1. Introduction
Gastroenteritis remains a significant global health concern as one of the leading causes of mortality, particularly in children [
1]. Annually, around 1.31 million deaths are related to diarrhea, with a substantial burden on children under five years old, who account for nearly 499,000 of these deaths [
2]. Its cause encompasses a spectrum of agents, including viruses, bacteria, parasites, and toxins. The most frequent etiological agents include noroviruses, which alone cause an estimated 210,000 deaths and 685 million diseases each year [
3]. Additionally, Rotavirus, Shigella spp and Salmonella spp are also highly prevalent [
2]. Viruses are usually the cause of around 25% of gastroenteritis cases [
4,
5]. Children under five years are disproportionately affected, with viral gastroenteritis accounting for more than 70% of cases in this population [
5].
The prognosis of gastroenteritis is notably worse in low and middle-income countries due to factors like malnutrition and inadequate sanitation [
2]. Despite the high morbidity and mortality, improvements in sanitation and vaccination can reduce gastroenteritis-related deaths. Continued public health initiatives can further mitigate this burden [
6].
The diagnosis routinely relies on clinical evaluation, laboratory tests, and imaging techniques [
6]. Rapid diagnosis is linked to a better patient prognosis, as early microbial diagnosis allows for prompt initiation of targeted therapies that can significantly reduce morbidity and mortality [
7], as well as avoid or limit inappropriate antibiotic prescription reducing unnecessary use of broad-spectrum antibiotics, ultimately combating antibiotic resistance effectively. This is essential for managing infections that can lead to severe complications, especially in vulnerable populations like children and immunocompromised patients [
8]. Delays in identifying the specific pathogen and its resistance profile are an important factor in treatment failure. This uncertainty forces clinicians to prescribe broad-spectrum antibiotics as a precaution. When the correct antibiotic is not administered in time, patient outcomes worsen, leading to increased mortality, longer hospital stays, higher healthcare costs, and can promote bacterial resistance [
9,
10]. Additionally, rapid diagnostic tests are crucial for early case identification and surveillance during outbreaks, as emphasized in the 100 Days Mission initiative, a global initiative that aims to prepare the world for the next epidemic/pandemic [
11].
The FilmArray Gastrointestinal (FAGI) panel is a syndromic multiplex PCR that detects common infectious diarrhea pathogens, including bacteria, parasites, and viruses. Given the importance of rapid and accurate diagnostics to improve clinical outcomes, the introduction of advanced diagnostic tools such as the FilmArray panel could have a significant impact on clinical practice, especially in hospital settings where the burden of infectious diseases is high [
12]. Comparing their effectiveness and cost-effectiveness with Standard of care (SOC) conventional methods is essential to validate their large-scale implementation.
Although several studies have evaluated the effectiveness of FilmArray compared to traditional SOC diagnostic tests [
13,
14,
15,
16,
17], this study aimed to evaluate the performance in a real-world setting, conducted in a major city with limited resources of a middle-income country. Furthermore, most of these studies were with a limited sample size. By focusing on the clinical and operational impact of the FilmArray panel, this study aims to contribute evidence to improve diagnostic practices and patient outcomes in similar resource-limited environments.
