1. Introduction
Precision oncology is the use of precision medicine in oncology. In fact, the development of precision medicine has been primarily driven by the development of precision oncology. Precision oncology is the most studied and widely applied subarea of precision medicine.
Precision oncology refers to the use of broad molecular tumor characterization with the aim of personalized therapeutic management. In simple terms, the goal of precision medicine is to deliver the right cancer treatment to the right patient, at the right dose, at the right time.
The term ‘precision medicine’ first gained prominence after a publication by the US National Research Council in 2011 [
1]. Four years later, precision medicine has become a term that symbolizes the new age of medicine following the launch of the national Precision Medicine Initiative by then President Obama in the United States in 2015 [
2].
However, the use of molecular characterization of an individual patient’s tumor in routine oncologic practice roughly began 20 years ago, especially following the publication of the first draft of the Human Genome Project in 2003. Moreover, the idea and practice of precision medicine/oncology had even earlier origins, beginning in the 1980s and 1990s [
2,
3].
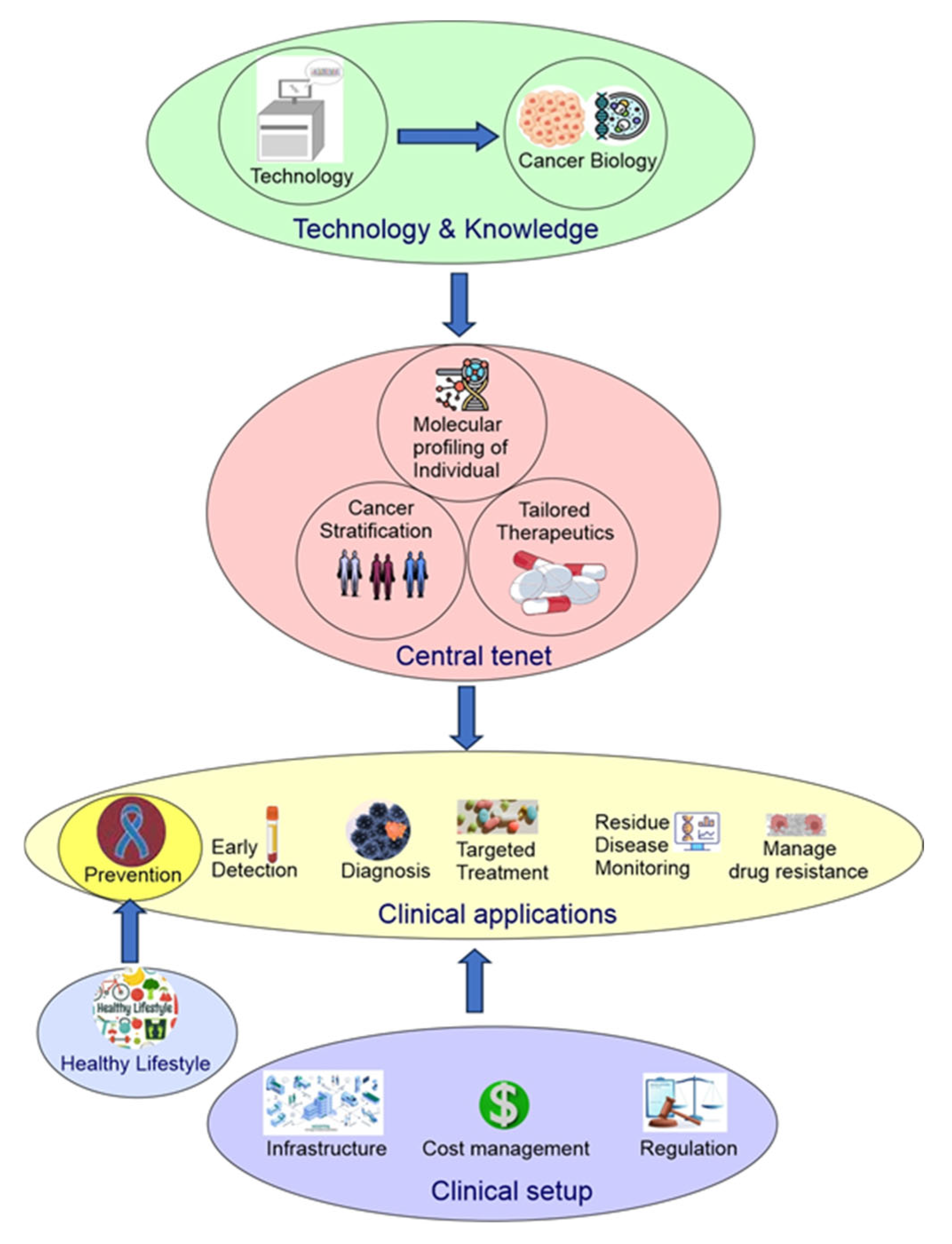
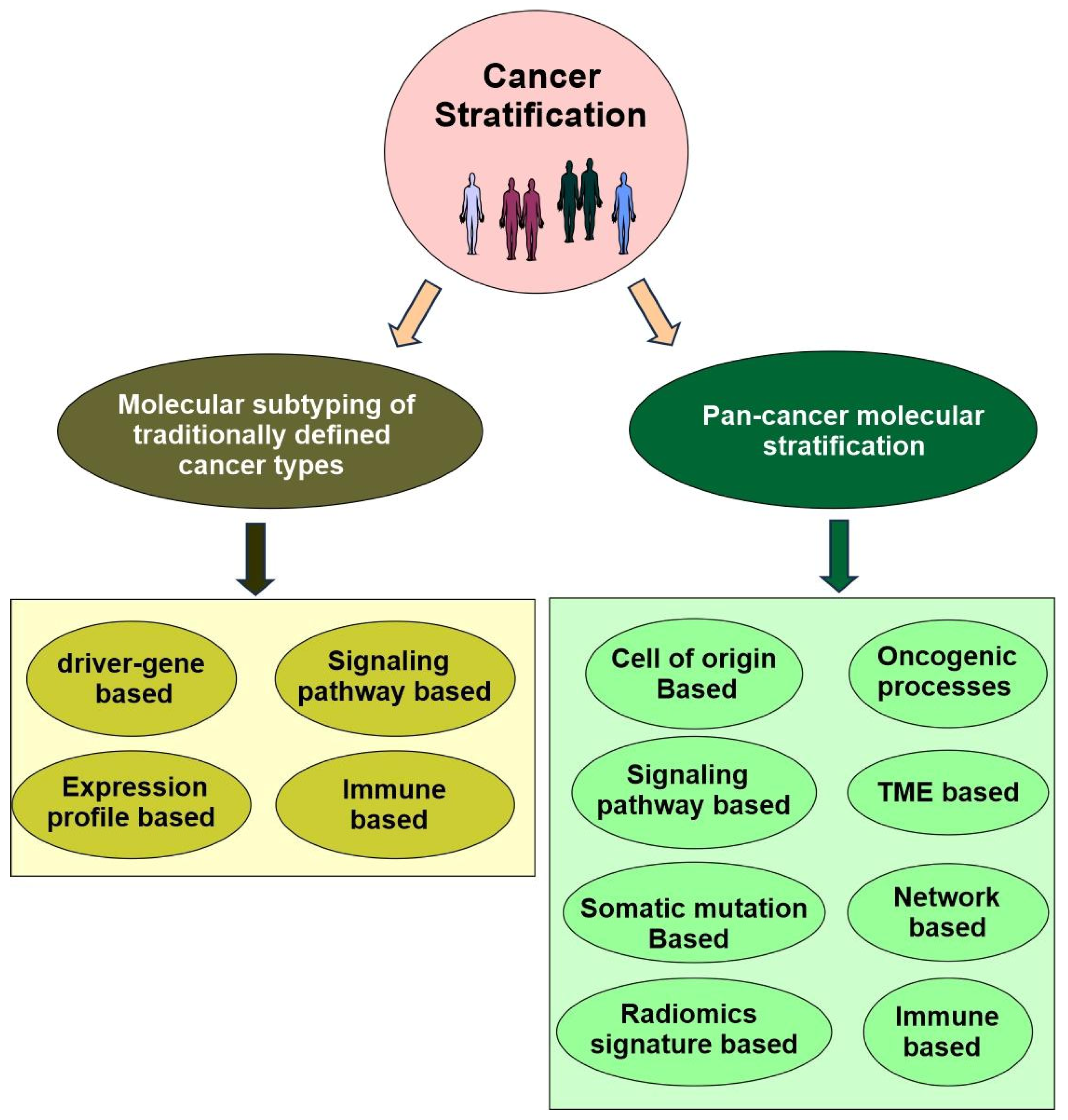
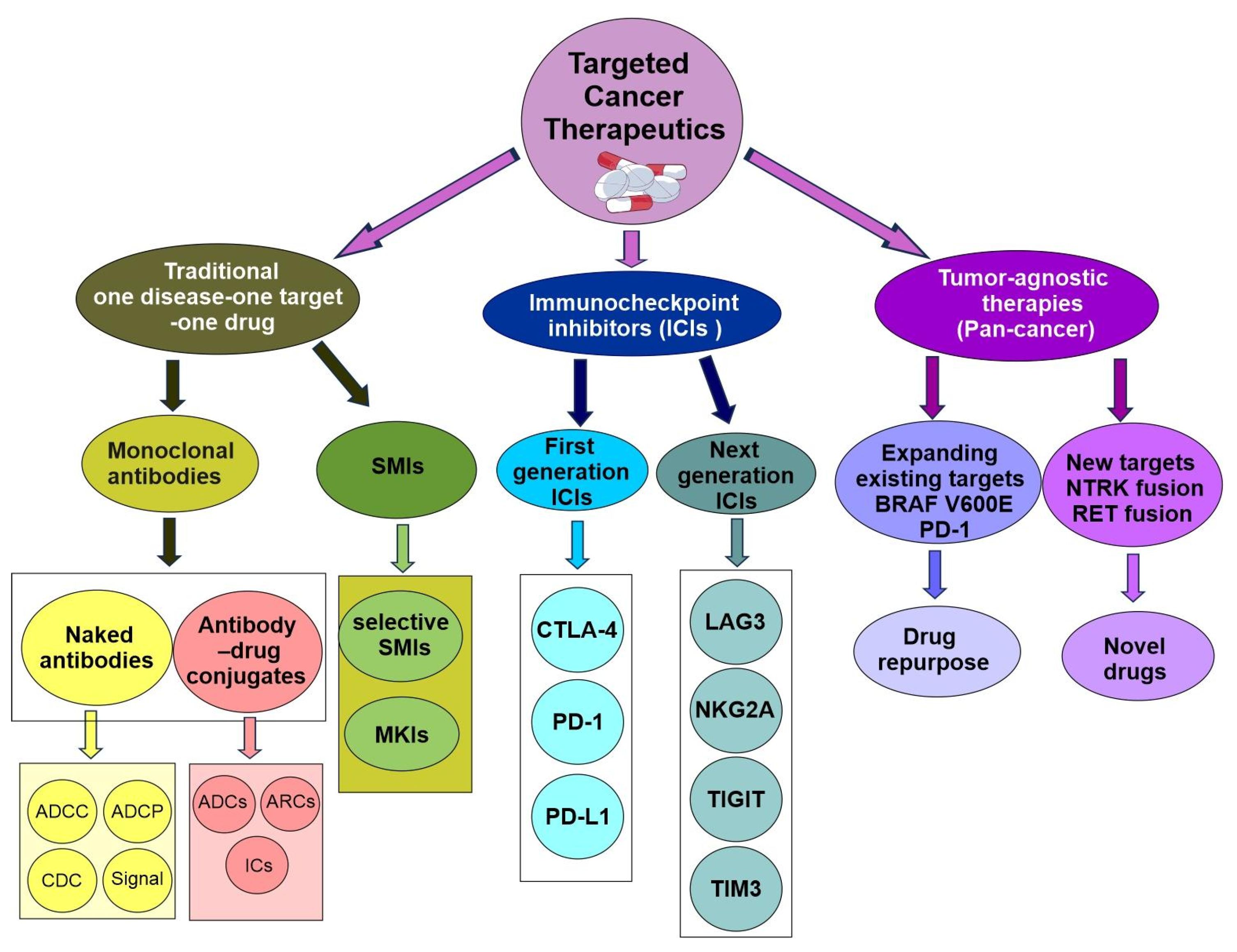
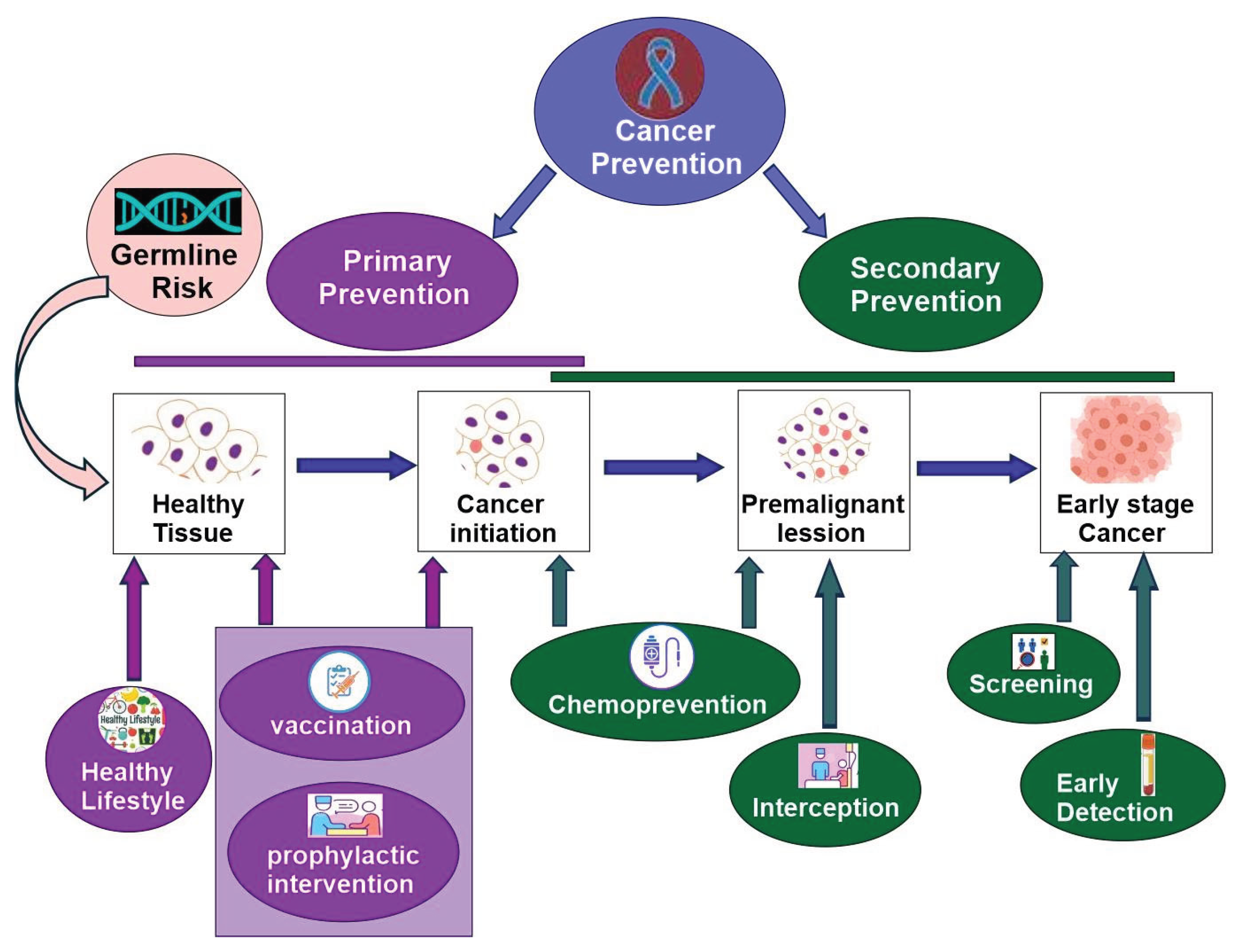
The early development of precision oncology was driven by a desire to move beyond blanket treatments for patients to a more refined, efficient, and patient-centred approach. To achieve this goal, three essential objectives must be met. First, the cancer needs to be stratified into various subtypes. Second, there must be tailored treatment available for each specific subtype. Third, comprehensive molecular profiling of each individual patient must be generated. When all three objectives are met, patients can be individually assigned to a particular cancer subtype and then treated with appropriate tailored therapies [
2]. In addition, early diagnosis is another important element of a successful cancer treatment. This becomes increasingly possible due to the rapid development of modern technology and deeper understanding of cancer biology.
Now, precision oncology has expanded to include modern technology (big data, single-cell spatial multiomics, molecular imaging, liquid biopsy, CRISPR gene editing, stem cells, organoids), a deeper understanding of cancer biology (driver cancer genes, single nucleotide polymorphism, cancer initiation, intratumor heterogeneity, tumor microenvironment ecosystem, pan-cancer), cancer stratification (subtyping of traditionally defined cancer types and pan-cancer re-classification based on shared properties across traditionally defined cancer types), clinical applications (cancer prevention, early detection, diagnosis, targeted therapy, minimal residual disease monitoring, managing drug resistance), lifestyle changes (physical activity, smoking cessation, reduced alcohol consumption, sunscreen), cost management, public policy, and more (
Figure 1) [
2,
4].
In this review, we will focus on the various pillars of precision oncology, with an emphasis on emerging trends, challenges, and future perspectives.
2. Emerging and Maturation of Technologies in Precision Oncology
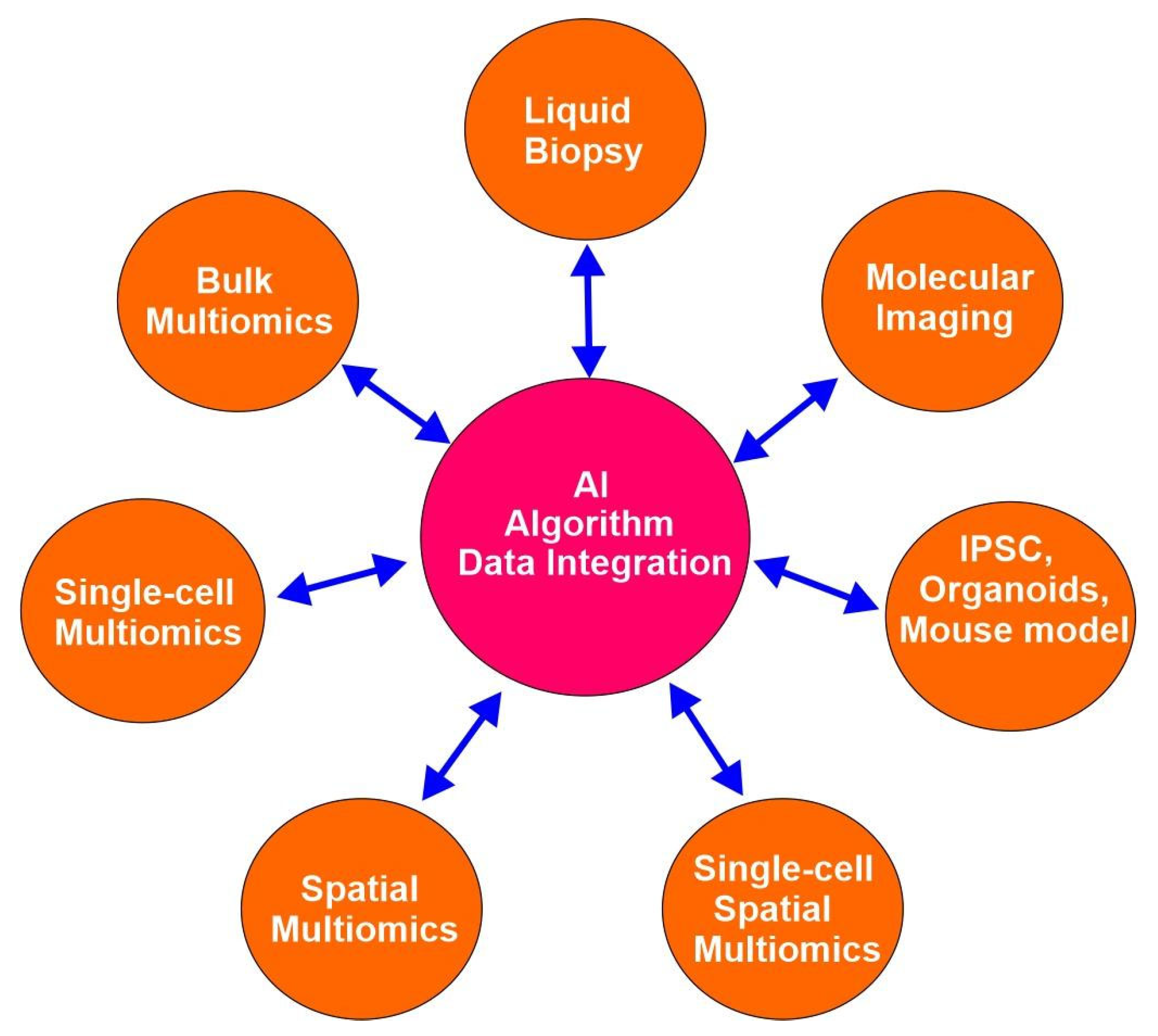
Advanced emerging technologies have revolutionized cancer research since the completion of the human genome project in the early 21st century and empowered precision oncology. These technologies include, but are not limited to bulk multiomics, single-cell multiomics, spatial multiomics, single-cell spatial multiomics, organoids, induced pluritopical stem cells (iPSCs), CRISPE gene editing, liquid biopsy, molecular imaging, and artificial intelligence (AI) (
Figure 2). These technologies help by providing a snapshot of any biological system of interest at an unprecedented resolution and dimension. Omics is a nomenclature broadly applied to the collective study of molecular characterization and quantification of biological molecules from various subdomains of molecular biology using high-throughput technology. These subdomains include genomics, epigenomics, transcriptomics, proteomics, and metabolomics, among others [
2].
The fundamental high-throughput technology in omics is Next-Generation Sequencing (NGS). NGS sequences millions of DNA fragments at once, producing enormous amounts of molecular data efficiently, quickly, and at a lower cost. It has advanced nearly every area of omics research.
However, these one-dimensional bulk omics struggle with many issues, such as intratumor heterogeneity and tumor microenvironment (TME). Recently developed technologies, including single-cell multiomics, spatial multiomics, and liquid biopsy, have allowed for a much deeper understanding of the novel aspects of tumor biology. In the following sections, we will discuss several cutting-edge technologies that have made important contributions to precision oncology.
2.1. Single-Cell Multiomics
Single-cell sequencings can reveal the specific effect of an individual cellular component. Since the first report of single-cell genome-wide mRNA sequencing in 2009 [
5], various single-cell cell sequencing methods have been developed, including single-cell DNA sequencing for genomics, single-cell DNA methylome sequencing quantifying DNA methylation, single-cell ATAC-seq (Assay for Transposase-Accessible Chromatin using sequencing) investigating chromatin accessibility at the single-cell level, single-cell proteomics quantifying the expressed proteome in an individual cell, and single-cell metabolomics [
6,
7].
Single-cell omics technologies offer high-resolution analysis of cellular diversity, overcoming the limitations of bulk methods that mask individual cell differences. These approaches enable the identification of distinct cell types and rare cell populations, as well as dynamic cell states. These techniques offer unprecedented sensitivity and resolution, empowering researchers to reveal the molecular landscape of individual cells [
7].
The emerging trend in single-cell omics is to integrate multimodal omics data within a single-cell to generate a holistic and comprehensive picture of cellular processes. Multimodal omics can help clarify complex cellular interactions, regulatory networks, and molecular mechanisms.
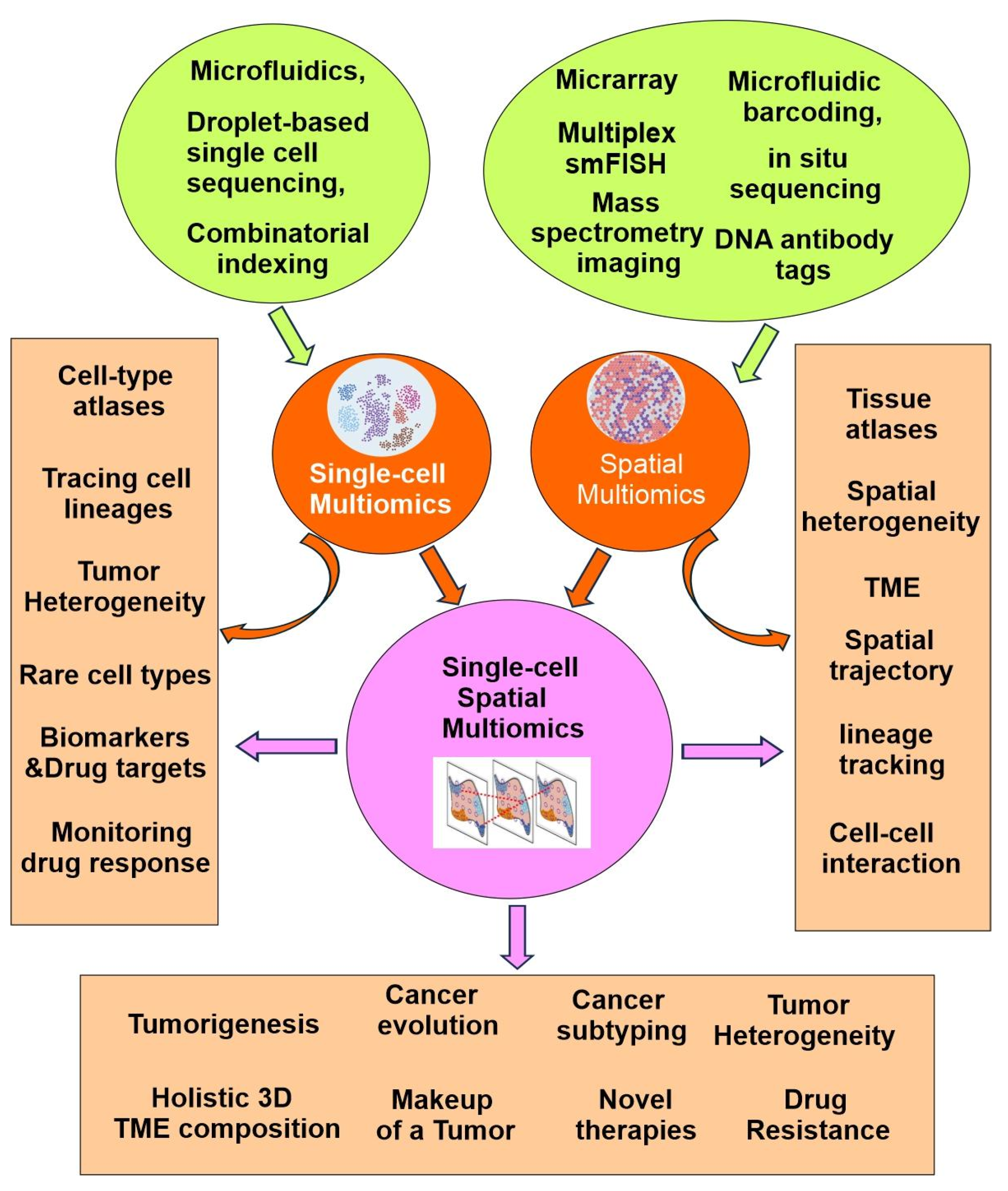
Importantly, the single-cell multiomics approach has revolutionized our ability to dissect cellular mechanisms by allowing for the concurrent measurement of multiple biomolecular layers from the same cell. This integrative perspective is particularly valuable for understanding cellular heterogeneity in complex tissues, disease microenvironments, and developmental processes. As a result, researchers are now able to trace lineage relationships, map cell fate decisions, and identify novel biomarkers with greater precision than ever before (
Figure 3) [
6,
7].
2.1.1. Technological Advancements in Single-Cell Multiomics
Single-cell multimodal omics techniques allow for the simultaneous analysis of genomics, transcriptomics, epitranscriptomics, epigenomics, proteomics, and metabolomics in individual cells, making them valuable for studying complex cellular processes. A more comprehensive understanding of cellular function and regulation can be achieved by integrating multimodal information [
6,
7].
Recent advancements in single-cell multiomics have been driven by the development of high-throughput platforms and innovative analytical methods that allow simultaneous measurement of multiple molecular modalities. Technologies such as microfluidics, droplet-based sequencing, and combinatorial indexing have greatly increased the scale and accuracy of single-cell analyses (
Figure 3). These innovations have not only expanded the capabilities of researchers to interrogate cellular complexity, but have also facilitated the integration of transcriptomic, genomic, epigenomic, and proteomic data within individual cells, paving the way for more holistic and nuanced biological insights.
Single-cell sequencing was named ‘Method of the Year’ in 2013 for its accessibility and versatility. Recent scRNA-seq techniques are vital for analysing intercellular variation at scale. Multiomics technologies expand on this by integrating transcriptomic data with other types, boosting throughput via cell multiplexing, tagging, and hashing.
