1. Introduction
Symmetry and asymmetry in gait and postural control are fundamental concepts in biomechanics, rehabilitation, and motor recovery. Efficient motor strategies are typically characterized by balanced plantar pressure distribution and stable postural sway, whereas deviations from symmetry may indicate compensatory mechanisms, musculoskeletal dysfunction, or neuromotor impairments [
1,
2,
3].
Objective methods such as baropodometry and stabilometry have become increasingly relevant for quantifying these phenomena. Baropodometric techniques have been applied to assess plantar loading in various clinical populations, including individuals with hemiparesis [
1], multiple sclerosis [
5], and chronic low back pain [
2]. Similarly, stabilometry effectively quantifies center-of-pressure (CoP) oscillations and postural sway, providing reliable indicators of balance control [
14,
17].
In pediatric populations, motor functionality develops rapidly and nonlinearly, making gait and postural assessment particularly challenging. Children display distinctive characteristics such as increased sway, variable gait mechanics, and posterior plantar loading tendencies [
9,
10,
11,
16,
29]. These patterns, although typical for developmental stages, can mask early signs of dysfunction. Moreover, children rely heavily on visual input to maintain balance, resulting in decreased postural stability under visual deprivation due to immature proprioceptive and vestibular systems [
7,
25]. Persistent asymmetries may become habitual, leading to inefficient motor patterns or long-term imbalances [
11,
12].
Baropodometric and stabilometric analyses are noninvasive, quantitative tools used to evaluate gait and postural symmetry. Baropodometry assesses plantar load and propulsion dynamics during static and dynamic tasks [
1,
9,
10], while stabilometry measures CoP displacement and sway under varying sensory conditions, using parameters such as sway path, area, and Romberg index [
14,
17]. These methods are valuable for identifying visual dependence and monitoring rehabilitation progress in children [
7,
25,
29]. Despite numerous studies exploring gait and postural asymmetries in clinical and healthy populations [
8,
9,
10,
11,
12,
13,
16,
25,
26], few have combined both approaches in pediatric subjects. The lack of normative baseline data limits differentiation between developmental variability and early pathology, including idiopathic toe walking, developmental coordination disorder, and neuromuscular conditions [
27,
28,
29].
To address this gap, the present single-case pilot study investigated the feasibility and sensitivity of combined baropodometric and stabilometric assessments in a healthy child. The study aimed to determine whether subtle asymmetries could be objectively quantified. We hypothesized that (HW1) baropodometry would reveal mild asymmetries in plantar loading, (HW2) stabilometry would confirm visual dependence under deprivation, and (HW3) the integration of both methods would demonstrate feasibility for early screening and preventive assessment in pediatric populations.
2. Materials and Methods
To explore these working hypotheses (HW1–HW3), this pilot study employed a baropodometric platform and stabilometric system to quantify plantar pressure distribution and postural sway in healthy pediatric subjects. The experimental design was structured to capture both static and dynamic load patterns, as well as balance control under visual and non-visual conditions.
Given the single-subject nature of this pilot study, no statistical significance testing (e.g., p-values or confidence intervals) was performed. The primary aim was to assess the feasibility and sensitivity of the combined baropodometric and stabilometric methods in detecting functional asymmetries rather than to conduct inferential group-level analyses.
2.1. Participants
This pilot study involved a single healthy pediatric participant (8 years old, male, no history of neurological or musculoskeletal disorders), who underwent preventive assessments using noninvasive baropodometric and stabilometric tools. The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Institutional Ethics Committee of Bucharest University of Economic Studies under approval number 4014/02.12.2025. The procedures posed no physical or psychological risks to the subject. Written informed consent was obtained from the child’s legal guardian prior to data collection.
Although the participant was clinically healthy and exhibited typical motor development, his selection was based on preliminary visual observations during the preventive evaluation. Subtle asymmetries in stance and gait, such as rearfoot load dominance and left-right imbalance, were noted by a trained pediatric physical therapist. These features, although subclinical, can become ingrained during motor development, potentially predisposing the child to compensatory postural strategies or inefficiencies if left unmonitored. Therefore, the present exploratory single-case pilot study design aimed to assess the feasibility and sensitivity of baropodometric and stabilometric tools for the early detection of functional asymmetries in a non-pathological pediatric profile.
2.2. Measurement Instruments
Evaluation was performed using a baropodometric platform (FreeMed®, Sensor Medica, Guidonia, Italy) and a computerized stabilometric system (FreeMed® Stabilometry Module, Sensor Medica, Italy), capable of recording plantar pressure distribution and center of pressure (CoP) oscillations in real time.
Both systems are designed for medical-grade neuromotor assessment and provide high-resolution spatial–temporal data, including dynamic gait phases, CoP trajectories, and load distribution. The platforms were equipped with pressure sensors with sampling frequencies exceeding 400 Hz, and the stabilometric system incorporated 2D CoP tracking under different sensory conditions. Real-time data acquisition is supported by FreeStep Pro software, which ensures standardized trial procedures and reproducible outputs.
These systems are CE marked and have been previously validated for pediatric use in patients with neurological or orthopedic conditions. Their combined use in a healthy subject allowed us to evaluate the baseline symmetry profiles under controlled conditions. Given the technical complexity and data density of each test (static and dynamic), starting with a single-participant pilot allowed us to assess the feasibility, compliance, and sensitivity of the tools across the three task conditions. These elements are critical for optimizing future protocol scalability.
According to the manufacturer’s specifications, these programs apply embedded Butterworth-type low-pass filtering to reduce high-frequency noise, exclude physiologically implausible values, and automatically smooth the center of pressure (CoP) trajectories. Artifact rejection is performed in real time based on the internal thresholds defined by the system. While these procedures ensure standardized processing, precise filtering parameters (e.g., cut-off frequencies and filter order) are not publicly disclosed by the vendor. Importantly, the same proprietary pipeline was applied uniformly across all conditions, ensuring the internal consistency of the results. However, this limitation highlights the need for a more transparent approach. In future studies, we plan to adopt open-source or custom MATLAB/Python-based signal-processing pipelines to allow full control over the preprocessing steps, improve reproducibility, and enhance cross-study comparability, particularly for CoP-related variables.
Baropodometric analysis included:
Static test: assessment of plantar load distribution between the left and right foot, and between the forefoot and rearfoot.
Dynamic test: Analysis of successive footprints during gait, including stance and propulsion phases.
Stabilometric analysis included:
Romberg test (eyes open and closed) was used to evaluate postural control and visual dependence.
Computation of the sway ellipse area and CoP trajectory (path length and area) as indicators of balance stability.
2.3. Experimental Protocol
The participant performed all trials barefoot, with the arms relaxed alongside the body:
Static analysis: upright stance for 30 s while focusing on a fixed visual target at the eye level. (
Figure 1,
Figure 2 and
Figure 3)
Dynamic analysis: walking across the platform at a self-selected pace, repeated three times; mean values were used. (
Figure 4,
Figure 5 and
Figure 6)
Stabilometric analysis (Romberg test): bipodal stance for 30 s with eyes open, followed by 30 s with eyes closed. (
Figure 7,
Figure 8 and Figure 9)
All trials were automatically recorded and processed using proprietary software.
2.4. Parameters Analyzed
Plantar load distribution: % load on the left vs. right foot; % load on the forefoot vs. rearfoot.
Dynamic gait parameters: step length (cm), contact time (ms), and peak propulsion pressure (kPa).
Stabilometric parameters:
CoP sway area (mm²) and path length (mm)
Anteroposterior and mediolateral oscillations (mm)
Romberg index (ratio of eyes closed to eyes open).
Table 1.
Parameters analyzed in baropodometric and stabilometric assessments.
Table 1.
Parameters analyzed in baropodometric and stabilometric assessments.
| Category |
Parameter |
Unit |
Description |
| Static plantar pressure |
Left vs. right load distribution |
% |
Relative distribution of plantar load between left and right foot |
| Static plantar pressure |
Forefoot vs. rearfoot load distribution |
% |
Relative distribution of plantar load between forefoot and rearfoot |
| Dynamic gait |
Step length |
cm |
Distance between two successive steps |
| Dynamic gait |
Contact time |
ms |
Duration of foot–ground contact |
| Dynamic gait |
Peak propulsion pressure |
kPa |
Maximum plantar pressure generated during propulsion |
| Stabilometry |
CoP sway area |
mm² |
Area covered by center of pressure oscillations |
| Stabilometry |
CoP path length |
mm |
Total length of the CoP trajectory during test |
| Stabilometry |
Romberg index |
ratio (eyes closed/open) |
Ratio of postural stability with eyes closed vs. eyes open |
These tests and parameters were selected because they are widely validated as reliable indicators of gait and postural symmetry in pediatric and clinical populations [
1,
5,
7,
14,
25].