2. Materials and Methods
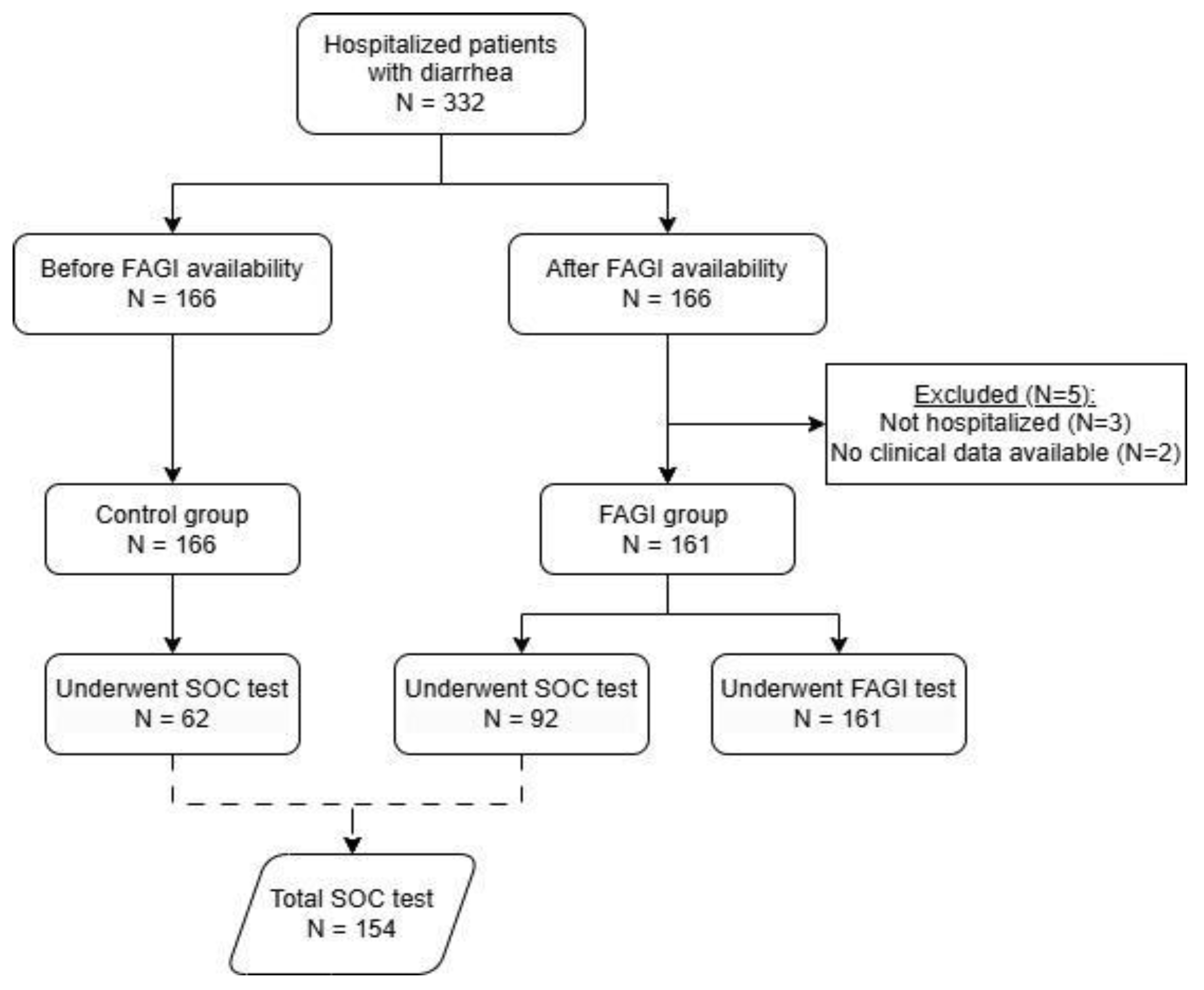
Study design - This retrospective observational study was conducted at São José Hospital for Infectious Diseases, a tertiary care center in Fortaleza, Ceará, Brazil. We compared diagnostic yield, turnaround time (TAT), Days of Treatment (DOT), Length of stay (LOS) and total cost of treatment between patients who were tested with FilmArray GI panel (FAGI) (from June 2019 to November 2020) and a historical control group (from December 2017 to October 2018) of the same number of patients consecutively included, immediately prior to the panel being made available at the hospital. The same medical team was involved in the treatment of patients from both groups. Patients with a suspected gastrointestinal infection were enrolled after completing electronic medical records regardless if the diarrheal syndrome was the cause of hospitalization or was contracted during hospitalization. Exclusion criteria were not having been hospitalized or lacking clinical or laboratory data in medical records. This study was approved by the local ethical committee, under the number CAAE 47310521.9.0000.5044. For the control group the above-mentioned inclusion and exclusion criteria and classification were maintained. In total, 332 patients were recruited, and 161 patients were included in the FAGI group and 166 in the control group.
Laboratory tests - BioFire FilmArray Gastrointestinal panel (FAGI - BioMerieux, Marcy L’Etoile, France) detects 22 pathogens in fecal swabs in about an hour. The pathogens include Campylobacter (jejuni, coli and upsaliensis), C. difficile (toxin A/B); P. shigelloides, Salmonella, Vibrio (parahaemolyticus, vulnificus and cholerae), Y. enterocolitica; Escherichia coli O157, Enteroaggregative Escherichia coli (EAEC), Enteropathogenic Escherichia coli (EPEC), Enterotoxigenic Escherichia coli (ETEC) lt/st, Shiga-like toxin-producing Escherichia coli (STEC) stx1/stx2, Shigella/Enteroinvasive Escherichia coli (EIEC), Cryptosporidium; C. cayetanensis; E. histolytica; G. lamblia, Adenovirus F 40/41, Astrovirus; Norovirus GI/GII, Rotavirus A and Sapovirus (I, II, IV e V).