Simultaneous analysis of the genome and transcriptome can directly identify alterations in genetic material since the transcriptome is the product of the genome via transcription. We can gain valuable information by monitoring mutations and sequence specificity during the transcription of DNA sequences to RNA sequences, which helps to uncover changes in cellular phenotype. The initial methods of this kind were gDNA-mRNA sequencing (DR-seq) and genome and transcriptome sequencing (G&T-seq). In DR-seq, preamplified nucleic acids from a single cell are divided into RNA and DNA and sequenced. Recently developed methods include simultaneous isolation of genomic DNA and total RNA (SIDR-seq) [
8], TARGET-seq [
9], direct nuclear tagmentation and RNA sequencing (DNTR-seq) [
10], and scONE-seq [
11].
Concurrent examination of the transcriptome and methylome provides key insights into how DNA methylation influences transcription in heterogeneous cell populations. The current methods include single-cell genome-wide methylome and transcriptome sequencing (scM&T-seq) [
12], scMT-seq [
13], and SMART-RRBS62 [
14].
Simultaneous examination of the epigenome and transcriptome within a single cell enables analysis of how epigenetic regulation relates to gene activity in single-cells, offering greater insight into cellular diversity and regulatory patterns. Current methods include sci-CAR [
15], scCAT-seq [
16], SNARE-seq [
17], Paired-seq [
18], SHARE-seq [
19], and ISSAAC-seq [
20].
Proteins are central to cellular structure and biochemical activity, acting as enzymes. Characterizing their post-translational modifications and interactions at the single-cell level is crucial. While several methods have been employed for this purpose, a significant advancement in co-profiling the transcriptome and proteome by high throughput was established in 2017, through cellular indexing of transcriptomes and epitopes by sequencing (CITE-seq). This method enables the integration of multiplexed protein marker detection with transcriptome profiling across thousands of single-cells [
21]. This was followed by the development of RNA expression and protein sequencing assay (REAP-seq)[
22] and SCITO-seq [
23].
Single Nuclei RNA-Seq (snRNA-Seq)
While scRNA-seq offers valuable insights, it has limitations. Firstly, it requires tissues to be processed into single-cell suspensions, a step involving enzymatic incubation at high temperatures that can cause artifacts and noise, detectable only after sequencing. Additionally, this process may favour easily dissociable cells, leading to biased cellular representation.
Single nuclei RNA-seq (snRNA-seq) addresses these issues by profiling gene expression from isolated nuclei, making it suitable for archived or hard-to-dissociate tissues. This method reduces bias in cell type isolation and better reveals the cellular basis of disease, enabling identification of otherwise difficult-to-isolate cell types.
In 2019, Wu et al. conducted a genomic study of the kidney, comparing scRNA-seq and snRNA-seq methods. Their results indicated that snRNA-seq achieves a comparable gene detection rate to scRNA-seq in adult kidney tissue, while also offering advantages such as compatibility with frozen samples and reduced dissociation bias. That same year, Joshi et al. applied snRNA-seq in a human lung biology study and observed that this approach enabled the identification of cell types from both frozen healthy and fibrotic lung tissues without bias [
24]. Sequencing adult mammalian heart tissue is challenging due to difficulties in tissue dissociation without cellular damage. Nevertheless, in 2020, researchers in Germany reported sequencing an adult mammalian heart using snRNA-seq and provided data on cell-type distributions within the tissue [
25].
2.1.2. Opportunities Provided by Single-Cell Multiomics
Single-cell multiomics is an emerging tool in molecular and cell biology that offers detailed insights into complex cellular environments. With the maturation of the technology and the increase in number of profiled cells, single-cell multiomics has empowered the identification of previously unknown rare cell types, the elucidation of cellular compositions, the characterization of cellular interactions in complex tissues, and the expansion of single-cell atlases for both diseased and healthy human tissues. The Human Cell Atlas (HCA) project seeks to profile all human cells in order to construct a comprehensive reference map. Since its launch, the HCA has assembled single-cell atlases at a large scale. The data collected by the project includes the fluxome, genome, metabolome, proteome, and transcriptome. Overall, the advent of single-cell multiomics has revolutionized the field of precision oncology, providing novel strategies for cancer management (
Figure 3).
2.1.2.1. Tracing Cell Lineages
Single-cell multiomics is mainly used to construct cellular lineage trees that track disease evolution. These trees help identify new cell types, trace cell lineages, and find biomolecular markers by thoroughly profiling cells at various developmental stages [
6].
Single-cell multiomics allow for the simultaneous collection of information regarding genomic copy number variations, the DNA methylome, nucleosome occupancy and the transcriptome of single-cells, which can reveal new cell types and their roles in a studied lineage. Profiling transcriptomes alongside chromatin accessibility, DNA methylation, histone modifications, and nucleosome organization offers new insights into cell identity and epigenetic processes in lineage priming [
26]. Integrating epigenome and transcriptome data from single-cells helps to reveal how DNA modifications drive cell differentiation. Single-cell proteomics methods analyse lineage-specific transcription factors and their abundance over time, which contributes to our understanding of how protein levels change as cells differentiate and ultimately leads to the maintenance or emergence of a lineage trajectory [
27].
Single-cell multiomics has had a large impact on cell lineage classification for cancer and our understanding of evolution of tumor cell states and types. The integration of genome, transcriptome, and lineage reporter techniques facilitates lineage tracing in cancer research. Insights into the persistence of epigenetic states and genetic mutations may contribute to the informed development of new therapies. Recent studies show that single-cell lineage analysis helps explain drug resistance in glioblastoma [
28] and clarifies which chronic lymphocytic leukemia lineages respond to treatment using combined transcriptome and methylome data [
29]. Overall, single-cell multiomics has greatly advanced disease lineage classification, tumor identification, and our understanding of cell state evolution.
2.1.2.2. Production of Cell-Type Atlases of Various Organs
Single-cell multiomics datasets grow more complex with additional samples, conditions, and acquisition methods. Integration methods aim to reduce batch effects while preserving biological variation. The Cancer Genome Atlas (TCGA) provides multiomics data focused on cancer, including over 20,000 primary cancer samples and their matched normal counterparts from 33 cancer types. This dataset includes genomic, epigenomic, transcriptomic, and proteomic information. TCGA is the largest repository of cancer multiomics data and is widely used in scientific research. The role of TCGA in supporting different areas of cancer research, including pan-cancer studies, has been reviewed in previous sections.
2.1.2.3. Tumor Heterogeneity, Immunology, and Genetics
Single-cell multiomics technologies have added unprecedented breadth and depth into cancer research. Significant comprehensive and transformative knowledge are generated in immuno-oncology research. Single-cell multiomics helps researchers to define tumour and immune cell states and the interplay between them, identify predictive biomarkers of treatment response, infer the complex nature of antigen–immune receptor dynamics, and guide the development of therapeutics for multiple cancer types.
Integration Analysis of Single-Cell Multiomics reveals prostate cancer heterogeneity [
30]. This study integrates single-cell RNA sequencing, spatial transcriptomics, and bulk ATAC-sequencing data obtained from a cohort of prostate cancer patients and healthy controls. In summary, the cellular heterogeneity is delineated in the stage-specific prostate cancer microenvironment at single-cell resolution, uncovering their reciprocal crosstalk with disease progression, which can be helpful in promoting prostate cancer diagnosis and therapy.
Single-cell multiomics uncover intra-cell-line heterogeneity across human cancer cell lines [
31]. This study conducted single-cell RNA-seq on 42 human cell lines and ATAC-seq on 39 lines to demonstrate transcriptomic and epigenetic heterogeneity within each line. This study conducts single-cell multiomics analysis of widely used human cancer cell lines, providing information about intra-cell-line heterogeneity and its dynamics that may be useful for future research involving cancer cell lines.
Single-cell multiomics with clonal resolution reveals differentiation pathways in acute myeloid leukemia [
32]. Inter-patient variability and the similarity of healthy and leukemic stem cells (LSCs) have impeded the characterization of LSCs in acute myeloid leukemia (AML) and their differentiation landscape. The study presents CloneTracer, a new method that provides clonal resolution for single-cell RNA-seq data. In 19 AML patient samples, CloneTracer identified leukemic differentiation pathways. Taken together, CloneTracer reveals a differentiation landscape that mimics its healthy counterpart and may determine biology and therapy response in AML.
Single-cell multiomics is also employed to characterize the cancer immunosenescence landscape, which shows that patients exhibiting higher levels of immunosenescence signature have poorer prognoses.
Single-cell multiomics sequencing facilitates complementary therapeutic strategies by identifying region-specific characteristics of glioblastoma [
33]. In this study, paired tissues from the tumor core (TC) and peritumoral brain (PTB) were collected for integrated snRNA-seq and snATAC-seq analyses. The findings indicate molecular changes in infiltrated GBM cells and demonstrate the potential for combination therapy targeting intratumor heterogeneity both within and beyond the GBM region.
Single-cell multiomics identifies chronic inflammation as a driver of TP53-mutant leukemic evolution [
34]. In this study an allelic-resolution single-cell multiomic analysis was performed in hematopoietic stem and progenitor cells from individuals with myeloproliferative neoplasms who progressed to TP53-mutant secondary acute myeloid leukemia. This study reveals a previously unknown effect of chronic inflammation, supporting improved risk assessment, early detection, and treatment strategies for TP53-mutant leukemia, with implications for other cancers.
Single-cell multiomics reveals that FABP1 + renal cell carcinoma drive tumor angiogenesis through the PLG-PLAT axis under fatty acid reprogramming [
35].
In another study, a barcode-shared transcriptome and chromatin accessibility map of 117,911 human lung cells from age/sex-matched ever- and never-smokers were developed to profile context-specific gene regulation. The finding indicates a context-dependent function for susceptibility genes [
36].
A single-cell multiomics atlas from 695,819 pre-infusion CAR T cells was examined to investigate the molecular determinants of ultralong CAR T cell persistence. The results reveal key mediators of lasting CAR T therapy response and indicate that enhancing type 2 functionality in CAR T cells may help maintain long-term remission [
37].
These methods have also been used to study immune-checkpoint blockade (ICB) therapies for human cancer. A study analyzing published single-cell data found that CXCL13+CD8+ T cells are associated with better ICB responses across tumor types [
38].
2.2. Spatial-Multiomics
Although single-cell multiomics has provided valuable insights into cellular heterogeneity, it lacks spatial context. Single-cell multiomics methods require cell dissociation, resulting in loss of information about cellular physical interactions. This spatial context is essential to many biological processes. Spatial multiomics overcomes this limitation by enabling the precise localization and molecular characterization of individual cells within their tissue environments [
39]. The advancements demonstrated by these innovative techniques are expected to build upon—and potentially surpass—the considerable progress achieved through dissociated single-cell approaches (
Figure 3) [
6,
7,
40].
2.2.1. Technological Advancements in Spatial Multiomics
Methods for spatial mono-omics including spatial transcriptomics, epigenomics, proteomics and metabolomics have progressed tremendously in the last decade. Single-cell multiomics provides data about gene regulation across different omics layers but does not offer the spatial information needed to analyze cellular functions within tissues. Now, the emerging trend is to integrate spatial mono-omics methods to perform spatial multiomics. Spatial multiomics facilitates the concurrent analysis of various data modalities—including transcriptomics, proteomics, genomics, epigenomics, and metabolomics—within a single tissue section (Liu, 2024).
Most spatial multiomics techniques build upon existing mono-omics methods, such as array-based spatial transcriptomics, microfluidic barcoding, DNA antibody tags, multiplex smFISH, in situ sequencing, and mass spectrometry imaging (
Figure 3) [
40]. These approaches can be applied independently to adjacent tissue sections, sequentially or concurrently on the same section, depending on analyte quality and compatibility. The number of analytes analyzed across molecular levels varies by method. Spatial multiomics is often complemented by histological stains like H&E for additional morphological context.
Integrating multiomics data remains technically challenging, requiring advanced computational and statistical tools. Interpretation is further complicated by environmental variability and technical noise, making the development of robust analytical methods for large-scale datasets crucial to fully realize the potential of spatial multiomics.
2.2.2. Applications of Spatial-Multiomics
Spatial multiomics advances precision oncology by providing detailed insights into tumor cell composition and tissue architecture. It also reveals cell-cell interactions and provides key insights into the spatial organization of the TME. Spatial multiomics is able to identify key cell-cell signaling pathways that drive tumor progression and affect treatment response. As a results, spatial multiomics has broad applications, including spatial-based heterogeneity in cancers, spatial-related crosstalk in tumor immunology, spatial trajectory and lineage tracking of tumor cells, biomarker discovery, disease mechanisms, drug target identification, and the development of novel therapies (
Figure 3) [
41].
Recently, various spatial multiomics methods have been employed in precision oncology. For example, spatial transcriptomics, metabolomics, and proteomics were integrated to analyze glioblastoma and demonstrated bidirectional tumor-host interdependence. Notably, they revealed that hypoxia significantly affects glioma architecture and induces chromosomal rearrangements [
42]. Another study uses digital spatial profiling (DSP) technology to quantitate transcript and protein abundance in spatially distinct regions of metastatic prostate cancer. It shows that DSP is a great technology which can accurately classify tumor phenotype, assess tumor heterogeneity, and identify aspects of tumor biology involving the immunological composition of metastases [
43]. Another spatial multiomics study reveals the impact of tumor ecosystem heterogeneity on immunotherapy efficacy in patients with advanced non-small cell lung cancer treated with a bispecific antibody [
44]. Spatial multiomics has also been used to map immune activity in HPV-negative head and neck squamous cell carcinoma. The study evaluates intertumor heterogeneity using a 27-gene expression signature to stratify tumors by their immunologic activity status. This study shows that gene expression and cell colocalization signatures can predict immunological activity and immunotherapy response in HNSCC [
45]. Through spatial multiomics, it is revealed that SPP1+ fibroblasts play a pivotal role in determining metabolic heterogeneity and promoting metastatic growth of colorectal cancer liver metastasis [
46]. A comprehensive spatial multiomics strategy involving imaging mass cytometry (IMC), spatial proteomics, single-nucleus RNA-seq (snRNA-seq) and multiplex immunofluorescence have been developed for profiling breast cancer oligo-recurrent lung metastasis. This comprehensive analysis facilitates the development of therapeutic options to treat lung metastasis from breast cancer [
47]. Spatial multiomics is also used to analyze tumor-stroma boundary cell features to predict breast cancer progression and therapy response [
48].
Combined imaging-based spatial metabolomics and lipidomics with microarray-based spatial transcriptomics are employed to visualize intratumor metabolic heterogeneity in gastric cancer. This study provides a highly integrated picture of intratumor heterogeneity and reveals unique transcriptional features and significant immune-metabolic changes [
49]. Spatial multiomics has also been used to investigate the spatial distribution of intratumoral microbiota in breast cancer and their interactions with the local TME. The data revealed some novel roles of microbiota in breast cancer and identified potential therapeutic targets [
50].
2.3. Single-Cell-Spatial Multiomics and Human Tumor Atlas Network (HTAN)
As discussed above, both single-cell multiomics and spatial multiomics have its unique advantage and limitations. To maximize the advantages and overcome the limitations, single-cell spatial multiomics have emerged as the most powerful tool to reveal the molecular profiles of both normal and cancer cells/tissues in a temporal-spatial dynamic way. Integrating spatial multiomic data with single-cell multiomic data opens possibilities to add anatomical dimensions to existing datasets and to better understand cell-type-specific molecular profiles in humans (
Figure 3).
Single-cell spatial multiomics were initially developed as single-cell spatial transcriptomics by combining single-cell RNAseq with spatial transcriptomics. With the inclusion of more and more other single-cell mono-omics and spatial mono-omics, it truly becomes single-cell spatial multiomics. However, currently, based on the purpose of the study, most studies only combine select single-cell mono-omics (such as single-cell transcriptomic, single-cell proteomics, single-cell epigenomics etc.) with select spatial mono omics (such as spatial transcriptomics, spatial proteomics, and spatial epigenomics etc.).
Single-cell spatial multiomics-based international initiatives have emerged to facilitate the advancement and application of precision oncology. The Human Tumor Atlas Network (HTAN) is a prominent representative. HTAN leverages scientific collaboration to integrate samples, analytical modalities, and tools into detailed atlases of tumor evolution. HTAN offers a multidimensional view of cancer biology by expanding our spatial understanding of molecular, cellular and tissue features, which greatly helps the advancement of precision oncology.
Since 2018, HTAN researchers have gathered single-cell spatial multiomics data and used advanced analytical methods to better understand tumor ecosystems across various organs and types. This project demonstrates how spatial and single-cell data advances knowledge of cancer progression and supports the discovery of new tumorigenesis mechanisms. Following are some important contributions from the HTAN researchers, as well as from the broad scientific community (
Figure 3).
2.3.1. Tumor Evolution and Microenvironment Interactions in 2D and 3D Space
By using spatially resolved single-cell genomics, transcriptomics and proteomics
, a comprehensive study characterized 131 tumour spatial transcriptomics sections across 6 different cancers: uterine corpus endometrial carcinoma, cholangiocarcinoma, pancreatic ductal adenocarcinoma, colorectal carcinoma, breast cancer, and pancreatic ductal adenocarcinoma. The findings from this research have made significant contributions to the understanding of spatial tumour evolution through interactions with the local microenvironment in 2D and 3D space, providing valuable insights into tumour biology [
51].
2.3.2. Temporal Recording of Development and Precancer
Lineage tracing methods based on CRISPR evolving barcodes are utilized in studies of mouse development and mouse models of colorectal cancer. The findings reveal the polyclonal make-up of early cancers and their decreasing clonal diversity during the transition to advanced cancers. This result was also observed in human colorectal cancer samples at various stages of progression [
52].
2.3.3. Molecular Pathways Associated with Early Tumorigenesis in Familial Adenomatous Polyposis (FAP)
Single-cell spatial multiomics, including transcriptomic, proteomic, metabolomic and lipidomic, were integrated to profile 93 samples, consisting of normal mucosa, benign polyps, or dysplastic polyps, from six persons with FAP. The results generated by this research reveal key genomic, molecular, and cellular events during the earliest steps in colorectal cancer formation and potential mechanisms of pharmaceutical prophylaxis [
53].
Besides HTAN associated studies, single-cell spatial multiomics has been employed by the scientific community to study various aspects of many cancer types.
2.3.4. Cancer Subtype Stratification
Single-cell spatial multiomics has been instrumental in cancer subtype stratification. The spatial immunophenotypes were assigned in TNBC by integrating spatial phenotypes and immunity effectors with multiplexed immunofluorescent imaging, scRNA-seq and TCR repertoire analysis, which helped to elucidate T cell evasion pathways in response to ICB [
54]. By integrating data generated with scRNA-seq and spatial transcriptomics sequencing, as well as bulk RNA sequencing, proteomic analysis, and genome sequencing, a recent study reveals novel subtypes of hepatocellular carcinoma [
55].
2.3.5. Cancer-Associated Fibroblasts (CAF)
It is recognized that CAF plays an important role in cancer development, and single-cell spatial multiomics has been used to study CAF. Through integrative analyses of over 14 million cells from 10 cancer types across 7 spatial transcriptomics and proteomics platforms, a recent study validates and characterizes four distinct spatial CAF subtypes, which facilitates novel approaches to target and modulate CAFs [
56]. Integrating spatial and single-cell transcriptomes reveals the role of COL1A2(+) MMP1(+/-) cancer-associated fibroblasts in ER-positive breast cancer [
57].
2.3.6. Tumor Heterogeneity and Holistic TME Cellular Components
While tumor heterogeneity and TME cellular components have been studied by single-cell omics and spatial omics. Single-cell spatial omics allows for a deeper and broader understanding.
An integrated single-cell spatial multiomics landscape of WHO grade 2-4 diffuse gliomas has revealed locoregional metabolomic regulators of glioma growth [
58]. A high-throughput single-nucleus snRNA-seq and snATAC-seq multiomic dataset from matching "core" and "margin" dissections in four distinct grade 4 High-Grade Gliomas (HGG) patients are combined with new spatial transcriptomics data from two additional HGG samples to evaluate "core-to-margin" transition, which provides insights into the residual disease biology of tumors and the microenvironment at the infiltrative margin [
59]. By integrating 12 spatial and single-cell technologies, a recent study characterized tumor neighborhoods and cellular interactions in three skin cancer types [
60]. In neuroblastoma, single-cell multiomics from a mouse spontaneous tumor model and spatial transcriptomics from human patient samples are used to dissect the transcriptional and epigenetic landscapes governing developmental states and demonstrates tumour developmental plasticity [
61].
Multimodal single-cell-resolved spatial proteomics has been employed to reveal pancreatic tumor heterogeneity [
62]. Single-cell spatial multiomics has been used in several studies to gain insights into deadly pancreatic cancers. For example, immune dysfunction in pancreatic cancer has been analyzed by single-cell spatial multiomics, which reveals novel mechanisms underlying disease development [
63].
2.4. Patient-Derived Tumor Organoids (PDTO)
The identification of features specific to each patient and tumor is central to the development of precision medicine and preclinical studies for cancer treatment. However, cancer is associated with a high degree of inter- and intra-tumor heterogeneity, which leads to considerable variability in clinical response to common treatments across patients. This heterogeneity has hindered precision cancer treatments until the emergence of PDTOs. PDTOs stably recapitulate the structures, specific functions, molecular characteristics, genomics alterations, and expression profiles of primary tumors, as well as permit genomic and environmental manipulation. PDTOs are an indispensable tool in precision oncology to mimic illnesses, explore mechanisms, identify innovative therapeutic targets, screen and assess novel drugs in a high-throughput manner, and customize treatment regimens for individual cancer patients [
64]
-[
68].
2.4.1. A Brief History
An organoid is a three-dimensional structure created in vitro that replicates key functional, structural, and biological characteristics of an organ in a simplified and smaller form. Organoids are derived from either pluripotent or tissue-resident stem (embryonic or adult) or progenitor or differentiated cells from healthy or diseased tissues, such as tumours [
69].
It was proposed over a century ago that complex tissue/organ structures could be recreated in vitro through self-organization and regeneration and could be utilized to recapitulate parts of complete tissues or organs. The notable plasticity of embryonic tissue was initially suggested by observations of cell dissociation and subsequent reaggregation in vertebrates in the mid-20th-century. Scientists have sought to maintain or recreate tissue/organ complexity through various three-dimensional (3D) cell culture approaches. The spheroid model was proposed in the early 1970s by radiobiologists [
70]. These compact spherical structures, typically over 1 mm in size, are mainly derived from immortalized cell lines. In 1987, the optimization of cell culture conditions enabled mammary epithelial cells to assemble into 3D spheroids and ducts [
71]. In 1998, human pluripotent stem cells (hPSCs) were successfully extracted from human blastocysts, opening the door for the development of regenerative medicine [
72]. In the early years of the 21st century, iPSCs were successfully generated through the reprogramming of mouse and human fibroblasts. iPSCs are similar to embryonic stem cells. Pluripotent stem cells serve as organ progenitors capable of differentiating into various cell types in culture, which has greatly advanced the development of three-dimensional organoid models [
73].
Over the past decade, PDTOs have contributed to developments in 3D culture in precision oncology research. In 2009, it was shown that an adult intestinal stem cell expressing the LGR5 receptor, isolated from mice, could be cultured to form structures and cellular diversity resembling the crypts and villi of the intestinal epithelium [
74]. Organotypic cultures have since been created from various primary tumors and have shown to better mimic original tumor features than traditional cell lines. An effective PDTO can grow, store, and freeze cells that maintain the genetic and histological features of the original tumour. In addition, PDTOs are amenable to modelling TME cell heterogeneity and heterotypic cell interactions through co-culture with non-neoplastic cell types, including cancer-associated fibroblasts (CAFs) and various immune-cell types. As a result, PDTOs demonstrate utility in various aspects of cancer research, including cancer therapies, disease progression and tumour niche factor requirements [
67].
2.4.2. Application of PDTOs
2.4.2.1. Cancer Biology
Organoids including PDTOs are increasingly being used to understand cancer biology. Organoids have been used to model the stages of tumorigenesis in various types of tumors. The formation of organoid from cells can be evaluated to reveal different stages of tumor evolution. Observing this process shows that inactivating tumor suppressor genes (such as TP53, PTEN, or APC) and activating oncogenes (such as KRAS) are keys to tumor formation. Studying the shift from healthy to tumor organoids helps clarify the molecular basis of tumor initiation and may reveal novel biomarkers for early cancer diagnosis, advancing precision oncology [
67]. Tumor organoid models may also be relevant for mimicking the genomic evolution of tumors, as shown by a recent study in bladder cancer [
75].
Mechanisms underlying drug resistance are dynamic and sequential, including irreversible mutational changes, epigenetic changes, metabolic reprogramming, modification of the tumor microenvironment, and epithelial–mesenchymal transition. These changes are difficult to observe in patients or animal models. Organoids have shown potential to recapitulate the clinical response of the original tumor and thus could be used to track the sequence of resistance acquisition and identify the involved mechanisms in a reproducible and more relevant manner. Furthermore, combined with imaging techniques, the different responses of cells within the PDTO can be analyzed separately to overcome the challenges imposed by cell heterogeneity.
Recently, researchers have used molecular comparisons between PDTOs from chemotherapy-treated patients and those from untreated tumors to find targetable signaling pathways [
76]. Another method is growing tumor organoids from chemotherapy-treated PDXs in mice to measure parameters not assessable in vivo [
77]. Organoids have also been used to model acquired resistance in pancreatic cancer [
78].
In recent years, a three-dimensional (3D) organoid culture of human tumour tissue has gained recognition as a cost-effective and representative platform for modelling cancer heterogeneity and tumour microenvironment interactions in vitro.
Organoid models from human tumors capture both intra- and intertumoral diversity, reflecting the (epi)genetic and phenotypic variation among neoplastic cell subclones and their tumor-specific morphology. Studies have modeled patient-to-patient heterogeneity by creating ‘living biobanks’ of organoids derived from cancer tissues. Pancreatic cancer organoids from a genetically and phenotypically comprehensive cohort of 138 patient tumor samples have been established, which revealed population-level genetic and transcriptomic signatures associated with anticancer drug responses [
79]. A biobank consisting of 55 colorectal cancer organoid lines was established, representing a range of tumor phenotypes, including both primary and metastatic lesions [
80].
Cancer organoids also enable modelling of TME heterogeneity, including the presence and functions of non-neoplastic TME cells, the signalling of niche-specific soluble factors and the altered composition of the extracellular matrix (ECM). Recent studies have aimed to create culture platforms that better reflect TME cell diversity and their interactions. It is shown that native CAFs and immune cell types could be retained in PDTOs to test personalized immunotherapies [
81]. The authors recreated the in vivo tumor-infiltrating T-cell repertoire and modelled patient-specific PD1/PDL1-dependent immune suppression. Schmalzier et al. also introduced a platform to evaluate cancer immunotherapies using human CAR-engineered natural killer cells targeted at patient-derived CRC organoids [
82].
2.4.2.2. Clinical Application
Organoids offer multifold potential applications, including high-throughput screening of anti-cancer drugs, evaluation of drug toxicity and side effects, identification of therapeutic targets and drug candidates, predicting drug sensitivity, customized therapy in clinical settings, emulation of pathological processes for disease modeling, as well as enhance fundamental research through CRISPR-Cas9 gene editing [
65]
A major clinical application of PDTOs is drug screening. The PDTO model allows for high-throughput screening of therapeutic options, making it possible to identify tumor subtypes that could preferentially benefit patients. Tumor organoids derived from rectal cancer patients have been used to conduct drug sensitivity tests. These findings were used to guide patient treatment with a success rate of 88% in terms of effectiveness [
83]. Another study utilizes lung cancer organoids for high-throughput drug screening and prediction of drug response, which could potentially facilitate personalized cancer treatment strategies [
84]. Through high-throughput drug screening, a study evaluated 76 drugs across 30 PDOs obtained from pancreatic tumors and showed the potential of the PRMT5 inhibitor EZP015556 in inhibiting MTAP-negative tumors. Moreover, the generated data base was used for screening addition drug candidates [
85]. Another organoid platform was developed for high-throughput screening of 2,427 drugs to test their sensitivity colorectal cancer [
86]. Panels of PDTOs from various tumor types have been used to screen therapeutic molecules. In gastric cancer, nine PDTOs were exposed to 37 clinical and developmental compounds, confirming their responsiveness to existing targeted therapies [
87]. Similarly, colorectal cancer-derived PDTOs were screened with 83 molecules, highlighting links between drug efficacy and specific genetic alterations [
67]. By recapitulating tumor heterogeneity and imitating the characteristics of the original tumor, the PDTO model allows for high-throughput screening of numerous emerging therapeutic options.
PDTO panels are utilized to identify predictive molecular signatures—including genomic, transcriptomic, and proteomic markers—associated with treatment responses. Increasing evidence demonstrates that PDTOs can accurately forecast the responsiveness of their source tumors to anticancer therapies [
88].