3. Results
Given the single-subject nature of this pilot study, no statistical significance testing (e.g., p-values or confidence intervals) was performed. The primary aim was to assess the feasibility and sensitivity of the combined baropodometric and stabilometric methods in detecting functional asymmetries rather than to conduct inferential group-level analyses.
As this study involved only a single pediatric participant, the results are presented descriptively. Statistical outputs, such as p-values, were not applicable. These findings illustrate the potential of the proposed methods for detecting subtle asymmetries in individual assessments.
The results are presented in relation to the working hypotheses formulated in the introduction.
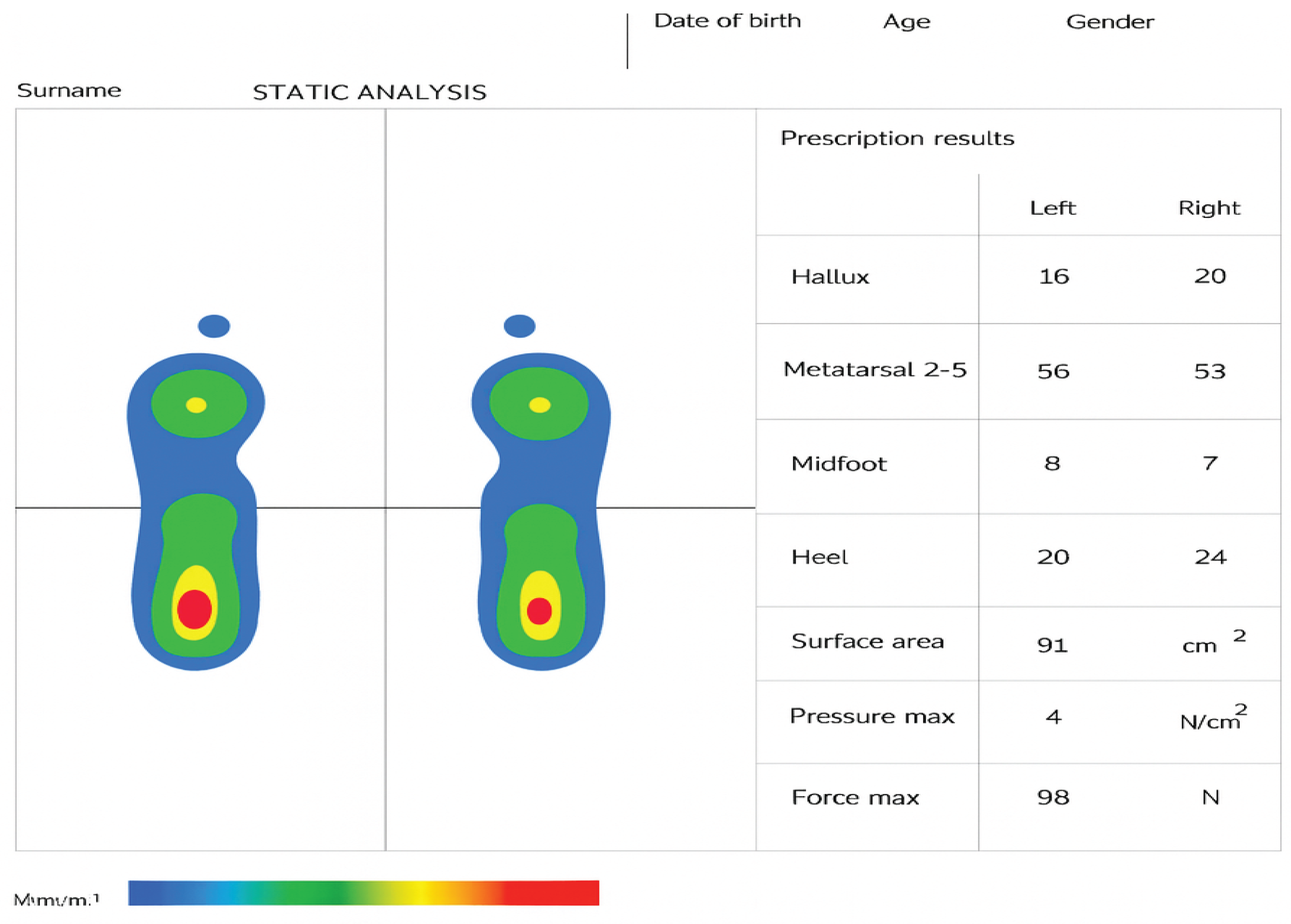
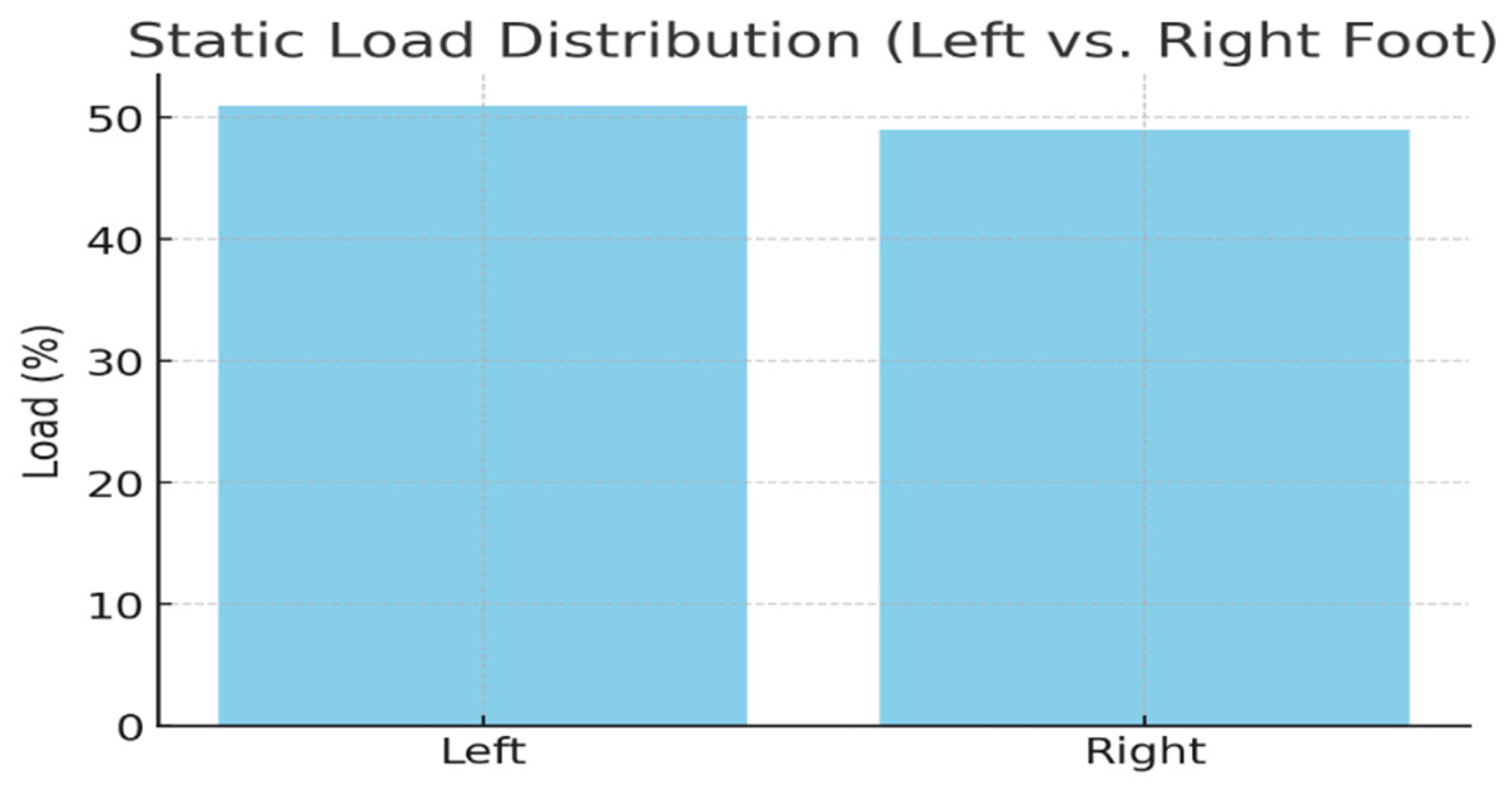
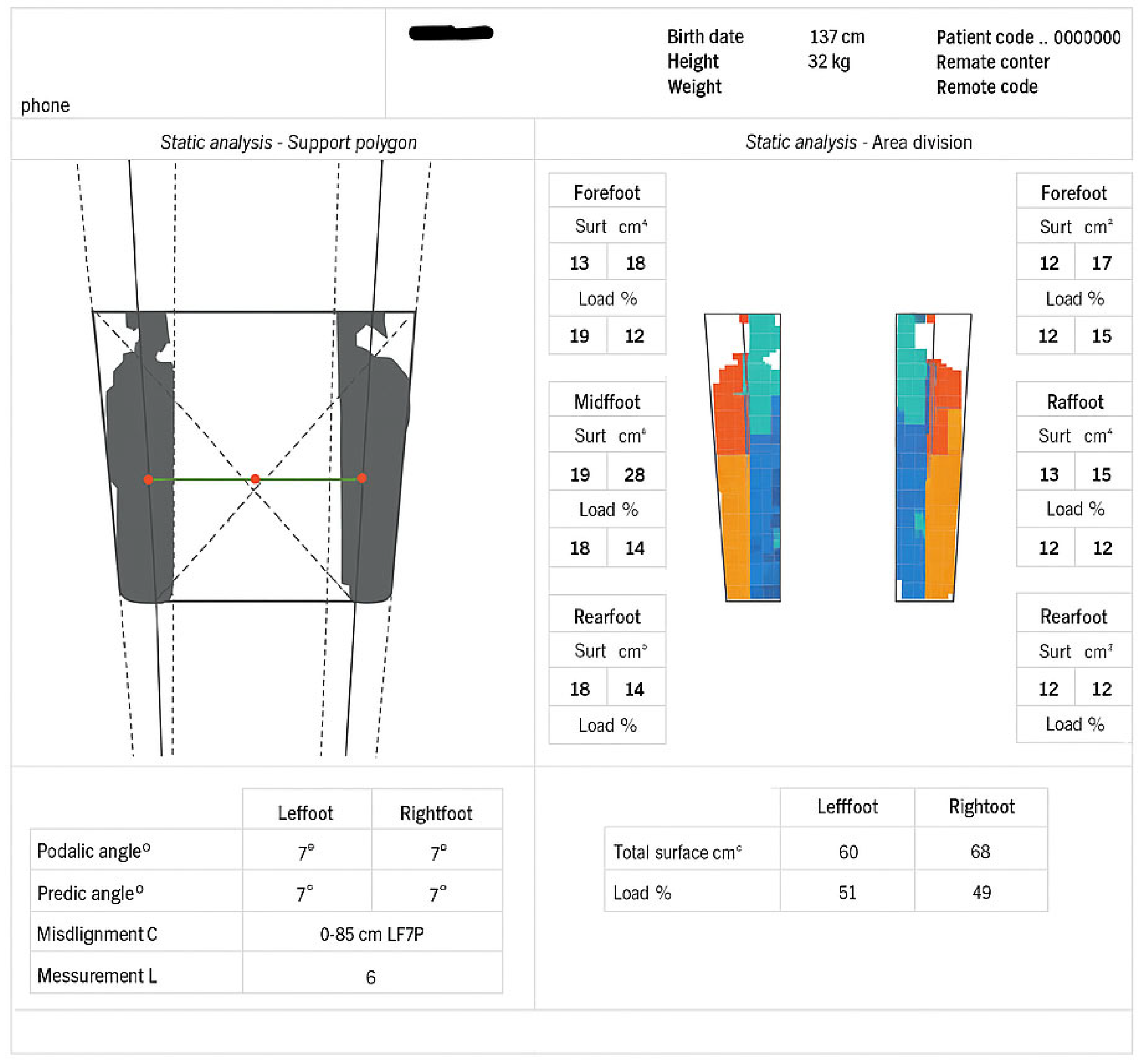
HW1 (Baropodometric analysis): Static plantar pressure distribution indicated a slight left–right asymmetry, with a predominance of left-foot loading (51%) compared to the right (49%), and a posterior tendency with greater rearfoot support (62%). Dynamic analysis confirmed this pattern, with