FAGI tests were performed according to the manufacturer’s instructions - out of the hospital of this study - at LACEN (Laboratório Central de Saúde Pública) which has limited opening hours (from Monday to Friday 8 am to 4 pm and on weekends 10 am to 12 pm). Standard of care (SOC) tests were performed according to the hospital’s routine tests available for gastroenteritis investigation. Those included parasitological examination of feces, stool culture, special stains for Cystoisospora and Cryptosporidium research, and C. difficile toxins A/B by enzyme-linked immunosorbent assay. No specific guidelines and restrictions were in place for clinicians regarding microbiological testing and therefore practice was at the clinician’s discretion. Therefore, some patients in both groups did not undergo these tests.
Statistical analysis - The SOC test was analyzed separately for the control group and the FAGI group, as well as collectively, considering the total number of SOC tests performed in both groups. The time from collection to results for the SOC tests was considered as the longest time for the test result. Treatment costs were calculated by multiplying the total number of antimicrobial doses used per patient by the cost per dose. Statistical analyses were performed using RStudio version 4.1.1. The Shapiro test was used to assess normality. Comparisons between groups were performed using a two-tailed Wilcoxon test for non-parametric continuous variables and a two-tailed Fisher’s exact test for binary categorical variables. A p-value of <0.05 was considered statistically significant. Graphics were generated with libraries ggsci, tidyverse, ggpubr, dplyr and irr and ggplot2.
3. Results
A total of 332 patients were divided into two groups: FAGI (n=166, 153 adults and 13 children) and control (n=166, 154 adults and 12 children). Five patients were excluded from the FAGI group: three were not hospitalized, and two lacked available clinical or laboratory data (
Figure 1). The median age was 37 years (ranging from 6 months to 71 years) in the control group and 39 years (1 month to 87 years) in the FAGI group, with 38% and 28% of women, respectively. Most of the patients were positive for HIV being 83% of the control group and 75% of the FAGI group (p =0.06). There were no significant differences between the groups in terms of mortality rate (p=0.77) or LOS (p=0.44). Notably, there was a significant 30% reduction in the antibiotic use in the FAGI group compared to the Control group (p<0.001). The total number of antimicrobials used per patient was reduced by 50% (p<0.001), with a 37% reduction in the overall antimicrobial use (p<0.001). Patients in the FAGI group had a median of 5 days shorter duration of antimicrobial DOT (median days: 6 vs. 11, p<0.001), 83% reduction of total antimicrobial costs (median total cost: BRL 4,697 vs. BRL 27,174, p<0.001), and an increase of 77% in the number of pathogens detected (median: 103 vs. 24, p<0.001) compared to the control group (
Supplementary Figure S1). It is important to note that one of the primary contributors to the substantial cost difference was the use of liposomal amphotericin/lipid complex for empirical therapy in some patients with suspected Histoplasma-related diarrhea. These findings are summarized in
Table 1.
In the control group, 62 patients underwent SOC tests. In the FAGI group, all patients had FilmArray tests, and 92 also had SOC tests. Then we compared the results of the total number of patients that underwent SOC tests (n=154) with Filmarray (n=161). The use of FilmArray significantly increased the number of samples with a pathogen identified, with 64% positivity compared to 32% in those tested with SOC methods (p<0.001). The median number of pathogens detected per sample was also higher in the FilmArray group, with a median of 2 pathogens (range 1-5), compared to a median of 0 (range 0-2) for the SOC test (p<0.001). Furthermore, FilmArray reduced the TAT from sample collection to diagnostic result by 18%, with a median time of 60 hours (range 5-500), compared to 73 hours (range 12-394; p<0.001) for SOC tests. When the time from sample shipping to result was evaluated, FilmArray reduced the time by 38% with a median time of 45 hours (range 5-500; p<0.001). These results are summarized in
Table 2 and
Supplementary Figure S2.