2.4.3. Challenges and Limitations
Despite the rapid development and wide application and unique ability to address difficult questions facing precision oncology, current PTDOs have several limitations and challenges. The experimental protocols are still too complicated, which hinders the timely delivery of reliable data to the clinicians for optimal clinical management. Organoid creation and maintenance are expensive, raising concerns about cost. Tumor tissues are complex and varied, but current organoids do not fully reflect this diversity in vitro. Success rates for generating cancer organoids differ widely across tumor types. Despite improvements in protocols, techniques remain variable and difficult to reproduce due to non-standardized tissue sources, processing methods, media, and matrices [
64,
65,
67].
Moving forward, the emerging trend is to develop more complex models that recapitulate in vivo structure and function as faithfully as possible and enhance its application value in clinical treatment and drug development. Tumor organoids can be co-cultured with non-tumor cells or iPSC-derived organoids, which enables the investigation TME and the effects of immune cells in the absence of an immune system. Moreover, organoids can be integrated with advanced technologies such as 3D printing and organ chips to create engineered organs.
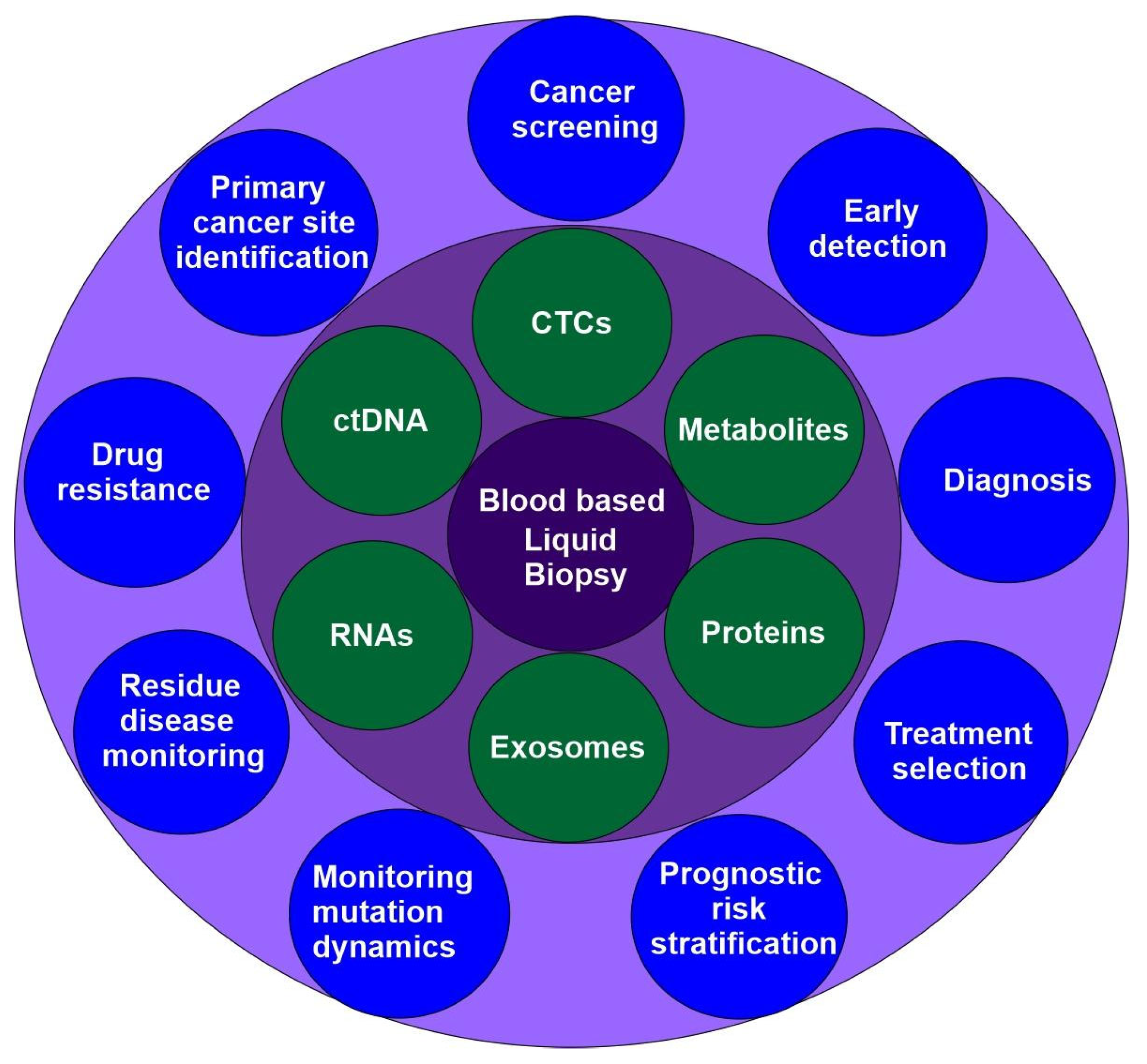
2.5. Liquid Biopsy
Liquid biopsy is an emerging precision medicine method that examines blood and other body fluids for insights into a patient’s health. It is a non-invasive technique for identifying and analyzing biomarkers such as circulating tumor cells (CTCs), cell-free DNA (cfDNA), circulating carcinoma proteins, circulating miRNAs, and exosomes. It allows for real-time monitoring of a patient’s cancer mutations and genomic profile. Liquid biopsies are quicker, safer, and more practical than conventional tissue biopsies, and they also allow for serial samples to monitor tumor evolution over time (
Figure 4) [
89,
90]. Although liquid biopsy has the potential to disrupt the field of medical diagnosis, it is met by various challenges such as limited tumor-derived components, less specificity, and inadequate advancement in methods to isolate biomarkers.
Liquid biopsies include both blood-based and non-blood-based methods. Due to its prominence, blood-based biopsies also are referred to as liquid biopsies. Non-blood-based liquid biopsies include urine analysis, breath analysis, and saliva analysis, which were recently reviewed by other articles [
91,
92] and will not be discussed here.
2.5.1. Circulating Tumors Cells (CTCs)
First discovered in 1869 by Thomas Ashworth, CTCs are cancer cells shed into the bloodstream from primary or metastatic tumor sites [
90,
93]. In the last 20 years, CTCs have been detected across a breadth of malignancies of both epithelial and non-epithelial origin including prostate cancer, ovarian cancer, gastric cancer, colorectal cancer, bladder cancer, renal cancer, lung cancer, glioblastoma, melanoma [
94,
95]. CTCs are traditionally characterized as nucleated cells present in a blood sample that exhibits negative staining for the ubiquitous leukocyte marker CD45 while demonstrating positive staining for epithelial cytokeratin.
Analysis of CTCs through liquid biopsy has been used for decades in various cancer types, showing applications in early diagnosis, prognostic risk assessment, disease monitoring, and informing personalized treatment decisions. CTCs are intact tumor cells that originate from primary or metastatic tumors. This characteristic enables CTCs to serve as a source of information at multiple molecular levels, including DNA, RNA, protein, and metabolites. In addition, CTC monitoring uses routine blood draws rather than tissue biopsies, offering a less invasive and more repeatable method for detecting cancer and assessing its progression.
Major challenges are that CTCs exhibit high heterogeneity and have a short half-life of just 1-2.4 hours in circulation, existing at extremely low concentrations in peripheral blood [
90]. It has been estimated that although millions of CTCs are shed daily into the circulation per gram of tumor tissue, CTCs still comprise only a minute fraction of total cells present in blood, with as few as one tumor cell per 10 billion blood cells [
95]. Facing these challenges, the clinical potential of CTC-based diagnosis has not been fully realized due to the limitation of the existing methods and devices to harvest CTCs and their clusters from peripheral blood [
96]. Therefor, the advancement of CTCs in precision oncology is significantly dependent on the advancement of CTC enrichment technology.
All CTC isolation strategies exploit unique properties of CTCs including distinct immunological, molecular, and/or bio-physical properties. These strategies are classified into two main classes: methods that achieve up to 10[
4]-fold CTC enrichment and methods that achieve up to 10[
8]-fold enrichment [
95,
97]. The methods for 10[
4]-fold enrichment include direct visualization of CTCs, CTC capture based on size or physical properties, positive immunoselection of CTCs, and depletion of hematopoietic cells to achieve negative enrichment of CTCs. To achieve10[
8]-fold enrichment, additional purification is required and typically involves labeling residual white blood cells and CTCs using fluorescence-conjugated antibodies, optically identifying CTCs, and sorting them individually. The use of droplet-based single-cell RNA sequencing (scRNA-seq) technologies is another approach [
95,
97].
In addition to CTCs, metastasis is facilitated by dissemination of cell clusters containing CTCs. Some CTCs travel in clusters, ranging from doublets to dozens of cancer cells tethered together. Some clusters may include tumor-derived fibroblasts, blood-derived leukocytes, or other cells. Other methods have also been developed to isolate CTC clusters. For example, negative enrichment of CTC clusters from peripheral blood samples based on the apoptosis resistance of malignant cells of tumorigenic origin and enrichment by immunocytochemistry profiling [
96,
98].
2.5.2. Circulating Tumor DNA (ctDNA)
ctDNA comprises small fragments of DNA that are released by tumor cells into the blood and tissue fluids. The molecular similarities observed between plasma ctDNA and tumor tissue, combined with the practicality of measurement via blood draw, suggest that ctDNA may serve as a biomarker for primary cancer screening. Plasma ctDNA concentration is related to tumor location, size, and disease extent. Detection of ctDNA in liquid biopsy material has gained attention due to recent advancements in DNA technologies.
Half a century ago, scientists realized that plasma levels of free DNA increased in cancer patients [
99]. Specific mutated genes began to be identified in the blood of cancer patients in the form of ctDNA about 20 years ago, including KRAS and PIK3CA in patients with colorectal cancer [
100], EGFR in breast cancer patients [
101] and in NSCLC patients [
101,
102]. Many studies demonstrate that the plasma ctDNA concentration is associated with tumor location, size, and extent of disease [
103]. For example, it is shown that ctDNA positivity is in 42%, 67% and 88% of patients with stage I, II, and III NSCLC, respectively [
104]. In 2014, the European Medicines Agency (EMA) approved the use of ctDNA for detecting EGFR mutations in NSCLC [
105]. ctDNA assay was recommended for cancer patients by the Society for Medical Oncology (ESMO) Precision Medicine Working Group in 2022 [
106].
Different cancers have different patterns of epigenetic characteristics (e.g., nucleosome distribution) and different preferential genomic breakpoints where ctDNA is generated, which forms the basis to predict the types of primary tumors. Although these signatures are not necessarily unique to one sub-type, it is still possible to identify the cancer type by comparing DNA methylation profiles, nucleosome footprints, and genetic alternations of ctDNA with those in the reference databases [
103,
107].
Because ctDNA is highly fragmented and scarce, increasing detection sensitivity remains a key research focus. With the development of second-generation sequencing, it is possible to detect multiple gene variants simultaneously and generate high-throughput data. Currently, ctDNA detection is well-developed and includes two main types: targeted PCR-based methods and nontargeted next-generation sequencing (NGS) techniques.
While ctDNA could be applied to other applications such as monitoring disease progression and evaluating treatment effectiveness, it is mostly used for cancer screening and diagnosis. It was initially used to screen for specific cancer types, and multiple platforms have been on the market including ExoDx prostate Intelliscore and SelectMDx for prostate cancer [
108], Shield [
109], Freenome test, and Epi proColon [
110] for colorectal cancer, Viome CancerDetect for oral and oropharyngeal cancer [
111], and a test for breast cancer [
112].
ctDNA now is heavily explored for multicancer early detection (MCED). With the years several MCED platforms have been developed including CancerSEEK and PANSEER for 8 solid tumors [
113,
114], TEC-seq for 4 solid tumors [
115], OverC for 6 solid tumors [
116], and ARISTOTLE for 10 solid tumors [
117]. The sensitivity of these tests varies between 29% and 98%, while the specificity is close to 100% [
103].
In recent years, more comprehensive studies have been conducted to screen and diagnose more cancers with or without symptoms. In 2023, the first large-scale prospective evaluation of an MCED diagnostic test in a symptomatic population was conducted in England and Wales (SYMPLIFY) [
118]. The study, which included 6,238 participants, assessed the performance of a methylation-based MCED diagnostic test in symptomatic patients referred from primary care. The findings indicate that the current MCED test may identify symptomatic patients for further investigation who do not meet existing referral criteria, pending confirmation in an interventional trial. The test may also have potential use in guiding decisions about which patients may not require additional investigations.
Another study, the NHS-Galleri trial (ISRCTN91431511), aims to establish whether an MCED test that screens asymptomatic individuals for cancer can reduce late-stage cancer incidence. This randomized controlled trial has enrolled over 140,000 individuals without cancer diagnosis or treatment and are not undergoing investigation for suspected cancer in England. The findings may provide valuable insights for determining the appropriateness of implementing the MCED test within population screening programs [
119]. At the same time, another large multi-institutional prospective study in the U.S, PATHFINDER, investigated the feasibility of cancer screening with MCED testing, using next-generation sequencing of cell-free DNA in peripheral blood, with a focus on diagnostic investigations in participants who tested positive for a cancer signal. The study detects cancer-specific methylation patterns from ctDNA in more than 50 distinct cancer type [
120]. This study supports the feasibility of MCED screening for cancer and underscores the need for further research investigating the test’s clinical utility.
2.5.3. Exosomes
Exosomes offer a promising option and can enhance liquid biopsy diagnostics in some cases. Exosomes carry less information than CTCs, but much more information than ctDNAs as they contain DNAs, RNAs, proteins, lipids, and others. Exosomes are secreted by living cells, offering a more representative view of the cellular state than cell-free DNA (ctDNA), which is primarily released by dying cells. The lipid bilayer of exosomes provides a stable environment for the biomolecules they carry, protecting them from degradation and making them reliable diagnostic indicators. The rich chemistry of exosomes offers various therapeutically relevant diagnostic options. There is a possibility that exosomes may be used for cancer screening and early diagnosis because of the information they disclosed about viable tumor cells. A cancer cell can release about 20,000 vesicles in 48 hours. Tumor-related exosomal biomarkers have been studied in cancers such as lung, breast, kidney, prostate, and colorectal cancer [
121].
In order to be used as a biomarker, exosomes must first be separated from the respective biofluid. Many methods have been developed over the years including the conventional methods such Centrifugation-Based Methods, Ultrafiltration Methods, Precipitation Methods, Field Flow Fractionation Methods, Chromatographic Methods, and Affinity Binding-Based methods [
122], as well as newly developed microfluidic technology-based methods. Advances in microfluidic technology enable efficient and portable exosome separation and detection, paving the way for point-of-care applications [
122,
123].
Combining different exosomal components (RNA, proteins, lipids) and integrating them with other liquid biopsy markers (like ctDNA) can improve diagnostic sensitivity and specificity. Mutations in exosomal RNA can complement ctDNA signals, enhancing mutation detection sensitivity. Studies indicate that cfDNA combined with exosomal RNA outperforms cfDNA analysis alone [
124].
2.5.4. Other Biomarkers
Liquid biopsies can also analyze other tumor-derived material like proteins, metabolites, and RNAs.
2.6. Non-Invasive Imaging Methods
Conventional oncology image analysis, utilizing modalities such as ultrasound, X-ray, CT, and MRI, has traditionally depended on manually defined features for the interpretation and evaluation of clinical images. The low precision has impeded the accurate diagnosis of the cancer, leading to more unnecessary biopsies. Recent breakthroughs in oncologic imaging leads to the emerging and development of cancer molecular imaging, which have transformed cancer diagnosis, treatment planning, and monitoring.
2.6.1. Cancer Molecular Imaging
Cancer molecular imaging is the non-invasive visualization of molecular and cellular processes characteristic to neoplasia, such as proliferation, glucose metabolism, and receptor expression. Several molecular imaging modalities are now available, including magnetic resonance, optical, and nuclear imaging [
125]. Cancer molecular imaging is mostly supported by dual-modality imaging, such as PET/CT (commercialized in 2001) and SPECT/CT (commercialized in 2004), which combine anatomical, metabolic, and functional information for more accurate diagnosis. [
126]. Other molecular imaging technologies have also improved significantly, enhancing their capabilities to support precision medicine. For example, MRI is able to generate high-resolution anatomic images of soft tissue. Optical imaging is empowered by the use of bioluminescence, fluorescence, and near-infrared imaging. Ultrasound imaging offers real-time, portable, nonradioactive options [
92,
126].
In recent years, significant novel developments of molecular imaging have been reported including the super-resolution fluorescence microscopy which allows nanoscale visualization of cellular processes, DNA-based point accumulation in nanoscale topography (DNA-PAINT) with sub-20 nm resolution, and photoacoustics that offers the ability to image deep tissues. Moreover, the accumulation of imaging data, coupled with advances in machine learning, has enabled the discovery of hidden biomarkers and quantitative features in cancer molecular images [
126].
RECIST is a system for evaluating tumor response to treatment by measuring changes in lesion size on standard imaging. However, it can be slow and sometimes inaccurate when assessing targeted therapies. Molecular imaging techniques have the potential to overcome this weakness due to its ability to quantitatively assess the response at the cellular, subcellular, or even molecular level [
127].
As precision medicine continues to evolve, the application of molecular imaging will continue to evolve alongside it, encompassing a wider range of clinical and research settings.
2.6.2. Omics Imaging, Radiomics and Imaging Genomics
Due to the widespread availability of omics data and improvements in imaging technologies, integrating biomedical image information with omics data has become feasible. This integration process can reveal the links between the micro-level molecular information generated by various omics with the macro-level structural and functional information provided by biomedical images. This newly emerging interdisciplinary field is named omics imaging.
Omics imaging focuses on integrating omics data (genomics, transcriptomics, proteomics, etc.) with structural, functional, and molecular imaging data. Bridging imaging and omics factors and exploring their connections has the potential to provide important new insights into the phenotypic characteristics and molecular mechanisms of cancer development. These, in turn, will impact the development of new diagnostic, prognostic, therapeutic, and preventive approaches, becoming an important component of precision oncology [
128].
Radiogenomics uses big data to aid cancer diagnosis and treatment decisions, offering insights into tumor biology and identifying key imaging biomarkers. These approaches have been validated in a variety of tumors including glioblastoma, breast cancer, liver cancer, colorectal cancer, gastric cancer, lung cancer, ovarian cancer, prostate cancer, retinoblastoma, head and neck squamous cell cancer [
129].
2.7. AI powered Data Integration, Machine Learning and Deep Learning
The primary objective of precision medicine is to combine substantial amounts of data from various databases into analytic frameworks that support the creation of diagnostic and therapeutic methods that are individualized and context specific. This data is generated by various layers of high-throughput technologies such as multiomics. However, it faces challenges over its dimensionality, interpretability, predictability, and high computational power demand. Integration of AI into precision oncology provides the best solution to overcome these challenges. AI can be used to build analytical models of complex disease to improve diagnostic accuracy, optimizing treatment strategies, and enhancing patient care through personalized interventions and remote monitoring that predict personalized health conditions and outcomes. AI has rapidly emerged as a transformative force in precision oncology and has revolutionized various aspects of cancer care from diagnosis to treatment [
130,
131].
2.7.1. Principles and Workflow
A workflow for data integration by AI modeling in precision medicine include the following steps: A) Selection of the data sources. A wide variety of data sources with diverse features are available for selection. B) Data collection and pre-processing. Different approaches to data collection and pre-processing are needed to deal with the diverse data sources. C) Integration of the diverse and heterogenous data through data processing and modeling. D) Application of the integrated data to precision medicine for diagnosis, treatment strategies, and outcome prediction [
130].
2.7.2. Subtypes of AI in Medicine
AI in medicine manifests in various subtypes, each with unique functionalities.
2.7.2.1. Machine learning
Machine learning is a branch of AI that uses algorithms to mimic human learning. It helps uncover patterns in medical data that may escape experts. Common healthcare algorithms include decision trees, support vector machines, and random forests, which analyse large datasets to predict treatment protocols and outcomes [
131,
132].
2.7.2.2. Deep learning
Deep learning constitutes a branch of machine learning that leverages multilayered neural networks to accomplish tasks including classification, regression, and representation learning. The discipline draws conceptual frameworks from biological neuroscience and focuses on organizing artificial neurons into hierarchical layers, which are "trained" to process information efficiently. Deep learning techniques are particularly effective for analyzing intricate data patterns, such as those found in images, natural language, and genomic sequences. Some common deep learning network architectures include fully connected networks, deep belief networks, recurrent neural networks, convolutional neural networks (CNN). CNN is a powerful deep learning method that enables the precise detection of malignant lesions.
2.7.2.3. Transfer Learning
Transfer learning is a technique in machine learning in which knowledge learned from a task is re-used in order to boost performance on a related task.
2.7.2.4. Natural Language Processing
Natural language processing enables machines to understand and generate human language. It is used to extract information from medical records, summarize patient histories, generate tailored treatment plans, transcribe patient-doctor interactions, and produce medical reports. Much patients’ information is stored in free-text format in electronic health records... Natural language processing techniques can be used to extract information from unstructured clinical notes and social media data, enabling analysis of patient experiences and disease trends [
133].
2.7.2.5. Computer Vision
Computer vision empowers machines to interpret and understand visual information from the world, such as images and videos, which is essential for medical image analysis, detecting abnormalities in X-rays or MRIs, and assisting in surgical procedures.
2.7.3. Application in Precision Oncology
2.7.3.1. Cancer detection
AI has been applied for the detection of almost all types of cancers including breast cancer, lung cancer, skin cancer, colorectal cancer, and prostate cancer.
AI-based tools for detecting breast cancer via mammography represent a rapidly advancing field, with many systems progressing toward real-world clinical application [
134]. Several AI products have received FDA clearance for assisting radiologists with the detection of breast cancer from mammograms, as well as in interpreting MRI and breast ultrasound examinations. Ongoing prospective studies are being conducted to assess these products within clinical settings. A recent clinical study in Sweden demonstrated that integrating AI into mammography screening workflows significantly decreased radiologists’ workload—by approximately 44%—without compromising diagnostic performance [
135]. The application of AI to predict future breast cancer risk is also explored by several studies and these AI risk prediction algorithms have been shown to outperform traditional risk models [
136]
-[
138].
Similar studies have applied deep learning to colonoscopy images and video for colorectal cancer screening and reported increased detection rate [
139]
-[
141]. AI has also been used to localize lung nodules for purpose to predict lung cancer risk [
142,
143] and to predict prostate cancer risk [
144,
145]. Advanced deep learning models have been developed for skin-cancer detection [
146].
2.7.3.2. Cancer treatment
AI algorithms are also being developed to improve treatment, including designing personalized treatments and monitoring treatment efficacy. For example, AI is used to predict the response to neoadjuvant chemotherapy in TNBC [
147] and in predicting the prognosis for breast cancer [
148] and colorectal cancer [
149].
2.7.3.3. Cancer biology
AI has been used for the interpretation of germline and somatic mutations observed in cancer. For example, deep learning was employed in a recent study to detect pathogenic germline variant in prostate cancer and melanoma [
150]. Various deep learning-based model have been used in recent research to identify driver genes and pathogenic variants. Researchers have developed a deep learning tool called Dig, which models mutation rates across the genome with high resolution. Applied to data from 37 different cancer types, this approach has proven more effective than several existing methods in pinpointing likely driver mutations, showing both higher sensitivity and accuracy [
151]. AlphaMissense, an AI tool developed using advancements from AlphaFold, has recently been used to assess missense mutations, suggesting that nearly one-third of all such protein variants could be disease-causing [
152]. Additionally, CancerVar, another deep learning-based platform, has been developed to predict the oncogenicity of somatic variants using both functional and clinical features [
153].
Multiple AI methods have developed cell-of-origin prediction, which is particularly relevant for cancers of an unknown primary. These AI models are based on various omics such as genomics [
154,
155], transcriptomics [
156], and proteomics [
157]. The OncoNPC model, trained using sequencing data from tens of thousands of tumor samples spanning over 20 cancer types, has demonstrated strong predictive power. When assessed on cancers of unknown origin, it successfully identified likely primary sites in about 41% of cases. It also identifies subgroups with significantly higher polygenic germline risk for the predicted cancer types [
155]. Another study developed a deep neural network model to classify cancers based on gene expression data. It analyzed transcriptomics data from 37 cancer types provided by TCGA to identify cancer tissue-of-origin specific gene expression signatures [
156]. Cross-protein transfer learning substantially improved disease variant prediction in a recent study [
157]. In this study, cross-protein transfer models were trained using deep mutational scanning data from only five proteins and achieved state-of-the-art performance on clinical variant interpretation for unseen proteins across the human proteome.
Various AI algorithms have also been established for detecting cancer specific neoantigens [
158,
159] and associated T-cell receptors [
160,
161]. Deep learning on pathology images are also used to analyze spatial organization and molecular correlation of tumor-infiltrating lymphocytes to better understand TME [
162].
Various AI models have also been developed for the purpose of cancer subclassification. For example, a comprehensive deep learning and transfer learning analytic model has been introduced for skin cancer classification [
163].
3. Complete Understanding of the Tumor Biology
A complete understanding of tumor biology is the key for cancer prevention, early detection and diagnosis, and effective treatment, which is also the ultimate goal of precision oncology. With the rapid development of novel and powerful technologies as discussed above, we now have a much deeper understanding of cancer biology. The discovery of novel knowledge and the emergence of novel concepts and principles have significantly advanced precision oncology.
3.1. Tumorigenesis/Cancer Initiation
Tumorigenesis is a complex, multistep process in which oncogenic mutations within normal cells initiate clonal expansion. This progression is significantly modulated by additional factors, including environmental tumor risk elements and epigenetic modifications, both of which can substantially affect early clonal proliferation and malignant transformation independently of mutational events [
164]. A deeper understanding of the earliest molecular events holds promise for translational applications, predicting individuals at high-risk of tumor and developing strategies to intercept malignant transformation.
3.1.1. Genomics and Cancer Genes
Mutation processes acting from embryological development onwards drives clonal evolution by generating variation in the tumor cell population. Some of these mutations occurs in cancer driver genes that fuel positive selection [
4,
164]. Driver genes are a specific subset of genes that harbor mutations directly contributing to the initiation and progression of cancer. These genes often regulate critical cellular processes such as the cell cycle, apoptosis, and DNA repair. Mutations in driver genes give a growth advantage to the cells and are thus positively selected; they promote clonal expansion and can lead to uncontrolled proliferation [
4,
164,
165].
Early genomic alterations encompass point mutations, short insertions, deletions, structural variations, copy number changes, gene fusions, and methylation differences. Analysis of exome data from 33 tumor types has identified 229 genes undergoing positive selection [
166]. Further investigation into somatic mutations across more than 28,000 tumors representing 66 cancer types has revealed 568 cancer-associated genes and provided insights into their roles in tumorigenesis [
167]. Utilizing data from 2,658 cancers across 38 tumor types provided by the Pan-Cancer Analysis of Whole Genomes (PCAWG) Consortium under the International Cancer Genome Consortium (ICGC), sixteen distinct signatures of structural variation have been characterized [
168]. In a recent study, MethSig was developed to specifically identify candidate DNA methylation driver genes of cancer progression and relapse from 22 cancer types. Chromosomal instability (CIN) leads to extensive losses, gains, and rearrangements of DNA. The resulting genomic complexity is recognized as a hallmark of cancer; however, no comprehensive framework currently exists to systematically quantify various forms of CIN or assess their impact on clinical phenotypes across cancer types. This study analyses the extent, diversity, and origin of chromosomal instability in 7,880 tumors spanning 33 distinct cancer entities. Seventeen copy number signatures defining specific CIN types have been identified, which facilitate drug response prediction and support the discovery of novel therapeutic targets [
169]. Accumulating evidence suggests that clones with aberrantly rewired epigenetic programs show increased tumor susceptibility in morphologically normal tissues [
170]. For example, during precancerous evolution of lung cancer, epigenomes undergo a stepwise progression, culminating in a high level of intra-tumor heterogeneity in invasive lesions. The phylogenetic patterns inferred from methylation aberrations resemble those based on somatic mutations, suggesting parallel methylation and genetic evolution [
171].
3.1.2. Clonal Expansion
Through intensive studies, the process of cancer initiation begins with healthy tissue through clonal expansion [
4]. Single-cell spatial multiomics and many other cutting-edge technologies have been employed to study cancer clonal expansion from normal tissue in many different cancer types [
172]
-[
174]. However, many issues remain unsolved and have become emerging research areas. For example, how can cancer driver events exist in normal tissues? Some studies suggest that selection pressure is different under different environments. NFKBIZ mutations may confer a selective advantage in a chronically inflamed environment; however, these mutations may be negatively selected in cancer and restrict tumor formation [
98]. Little is known about how such dynamic competition in normal epithelia influences early tumorigenesis. A recent study shows that the majority of newly formed oesophageal tumours are eliminated through competition with mutant clones in the adjacent normal epithelium [
175].