the left side contributing to a longer stance duration, while the right side generated higher propulsion forces. These findings support HW1 by demonstrating detectable asymmetries, even in a healthy subject.
HW2 (Stabilometric analysis): Stabilometric testing revealed increased postural sway under visual deprivation, with a larger sway ellipse area and a Romberg index exceeding 2.0. These results are consistent with those of HW2, indicating that children exhibit a strong reliance on vision to maintain balance.
HW3 (Combined feasibility): Together, the baropodometric and stabilometric results demonstrate the feasibility of integrating these complementary methods for symmetry and asymmetry assessment in pediatric populations, supporting HW3.
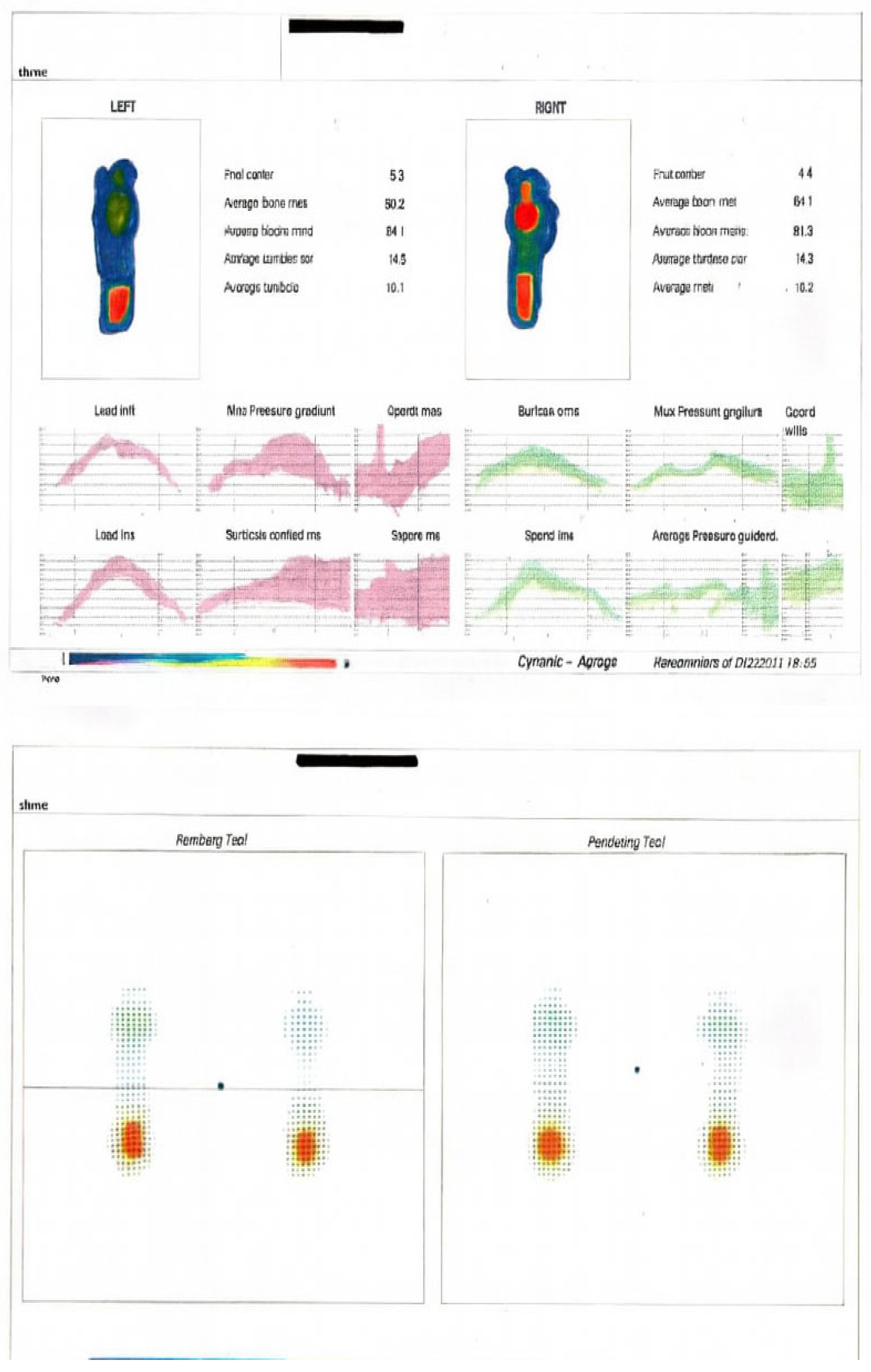
3.1. Static Baropodometric Analysis
The static baropodometric assessment revealed an overall balanced distribution of plantar loads, with a slight predominance in the left foot (51%) compared to the right foot (49%). Analysis of the anterior–posterior distribution showed that the rearfoot supported the majority of the load (62%), while the forefoot accounted for 38%.