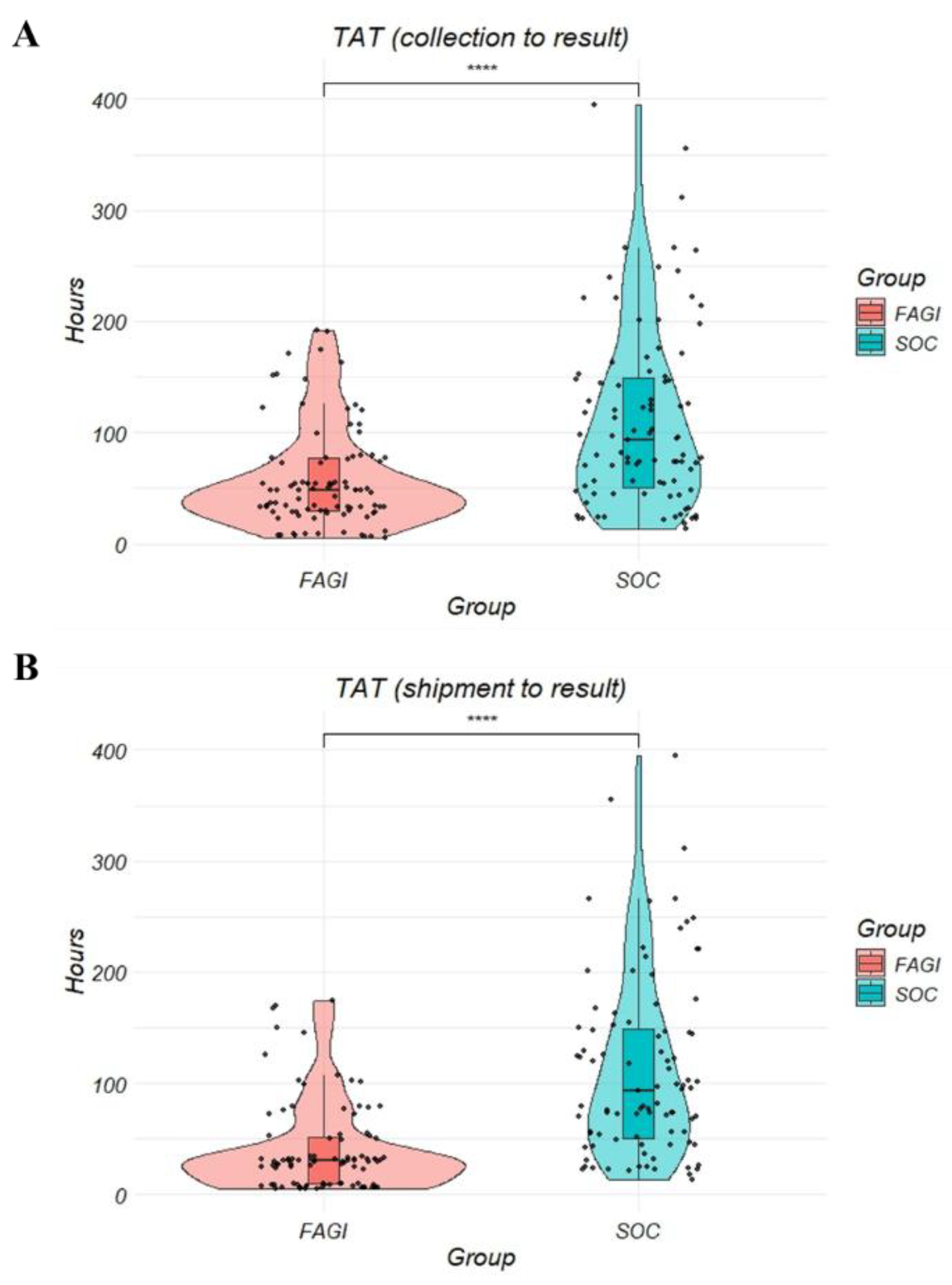
Next, to compare the turnaround times (TAT) of both diagnostic methods, we restricted our analysis to the subgroup of patients who underwent both FilmArray and SOC testing. This approach ensured a direct comparison by eliminating potential confounding factors from patients who received only one of the tests. Among the 92 patients from the FAGI group, FAGI demonstrated a 45h shorter TAT (median hours: 48 vs. 93, p<0.001) considering the collection time to result and a 63h shorter TAT (median hours: 30 vs. 93, p<0.001) considering the shipment time to result (
Figure 2) compared to SOC tests.