Understanding mechanisms driving the clonal expansion of normal tissue toward early cancer initiation will provide insight into cancer prevention and treatment and is thus an important topic being explored.
3.1.3. Environmental Carcinogenesis
The causal links between environmental exposures and cancer initiation has been gradually established [
176]
-[
179]. These environmental factors include chemical and radical insults, unhealthy metabolic behaviors such as alcohol consumption and smoking, and specific pathogenic infections. These environmental factors induce genetic and epigenetic alterations in transformed cells and have profound impacts on microenvironmental components that predispose to tumor initiation. For example, KRAS G12C mutations in NSCLC are generated through smoking-related mutagenesis [
180,
181].
However, many environmental factors cause cancer by mechanisms other than mutations [
182]. This non-mutagenic carcinogenesis is an emerging hot research topic [
4]. One likely mechanism is the deregulation of cancer-related gene expression through epigenetic modifications [
4,
183]
-[
185]. Another mechanism may be through chronic inflammation. Some studies indicate that many environmental factors cause local inflammation, which provides a different selection pressure in favor of cancer initiation [
164,
185]. The mechanisms by which inflammation facilitate early tumorigenesis include oxidative stress, DNA damage, mutation clone expansion, cell proliferation, and cell survival [
34,
98,
186,
187].
3.2. Tumor Heterogeneity
Thanks to the development of single-cell spatial multiomics, the concept of tumor heterogeneity has moved onto the center stage of cancer research. Both intertumoral and intratumoral heterogeneity are crucial factors for the complete understanding of molecular foundation of tumors. While intertumoral heterogeneity has been well studied and largely reflected by molecular stratifications based on driver genes, pathways, and expression profiles, intratumor heterogeneity (ITH) is much less understood and is an emerging area being extensively studied [
2,
4].
ITH is frequently observed in malignant tumors and results from dynamic changes involving genetic, epigenetic, transcriptomic, proteomic, metabolic, and microenvironmental factors. This complexity can influence tumor development and contribute to treatment resistance, potentially affecting the accuracy of clinical diagnosis, prognosis, and treatment planning. While multiomics technologies now provide comprehensive mapping of ITH at multiple molecular levels, there are ongoing challenges with applying these findings clinically.
ITH is a major mechanism conferring resistance to most targeted drugs because cancer cells of a given tumor are usually composed of a mixed population with diverse clonal or subclonal genetic structures.
In recent years, advanced technologies like the single-cell omics, spatial omics and CRISPR-based lineage tracing have substantially enriched our understanding of ITH. Each technology offers distinct advantage. Single-cell multiomics allow the dissection of ITH at cellular resolution. The single-cell layer of resolution provides the most precise lens through which the clonal complexity, lineage dynamics, and evolutionary trajectories of tumors can be observed [
188]. A recent study integrated bulk genomics data with co-occurrences of mutations from single-cell RNA sequencing data to reconstruct clonal trees in high-grade serous ovarian cancer and breast cancer and achieved high resolution and high-fidelity results [
189]. Spatial omics such as spatial transcriptomics holds great promise in deciphering the complex heterogeneity of cancer by providing localization-indexed gene expression information [
190]. Epigenomics is able to uncover the regulatory landscape of tumor heterogeneity. Proteomics provides functional diversity in cancer cells. However, due to the limitation of each technology, the integrated analysis of single-cell spatial multiomics become the most adopted method to explore ITH. Some recent studies highlight this progress in various tumor types [
191,
192,2024].
Due to their heterogeneity, the bulk tumour might include a diverse collection of cells harbouring distinct molecular signatures with different levels of sensitivity to treatment. This heterogeneity might be across different disease sites (spatial heterogeneity) or change over time (temporal heterogeneity). Heterogeneity provides the fuel for resistance. Indeed, drug resistance has been linked to the heterogeneity of many cancers [
193,
194]. Using single-cell transcriptomics, a recent study of pediatric Burkitt lymphoma reveals intra-tumor heterogeneity and markers of therapy resistance [
195]. An accurate assessment of tumour heterogeneity is essential for the development of effective therapies. Current strategies to combat heterogeneity-related drug resistance include (1) upfront treatment with potent pan-inhibitory TKIs, instead of reserving them for the second-line; (2) design of dosing schedules based on the mathematical model of the tumor heterogeneity; and (3) combinatorial approaches that pair therapies targeting the predominant, drug-sensitive population of clones in addition to the various subsets of drug-resistant and drug-tolerant cells [
193]. More recently, a study showed that intratumor heterogeneity of EGFR expression mediates targeted therapy resistance and formation of drug tolerant microenvironment. Moreover, pharmacological induction of EGFR using epigenetic inhibitors sensitizes the resistant cells to EGFR inhibition, which suggests that intrinsic drug resistance can be prevented or reversed using combination therapies [
196].
3.3. Holistic TME Ecosystem
A tumor is not a simple collection of cancer cells; rather, it is composed of a multitude of cell types that interact with each other to constitute the TME. The TME is a complex ecosystem of cancer cells, stromal cells, immune cells, and signaling molecules. In the absence of single-cell spatial omics, it is difficult to either distinguish tumor-associated signals of other components or understand the spatial distribution and interaction among cells in the tumor and TME. The advancement of single-cell spatial multiomics has propelled a profound paradigm shift in the understanding of tumor and TME cellular components and heterogeneity. Recent studies with single-cell spatial multiomics have revealed multiple tumor-enriched cell types including immune cells, CAFs, and other stromal cells with diverse functions.
However, the current understanding of the makeup of a tumor is still incomplete and coarse-grained. More research is needed to achieve a complete depiction of the tumor. We need to determine if we have identified most cell types or much more needs to be discovered, if all cell types are heterogeneous with multiple subtypes, what are the functions of these identified cells, what cell types are universal and what are cancer type-specific, and what are the critical factors leading to the makeup of the TME?
Through integrative analyses of over 14 million cells from 10 cancer types across 7 spatial transcriptomics and proteomics platforms, a recent study discovered, validated, and characterized four distinct spatial CAF subtypes. These subtypes are conserved across cancer types and independent of spatial omics platforms. Notably, they exhibit distinct spatial organizational patterns, neighboring cell compositions, interaction networks, and transcriptomic profiles. Their abundance and composition vary across tissues, shaping TME characteristics such as levels, distribution, and state composition of tumor-infiltrating immune cells, tumor immune phenotypes, and patient survival. This study enriches our understanding of CAF spatial heterogeneity in cancer and paves the way for novel approaches to target and modulate CAFs [
197]. Another study with single-cell/single-nucleus RNA sequencing and spatial transcriptomics on 62 samples from 25 pancreatic ductal adenocarcinoma (PDAC) patients have uncovered distinct cellular subtypes involved in neural invasion in pancreatic cancer [
198]. By using single-cell spatial multiomics, another study revealed the potential involvement of SPP1+ fibroblasts in determining metabolic heterogeneity and promoting metastatic growth of colorectal cancer liver metastasis [
199]. Phenotypic heterogeneity and plasticity in colorectal cancer (CRC) have a crucial role in tumor progression, metastasis, and therapy resistance. Single-cell spatial multiomics data are generated from metastatic colorectal samples, which reveals regenerative and inflammatory cancer cell states, identifies AP-1 and NF-dB as key regulators of the regenerative cell states, and locates the regenerative cells at the invasive edge in an immunosuppressive niche [
200].
Immune evasion is a major obstacle in cancer treatment, enabling tumors to avoid immune detection and complicating therapies, which leads to poorer patient outcomes [
201]. To combat tumor immune evasion, further research is needed to understand tumor immune evasion mechanisms. We need to know which cell types are integral to tumor immune evasion and what suppression mechanisms are present within the tumor. Are these mechanisms universal or cancer-type specific? TME actively shapes the immune response through various mechanisms that collectively promote immune suppression and allow tumor cells to avoid immune surveillance. Currently, several mechanisms have been identified. TME may promote immune evasion by recruiting and polarizing immune cells into immunosuppressive phenotypes by secreting cytokines that can either stimulate or suppress immune evasion, by influencing the expression of immune checkpoint molecules, and by metabolic reprogramming [
201].
Recently, by integrating human colorectal single-cell transcriptomic data from approximately 200 donors, a study comprehensively characterized transcriptional remodeling in the TME and identified divergent TME subtypes in which cancer cells exploit different immune evasion mechanisms [
202]. It is also shown recently that spatial architecture of myeloid and T Cells orchestrates immune evasion in lung cancer [
203]. Another research classified CRC into five TME subtypes with distinct response rates to immunotherapy. [
204].
4. Cancer Stratification
As an essential objective of precision oncology, cancer stratification is the task of classifying a cancer into distinct patient subgroups based on specific patient characteristics, which can then guide treatment decisions based on which subgroup a patient belongs to [
205]. An active and growing body of work is exploring different approaches for identifying homogeneous patient subgroups, ranging from qualitative models that are based on clinical observations alone to quantitative models that integrate measurements from diverse high-throughput biotechnologies [
206,
207]. Cancer stratification can benefit both cancer research and the cancer treatment.
4.1. Brief History
For centuries, people believed that cancer was one disease. When Hippocrates wrote about cancer in 400 B.C., for instance, he said that cancer was a single disease that would not fully go away, even after surgery. It has since been realized that cancer is not a single disease; instead, it is a collection of hundreds of different diseases. Although cancer stratification has been conducted for many years, it was conducted as a by-product of clinical experience in the old time. When clinicians noticed the presence of patterns or groups of outlier patients, they performed a more thorough (retrospective or prospective) study to confirm their existence. However, this type of subtyping was limited by the expertise and resources of individual doctors.
Collective efforts have been made to stratify cancers systematically based on their location (tissue, organ, and system), morphology, and histology. Cancers are traditionally classified four ways: (I) broadly, by tissue, organ, and system; then by (II) specific type, and (III) grade according to WHO classifications; and (IV) finally by spread according to the Tumor Node Metastasis (TNM) system. These classifications have significantly influenced clinical oncology, cancer research, and oncologist and pathologist training [
208].
Starting in 2000, the WHO classifications began to include biologic and molecular–genetic features. The completion of the Human Genome Program and the advancement of high-throughput biotechnologies have provided the means for measuring differences among individuals at the cellular and molecular levels. The cost of measuring various “–omics” data (such as genomic, proteomic, and metabolomics data) has decreased significantly, enabling scientists to collect such data on a large number of patients. Thus, research has shifted toward computationally driven approaches to identify subtypes. These developments led to the era of precision oncology, which have had a strong impact on cancer diagnosis and treatment [
4,
208].
In precision oncology, molecular cancer stratification now falls into two categories. One is the molecular subtyping of traditionally defined cancer types, which is the initial strategy and is still advancing now. The other one is pan-cancer molecular stratification, which is more newly developed and has the potential to revolutionize precision oncology (
Figure 5).
4.2. Molecular Subtyping of Traditionally Defined Cancer Types
While there are many ways to further subtype traditionally defined cancer types, the major strategies include cancer driver gene based-stratification, signaling pathway alteration-based stratification, expression profile-based stratification, and immune based stratification (
Figure 5).
4.2.1. Cancer Driver Gene-Based Stratification
Traditional molecular cancer stratification relies on genetic and epigenetic drivers and expression profiles. This method identifies anti-tumor targets and guides personalized cancer therapy development. For example, breast cancer caused by
erbB2 driver gene is classified as a HER2-enriched breast cancer subgroup. This stratification allows the development of tailored therapy to specifically target HER2. The development and clinical application of the therapeutic monoclonal anti-HER2 antibody is one the first successful examples. Another successful example is the classification of the non-small cell lung cancer (NLCSC) caused by the mutation of driver gene
erbB1. Based on this stratification, a small molecular inhibitor gefitinib was developed and successfully applied for treating this group of patients. A third example is the stratification of cancers caused by BRAF V600E mutations. V600E is a driver mutation in many tumors, including melanoma. The targeted therapeutic drug Vemurafenib was developed, which is effective in treating melanoma harboring V600E mutation [
209]
Identifying molecular cancer drivers is critical for precision oncology. More comprehensive research has been done in recent years to identify novel cancer driver genes and explore the opportunities to target these cancer driver genes specifically in multiple types of cancers. In a recent analysis spanning 9,423 tumor exomes from 33 different types of cancers collected in The Cancer Genome Atlas projects (TCGA), 299 driver genes were identified with implications regarding their anatomical sites and cancer/cell types [
166].
A recent study examined the genomic sequences of 20,331 primary tumours from 41 different human cancer types to identify and catalogue driver mutations in 727 recognised cancer genes. The results indicate notable variations in the frequency of cancer gene mutations among cancer types, with tumour suppressor genes (94%), oncogenes (93%), transcription factors (72%), kinases (64%), cell surface receptors (63%), and phosphatases (22%) frequently involved. The analysis also showed that cancer gene mutations commonly co-occur rather than occur exclusively across all cancer types. Furthermore, the study reported that patients with tumours exhibiting different combinations of gene mutation patterns demonstrate varying survival outcomes. These results offer further information about the genetic features of cancer and contribute to our understanding of the mechanisms underlying various forms of cancer [
210].
A recent study analysed whole-genome sequencing data from 10,478 patients across 35 cancer types recruited for the UK 100,000 Genomes Project. The research identified 330 candidate driver genes, including 74 previously unreported in any form of cancer. Findings indicated that approximately 55% of the patients possessed at least one clinically relevant mutation which may predict either responsiveness or resistance to specific treatments, as well as eligibility for clinical trials. Through computational chemogenomic analysis of cancer mutations, the study highlights additional targets for compounds that may be promising candidates for future clinical trials. This work constitutes one of the most comprehensive initiatives to date to identify cancer driver genes in a real-world setting and evaluate their significance in guiding precision oncology [
211].
4.2.2. Signaling Pathway Alteration-Based Stratification
It is quite often that cancer is not caused by a single gene modification, but multiple alterations along a signaling cascade. The alteration of an oncogenic signaling pathway is the combined effects of multiple alterations; cancers that share these common features could be classified into a specific group and treated with targeted therapeutic drugs.
Signaling pathways have been used to further subtype specific cancers for many years. For example, a large volume of research has explored oncogenic signaling pathways associated with TNBC, including the cell cycle, DNA damage response, and androgen receptor (AR) signaling pathways, to identify more efficient targeted therapies [
212]. In addition, the dysregulation of Wnt signaling in TNBCs has also been explored for its potential biological roles in molecular subtyping [
116].
Pathway-based clustering methods have been developed by incorporating biological pathway databases [
213]. Pathifier discovered several pathways which are significantly associated with patient survival in glioblastoma and colorectal cancer [
214]. Several pathways identified by Pathifier were significantly associated with survival of glioblastoma patients. R-Path Cluster identified two subtypes of glioblastoma and several pathways associated with the cancer progression [
215]. As a follow up, a pathway-based deep clustering method (PACL) for molecular subtyping of cancer was introduced. The patient groups clustered by PACL may correspond to subtypes which are significantly associated with distinct survival distributions [
215].
In addition, pan-cancer analysis of signaling pathways have contributed significantly to pan-cancer molecular stratification [
216], which will be discussed later.
4.2.3. Expression Profile-Based Stratification
In precision oncology, the molecular stratification of cancer is mostly based on the molecular profiling of the cancers. Initially, the molecular profiling is mostly based on the genomics of the cancer, which then expanded to the expression profiles defined the transcriptomics and proteomics. More recently, epigenomics, metabolomics, microbiomics and/or metagenomics were all included in the molecular profiling of patients. The advancement of these omics is due to the progress of high-throughput technologies, which have revolutionized medical research since the completion of human genome project at the beginning of millennium. These new technologies can generate a snapshot of any biological system of interest at an unprecedentedly high resolution.
The molecular stratification based on multiomics is mostly to further subtype cancers defined by histology or anatomic origin. For breast cancer, TNBC was further subtyped to 4 or more subgroups based on Omics. In 2011, Lehmann et al. from VICC used k-means clustering method to study gene expression profiles of 587 TNBCs and separate them into six subtypes [
217]. In 2016, they found that transcripts in the IM and MSL subtypes were not contributed from cancer cells directly, so the classification criterion of TNBC type was refined into TNBC type-4 with BL1, BL2, LAR, and M [
217]. In accordance with the VICC subtyping system, Burstein et al. applied mRNA profiling to 198 TNBC samples using non-negative matrix factorization (NMF) clustering and identified four TNBC subtypes with distinct molecular characteristics in 2015 [
218]. Subsequently, researchers at Fudan University Shanghai Cancer Center (FUSCC) sequenced 465 TNBC samples and used multiomics data to define four mRNA-based clusters, further proposing targeted treatment strategies for each cluster [
219]. The FUSCC group profiled the polar metabolome and lipidome in 330 TNBC samples and 149 normal breast tissues, creating a metabolomic atlas. They identified three TNBC subgroups: C1 (enriched ceramides and fatty acids), C2 (upregulated metabolites related to oxidation and glycosyl transfer), and C3 (least metabolic dysregulation) [
220].
For Colorectal cancer (CRC), four consensus molecular subtypes (CMSs) derived from large-scale gene expression profiles have been defined with each subtype associated with unique oncogenic processes [
221]. CMS classification for CRC includesCMS1 (14%)—hypermutated, microsatellite unstable, strong immune activation; CMS2 (37%)—epithelial, WNT/MYC signaling; CMS3 (13%)—epithelial, metabolic dysregulation; and CMS4 (23%)—mesenchymal, TGF-β activation, stromal invasion, angiogenesis. Mixed samples (13%) may indicate transitional or heterogeneous phenotypes. CMS is currently the most robust and interpretable CRC classification, forming the basis for future stratified and targeted therapies [
221].
Furthermore, epigenetic profiling has been investigated for tumor stratification and the identification of tumor subtypes. Notably, methylation profiling of cfDNA obtained from blood samples of cancer patients provides valuable insights into tumor subtypes. For example, a recent study on small cell lung cancer developed a cfDNA methylation-based method capable of distinguishing clinically relevant subtypes [
222]. This liquid biopsy approach may enhance the clinical application of genomics-informed molecular tumor subtyping.
4.3. Pan-Cancer Molecular Stratification
While molecular subtyping has been mostly employed to further subtype the traditional cancer types organized by histology or anatomic origin, a new trend is to develop pan-cancer classification. Cancers in different organs and tissues have similarities at the molecular level, and their similarity is even greater than that of the same tumors, suggesting the possibility for the re-classification of cancers by pan-cancer molecular stratification across the traditionally defined cancer types. Pan-cancer molecular stratification allows more accurate and effective targeted treatment of cancer patients, which becomes an important part of precision oncology.
The current major strategies for pan-cancer molecular stratification include cell of origin-based stratification, oncogenic processes-based stratification, oncogenic signaling pathway-based stratification, TME-based stratification, somatic mutation-based stratification, network-based stratification, radiomics signature-based stratification, and immune based stratification (
Figure 5)
4.3.1. Pan-Cancer Molecular Stratification Based on the Cell of Origin
The Cancer Genome Atlas (TCGA) consortium, a large-scale collaboration initiated and supported by the National Cancer Institute (NCI) and National Human Genome Research Institute (NHGRI), contributed significantly to pan-cancer molecular stratification by producing the Pan-Cancer Altas. From an analysis of over 11,000 tumors from 33 of the most prevalent forms of cancer, the Pan-Cancer Atlas provides a uniquely comprehensive, in-depth, and interconnected understanding of how, where, and why tumors arise in humans. This data generated the first wave of pan-cancer molecular stratification.
The cell of origin in cancer is defined as the normal cell that acquires the first cancer-promoting mutation(s) [
223]. Analysis of 11,000 tumor samples across 33 tumor types reveals that the cell-of-origin among different cancer types is a prominent feature of the tumor classification [
224]. A new 28-clustering of tumor types was proposed to reclassify human tumors. The two-thirds of molecular subclassifications show varying degrees of heterogeneity, and the most diverse cluster contains 25 tumor types. The findings from this study indicates that cell-of-origin influences, but does not fully determine, tumor classification. Therefore, the traditional tumor classification organized by histology or anatomic origin should be supplemented by the Pan-Cancer Atlas molecular taxonomy based on molecular similarity shared by tumors across distinct tissue types [
224].
Indeed, a study analysis of molecular data on 2,579 tumors from TCGA of invasive breast cancer and four gynecological cancers including uterine corpus endometrial carcinoma, high-grade serous ovarian cystadenocarcinoma, cervical squamous cell carcinoma and endocervical adenocarcinoma, and uterine carcinosarcoma, identified shared and unique molecular features, clinically significant subtypes, and potential therapeutic targets. This study utilized 16 key molecular features to identify five prognostic subtypes and constructed a decision tree that assigns patients to these subtypes using six features which can be analyzed in clinical laboratories [
225].
Another study analyzed 921 adenocarcinomas of the esophagus, stomach, colon, and rectum to examine shared and distinguishing molecular characteristics of gastrointestinal tract adenocarcinomas (GIACs). Five molecular subtypes Epstein-Barr virus (EBV)-positive, hypermutated-single-nucleotide variant predominant (HM-SNV), microsatellite instability (MSI), chromosomal instability (CIN), and genomically stable (GS) are identified among GIACs [
226]. Squamous cell carcinomas can also be classified into different subgroups based on genomic, pathway network, and immunologic features [
227]. Renal cell carcinoma (RCC) encompasses multiple histologically distinct malignancies, each characterized by unique genetic drivers, clinical trajectories, and therapeutic responses. Analysis of 843 RCC cases spanning the three principal histologic subtypes—including 488 clear cell RCCs, 274 papillary RCCs, and 81 chromophobe RCCs—demonstrates distinct characteristics for each subtype. These findings provide a foundation for the development of targeted therapeutic and management strategies tailored to individual RCC subtypes [
228].
More recently, it has been revealed that the cell-of-origin influences pancreatic cancer subtypes, which provide insight into the fundamental impact that the very earliest events in carcinogenesis can have on cancer evolution [
229]. Diffuse large B-cell lymphoma (DLBCL) is a heterogeneous group of cancers classified together on the basis of morphology, immunophenotype, genetic alterations, and clinical behavior. DLBCL is one of the earliest cancers being subtyped based on the cell of origin. Through the years, the cell of origin subtypes of DLBCL have been refined by various methods [
219,
230,
231]. Recently, a refined subtyping based on integrated multiomic analysis on 228 relapsed/refractory DLBCL samples was able to distinguish subtype-specific mechanisms of treatment resistance and relapse, which facilitates the development of personalized treatment of this high-risk group [
232].
By applying five different machine learning approaches to multiomic data from 8,791 TCGA tumor samples comprising 106 subtypes from 26 different cancer cohorts, a very recent study built models based upon small numbers of features that can classify new samples into previously defined TCGA molecular subtypes. These models are further validated by using external datasets. [
233].
It is worth noting that cell-of origin has also been used to further subtype specific cancers. For example, diffuse large B-cell lymphoma (DLBCLs) is grouped into three distinct molecular subtypes based on the putative cell of origin (COO): the activated B-cell-like (ABC), the germinal B-cell-like (GCB), and the unclassifiable subtype as defined by array-based gene expression profiling [
234,
235]. Further studies have determined cell-of-origin subtypes of diffuse large B-cell lymphoma using gene expression in formalin-fixed paraffin-embedded [
230] and have developed a platform independent protein-based cell-of-origin subtyping of diffuse large B-cell lymphoma in formalin-fixed paraffin-embedded tissue [
236].
4.3.2. Pan-Cancer Molecular Stratification Based on the Oncogenic Processes
The Pan-Cancer Atlas provides a panoramic view of the oncogenic processes that contribute to human cancer. A comprehensive study which analyzed the oncogenic processes across 11,000 tumors from 33 cancer types revealed that germline genome affects somatic genomic landscape in a pathway-dependent fashion; genome mutations impact expression, signaling, and multiomic profiles; and mutation burdens and drivers influence immune-cell composition in the microenvironment [
237]. The results offer the opportunity for pan-cancer molecular stratification and targeted therapies based on these important oncogenic processes and will provide a foundation for future personalized cancer care.
A companion study with the TCGA performed immunogenomics analyses of more than 10,000 tumors and have identified six immune subtypes that encompass multiple cancer types. These six immune subtypes differ by somatic aberrations, microenvironment, and survival, which defines immune response patterns impacting prognosis. These analyses serve as a resource for exploring immunogenicity across cancer types and set a foundation for future targeted studies to further advance precision oncology [
238]. A recent study processes 364 individual tumors cross cancer types by clustering upon 10 features and identifies 12 unique tumor archetypes spanning cancer type. Each archetype concentrates similarities in additional immune and tumor features. Dominant archetypes aid in tumor classification and identifying therapeutic targets [
239].
We discuss above that cancer driver genes play an important role in the further subtyping of the traditionally defined cancer types. Recent studies indicate that the analysis of cancer driver genes across multiple cancer types could also serve for pan-cancer molecular stratification. A Pan-Cancer and PanSoftware analysis spanning 9423 tumor exomes from 33 cancer types used 26 computational tools to catalog driver genes and mutations and thus identify 299 driver genes. It reveals that driver genes and mutations are shared across anatomical origins and cell types and thus could form the basis for pan-cancer molecular stratification and targeted treatment [
166]. Similarly, another research highlights the driver gene fusion in pan-cancer molecular grouping and its clinical implication [
240].
Pan-cancer analysis has also focused on identifying the molecular subtypes associated with specific driver genes. It is shown that SF3B4 is strongly expressed in patients cross cancer types and the expression level is correlated with their survival [
241]. By using hepatocellular carcinoma (HCC) as a model, this study illustrates the role of SF3B4 as an oncogenic factor in HCC, highlighting its potential as a pan-cancer therapeutic target and diagnostic biomarker [
241]. Analysis of 56 MET-F–positive tumors from an institutional cohort of 91,119 patients (79,864 DNA sequencing plus 11,255 RNA sequencing) uncovered two forms of MET-F pathobiology. MET fusions are primary drivers of tumor growth in multiple tumor types – lung cancer and gliomas – and can be effectively targeted with either type I (crizotinib, capmatinib, tepotinib, and savolitinib) or type II (cabozantinib) MET TKIs, with best responses in tumors harboring fusions with partner homodimerization [
242].
In addition, pan-cancer analysis of TCGA data across 11,000 tumors from 33 cancer types have been performed for other important oncogenic process including mRNA splicing [
240,
243], IncRNA [
244,
245], enhancer expression [
246], and aneuploidy [
247].
A recent study presents a novel method based on patient-specific gene regulatory network to identify cancer subtypes based on patient-specific molecular systems. By applying the data collected in TCGA, this study indicates that the novel method is able to identify more clinically meaningful cancer subtypes than the existing subtypes and found that the identified subtypes comprised different molecular features [
248]. A recent study introduces a framework for cancer molecular subtyping by identifying specific co-expression modules, generating network features through adjusted edge correlations, and training a deep neural network for multi-class classification. Applied to breast cancer and stomach adenocarcinoma, this method outperforms existing approaches [
249].
4.3.3. Pan-Cancer Molecular Stratification Based on Oncogenic Signaling Pathways
In its comprehensive analysis of tumor signaling pathways, the Pan-Cancer Atlas reveals patterns of vulnerabilities that will aid in molecular stratification and the development of personalized treatments and new combination therapies. Using mutations, copy-number changes, mRNA expression, gene fusions and DNA methylation in 9,125 tumors cross 33 cancer types, a comprehensive study analyzed ten oncogenic signaling pathways including PI-3-Kinase/Akt, Hippo, Myc, RTK-RAS, Notch, Nrf2, TGFβ signaling, p53, β-catenin/Wnt and cell cycle. It showed that 89% of tumors had at least one driver alteration in these pathways, and 57% of tumors had at least one alteration potentially targetable by currently available drugs. 30% of tumors had multiple targetable alterations, indicating opportunities for combination therapy. Based on this data, tumors can be stratified into 64 subtypes [
216].
Seven major metabolic processes and their clinical relevance are analyzed by using molecular data of 9125 patient samples from TCGA. This study provides a pan-cancer classification of metabolic expression subtypes in 33 TCGA cancer types. It shows that metabolic expression subtypes share consistent prognostic patterns across cancer types. Moreover, the metabolic expression subtypes reveal therapeutic targets and are associated with sensitivity to drugs in clinical use [
250]. An extensive molecular characterization of 929 ubiquitin-related genes and 95 deubiquitinase genes is performed with multidimensional omic data of 9125 tumor samples across 33 cancer types from TCGA. It reveals consistent prognostic patterns of tumor subtypes defined by ubiquitin pathway genes. This study highlights the importance of the ubiquitin pathway in cancer development and molecular stratification, which lays a foundation for developing relevant therapeutic strategies [
251].
Many other signaling pathways including TGF-β [
252], Hippo [
244], Ras [
212], RNA splicing [
253], and DNA damage repair [
254] are also comprehensively characterized based on TCGA data of 33 cancer types. These analyses establish initial pan-cancer molecular stratification based on oncogenic signaling pathways.
