.53) |
| CMJAT - average speed concentric phase (m/s) | 1.23 (1.12, 1.39) |
| CMJAT - maximum concentric power (kW) | 2.11 (1.76, 3.34) |
| CMJAT - average concentric power (kW) | 1.08 (0.89, 1.53) |
| Gait Parameters | CVA | Lateral translationhead | AHT | Lateral angulation head | ||||
|---|---|---|---|---|---|---|---|---|
| r | p | r | P | r | p | r | p | |
| Cadence | 0.51* | < 0.001 | -0.74* | < 0.001 | -0.51* | < 0.001 | -0.27* | 0.006 |
| Speed (m/s) | 0.52* | < 0.001 | -0.46* | < 0.001 | -0.44* | < 0.001 | -0.37* | < 0.001 |
| Symmetry index | 0.54* | < 0.001 | -0.70* | < 0.001 | 0.02 | 0.854 | -0.31* | 0.003 |
| %Left stride length (%height) | 0.43* | < 0.001 | -0.42* | < 0.001 | -0.48* | < 0.001 | -0.31* | 0.003 |
| %Right stride length (%height) | 0.51* | < 0.001 | -0.51* | < 0.001 | -0.46* | < 0.001 | -0.32* | 0.01 |
| Left propulsion index | 0.54* | < 0.001 | -0.36* | 0.001 | -0.47* | < 0.001 | -0.36* | < 0.001 |
| Right propulsion index | 0.55* | < 0.001 | -0.29* | 0.015 | -0.39* | 0.001 | -0.39* | < 0.001 |
| Tilt - symmetry index | 0.57* | < 0.001 | -0.51* | < 0.001 | -0.62* | < 0.001 | -0.45* | < 0.001 |
| Tilt - left – range | 0.58* | < 0.001 | -0.21* | 0.004 | -0.81* | < 0.001 | -0.37* | < 0.001 |
| Tilt - right - range | 0.54* | < 0.001 | -0.23* | 0.004 | -0.47* | < 0.001 | -0.26* | 0.011 |
| Obliquity – symmetry index | 0.56* | < 0.001 | -0.06* | < 0.001 | -0.75* | < 0.001 | -0.40* | < 0.001 |
| Obliquity - Left - Range | 0.45* | < 0.001 | -0.49* | < 0.001 | -0.65* | < 0.001 | -0.26* | 0.011 |
| Obliquity - right – Range | 0.54* | < 0.001 | -0.25* | 0.005 | -0.64* | < 0.001 | -0.25* | 0.011 |
| Rotation - symmetry Index | 0.52* | < 0.001 | -0.69* | < 0.001 | -0.27* | 0.010 | -0.43* | < 0.001 |
| Rotation - left - range | 0.46* | < 0.001 | -0.33* | 0.001 | -0.42* | < 0.001 | -0.10 | 0.3 |
| Rotation - right - range | 0.46* | < 0.001 | -0.24* | 0.005 | -0.41* | < 0.001 | -0.26* | 0.011 |
| Physical Performance Skills | CVA | Lateral translationhead | AHT | Lateral angulation head | ||||
|---|---|---|---|---|---|---|---|---|
| r | p | r | p | r | p | r | p | |
| CMJ - flight height (cm) | 0.41* | < 0.001 | -0.39* | < 0.001 | -0.44* | < 0.001 | -0.37* | < 0.001 |
| CMJ – take-off force (kN) | 0.39* | < 0.001 | -0.40* | < 0.001 | -0.65* | < 0.001 | -0.38* | < 0.001 |
| CMJ - impact force (kN) | 0.24 | 0.052 | -0.48* | < 0.001 | -0.55* | < 0.001 | -0.39* | < 0.001 |
| Take-off speed (m/s) | 0.39* | < 0.001 | -0.43* | < 0.001 | -0.49* | < 0.001 | -0.38* | < 0.001 |
| CMJ - peak speed (m/s) | 0.38* | < 0.001 | -0.42* | < 0.001 | -0.49* | < 0.001 | -0.40* | < 0.001 |
| CMJ - average speed concentric phase (m/s) | 0.41* | < 0.001 | -0.42* | < 0.001 | -0.57* | < 0.001 | -0.40* | < 0.001 |
| CMJ - maximum Concentric Power (kW) | 0.27* | 0.03 | -0.31* | 0.003 | -0.41* | < 0.001 | -0.40* | < 0.001 |
| CMJ - average concentric power (kW) | 0.52* | < 0.001 | -0.54* | < 0.001 | -0.48* | < 0.001 | -0.39* | < 0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





