Submitted:
29 January 2024
Posted:
30 January 2024
Read the latest preprint version here
Abstract
Keywords:
Introduction
Methodology
Discussion
- Gradual separation of hundreds of millions of people from their natural origins, through a mass relocation into hyper-industrialized megalopolises, mostly by international means.
- Increasing technology abuse and dependence in young children. Risking a gradual, but certain replacement of manual work with automated, robotics-mediated work, leading gradually to a general loss of human workforce.
- Direct and indirect manipulation of the human genome, such as gene therapy using foreign genetic information, as well as an increasing manipulation of the environment respectively.
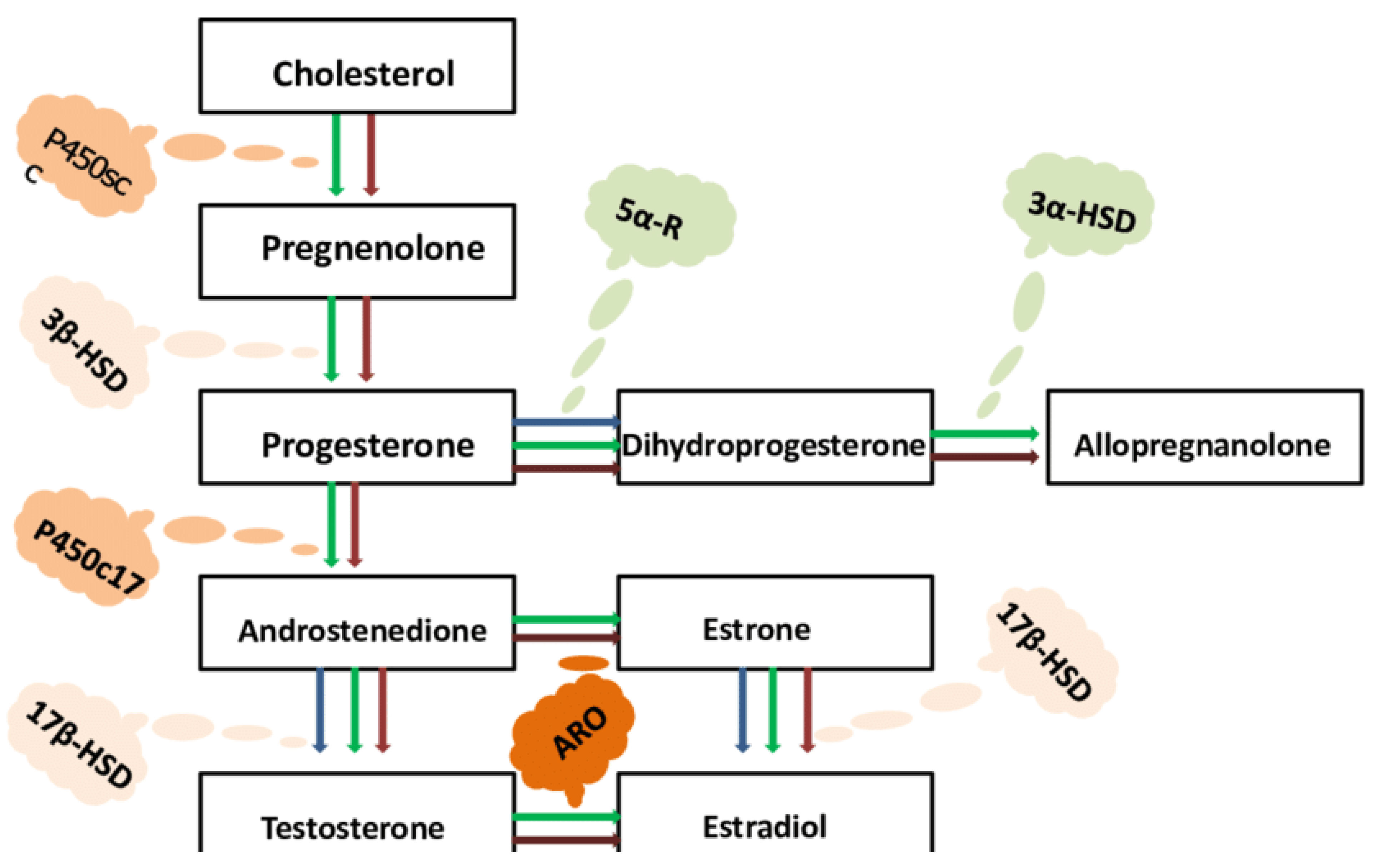
- Widespread consumption of junk food, fast food and unhealthy beverages by young children. Fast food often contains various hormones, which may play a considerable role in creating or amplifying delays in neurogenesis and neurological development in children, potentially affecting them for many years after.
- A significant decrease of social interest in civilizational values and unspoken rules that primarily contributed to the establishment and maintenance of society.
- Incomplete availability of resources and logistical pathways to offer immunomodulatory treatment for pregnant mothers experiencing moderate and severe infectious diseases. Insufficient clinical focus upon the importance of natural immunity in prophylaxis and early treatment of infectious diseases of concern.
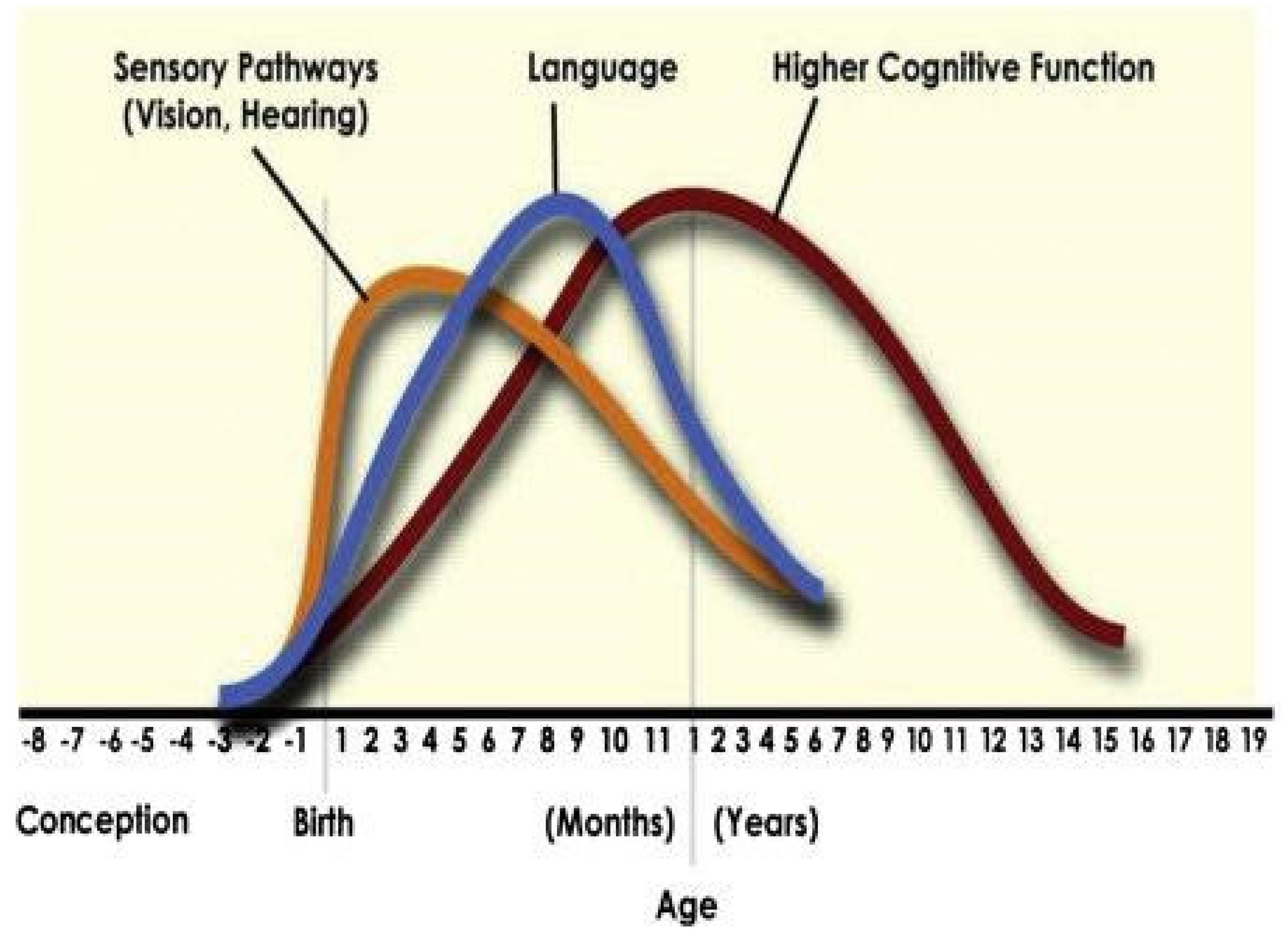
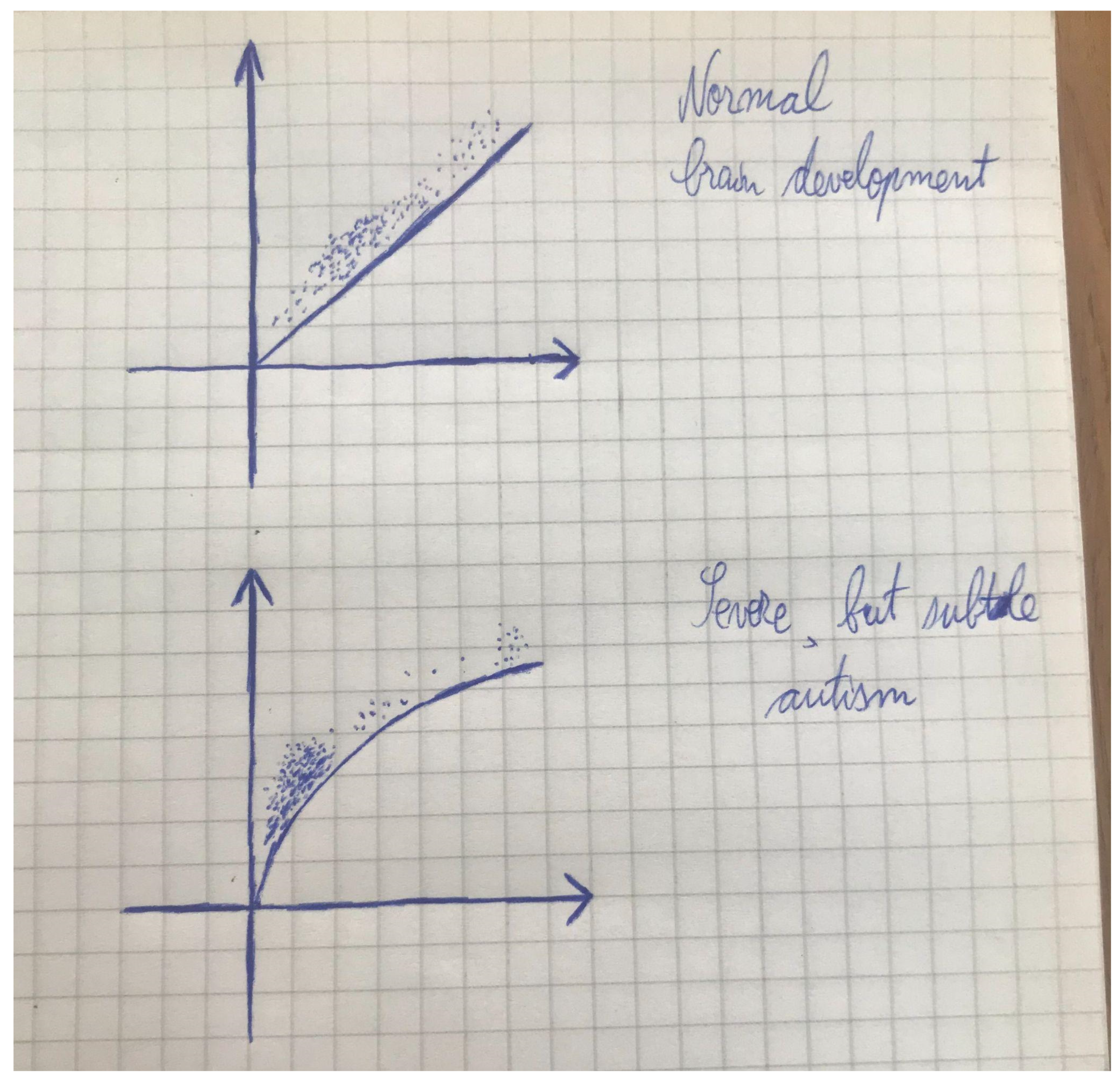
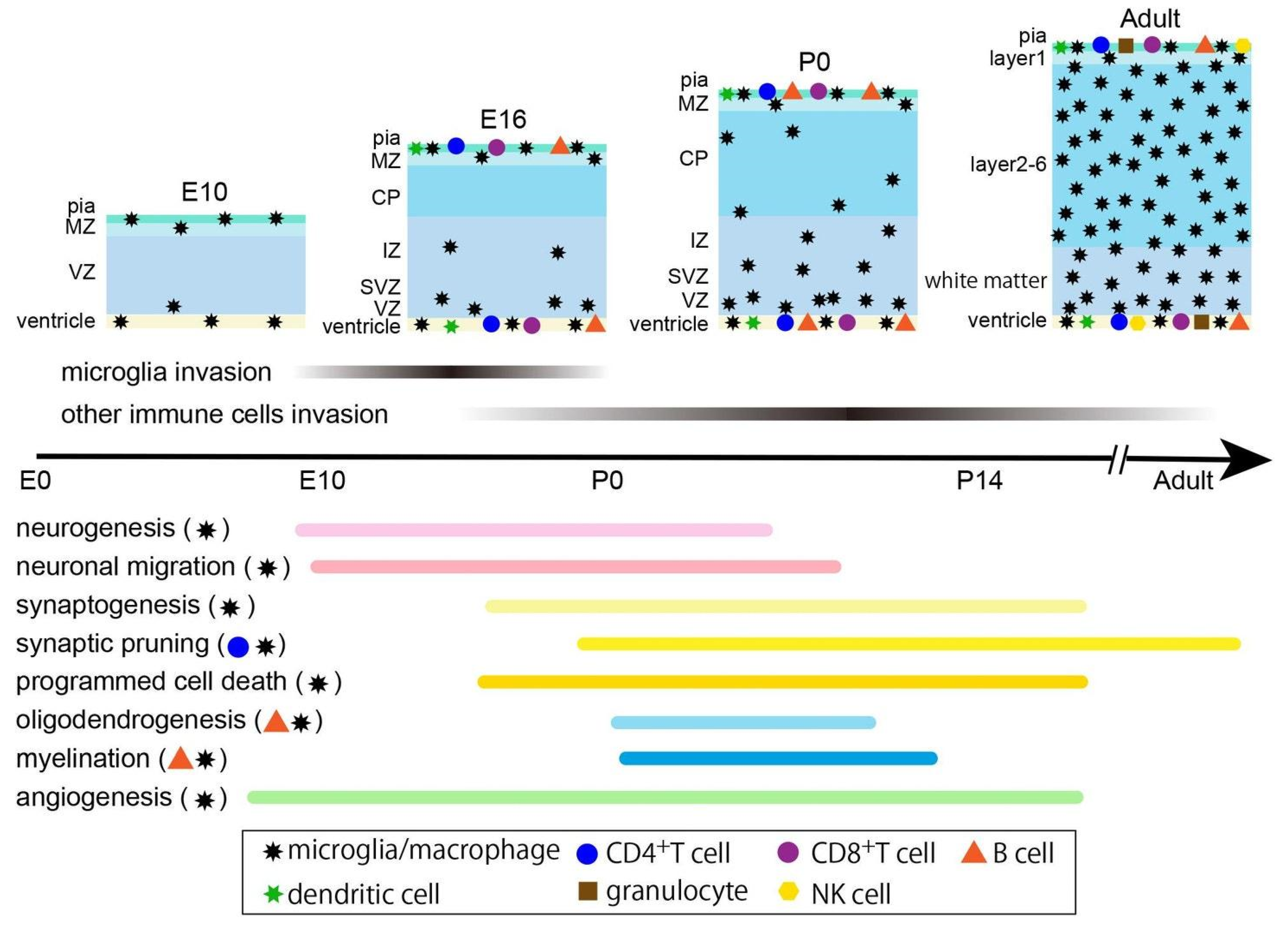
- Potentially major factor: The administration of 28-32 vaccine doses or more, including one or more doses of the experimental COVID-19 vaccine using the genetic information of a viral protein with potential characteristics of a superantigen, in babies aged 0-2, who are in critical stages or neuro-immunological development. Moreover, the increase of infant vaccine doses, from 12-15 in the 1980s, to about 30 or locally 35 by 2015, and to 40-45 doses and locally more from 2022, has been accompanied by an insufficient focus upon the potential roles of early innate immune activation in the vaccinological combat against infectious diseases of individual and public health concern, and applications of early innate immune activation into vaccinology would promote neurogenesis and neuroprotection more substantially. The number of administered childhood vaccine doses has recently risen from 45 in 2015 to 76 in 2022, in the United States of America. The administration of vaccines that contain multiple antigens each may strengthen the pressurizing effects upon the brain to develop, thereby raising the possibility and extent of the ulterior onset of neurodevelopmental delays. The addition of heavy metals, including mercury, as a vaccine adjuvant in rather many cases can only further amplify such effects of neuro-immunology-related developmental delays and damages.
- Hyper-automation and lack of healthy work and study environments, leading to privation from essential human contact and direct instruction and mentorship during key stages of neuronal growth.