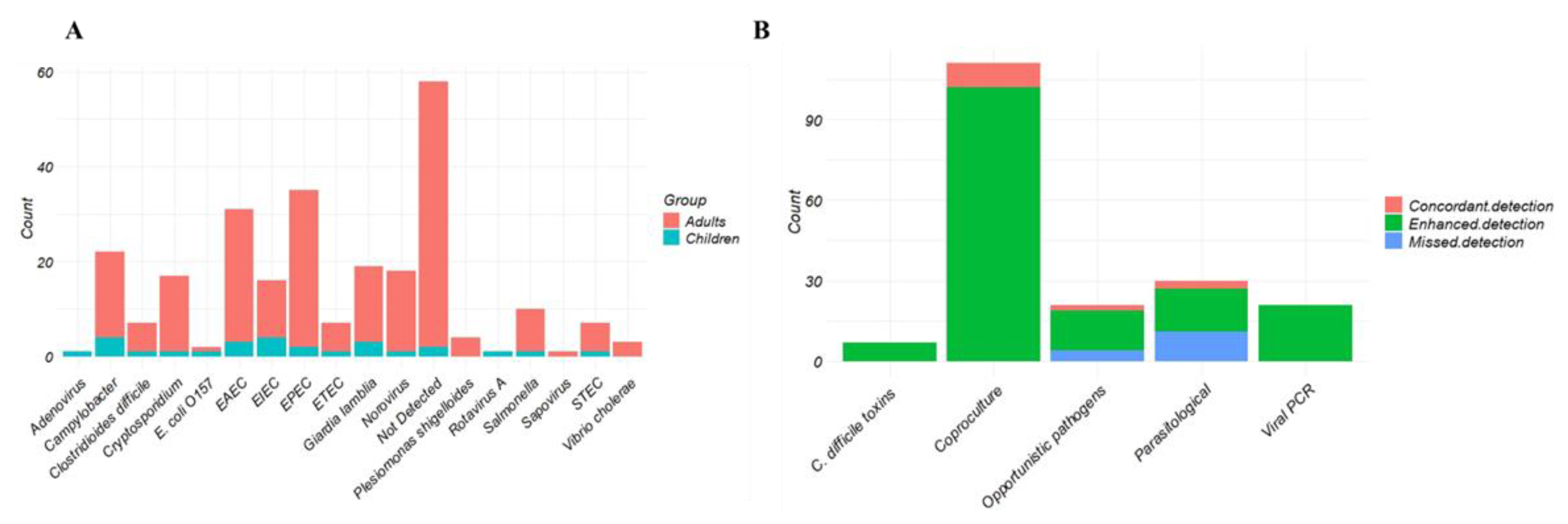
FilmArray identified 201 targets in the FAGI group. The most common were EPEC (n = 35), EAEC (n = 31), Campylobacter (n = 22), Giardia lamblia (n = 19) and Norovirus (n = 18). There were 58 samples without a pathogen detected by FilmArray, with a positivity rate of 64% (62% in adults and 85% in pediatric patients;
Figure 3A,
Table 3). Additionally, we observed an 88% higher pathogen detection rate for FilmArray. There were 187 pathogens detected only by FAGI, 15 detected only by SOC and 14 identified by both methods
Table 3). However, there was one missed detection of Entamoeba histolytica in one patient. Moreover, some parasites (Ascaris lumbricoides, Endolimax nana, Entamoeba coli, Hookworm and Cystoisospora belli) not included at the FAGI panel were also missed (
Figure 3B,
Table 3).
4. Discussion
The findings of this study indicate that the FilmArray Gastrointestinal (FAGI) panel significantly enhances the diagnosis of gastroenteritis compared to SOC methods. The study provides valuable insights into the challenges and opportunities associated with implementing advanced diagnostic technologies in settings where healthcare resources are scarce. Patients in the FAGI group had a shorter duration of antimicrobial treatment, reduced treatment costs, and a higher number of pathogens detected compared to those who underwent SOC testing, highlighting the advantages of molecular diagnostic methods.
Several studies support the efficacy of multiplex PCR panels like FilmArray in improving diagnostic accuracy and clinical outcomes. Beal et al. demonstrated that the use of the FilmArray panel reduced the time from stool collection to discharge by 15%, which consequently shortened the total health care costs in
$293.61 per patient [
19]. Similarly, Cybulski et al., found that FilmArray improved the sample detection of pathogens 6 times (35.3% of specimens, compared to 6.0% for culture). Also, the median time from collection to result was 18 hours for FilmArray and 47 hours for culture [
12]. Additionally, they found a reduction of 50 hours from collection to initiation of antimicrobial therapy leading to more targeted and effective treatments. Indeed, other studies also concluded that FilmArray can positively impact the medical management of gastroenteritis [
17,
20,
21]. Another study showed that FilmArray provides results in a median time of 2.2 hours compared to 77.5 hours for culture methods [
22]. Despite the significant reduction observed with the use of the FilmArray Gastrointestinal panel, we did not find such a drastic reduction in diagnostic time (60h vs 73h) as expected. It is important to note that in this study, the FilmArray was not available in the hospital’s routine laboratory. The samples had to be sent to an external laboratory, which subjected them to transportation time and the laboratory’s availability to perform the tests. This logistical process, which included weekends and holidays when the reference laboratory was not operating, contributed significantly to the increase in total diagnostic time. Although the test itself takes only one hour to complete, external factors considerably delayed the delivery of results. Even so, we evidenced a major impact on the costs of treatment and use of antimicrobials.