Although the total acquisition time for each static condition was 30 s, only the central 20 s were used for analysis to exclude transient postural adjustments at the start and anticipatory behaviors near the end of the trial. This segmentation approach has been recommended in pediatric stabilometry to improve the reliability of sway-related parameters [
25,
27].
These findings indicate a mild asymmetry characterized by a posterior loading tendency, which may reflect the developmental features of pediatric posture. The detailed values are presented in
Table 1, and the distribution of plantar loads between the left and right feet is graphically represented in
Figure 1,
Figure 2 and
Figure 3.
Table 1.
Static baropodometric data. Distribution of plantar load between left and right foot, and between forefoot and rearfoot.
Table 1.
Static baropodometric data. Distribution of plantar load between left and right foot, and between forefoot and rearfoot.
| Foot |
Load (%) |
Forefoot (%) |
Rearfoot (%) |
| Left |
51 |
37 |
63 |
| Right |
49 |
39 |
61 |
Figure 1.
Static analysis.
Figure 1.
Static analysis.
Figure 2.
Static load distribution. Percentage of plantar load between the left and right foot, as measured in the static baropodometric test.
Figure 2.
Static load distribution. Percentage of plantar load between the left and right foot, as measured in the static baropodometric test.
Figure 3.
Static analysis support polygon.
Figure 3.
Static analysis support polygon.
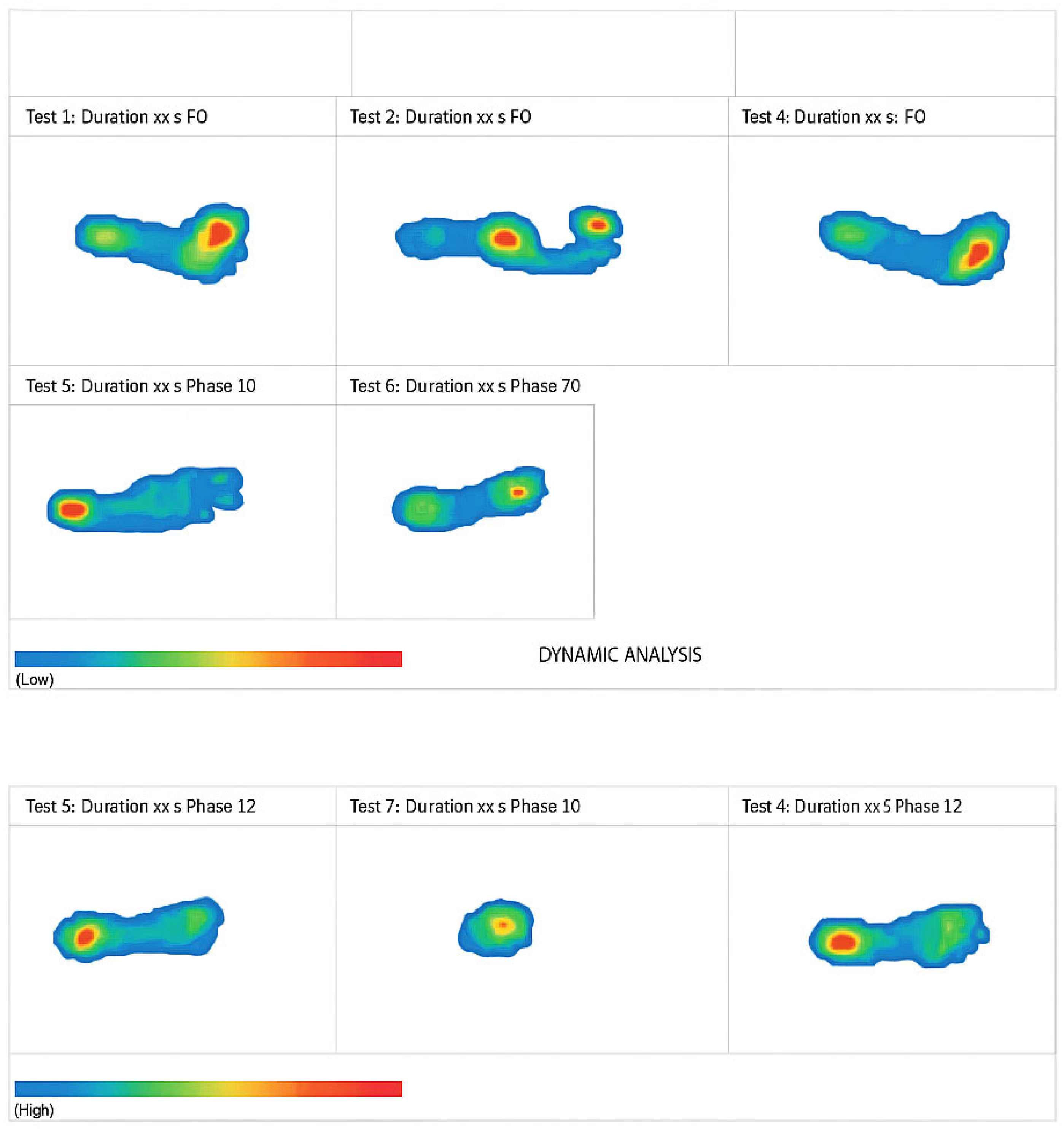
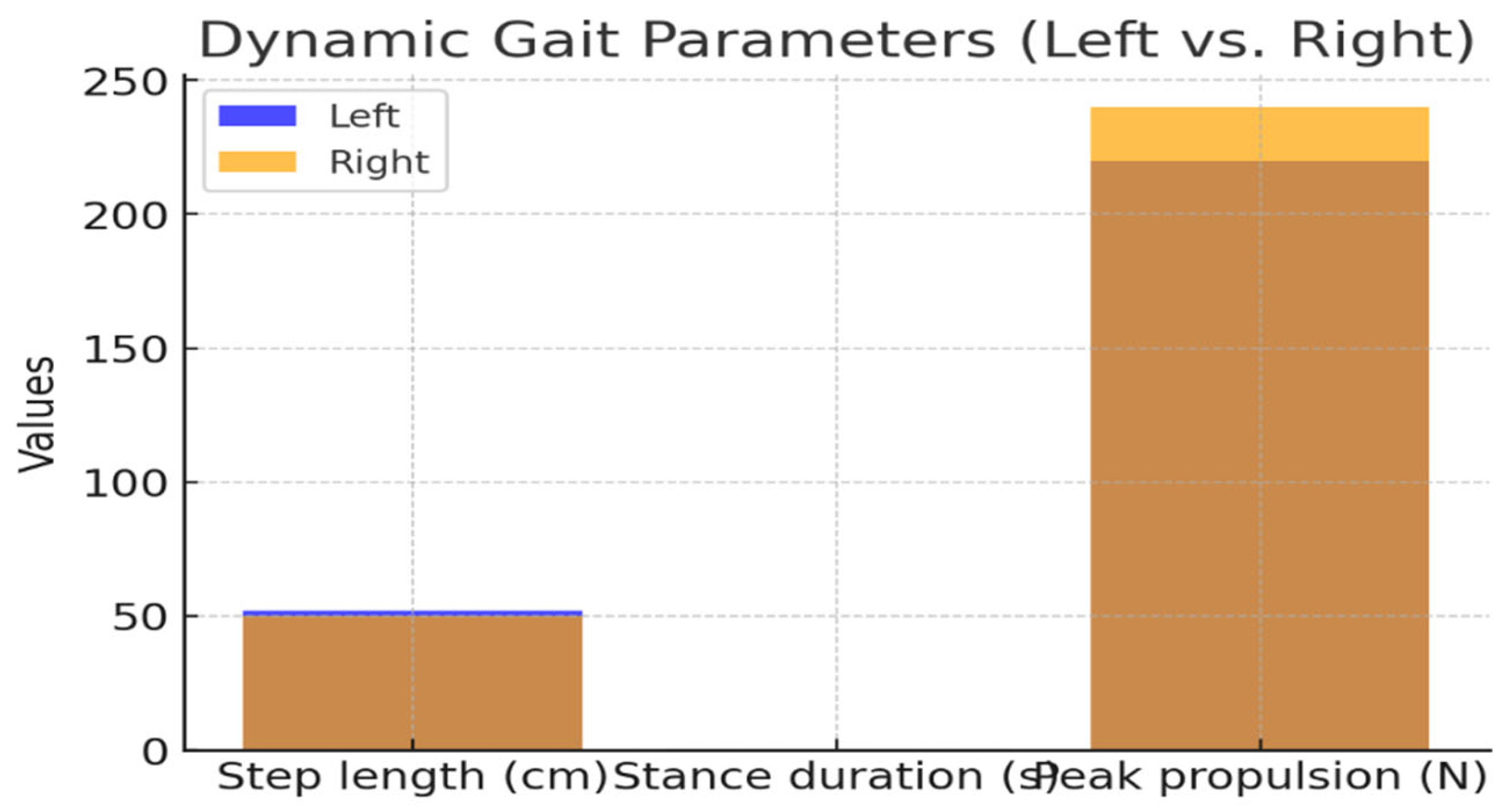
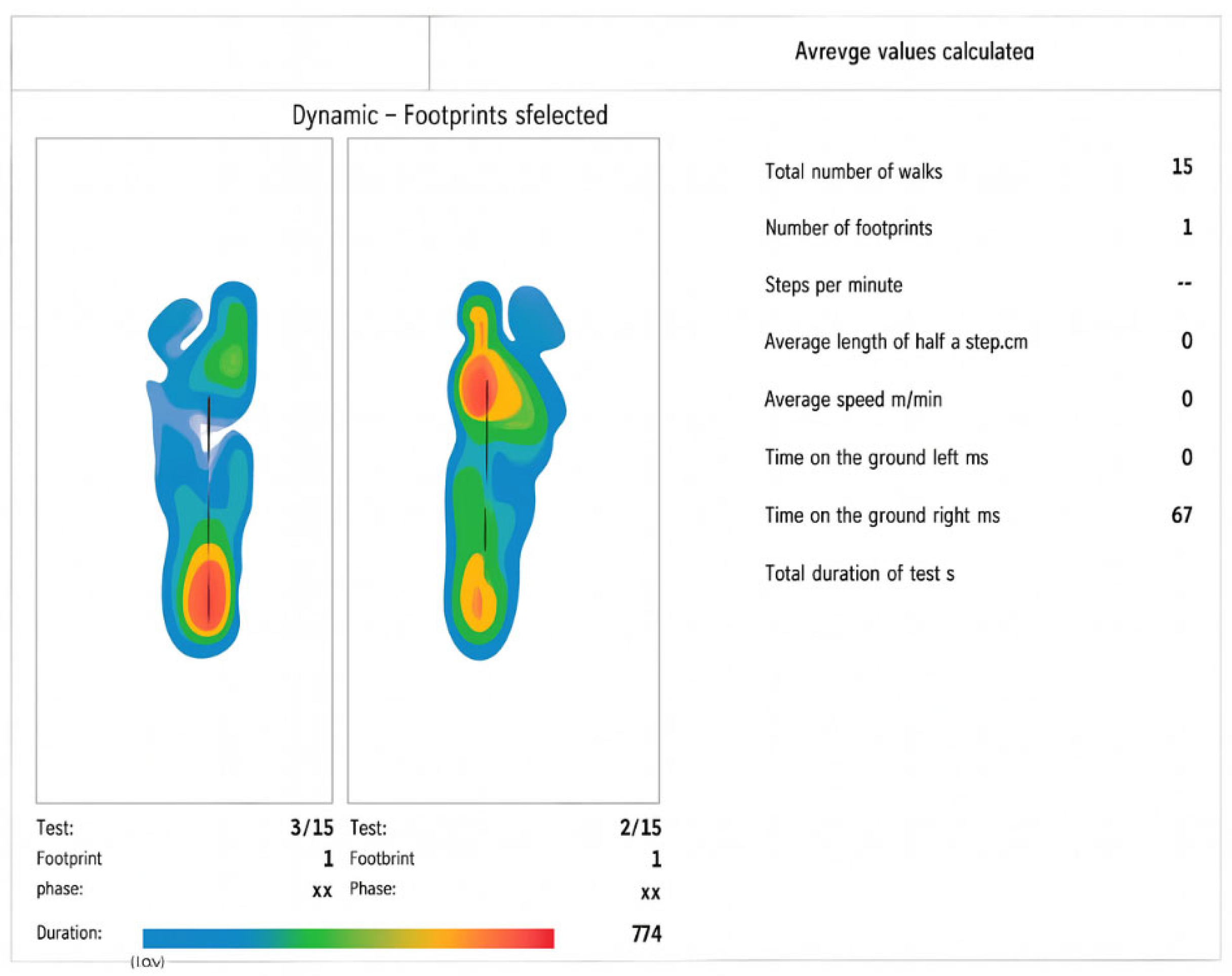
3.2. Dynamic Baropodometric Analysis
During the dynamic assessment of gait, successive footprints demonstrated consistent sequencing; however, subtle asymmetries were observed between the two limbs. The left foot exhibited a slightly longer step length (52 cm vs. 50 cm) and a longer stance duration (0.72 s vs. 0.68 s), suggesting its role in contributing to overall stability. In contrast, the right foot generated higher peak propulsion forces (240 N vs. 220 N), reflecting a greater contribution to the forward progression. These complementary asymmetries illustrate a functional differentiation between stability and propulsion during gait, which has been described as a characteristic of pediatric motor development. The specific values are summarized in