- Increased repetitive patterns in the individual and collective thinking and behavior caused by the gradual, but certain separation of humankind from her natural roots.
- Polarization of resource-based, economic, financial, academic and professional power, turning the world, not even into a bipolar arena, where the disadvantaged matter in society, but outright into a unipolar arena, where the disadvantaged are treated like they are nonexistent, reducing the extent of middle class to its extinction and separating society into the poor class, consisting of over 99% of the world’s population, and the rich class, consisting of less than 1% of the world’s population. Placing much of the blame of the corrupt leadership on the poorer segments of society, instead of using the gained multi-billion financial resources to support the poor in conducting themselves adequately to support the reconstruction of Nature and simultaneously the reunification of humankind with Nature, instead of punishing her by separating her into hyper-industrialized environments by means of psychological and financial force.
- Manipulation of healthy educational patterns, by allowing children and teenagers to be exposed to environmental factors that would induce delays in the development of healthy cognitive function and behavior.
- Manipulation of imagery via social media and television. Prioritization of unhealthy thinking and behaviors.
- Manipulation of frequencies (i.e. the change of the music frequency from 432 Hz to 440 Hz in 1938), making people more irritable, angrier and more aggressive, thereby increasing levels of testosterone, which will increase the incidence of excess testosterone, which in turn will ultimately increase the incidence of serious neurodevelopmental delays.
- Manipulation of music, including the usage of negative subliminal messages, indirectly or directly increasing the epigenetic stimulation of testosterone synthesis and ultimately leading to an excess of aggression, anger and hopelessness.
- An exponential increase of the incidences of serious early childhood trauma, causing neurological damage and often major neurodevelopmental delays.
- The widespread usage of genetically-modified organisms (GMOs), which is promoted by the currents of Malthusianism and Cornucopianism. Notably, Dr. Pierre Verhulst, who obtained his PhD in biology at the age of 25, theorized that the natural environment is fully capable of self-regulation, meaning that the human population is equally manageable by Nature. Likewise, any artificial attempt of population growth control may represent a scientifically heretical approach, leading to increased risks of inducing unprecedented harm to major fragments of the human civilization in the end.
- Manipulation of the climate, such as an attempt to block ultraviolet light from the sun in the atmosphere in the name of combating heat waves during the summer.
- A substantially decreased use and availability of natural remedies in healthcare settings with a progressively heavier reliance on pharmaceuticals instead.
- An increasingly widespread administration of medical drugs that often bring controversial health outcomes.
- Sedentary lifestyle induced by many, if not all listed factors above.
