1. Introduction
Abdominal aortic aneurysms (AAAs) are sporadic among children, with few cases documented in medical literature. The causes of AAAs in pediatric patients vary and can include congenital anomalies, infections, connective tissue disorders, and trauma [
1]. Surgical intervention is typically necessary due to the high risk of rupture and its associated morbidity and mortality [
2,
3,
4]. The choice between open surgical and endovascular approaches for AAA repair depends on factors such as anatomical suitability, patient age, and long-term outcomes. In pediatric cases, the open surgical approach is often preferred to ensure durable long-term results and accommodate growth [
5,
6,
7].
Open AAA repair can be complicated by significant post-operative pain, which may result in prolonged immobility and difficulty clearing the airways. These issues can contribute to poorer outcomes, including extended hospital stays and an increased risk of pulmonary complications [
8,
9]. Given these complications, effective post-operative pain management is essential. The approach to pain control following open AAA repair has evolved from relying solely on epidural analgesia to incorporating alternative methods, such as rectus sheath blocks (RSBs) [
10]. Epidural analgesia carries risks, including bleeding complications, particularly in patients who require perioperative anticoagulation. In contrast, rectus sheath blocks (RSBs) have a much lower risk profile [
10]. Studies have shown that rectus sheath blocks (RSBs) can significantly reduce opioid consumption and enhance pain control in patients undergoing major abdominal surgeries, including open AAA repair. For instance, Cleary et al. found that patients who received rectus sheath blocks (RSBs) had a shorter time to extubation, reduced postoperative opioid requirements, and shorter hospital stays compared to those who received only general anesthesia [
11].
Liposomal bupivacaine, a novel sustained-release formulation of bupivacaine hydrochloride, has been increasingly utilized for postoperative pain management due to its extended duration of action. This formulation encapsulates bupivacaine within multivesicular liposomes, allowing for a prolonged analgesic effect lasting up to 72 hours post-administration [
12,
13]. The use of liposomal bupivacaine has been shown to reduce the need for opioid analgesics, thereby minimizing opioid-related adverse events and enhancing patient recovery [
13,
14]. In the pediatric population, although liposomal bupivacaine is not yet FDA-approved, its off-label use has been explored with promising results in terms of safety and efficacy [
15,
16,
17].
This case report describes the use of multilevel, bilateral ultrasound-guided rectus sheath blocks (bURSBs) with liposomal bupivacaine and dexamethasone in an 8-year-old patient undergoing open AAA repair. It highlights this approach as a potentially effective and safe alternative to neuraxial anesthesia, as part of a multimodal approach, in high-risk pediatric surgical patients.
2. Case Description
Special approval was obtained from the patient and her family, the pharmacy, and the transplant surgeon to use liposomal bupivacaine off-label for a peripheral nerve block in this pediatric patient. The patients’ parents gave written informed consent for the presentation of this report.
This is an 8-year-old male (131.5 cm, 26.7 kg), with no medical history, except migraines, who was initially seen in the emergency department after his pediatrician discovered a left brachial pseudoaneurysm. Further evaluation revealed several aneurysms, including a large infrarenal aortic aneurysm measuring 4.5 cm. Given the size and risk of rupture, vascular surgery was recommended to repair the abdominal aortic aneurysm (AAA). Ultrasound-guided, multiple-level bilateral rectus sheath blocks with liposomal bupivacaine, bupivacaine, and dexamethasone were chosen for postoperative pain control.