Table 2, and the comparison of step length, stance duration, and propulsion forces between the left and right sides is illustrated in
Figure 4,
Figure 5 and
Figure 6.
Table 2.
Dynamic gait data. Comparison of step length, stance duration, and propulsion force between the left and right foot.
Table 2.
Dynamic gait data. Comparison of step length, stance duration, and propulsion force between the left and right foot.
| Parameter |
Left Foot |
Right Foot |
| Step length (cm) |
52 |
50 |
| Stance duration (s) |
0.72 |
0.68 |
| Peak propulsion (N) |
220 |
240 |
Figure 4.
Dynamic_analysis
Figure 4.
Dynamic_analysis
Figure 5.
Dynamic gait parameters. Comparison of step length, stance duration, and peak propulsion force between the left and right foot.
Figure 5.
Dynamic gait parameters. Comparison of step length, stance duration, and peak propulsion force between the left and right foot.
Figure 6.
Dynamic foot print analyses
Figure 6.
Dynamic foot print analyses
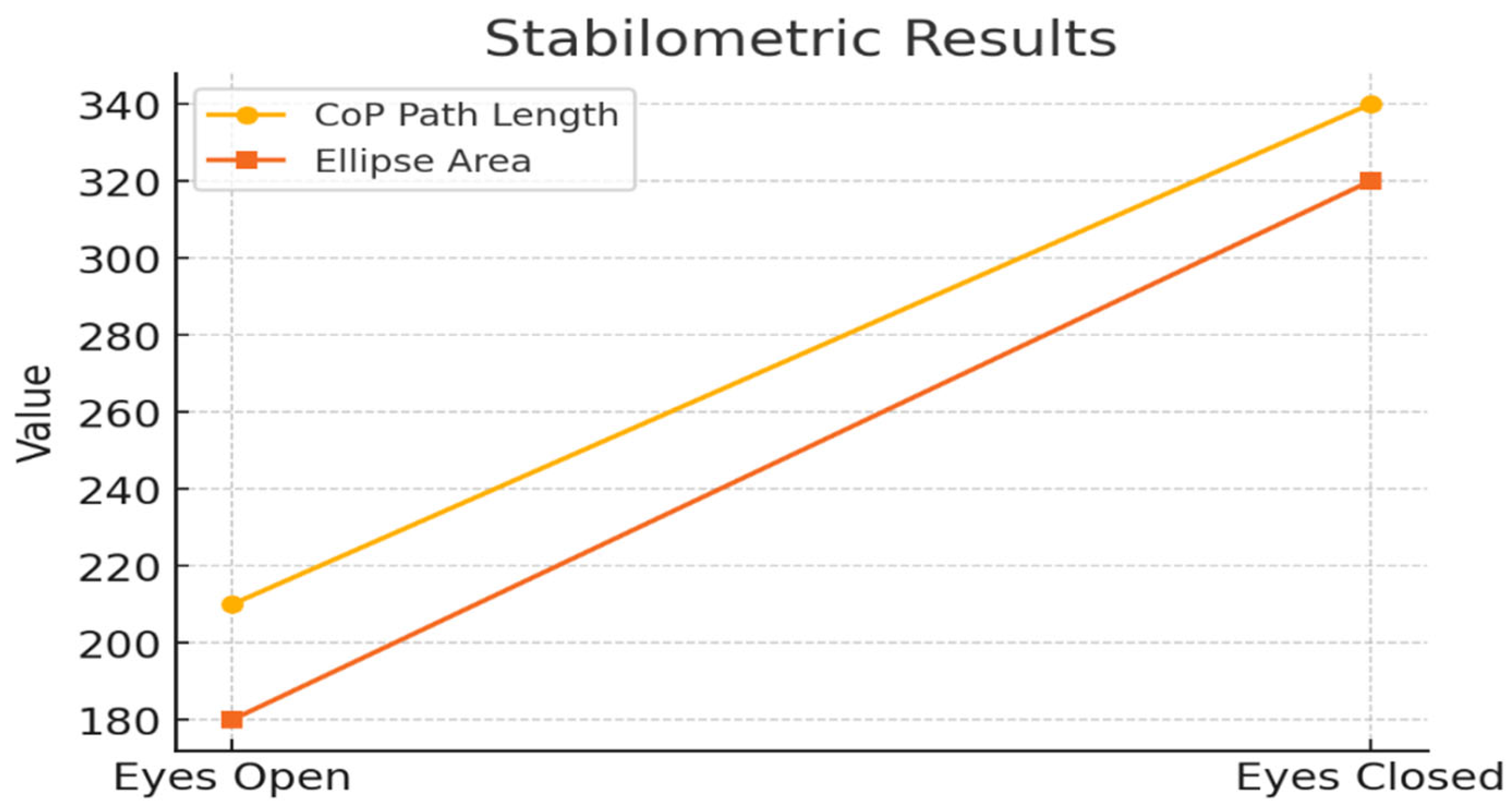
3.3. Stabilometric Analysis
The stabilometric evaluation highlighted an increase in postural sway when the visual input was removed. With eyes open, the center of pressure (CoP) path length was 210 mm, and the sway ellipse area was 180 mm², values that remained within the expected range for a stable stance, although mediolateral oscillations were evident. With eyes closed, both parameters increased markedly (340 mm for path length and 320 mm² for ellipse area), indicating reduced postural stability in the absence of visual guidance. The Romberg index exceeded 2.0, confirming a strong reliance on visual input for balance control, which is consistent with the pediatric postural strategies described in the literature. The corresponding stabilometric values are reported in
Table 3, and the differences between the eyes-open and eyes-closed conditions are depicted in
Figure 7 and
Figure 8.