Conclusion
References
- Pollard, A.J., Bijker, E.M. A guide to vaccinology: from basic principles to new developments. Nat Rev Immunol 21, 83–100 (2021). [CrossRef]
- Yang, J., Qi, F., Gu, H., Zou, J., Yang, Y., Yuan, Q., & Yao, Z. (2016). Neonatal BCG vaccination of mice improves neurogenesis and behavior in early life. Brain research bulletin, 120, 25–33. [CrossRef]
- Morimoto K and Nakajima K (2019) Role of the Immune System in the Development of the Central Nervous System. Front. Neurosci. 13:916. [CrossRef]
- Baines KJ, Hillier DM, Haddad FL, Rajakumar N, Schmid S and Renaud SJ (2020) Maternal Immune Activation Alters Fetal Brain Development and Enhances Proliferation of Neural Precursor Cells in Rats. Front. Immunol. 11:1145. [CrossRef]
- Denes A and Miyan JA (2014) Brain-immune interactions in health and disease. Front. Neurosci. 8:382. [CrossRef]
- Kamimura D, Yamada M, Harada M, Sabharwal L, Meng J, Bando H, Ogura H, Atsumi T, Arima Y and Murakami M (2013) The gateway theory: bridging neural and immune interactions in the CNS. Front. Neurosci. 7:204. [CrossRef]
- Geenen V, Bodart G, Henry S, Michaux H, Dardenne O, Charlet-Renard C, Martens H and Hober D (2013) Programming of neuroendocrine self in the thymus and its defect in the development of neuroendocrine autoimmunity. Front. Neurosci. 7:187. [CrossRef]
- Goyal D. K. and Miyan J. A. (2014) Neuro-immune abnormalities in autism and their relationship with the environment: a variable insult model for autism. Front. Endocrinol. 5:29. [CrossRef]
- Sherwood, E. R., Burelbach, K. R., McBride, M. A., Stothers, C. L., Owen, A. M., Hernandez, A., Patil, N. K., Williams, D. L., & Bohannon, J. K. (2022). Innate Immune Memory and the Host Response to Infection. Journal of immunology (Baltimore, Md. : 1950), 208(4), 785–792. [CrossRef]
- Wendeln, A. C., Degenhardt, K., Kaurani, L., Gertig, M., Ulas, T., Jain, G., Wagner, J., Häsler, L. M., Wild, K., Skodras, A., Blank, T., Staszewski, O., Datta, M., Centeno, T. P., Capece, V., Islam, M. R., Kerimoglu, C., Staufenbiel, M., Schultze, J. L., Beyer, M., … Neher, J. J. (2018). Innate immune memory in the brain shapes neurological disease hallmarks. Nature, 556(7701), 332–338. [CrossRef]
- Netea, M. G., Quintin, J., & van der Meer, J. W. (2011). Trained immunity: a memory for innate host defense. Cell host & microbe, 9(5), 355–361. [CrossRef]
- Kloc, M., Kubiak, J. Z., Zdanowski, R., & Ghobrial, R. M. (2022). Memory Macrophages. International journal of molecular sciences, 24(1), 38. [CrossRef]
- Taylor M. W. (2014). Interferons. Viruses and Man: A History of Interactions, 101–119. [CrossRef]
- Chandwani, M. N., Creisher, P. S., & O’Donnell, L. A. (2019). Understanding the Role of Antiviral Cytokines and Chemokines on Neural Stem/Progenitor Cell Activity and Survival. Viral immunology, 32(1), 15–24. [CrossRef]
- Borsini, A., Cattaneo, A., Malpighi, C., Thuret, S., Harrison, N. A., MRC ImmunoPsychiatry Consortium, Zunszain, P. A., & Pariante, C. M. (2018). Interferon-Alpha Reduces Human Hippocampal Neurogenesis and Increases Apoptosis via Activation of Distinct STAT1-Dependent Mechanisms. The international journal of neuropsychopharmacology, 21(2), 187–200. [CrossRef]
- Borsini, A., Pariante, C. M., Zunszain, P. A., Hepgul, N., Russell, A., Zajkowska, Z., Mondelli, V., & Thuret, S. (2019). The role of circulatory systemic environment in predicting interferon-alpha-induced depression: The neurogenic process as a potential mechanism. Brain, behavior, and immunity, 81, 220–227. [CrossRef]
- Su, K. P., Lai, H. C., Peng, C. Y., Su, W. P., Chang, J. P., & Pariante, C. M. (2019). Interferon-alpha-induced depression: Comparisons between early- and late-onset subgroups and with patients with major depressive disorder. Brain, behavior, and immunity, 80, 512–518. [CrossRef]
- Lin, J. Y., Kuo, R. L., & Huang, H. I. (2019). Activation of type I interferon antiviral response in human neural stem cells. Stem cell research & therapy, 10(1), 387. [CrossRef]
- Bhat, H., Lang, K. S., Hardt, C., & Lang, J. (2019). Interferon in the CNS. Neuro-Signals, 27(S1), 44–53. [CrossRef]
- Owens, T., Khorooshi, R., Wlodarczyk, A., & Asgari, N. (2014). Interferons in the central nervous system: a few instruments play many tunes. Glia, 62(3), 339–355. [CrossRef]
- Blank, T., & Prinz, M. (2017). Type I interferon pathway in CNS homeostasis and neurological disorders. Glia, 65(9), 1397–1406. [CrossRef]
- Raftopoulou, S., Rapti, A., Karathanasis, D., Evangelopoulos, M. E., & Mavragani, C. P. (2022). The role of type I IFN in autoimmune and autoinflammatory diseases with CNS involvement. Frontiers in neurology, 13, 1026449. [CrossRef]
- McDonough, A., Lee, R. V., & Weinstein, J. R. (2017). Microglial Interferon Signaling and White Matter. Neurochemical research, 42(9), 2625–2638. [CrossRef]
- Giacobbe, J., Pariante, C. M., & Borsini, A. (2020). The innate immune system and neurogenesis as modulating mechanisms of electroconvulsive therapy in pre-clinical studies. Journal of psychopharmacology (Oxford, England), 34(10), 1086–1097. [CrossRef]
- Nettis, M. A., & Pariante, C. M. (2020). Is there neuroinflammation in depression? Understanding the link between the brain and the peripheral immune system in depression. International review of neurobiology, 152, 23–40. [CrossRef]
- Marques, A. H., Cizza, G., & Sternberg, E. (2007). Interações imunocerebrais e implicações nos transtornos psiquiátricos [Brain-immune interactions and implications in psychiatric disorders]. Revista brasileira de psiquiatria (Sao Paulo, Brazil : 1999), 29 Suppl 1, S27–S32. [CrossRef]
- Li, X. X., Lee, J. D., Kemper, C., & Woodruff, T. M. (2019). The Complement Receptor C5aR2: A Powerful Modulator of Innate and Adaptive Immunity. Journal of immunology (Baltimore, Md. : 1950), 202(12), 3339–3348. [CrossRef]
- Yu, S., Wang, D., Huang, L., Zhang, Y., Luo, R., Adah, D., Tang, Y., Zhao, K., & Lu, B. (2019). The complement receptor C5aR2 promotes protein kinase R expression and contributes to NLRP3 inflammasome activation and HMGB1 release from macrophages. The Journal of biological chemistry, 294(21), 8384–8394. [CrossRef]
- Hernandez, M. X., Namiranian, P., Nguyen, E., Fonseca, M. I., & Tenner, A. J. (2017). C5a Increases the Injury to Primary Neurons Elicited by Fibrillar Amyloid Beta. ASN neuro, 9(1), 1759091416687871. [CrossRef]
- Pamies, D., Sartori, C., Schvartz, D., González-Ruiz, V., Pellerin, L., Nunes, C., Tavel, D., Maillard, V., Boccard, J., Rudaz, S., Sanchez, J. C., & Zurich, M. G. (2021). Neuroinflammatory Response to TNFα and IL1β Cytokines Is Accompanied by an Increase in Glycolysis in Human Astrocytes In Vitro. International journal of molecular sciences, 22(8), 4065. [CrossRef]
- Dhungana, H., Rolova, T., Savchenko, E., Wojciechowski, S., Savolainen, K., Ruotsalainen, A. K., Sullivan, P. M., Koistinaho, J., & Malm, T. (2013). Western-type diet modulates inflammatory responses and impairs functional outcome following permanent middle cerebral artery occlusion in aged mice expressing the human apolipoprotein E4 allele. Journal of neuroinflammation, 10, 102. [CrossRef]
- Mäkinen, E., Lensu, S., Honkanen, M., Laitinen, P., Wikgren, J., Koch, L. G., Britton, S. L., Kainulainen, H., Pekkala, S., & Nokia, M. S. (2021). Rats bred for low intrinsic aerobic exercise capacity link obesity with brain inflammation and reduced structural plasticity of the hippocampus. Brain, behavior, and immunity, 97, 250–259. [CrossRef]
- Rudick, R. A., & Ransohoff, R. M. (1995). Biologic effects of interferons: relevance to multiple sclerosis. Multiple sclerosis (Houndmills, Basingstoke, England), 1 Suppl 1, S12–S16.
- Javed, A., & Reder, A. T. (2006). Therapeutic role of beta-interferons in multiple sclerosis. Pharmacology & therapeutics, 110(1), 35–56. [CrossRef]
- Li, Y., Zhao, L., Luo, Z., Zhang, Y., Lv, L., Zhao, J., Sui, B., Huang, F., Cui, M., Fu, Z. F., & Zhou, M. (2020). Interferon-λ Attenuates Rabies Virus Infection by Inducing Interferon-Stimulated Genes and Alleviating Neurological Inflammation. Viruses, 12(4), 405. [CrossRef]
- Qi, F., Zuo, Z., Yang, J., Hu, S., Yang, Y., Yuan, Q., Zou, J., Guo, K., & Yao, Z. (2017). Combined effect of BCG vaccination and enriched environment promote neurogenesis and spatial cognition via a shift in meningeal macrophage M2 polarization. Journal of neuroinflammation, 14(1), 32. [CrossRef]
- Qi, F., Zuo, Z., Hu, S., Xia, Y., Song, D., Kong, J., Yang, Y., Wu, Y., Wang, X., Yang, J., Hu, D., Yuan, Q., Zou, J., Guo, K., Xu, J., & Yao, Z. (2018). An enriched environment restores hepatitis B vaccination-mediated impairments in synaptic function through IFN-γ/Arginase1 signaling. Brain, behavior, and immunity, 71, 116–132. [CrossRef]
- Yang, J., Qi, F., Yang, Y., Yuan, Q., Zou, J., Guo, K., & Yao, Z. (2016). Neonatal hepatitis B vaccination impaired the behavior and neurogenesis of mice transiently in early adulthood. Psychoneuroendocrinology, 73, 166–176. [CrossRef]
- Wang, X., Yang, J., Xing, Z., Zhang, H., Wen, Y., Qi, F., Zuo, Z., Xu, J., & Yao, Z. (2018). IL-4 mediates the delayed neurobehavioral impairments induced by neonatal hepatitis B vaccination that involves the down-regulation of the IL-4 receptor in the hippocampus. Cytokine, 110, 137–149. [CrossRef]
- Qi, F., Yang, J., Xia, Y., Yuan, Q., Guo, K., Zou, J., & Yao, Z. (2016). A(H1N1) vaccination recruits T lymphocytes to the choroid plexus for the promotion of hippocampal neurogenesis and working memory in pregnant mice. Brain, behavior, and immunity, 53, 72–83.