The median hospitalization duration for the FAGI group was 13 days (ranging from 1 to 114 days), compared to 12 days (ranging from 1 to 110 days) for the control group. However, it has been previously evidenced by Torres-Miranda et al. that hospital LOS was shorter (3 vs. 7.5 days) for the FilmArray group compared to standard methods [
20]. Accordingly, Carmon et al., evidenced a reduction in LOS in patients with a positive FilmArray gastrointestinal result (2 days) compared to negative test results [
17]. DelRusso et al. found a reduction of 1.6 days in LOS. Although this difference was not statistically significant (p = 0.13), they also observed a reduction of 24 h in time to de-escalation (p < 0.001) and a reduction of 30h in TAT (p < 0.001) [
23]. It is important to highlight that this study period coincided with the COVID-19 pandemic, during which many cases experienced prolonged hospital stays due to complications related to COVID-19 [
24]. This context made it challenging to directly compare the FAGI group with the historical control group, which was observed in the year before the pandemic.
We observed a reduction of antimicrobial use per patient of 37% in the FAGI group compared to the control. This reduction aligns with the goals of antimicrobial stewardship programs, which aim to optimize antibiotic use and reduce resistance [
25,
26]. The use of molecular diagnostic tests such as FAGI in clinical practice can decrease the unnecessary use of antibiotics [
14,
27]. By providing rapid and accurate results, FilmArray enables clinicians to make informed decisions about antibiotic prescriptions, thereby minimizing unnecessary broad-spectrum antibiotic use. Moreover, the benefits of using FilmArray are notable. The reduction in the length of hospital stays, seen by other authors, and the shorter duration of antimicrobial treatment may contribute to decreased overall healthcare costs. Although we have not evaluated overall costs, the reduction and shorter duration of antimicrobial treatment may contribute to decreased total healthcare costs
The economic impact is also a crucial factor. Although the initial costs of multiplex molecular testing may be higher, the reduction in overall treatment costs and the shortened length of hospital stay may justify the costs in the long term [
28]. Ambrosius-Eichner et al. (2024) showed that FimArray GI panel significantly improve pathogen detection rates (39.9% vs. 15% with SOC methods). Our study reinforces these observations, showing that FAGI is not only more time-efficient but may also be cost-effective by reducing the costs of antimicrobial treatment by 83%.
Studies like this are crucial in assessing the impact of molecular diagnostics, such as multiplex PCR panels, in low- and middle-income countries like Brazil. These advanced diagnostic tools, while often expensive, have the potential to significantly improve clinical outcomes through rapid and accurate pathogen detection. However, a limitation of our study is that we could not comprehensively evaluate the total hospitalization costs, including hospital and diagnostic testing expenses. This gap underscores the need for further research to substantiate the cost-effectiveness of high-priced diagnostic kits like the FilmArray in resource-limited settings. While the upfront costs of multiplex PCR panels may be higher, the long-term savings and improved patient outcomes could justify their broader adoption.
The FilmArray GI Panel provides faster results, which is crucial for timely treatment decisions in patients with gastroenteritis [
21,
27,
29]. Despite its advantages, there are concerns regarding the potential for false positives and the appropriateness of testing in late-stage hospital admissions, suggesting a need for diagnostic stewardship [
18]. Other limitations of this study include its retrospective design, which does not allow for proper randomization of patients based on their comorbidities or standardization of the attending physicians’ practices regarding the collection of SOC tests and the prescription of antimicrobials. Additionally, it should be noted that the medical team remained consistent throughout the study period, which may mitigate some variability in clinical practices but does not entirely eliminate potential biases.
It is important to note that the fact that this study was conducted in an infectious disease hospital likely contributed to limit the inappropriate use of antimicrobials, given the specialized focus of the institution. To achieve similar results in general hospitals, it is essential that the interpretation of the panel results and subsequent clinical decisions are evaluated and defined in collaboration with an infectious diseases team.