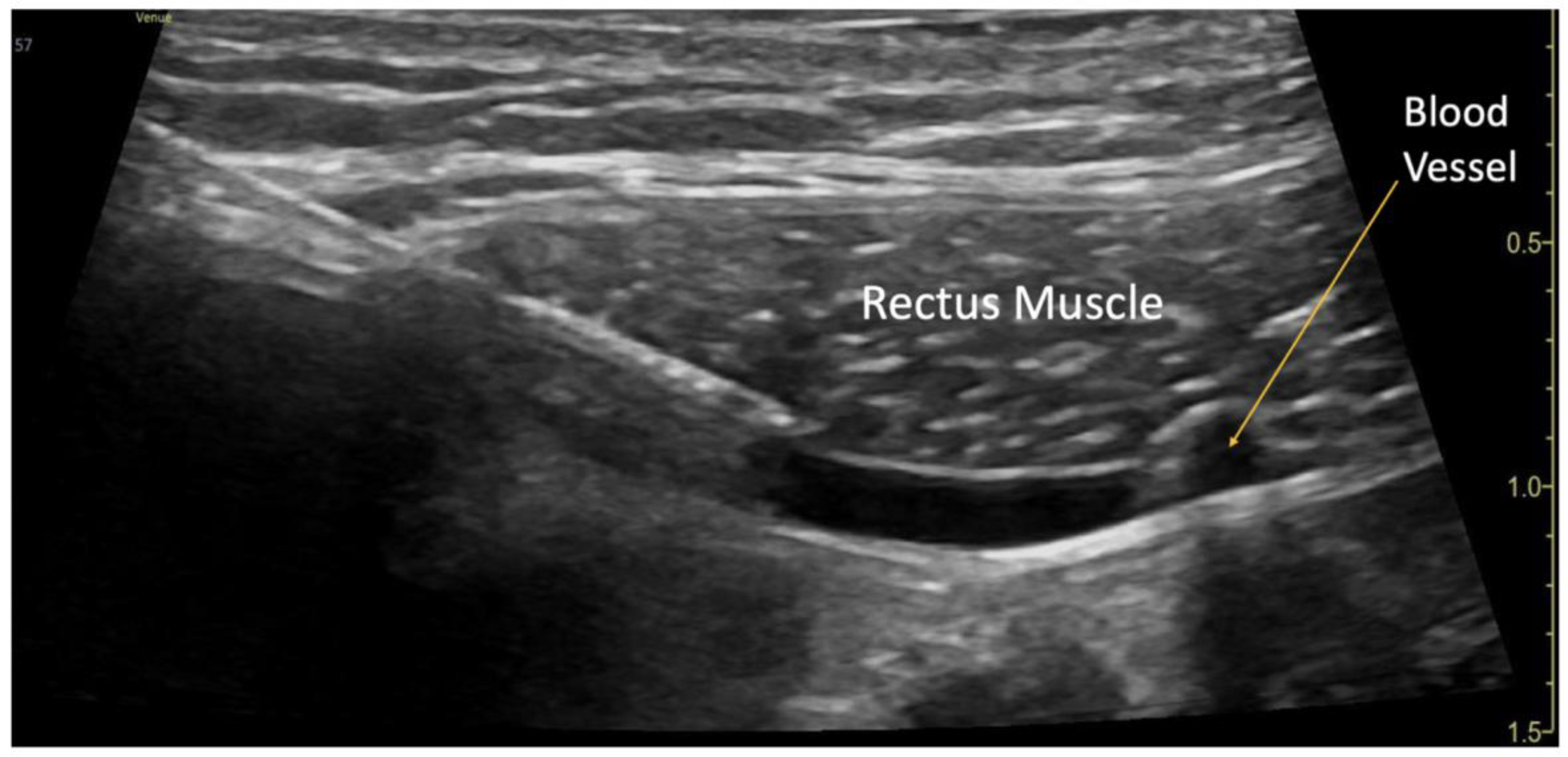
The blocks were performed while the patient was under general anesthesia, before surgery started, and after sterile preparation. A high-frequency linear transducer was positioned at the level of the umbilicus and moved laterally a few centimeters until the lateral border of the rectus muscle was visualized. An echogenic needle, 22-gauge, 50-mm Sono-TAP (Pajunck Medical Inc., Geisingen, Germany) was advanced medially from the lateral edge of the probe; final needle placement was at the lateral border of the rectus muscle, deep to the muscle, yet superficial to the posterior aspect of the rectus sheath, and not pre-peritoneal nor intraabdominal. A few milliliters (mL) of saline solution were injected until the spread of medication was visualized in the correct location (
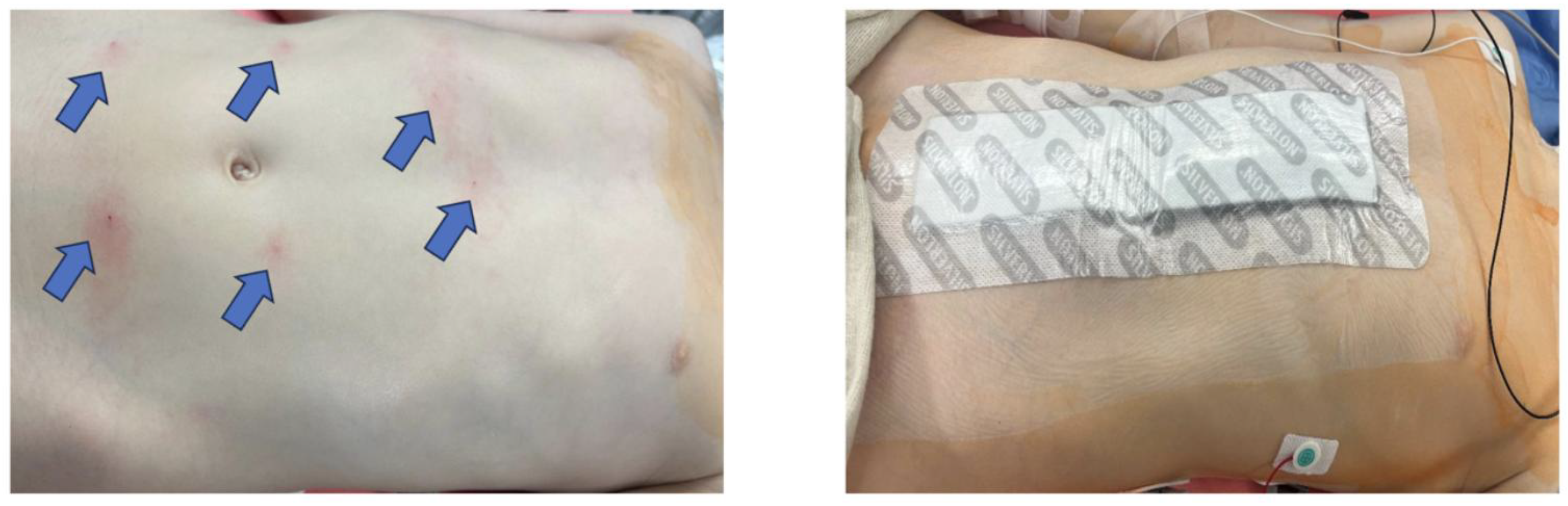
Figure 1), followed by three milliliters (mL) of local anesthetic mixture (liposomal bupivacaine 113.05 mg, bupivacaine 0.25%, 32.5 mg, and dexamethasone PF, 5mg -total volume 22 mL). This procedure was repeated at the contralateral site. Two more bilateral local anesthetic injections under the rectus muscle were performed at the level of T7 and T12 dermatomes (