A recent study analyzed proteomic data from 2,404 samples and transcriptomic data from 7,752 samples across 13 cancers. By comparing normal and tumor tissues, researchers found multiple dysregulated pathways, such as mRNA splicing, interferon, fatty acid metabolism, and complement coagulation cascade. Pan-cancer subtypes were identified by tracking proteins consistently up- or down-regulated across tumor stages. In addition, prognostic risk stratification models are also established based on dysregulated genes. This study reveals that small molecule inhibitors targeting various signaling pathway might be effective treatments for pan-cancer, thereby supporting drug repurposing [
255].
Another recent study developed the PathClustNet algorithm, a pathway-based clustering method designed to identify cancer subtypes. This method first detects gene clusters and identifies overrepresented pathways associated with them. Based on the pathway enrichment scores, it reveals cancer subtypes by clustering analysis.
4.3.4. Pan-Cancer Stratification Based on the Tumor Microenvironment
Cancer molecular typing extends beyond cancer cells to include the tumor microenvironment (TME), which significantly impacts clinical outcomes and therapy response. Tumor-infiltrating immune cells influence tumor progression and treatment success, while cancer-associated fibroblasts and stromal cell angiogenic signals also affect outcomes (Fridman et al., 2012; Chen and Mellman, 2017; Liu, 2019; Pommier, 2016; Schaaf, 2018; Tao, 2017). Subtyping cancer by tumor-immune microenvironment profile can enhance personalized treatment.
A comprehensive study developed an accessible transcriptomic analysis platform for TME classification. Analysis of over 10,000 cancer patients revealed four TME subtypes shared by 20 cancers. These subtypes predict immunotherapy response, with immune-favorable TMEs linked to better outcomes. Therefore, TME subtypes serve as broad immunotherapy biomarkers across cancer types, reflecting both tumor and microenvironment features [
256].
Cancer-associated fibroblasts (CAFs) are a multifaceted cell population that significantly contribute to reshaping the tumor microenvironment (TME). Through multiple pathways, activated CAFs can promote tumor growth, angiogenesis, invasion, and metastasis, along with extracellular matrix (ECM) remodeling and even chemoresistance. The mutual effects of CAFs and the tumor immune microenvironment (TIME) have also been identified as key factors in promoting tumor progression [
257].
A recent study utilized pan-cancer single-cell and spatial transcriptomics analysis to identify the subpopulation of CAFs via senescence related genes, classifying the neuroblastoma patients into high and low risk groups according to median risk score. The low-risk group had a superior survival outcome, an abundant immune infiltration, a different mutation landscape, and an enhanced sensitivity to immunotherapy [
258].
Using a training cohort of 88 HCC single-cell RNA sequencing (scRNA-seq) samples and a validation cohort of 94 samples, encompassing over 1.2 million cells, a study characterized CAFs in hepatocellular carcinoma patients into three fibroblast subpopulations. Among them, VEGFA + CAFs subtype was induced by hypoxic TME and associated with poorer prognosis [
56].
Using single-cell RNA sequencing and spatial transcriptomics, another study investigated the characteristics and functional information of CAF subtypes and explored the intercellular communication between CAFs and malignant epithelial cells in gastric cancer. Cells were classified into nine categories, and analysis showed a correlation between the proportions of epithelial cells and fibroblasts. Six distinct fibroblast subpopulations were also identified, each associated with specific biological processes and immune functions [
259].
Through integrative analyses of over 14 million cells from 10 cancer types across 7 spatial transcriptomics and proteomics platforms, a recent study discovered, validated, and characterized four distinct spatial CAF subtypes. These subtypes are conserved across cancer types and independent of spatial omics platforms [
56].
4.3.5. Other Approaches for Pan-Cancer Molecular Stratification
Molecular mechanisms underlying cancer metastasis span diverse tissues of origin. A recent study attempted to perform a pan-cancer stratification of cancer metastasis based on cell lineage. The transcriptomes of patient-derived xenografts and patient tumor metastases were collected from 38 studies with over 3,000 patients and 4,000 tumors. The analysis revealed four expression-based subtypes of metastasis transcending tumor lineage, which underpins metastases beyond tissue-oriented domains and has important therapeutic implications [
260].
Network-based stratification (NBS) approaches have been used in a recent study for integrated stratification of three types of cancers including ovarian, bladder, and uterine cancer. It showed that integrated NBS subtypes are more significantly associated with overall survival [
261].
Immune response has also been explored for pan-cancer stratification. Many tissue functions are achieved through the complex coordination of immune cells [
262]. The immune response is the result of a coordinated action of a collection of immune cell subsets, which allows it to be used as a signature to group tumors to various subtypes [
263]
-[
265]. In a recent study, cell type compositional and transcriptomic data from 364 fresh surgical specimens across 12 tumor types were used to identify conserved tumor immune archetypes. This study successfully identified and validated 12 unique tumor immune archetypes. This data has become a valuable resource for studying cancer immunity and cancer targets, which will greatly improve response to cancer immunotherapy [
239].
Pan-cancer molecular stratification based on somatic point mutations have also been explored. Statistical analysis of mutation profiles is challenging due to the low frequency of most mutations, the varying mutation rates across tumours, and the presence of a majority of passenger events that hide the contribution of driver events. An innovative study provides a method, NetNorM, to represent whole-exome somatic mutation data in a form that enhances cancer-relevant information using a gene network as background knowledge. Using data from 8 cancer types from The Cancer Genome Atlas (TCGA), it is shown that this method improves survival prediction and unsupervised patient stratification [
266]. More recently, a new machine learning pipeline has been developed to identify protein-coding genes mutated in many samples to identify cancer subtypes. Data from 12,270 samples collected from the international cancer genome consortium, covering 19 cancer types are tested and 17 different cancer subtypes have been identified [
267].
Cancer cells become immortalized through telomere maintenance mechanisms, such as telomerase reverse transcriptase (TERT) activation. A systematic analysis of TERT high and low cancers using multidimensional data from TCGA depicts a telomerase-associated molecular landscape in cancers. Random forest classifiers were generated to identify cancer subtypes [
268].
A recently developed framework for molecular subtyping of cancer is through the identification of a robust specific co-expression module for each subtype of cancer. When applied to breast cancer (BRCA) and stomach adenocarcinoma (STAD) molecular subtyping, it has a superior classification performance over existing methods [
249].
The rapid development of machine learning and deep learning has significantly improved the efficiency of cancer diagnosis. Deep learning-based radiomics signatures show promise in identifying cancer subtypes, which is crucial for precision cancer treatment [
269].
5. Targeted Cancer Therapeutics
The importance of tumor stratification is to allow targeted treatment for each subtype. Therefore, an effective therapeutic treatment tailored to each cancer subtype must be available to make precision medicine successful [
2]. While targeted therapy for cancer treatment started long before the arrival of the precision medicine era, the rapid expansion and progress of targeted therapy only occurred after the sequencing of the human genome and the development of advanced technology for high-through put analysis of multiomics for tissue samples and single-cells.
5.1. Brief History
Before the emergence of targeted therapy, cancers were treated by a combination of surgery, chemotherapy, and radiotherapy.
The origin of radiotherapy dates back to the late XIX century, when it was used for the treatment of breast cancer and epithelioma of the mouth [
270]. Modern radiotherapy was established in 1920 when Claudius Regaud demonstrated that radiation fractionation could effectively treat several human cancers by minimizing treatment-related side effects. Despite these advances, surgical intervention remains the sole therapeutic option for advanced or non-solid tumors. A significant milestone was marked in the mid-20th century with the introduction of chemotherapy, following the serendipitous discovery of the first DNA alkylating agent, nitrogen mustard. Mechlorethamine was the initial nitrogen mustard employed clinically as an alkylating agent, primarily used in patients with prostate cancer and various lymphoid malignancies, including Hodgkin’s disease, lympho-reticulosarcomatosis, and lymphatic leukemia [
271]. Afterwards, many types of chemotherapy drugs with different action modes were introduced in cancer treatment, leading to significant improvements in survival rate, especially for patients with onco-hematological diseases. Chemotherapy in combination with radiation therapy and surgery has been the dominant treatment for all types of cancers for more than half a century.
However, chemotherapy’s toxicity to normal tissues and the development of drug resistance mechanisms by tumor cells represented important obstacles to overcome [
272]. Subsequently, with the understanding of cancer biology including its genetic basis and the discovery of oncogene and tumor suppressor, the idea to target altered proteins to treat cancer emerged and were explored in the final quarter of the last century [
2,
273]. These approaches have significantly increased the effectiveness of treatments and the survival rates of cancer patients.
The real development of targeted therapy comes at the beginning of the 21st century with the success of the human genome project and the rapid development of molecular biology technology, which provides the precise detection of genome, transcriptome, and proteome changes. By using these methods, researchers can explore the mechanisms underlying cancer and design new targets specific for the pathogenic molecules [
274]. By specifically targeting and binding to abnormal genes or proteins, the novel regimen enables personalized and efficient therapy. Over the past years, the striking breakthroughs of gene editing and cell therapy techniques have led targeted therapy into a vigorous development stage.
To date, besides the development of novel targeted drugs, pharmaco-omics is employed to identify drugs best for each individual. Pharmaco-omics selects the right drugs and dosages for each individual based on the person’s particular genetic/molecular makeup, as well as a person’s environment, diet, age, lifestyle, and state of health. Moreover, functional precision medicine is applied to examine the direct response of patient-derived cancer cells to various selected drugs in vitro.
5.2. The Development and Current Status of Targeted Therapies
The current strategies for developing targeted cancer therapies can be classified into 3 broad categories: the one disease-one target-one drug approach, the systematic targeting immune inhibition approach, and the Pan-Cancer approach (Tumor-Agnostic Therapies) (
Figure 6).
5.2.1. The One Disease-One Target-One Drug Approach
The one disease-one target-one drug approach was the initial strategy for targeted cancer therapies in precision oncology. There are two main categories of drugs developed in this approach: antibodies and small molecules (
Figure 6). In the initial phase of targeted therapy for cancers, antibodies and small molecular inhibitors were designed based on the identification of cancer-driving oncoproteins for each specific cancer type.
5.2.1.1. Monoclonal antibodies
Köhler and Milstein revolutionized anti-cancer therapeutics with the development of hybridoma technology to produce monoclonal antibodies in 1970s. Initially, the produced monoclonal antibodies were mouse antibodies. Subsequently, the mouse antibody was gradually humanized to avoid an undesired immune response and to better suit its clinical application. Eventually, 4 types of monoclonal antibodies became available: murine, chimeric, humanized, and human monoclonal antibodies, which differ from each other by the percentage of murine protein portion present in the immunoglobulin [
275]. While the initial antibodies were all naked antibody based on the nature properties of IgG, the engineered antibodies and antibody-drug conjugates have emerged as more effective alternatives.
A very successful example is the development of trastuzumab, an antibody targeting cell surface receptor HER2 to treat HER2-positive breast cancer. In 1987, Slamon et al. identified HER2 gene amplification in roughly 30% of breast cancer tumors, which correlated with poor prognosis [
276]. Hudziak et al. developed the HER2-specific monoclonal antibody 4D5 in 1989, demonstrating antiproliferative effects on HER2-positive cells [
277]. The antibody was humanized in 1992 for clinical use, becoming Trastuzumab, which showed substantial benefits for HER2-positive breast cancer patients and received approval in the USA (1998) and Europe (2000).
The first monoclonal antibody approved for cancer treatment was Rituximab in 1997 for use in relapsed/refractory indolent non-Hodgkin lymphomas (NHL). Rituximab, a hybrid antibody, has specific affinity for the B-lymphocyte transmembrane protein, CD20, which is expressed on most malignant B cells [
278].
Following the approval of the above first two antibodies, many more monoclonal antibodies have been developed and approved for the treatment of various cancers. Until 2024, there have been 84 cancer therapeutic antibodies approved by the FDA. Tumour antigens that have been successfully targeted include epidermal growth factor receptor (EGFR), ERBB2, vascular endothelial growth factor (VEGF), cytotoxic T lymphocyte-associated antigen 4 (CTLA4), CD20, CD30 and CD52 [
2]. The therapeutic antibodies generated in the early stages are all naked antibodies that utilize its natural properties, including ADCC, ADCP, CDC, and the inhibition of cell signaling.
Despite its huge success, treatment using mAbs alone is often insufficient, and it is often less lethal against cancer cells compared to chemotherapy. Accordingly, the antibody–drug conjugate (ADC) was introduced as an innovative strategy to leverage the specific targeting ability of monoclonal antibodies (mAbs) with the high potency of cytotoxic agents. An ADC is composed of a tumor-specific mAb chemically linked to a cytotoxic payload via a carefully engineered linker [
2,
279,
280]. Since the first ADC Mylotarg
® (gemtuzumab ozogamicin) was approved in 2000 by the FDA [
281], there have been 15 ADCs which received market approval by the FDA including two newly approved in 2025. Moreover, over 100 ADC candidates are in the clinical stages of testing for future use. In addition, antibodies have also been conjugated with cytokines (Immunocytokines, ICs) and radionuclide (ARCs). This kind of anti-cancer drug, known as "biological missiles", is leading a new era of targeted cancer therapy [
280] (
Figure 6).
5.2.1.2. Small molecular inhibitors (SMIs)
It is well established that various gene mutations and protein modifications cause oncogenic alteration of key signaling pathways, which lead to the cancer development. Targeting these oncogenic signaling pathways is thus an effective approach to treat cancer. Besides therapeutic monoclonal antibodies, this approach has led to the development of SMIs able to selectively bind to molecular targets, mostly protein kinases, present in the tumor cells.
There are two types of SMIs based on their selectivity: selective SMIs that are highly selective with single or fewer targets and multikinase inhibitors (MKIs) that have low specificity and exert their anticancer activity by simultaneously targeting a broad spectrum of the human kinases [
274] (
Figure 6). Selective small molecule inhibitors can be further categorized into selective small molecule kinase inhibitors and selective small molecule nonkinase inhibitors, depending on whether the substrate is a protein kinase (Liu, 2022).
The landmark event in the revolution of targeted therapy was the development in the early ’90s of the first multikinase inhibitor, Imatinib mesylate. This small molecule inhibitor targets multiple tyrosine kinases such as CSF1R, ABL, c-KIT, FLT3, and PDGFR-β. Specifically, it is used for chronic myelogenous leukemia (CML) and acute lymphocytic leukemia (ALL). Imatinib was approved for medical use in the United States in 2001. It is on the World Health Organization’s List of Essential Medicines.
Gefitinib represents the first FDA approved selective small molecular inhibitor tar-geting EGFR. Gefitinib interacts with the EGFR ATP-binding site and is able to inhibit the abnormal activation of MAPK and PI3K/AKT pathways overexpressed in cancer cells (Nicholson et al., 2001; Yarden, 2001). In early groundbreaking studies, only non-small cell long cancer patients with EGFR mutations were found to be responsive to gefitinib.
Among the selective serine/threonine kinase inhibitors, BRAF inhibitors (Vemuraf-enib and Dabrafenib) and MEK inhibitors (Trametinib and Cobimetinib) are widely used in clinical practice for the treatment of mutated BRAFV600E melanomas, providing significant improvement in survival rates (Robert et al., 2015).
Selective small molecule inhibitors typically interact with a single molecular target, thereby suppressing target-specific cell signaling pathways. Certain cancers are highly dependent on specific dysfunctions affecting processes such as proliferation, survival, apoptosis, differentiation, metabolism, and immune modulation. By antagonizing these critical targets, selective small molecule inhibitors can inhibit aberrant functions or restore normal activity, offering therapeutic benefits in tumor management. Patients undergoing treatment with these agents usually require rigorous screening for the presence or absence of defined genetic alterations, as identified in solid tumor tissue, circulating tumor cells, or other body fluids. Under these circumstances, selective small molecule inhibitors enable effective tumor targeting while minimizing adverse effects associated with off-target inhibition.
Most small molecule inhibitors belong to protein kinase inhibitors. However, drugs involved in DNA repair, epigenetics, apoptosis, tumor metabolism, and beyond are also being discovered. Recently, targets previously viewed as undruggable or difficult to target, such as RAS, have also received approval. Small molecule inhibitors continue to face ongoing challenges, including low response rates and the development of drug resistance.
To date, there are more than 80 FDA-approved small molecular inhibitors. Among the approved drugs, 43 inhibit receptor protein-tyrosine kinases, 20 blocks nonreceptor protein-tyrosine kinases, and 13 target protein-serine/threonine protein kinases are directed against dual specificity protein kinases (MEK1/2). The data indicate that 69 of these drugs are prescribed for the treatment of neoplasms [
38,
282].
5.2.2. Immune Checkpoint Inhibitors
The 2018 Nobel Prize in Physiology or Medicine was jointly awarded to James P. Allison and Tasuku Honjo “for their discovery of cancer therapy by inhibition of negative immune regulation”. This highlights the prominence and significance of immune checkpoint inhibitors (ICIs) in cancer therapy.
Besides targeting cancer driving molecules within the cancer cells, it is realized that a dynamic crosstalk exists between the immune system and tumor cells which regulates immune evasion, immunoediting, immunosuppression, and immunosurveillance in the TME. Thus, novel research has focused on engaging components of the adaptive immune system. Immune checkpoints engage when proteins on the surface of immune cells called T cells recognize and bind to partner proteins on other cells, including tumor cells. These proteins are called immune checkpoint proteins. When the checkpoint and partner proteins bind together, they send an “off” signal to the T cells. This in part accounts for the aggressiveness of many tumor types including solid and hematologic cancers and explains their ability to evade the immune system [
283].
Cytotoxic T lymphocyte-associated protein 4 (CTLA-4) was first identified in 1991 as a second receptor for the T cell co-stimulation ligand B7 [
284,
285]. Following the identification that the function of CTLA-4 and B7 is to suppress T-cell activation, it was shown in 1996 that anti-CTLA-4 antibodies could clear carcinomas and fibrosarcomas from mice, which provided the first in vivo evidence of efficacy for a checkpoint inhibitor as an anti-cancer therapy [
285]. The engineered antibodies targeting CTLA-4, Yervoy (ipilimumab), was approved by the FDA for the treatment of metastatic melanoma in 2011, which marked the first FDA approved ICI and started the rapid expansion of ICI for cancer immune therapy.
Following this, engineered antibodies against programmed cell death-1 (PD-1) and its ligand (PD-L1) immediately gained FDA approval for use against multiple cancer types because of their effect on patient survival. CTLA-4, PD-1, and PD-L1 are first generation targets of ICIs (
Figure 6). These discoveries were followed by a significant rise in the identification of novel immune checkpoint targets including LAG3, NKG2A, TIGIT, and TIM3. ICIs targeting these next-generation targets have been developed and many of them are on different stages of clinical trials (
Figure 6).
To date, 11 ICIs has been approved by FDA to target T cells via CTLA4 (ipilimumab (Yervoy
®)) or PD1 (cemiplimab-rwlc (Libtayo), nivolumab (Opdivo
®), and pembrolizumab (Key-truda
®)), and target cancer cells and antigen-presenting cell in the tumor micro-en-vironment via PDL1 (and durval-umab (Imfinzi
®), avelumab (Bavencio
®), and ate-zoli-zumab (Tecentriq)). These ICIs are approved for the treatment of many tumors including breast cancer, bladder cancer, cervical cancer, colon cancer, head and neck cancer, Hodgkin lymphoma, liver cancer, lung cancer, renal cell cancer (a type of kidney cancer), skin cancer, melanoma, stomach cancer, and rectal cancer. Currently, many ICIs are in clinical trials including 13 antibodies to first-generation targets CTLA4, PD1, and PDL1, as well as four antibodies to next-generation targets LAG3, NKG2A, TIGIT, and TIM3 [
2,
286].
The new progress in the field includes the development of biAbs that simultaneously engage two different immune checkpoints, such as PD1 × LAG3, PD1 × CTLA4, or PDL1 × CTLA4. Combining two ICIs in one biAb as opposed to a mixture of two individual mAbs has cost-saving potential. Moreover, small molecular inhibitors targeting immune checkpoints are also actively explored. Small molecular inhibitors interact with immune checkpoints through multiple mechanisms, such as blocking signaling between tumorigenic factors, promoting immune tolerance, and inhibiting immune inhibitors via epigenetic repression. Many small molecular inhibitors are on various stages of clinical trials [
283].
5.2.3. Tumor-Agnostic Therapies, Also Known as Pan-Cancer, or Histology-Independent Therapies
At the beginning, targeted therapy was focused on the development of a series of drugs, each of which was intended to treat a single tumor type with a single molecular aberration. Tumor-agnostic therapies, also known as pan-tumor or histology-independent therapies, are a relatively new approach in cancer treatment that focuses on targeting specific genetic mutations or alterations that drive tumor growth rather than treating tumors based on their location or tissue of origin. The concept behind tumor-agnostic therapies is that some genetic mutations can be drivers of cancer development and progression, irrespective of where the tumor is in the body.
The above discussed ICIs could be considered the earliest tumor-agnostic therapies. In 2017, the FDA expanded the application of Keytruda (pembrolizumab)—which blocks PD-1—to include any metastatic or nonremovable solid tumor exhibiting microsatellite instability-high (MSI-H) or mismatch repair deficiency (dMMR). This was the FDA’s first tissue/site-agnostic approval, meaning that the criteria for patient eligibility are based not on the location of the tumor, but on those molecular characteristics. The field of tumor-agnostic therapy was really set in motion with this landmark FDA approval.
Subsequently, Vitrakvi
® (Larotrectinib), an NTRK inhibitor targeting the NTRK gene fusions found in multiple cancers, received accelerated FDA approval in 2018. The drug functions as a tyrosine kinase inhibitor, blocking TRK proteins to prevent cancer cell growth and induce cell death. Specifically, Vitrakvi
® was approved to treat adults and children with certain solid tumors that have spread or cannot be removed by surgery and have the NTRK gene fusion. This is another example of the pan-tumor targeted therapy approved by the FDA, which further underscored the potential of tumor-agnostic therapies. In the following years, more tumor-agnostic therapies were approved by the FDA, including targeted therapies (BRAF V600E, RET fusion), immunotherapies (tumor mutational burden ≥10 mutations per megabase, dMMR) and an antibody-drug conjugate (Her2-positive-immunohistochemistry 3+ expression) with pan-cancer efficacy [
287].
While the drugs targeting PD-1 BRAF V600E and RET fusion for pan-cancer treatment is considered as an expansion of the existing drugs for pan-cancer, Vitrakvi
® targeting NTRK is a drug truly developed for pan-cancer treatment (
Figure 6).
Hand in hand with pan-cancer molecular stratification, pan-cancer drug development has evolved rapidly. A recent study performed a pan-cancer analysis of antibody-drug conjugate targets and putative predictors of treatment response [
288]. In this study, 121 ADCs clinical trials with 54 targets in 31 cancer types were analyzed and compared with corresponding normal tissues. The analysis indicated that certain ADC are most suitable for a subgroup of cancer types and co-expression of multiple targets was common, which suggests opportunities for pan-cancer therapy with ADC combinations.
Moreover, pan-cancer proteogenomics conducted by the Clinical Proteomic Tumor Analysis Consortium (CPTAC) significantly expanded the landscape of therapeutic targets. The study analyzed over 1,000 prospectively collected, treatment-naive primary tumors spanning 10 cancer types, many with matched normal adjacent tissues. By integrating this dataset with other public datasets, this study provides insights into existing cancer drug targets and systematically identifies candidate new targets for drug repurposing or development [
289].
Recent pan-cancer analysis identifies CD155 as a promising target for CAR-T cell therapy [
290], and identifies MUC1 as a pan-cancer target for drug development for a diverse array of solid tumors and hematological malignancies [
291]. Moreover, a recent study explores the possibility to include novel non-protein molecules as pan-cancer targets. They suggest that high mannose (Man 9) oligosaccharides and phosphatidylserine (PS) as non-protein targets for CAR-T therapy [
292].
6. Cancer Prevention
While cancer cannot be completely prevented, cancer prevention is key to reducing cancer risk. Cancer prevention involves characterizing the prevalence of cancer, identifying etiological factors, and systematically assessing and implementing preventive interventions. Traditionally, research in cancer prevention has emphasized reducing both the incidence of cancer and the mortality associated with the disease.
Cancer risk depends on both genetics and environmental factors like behavior, lifestyle, and environmental exposure. Prevention is possible at all stages of cancer development. Multiple strategies for prevention and early detection have been established to decrease cancer incidence, encompassing primary, secondary, and tertiary levels of intervention [
4,
293]. In general, cancer prevention strategies are classified into primary prevention and secondary prevention based on the timing of the intervention (
Figure 7). Other strategies to prevent cancer progression from early stages to metastasis could be instead considered as cancer treatment.
6.1. Primary Prevention by Vaccination and Prophylactic Intervention
The aim of primary prevention is to reduce cancer incidence by targeting the general population and people with germline risk. This can be achieved through medical interventions, reducing environmental exposures, and lifestyle changes. Medical intervention includes vaccination and other prophylactic interventions (
Figure 7). Some examples are prevention of cervical cancer by human papillomavirus (HPV) vaccination and prevention of liver cancer by vaccination against hepatitis B virus. However, only limited types of cancer are caused by viruses and can be potentially prevented by vaccines. To broaden the application of vaccines, tumor-specific neo-antigens are explored for preventive vaccination with several ongoing clinical trials [
4].
Prophylactic intervention is employed following identification of high-risk individuals, such as risk-reducing mastectomy for carriers of BRCA1 or BRCA2 mutations [
4]. For other cancer-predisposition syndromes, the focus of management remains on early detection. High-throughput sequencing is facilitating broader access to germline testing in the clinic, resulting in vast amounts of information concerning genetic variants in the population, leading to a refinement of prevention [
294]
-[
298]. Lifestyle changes include alterations in physical activity or diet, tobacco cessation, or the use of sunscreen, which reduces one’s exposure to environmental carcinogens [
4,
293].
6.2. Secondary Prevention
Secondary prevention strategies include chemoprevention, interception, screening, and early detection, which usually targets premalignant lesions (Figure 7).
6.2.1. Chemoprevention
The broad use of medication to prevent disease is a common strategy used in cancer and other diseases. It is shown that tamoxifen reduces breast cancer incidence in women deemed to be at high risk of cancer development by a third, even after treatment cessation [
299,
300]. A more recent study showed a relative risk reduction in breast cancer incidence of 65% [
301] and 49% [
302,
303] after treatment with exemestane and anastrozole, respectively. Due to the link between inflammation and cancer development, non-steroidal anti-inflammatory drugs (NSAIDs) and COX2 selective inhibitors (COXIBs), have been utilized as chemopreventive agents. Aspirin has been shown to reduce the incidence of distant metastasis and increase survival in CRC [
304]
-[
306].
However, adverse effects associated with exposure to tamoxifen (endometrial cancers and venous thromboembolism) and aromatase inhibitors (bone fractures) have restricted uptake of chemoprevention drugs outside clinical trials [
307]. To overcome the side effects of cancer preventive chemicals, current studies focus on the phytochemical products for cancer chemoprevention. A recent study identified 22 phenolic components from M. citrine fruit extract (MCE) using LC-ESI-MS/MS, which may act as potential future therapeutic agents for cancer prevention [
308]. The other compounds include Polyphenol-60 from Green Tea for BC prevention [
309], glutelin hydrolysate from riceberry bran residues for the prevention of liver and colon carcinogenesis, phenolic-rich plant extracts from
Lippia citriodora and
Olea europaea for pancreatic cancer prevention [
310], anthocyanins from various berries for colorectal cancer prevention [
311], and Tacrinocerins, which are Tacrine Hybrids with α-Onocerin from
Phlegmariurus, for lymphoblastic leukemia [
312]. In the long run, new, more effective chemopreventive agents with fewer side effects need to be developed before chemoprevention can be more widely accepted.
6.2.2. Interception
Interception lies at the interface of cancer prevention and early detection. Instead of just treating malignancies, Janssen scientists hope to find and eliminate potentially dangerous precancerous cells or disease-driving biological conditions to intercept the disease process and prevent a cancer from ever forming.
For a successful cancer interception, it is essential to understand what drives the progression from premalignancy to malignancy. As discussed above, with the rapid advancement of modern technologies, the efforts through precision oncology have identified many important mechanisms underlying cancer initiation [
4,
164], which provides a foundation for the development of cancer interception methods.
Indeed, some significant progress has been made. Clinically, interception is already well-established using “mechanical” means including the removal of benign adenomatous colon polyps at screening colonoscopy for colorectal cancer interception, detection and removal of cervical intraepithelial neoplasia (CIN3) at colposcopy for cervical cancer interception, and risk-reducing bilateral sapling-oophorectomy for ovary cancer [
313]. In addition, medical interception has also been successfully applied for some cancers. For example, in individuals with von Hippel–Lindau Disease treatment with Belzutifan (an oral hypoxia-inducible factor 2α inhibitor) effectively intercepts the growth of renal cell carcinoma and other tumors by blocking a key biological pathway in oncogenesis [
314]. Immuno-interception is also explored as strategy, which eliminate neoplastic lesions at their earliest stages by mobilizing a specific immune response.