Table 3.
Stabilometric data. Center of pressure (CoP) trajectory, ellipse area, and Romberg index under eyes-open and eyes-closed conditions.
Table 3.
Stabilometric data. Center of pressure (CoP) trajectory, ellipse area, and Romberg index under eyes-open and eyes-closed conditions.
| Condition |
CoP Path Length (mm) |
Ellipse Area (mm²) |
Romberg Index |
| Eyes Open |
210 |
180 |
1.0 |
| Eyes Closed |
340 |
320 |
2.1 |
Figure 7.
Biopodalic_analysis
Figure 7.
Biopodalic_analysis
Figure 8.
Stabilometric results. Center of pressure (CoP) trajectory length and sway ellipse area under eyes-open and eyes-closed conditions.
Figure 8.
Stabilometric results. Center of pressure (CoP) trajectory length and sway ellipse area under eyes-open and eyes-closed conditions.
In summary, the static analysis revealed a mild left–right asymmetry in plantar loading, with the left foot supporting 51% of body weight compared to 49% on the right, and a predominance of rearfoot loading (62%) relative to the forefoot (38%) (
Table 1,
Figure 1,
Figure 2 and
Figure 3). This posterior loading strategy is commonly described in children, as the maturation of gait is associated with the progressive redistribution of plantar pressures toward a more balanced forefoot–rearfoot pattern. Previous pediatric studies have shown that younger children exhibit greater variability and asymmetry in static support, which tends to decrease with age as motor control improves.
Dynamic assessment further highlighted subtle gait asymmetries (
Table 2 and
Figure 4,
Figure 5 and
Figure 6). The left foot demonstrated a slightly longer step length (52 cm vs. 50 cm) and stance duration (0.72 s vs. 0.68 s), suggesting a stabilizing role, whereas the right foot exhibited higher peak propulsion forces (240 N vs. 220 N), reflecting a greater contribution to forward progression. Such side-specific differences are consistent with developmental gait patterns, where one limb often provides stability, while the contralateral limb contributes more to propulsion. Pediatric gait literature describes these asymmetries as part of a transitional process toward a mature, more symmetrical gait pattern typically reached in late childhood.
Stabilometric evaluation confirmed increased postural sway under visual deprivation (
Table 3,
Figure 7 and
Figure 8). With eyes open, the CoP path length was 210 mm and the sway ellipse area was 180 mm²; with eyes closed, these values increased to 340 mm and 320 mm², respectively. The Romberg index exceeded 2.0, indicating a strong dependence on visual input for balance control. This finding is in line with prior research showing that children rely more heavily on visual cues for maintaining postural stability, as proprioceptive and vestibular integration remains less efficient than in adults. Pediatric stabilometric studies have consistently reported larger sway amplitudes and higher Romberg indices, suggesting that balance control mechanisms are still maturing throughout early and middle childhood.
Taken together, these results demonstrate that even in healthy pediatric subjects, objective baropodometric and stabilometric analyses can identify functional asymmetries and developmental characteristics of gait and posture. The combination of mild plantar asymmetry, complementary gait dynamics, and visual dependence for balance illustrates typical variability in pediatric motor control. Supported by both numerical data (
Table 1,
Table 2 and
Table 3) and graphical representations (
Figure 1,
Figure 2,
Figure 3,
Figure 4,
Figure 5,
Figure 6,
Figure 7 and
Figure 8), these findings emphasize the feasibility of detecting relevant asymmetries in pediatric populations and highlight the potential role of these tools in rehabilitation and developmental monitoring.
4. Discussion
This pilot study examined gait and postural symmetry in a healthy pediatric subject, guided by three working hypotheses (HW1–HW3). The discussion is therefore organized around these hypotheses, emphasizing the consistency of the findings with the existing literature and their relevance for pediatric assessment and rehabilitation. The results demonstrated subtle but measurable asymmetries in plantar pressure distribution, gait parameters, and postural control.
While the present findings highlight the presence of detectable functional asymmetries in a clinically healthy pediatric subject, they should not be interpreted as conclusive evidence regarding the normative nature of such asymmetries. Rather, these observations may reflect normal developmental variability; however, larger, age-stratified studies are necessary to validate this hypothesis and distinguish adaptive features from early signs of dysfunction.
4.1. HW1 – Baropodometric Analysis and Plantar Load Asymmetries
Static analysis revealed a slight predominance of left-foot loading and posterior distribution of plantar pressure. This pattern is consistent with the findings of Monteiro-Rodrigues et al. [
6], who reported rearfoot dominance in adults, and with pediatric studies demonstrating posterior support strategies during growth [
9,
10]. Dynamic analysis further emphasized the complementary roles of the limbs: the left foot primarily contributed to stability, whereas the right foot generated greater propulsion forces. Similar asymmetric contributions have been described in both healthy children [
12,
16] and pathological contexts, such as idiopathic toe walking [
27]. These results support HW1 by showing that baropodometry can detect subtle but measurable asymmetries, even in children without clinical pathology. While such asymmetries may represent adaptive mechanisms facilitating motor development, their persistence could predispose to musculoskeletal imbalance, underscoring the preventive value of baropodometric assessments in pediatric populations.
4.2. HW2 – Stabilometric Analysis and Visual Dependence in Postural Control
Stabilometry allows for the detection of postural instability and sensory integration inefficiencies, even in children who are otherwise considered healthy. The Romberg index >2.0 observed in our participant reflects a strong reliance on visual input for balance—a common feature in pediatric postural control strategies due to the immaturity of proprioceptive and vestibular systems [
29]. These findings are consistent with the hypothesis that postural control in children relies heavily on visual input, as evidenced by increased sway and Romberg index under visual deprivation, and aligns with previous studies that highlight exaggerated sway responses in children under visual deprivation, confirming the sensitivity of stabilometric parameters such as sway area and path length [
7,
25]. Therefore, stabilometry not only quantifies balance performance but also reveals how children utilize sensory input for postural control, making it a valuable tool for early screening and developmental profiling.
Stabilometry allows for the detection of postural instability and sensory integration inefficiencies, even in children who are otherwise considered healthy. In our study, the Romberg index exceeded 2.0, indicating a strong visual dependence for maintaining balance. This is a well-documented characteristic in pediatric populations, as proprioceptive and vestibular systems are still maturing and are often less efficient than visual input during early development [
7,
25,
29].
Parameters such as sway area, path length, and CoP displacement provide quantifiable insights into how children manage upright stance under different sensory conditions. In this case, increased sway in the absence of visual input confirmed the expected reliance on vision and demonstrated the tool's sensitivity in capturing sensorimotor strategies. As such, stabilometry not only measures balance ability but also characterizes the sensory strategies employed, making it an important tool for developmental screening and early identification of postural control inefficiencies.