- Xia, Y., Qi, F., Zou, J., Yang, J., & Yao, Z. (2014). Influenza vaccination during early pregnancy contributes to neurogenesis and behavioral function in offspring. Brain, behavior, and immunity, 42, 212–221. [CrossRef]
- Han, V. X., Patel, S., Jones, H. F., Nielsen, T. C., Mohammad, S. S., Hofer, M. J., Gold, W., Brilot, F., Lain, S. J., Nassar, N., & Dale, R. C. (2021). Maternal acute and chronic inflammation in pregnancy is associated with common neurodevelopmental disorders: a systematic review. Translational psychiatry, 11(1), 71. [CrossRef]
- Zhang, Z., & van Praag, H. (2015). Maternal immune activation differentially impacts mature and adult-born hippocampal neurons in male mice. Brain, behavior, and immunity, 45, 60–70. [CrossRef]
- Meyer, U., Nyffeler, M., Yee, B. K., Knuesel, I., & Feldon, J. (2008). Adult brain and behavioral pathological markers of prenatal immune challenge during early/middle and late fetal development in mice. Brain, behavior, and immunity, 22(4), 469–486. [CrossRef]
- Han, V. X., Patel, S., Jones, H. F., & Dale, R. C. (2021). Maternal immune activation and neuroinflammation in human neurodevelopmental disorders. Nature reviews. Neurology, 17(9), 564–579. [CrossRef]
- Han, V. X., Patel, S., Jones, H. F., Nielsen, T. C., Mohammad, S. S., Hofer, M. J., Gold, W., Brilot, F., Lain, S. J., Nassar, N., & Dale, R. C. (2021). Maternal acute and chronic inflammation in pregnancy is associated with common neurodevelopmental disorders: a systematic review. Translational psychiatry, 11(1), 71. [CrossRef]
- Lombardo, M. V., Moon, H. M., Su, J., Palmer, T. D., Courchesne, E., & Pramparo, T. (2018). Maternal immune activation dysregulation of the fetal brain transcriptome and relevance to the pathophysiology of autism spectrum disorder. Molecular psychiatry, 23(4), 1001–1013. [CrossRef]
- Haddad, F. L., Patel, S. V., & Schmid, S. (2020). Maternal Immune Activation by Poly I:C as a preclinical Model for Neurodevelopmental Disorders: A focus on Autism and Schizophrenia. Neuroscience and biobehavioral reviews, 113, 546–567. [CrossRef]
- Trifonova, E. A., Mustafin, Z. S., Lashin, S. A., & Kochetov, A. V. (2022). Abnormal mTOR Activity in Pediatric Autoimmune Neuropsychiatric and MIA-Associated Autism Spectrum Disorders. International journal of molecular sciences, 23(2), 967. [CrossRef]
- Han, V. X., Patel, S., Jones, H. F., Nielsen, T. C., Mohammad, S. S., Hofer, M. J., Gold, W., Brilot, F., Lain, S. J., Nassar, N., & Dale, R. C. (2021). Maternal acute and chronic inflammation in pregnancy is associated with common neurodevelopmental disorders: a systematic review. Translational psychiatry, 11(1), 71. [CrossRef]
- Meltzer, A., & Van de Water, J. (2017). The Role of the Immune System in Autism Spectrum Disorder. Neuropsychopharmacology : official publication of the American College of Neuropsychopharmacology, 42(1), 284–298. [CrossRef]
- Beversdorf, D. Q., Stevens, H. E., & Jones, K. L. (2018). Prenatal Stress, Maternal Immune Dysregulation, and Their Association With Autism Spectrum Disorders. Current psychiatry reports, 20(9), 76. [CrossRef]
- McLellan, J., Kim, D., Bruce, M., Ramirez-Celis, A., & Van de Water, J. (2022). Maternal Immune Dysregulation and Autism-Understanding the Role of Cytokines, Chemokines and Autoantibodies. Frontiers in psychiatry, 13, 834910. [CrossRef]
- Jones, K. L., & Van de Water, J. (2019). Maternal autoantibody related autism: mechanisms and pathways. Molecular psychiatry, 24(2), 252–265. [CrossRef]
- Beversdorf, D. Q., Shah, A., Jhin, A., Noel-MacDonnell, J., Hecht, P., Ferguson, B. J., Bruce, D., Tilley, M., & Talebizadeh, Z. (2021). microRNAs and Gene-Environment Interactions in Autism: Effects of Prenatal Maternal Stress and the SERT Gene on Maternal microRNA Expression. Frontiers in psychiatry, 12, 668577. [CrossRef]
- Boktor, J. C., Adame, M. D., Rose, D. R., Schumann, C. M., Murray, K. D., Bauman, M. D., Careaga, M., Mazmanian, S. K., Ashwood, P., & Needham, B. D. (2022). Global metabolic profiles in a non-human primate model of maternal immune activation: implications for neurodevelopmental disorders. Molecular psychiatry, 10.1038/s41380-022-01752-y. Advance online publication. [CrossRef]
- Abdallah, M. W., Larsen, N., Grove, J., Nørgaard-Pedersen, B., Thorsen, P., Mortensen, E. L., & Hougaard, D. M. (2013). Amniotic fluid inflammatory cytokines: potential markers of immunologic dysfunction in autism spectrum disorders. The world journal of biological psychiatry : the official journal of the World Federation of Societies of Biological Psychiatry, 14(7), 528–538. [CrossRef]
- Abdallah, M. W., Larsen, N., Mortensen, E. L., Atladóttir, H. Ó., Nørgaard-Pedersen, B., Bonefeld-Jørgensen, E. C., Grove, J., & Hougaard, D. M. (2012). Neonatal levels of cytokines and risk of autism spectrum disorders: an exploratory register-based historic birth cohort study utilizing the Danish Newborn Screening Biobank. Journal of neuroimmunology, 252(1-2), 75–82. [CrossRef]
- Abdallah, M. W., Larsen, N., Grove, J., Bonefeld-Jørgensen, E. C., Nørgaard-Pedersen, B., Hougaard, D. M., & Mortensen, E. L. (2013). Neonatal chemokine levels and risk of autism spectrum disorders: findings from a Danish historic birth cohort follow-up study. Cytokine, 61(2), 370–376. [CrossRef]
- Abdallah, M. W., Pearce, B. D., Larsen, N., Greaves-Lord, K., Nørgaard-Pedersen, B., Hougaard, D. M., Mortensen, E. L., & Grove, J. (2012). Amniotic fluid MMP-9 and neurotrophins in autism spectrum disorders: an exploratory study. Autism research : official journal of the International Society for Autism Research, 5(6), 428–433. [CrossRef]
- Missault, S., Van den Eynde, K., Vanden Berghe, W., Fransen, E., Weeren, A., Timmermans, J. P., Kumar-Singh, S., & Dedeurwaerdere, S. (2014). The risk for behavioural deficits is determined by the maternal immune response to prenatal immune challenge in a neurodevelopmental model. Brain, behavior, and immunity, 42, 138–146. [CrossRef]
- Han, V. X., Jones, H. F., Patel, S., Mohammad, S. S., Hofer, M. J., Alshammery, S., Maple-Brown, E., Gold, W., Brilot, F., & Dale, R. C. (2022). Emerging evidence of Toll-like receptors as a putative pathway linking maternal inflammation and neurodevelopmental disorders in human offspring: A systematic review. Brain, behavior, and immunity, 99, 91–105. [CrossRef]
- Chen, S., Zhao, S., Dalman, C., Karlsson, H., & Gardner, R. (2021). Association of maternal diabetes with neurodevelopmental disorders: autism spectrum disorders, attention-deficit/hyperactivity disorder and intellectual disability. International journal of epidemiology, 50(2), 459–474. [CrossRef]
- Wiegersma, A. M., Dalman, C., Lee, B. K., Karlsson, H., & Gardner, R. M. (2019). Association of Prenatal Maternal Anemia With Neurodevelopmental Disorders. JAMA psychiatry, 76(12), 1294–1304. [CrossRef]
- Wang, Z., Chan, A., Coghill, D., Ip, P., Lau, W., Simonoff, E., Brauer, R., Wei, L., Wong, I., & Man, K. (2021). Association Between Prenatal Exposure to Antipsychotics and Attention-Deficit/Hyperactivity Disorder, Autism Spectrum Disorder, Preterm Birth, and Small for Gestational Age. JAMA internal medicine, 181(10), 1332–1340. [CrossRef]
- Brand, J. S., Lawlor, D. A., Larsson, H., & Montgomery, S. (2021). Association Between Hypertensive Disorders of Pregnancy and Neurodevelopmental Outcomes Among Offspring. JAMA pediatrics, 175(6), 577–585. [CrossRef]
- Bergdolt, L., & Dunaevsky, A. (2019). Brain changes in a maternal immune activation model of neurodevelopmental brain disorders. Progress in neurobiology, 175, 1–19. [CrossRef]
- Ryan, A. M., & Bauman, M. D. (2022). Primate Models as a Translational Tool for Understanding Prenatal Origins of Neurodevelopmental Disorders Associated With Maternal Infection. Biological psychiatry. Cognitive neuroscience and neuroimaging, 7(5), 510–523. [CrossRef]