With advances in biological insights and precision technology, it is likely that in the future, individuals could be optimally risk-stratified based on their genetics, lifestyle, environmental exposure, and/or other clinical findings. On the basis of this risk stratification, individuals could be intermittently treated with biologically informed interception interventions and monitored by measuring appropriate biomarkers and optimal early detection.
6.2.3. Cancer Screening
Cancer screening and early detection has also been considered as secondary prevention of cancers. The goal of cancer screening and early detection is to cure cancer by detecting premalignant lesions or malignancy prior to the onset of symptoms, which offers the most effective time to treat cancer [
315]. Cancer screening significantly contributed to the 25% decrease of the overall cancer mortality rate over the last 100 years. The decline in mortality rate is particularly significant for some broadly screened cancers including breast cancer and colorectal cancer, both of which have a vigorous screening program in place.
The Wilson criteria for disease screening with 9 guiding principles were proposed in 1968 by WHO [
316]. (
Table 1).
Based on the cancer type, screening methods can be either direct or indirect. The direct method is to directly visualize and access the target organ as in colorectal and cervical cancer. Indirect methods rely on the measurement of biomarkers associated with cancer (e.g., CA-125 or PSA for prostate cancer), or radiographic imaging (e.g., mammography for breast cancer).
Due to tumor heterogeneity, indirect methods of cancer screening frequently lead to compromised screening efficacy due a decrease in performance characteristics of the screening technique and an increase in overdiagnosis and overtreatment [
317]. Ideally, cancer screening is undertaken when the risk of cancer is high enough to justify the risk of overdiagnosis and overtreatment in an otherwise healthy population.
Through the evaluation of outcomes associated with commonly screened cancer types—including breast, prostate, cervical, colorectal, and lung cancers—several key insights have emerged: (1) invasive cancers exhibit a spectrum of biological behaviour, ranging from indolent to highly aggressive forms; (2) the majority of precancerous lesions are not obligatory precursors to invasive cancers; (3) effective screening programs that target precursor lesions or early-stage malignancies should result in a corresponding decrease in advanced-stage cancer incidence; and (4) the benefits of screening are not uniformly distributed across all individuals.
Learning from these lessons, a recent article provided corresponding improvements by incorporating key clinical questions at each step of the screening ’cascade’ proposed by Harris et al. [
318]. Based on clinical characteristics and molecular profiles of detected cancers, the new model is designed to enable precision screening through individualized risk prediction [
317]. Specifically, screening decisions should take into account a person’s pretest probability of cancer, the threshold risk level where testing would provide net benefit, and patient perspectives regarding risk tolerance. The screen should mitigate overdiagnosis by testing strategies that lower the chance of detecting unimportant lesions.
Overall, due to the heterogeneous nature of cancers, the screening strategy has to be tailored for each cancer type with the consideration of the unique characters of each population group. The knowledge regarding who is at risk of which cancers, in terms of both site and biology, is critical and needed to improve cancer screening.
6.2.3. Early Detection
The aim of early detection is to reduce the proportion of patients diagnosed with cancer at a late stage to maximize the probability of cure (Hawkes, 2019).
The above discussed cancer screening is a major approach for cancer early detection. For many cancers, such as lung, breast, cervical, and colorectal cancers, this is a crucial aspect of cancer control. Many studies have demonstrated the value of cancer screening in lowering the mortality rate. Between 2013 and 2017 in the UK, 1-year net survival rates for CRC were 97.7% at stage 1 versus 43.9% at stage 4; for lung cancer, 87.7% at stage 1 and 19.3% at stage 4; and for breast cancer, 100% at stage 1 and 66% at stage 4 (Office for National Statistics, 2019). Screening programs have been shown to reduce mortality in many types of cancers [
4,
319]
-[
323]. Many assays and platforms have been established to employ ctDNA technology in early cancer detection. These assays and platforms include CancerSEEK, DETECT-A, Galleri assay, whole-genome sequencing for copy number variation (WGS-CNV), and whole-genome bisulfite sequencing (WGBS) [
324]
-[
328].
A recent study with a targeted multi-cancer early detection (MCED) approach evaluated more than 100,000 informative methylation regions among 6,689 participants (including 2,482 cancer patients in more than 50 cancer types). The study showed high sensitivity in detecting cancers in its early stages [
329]. Beyond methylation profiling, fragmentomics and topological analyses are alternative approaches to ctDNA analysis [
330,
331].
AI has also been introduced to enhance the analysis of huge ctDNA databases to increase the sensitivity and specificity for early cancer detection. In a recent study, a bio-hybrid platform comprising trained detection canines and AI tools was employed to detect breast, lung, prostate, and colorectal cancer in breath samples of 1386 participants. The results demonstrated high sensitivity and specificity and enables early-stage cancer detection [
332].
The promise of ctDNA assays in early cancer detection may be further enhanced by our understanding of ctDNA kinetics and the relationship of ctDNA fraction that may complement conventional pathological tumour staging. This understanding may identify patients with tumors that are more likely to recur following surgical intervention and in whom neoadjuvant and adjuvant treatment can be tailored accordingly.
7. Cancer Diagnosis
Once cancer is suspected, a definitive diagnosis typically requires histopathology. These techniques not only confirm malignancy but also classify cancer by subtype, grade, and stage.
7.1. History
In ancient times, the diagnosis of cancer was rudimentary, primarily based on visual and palpable observations. The advent of the microscope in the 17th century allowed scientists to examine cells and tissues more closely, leading to the discovery of certain cancerous cells. By the 19th century, advancements in histopathology and the establishment of laboratory medicine significantly improved the accuracy of cancer diagnoses.
In modern time, cancer diagnosis usually involves personal and family medical history, physical examination, lab testing, imaging, and biopsy, the last of which is often the only and final test to either confirm or deny a cancer diagnosis. These tests often follow a positive screening test or a symptom.
Some common types of lab tests used to help diagnose cancer include blood chemistry tests, complete blood count (CBC), cytogenetic analysis, immunophenotyping, liquid biopsy, sputum cytology, tumor marker tests, urinalysis, and urine cytology. Imaging tests used in cancer diagnosis include CT, MRI, nuclear scan, bone scan, PET scan, ultrasound, and X-rays.
The traditional biopsy is a procedure to remove a piece of tissue or a sample of cells from the body so that it can be tested in a laboratory. Types of tissue biopsy include needle biopsy, endoscopic biopsy, skin biopsy, bone marrow biopsy, and surgical biopsy. These biopsies are all tissue-based invasive biopsy. Tissue biopsy has been the gold standard in cancer diagnosis, which allows for the typing and grading of the tumor cells and the identification of target expression for targeted therapies.
Tissue biopsies, typically performed under image guidance, are specialized invasive procedures associated with notable morbidity and financial considerations. These interventions often require patients to attend tertiary care centers equipped with advanced facilities. Beyond logistical challenges, several factors can limit tumor tissue acquisition, including difficulty in accessing the lesion, proximity of the tumor to critical organs or vascular structures, patient comorbidities, and patient hesitancy due to procedural risks. In many cases, repeat biopsies are clinically indicated.
As the world enters the era of precision oncology, cancer diagnosis tools have been modernized significantly to improve the accuracy of diagnosis and are more convenient for patients with lower costs and higher efficiency. In particular, non-invasive biopsies have made great advances.
7.2. Cancer Diagnosis by Liquid Biopsy
We have discussed the role of liquid biopsy in the early detection of cancer. Recently, CTCs have emerged as a compelling reservoir of biomarkers with profound implications for cancer diagnosis, prognosis, and recurrence prediction. For cancer diagnostics, the identification of CTCs in the bloodstream holds the potential for signaling the presence of a primary tumor. CTCs offer a distinctive advantage as they represent intact tumor cells released from primary or metastatic tumors. This unique characteristic allows CTCs to be used as a source of comprehensive information across various molecular levels, encompassing DNA, RNA, protein, and metabolites. Therefore, analysis of CTC provides more comprehensive and accurate early diagnosis of cancer. CTC monitoring uses routine blood drawings, making it less invasive and more convenient than tissue biopsies, and offers an easier way to detect and track cancer progression.
7.3. Diagnosis with Molecular Imaging
Cancer molecular imaging is the non-invasive visualization of molecular and cellular processes characteristic to neoplasia, such as proliferation, glucose metabolism, and re-captor expression. Their inherent characteristic of visualization of malignant cells has the potential to enhance cancer diagnosis and staging on multiple levels [
333]. In general, molecular imaging plays a vital role in cancer diagnosis by enabling early detection of cancer at the molecular level, accurate staging and assessment of tumor extent, identification of specific molecular targets for therapy, and monitoring of treatment response and disease progression.
Molecular imaging applications can make properties of carcinogenesis visible at much earlier time points because alterations on the cellular level are targeted and can potentially be detected as soon as they occur. For example, abnormalities in malignant cells’ glucose metabolism occur at very early time points in carcinogenesis [
334]. While differentiation between benign and malignant tumors on conventional CT and MRI can be difficult, molecular imaging allows for a much better assessment of tumor because functional properties of malignant cells are visualized.
Incorporation of AI into molecular imaging and radiomics have offered significant opportunities for advancement. Numerous dynamic applications of AI exist, including image interpretation and classification, data organization, information mining, storage, and integration, and much more. AI is anticipated to greatly assist pathologists in enhancing diagnostic specificity because of its broad application in biomedical imaging technology [
335,
336]
Future directions for molecular imaging in cancer diagnosis include nanotechnology, multimodal imaging, and radiomics and AI. Nanoparticles can target tumor cells and cross cellular membranes, which may lead to highly sensitive imaging agents with therapeutic capabilities. Combining various imaging techniques, such as PET/MRI or PET/CT, provides more detailed multi-layer information, which may become standard in cancer diagnosis. Moreover, incorporation of AI into radiomics will enhance diagnostic accuracy and sensitivity.
Simultaneously, progress in imaging equipment, innovative algorithms, and AI has opened avenues to increase the efficiency and accuracy of cancer diagnosis.
8. Future Perspectives and Conclusions
Despite being the most developed area in precision medicine, precision oncology is still in its early stage.
While the innovative technologies are still emerging, the focus of the immediate future is to integrate the vast data generated by various methods. We have seen a clear effort in the scientific community to achieve this. AI has rapidly emerged as a transformative force and may play a vital role in this regard. The convergence of AI and precision medicine promises to revolutionize health care. AI leverages sophisticated computation and inference to generate insights, enables the system to reason and learn, and empowers clinician decision making through augmented intelligence [
131,
337]. However, we also face implication barriers and ethical challenges that need to be overcome. These challenges include algorithmic bias, over-reliance, best data analytics, computational power, transparency, and impact on the healthcare workforce [
130,
131].
AI enables comprehensive analysis of varied data, enhancing disease characterization, prognosis, and treatment prediction. However, issues like interpretability, reliability, generalizability, and ethics remain significant as these tools move from research to clinical use [
130,
131].
As we need to further understand the biology of tumor cells, emerging and future studies will explore intratumor heterogeneity and consider tumor cells and TME as one ecosystem to understand the interactions among tumor and non-tumor cells withing the ecosystem. Cancer driver genes and clonal expansion concepts have advanced our understanding of tumor initiation enormously and will continue to be developed for a complete understanding of the transition of cells from pre-malignant to malignant. This is crucial for early and accurate intervention to prevent cancer.
Pan-cancer analysis has gained momentum recently and may have profound implication in future precision medicine including cancer subtype stratification and targeted treatment. It is possible that cancers can be re-classified not only by cancer cells but also by other cell types in the TME. For example, reclassification of cancer by immune cells subtypes across traditional defined cancer types could maximize the efficacy of immunotherapy [
2,
239,
338].
Despite the rapid development, well-accepted concepts and principles, accumulated data, and acknowledged merits of precision oncology, its full potential for advancing cancer prevention and treatment remains unrealized due to the vast translational challenges. To achieve of the true potential of precision oncology, future studies must focus on overcoming these translation challenges including clinical infrastructure, economic burden, regulation, health care policy, and administrative alignment.
Author Contributions
All three authors R.C.W., D. Q. and Z.W. were involved in the drafting and revision of the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
Our research was funded in part by grants from the Canadian Institutes of Health Research (CIHR) to Z.W.
Acknowledgments
This work was supported by CIHR grants to Z.W.
Conflicts of Interest
The authors declare no conflict of interest.
References
- National Research Council Committee on, A.F. f. D. a. N. T. o. D. in Toward Precision Medicine: Building a Knowledge Network for Biomedical Research and a New Taxonomy of Disease (National Academies Press (US) Copyright © 2011, National Academy of Sciences., 2011).
- Wang, R.C.; Wang, Z. Precision Medicine: Disease Subtyping and Tailored Treatment. Cancers 2023, 15, 3837. [Google Scholar] [CrossRef]
- Doroshow, D.B.; Doroshow, J.H. Genomics and the History of Precision Oncology. Surgical oncology clinics of North America 2020, 29, 35–49. [Google Scholar] [CrossRef]
- Pich, O.; et al. The translational challenges of precision oncology. Cancer Cell 2022, 40, 458–478. [Google Scholar] [CrossRef]
- Tang, F.; et al. mRNA-Seq whole-transcriptome analysis of a single cell. Nature methods 2009, 6, 377–382. [Google Scholar] [CrossRef]
- Baysoy, A.; Bai, Z.; Satija, R.; Fan, R. The technological landscape and applications of single-cell multi-omics. Nature Reviews Molecular Cell Biology 2023, 24, 695–713. [Google Scholar] [CrossRef]
- Lim, J.; et al. Advances in single-cell omics and multiomics for high-resolution molecular profiling. Experimental & Molecular Medicine 2024, 56, 515–526. [Google Scholar] [CrossRef]
- Han, K.Y.; et al. SIDR: Simultaneous isolation and parallel sequencing of genomic DNA and total RNA from single cells. Genome research 2018, 28, 75–87. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez-Meira, A.; et al. Unravelling Intratumoral Heterogeneity through High-Sensitivity Single-Cell Mutational Analysis and Parallel RNA Sequencing. Molecular cell 2019, 73, 1292–1305.e1298. [Google Scholar] [CrossRef] [PubMed]
- Zachariadis, V.; Cheng, H.; Andrews, N.; Enge, M. A Highly Scalable Method for Joint Whole-Genome Sequencing and Gene-Expression Profiling of Single Cells. Molecular cell 2020, 80, 541–553.e545. [Google Scholar] [CrossRef] [PubMed]
- Yu, L.; et al. scONE-seq: A single-cell multi-omics method enables simultaneous dissection of phenotype and genotype heterogeneity from frozen tumors. Science Advances 2023, 9, eabp8901. [Google Scholar] [CrossRef]
- Angermueller, C.; et al. Parallel single-cell sequencing links transcriptional and epigenetic heterogeneity. Nature methods 2016, 13, 229–232. [Google Scholar] [CrossRef] [PubMed]
- Hu, Y.; et al. Simultaneous profiling of transcriptome and DNA methylome from a single cell. Genome biology 2016, 17, 88. [Google Scholar] [CrossRef]
- Gu, H.; et al. Smart-RRBS for single-cell methylome and transcriptome analysis. Nature protocols 2021, 16, 4004–4030. [Google Scholar] [CrossRef]
- Cao, J.; et al. Joint profiling of chromatin accessibility and gene expression in thousands of single cells. Science 2018, 361, 1380–1385. [Google Scholar] [CrossRef]
- Liu, L.; et al. Deconvolution of single-cell multi-omics layers reveals regulatory heterogeneity. Nature communications 2019, 10, 470. [Google Scholar] [CrossRef]
- Chen, S.; Lake, B.B.; Zhang, K. High-throughput sequencing of the transcriptome and chromatin accessibility in the same cell. Nature biotechnology 2019, 37, 1452–1457. [Google Scholar] [CrossRef] [PubMed]
- Zhu, C.; et al. An ultra high-throughput method for single-cell joint analysis of open chromatin and transcriptome. Nature structural & molecular biology 2019, 26, 1063–1070. [Google Scholar] [CrossRef]
- Ma, S.; et al. Chromatin Potential Identified by Shared Single-Cell Profiling of RNA and Chromatin. Cell 2020, 183, 1103–1116.e1120. [Google Scholar] [CrossRef]
- Xu, W.; et al. ISSAAC-seq enables sensitive and flexible multimodal profiling of chromatin accessibility and gene expression in single cells. Nature methods 2022, 19, 1243–1249. [Google Scholar] [CrossRef]
- Stoeckius, M.; et al. Simultaneous epitope and transcriptome measurement in single cells. Nature methods 2017, 14, 865–868. [Google Scholar] [CrossRef]
- Peterson, V.M.; et al. Multiplexed quantification of proteins and transcripts in single cells. Nature biotechnology 2017, 35, 936–939. [Google Scholar] [CrossRef]
- Hwang, B.; et al. SCITO-seq: Single-cell combinatorial indexed cytometry sequencing. Nature methods 2021, 18, 903–911. [Google Scholar] [CrossRef]
- Wu, H.; Kirita, Y.; Donnelly, E.L.; Humphreys, B.D. Advantages of Single-Nucleus over Single-Cell RNA Sequencing of Adult Kidney: Rare Cell Types and Novel Cell States Revealed in Fibrosis. Journal of the American Society of Nephrology: JASN 2019, 30, 23–32. [Google Scholar] [CrossRef] [PubMed]
- Wolfien, M.; et al. Single-Nucleus Sequencing of an Entire Mammalian Heart: Cell Type Composition and Velocity. Cells 2020, 9, 318. [Google Scholar] [CrossRef] [PubMed]
- Woodworth, M.B., Girskis, K. M.; Walsh, C.A. Building a lineage from single cells: Genetic techniques for cell lineage tracking. Nature reviews. Genetics 2017, 18, 230–244. [CrossRef]
- Palii, C.G.; et al. Single-Cell Proteomics Reveal that Quantitative Changes in Co-expressed Lineage-Specific Transcription Factors Determine Cell Fate. Cell stem cell 2019, 24, 812–820.e815. [Google Scholar] [CrossRef] [PubMed]
- Eyler, C.E.; et al. Single-cell lineage analysis reveals genetic and epigenetic interplay in glioblastoma drug resistance. Genome Biol 2020, 21, 174. [Google Scholar] [CrossRef]
- Gaiti, F.; et al. Epigenetic evolution and lineage histories of chronic lymphocytic leukaemia. Nature 2019, 569, 576–580. [Google Scholar] [CrossRef]
- Bian, X.; et al. Integration Analysis of Single-Cell Multi-Omics Reveals Prostate Cancer Heterogeneity. Advanced science (Weinheim, Baden-Wurttemberg, Germany) 2024, 11, e2305724. [Google Scholar] [CrossRef]
- Zhu, Q.; et al. Single cell multi-omics reveal intra-cell-line heterogeneity across human cancer cell lines. Nature communications 2023, 14, 8170. [Google Scholar] [CrossRef]
- Beneyto-Calabuig, S.; et al. Clonally resolved single-cell multi-omics identifies routes of cellular differentiation in acute myeloid leukemia. Cell stem cell 2023, 30, 706–721.e708. [Google Scholar] [CrossRef]
- Wang, X.; et al. Single-cell multi-omics sequencing uncovers region-specific plasticity of glioblastoma for complementary therapeutic targeting. Sci Adv 2024, 10, eadn4306. [Google Scholar] [CrossRef]
- Rodriguez-Meira, A.; et al. Single-cell multi-omics identifies chronic inflammation as a driver of TP53-mutant leukemic evolution. Nature genetics 2023, 55, 1531–1541. [Google Scholar] [CrossRef]
- Wang, Y.; et al. Single-cell multi-omics reveals that FABP1 + renal cell carcinoma drive tumor angiogenesis through the PLG-PLAT axis under fatty acid reprogramming. Molecular cancer 2025, 24, 179. [Google Scholar] [CrossRef] [PubMed]
- Long, E.; et al. Context-aware single-cell multiomics approach identifies cell-type-specific lung cancer susceptibility genes. Nature communications 2024, 15, 7995. [Google Scholar] [CrossRef] [PubMed]
- Bai, Z.; et al. Single-cell CAR T atlas reveals type 2 function in 8-year leukaemia remission. Nature 2024, 634, 702–711. [Google Scholar] [CrossRef]
- Liu, B.; Zhang, Y.; Wang, D.; Hu, X.; Zhang, Z. Single-cell meta-analyses reveal responses of tumor-reactive CXCL13(+) T cells to immune-checkpoint blockade. Nature cancer 2022, 3, 1123–1136. [Google Scholar] [CrossRef]
- Liu, X.; et al. Spatial multi-omics: Deciphering technological landscape of integration of multi-omics and its applications. Journal of Hematology & Oncology 2024, 17, 72. [Google Scholar] [CrossRef]
- Vandereyken, K.; Sifrim, A.; Thienpont, B.; Voet, T. Methods and applications for single-cell and spatial multi-omics. Nature reviews. Genetics 2023, 24, 494–515. [Google Scholar] [CrossRef] [PubMed]
- Du, Y.; Ding, X.; Ye, Y. The spatial multi-omics revolution in cancer therapy: Precision redefined. Cell Reports Medicine 2024, 5. [Google Scholar] [CrossRef]
- Ravi, V.M.; et al. Spatially resolved multi-omics deciphers bidirectional tumor-host interdependence in glioblastoma. Cancer Cell 2022, 40, 639–655.e613. [Google Scholar] [CrossRef]
- Brady, L.; et al. Inter- and intra-tumor heterogeneity of metastatic prostate cancer determined by digital spatial gene expression profiling. Nature communications 2021, 12, 1426. [Google Scholar] [CrossRef] [PubMed]
- Song, X.; et al. Spatial multi-omics revealed the impact of tumor ecosystem heterogeneity on immunotherapy efficacy in patients with advanced non-small cell lung cancer treated with bispecific antibody. Journal for immunotherapy of cancer 2023, 11. [Google Scholar] [CrossRef]
- Zwing, N.; et al. Mapping immune activity in HPV-negative head and neck squamous cell carcinoma: A spatial multiomics analysis. Journal for immunotherapy of cancer 2025, 13. [Google Scholar] [CrossRef]
- Gao, Y.; et al. Spatial multi-omics reveals the potential involvement of SPP1<sup>+</sup> fibroblasts in determining metabolic heterogeneity and promoting metastatic growth of colorectal cancer liver metastasis. Molecular Therapy 2025, 33, 3680–3700. [Google Scholar] [CrossRef]
- Gao, Y.; et al. Spatial multi-omics profiling of breast cancer oligo-recurrent lung metastasis. Oncogene 2025, 44, 2268–2282. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.; et al. Spatial multi-omics analysis of tumor-stroma boundary cell features for predicting breast cancer progression and therapy response. Frontiers in cell and developmental biology 2025, 13, 1570696. [Google Scholar] [CrossRef] [PubMed]
- Sun, C.; et al. Spatially resolved multi-omics highlights cell-specific metabolic remodeling and interactions in gastric cancer. Nature communications 2023, 14, 2692. [Google Scholar] [CrossRef]
- Zhao, F.; et al. Integrated spatial multi-omics profiling of Fusobacterium nucleatum in breast cancer unveils its role in tumour microenvironment modulation and cancer progression. Clinical and translational medicine 2025, 15, e70273. [Google Scholar] [CrossRef]
- Mo, C.-K.; et al. Tumour evolution and microenvironment interactions in 2D and 3D space. Nature 2024, 634, 1178–1186. [Google Scholar] [CrossRef]
- Islam, M.; et al. Temporal recording of mammalian development and precancer. Nature 2024, 634, 1187–1195. [Google Scholar] [CrossRef] [PubMed]
- Esplin, E.D.; et al. Multiomic analysis of familial adenomatous polyposis reveals molecular pathways associated with early tumorigenesis. Nature cancer 2024, 5, 1737–1753. [Google Scholar] [CrossRef] [PubMed]
- Hammerl, D.; et al. Spatial immunophenotypes predict response to anti-PD1 treatment and capture distinct paths of T cell evasion in triple negative breast cancer. Nature communications 2021, 12, 5668. [Google Scholar] [CrossRef]
- Li, S.; et al. Integrative multi-omics analysis reveals a novel subtype of hepatocellular carcinoma with biological and clinical relevance. Frontiers in immunology 2024, 15, 1517312. [Google Scholar] [CrossRef]
- Liu, Y.; Dong, G.; Yu, J.; Liang, P. Integration of single-cell and spatial transcriptomics reveals fibroblast subtypes in hepatocellular carcinoma: Spatial distribution, differentiation trajectories, and therapeutic potential. Journal of translational medicine 2025, 23, 198. [Google Scholar] [CrossRef]
- Yu, Z.H.; et al. Integrating spatial and single-cell transcriptomes reveals the role of COL1A2(+) MMP1(+/-) cancer-associated fibroblasts in ER-positive breast cancer. Cancer cell international 2025, 25, 82. [Google Scholar] [CrossRef]
- Ma, Y.; et al. Integrated single cell spatial multi-omics landscape of WHO grades 2-4 diffuse gliomas identifies locoregional metabolomic regulators of glioma growth. bioRxiv: The preprint server for biology 2025. [Google Scholar] [CrossRef]
- Pai, B.; et al. Spatial Multi-omics Defines a Shared Tumor Infiltrative Signature at the Resection Margin in High-Grade Gliomas. Cancer research. 2025. [Google Scholar] [CrossRef]
- Prakrithi, P.; et al. Integrating 12 Spatial and Single Cell Technologies to Characterise Tumour Neighbourhoods and Cellular Interactions in three Skin Cancer Types. bioRxiv: The preprint server for biology 2025. [Google Scholar] [CrossRef]
- Xu, Y.; et al. Single-cell MultiOmics and spatial transcriptomics demonstrate neuroblastoma developmental plasticity. Developmental cell. 2025. [Google Scholar] [CrossRef]
- Xu, Y.; et al. Multimodal single cell-resolved spatial proteomics reveal pancreatic tumor heterogeneity. Nature communications 2024, 15, 10100. [Google Scholar] [CrossRef]
- Yousuf, S.; et al. Spatially Resolved Multi-Omics Single-Cell Analyses Inform Mechanisms of Immune Dysfunction in Pancreatic Cancer. Gastroenterology 2023, 165, 891–908.e814. [Google Scholar] [CrossRef] [PubMed]
- LeSavage, B.L., Suhar, R.A., Broguiere, N., Lutolf, M. P.; Heilshorn, S.C. Next-generation cancer organoids. Nature materials 2022, 21, 143–159. [CrossRef]
- Qu, S.; et al. Patient-derived organoids in human cancer: A platform for fundamental research and precision medicine. Molecular biomedicine 2024, 5, 6. [Google Scholar] [CrossRef]
- Takagi, K.; Takagi, M.; Hiyama, G.; Goda, K. A deep-learning model for characterizing tumor heterogeneity using patient-derived organoids. Scientific Reports 2024, 14, 22769. [Google Scholar] [CrossRef]
- Thorel, L.; et al. Patient-derived tumor organoids: A new avenue for preclinical research and precision medicine in oncology. Exp Mol Med 2024, 56, 1531–1551. [Google Scholar] [CrossRef] [PubMed]
- Rauner, G.; et al. Single-cell organogenesis captures complex breast tissue formation in three dimensions. Development (Cambridge, England) 2025, 152. [Google Scholar] [CrossRef]
- Zhao, Z.; et al. Organoids. Nature Reviews Methods Primers 2022, 2, 94. [Google Scholar] [CrossRef]
- Sutherland, R.M., Inch, W.R., McCredie, J. A.; Kruuv, J. A multi-component radiation survival curve using an in vitro tumour model. International journal of radiation biology and related studies in physics, chemistry, and medicine 1970, 18, 491–495. [CrossRef] [PubMed]
- Li, M.L.; et al. Influence of a reconstituted basement membrane and its components on casein gene expression and secretion in mouse mammary epithelial cells. Proceedings of the National Academy of Sciences of the United States of America 1987, 84, 136–140. [Google Scholar] [CrossRef]
- Thomson, J.A.; et al. Embryonic stem cell lines derived from human blastocysts. Science 1998, 282, 1145–1147. [Google Scholar] [CrossRef]
- Takahashi, K.; Yamanaka, S. Induction of pluripotent stem cells from mouse embryonic and adult fibroblast cultures by defined factors. Cell 2006, 126, 663–676. [Google Scholar] [CrossRef]
- Sato, T.; et al. Single Lgr5 stem cells build crypt-villus structures in vitro without a mesenchymal niche. Nature 2009, 459, 262–265. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.H.; et al. Tumor Evolution and Drug Response in Patient-Derived Organoid Models of Bladder Cancer. Cell 2018, 173, 515–528.e517. [Google Scholar] [CrossRef] [PubMed]
- Farshadi, E.A.; et al. Organoids Derived from Neoadjuvant FOLFIRINOX Patients Recapitulate Therapy Resistance in Pancreatic Ductal Adenocarcinoma. Clinical cancer research: An official journal of the American Association for Cancer Research 2021, 27, 6602–6612. [Google Scholar] [CrossRef]
- Huang, L.; et al. PDX-derived organoids model in vivo drug response and secrete biomarkers. JCI insight 2020, 5. [Google Scholar] [CrossRef] [PubMed]
- Hadj Bachir, E.; et al. A new pancreatic adenocarcinoma-derived organoid model of acquired chemoresistance to FOLFIRINOX: First insight of the underlying mechanisms. Biology of the cell 2022, 114, 32–55. [Google Scholar] [CrossRef]
- Tiriac, H.; et al. Organoid profiling identifies common responders to chemotherapy in pancreatic cancer. Cancer discovery 2018, 8, 1112–1129. [Google Scholar] [CrossRef]
- Fujii, M.; et al. A colorectal tumor organoid library demonstrates progressive loss of niche factor requirements during tumorigenesis. Cell stem cell 2016, 18, 827–838. [Google Scholar] [CrossRef]
- Neal, J.T.; et al. Organoid modeling of the tumor immune microenvironment. Cell 2018, 175, 1972–1988.e1916. [Google Scholar] [CrossRef]
- Schnalzger, T.E.; et al. 3D model for CAR-mediated cytotoxicity using patient-derived colorectal cancer organoids. The EMBO journal 2019, 38, e100928. [Google Scholar] [CrossRef] [PubMed]
- Vlachogiannis, G.; et al. Patient-derived organoids model treatment response of metastatic gastrointestinal cancers. Science 2018, 359, 920–926. [Google Scholar] [CrossRef]
- Kim, M.; et al. Patient-derived lung cancer organoids as in vitro cancer models for therapeutic screening. Nature communications 2019, 10, 3991. [Google Scholar] [CrossRef]
- Driehuis, E.; et al. Pancreatic cancer organoids recapitulate disease and allow personalized drug screening. Proceedings of the National Academy of Sciences of the United States of America 2019, 116, 26580–26590. [Google Scholar] [CrossRef]
- Kondo, J.; et al. High-throughput screening in colorectal cancer tissue-originated spheroids. Cancer science 2019, 110, 345–355. [Google Scholar] [CrossRef]
- Yan, H.H. N.; et al. A Comprehensive Human Gastric Cancer Organoid Biobank Captures Tumor Subtype Heterogeneity and Enables Therapeutic Screening. Cell stem cell 2018, 23, 882–897.e811. [Google Scholar] [CrossRef] [PubMed]
- Verduin, M.; Hoeben, A.; De Ruysscher, D.; Vooijs, M. Patient-Derived Cancer Organoids as Predictors of Treatment Response. Frontiers in oncology 2021, 11, 641980. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Chang, S.; Li, G.; Sun, Y. Application of liquid biopsy in precision medicine: Opportunities and challenges. Frontiers of medicine 2017, 11, 522–527. [Google Scholar] [CrossRef]
- Adhit, K.K., Wanjari, A., Menon, S.; K, S. Liquid Biopsy: An Evolving Paradigm for Non-invasive Disease Diagnosis and Monitoring in Medicine. Cureus 2023, 15, e50176. [CrossRef]
- Dipasquale, A.; Pisapia, P.; Reduzzi, C. Liquid biopsy through non-blood fluids: The show must go on. The journal of liquid biopsy 2024, 6, 100272. [Google Scholar] [CrossRef]
- Chacko, N.; Ankri, R. Non-invasive early-stage cancer detection: Current methods and future perspectives. Clinical and experimental medicine 2024, 25, 17. [Google Scholar] [CrossRef]
- Ashworth, T. A case of cancer in which cells similar to those in the tumours were seen in the blood after death. Aust Med J. 1869, 14, 146. [Google Scholar]
- Allard, W.J.; et al. Tumor cells circulate in the peripheral blood of all major carcinomas but not in healthy subjects or patients with nonmalignant diseases. Clinical cancer research: An official journal of the American Association for Cancer Research 2004, 10, 6897–6904. [Google Scholar] [CrossRef]
- Dai, C.S.; et al. Circulating tumor cells: Blood-based detection, molecular biology, and clinical applications. Cancer Cell 2025, 43, 1399–1422. [Google Scholar] [CrossRef] [PubMed]
- Gaya, A.; et al. Evaluation of circulating tumor cell clusters for pan-cancer noninvasive diagnostic triaging. Cancer cytopathology 2021, 129, 226–238. [Google Scholar] [CrossRef] [PubMed]
- Edd, J.F.; et al. Isolation of circulating tumor cells. iScience 2022, 25, 104696. [Google Scholar] [CrossRef]
- Kakiuchi, N.; et al. Frequent mutations that converge on the NFKBIZ pathway in ulcerative colitis. Nature 2020, 577, 260–265. [Google Scholar] [CrossRef]
- Leon, S.A., Shapiro, B., Sklaroff, D. M.; Yaros, M.J. Free DNA in the serum of cancer patients and the effect of therapy. Cancer research 1977, 37, 646–650.