Stabilometric assessment revealed strong reliance on visual input, with enlarged sway areas and a Romberg index greater than 2.0 under eyes-closed conditions. These results confirm HW2 and are in line with previous studies showing that children rely more heavily on vision to maintain balance than adults [
25,
29]. Shibata and Yoshida [
7] similarly reported that targeted rehabilitation could reduce postural instability under visual deprivation, supporting the importance of sensory training in balance development. Further evidence from VR-based postural control interventions [
28] and EMG-based gait analyses [
12] highlights the role of multimodal sensory integration in pediatric motor control. Moreover, exaggerated visual dependence has been observed in children with developmental coordination disorders or neuromuscular impairments [
27,
28], suggesting that stabilometry is a valuable diagnostic and monitoring tool in both healthy and clinical populations.
4.3. HW3 – Combined Feasibility of Baropodometric and Stabilometric Assessment
The integration of baropodometric and stabilometric findings provides strong support for HW3, demonstrating the feasibility of these complementary methods in pediatric evaluation. Baropodometry offers detailed information on plantar load distribution, gait phases, and propulsion, whereas stabilometry captures postural sway and sensory reliance. Together, they provide a holistic picture of motor function and symmetry, aligning with prior work that has emphasized the need for multimodal assessment in rehabilitation and sports science [
2,
6,
18]. In the pediatric context, this combined approach has significant potential for early screening, preventive interventions, and individualized rehabilitation strategies, particularly for children with orthopedic or neuromotor vulnerabilities. By highlighting both functional asymmetries and sensory integration patterns, this methodology contributes to a more comprehensive understanding of motor development and its clinical application.
4.4. Clinical Implications
Although this study included only a single, healthy pediatric subject, the findings were clinically meaningful. Detecting asymmetries in such cases is critical because early compensatory mechanisms—if unnoticed—may become habitual and lead to long-term deviations. The observed patterns in this case underscore the utility of integrating objective motor assessments into routine pediatric evaluations to identify at-risk profiles even in the absence of pathology [
8,
28,
16].
Beyond diagnostic screening, stabilometry has shown utility in clinical monitoring, including post-intervention assessments. In populations with neuromotor vulnerabilities, such as children with hereditary neuropathies or developmental coordination disorders, stabilometric analysis has been used to track improvements following rehabilitation protocols such as proprioceptive training or visual-motor exercises [
2,
27,
28]. Moreover, its application extends to healthy children as a preventive measure, helping clinicians and therapists detect patterns that may predict future postural or motor inefficiencies. Its non-invasive format and ease of use also support its integration into school-based health assessments and sports programs.
Stabilometry is not only valuable for diagnostic screening but also for tracking therapeutic outcomes in pediatric populations. Previous studies have shown that children with hereditary sensory neuropathies, idiopathic toe walking, or developmental coordination disorders demonstrate distinct postural sway patterns and elevated Romberg indices, which improve following targeted rehabilitation programs [
2,
27,
28]. The noninvasive and user-friendly nature of stabilometric platforms makes them especially suitable for use in young children and across various clinical and educational environments.
Moreover, their integration into routine pediatric evaluations or school-based screenings could offer meaningful insights into motor development trajectories. Even in healthy children, early identification of excessive sway or atypical sensory reliance may inform preventive strategies and support individualized interventions that promote long-term neuromotor efficiency.
Baropodometry and stabilometry have been validated in hemiparetic [
1], MS [
5], and scoliosis populations [
3]. Extending their application to pediatric practice may help detect early asymmetries and monitor rehabilitation effects. Foot type differences [
9], prosthesis use [
8], and pathological gait conditions [
27,
28] all demonstrate the value of plantar pressure analysis in guiding interventions.
Additionally, reliability studies have confirmed that baropodometric measures are valid for children aged 4–12 years [
26], supporting the feasibility of their integration in pediatric care.
4.5. Gait and Postural Symmetry Assessment in Pediatric Prevention and Rehabilitation
The assessment of gait and postural symmetry is not only of scientific relevance but also of clinical and preventive importance. In children, asymmetries may initially appear as functional adaptations during growth; however, if not identified early, they can predispose children to postural deviations, musculoskeletal imbalances, or inefficient motor patterns [
9,
10,
29]. Baropodometric and stabilometric analyses, by providing objective and quantifiable data, enable clinicians to detect such deviations at a subclinical stage before they evolve into overt pathology.
From a
preventive perspective, integrating these methods into routine pediatric evaluations may support the identification of children at risk of developing postural or gait abnormalities, such as flatfoot, idiopathic toe walking, or balance deficits associated with poor sensory integration [
11,
16,
27]. Early detection can guide targeted interventions, including proprioceptive training, corrective exercise, and adapted motor activity programs in schools or community health initiatives [
2,
25,
28].
From a
rehabilitation perspective, these tools have the advantage of objectively monitoring treatment progress. They can quantify changes in plantar load redistribution, improvements in balance control, and reductions in asymmetry following interventions such as manual therapy, perceptive rehabilitation, or VR-based balance training [
5,
7,
13,
28]. For pediatric populations recovering from orthopedic injuries or neuromotor disorders, baropodometric and stabilometric assessments offer outcome measures and motivational feedback to both families and therapists.
Ultimately, combining prevention and rehabilitation approaches based on gait and postural symmetry analyses may contribute to promoting healthier motor development trajectories, reducing long-term risks, and enhancing children’s quality of life.
4.6. Future Research Directions
This single-case feasibility study provides a methodological foundation for future research on pediatric gait and postural symmetry. Given the limited sample size, subsequent studies should recruit larger age-stratified pediatric cohorts through collaborations with schools and sports centers to establish normative datasets for plantar pressure and stabilometric indices. These reference values are crucial for distinguishing typical developmental variability from early indicators of dysfunction.
Longitudinal research is needed to examine how gait and postural asymmetries evolve throughout childhood and to determine whether specific patterns, such as posterior load predominance or left–right imbalance, predict future musculoskeletal or neuromotor issues. Comparative studies between healthy children and those with orthopedic or neurological conditions (e.g., idiopathic toe walking and developmental coordination disorder) could clarify whether such asymmetries are adaptive or maladaptive.
Future work should also incorporate additional parameters, including intra-subject variability and the influence of physiological factors, such as respiration, to improve the precision of stabilometric assessments. The adoption of open-source data processing and advanced technologies, such as wearable sensors, machine learning algorithms, and real-time biofeedback, may enhance reproducibility and allow continuous monitoring in both clinical and preventive settings.
These findings reinforce the idea that functional asymmetries are integral to motor development. Distinguishing developmental variability from maladaptive asymmetry is essential for timely rehabilitation. By extending the scope of symmetry to pediatric populations, this study emphasizes the importance of early screening and objective monitoring of gait and postural symmetry.
Ultimately, interdisciplinary collaboration among clinicians, biomechanists, engineers, and educators is essential to expand this proof-of-concept into larger frameworks for pediatric rehabilitation and motor development research.
5. Conclusions
This single-case brief report demonstrated that combined baropodometric and stabilometric assessment effectively detects subtle functional asymmetries in gait and postural control in healthy pediatric subjects. The integration of these tools highlights their feasibility for early screening and preventive monitoring in rehabilitation and sports. Mild asymmetries in plantar load, dynamic gait parameters, and visual dependence for balance represent normal developmental variability but may serve as early indicators of neuromotor inefficiency if persistent.
By linking plantar pressure and postural stability with potential compensatory mechanisms affecting knee alignment, this approach contributes to the ongoing advances in gait symmetry and knee kinematic research. These findings provide a methodological foundation for future large-scale pediatric studies and reinforce the importance of objective symmetry-based assessment tools in developmental and rehabilitative practice.
Author Contributions
Conceptualization, methodology, validation, formal analysis, investigation, data curation, writing—original draft preparation, writing—review and editing, visualization, supervision: Teodora Dominteanu, Amelia Elena Stan and Andreea Voinea. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article. Written informed consent was obtained from the participant’s legal guardian for participation and for the publication of anonymized data. Ethical review and approval were waived for this study in accordance with national legislation, as it involved a single healthy participant evaluated during routine clinical practice. The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Institutional Ethics Committee of Bucharest University of Economic Studies under approval number 4014/02.12.2025. The procedures posed no physical or psychological risks to the subject. Written informed consent was obtained from the child’s legal guardian prior to data collection.