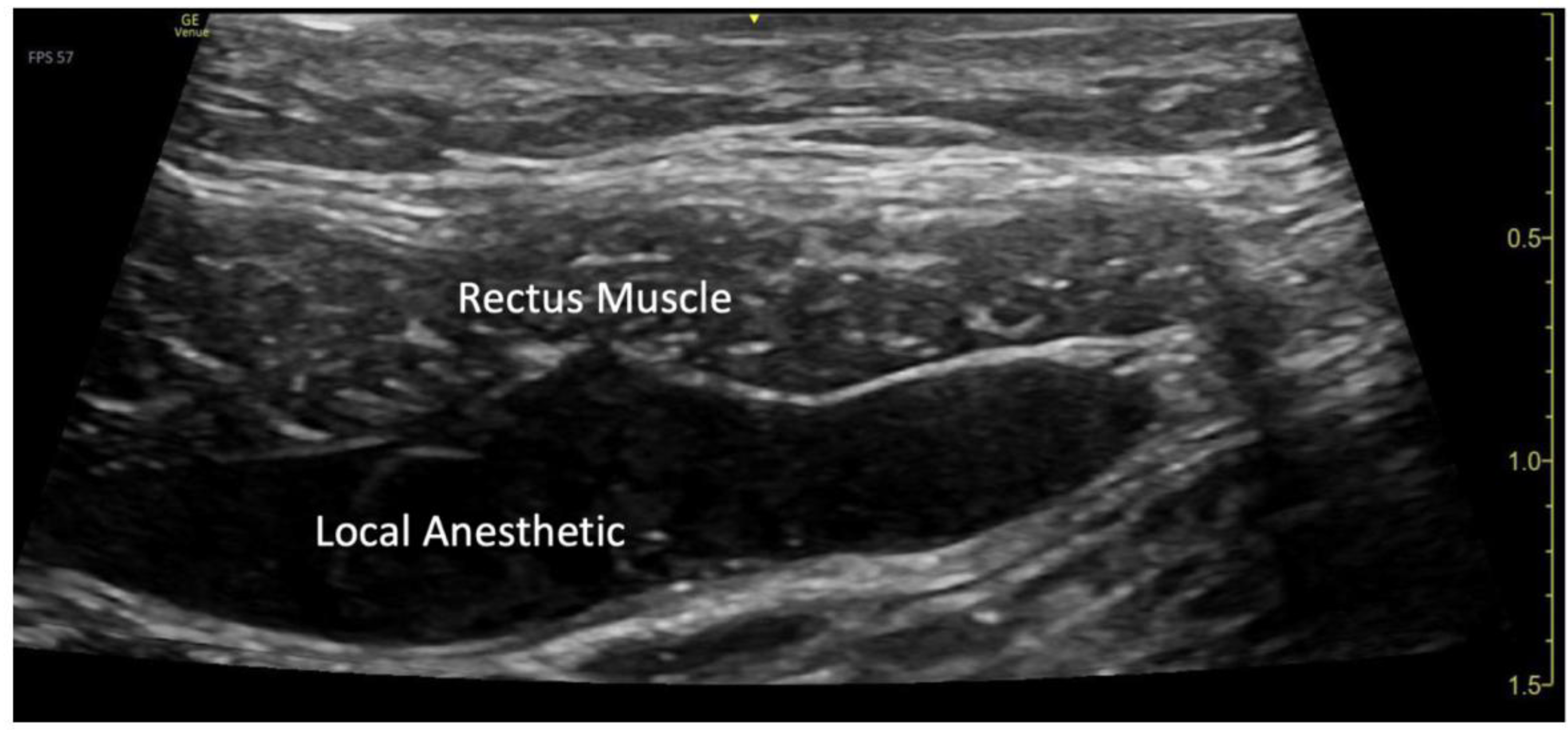
Figure 3a). A total of six rectus sheath blocks were performed with 22 ml of local anesthetic mixture. After the blocks were performed, medication spread behind the rectus muscle was visualized as a bulge into the space under the rectus sheath muscle from the xiphoid to the pubic symphysis (
Figure 2), as described by Visoiu et al, [
18] matching the incision performed (
Figure 3b). The surgery then conducted was an open infrarenal abdominal aortic aneurysm repair with a Hemashift Gold 12mm graft and a 6mm limb used for aortic graft to common iliac aneurysm repair. The duration of anesthesia was 374 minutes, the aortic cross-clamp time was 95 minutes, and total blood loss for the operation was 50mL. The surgery was uneventful, and intraoperative hemodynamic stability was adequately maintained. The patient was extubated in the operating room.
Figure 1.
Rectus Sheath Block Procedure. A blood vessel was visualized in the plane underneath the rectus muscle.
Figure 1.
Rectus Sheath Block Procedure. A blood vessel was visualized in the plane underneath the rectus muscle.
Figure 2.
Visualization of local anesthetic spread under the rectus muscle.