- Diehl, F.; et al. Circulating mutant DNA to assess tumor dynamics. Nature medicine 2008, 14, 985–990. [Google Scholar] [CrossRef]
- Chen, B.C.; et al. Rac1 regulates peptidoglycan-induced nuclear factor-kappaB activation and cyclooxygenase-2 expression in RAW 264.7 macrophages by activating the phosphatidylinositol 3-kinase/Akt pathway. Mol Immunol 2009, 46, 1179–1188. [Google Scholar] [CrossRef]
- Kuang, Y.; et al. Noninvasive detection of EGFR T790M in gefitinib or erlotinib resistant non-small cell lung cancer. Clinical cancer research: An official journal of the American Association for Cancer Research 2009, 15, 2630–2636. [Google Scholar] [CrossRef]
- Hsieh, R.W.; Symonds, L.K.; Siu, J.; Cohen, S.A. in International Review of Cell and Molecular Biology Vol. 391 (eds Lorenzo Galluzzi & Sheila Spada) 43-93 (Academic Press, 2025).
- Chabon, J.J.; et al. Integrating genomic features for non-invasive early lung cancer detection. Nature 2020, 580, 245–251. [Google Scholar] [CrossRef]
- Parums, D.V. A Review of Circulating Tumor DNA (ctDNA) and the Liquid Biopsy in Cancer Diagnosis, Screening, and Monitoring Treatment Response. Medical science monitor: International medical journal of experimental and clinical research 2025, 31, e949300. [Google Scholar] [CrossRef]
- Pascual, J.; et al. ESMO recommendations on the use of circulating tumour DNA assays for patients with cancer: A report from the ESMO Precision Medicine Working Group. Annals of oncology: Official journal of the European Society for Medical Oncology 2022, 33, 750–768. [Google Scholar] [CrossRef]
- Jiang, P.; et al. Preferred end coordinates and somatic variants as signatures of circulating tumor DNA associated with hepatocellular carcinoma. Proceedings of the National Academy of Sciences of the United States of America 2018, 115, e10925–e10933. [Google Scholar] [CrossRef]
- Margolis, E.; et al. Predicting high-grade prostate cancer at initial biopsy: Clinical performance of the ExoDx (EPI) Prostate Intelliscore test in three independent prospective studies. Prostate Cancer and Prostatic Diseases 2022, 25, 296–301. [Google Scholar] [CrossRef]
- Chung, D.C.; et al. A Cell-free DNA Blood-Based Test for Colorectal Cancer Screening. The New England journal of medicine 2024, 390, 973–983. [Google Scholar] [CrossRef] [PubMed]
- Shirley, M. Epi proColon(®) for Colorectal Cancer Screening: A Profile of Its Use in the USA. Molecular diagnosis & therapy 2020, 24, 497–503. [Google Scholar] [CrossRef]
- Banavar, G.; et al. Detecting salivary host and microbiome RNA signature for aiding diagnosis of oral and throat cancer. Oral oncology 2023, 145, 106480. [Google Scholar] [CrossRef] [PubMed]
- Wang, W.; He, Y.; Yang, F.; Chen, K. Current and emerging applications of liquid biopsy in pan-cancer. Translational oncology 2023, 34, 101720. [Google Scholar] [CrossRef] [PubMed]
- Cohen, J.D.; et al. Detection and localization of surgically resectable cancers with a multi-analyte blood test. Science 2018, 359, 926–930. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; et al. Non-invasive early detection of cancer four years before conventional diagnosis using a blood test. Nature communications 2020, 11, 3475. [Google Scholar] [CrossRef] [PubMed]
- Phallen, J.; et al. Direct detection of early-stage cancers using circulating tumor DNA. Science translational medicine 2017, 9, eaan2415. [Google Scholar] [CrossRef]
- Yang, X.; et al. Wnt signaling in triple-negative breast cancers: Its roles in molecular subtyping and cancer cell stemness and its crosstalk with non-coding RNAs. Life sciences 2022, 300, 120565. [Google Scholar] [CrossRef]
- Dempsey, A.A.; et al. Aristotle: A single blood test for pan-cancer screening. Journal of Clinical Oncology 2020, 38, e15037–e15037. [Google Scholar] [CrossRef]
- Nicholson, B.D.; et al. Multi-cancer early detection test in symptomatic patients referred for cancer investigation in England and Wales (SYMPLIFY): A large-scale, observational cohort study. The Lancet Oncology 2023, 24, 733–743. [Google Scholar] [CrossRef]
- Neal, R.D.; et al. Cell-Free DNA-Based Multi-Cancer Early Detection Test in an Asymptomatic Screening Population (NHS-Galleri): Design of a Pragmatic, Prospective Randomised Controlled Trial. Cancers 2022, 14. [Google Scholar] [CrossRef]
- Schrag, D.; et al. Blood-based tests for multicancer early detection (PATHFINDER): A prospective cohort study. The Lancet 2023, 402, 1251–1260. [Google Scholar] [CrossRef]
- Hao, X.; et al. Exosome-Based Liquid Biopsy in Early Screening and Diagnosis of Cancers. Dose-response: A publication of International Hormesis Society 2025, 23, 15593258251344480. [Google Scholar] [CrossRef]
- Theel, E.K.; Schwaminger, S.P. Microfluidic Approaches for Affinity-Based Exosome Separation. International journal of molecular sciences 2022, 23. [Google Scholar] [CrossRef] [PubMed]
- Li, G.; Tang, W.; Yang, F. Cancer Liquid Biopsy Using Integrated Microfluidic Exosome Analysis Platforms. Biotechnology journal 2020, 15, e1900225. [Google Scholar] [CrossRef] [PubMed]
- Yu, W.; et al. Exosome-based liquid biopsies in cancer: Opportunities and challenges. Annals of Oncology 2021, 32, 466–477. [Google Scholar] [CrossRef]
- Juweid, M.E.; et al. Beyond fluorodeoxyglucose: Molecular imaging of cancer in precision medicine. CA: A cancer journal for clinicians 2025, 75, 226–242. [Google Scholar] [CrossRef]
- Wang, T.; Ni, Y.; Liu, L. Innovative Imaging Techniques for Advancing Cancer Diagnosis and Treatment. Cancers 2024, 16. [Google Scholar] [CrossRef]
- Bai, J.-W.; Qiu, S.-Q.; Zhang, G.-J. Molecular and functional imaging in cancer-targeted therapy: Current applications and future directions. Signal transduction and targeted therapy 2023, 8, 89. [Google Scholar] [CrossRef]
- Antonelli, L., Guarracino, M.R., Maddalena, L.; Sangiovanni, M. Integrating imaging and omics data: A review. Biomedical Signal Processing and Control 2019, 52, 264–280. [CrossRef]
- Shui, L.; et al. The Era of Radiogenomics in Precision Medicine: An Emerging Approach to Support Diagnosis, Treatment Decisions, and Prognostication in Oncology. Frontiers in oncology 2020, 10, 570465. [Google Scholar] [CrossRef] [PubMed]
- Martínez-García, M.; Hernández-Lemus, E. Data Integration Challenges for Machine Learning in Precision Medicine. Frontiers in medicine 2021, 8, 784455. [Google Scholar] [CrossRef]
- Basubrin, O. Current Status and Future of Artificial Intelligence in Medicine. Cureus 2025, 17, e77561. [Google Scholar] [CrossRef]
- Bellini, V.; et al. Understanding basic principles of Artificial Intelligence: A practical guide for intensivists. Acta bio-medica: Atenei Parmensis 2022, 93, e2022297. [Google Scholar] [CrossRef]
- Wu, H.; et al. A survey on clinical natural language processing in the United Kingdom from 2007 to 2022. NPJ digital medicine 2022, 5, 186. [Google Scholar] [CrossRef]
- Lotter, W.; et al. Artificial Intelligence in Oncology: Current Landscape, Challenges, and Future Directions. Cancer discovery 2024, 14, 711–726. [Google Scholar] [CrossRef]
- Lång, K.; et al. Artificial intelligence-supported screen reading versus standard double reading in the Mammography Screening with Artificial Intelligence trial (MASAI): A clinical safety analysis of a randomised, controlled, non-inferiority, single-blinded, screening accuracy study. The Lancet. Oncology 2023, 24, 936–944. [Google Scholar] [CrossRef]
- Yala, A.; et al. Multi-Institutional Validation of a Mammography-Based Breast Cancer Risk Model. Journal of clinical oncology: Official journal of the American Society of Clinical Oncology 2022, 40, 1732–1740. [Google Scholar] [CrossRef]
- Arasu, V.A.; et al. Comparison of Mammography AI Algorithms with a Clinical Risk Model for 5-year Breast Cancer Risk Prediction: An Observational Study. Radiology 2023, 307, e222733. [Google Scholar] [CrossRef] [PubMed]
- Eriksson, M.; Czene, K.; Vachon, C.; Conant, E.F.; Hall, P. Long-Term Performance of an Image-Based Short-Term Risk Model for Breast Cancer. Journal of clinical oncology: Official journal of the American Society of Clinical Oncology 2023, 41, 2536–2545. [Google Scholar] [CrossRef]
- Zhou, D.; et al. Diagnostic evaluation of a deep learning model for optical diagnosis of colorectal cancer. Nature communications 2020, 11, 2961. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, O.F. Deep learning for colorectal polyp detection: Time for clinical implementation? The lancet. Gastroenterology & hepatology 2020, 5, 330–331. [Google Scholar] [CrossRef]
- Misawa, M.; Kudo, S.E.; Mori, Y. Computer-aided detection in real-world colonoscopy: Enhancing detection or offering false hope? The lancet. Gastroenterology & hepatology 2023, 8, 687–688. [Google Scholar] [CrossRef]
- Nam, J.G.; et al. AI Improves Nodule Detection on Chest Radiographs in a Health Screening Population: A Randomized Controlled Trial. Radiology 2023, 307, e221894. [Google Scholar] [CrossRef]
- Mikhael, P.G.; et al. Sybil: A Validated Deep Learning Model to Predict Future Lung Cancer Risk From a Single Low-Dose Chest Computed Tomography. Journal of clinical oncology: Official journal of the American Society of Clinical Oncology 2023, 41, 2191–2200. [Google Scholar] [CrossRef]
- Hamm, C.A.; et al. Interactive Explainable Deep Learning Model Informs Prostate Cancer Diagnosis at MRI. Radiology 2023, 307, e222276. [Google Scholar] [CrossRef]
- Sunoqrot, M.R.S., Saha, A., Hosseinzadeh, M., Elschot, M.; Huisman, H. Artificial intelligence for prostate MRI: Open datasets, available applications, and grand challenges. European radiology experimental 2022, 6, 35. [CrossRef]
- Kaur, R.; GholamHosseini, H.; Lindén, M. Advanced Deep Learning Models for Melanoma Diagnosis in Computer-Aided Skin Cancer Detection. Sensors (Basel, Switzerland) 2025, 25. [Google Scholar] [CrossRef]
- Ogier du Terrail, J.; et al. Federated learning for predicting histological response to neoadjuvant chemotherapy in triple-negative breast cancer. Nature medicine 2023, 29, 135–146. [Google Scholar] [CrossRef]
- Binder, A.; et al. Morphological and molecular breast cancer profiling through explainable machine learning. Nature Machine Intelligence 2021, 3, 355–366. [Google Scholar] [CrossRef]
- Skrede, O.J.; et al. Deep learning for prediction of colorectal cancer outcome: A discovery and validation study. Lancet (London, England) 2020, 395, 350–360. [Google Scholar] [CrossRef]
- AlDubayan, S.H.; et al. Detection of Pathogenic Variants With Germline Genetic Testing Using Deep Learning vs Standard Methods in Patients With Prostate Cancer and Melanoma. Jama 2020, 324, 1957–1969. [Google Scholar] [CrossRef]
- Sherman, M.A.; et al. Genome-wide mapping of somatic mutation rates uncovers drivers of cancer. Nature biotechnology 2022, 40, 1634–1643. [Google Scholar] [CrossRef] [PubMed]
- Cheng, J.; et al. Accurate proteome-wide missense variant effect prediction with AlphaMissense. Science 2023, 381, eadg7492. [Google Scholar] [CrossRef]
- Li, Q.; et al. CancerVar: An artificial intelligence-empowered platform for clinical interpretation of somatic mutations in cancer. Sci Adv 2022, 8, eabj1624. [Google Scholar] [CrossRef] [PubMed]
- Penson, A.; et al. Development of Genome-Derived Tumor Type Prediction to Inform Clinical Cancer Care. JAMA oncology 2020, 6, 84–91. [Google Scholar] [CrossRef] [PubMed]
- Moon, I.; et al. Machine learning for genetics-based classification and treatment response prediction in cancer of unknown primary. Nature medicine 2023, 29, 2057–2067. [Google Scholar] [CrossRef]
- Divate, M.; et al. Deep Learning-Based Pan-Cancer Classification Model Reveals Tissue-of-Origin Specific Gene Expression Signatures. Cancers 2022, 14. [Google Scholar] [CrossRef]
- Jagota, M.; et al. Cross-protein transfer learning substantially improves disease variant prediction. Genome Biol 2023, 24, 182. [Google Scholar] [CrossRef]
- Jurtz, V.; et al. NetMHCpan-4.0: Improved Peptide-MHC Class I Interaction Predictions Integrating Eluted Ligand and Peptide Binding Affinity Data. Journal of immunology (Baltimore, Md.: 1950) 2017, 199, 3360–3368. [Google Scholar] [CrossRef]
- Sarkizova, S.; et al. A large peptidome dataset improves HLA class I epitope prediction across most of the human population. Nature biotechnology 2020, 38, 199–209. [Google Scholar] [CrossRef]
- Sidhom, J.W., Larman, H.B., Pardoll, D. M.; Baras, A.S. DeepTCR is a deep learning framework for revealing sequence concepts within T-cell repertoires. Nature communications 2021, 12, 1605. [CrossRef]
- Lu, T.; et al. Deep learning-based prediction of the T cell receptor-antigen binding specificity. Nat Mach Intell 2021, 3, 864–875. [Google Scholar] [CrossRef]
- Saltz, J.; et al. Spatial Organization and Molecular Correlation of Tumor-Infiltrating Lymphocytes Using Deep Learning on Pathology Images. Cell Rep 2018, 23, 181–193.e187. [Google Scholar] [CrossRef] [PubMed]
- Shakya, M.; Patel, R.; Joshi, S. A comprehensive analysis of deep learning and transfer learning techniques for skin cancer classification. Scientific Reports 2025, 15, 4633. [Google Scholar] [CrossRef]
- Zhang, S.; et al. Tumor initiation and early tumorigenesis: Molecular mechanisms and interventional targets. Signal transduction and targeted therapy 2024, 9, 149. [Google Scholar] [CrossRef]
- Ostroverkhova, D.; Przytycka, T.M.; Panchenko, A.R. Cancer driver mutations: Predictions and reality. Trends in Molecular Medicine 2023, 29, 554–566. [Google Scholar] [CrossRef]
- Bailey, M.H.; et al. Comprehensive Characterization of Cancer Driver Genes and Mutations. Cell 2018, 173, 371–385.e318. [Google Scholar] [CrossRef] [PubMed]
- Martínez-Jiménez, F.; et al. A compendium of mutational cancer driver genes. Nature Reviews Cancer 2020, 20, 555–572. [Google Scholar] [CrossRef]
- Li, Y.; et al. Patterns of somatic structural variation in human cancer genomes. Nature 2020, 578, 112–121. [Google Scholar] [CrossRef]
- Drews, R.M.; et al. A pan-cancer compendium of chromosomal instability. Nature 2022, 606, 976–983. [Google Scholar] [CrossRef]
- Takeshima, H.; Ushijima, T. Accumulation of genetic and epigenetic alterations in normal cells and cancer risk. NPJ Precis Oncol 2019, 3, 7. [Google Scholar] [CrossRef] [PubMed]
- Hu, X.; et al. Evolution of DNA methylome from precancerous lesions to invasive lung adenocarcinomas. Nature communications 2021, 12, 687. [Google Scholar] [CrossRef] [PubMed]
- Kakiuchi, N.; Ogawa, S. Clonal expansion in non-cancer tissues. Nature reviews. Cancer 2021, 21, 239–256. [Google Scholar] [CrossRef] [PubMed]
- Li, R.; et al. A body map of somatic mutagenesis in morphologically normal human tissues. Nature 2021, 597, 398–403. [Google Scholar] [CrossRef]
- Moore, L.; et al. The mutational landscape of human somatic and germline cells. Nature 2021, 597, 381–386. [Google Scholar] [CrossRef]
- Colom, B.; Jones, P.H. Clonal analysis of stem cells in differentiation and disease. Current opinion in cell biology 2016, 43, 14–21. [Google Scholar] [CrossRef]
- Alexandrov, L.B.; et al. Signatures of mutational processes in human cancer. Nature 2013, 500, 415–421. [Google Scholar] [CrossRef]
- Alexandrov, L.B.; et al. The repertoire of mutational signatures in human cancer. Nature 2020, 578, 94–101. [Google Scholar] [CrossRef]
- Kucab, J.E.; et al. A Compendium of Mutational Signatures of Environmental Agents. Cell 2019, 177, 821–836.e816. [Google Scholar] [CrossRef]
- Zou, X.; et al. Validating the concept of mutational signatures with isogenic cell models. Nature communications 2018, 9, 1744. [Google Scholar] [CrossRef] [PubMed]
- Muiños, F.; Martínez-Jiménez, F.; Pich, O.; Gonzalez-Perez, A.; Lopez-Bigas, N. In silico saturation mutagenesis of cancer genes. Nature 2021, 596, 428–432. [Google Scholar] [CrossRef] [PubMed]
- Temko, D., Tomlinson, I.P.M., Severini, S., Schuster-Böckler, B.; Graham, T.A. The effects of mutational processes and selection on driver mutations across cancer types. Nature communications 2018, 9, 1857. [CrossRef] [PubMed]
- Riva, L.; et al. The mutational signature profile of known and suspected human carcinogens in mice. Nature genetics 2020, 52, 1189–1197. [Google Scholar] [CrossRef]
- Zhao, X.; et al. Genome-wide alterations of DNA methylation and hydroxymethylation in uroepithelial cells revealed potential carcinogenicity of halobenzoquinone disinfection byproducts. Environmental pollution (Barking, Essex: 1987) 2025, 384, 127001. [Google Scholar] [CrossRef]
- Seno, A.; et al. Genome-wide mapping of arsenic-activated Nrf2 reveals metabolic and epigenetic reprogramming in induced pluripotent stem cells. Redox biology 2025, 86, 103773. [Google Scholar] [CrossRef] [PubMed]
- Sadiq, I.Z. Environmental carcinogens and cancer Risk: Sustainable strategies for public health protection. Chemosphere 2025, 385, 144580. [Google Scholar] [CrossRef] [PubMed]
- Zhu, M.; et al. Somatic Mutations Increase Hepatic Clonal Fitness and Regeneration in Chronic Liver Disease. Cell 2019, 177, 608–621.e612. [Google Scholar] [CrossRef]
- Lou, Y.; et al. TNFAIP8 protein functions as a tumor suppressor in inflammation-associated colorectal tumorigenesis. Cell death & disease 2022, 13, 311. [Google Scholar] [CrossRef]
- Dong, W.; et al. Integrating single-cell and spatial transcriptomics reveals the cellular heterogeneity of vestibular schwannoma. NPJ Precis Oncol 2025, 9, 228. [Google Scholar] [CrossRef]
- Jun, S.H.; et al. Reconstructing clonal tree for phylo-phenotypic characterization of cancer using single-cell transcriptomics. Nature communications 2023, 14, 982. [Google Scholar] [CrossRef]
- Zuo, C.; et al. Elucidating tumor heterogeneity from spatially resolved transcriptomics data by multi-view graph collaborative learning. Nature communications 2022, 13, 5962. [Google Scholar] [CrossRef] [PubMed]
- Yu, X.; Liu, R.; Gao, W.; Wang, X.; Zhang, Y. Single-cell omics traces the heterogeneity of prostate cancer cells and the tumor microenvironment. Cellular & molecular biology letters 2023, 28, 38. [Google Scholar] [CrossRef]
- Quek, C.; et al. Single-cell spatial multiomics reveals tumor microenvironment vulnerabilities in cancer resistance to immunotherapy. Cell Rep 2024, 43, 114392. [Google Scholar] [CrossRef]
- Dagogo-Jack, I.; Shaw, A.T. Tumour heterogeneity and resistance to cancer therapies. Nature Reviews Clinical Oncology 2018, 15, 81–94. [Google Scholar] [CrossRef]
- Kanayama, K.; et al. Extrachromosomal DNA Dynamics Contribute to Intratumoral Receptor Tyrosine Kinase Genetic Heterogeneity and Drug Resistance in Gastric Cancer. Molecular cancer research: MCR 2025, 23, 503–514. [Google Scholar] [CrossRef]
- Corinaldesi, C.; et al. Single-cell transcriptomics of pediatric Burkitt lymphoma reveals intra-tumor heterogeneity and markers of therapy resistance. Leukemia 2025, 39, 189–198. [Google Scholar] [CrossRef]
- Alsaed, B.; et al. Intratumor heterogeneity of EGFR expression mediates targeted therapy resistance and formation of drug tolerant microenvironment. Nature communications 2025, 16, 28. [Google Scholar] [CrossRef]
- Liu, Y.; et al. Conserved spatial subtypes and cellular neighborhoods of cancer-associated fibroblasts revealed by single-cell spatial multi-omics. Cancer Cell 2025, 43, 905–924.e906. [Google Scholar] [CrossRef] [PubMed]
- Chen, M.-M.; et al. Integrated single-cell and spatial transcriptomics uncover distinct cellular subtypes involved in neural invasion in pancreatic cancer. Cancer Cell 2025, 43, 1656–1676.e1610. [Google Scholar] [CrossRef]
- Gao, Y.; et al. Spatial multi-omics reveals the potential involvement of SPP1(+) fibroblasts in determining metabolic heterogeneity and promoting metastatic growth of colorectal cancer liver metastasis. Molecular therapy: The journal of the American Society of Gene Therapy 2025, 33, 3680–3700. [Google Scholar] [CrossRef] [PubMed]
- Ogden, S.; et al. Phenotypic heterogeneity and plasticity in colorectal cancer metastasis. Cell Genomics 2025, 5. [Google Scholar] [CrossRef] [PubMed]
- Tufail, M.; Jiang, C.-H.; Li, N. Immune evasion in cancer: Mechanisms and cutting-edge therapeutic approaches. Signal transduction and targeted therapy 2025, 10, 227. [Google Scholar] [CrossRef] [PubMed]
- Chu, X.; et al. Integrative single-cell analysis of human colorectal cancer reveals patient stratification with distinct immune evasion mechanisms. Nature cancer 2024, 5, 1409–1426. [Google Scholar] [CrossRef]
- Enfield, K.S. S.; et al. Spatial Architecture of Myeloid and T Cells Orchestrates Immune Evasion and Clinical Outcome in Lung Cancer. Cancer discovery 2024, 14, 1018–1047. [Google Scholar] [CrossRef] [PubMed]
- Xiang, J.; et al. Integrating transcriptomics and machine learning for immunotherapy assessment in colorectal cancer. Cell Death Discovery 2024, 10, 162. [Google Scholar] [CrossRef] [PubMed]
- Saria, S.; Goldenberg, A. Subtyping: What It is and Its Role in Precision Medicine. IEEE Intelligent Systems 2015, 30, 70–75. [Google Scholar] [CrossRef]
- Verhaak, R.G.; et al. Integrated genomic analysis identifies clinically relevant subtypes of glioblastoma characterized by abnormalities in PDGFRA, IDH1, EGFR, and NF1. Cancer Cell 2010, 17, 98–110. [Google Scholar] [CrossRef]
- Wei, S.; et al. Ten Years of EWAS. Advanced science (Weinheim, Baden-Wurttemberg, Germany) 2021, 8, e2100727. [Google Scholar] [CrossRef]
- Carbone, A. Cancer Classification at the Crossroads. Cancers 2020, 12, 980. [Google Scholar] [CrossRef] [PubMed]
- Chapman, P.B.; et al. Improved survival with vemurafenib in melanoma with BRAF V600E mutation. The New England journal of medicine 2011, 364, 2507–2516. [Google Scholar] [CrossRef]
- Sinkala, M. Mutational landscape of cancer-driver genes across human cancers. Sci Rep 2023, 13, 12742. [Google Scholar] [CrossRef]
- Kinnersley, B.; et al. Analysis of 10,478 cancer genomes identifies candidate driver genes and opportunities for precision oncology. Nature genetics 2024, 56, 1868–1877. [Google Scholar] [CrossRef]
- Way, G.P.; et al. Machine Learning Detects Pan-cancer Ras Pathway Activation in The Cancer Genome Atlas. Cell Reports 2018, 23, 172–180.e173. [Google Scholar] [CrossRef]
- Wu, M.Y., Dai, D.Q., Zhang, X. F.; Zhu, Y. Cancer subtype discovery and biomarker identification via a new robust network clustering algorithm. PLoS ONE 2013, 8, e66256. [CrossRef]
- Drier, Y.; Sheffer, M.; Domany, E. Pathway-based personalized analysis of cancer. Proceedings of the National Academy of Sciences of the United States of America 2013, 110, 6388–6393. [Google Scholar] [CrossRef]
- Mallavarapu, T.; Hao, J.; Kim, Y.; Oh, J.H.; Kang, M. Pathway-based deep clustering for molecular subtyping of cancer. Methods (San Diego, Calif.) 2020, 173, 24–31. [Google Scholar] [CrossRef]
- Sanchez-Vega, F.; et al. Oncogenic Signaling Pathways in The Cancer Genome Atlas. Cell 2018, 173, 321–337.e310. [Google Scholar] [CrossRef]
- Lehmann, B.D.; et al. Identification of human triple-negative breast cancer subtypes and preclinical models for selection of targeted therapies. The Journal of clinical investigation 2011, 121, 2750–2767. [Google Scholar] [CrossRef] [PubMed]