Acknowledgments
During the preparation of this manuscript, the authors used ChatGPT (OpenAI, San Francisco, CA, USA) and Paperpal (Cactus Communications, Mumbai, India) for English translation, grammar improvement, and proofreading support. The authors have carefully reviewed and edited the output, and take full responsibility for the content of this publication.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
References
- De Menezes, L.T.; Barbosa, P.H.F.A.; Costa, A.S.; Mundim, A.C.; Ramos, G.C.; Paz, C.C.S.C.; Martins, E.F. Baropodometric technology used to analyze types of weight-bearing during hemiparetic upright position. Fisioter. em Mov. 2012, 25(3), 583–594. [Google Scholar] [CrossRef]
- Paolucci, T.; Fusco, A.; Iosa, M.; Grasso, M.R.; Spadini, E.; Paolucci, S.; Saraceni, V.M.; Morone, G. The efficacy of a perceptive rehabilitation on postural control in patients with chronic nonspecific low back pain. Clin. Rehabil. 2012, 26(4), 335–345. [Google Scholar] [CrossRef] [PubMed]
- Marin, L.; Kawczyński, A.; Carnevale Pellino, V.; Febbi, M.; Silvestri, D.; Pedrotti, L.; Lovecchio, N.; Vandoni, M. Displacement of centre of pressure during rehabilitation exercise in adolescent idiopathic scoliosis patients. J. Clin. Med. 2021, 10(13), 2837. [Google Scholar] [CrossRef] [PubMed]
- Doshi, K.B.; Moon, S.H.; Whitaker, M.D.; Lockhart, T.E. Assessment of gait and posture characteristics using a smartphone wearable system for persons with osteoporosis with and without falls. Sci. Rep. 2023, 13(1), 538. [Google Scholar] [CrossRef]
- Maden, T.K.; Bayramlar, K.Y.; Yakut, Y. The effect of cervical mobilization on balance and static plantar loading distribution in patients with multiple sclerosis: A randomized crossover study. Neurosciences 2022, 27(1), 31–39. [Google Scholar] [CrossRef]
- Monteiro-Rodrigues, L.; Nuno, S.L.; Granja, T.; Florindo, M.E.; Gregório, J.; Atalaia, T. Perfusion, stance and plantar pressure asymmetries in the absence of disease—A pilot study. Symmetry 2022, 14(3), 441. [Google Scholar] [CrossRef]
- Shibata, D.; Yoshida, Y. Self-Mobilization Exercise Program Improved Postural Stability in the Anterior-Posterior Direction with Eyes Closed. Symmetry 2023, 15(7), 1321. [Google Scholar] [CrossRef]
- Glowinski, S.; et al. Gait analysis with an upper limb prosthesis in a child: Influence on plantar pressures and gait symmetry. J. Clin. Med. 2025, 14(7), 2245. [Google Scholar] [CrossRef]
- Molina-García, C.; Álvarez-Salvago, F.; Pujol-Fuentes, C.; López-del-Amo-Lorente, A.; Ramos-Petersen, L.; Martínez-Sebastián, C.; Martínez-Amat, A.; Jiménez-García, J.D.; De Diego-Moreno, M. Influence of foot type on physical characteristics, laxity, strength and baropodometry in children aged 5–10 years. Appl. Sci. 2024, 14(19), 8578. [Google Scholar] [CrossRef]
- Mocanu, G.; et al. Analysis of the influence of age stages on static plantar pressure indicators using a baropodometric platform. Appl. Sci. 2021, 11(16), 7320. [Google Scholar] [CrossRef]
- Kojić, M.; et al. The relationship between foot status and motor status in preschool-aged children. Healthcare 2021, 9(8), 936. [Google Scholar] [CrossRef] [PubMed]
- Daunoravičienė, K.; et al. EMG-based analysis of gait symmetry in healthy children. Sensors 2021, 21(17), 5983. [Google Scholar] [CrossRef] [PubMed]
- Chernik, N.D.; Young, M.W.; Jacobson, R.N.; Kantounis, S.J.; Lynch, S.K.; Virga, J.Q.; Cannata, M.J. Effects of high-intensity training on gait symmetry and locomotor performance in neurodivergent children: A pilot study. Symmetry 2025, 17(7), 1073. [Google Scholar] [CrossRef]
- Fullin, A.; Caravaggi, P.; Picerno, P.; Mosca, M.; Caravelli, S.; De Luca, A.; Lucariello, A.; De Blasiis, P. Variability of postural stability and plantar pressure parameters in healthy subjects evaluated by a novel pressure plate. Int. J. Environ. Res. Public Health 2022, 19(5), 2913. [Google Scholar] [CrossRef]
- Abou Ghaida, H.; Poffo, L.; Le Page, R.; Goujon, J.-M. Effect of Sensor Size, Number and Position under the Foot to Measure the Center of Pressure (CoP) Displacement and Total Center of Pressure (CoPT) Using an Anatomical Foot Model. Sensors 2023, 23(10), 4848. [Google Scholar] [CrossRef]
- Liu, W.; et al. Biomechanical characteristics of typically developing toddlers. Children 2022, 9(3), 406. [Google Scholar] [CrossRef]
- Serrato-Pedrosa, J.A.; et al. Biomechanical evaluation of plantar pressure distribution in soft tissue during standing. Appl. Sci. 2024, 14(4), 1650. [Google Scholar] [CrossRef]
- Taborri, J.; et al. Comparison of Machine Learning Algorithms Fed with Mobility-Related and Baropodometric Measurements to Identify Temporomandibular Disorders. Sensors 2024, 24(11), 3646. [Google Scholar] [CrossRef]
- Loukovitis, A.; et al. Test–retest reliability of PODOSmart® gait analysis insoles. Sensors 2021, 21(22), 7532. [Google Scholar] [CrossRef]
- Babović, S.S.; et al. Labeling of baropodometric analysis data using computer vision: Evaluation of foot progression angle. Medicina 2023, 59(5), 840. [Google Scholar] [CrossRef]
- Fan, Y.; Fan, Y.; Li, Z.; Lv, C.; Luo, D. Natural gaits of the non-pathological flat foot and high-arched foot. arXiv. 2010. Available online: https://arxiv.org/abs/1012.3816.
- Patwari, M.; Chazistergos, P.; Sundar, L.; Chockalingam, N.; Ramachandran, A.; Naemi, R. A quantitative comparison of plantar soft tissue strainability distribution and homogeneity between ulcerated and non-ulcerated patients using ultrasound strain elastography. Proc Inst Mech Eng H. 2022, 236(5), 722–729. [Google Scholar] [CrossRef] [PubMed]
- Serrato-Pedrosa, J.A.; et al. Numerical Analysis of the Plantar Pressure Points during the Stance Phases for the Design of a 3D-Printable Patient-Specific Insole. Symmetry 2024, 6(3), 429–456. [Google Scholar] [CrossRef]
- Wang, Y.; Zhang, P.; Chen, G.; Jiang, T.; Zou, Y. Comparison of the asymmetries in foot posture, gait and plantar pressure between patients with unilateral and bilateral knee osteoarthritis based on a cross-sectional study. Sci. Rep. 2024, 14, 26761. [Google Scholar] [CrossRef] [PubMed]
- Gurău, T.V.; et al. Static Baropodometric Assessment for Musculoskeletal Rehabilitation: Plantar Pressure and Postural Load Distribution in Young Adults. Life 2025, 15(9), 1354. [Google Scholar] [CrossRef]
- Bittar K.C.B..; et al. Reliability of plantar pressure and postural control measures of children from 4 to 12 years: analysis by baropodometry. Motriz: rev. educ. fis. 2020, 26 (03). [CrossRef]
- Baptista, C.R.J.A.; et al. Characterizing postural oscillation in children and adolescents with hereditary sensorimotor neuropathy. PLoS ONE 2018, 13(10), e0204949. [Google Scholar] [CrossRef]
- Purpura, G.; et al. Use of Virtual Reality in School-Aged Children with Developmental Coordination Disorder: A Novel Approach. Sensors 2024, 24(17), 5578. [Google Scholar] [CrossRef]
- Kiefer, A.W.; et al. Postural control development from late childhood through young adulthood. Gait Posture 2021, 86, 169–173. [Google Scholar] [CrossRef]
- Feng, Z.Y.; Li, J.Y.; Li, Y.W.; et al. Long term gait postural characteristics of children with general foot pain using smartphone connected wearable sensors. Sci. Rep. 2025, 15, 7767. [Google Scholar] [CrossRef]
- Shulman, D.; et al. Gait Symmetry Analysis in Patients after Treatment of Pilon Fractures by the Ilizarov Method. Symmetry 2021, 13(2), 349. [Google Scholar] [CrossRef]
- Eldridge, S. M.; Lancaster, G. A.; Campbell, M. J.; Thabane, L.; Hopewell, S.; Coleman, C. L.; Bond, C. M. Defining feasibility and pilot studies in preparation for randomised controlled trials: Development of a conceptual framework. PLoS ONE 2016, 11(3), e0150205. [Google Scholar] [CrossRef]
- Hertzog, M. A. Considerations in determining sample size for pilot studies. Research in Nursing & Health 2008, 31(2), 180–191. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).