- Vlasova, R. M., Iosif, A. M., Ryan, A. M., Funk, L. H., Murai, T., Chen, S., Lesh, T. A., Rowland, D. J., Bennett, J., Hogrefe, C. E., Maddock, R. J., Gandal, M. J., Geschwind, D. H., Schumann, C. M., Van de Water, J., McAllister, A. K., Carter, C. S., Styner, M. A., Amaral, D. G., & Bauman, M. D. (2021). Maternal Immune Activation during Pregnancy Alters Postnatal Brain Growth and Cognitive Development in Nonhuman Primate Offspring. The Journal of neuroscience : the official journal of the Society for Neuroscience, 41(48), 9971–9987. [CrossRef]
- Bauman, M. D., Iosif, A. M., Smith, S. E., Bregere, C., Amaral, D. G., & Patterson, P. H. (2014). Activation of the maternal immune system during pregnancy alters behavioral development of rhesus monkey offspring. Biological psychiatry, 75(4), 332–341. [CrossRef]
- Zhang, J., Yao, P., Han, W., Luo, Y., Li, Y., Yang, Y., Xia, H., Chen, Z., Chen, Q., Wang, H., Yang, L., Li, H., Hu, C., Huang, H., Peng, Z., Tan, X., Li, M., & Yang, J. (2022). Maternal Prenatal Inflammation Increases Brain Damage Susceptibility of Lipopolysaccharide in Adult Rat Offspring via COX-2/PGD-2/DPs Pathway Activation. International journal of molecular sciences, 23(11), 6142. [CrossRef]
- Li, Y., Luo, W., Zhang, J., Luo, Y., Han, W., Wang, H., Xia, H., Chen, Z., Yang, Y., Chen, Q., Li, H., Yang, L., Hu, C., Huang, H., Peng, Z., Tan, X., Li, M., & Yang, J. (2022). Maternal Inflammation Exaggerates Offspring Susceptibility to Cerebral Ischemia-Reperfusion Injury via the COX-2/PGD2/DP2 Pathway Activation. Oxidative medicine and cellular longevity, 2022, 1571705. [CrossRef]
- Careaga, M., Murai, T., & Bauman, M. D. (2017). Maternal Immune Activation and Autism Spectrum Disorder: From Rodents to Nonhuman and Human Primates. Biological psychiatry, 81(5), 391–401. [CrossRef]
- Weir, R. K., Forghany, R., Smith, S. E., Patterson, P. H., McAllister, A. K., Schumann, C. M., & Bauman, M. D. (2015). Preliminary evidence of neuropathology in nonhuman primates prenatally exposed to maternal immune activation. Brain, behavior, and immunity, 48, 139–146. [CrossRef]
- Rose, D. R., Careaga, M., Van de Water, J., McAllister, K., Bauman, M. D., & Ashwood, P. (2017). Long-term altered immune responses following fetal priming in a non-human primate model of maternal immune activation. Brain, behavior, and immunity, 63, 60–70. [CrossRef]
- Missault, S., Van den Eynde, K., Vanden Berghe, W., Fransen, E., Weeren, A., Timmermans, J. P., Kumar-Singh, S., & Dedeurwaerdere, S. (2014). The risk for behavioural deficits is determined by the maternal immune response to prenatal immune challenge in a neurodevelopmental model. Brain, behavior, and immunity, 42, 138–146. [CrossRef]
- Tan, J. W. Y., Lee, O. P. E., & Leong, M. C. (2021). Vitamin C deficiency as an unusual cause of pulmonary hypertension and refusal to walk. Cardiology in the young, 31(2), 322–324. [CrossRef]
- Vuillermot, S., Luan, W., Meyer, U., & Eyles, D. (2017). Vitamin D treatment during pregnancy prevents autism-related phenotypes in a mouse model of maternal immune activation. Molecular autism, 8, 9. [CrossRef]
- Gáll, Z., & Székely, O. (2021). Role of Vitamin D in Cognitive Dysfunction: New Molecular Concepts and Discrepancies between Animal and Human Findings. Nutrients, 13(11), 3672. [CrossRef]
- Ong, Z. Y., & Muhlhausler, B. S. (2011). Maternal “junk-food” feeding of rat dams alters food choices and development of the mesolimbic reward pathway in the offspring. FASEB journal : official publication of the Federation of American Societies for Experimental Biology, 25(7), 2167–2179. [CrossRef]
- Saurman, V., Margolis, K. G., & Luna, R. A. (2020). Autism Spectrum Disorder as a Brain-Gut-Microbiome Axis Disorder. Digestive diseases and sciences, 65(3), 818–828. [CrossRef]
- Chernikova, M. A., Flores, G. D., Kilroy, E., Labus, J. S., Mayer, E. A., & Aziz-Zadeh, L. (2021). The Brain-Gut-Microbiome System: Pathways and Implications for Autism Spectrum Disorder. Nutrients, 13(12), 4497. [CrossRef]
- Alharthi, A., Alhazmi, S., Alburae, N., & Bahieldin, A. (2022). The Human Gut Microbiome as a Potential Factor in Autism Spectrum Disorder. International journal of molecular sciences, 23(3), 1363. [CrossRef]
- Wang, X., Yang, J., Zhang, H., Yu, J., & Yao, Z. (2019). Oral probiotic administration during pregnancy prevents autism-related behaviors in offspring induced by maternal immune activation via anti-inflammation in mice. Autism research : official journal of the International Society for Autism Research, 12(4), 576–588. [CrossRef]
- Haddad, F. L., Patel, S. V., & Schmid, S. (2020). Maternal Immune Activation by Poly I:C as a preclinical Model for Neurodevelopmental Disorders: A focus on Autism and Schizophrenia. Neuroscience and biobehavioral reviews, 113, 546–567. https://doi.org/10.1016/j.neubiorev.2020.04.012Delorme, T. C., Srivastava, L. K., & Cermakian, N. (2021). Altered circadian rhythms in a mouse model of neurodevelopmental disorders based on prenatal maternal immune activation. Brain, behavior, and immunity, 93, 119–131. https://doi.org/10.1016/j.bbi.2020.12.030.
- Morimoto K. and Nakajima K. (2019) Role of the Immune System in the Development of the Central Nervous System. Front. Neurosci. 13:916. [CrossRef]
- Mueller, F. S., Polesel, M., Richetto, J., Meyer, U., & Weber-Stadlbauer, U. (2018). Mouse models of maternal immune activation: Mind your caging system!. Brain, behavior, and immunity, 73, 643–660. [CrossRef]
- Smolders, S., Notter, T., Smolders, S., Rigo, J. M., & Brône, B. (2018). Controversies and prospects about microglia in maternal immune activation models for neurodevelopmental disorders. Brain, behavior, and immunity, 73, 51–65. [CrossRef]
- Fernández de Cossío, L., Guzmán, A., van der Veldt, S., & Luheshi, G. N. (2017). Prenatal infection leads to ASD-like behavior and altered synaptic pruning in the mouse offspring. Brain, behavior, and immunity, 63, 88–98. [CrossRef]
- Tsukada, T., Shimada, H., Sakata-Haga, H., Iizuka, H., & Hatta, T. (2019). Molecular mechanisms underlying the models of neurodevelopmental disorders in maternal immune activation relevant to the placenta. Congenital anomalies, 59(3), 81–87. [CrossRef]
- Meyer U. (2019). Neurodevelopmental Resilience and Susceptibility to Maternal Immune Activation. Trends in neurosciences, 42(11), 793–806. [CrossRef]
- Massrali, A., Adhya, D., Srivastava, D. P., Baron-Cohen, S., & Kotter, M. R. (2022). Virus-Induced Maternal Immune Activation as an Environmental Factor in the Etiology of Autism and Schizophrenia. Frontiers in neuroscience, 16, 834058. [CrossRef]
- Cheng, M. H., Zhang, S., Porritt, R. A., Noval Rivas, M., Paschold, L., Willscher, E., Binder, M., Arditi, M., & Bahar, I. (2020). Superantigenic character of an insert unique to SARS-CoV-2 spike supported by skewed TCR repertoire in patients with hyperinflammation. Proceedings of the National Academy of Sciences of the United States of America, 117(41), 25254–25262. [CrossRef]
- Noval Rivas, M., Porritt, R. A., Cheng, M. H., Bahar, I., & Arditi, M. (2022). Multisystem Inflammatory Syndrome in Children and Long COVID: The SARS-CoV-2 Viral Superantigen Hypothesis. Frontiers in immunology, 13, 941009. [CrossRef]
- Porritt, R. A., Paschold, L., Rivas, M. N., Cheng, M. H., Yonker, L. M., Chandnani, H., Lopez, M., Simnica, D., Schultheiß, C., Santiskulvong, C., Van Eyk, J., Fasano, A., Bahar, I., Binder, M., & Arditi, M. (2020). Identification of a unique TCR repertoire, consistent with a superantigen selection process in Children with Multi-system Inflammatory Syndrome. bioRxiv : the preprint server for biology, 2020.11.09.372169. [CrossRef]
- Wong, H., & Hoeffer, C. (2018). Maternal IL-17A in autism. Experimental neurology, 299(Pt A), 228–240. [CrossRef]
- Choi, G. B., Yim, Y. S., Wong, H., Kim, S., Kim, H., Kim, S. V., Hoeffer, C. A., Littman, D. R., & Huh, J. R. (2016). The maternal interleukin-17a pathway in mice promotes autism-like phenotypes in offspring. Science (New York, N.Y.), 351(6276), 933–939. [CrossRef]
- Li, Q., Li, J., Tian, J., Zhu, B., Zhang, Y., Yang, K., Ling, Y., & Hu, Y. (2012). IL-17 and IFN-γ production in peripheral blood following BCG vaccination and Mycobacterium tuberculosis infection in human. European review for medical and pharmacological sciences, 16(14), 2029–2036.