- Burstein, M.D.; et al. Comprehensive genomic analysis identifies novel subtypes and targets of triple-negative breast cancer. Clinical cancer research: An official journal of the American Association for Cancer Research 2015, 21, 1688–1698. [Google Scholar] [CrossRef]
- Jiang, Y.Z.; et al. Genomic and Transcriptomic Landscape of Triple-Negative Breast Cancers: Subtypes and Treatment Strategies. Cancer Cell 2019, 35, 428–440.e425. [Google Scholar] [CrossRef]
- Xiao, Y.; et al. Comprehensive metabolomics expands precision medicine for triple-negative breast cancer. Cell research 2022, 32, 477–490. [Google Scholar] [CrossRef] [PubMed]
- Guinney, J.; et al. The consensus molecular subtypes of colorectal cancer. Nature medicine 2015, 21, 1350–1356. [Google Scholar] [CrossRef]
- Chemi, F.; et al. cfDNA methylome profiling for detection and subtyping of small cell lung cancers. Nature cancer 2022, 3, 1260–1270. [Google Scholar] [CrossRef]
- Visvader, J.E. Cells of origin in cancer. Nature 2011, 469, 314–322. [Google Scholar] [CrossRef] [PubMed]
- Hoadley, K.A.; et al. Cell-of-Origin Patterns Dominate the Molecular Classification of 10,000 Tumors from 33 Types of Cancer. Cell 2018, 173, 291–304.e296. [Google Scholar] [CrossRef]
- Berger, A.C.; et al. A Comprehensive Pan-Cancer Molecular Study of Gynecologic and Breast Cancers. Cancer Cell 2018, 33, 690–705.e699. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; et al. Comparative Molecular Analysis of Gastrointestinal Adenocarcinomas. Cancer Cell 2018, 33, 721–735.e728. [Google Scholar] [CrossRef]
- Campbell, J.D.; et al. Genomic, Pathway Network, and Immunologic Features Distinguishing Squamous Carcinomas. Cell Reports 2018, 23, 194–212.e196. [Google Scholar] [CrossRef]
- Ricketts, C.J.; et al. The Cancer Genome Atlas Comprehensive Molecular Characterization of Renal Cell Carcinoma. Cell Reports 2018, 23, 313–326.e315. [Google Scholar] [CrossRef]
- Flowers, B.M.; et al. Cell of Origin Influences Pancreatic Cancer Subtype. Cancer discovery 2021, 11, 660–677. [Google Scholar] [CrossRef]
- Scott, D.W.; et al. Determining cell-of-origin subtypes of diffuse large B-cell lymphoma using gene expression in formalin-fixed paraffin-embedded tissue. Blood 2014, 123, 1214–1217. [Google Scholar] [CrossRef]
- Yan, W.H.; et al. Cell-of-Origin Subtyping of Diffuse Large B-Cell Lymphoma by Using a qPCR-based Gene Expression Assay on Formalin-Fixed Paraffin-Embedded Tissues. Frontiers in oncology 2020, 10, 803. [Google Scholar] [CrossRef]
- Walker, J.S.; et al. Integrated genomics with refined cell-of-origin subtyping distinguishes subtype-specific mechanisms of treatment resistance and relapse in diffuse large B-cell lymphoma. Blood Cancer Journal 2025, 15, 120. [Google Scholar] [CrossRef] [PubMed]
- Ellrott, K.; et al. Classification of non-TCGA cancer samples to TCGA molecular subtypes using compact feature sets. Cancer Cell 2025, 43, 195–212.e111. [Google Scholar] [CrossRef]
- Rosenwald, A.; et al. The use of molecular profiling to predict survival after chemotherapy for diffuse large-B-cell lymphoma. The New England journal of medicine 2002, 346, 1937–1947. [Google Scholar] [CrossRef]
- Rutherford, S.C.; Leonard, J.P. DLBCL Cell of Origin: What Role Should It Play in Care Today? Oncology (Williston Park, N.Y.) 2018, 32, 445–449. [Google Scholar]
- Reinders, J.; et al. Platform independent protein-based cell-of-origin subtyping of diffuse large B-cell lymphoma in formalin-fixed paraffin-embedded tissue. Sci Rep 2020, 10, 7876. [Google Scholar] [CrossRef] [PubMed]
- Ding, L.; et al. Perspective on Oncogenic Processes at the End of the Beginning of Cancer Genomics. Cell 2018, 173, 305–320.e310. [Google Scholar] [CrossRef]
- Thorsson, V.; et al. The Immune Landscape of Cancer. Immunity 2018, 48, 812–830.e814. [Google Scholar] [CrossRef] [PubMed]
- Combes, A.J.; et al. Discovering dominant tumor immune archetypes in a pan-cancer census. Cell 2022, 185, 184–203.e119. [Google Scholar] [CrossRef]
- Gao, Q.; et al. Driver Fusions and Their Implications in the Development and Treatment of Human Cancers. Cell Reports 2018, 23, 227–238.e223. [Google Scholar] [CrossRef] [PubMed]
- Shi, Y.; et al. Pan-cancer oncogenic properties and therapeutic potential of SF3B4. Cancer Gene Therapy 2025, 32, 706–720. [Google Scholar] [CrossRef]
- Febres-Aldana, C.A.; et al. Pan-Cancer Analysis of Oncogenic MET Fusions Reveals Distinct Pathogenomic Subsets with Differential Sensitivity to MET-Targeted Therapy. Cancer discovery 2025, 15, 1141–1158. [Google Scholar] [CrossRef]
- Kahles, A.; et al. Comprehensive Analysis of Alternative Splicing Across Tumors from 8,705 Patients. Cancer Cell 2018, 34, 211–224.e216. [Google Scholar] [CrossRef]
- Wang, Y.; et al. Comprehensive Molecular Characterization of the Hippo Signaling Pathway in Cancer. Cell Reports 2018, 25, 1304–1317.e1305. [Google Scholar] [CrossRef]
- Chiu, H.-S.; et al. Pan-Cancer Analysis of lncRNA Regulation Supports Their Targeting of Cancer Genes in Each Tumor Context. Cell Reports 2018, 23, 297–312.e212. [Google Scholar] [CrossRef]
- Chen, H.; et al. A Pan-Cancer Analysis of Enhancer Expression in Nearly 9000 Patient Samples. Cell 2018, 173, 386–399.e312. [Google Scholar] [CrossRef]
- Taylor, A.M.; et al. Genomic and Functional Approaches to Understanding Cancer Aneuploidy. Cancer Cell 2018, 33, 676–689.e673. [Google Scholar] [CrossRef]
- Nakazawa, M.A.; et al. Novel cancer subtyping method based on patient-specific gene regulatory network. Scientific Reports 2021, 11, 23653. [Google Scholar] [CrossRef] [PubMed]
- Sun, P.; et al. Molecular Subtyping of Cancer Based on Distinguishing Co-Expression Modules and Machine Learning. Frontiers in genetics 2022, 13, 866005. [Google Scholar] [CrossRef] [PubMed]
- Peng, X.; et al. Molecular Characterization and Clinical Relevance of Metabolic Expression Subtypes in Human Cancers. Cell Reports 2018, 23, 255–269.e254. [Google Scholar] [CrossRef]
- Ge, Z.; et al. Integrated Genomic Analysis of the Ubiquitin Pathway across Cancer Types. Cell Reports 2018, 23, 213–226.e213. [Google Scholar] [CrossRef]
- Korkut, A.; et al. A Pan-Cancer Analysis Reveals High-Frequency Genetic Alterations in Mediators of Signaling by the TGF-β Superfamily. Cell Systems 2018, 7, 422–437.e427. [Google Scholar] [CrossRef] [PubMed]
- Seiler, M.; et al. Somatic Mutational Landscape of Splicing Factor Genes and Their Functional Consequences across 33 Cancer Types. Cell Reports 2018, 23, 282–296.e284. [Google Scholar] [CrossRef]
- Knijnenburg, T.A.; et al. Genomic and Molecular Landscape of DNA Damage Repair Deficiency across The Cancer Genome Atlas. Cell Reports 2018, 23, 239–254.e236. [Google Scholar] [CrossRef]
- Hu, G.S.; et al. Integrated Analysis of Proteome and Transcriptome Profiling Reveals Pan-Cancer-Associated Pathways and Molecular Biomarkers. Molecular & cellular proteomics: MCP 2025, 24, 100919. [Google Scholar] [CrossRef] [PubMed]
- Bagaev, A.; et al. Conserved pan-cancer microenvironment subtypes predict response to immunotherapy. Cancer Cell 2021, 39, 845–865.e847. [Google Scholar] [CrossRef] [PubMed]
- Mao, X.; et al. Crosstalk between cancer-associated fibroblasts and immune cells in the tumor microenvironment: New findings and future perspectives. Molecular cancer 2021, 20, 131. [Google Scholar] [CrossRef]
- Li, S.; Luo, J.; Liu, J.; He, D. Pan-cancer single cell and spatial transcriptomics analysis deciphers the molecular landscapes of senescence related cancer-associated fibroblasts and reveals its predictive value in neuroblastoma via integrated multi-omics analysis and machine learning. Frontiers in immunology 2024, 15, 1506256. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; et al. Single-cell RNA sequencing and spatial transcriptomics reveal the heterogeneity and intercellular communication of cancer-associated fibroblasts in gastric cancer. Journal of translational medicine 2025, 23, 344. [Google Scholar] [CrossRef]
- Zhang, Y.; Chen, F.; Creighton, C.J. Pan-cancer molecular subtypes of metastasis reveal distinct and evolving transcriptional programs. Cell reports. Medicine 2023, 4, 100932. [Google Scholar] [CrossRef]
- Liou, K.; Wang, J.-P. Integrating genetic and gene expression data in network-based stratification analysis of cancers. BMC Bioinformatics 2025, 26, 126. [Google Scholar] [CrossRef]
- Mujal, A.M.; Krummel, M.F. Immunity as a continuum of archetypes. Science 2019, 364, 28–29. [Google Scholar] [CrossRef]
- Barry, K.C.; et al. A natural killer-dendritic cell axis defines checkpoint therapy-responsive tumor microenvironments. Nature medicine 2018, 24, 1178–1191. [Google Scholar] [CrossRef]
- Böttcher, J.P.; et al. NK Cells Stimulate Recruitment of cDC1 into the Tumor Microenvironment Promoting Cancer Immune Control. Cell 2018, 172, 1022–1037.e1014. [Google Scholar] [CrossRef]
- Binnewies, M.; et al. Unleashing Type-2 Dendritic Cells to Drive Protective Antitumor CD4(+) T Cell Immunity. Cell 2019, 177, 556–571.e516. [Google Scholar] [CrossRef]
- Le Morvan, M.; Zinovyev, A.; Vert, J.P. NetNorM: Capturing cancer-relevant information in somatic exome mutation data with gene networks for cancer stratification and prognosis. PLoS computational biology 2017, 13, e1005573. [Google Scholar] [CrossRef]
- Ghareyazi, A.; et al. Pan-cancer integrative analysis of whole-genome De novo somatic point mutations reveals 17 cancer types. BMC Bioinformatics 2022, 23, 298. [Google Scholar] [CrossRef]
- Luo, Z.; et al. Pan-cancer analysis identifies telomerase-associated signatures and cancer subtypes. Molecular cancer 2019, 18, 106. [Google Scholar] [CrossRef]
- Rahman, A.; et al. Machine learning and deep learning-based approach in smart healthcare: Recent advances, applications, challenges and opportunities. AIMS public health 2024, 11, 58–109. [Google Scholar] [CrossRef] [PubMed]
- Nakayama, D.K.; Bonasso, P.C. The History of Multimodal Treatment of Wilms’ Tumor. The American surgeon 2016, 82, 487–492. [Google Scholar] [CrossRef] [PubMed]
- Falzone, L.; Salomone, S.; Libra, M. Evolution of Cancer Pharmacological Treatments at the Turn of the Third Millennium. Frontiers in pharmacology 2018, 9, 1300. [Google Scholar] [CrossRef]
- Chabner, B.A.; Roberts, T.G., Jr. Timeline: Chemotherapy and the war on cancer. Nature reviews. Cancer 2005, 5, 65–72. [Google Scholar] [CrossRef] [PubMed]
- Krause, D.S.; Van Etten, R.A. Tyrosine kinases as targets for cancer therapy. The New England journal of medicine 2005, 353, 172–187. [Google Scholar] [CrossRef]
- Bedard, P.L.; Hyman, D.M.; Davids, M. S.; Siu, L.L. Small molecules, big impact: 20 years of targeted therapy in oncology. Lancet (London, England) 2020, 395, 1078–1088. [Google Scholar] [CrossRef]
- Pento, J.T. Monoclonal Antibodies for the Treatment of Cancer. Anticancer research 2017, 37, 5935–5939. [Google Scholar] [CrossRef]
- Slamon, D.J.; et al. Human breast cancer: Correlation of relapse and survival with amplification of the HER-2/neu oncogene. Science 1987, 235, 177–182. [Google Scholar] [CrossRef]
- Hudziak, R.M.; et al. p185HER2 monoclonal antibody has antiproliferative effects in vitro and sensitizes human breast tumor cells to tumor necrosis factor. Molecular and cellular biology 1989, 9, 1165–1172. [Google Scholar] [CrossRef]
- Salles, G.; et al. Rituximab in B-Cell Hematologic Malignancies: A Review of 20 Years of Clinical Experience. Advances in therapy 2017, 34, 2232–2273. [Google Scholar] [CrossRef]
- Lambert, J.M.; Berkenblit, A. Antibody-Drug Conjugates for Cancer Treatment. Annu Rev Med 2018, 69, 191–207. [Google Scholar] [CrossRef]
- Fu, Z.; Li, S.; Han, S.; Shi, C.; Zhang, Y. Antibody drug conjugate: The "biological missile" for targeted cancer therapy. Signal transduction and targeted therapy 2022, 7, 93. [Google Scholar] [CrossRef] [PubMed]
- Bross, P.F.; et al. Approval summary: Gemtuzumab ozogamicin in relapsed acute myeloid leukemia. Clinical cancer research: An official journal of the American Association for Cancer Research 2001, 7, 1490–1496. [Google Scholar] [PubMed]
- Roskoski, R. Properties of FDA-approved small molecule protein kinase inhibitors: A 2024 update. Pharmacological Research 2024, 200, 107059. [Google Scholar] [CrossRef] [PubMed]
- Smith, W.M.; et al. Therapeutic targeting of immune checkpoints with small molecule inhibitors. American journal of translational research 2019, 11, 529–541. [Google Scholar] [PubMed]
- Linsley, P.S.; et al. CTLA-4 is a second receptor for the B cell activation antigen B7. The Journal of experimental medicine 1991, 174, 561–569. [Google Scholar] [CrossRef]
- Bashyam, H. CTLA-4: From conflict to clinic. The Journal of experimental medicine 2007, 204, 1243. [Google Scholar] [CrossRef]
- Kaushik, I.; Ramachandran, S.; Zabel, C.; Gaikwad, S.; Srivastava, S.K. The evolutionary legacy of immune checkpoint inhibitors. Seminars in Cancer Biology 2022, 86, 491–498. [Google Scholar] [CrossRef]
- Subbiah, V.; Gouda, M.A.; Ryll, B.; Burris, H.A., 3rd; Kurzrock, R. The evolving landscape of tissue-agnostic therapies in precision oncology. CA: A cancer journal for clinicians 2024, 74, 433–452. [Google Scholar] [CrossRef]
- Bosi, C.; et al. Pan-cancer analysis of antibody-drug conjugate targets and putative predictors of treatment response. European journal of cancer (Oxford, England: 1990) 2023, 195, 113379. [Google Scholar] [CrossRef]
- Savage, S.R.; et al. Pan-cancer proteogenomics expands the landscape of therapeutic targets. Cell 2024, 187, 4389–4407.e4315. [Google Scholar] [CrossRef]
- Liu, X.; et al. Pan-cancer analysis identifies CD155 as a promising target for CAR-T cell therapy. Genome Medicine 2025, 17, 64. [Google Scholar] [CrossRef]
- Grewal, U.S.; Kurzrock, R. Mucin-1: A promising pan-cancer therapeutic target. npj Precision Oncology 2025, 9, 218. [Google Scholar] [CrossRef] [PubMed]
- Varkey, A.; et al. Employing novel pan-cancer targets for immunotherapy in leukemias and solid tumors. Journal of Clinical Oncology 2025, 43, 2582–2582. [Google Scholar] [CrossRef]
- Loomans-Kropp, H.A.; Umar, A. Cancer prevention and screening: The next step in the era of precision medicine. npj Precision Oncology 2019, 3, 3. [Google Scholar] [CrossRef] [PubMed]
- Manchanda, R.; et al. Cost-Effectiveness of Unselected Multigene Germline and Somatic Genetic Testing for Epithelial Ovarian Cancer. Journal of the National Comprehensive Cancer Network: JNCCN 2024, 22. [Google Scholar] [CrossRef]
- Tibiletti, M.G.; et al. From Therapy to Cancer Prevention Using HRD Testing on Patients with High-grade Ovarian Cancer. Cancer prevention research (Philadelphia, Pa.) 2025, 18, 393–400. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez-Hernandez, A.; et al. Prevalence and clinical impact of germline pathogenic variants in breast cancer: A descriptive large single-center study. ESMO open 2025, 10, 104543. [Google Scholar] [CrossRef]
- Shore, N.; et al. Implementation of Universal Germline Genetic Testing Into Standard of Care for Patients With Prostate Cancer: The Time Is Now. JCO oncology practice 2025, 21, 747–753. [Google Scholar] [CrossRef]
- Marabelli, M.; et al. Germline Testing in Breast Cancer: A Single-Center Analysis Comparing Strengths and Challenges of Different Approaches. Cancers 2025, 17. [Google Scholar] [CrossRef]
- Cuzick, J.; et al. First results from the International Breast Cancer Intervention Study (IBIS-I): A randomised prevention trial. Lancet (London, England) 2002, 360, 817–824. [Google Scholar] [CrossRef]
- Cuzick, J.; et al. Tamoxifen for prevention of breast cancer: Extended long-term follow-up of the IBIS-I breast cancer prevention trial. The Lancet. Oncology 2015, 16, 67–75. [Google Scholar] [CrossRef]
- Goss, P.E.; et al. Exemestane for breast-cancer prevention in postmenopausal women. The New England journal of medicine 2011, 364, 2381–2391. [Google Scholar] [CrossRef] [PubMed]
- Cuzick, J.; et al. Anastrozole for prevention of breast cancer in high-risk postmenopausal women (IBIS-II): An international, double-blind, randomised placebo-controlled trial. Lancet (London, England) 2014, 383, 1041–1048. [Google Scholar] [CrossRef]
- Hale, M.J., Howell, A., Dowsett, M., Cuzick, J.; Sestak, I. Tamoxifen related side effects and their impact on breast cancer incidence: A retrospective analysis of the randomised IBIS-I trial. Breast (Edinburgh, Scotland) 2020, 54, 216–221. [CrossRef]
- Liao, X.; et al. Aspirin use, tumor PIK3CA mutation, and colorectal-cancer survival. The New England journal of medicine 2012, 367, 1596–1606. [Google Scholar] [CrossRef] [PubMed]
- Rothwell, P.M.; et al. Effect of daily aspirin on risk of cancer metastasis: A study of incident cancers during randomised controlled trials. Lancet (London, England) 2012, 379, 1591–1601. [Google Scholar] [CrossRef]
- Guo, C.G.; et al. Aspirin Use and Risk of Colorectal Cancer Among Older Adults. JAMA oncology 2021, 7, 428–435. [Google Scholar] [CrossRef]
- Smith, S.G.; et al. Factors affecting uptake and adherence to breast cancer chemoprevention: A systematic review and meta-analysis. Annals of oncology: Official journal of the European Society for Medical Oncology 2016, 27, 575–590. [Google Scholar] [CrossRef] [PubMed]
- Hamed, A.R.; et al. Phenolic profiling unravels the chemopreventive components of Melaleuca citrina (Curtis) Dum.Cours. fruits by integrating LC-MS/MS, in vitro studies, docking and molecular dynamic simulation. Natural product research 2025, 1–13. [Google Scholar] [CrossRef]
- Gal, A.F.; et al. Limited Chemopreventive Effects of Oral Administration of Polyphenol-60 from Green Tea in the MNU-Induced Rat Mammary Tumor Model. Antioxidants (Basel, Switzerland) 2025, 14. [Google Scholar] [CrossRef]
- Villegas-Aguilar, M.D. C.; et al. Select bioavailable metabolites from Lippia citriodora and Olea europaea extracts exhibit anticancer effects on pancreatic cancer cell lines. Food & function 2025. [Google Scholar] [CrossRef]
- Jaglarz-Biały, K.; et al. The analysis of the composition and antioxidant properties of freeze-dried chokeberry, strawberry, blackberry and selected raspberry fruits. Folia medica Cracoviensia 2024, 64, 47–57. [Google Scholar] [CrossRef]
- Ngernnak, C.; Wongsuwan, S.; Ruchirawat, S.; Thasana, N. Synthesis and Evaluation of Tacrinocerins, Tacrine Hybrids with α-Onocerin from Phlegmariurus nummulariifolius (Blume) Ching, as a Novel Class of Acetylcholinesterase Inhibitor. Chemistry, an Asian journal 2025, e00705. [Google Scholar] [CrossRef]
- Domchek, S.M.; Vonderheide, R.H. Advancing Cancer Interception. Cancer discovery 2024, 14, 600–604. [Google Scholar] [CrossRef]
- Jonasch, E.; et al. Belzutifan for Renal Cell Carcinoma in von Hippel-Lindau Disease. The New England journal of medicine 2021, 385, 2036–2046. [Google Scholar] [CrossRef]
- Loud, J.T.; Murphy, J. Cancer Screening and Early Detection in the 21(st) Century. Seminars in oncology nursing 2017, 33, 121–128. [Google Scholar] [CrossRef]
- Wilson, J.M.; Jungner, Y.G. [Principles and practice of mass screening for disease]. Boletin de la Oficina Sanitaria Panamericana. Pan American Sanitary Bureau 1968, 65, 281–393. [Google Scholar]
- Shieh, Y.; et al. Population-based screening for cancer: Hope and hype. Nature Reviews Clinical Oncology 2016, 13, 550–565. [Google Scholar] [CrossRef] [PubMed]
- Harris, R.P., Wilt, T. J.; Qaseem, A. A value framework for cancer screening: Advice for high-value care from the American College of Physicians. Annals of internal medicine 2015, 162, 712–717. [CrossRef] [PubMed]
- Kronborg, O. Colon polyps and cancer. Endoscopy 2004, 36, 3–7. [Google Scholar] [CrossRef]
- Lindholm, E.; Brevinge, H.; Haglind, E. Survival benefit in a randomized clinical trial of faecal occult blood screening for colorectal cancer. The British journal of surgery 2008, 95, 1029–1036. [Google Scholar] [CrossRef] [PubMed]
- Hewitson, P.; Glasziou, P.; Irwig, L.; Towler, B.; Watson, E. Screening for colorectal cancer using the faecal occult blood test, Hemoccult. The Cochrane database of systematic reviews 2007, 2007, Cd001216. [Google Scholar] [CrossRef]
- de, K.o.n.i.n.g. H. J.; et al. Reduced Lung-Cancer Mortality with Volume CT Screening in a Randomized Trial. The New England journal of medicine 2020, 382, 503–513. [Google Scholar] [CrossRef]
- Duffy, S.W.; et al. Effect of mammographic screening from age 40 years on breast cancer mortality (UK Age trial): Final results of a randomised, controlled trial. The Lancet. Oncology 2020, 21, 1165–1172. [Google Scholar] [CrossRef]
- Cohen, J.D.; et al. Detection and localization of surgically resectable cancers with a multi-analyte blood test. Science 2018, 359, 926–930. [Google Scholar] [CrossRef]
- Zhou, B.; et al. Whole-genome sequencing analysis of CNV using low-coverage and paired-end strategies is efficient and outperforms array-based CNV analysis. Journal of medical genetics 2018, 55, 735–743. [Google Scholar] [CrossRef] [PubMed]
- Oxnard, G.R.; Paweletz, C.P. Regarding the Congruence Between 2 Circulating Tumor DNA Sequencing Assays. JAMA oncology 2018, 4, 1428–1429. [Google Scholar] [CrossRef] [PubMed]
- Lennon, A.M.; et al. Feasibility of blood testing combined with PET-CT to screen for cancer and guide intervention. Science 2020, 369. [Google Scholar] [CrossRef] [PubMed]
- Gong, T.; et al. Analysis and Performance Assessment of the Whole Genome Bisulfite Sequencing Data Workflow: Currently Available Tools and a Practical Guide to Advance DNA Methylation Studies. Small methods 2022, 6, e2101251. [Google Scholar] [CrossRef]
- Liu, M.C.; et al. Sensitive and specific multi-cancer detection and localization using methylation signatures in cell-free DNA. Annals of Oncology 2020, 31, 745–759. [Google Scholar] [CrossRef]
- Lo, Y.M. D.; Han, D.S.C.; Jiang, P.; Chiu, R.W.K. Epigenetics, fragmentomics, and topology of cell-free DNA in liquid biopsies. Science 2021, 372. [Google Scholar] [CrossRef]
- Jiang, P.; et al. Plasma DNA End-Motif Profiling as a Fragmentomic Marker in Cancer, Pregnancy, and Transplantation. Cancer discovery 2020, 10, 664–673. [Google Scholar] [CrossRef]
- Half, E.; et al. Non-invasive multiple cancer screening using trained detection canines and artificial intelligence: A prospective double-blind study. Scientific Reports 2024, 14, 28204. [Google Scholar] [CrossRef]
- Hussain, T.; Nguyen, Q.T. Molecular imaging for cancer diagnosis and surgery. Advanced drug delivery reviews 2014, 66, 90–100. [Google Scholar] [CrossRef] [PubMed]
- Kircher, M.F.; Hricak, H.; Larson, S.M. Molecular imaging for personalized cancer care. Molecular oncology 2012, 6, 182–195. [Google Scholar] [CrossRef] [PubMed]
- Tiwari, A.; Mishra, S.; Kuo, T.R. Current AI technologies in cancer diagnostics and treatment. Molecular cancer 2025, 24, 159. [Google Scholar] [CrossRef]
- SAlshuhri, M.; et al. Artificial intelligence in cancer diagnosis: Opportunities and challenges. Pathology - Research and Practice 2024, 253, 154996. [Google Scholar] [CrossRef] [PubMed]
- Johnson, K.B.; et al. Precision Medicine, AI, and the Future of Personalized Health Care. Clinical and translational science 2021, 14, 86–93. [Google Scholar] [CrossRef]
- Zheng, L.; et al. Pan-cancer single-cell landscape of tumor-infiltrating T cells. Science 2021, 374, abe6474. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).