Figure 2.
Visualization of local anesthetic spread under the rectus muscle.
Figure 3.
(a) Location of the rectus sheath blocks; (b) Bandage covering the surgical incision site.
Figure 3.
(a) Location of the rectus sheath blocks; (b) Bandage covering the surgical incision site.
Table 2. 25 mcg/kg, intravenous methadone at 0.22 mg/kg, and ketamine at 1.87 mg/kg. Acetaminophen was administered at 14.98 mg/kg intravenously. Postoperative medications can be found in
Table 1. The patient was discharged in stable condition on POD 6 with acetaminophen 400 mg to take as needed for pain control and aspirin 81mg daily.
Table 1.
Medication Administration.
Table 1.
Medication Administration.
| |
Fentanyl
(mcg/kg) |
Methadone IV (mcg/kg) |
Ketamine
(mg/kg) |
Hydromorphone (mcg/kg) |
Acetaminophen IV or PO (mg/kg) |
Ketorlac (mg/kg) |
| Intraoperatively |
2.25 |
0.22 |
1.87 |
0 |
14.98 |
0 |
| Postoperative Day 0 |
0 |
0.11 |
0.66 |
0 |
14.98 |
0 |
| POD 1 |
0 |
0.22 |
1.14 |
5.99 |
74.9 |
0 |
| POD 2 |
0 |
0.22 |
0 |
0 |
74.9 |
0 |
| POD 3 |
0 |
0.17 |
0 |
0 |
44.94 |
1.57 |
| POD 4 |
0 |
0.06 |
0 |
3.75 |
59.92 |
2.1 |
| POD 5 |
0 |
0.06 |
0 |
0 |
29.96 |
0.52 |
| POD 6 |
0 |
0 |
0 |
0 |
As needed |
0 |
Table 2.