- Shen, H., Wang, Y., Chen, C. Y., Frencher, J., Huang, D., Yang, E., Ryan-Payseur, B., & Chen, Z. W. (2015). Th17-related cytokines contribute to recall-like expansion/effector function of HMBPP-specific Vγ2Vδ2 T cells after Mycobacterium tuberculosis infection or vaccination. European journal of immunology, 45(2), 442–451. [CrossRef]
- Wozniak, T. M., Saunders, B. M., Ryan, A. A., & Britton, W. J. (2010). Mycobacterium bovis BCG-specific Th17 cells confer partial protection against Mycobacterium tuberculosis infection in the absence of gamma interferon. Infection and immunity, 78(10), 4187–4194. [CrossRef]
- Burl, S., Adetifa, U. J., Cox, M., Touray, E., Ota, M. O., Marchant, A., Whittle, H., McShane, H., Rowland-Jones, S. L., & Flanagan, K. L. (2010). Delaying bacillus Calmette-Guérin vaccination from birth to 4 1/2 months of age reduces postvaccination Th1 and IL-17 responses but leads to comparable mycobacterial responses at 9 months of age. Journal of immunology (Baltimore, Md. : 1950), 185(4), 2620–2628. [CrossRef]
- Freches, D., Romano, M., Korf, H., Renauld, J. C., Van Snick, J., Uyttenhove, C., & Huygen, K. (2011). Increased pulmonary tumor necrosis factor alpha, interleukin-6 (IL-6), and IL-17A responses compensate for decreased gamma interferon production in anti-IL-12 autovaccine-treated, Mycobacterium bovis BCG-vaccinated mice. Clinical and vaccine immunology : CVI, 18(1), 95–104. [CrossRef]
- Pitt, J. M., Stavropoulos, E., Redford, P. S., Beebe, A. M., Bancroft, G. J., Young, D. B., & O’Garra, A. (2012). Blockade of IL-10 signaling during bacillus Calmette-Guérin vaccination enhances and sustains Th1, Th17, and innate lymphoid IFN-γ and IL-17 responses and increases protection to Mycobacterium tuberculosis infection. Journal of immunology (Baltimore, Md. : 1950), 189(8), 4079–4087. [CrossRef]
- Kim, S., Kim, H., Yim, Y. S., Ha, S., Atarashi, K., Tan, T. G., Longman, R. S., Honda, K., Littman, D. R., Choi, G. B., & Huh, J. R. (2017). Maternal gut bacteria promote neurodevelopmental abnormalities in mouse offspring. Nature, 549(7673), 528–532. [CrossRef]
- Knuesel, I., Chicha, L., Britschgi, M., Schobel, S. A., Bodmer, M., Hellings, J. A., Toovey, S., & Prinssen, E. P. (2014). Maternal immune activation and abnormal brain development across CNS disorders. Nature reviews. Neurology, 10(11), 643–660. [CrossRef]
- Bergdolt, L., & Dunaevsky, A. (2019). Brain changes in a maternal immune activation model of neurodevelopmental brain disorders. Progress in neurobiology, 175, 1–19. [CrossRef]
- Bauman, M. D., & Van de Water, J. (2020). Translational opportunities in the prenatal immune environment: Promises and limitations of the maternal immune activation model. Neurobiology of disease, 141, 104864. [CrossRef]
- Ashe, P. C., Berry, M. D., & Boulton, A. A. (2001). Schizophrenia, a neurodegenerative disorder with neurodevelopmental antecedents. Progress in neuro-psychopharmacology & biological psychiatry, 25(4), 691–707. https://doi.org/10.1016/s0278-5846(01)00159-2Rund B. R. (2009). Is schizophrenia a neurodegenerative disorder?. Nordic journal of psychiatry, 63(3), 196–201. https://doi.org/10.1080/08039480902767286.
- Kochunov, P., & Hong, L. E. (2014). Neurodevelopmental and neurodegenerative models of schizophrenia: white matter at the center stage. Schizophrenia bulletin, 40(4), 721–728. [CrossRef]
- Stone, W. S., Phillips, M. R., Yang, L. H., Kegeles, L. S., Susser, E. S., & Lieberman, J. A. (2022). Neurodegenerative model of schizophrenia: Growing evidence to support a revisit. Schizophrenia research, 243, 154–162. [CrossRef]
- Chien, Y. L., Lin, H. Y., Tung, Y. H., Hwang, T. J., Chen, C. L., Wu, C. S., Shang, C. Y., Hwu, H. G., Tseng, W. I., Liu, C. M., & Gau, S. S. (2022). Neurodevelopmental model of schizophrenia revisited: similarity in individual deviation and idiosyncrasy from the normative model of whole-brain white matter tracts and shared brain-cognition covariation with ADHD and ASD. Molecular psychiatry, 10.1038/s41380-022-01636-1. Advance online publication. [CrossRef]
- Mooij, S., Henson, R., Waldorp, L. J., & Kievit, R. A. (2018). Age Differentiation within Gray Matter, White Matter, and between Memory and White Matter in an Adult Life Span Cohort. The Journal of neuroscience : the official journal of the Society for Neuroscience, 38(25), 5826–5836. [CrossRef]
- Cropley, V. L., Klauser, P., Lenroot, R. K., Bruggemann, J., Sundram, S., Bousman, C., Pereira, A., Di Biase, M. A., Weickert, T. W., Weickert, C. S., Pantelis, C., & Zalesky, A. (2017). Accelerated Gray and White Matter Deterioration With Age in Schizophrenia. The American journal of psychiatry, 174(3), 286–295. [CrossRef]
- Fletcher, E., Gavett, B., Harvey, D., Farias, S. T., Olichney, J., Beckett, L., DeCarli, C., & Mungas, D. (2018). Brain volume change and cognitive trajectories in aging. Neuropsychology, 32(4), 436–449. [CrossRef]
- Rao, J., Chiappelli, J., Kochunov, P., Regenold, W. T., Rapoport, S. I., & Hong, L. E. (2015). Is schizophrenia a neurodegenerative disease? Evidence from age-related decline of brain-derived neurotrophic factor in the brains of schizophrenia patients and matched nonpsychiatric controls. Neuro-degenerative diseases, 15(1), 38–44. [CrossRef]
- Lasoń, W., Jantas, D., Leśkiewicz, M., Regulska, M., & Basta-Kaim, A. (2023). The Vitamin D Receptor as a Potential Target for the Treatment of Age-Related Neurodegenerative Diseases Such as Alzheimer’s and Parkinson’s Diseases: A Narrative Review. Cells, 12(4), 660. [CrossRef]
- Hollander, E., Wang, A. T., Braun, A., & Marsh, L. (2009). Neurological considerations: autism and Parkinson’s disease. Psychiatry research, 170(1), 43–51. [CrossRef]
- Dinan, T. G., & Cryan, J. F. (2017). The Microbiome-Gut-Brain Axis in Health and Disease. Gastroenterology clinics of North America, 46(1), 77–89. [CrossRef]
- Sung, P. S., Lin, P. Y., Liu, C. H., Su, H. C., & Tsai, K. J. (2020). Neuroinflammation and Neurogenesis in Alzheimer’s Disease and Potential Therapeutic Approaches. International journal of molecular sciences, 21(3), 701. [CrossRef]
- Deneubourg, C., Ramm, M., Smith, L. J., Baron, O., Singh, K., Byrne, S. C., Duchen, M. R., Gautel, M., Eskelinen, E. L., Fanto, M., & Jungbluth, H. (2022). The spectrum of neurodevelopmental, neuromuscular and neurodegenerative disorders due to defective autophagy. Autophagy, 18(3), 496–517. [CrossRef]
- Young, H. K., Barton, B. A., Waisbren, S., Portales Dale, L., Ryan, M. M., Webster, R. I., & North, K. N. (2008). Cognitive and psychological profile of males with Becker muscular dystrophy. Journal of child neurology, 23(2), 155–162. [CrossRef]
- Koeks, Z., Hellebrekers, D. M. J., van de Velde, N. M., Alleman, I., Spitali, P., van Duyvenvoorde, H. A., Verschuuren, J. J. G. M., Hendriksen, J. G. M., & Niks, E. H. (2022). The neurocognitive profile of adults with Becker muscular dystrophy in the Netherlands. Journal of neuromuscular diseases, 9(4), 543–553. [CrossRef]
- Balasubramanian, M., Fratzl-Zelman, N., O’Sullivan, R., Bull, M., Fa Peel, N., Pollitt, R. C., Jones, R., Milne, E., Smith, K., Roschger, P., Klaushofer, K., & Bishop, N. J. (2018). Novel PLS3 variants in X-linked osteoporosis: Exploring bone material properties. American journal of medical genetics. Part A, 176(7), 1578–1586. [CrossRef]
- Yousefi, B., Kokhaei, P., Mehranfar, F., Bahar, A., Abdolshahi, A., Emadi, A., & Eslami, M. (2022). The role of the host microbiome in autism and neurodegenerative disorders and effect of epigenetic procedures in the brain functions. Neuroscience and biobehavioral reviews, 132, 998–1009. [CrossRef]
- Cryan, J. F., O’Riordan, K. J., Sandhu, K., Peterson, V., & Dinan, T. G. (2020). The gut microbiome in neurological disorders. The Lancet. Neurology, 19(2), 179–194. [CrossRef]
- Chen, Y., Xu, J., & Chen, Y. (2021). Regulation of Neurotransmitters by the Gut Microbiota and Effects on Cognition in Neurological Disorders. Nutrients, 13(6), 2099. [CrossRef]
- Fang, P., Kazmi, S. A., Jameson, K. G., & Hsiao, E. Y. (2020). The Microbiome as a Modifier of Neurodegenerative Disease Risk. Cell host & microbe, 28(2), 201–222. https://doi.org/10.1016/j.chom.2020.06.008Sasmita A. O. (2019). Modification of the gut microbiome to combat neurodegeneration. Reviews in the neurosciences, 30(8), 795–805. https://doi.org/10.1515/revneuro-2019-0005.