In conclusion, this study underscores the clinical and economic advantages of the FilmArray Gastrointestinal panel over conventional diagnostic methods for gastroenteritis. The implementation of such molecular diagnostics can enhance patient care by enabling timely, accurate diagnosis and more effective treatment strategies.
Supplementary Materials
The following supporting information can be downloaded at the website of this paper posted on Preprints.org, Supplementary Figure S1: Hospitalization comparison between groups. Supplementary Figure S2: Laboratory variables comparison between patients that underwent FilmArray.
Author Contributions
Conceptualization and Methodology, G.A.L and J.F.O; Validation, G.A.L; Formal Analysis, M.F.C.; Investigation, G.A.L, K.F.C, P.P.N.B and F.B.P.M.; Writing – Original Draft Preparation, M.F.C.; Writing – Review & Editing, G.A.L, J.S and J.F.O; Visualization, M.F.C. and J.F.O; Supervision, G.A.L and J.F.O; Project Administration, J.S and J.F.O; Funding Acquisition, G.A.L and J.F.O. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board (or Ethics Committee) of HOSPITAL SÃO JOSÉ (protocol code CAAE 47310521.9.0000.5044 and 05/22/2022.
Informed Consent Statement
Patient consent was waived due to the retrospective nature of the study, which relied solely on secondary data extracted from electronic medical records. No direct patient contact or intervention was involved, and all data were anonymized prior to analysis to ensure confidentiality.
Data Availability Statement
Data contained within the article.
Acknowledgements
We would like to thank Dr. Maisa Benette for her support in the follow-up of the progress of the article’s preparation activities.
Conflicts of Interest
This research received financial support from bioMérieux Brasil for data collection and statistical analysis. Sousa J and Ortega JF are employees of bioMérieux.
Abbreviations
The following abbreviations are used in this manuscript:
| FAGI |
FilmArray gastrointestinal panel |
| SOC |
Standard of care |
| TAT |
Turnaround time |
| DOT |
Days of Treatment |
| LOS |
Length of stay |
| LACEN |
Laboratório Central de Saúde Pública |
References
- World Health Organization (WHO). Diarrhoeal disease. https://www.who.int/news-room/fact-sheets/detail/diarrhoeal-disease. 7 March 2024.
- GBD Diarrhoeal Diseases Collaborators. Estimates of global, regional, and national morbidity, mortality, and aetiologies of diarrhoeal diseases: a systematic analysis for the Global Burden of Disease Study 2015. Lancet Infect Dis. 2017; 17:909-948.
- Shah M.P, Hall AJ. Chapter 1 - Global Disease Burden of Foodborne Illnesses Associated With Norovirus. In: The Norovirus Features, Detection, and Prevention of Foodborne Disease. Academic Press, 2017.
- Schmidt MA, Groom HC, Rawlings AM et al. Incidence, Etiology, and Healthcare Utilization for Acute Gastroenteritis in the Community, United States. Emerg Infect Dis. 2022; 28:2234-2242. [CrossRef]
- Sharma PC, McCandless M, Sontakke SP, et al. Navigating Viral Gastroenteritis: Epidemiological Trends, Pathogen Analysis, and Histopathological Findings. Cureus. 2024; 16:e61197. [CrossRef]
- Rao RRT, Pratiksha B, Navyasri C, Kalita DJ, Alam S. Gastroenteritis: A Comprehensive Review. International Journal of Current Science Research and Review. 2024; 10:7511-7517.