- Fang X. (2016). Potential role of gut microbiota and tissue barriers in Parkinson’s disease and amyotrophic lateral sclerosis. The International journal of neuroscience, 126(9), 771–776. [CrossRef]
- Peterson C. T. (2020). Dysfunction of the Microbiota-Gut-Brain Axis in Neurodegenerative Disease: The Promise of Therapeutic Modulation With Prebiotics, Medicinal Herbs, Probiotics, and Synbiotics. Journal of evidence-based integrative medicine, 25, 2515690X20957225. [CrossRef]
- Alfonsetti, M., Castelli, V., & d’Angelo, M. (2022). Are We What We Eat? Impact of Diet on the Gut-Brain Axis in Parkinson’s Disease. Nutrients, 14(2), 380. [CrossRef]
- Moustafa, S. A., Mohamed, S., Dawood, A., Azar, J., Elmorsy, E., Rizk, N., & Salama, M. (2021). Gut brain axis: an insight into microbiota role in Parkinson’s disease. Metabolic brain disease, 36(7), 1545–1557. [CrossRef]
- Mulak, A., & Bonaz, B. (2015). Brain-gut-microbiota axis in Parkinson’s disease. World journal of gastroenterology, 21(37), 10609–10620. [CrossRef]
- Gonatopoulos-Pournatzis, T., Niibori, R., Salter, E. W., Weatheritt, R. J., Tsang, B., Farhangmehr, S., Liang, X., Braunschweig, U., Roth, J., Zhang, S., Henderson, T., Sharma, E., Quesnel-Vallières, M., Permanyer, J., Maier, S., Georgiou, J., Irimia, M., Sonenberg, N., Forman-Kay, J. D., Gingras, A. C., … Blencowe, B. J. (2020). Autism-Misregulated eIF4G Microexons Control Synaptic Translation and Higher Order Cognitive Functions. Molecular cell, 77(6), 1176–1192.e16. [CrossRef]
- Gonatopoulos-Pournatzis, T., Wu, M., Braunschweig, U., Roth, J., Han, H., Best, A. J., Raj, B., Aregger, M., O’Hanlon, D., Ellis, J. D., Calarco, J. A., Moffat, J., Gingras, A. C., & Blencowe, B. J. (2018). Genome-wide CRISPR-Cas9 Interrogation of Splicing Networks Reveals a Mechanism for Recognition of Autism-Misregulated Neuronal Microexons. Molecular cell, 72(3), 510–524.e12. [CrossRef]
- Irimia, M., Weatheritt, R. J., Ellis, J. D., Parikshak, N. N., Gonatopoulos-Pournatzis, T., Babor, M., Quesnel-Vallières, M., Tapial, J., Raj, B., O’Hanlon, D., Barrios-Rodiles, M., Sternberg, M. J., Cordes, S. P., Roth, F. P., Wrana, J. L., Geschwind, D. H., & Blencowe, B. J. (2014). A highly conserved program of neuronal microexons is misregulated in autistic brains. Cell, 159(7), 1511–1523. [CrossRef]
- Quesnel-Vallières, M., Irimia, M., Cordes, S. P., & Blencowe, B. J. (2015). Essential roles for the splicing regulator nSR100/SRRM4 during nervous system development. Genes & development, 29(7), 746–759. [CrossRef]
- Raj, B., Irimia, M., Braunschweig, U., Sterne-Weiler, T., O’Hanlon, D., Lin, Z. Y., Chen, G. I., Easton, L. E., Ule, J., Gingras, A. C., Eyras, E., & Blencowe, B. J. (2014). A global regulatory mechanism for activating an exon network required for neurogenesis. Molecular cell, 56(1), 90–103. [CrossRef]
- Raj, B., O’Hanlon, D., Vessey, J. P., Pan, Q., Ray, D., Buckley, N. J., Miller, F. D., & Blencowe, B. J. (2011). Cross-regulation between an alternative splicing activator and a transcription repressor controls neurogenesis. Molecular cell, 43(5), 843–850. [CrossRef]
- Saso, A., & Kampmann, B. (2017). Vaccine responses in newborns. Seminars in immunopathology, 39(6), 627–642. [CrossRef]
- Chaudhari T. (2021). Vaccinations in the newborn. Best practice & research. Clinical obstetrics & gynaecology, 76, 66–82. [CrossRef]
- Sakala, I. G., Eichinger, K. M., & Petrovsky, N. (2019). Neonatal vaccine effectiveness and the role of adjuvants. Expert review of clinical immunology, 15(8), 869–878. [CrossRef]
- Clemens, E. A., & Alexander-Miller, M. A. (2021). Understanding Antibody Responses in Early Life: Baby Steps towards Developing an Effective Influenza Vaccine. Viruses, 13(7), 1392. [CrossRef]
- Nguyen, M., Julien, JP. & Rivest, S. Innate immunity: the missing link in neuroprotection and neurodegeneration?. Nat Rev Neurosci 3, 216–227 (2002). [CrossRef]
- Lehnardt S. (2010). Innate immunity and neuroinflammation in the CNS: the role of microglia in Toll-like receptor-mediated neuronal injury. Glia, 58(3), 253–263. [CrossRef]
- Woods, J. A., Vieira, V. J., & Keylock, K. T. (2006). Exercise, inflammation, and innate immunity. Neurologic clinics, 24(3), 585–599. [CrossRef]
- Scheffer, D., & Latini, A. (2020). Exercise-induced immune system response: Anti-inflammatory status on peripheral and central organs. Biochimica et biophysica acta. Molecular basis of disease, 1866(10), 165823. [CrossRef]
- Petersen, A. M., & Pedersen, B. K. (2006). The role of IL-6 in mediating the anti-inflammatory effects of exercise. Journal of physiology and pharmacology : an official journal of the Polish Physiological Society, 57 Suppl 10, 43–51.
- Hsu, C. J., Wong, L. C., & Lee, W. T. (2021). Immunological Dysfunction in Tourette Syndrome and Related Disorders. International journal of molecular sciences, 22(2), 853. [CrossRef]
- Leonard, H. L., & Swedo, S. E. (2001). Paediatric autoimmune neuropsychiatric disorders associated with streptococcal infection (PANDAS). The international journal of neuropsychopharmacology, 4(2), 191–198. [CrossRef]
- Bellato, A., Norman, L., Idrees, I., Ogawa, C. Y., Waitt, A., Zuccolo, P. F., Tye, C., Radua, J., Groom, M. J., & Shephard, E. (2021). A systematic review and meta-analysis of altered electrophysiological markers of performance monitoring in Obsessive-Compulsive Disorder (OCD), Gilles de la Tourette Syndrome (GTS), Attention-Deficit/Hyperactivity disorder (ADHD) and Autism. Neuroscience and biobehavioral reviews, 131, 964–987. [CrossRef]
- Kurlan R. (1998). Tourette’s syndrome and ‘PANDAS’: will the relation bear out? Pediatric autoimmune neuropsychiatric disorders associated with streptococcal infection. Neurology, 50(6), 1530–1534. [CrossRef]
- Trifiletti, R. R., & Packard, A. M. (1999). Immune mechanisms in pediatric neuropsychiatric disorders. Tourette’s syndrome, OCD, and PANDAS. Child and adolescent psychiatric clinics of North America, 8(4), 767–775.
- Suhas, S., & Rao, N. P. (2019). Neurocognitive deficits in obsessive-compulsive disorder: A selective review. Indian journal of psychiatry, 61(Suppl 1), S30–S36. [CrossRef]
- Cox, D. J., Field, R. H., Williams, D. G., Baran, M., Bowie, A. G., Cunningham, C., & Dunne, A. (2015). DNA sensors are expressed in astrocytes and microglia in vitro and are upregulated during gliosis in neurodegenerative disease. Glia, 63(5), 812–825. [CrossRef]
- Elizalde-Díaz, J. P., Miranda-Narváez, C. L., Martínez-Lazcano, J. C., & Martínez-Martínez, E. (2022). The relationship between chronic immune response and neurodegenerative damage in long COVID-19. Frontiers in immunology, 13, 1039427. [CrossRef]
- Zengeler, K. E., & Lukens, J. R. (2021). Innate immunity at the crossroads of healthy brain maturation and neurodevelopmental disorders. Nature reviews. Immunology, 21(7), 454–468. [CrossRef]
- Filiano, A. J., Gadani, S. P., & Kipnis, J. (2015). Interactions of innate and adaptive immunity in brain development and function. Brain research, 1617, 18–27. [CrossRef]
- Filipello, F., Morini, R., Corradini, I., Zerbi, V., Canzi, A., Michalski, B., Erreni, M., Markicevic, M., Starvaggi-Cucuzza, C., Otero, K., Piccio, L., Cignarella, F., Perrucci, F., Tamborini, M., Genua, M., Rajendran, L., Menna, E., Vetrano, S., Fahnestock, M., Paolicelli, R. C., … Matteoli, M. (2018). The Microglial Innate Immune Receptor TREM2 Is Required for Synapse Elimination and Normal Brain Connectivity. Immunity, 48(5), 979–991.e8. [CrossRef]
- Al-Haddad, B., Oler, E., Armistead, B., Elsayed, N. A., Weinberger, D. R., Bernier, R., Burd, I., Kapur, R., Jacobsson, B., Wang, C., Mysorekar, I., Rajagopal, L., & Adams Waldorf, K. M. (2019). The fetal origins of mental illness. American journal of obstetrics and gynecology, 221(6), 549–562.
- Pape, K., Tamouza, R., Leboyer, M., & Zipp, F. (2019). Immunoneuropsychiatry – novel perspectives on brain disorders. Nature reviews. Neurology, 15(6), 317–328. [CrossRef]
- Ornoy, A., Weinstein-Fudim, L., & Ergaz, Z. (2015). Prenatal factors associated with autism spectrum disorder (ASD). Reproductive toxicology (Elmsford, N.Y.), 56, 155–169. [CrossRef]
- Gasser, B. A., Buerki, S. F., Kurz, J., & Mohaupt, M. G. (2021). Hyperandrogenism? Increased 17, 20-Lyase Activity? A Metanalysis and Systematic Review of Altered Androgens in Boys and Girls with Autism. International journal of molecular sciences, 22(22), 12324. [CrossRef]
- Figueiredo, C. P., Fontes-Dantas, F. L., da Poian, A. T., & Clarke, J. R. (2021). SARS-CoV-2-associated cytokine storm during pregnancy as a possible risk factor for neuropsychiatric disorder development in post-pandemic infants. Neuropharmacology, 201, 108841. [CrossRef]
- Xu, Z. X., Kim, G. H., Tan, J. W., Riso, A. E., Sun, Y., Xu, E. Y., Liao, G. Y., Xu, H., Lee, S. H., Do, N. Y., Lee, C. H., Clipperton-Allen, A. E., Kwon, S., Page, D. T., Lee, K. J., & Xu, B. (2020). Elevated protein synthesis in microglia causes autism-like synaptic and behavioral aberrations. Nature communications, 11(1), 1797. [CrossRef]
- Salter, M. W., & Stevens, B. (2017). Microglia emerge as central players in brain disease. Nature medicine, 23(9), 1018–1027. [CrossRef]
- Eberl, G. A new age for (mucosal) NeuroImmunology. Mucosal Immunol (2022). [CrossRef]
- Guglielmi, L., Servettini, I., Caramia, M., Catacuzzeno, L., Franciolini, F., D’Adamo, M. C., & Pessia, M. (2015). Update on the implication of potassium channels in autism: K(+) channelautism spectrum disorder. Frontiers in cellular neuroscience, 9, 34. [CrossRef]
- Reid, K. H., Guo, S. Z., & Iyer, V. G. (2000). Agents which block potassium-chloride cotransport prevent sound-triggered seizures in post-ischemic audiogenic seizure-prone rats. Brain research, 864(1), 134–137. [CrossRef]
- Martel, P., Leo, D., Fulton, S., Bérard, M., & Trudeau, L. E. (2011). Role of Kv1 potassium channels in regulating dopamine release and presynaptic D2 receptor function. PloS one, 6(5), e20402. [CrossRef]
- Fung, L. K., Libove, R. A., Phillips, J., Haddad, F., & Hardan, A. Y. (2014). Brief report: an open-label study of the neurosteroid pregnenolone in adults with autism spectrum disorder. Journal of autism and developmental disorders, 44(11), 2971–2977. [CrossRef]
- Geier, D. A., & Geier, M. R. (2006). A clinical trial of combined anti-androgen and anti-heavy metal therapy in autistic disorders. Neuro endocrinology letters, 27(6), 833–838.
- Palomba, S., Orio, F., Jr, Falbo, A., Oppedisano, R., Tolino, A., & Zullo, F. (2008). Tibolone reverses the cognitive effects caused by leuprolide acetate administration, improving mood and quality of life in patients with symptomatic uterine leiomyomas. Fertility and sterility, 90(1), 165–173. [CrossRef]
- Andrabi, S. S., Parvez, S., & Tabassum, H. (2017). Neurosteroids and ischemic stroke: progesterone a promising agent in reducing the brain injury in ischemic stroke. Journal of Environmental Pathology, Toxicology and Oncology, 36(3).
- Medical article indicating a possible efficacy of leuprolide acetate against Alzheimer’s Disease; available at: https://www.neurologyadvisor.com/topics/alzheimers-disease-and-dementia/leuprolide-acetate-potential-treatment-for-alzheimer-disease-in-women/.
- Schober, J. M., Kuhn, P. J., Kovacs, P. G., Earle, J. H., Byrne, P. M., & Fries, R. A. (2005). Leuprolide acetate suppresses pedophilic urges and arousability. Archives of sexual behavior, 34(6), 691–705. [CrossRef]
- Briken, P., Berner, W., Noldus, J., Nika, E., & Michl, U. (2000). Therapie mit dem LHRH-Agonisten Leuprorelinacetat bei Paraphilien und sexuell aggressiven Impulshandlungen [Treatment of paraphilia and sexually aggressive impulsive behavior with the LHRH-agonist leuprolide acetate]. Der Nervenarzt, 71(5), 380–385. [CrossRef]
- Hu, Z. Y., Bourreau, E., Jung-Testas, I., Robel, P., & Baulieu, E. E. (1987). Neurosteroids: oligodendrocyte mitochondria convert cholesterol to pregnenolone. Proceedings of the National Academy of Sciences of the United States of America, 84(23), 8215–8219. [CrossRef]
- Jung-Testas, I., Hu, Z. Y., Baulieu, E. E., & Robel, P. (1989). Neurosteroids: biosynthesis of pregnenolone and progesterone in primary cultures of rat glial cells. Endocrinology, 125(4), 2083–2091. [CrossRef]
- Máčová, L., Bičíková, M., Ostatníková, D., Hill, M., & Stárka, L. (2017). Vitamin D, neurosteroids and autism. Physiological research, 66(Suppl 3), S333–S340. [CrossRef]
- Maguire J. (2016). Neurosteroid Deficiency Associated With Epilepsy. Epilepsy currents, 16(2), 108–109. [CrossRef]
- Siracusano, M., Riccioni, A., Abate, R., Benvenuto, A., Curatolo, P., & Mazzone, L. (2020). Vitamin D Deficiency and Autism Spectrum Disorder. Current pharmaceutical design, 26(21), 2460–2474. https://pubmed.ncbi.nlm.nih.gov/32294031/.
- Cannell J. J. (2008). Autism and vitamin D. Medical hypotheses, 70(4), 750–759. [CrossRef]
- Stubbs, G., Henley, K., & Green, J. (2016). Autism: Will vitamin D supplementation during pregnancy and early childhood reduce the recurrence rate of autism in newborn siblings?. Medical hypotheses, 88, 74–78. [CrossRef]
- Kerley, C. P., Elnazir, B., Greally, P., & Coghlan, D. (2020). Blunted serum 25(OH)D response to vitamin D3 supplementation in children with autism. Nutritional neuroscience, 23(7), 537–542. [CrossRef]
- Grant W. B. (2019). Vitamin D and health in the Mediterranean countries. Hormones (Athens, Greece), 18(1), 23–35. [CrossRef]
- Reddy D. S. (2022). Neurosteroid replacement therapy for catamenial epilepsy, postpartum depression and neuroendocrine disorders in women. Journal of neuroendocrinology, 34(2), e13028. https://pubmed.ncbi.nlm.nih.gov/34506047/.
- Carp, T.; Metoudi, M.; Brown, B.; Ojha, V. Low-Dose Interferon I and III-Based Nasal Sprays: A Good-Looking COVID-19 Vaccine Candidate and a Therapy of the Future?. Preprints.org 2022, 2022120155. [CrossRef]
- Carp, T. N. Countering and tackling advanced first-line immune evasion represents the most feasible and precise approach to control and eradicate rabies.
- Calamassi, D., Li Vigni, M. L., Fumagalli, C., Gheri, F., Pomponi, G. P., & Bambi, S. (2022). The Listening to music tuned to 440 Hz versus 432 Hz to reduce anxiety and stress in emergency nurses during the COVID-19 pandemic: a double-blind, randomized controlled pilot study. Acta bio-medica : Atenei Parmensis, 93(S2), e2022149. [CrossRef]
- Calamassi, D., & Pomponi, G. P. (2019). Music Tuned to 440 Hz Versus 432 Hz and the Health Effects: A Double-blind Cross-over Pilot Study. Explore (New York, N.Y.), 15(4), 283–290. [CrossRef]
- Calamassi, D., Lucicesare, A., Pomponi, G. P., & Bambi, S. (2020). Music tuned to 432 Hz versus music tuned to 440 Hz for improving sleep in patients with spinal cord injuries: a double-blind cross-over pilot study. Acta bio-medica : Atenei Parmensis, 91(12-S), e2020008. [CrossRef]
- ALSUntangled Group (2014). ALSUntangled no. 23: the Rife machine and retroviruses. Amyotrophic lateral sclerosis & frontotemporal degeneration, 15(1-2), 157–159. [CrossRef]
- Carter, C. J., & Blizard, R. A. (2016). Autism genes are selectively targeted by environmental pollutants including pesticides, heavy metals, bisphenol A, phthalates and many others in food, cosmetics or household products. Neurochemistry international, S0197-0186(16)30197-8. Advance online publication. [CrossRef]
- Carter C. J. (2016). The barrier, airway particle clearance, placental and detoxification functions of autism susceptibility genes. Neurochemistry international, 99, 42–51. [CrossRef]
- Wong, C. T., Wais, J., & Crawford, D. A. (2015). Prenatal exposure to common environmental factors affects brain lipids and increases risk of developing autism spectrum disorders. The European journal of neuroscience, 42(10), 2742–2760. [CrossRef]
- Dietert, R. R., & Dietert, J. M. (2008). Potential for early-life immune insult including developmental immunotoxicity in autism and autism spectrum disorders: focus on critical windows of immune vulnerability. Journal of toxicology and environmental health. Part B, Critical reviews, 11(8), 660–680. [CrossRef]
- Dietert R. R. (2009). Developmental immunotoxicology: focus on health risks. Chemical research in toxicology, 22(1), 17–23. [CrossRef]
- van De Sande, M. M., van Buul, V. J., & Brouns, F. J. (2014). Autism and nutrition: the role of the gut-brain axis. Nutrition research reviews, 27(2), 199–214. [CrossRef]
- Kawicka, A., & Regulska-Ilow, B. (2013). How nutritional status, diet and dietary supplements can affect autism. A review. Roczniki Panstwowego Zakladu Higieny, 64(1), 1–12.
- Hsiao E. Y. (2014). Gastrointestinal issues in autism spectrum disorder. Harvard review of psychiatry, 22(2), 104–111. [CrossRef]
- Bellato, A., Norman, L., Idrees, I., Ogawa, C. Y., Waitt, A., Zuccolo, P. F., Tye, C., Radua, J., Groom, M. J., & Shephard, E. (2021). A systematic review and meta-analysis of altered electrophysiological markers of performance monitoring in Obsessive-Compulsive Disorder (OCD), Gilles de la Tourette Syndrome (GTS), Attention-Deficit/Hyperactivity disorder (ADHD) and Autism. Neuroscience and biobehavioral reviews, 131, 964–987. [CrossRef]
- Lutein, Brain, and Neurological Functions. (2015). Bioactive Nutraceuticals and Dietary Supplements in Neurological and Brain Disease, 41–47. [CrossRef]
- The Urban Child Institute (2011), Memphis’ Education Funding Misses Best Chance For Impact, https://urbanchildinstitute.org/articles/perceptions/memphis-education-funding-misses-best-chance-for-impact.
- Daniel Garisto (2022), The Universe Is Not Locally Real and the Physics Nobel Prize Winners Proved It, available at: https://www.scientificamerican.com/article/the-universe-is-not-locally-real-and-the-physics-nobel-prize-winners-proved-it/.
- Transcranial Magnetic Stimulation: https://neuromodec.org/what-is-transcranial-magnetic-stimulation-tms/.
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).