- Babaei A, Rafiee N, Taheri B, Sohrabi H, Mokhtarzadeh A. Recent Advances in Early Diagnosis of Viruses Associated with Gastroenteritis by Biosensors. Biosensors (Basel). 2022; 8:499. [CrossRef]
- Mo Y. Rapid Diagnostics for Antibiotic Resistance: Urgent Need for Strong Clinical Evidence. Clin Infect Dis. 2022; 75:2076-2078. [CrossRef]
- Asthana V, Nieves EM, Bugga P, et al. Development of a rapid, culture-free, universal microbial identification system using internal transcribed spacer targeting primers. J Infect Dis. 2024; 6:545. [CrossRef]
- De Waele JJ, Boelens J. Antimicrobial stewardship and molecular diagnostics: a symbiotic approach to combating resistance in the ED and ICU. Curr Opin Crit Care. 2024; 30:231-238. [CrossRef]
- Yimer SA, Booij BB, Tobert G, et al. Rapid diagnostic test: a critical need for outbreak preparedness and response for high priority pathogens. BMJ Glob Health. 2024; 9:e014386. [CrossRef]
- Cybulski RJ Jr, Bateman AC, Bourassa L, et al. Clinical Impact of a Multiplex Gastrointestinal Polymerase Chain Reaction Panel in Patients With Acute Gastroenteritis. Clin Infect Dis. 2018; 67:1688-1696. [CrossRef]
- Buss SN, Leber A, Chapin K et al. Multicenter evaluation of the BioFire FilmArray gastrointestinal panel for etiologic diagnosis of infectious gastroenteritis. J Clin Microbiol. 2015; 53:915-25. [CrossRef]
- Axelrad JE, Freedberg DE, Whittier S et al. Impact of Gastrointestinal Panel Implementation on Health Care Utilization and Outcomes. J Clin Microbiol. 2019; 57:e01775-18. [CrossRef]
- DiDiodato G, Allen A, Bradbury N et al. The Efficacy of the BioFire FilmArray Gastrointestinal Panel to Reduce Hospital Costs Associated With Contact Isolation: A Pragmatic Randomized Controlled Trial. Cureus. 2022;14:e27931. [CrossRef]
- Machiels JD, Cremers AJH, van Bergen-Verkuyten MCGT et al. Impact of the BioFire FilmArray gastrointestinal panel on patient care and infection control. PLoS One. 2020; 15:e0228596. [CrossRef]
- Carmon D, Rohana H, Azrad M, Peretz A. The Impact of a Positive Biofire® FilmArray® Gastrointestinal Panel Result on Clinical Management and Outcomes. Diagnostics (Basel). 2023; 4:1094.
- Madhavappallil J, Laracy J, Kamboj M, Yan J, Usiak S. Assessment of the FilmArray Gastrointestinal Pathogen PCR Panel at a Tertiary Cancer Center. Antimicrob Steward Healthc Epidemiol. 2024; 16:4. [CrossRef]
- Beal SG, Tremblay EE, Toffel S, Velez L, Rand KH. A Gastrointestinal PCR Panel Improves Clinical Management and Lowers Health Care Costs. J Clin Microbiol. 2017; 26:1457-17. [CrossRef]
- Torres-Miranda D, Akselrod H, Karsner R, et al. Use of BioFire FilmArray gastrointestinal PCR panel associated with reductions in antibiotic use, time to optimal antibiotics, and length of stay. BMC Gastroenterol. 2020; 20:246. [CrossRef]
- Truong J, Cointe A, Le Roux E, et al. Clinical impact of a gastrointestinal PCR panel in children with infectious diarrhoea. Arch Dis Child. 2022; 107:601-605. [CrossRef]
- Ambrosius-Eichner J, Hogardt M, Berger A, Dultz G, et al. Comparative evaluation of the detection rate, workflow and associated costs of a multiplex PCR panel versus conventional methods in diagnosis of infectious gastroenteritis. J Med Microbiol. 2024;73:2. [CrossRef]
- DelRusso K, Colmerauer J, Premus J. Impact of the BioFire FilmArray Blood Culture Identification 2 (BCID2) Panel on Time to Antimicrobial Escalation or De-escalation in a Community Health System. Open Forum Infect Dis. 2023; 27:10. [CrossRef]
- Lucijanic M, Marelic D, Stojic J, et al. Predictors of prolonged hospitalization of COVID-19 patients. Eur Geriatr Med. 2023; 3:511-516. [CrossRef]
- Lanckohr C, Bracht H. Antimicrobial stewardship. Curr Opin Crit Care. 2022; 28:551-556.
- Stocker M, Klingenberg C, Navér L, et al. Less is more: Antibiotics at the beginning of life. Nat Commun. 2023; 14:2423. [CrossRef]
- Keske Ş, Zabun B, Aksoy K et al. Rapid Molecular Detection of Gastrointestinal Pathogens and Its Role in Antimicrobial Stewardship. J Clin Microbiol. 2018; 56:e00148-18. [CrossRef]
- Hatfield K, Kabbani S, Currie D, et al. Utilization of multiplex molecular panels for urinary tract infections, Medicare claims, 2016 – 2022. Antimicrob Steward Healthc Epidemiol. 2024; 16:4. [CrossRef]
- Sever A, Ben Zvi H, Melamed SB, Sachs N, Krause I, Bilavsky E. Clinical impact of biofire gastrointestinal panel testing for hospitalized children with acute gastroenteritis. Acta Paediatr. 2023; 112:505-509. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).