Postoperative Pain Scores and Mobility.
Table 2.
Postoperative Pain Scores and Mobility.
| |
Average Pain Score/10 |
Highest Pain Score/10 |
Out of Bed in Chair (Y/N) |
Ambulation (Y/N) |
| Postoperative Day 0 |
0 |
0 |
N |
N |
| POD 1 |
0.5 |
6 |
Y |
N |
| POD 2 |
0.29 |
2 |
Y |
Y |
| POD 3 |
0.4 |
2 |
Y |
Y |
| POD 4 |
1 |
7 |
Y |
Y |
| POD 5 |
0.29 |
2 |
Y |
Y |
| POD 6 |
0 |
0 |
Y |
Y |
The ketamine administration resulted in the patient experiencing double vision and hallucinations on POD 0 and POD 1. Ketamine was discontinued on POD 1, which resulted in the resolution of side effects. He did develop headaches following the discontinuation of ketamine, which were alleviated through cold packs.
Postoperative pain scores remained consistently low throughout the hospital stay. The patient reported no pain on postoperative day (POD) 0. On POD 1, the average pain score was 0.5 out of 10, with a highest reported score of 6. By POD 2, pain decreased further to an average of 0.29 with a maximum of 2, and remained low on PODs 3 (average 0.4, max 2), 4 (average 1, max 7), and 5 (average 0.29, max 2). The patient reported no pain on POD 6. The maximum pain scores on POD 2 and 3 were attributed to headaches, while those on POD 0, 1, 4, and 5 were attributed to post-operative incisional pain.
Functional recovery milestones were achieved promptly. The patient was initially bedbound on POD 0 but was able to get out of bed to a chair by POD 1. Ambulation began on POD 2 and continued through POD 6. There was a concern for post-operative ileus, and the patient was NPO for 48 hours post-op, but this concern resolved with the patient tolerating liquids on POD 3, solids on POD 4, and having a bowel movement on POD 4. Complete pain scores and functional recovery milestones can be found in
Table 2.
Plasma bupivacaine levels were measured on PODs 1 through 3 and remained within safe limits: 0.11 mcg/ml on POD 1, 0.093 mcg/ml on POD 2, and 0.11 mcg/ml on POD 3.
Numbness on each side of the body could not initially be investigated due to the large dressing covering the incision area. By POD 5, the patient reported bilateral numbness along portions of the incision, which resolved one day later.
3. Discussion
This case demonstrates the successful use of ultrasound-guided multilevel bilateral rectus sheath blocks (RSBs) with bupivacaine, liposomal bupivacaine, and dexamethasone for postoperative pain management in an 8-year-old patient undergoing open abdominal aortic aneurysm (AAA) repair—a rare and complex surgical procedure in the pediatric population.
In this challenging case, multilevel bilateral ultrasound guided RSBs were chosen as the most appropriate regional anesthesia for postoperative pain management. Before surgery, we evaluated several other regional pain control options, but each had significant drawbacks. An epidural catheter was considered; however, due to the patient's multiple aneurysms, we were concerned about the possibility of an aneurysm in the epidural space. Additionally, we anticipated the need for anticoagulation both during and after surgery, as well as potential postoperative intubation, which could complicate the neurological examination of the extremities. Paravertebral catheters were another option but posed similar risks to the epidural approach. Bilateral rectus sheath catheters were considered; however, we were concerned that they would not provide adequate analgesia for such a large incision, as the maximum volume of local anesthetic deliverable through each catheter would be limited to 3.4 ml/hr. Moreover, these catheters would need to be placed at the end of surgery, as they would be near the surgical incisions.
Rectus sheath blocks (RSBs) have proven effective in reducing postoperative opioid consumption, facilitating early extubation, and promoting early mobilization and discharge [
10,
11]. For example, Cleary et al. reported that RSBs, with or without catheter insertion, performed for pain control after adult aortic aneurysm surgeries, resulted in shorter extubation times, reduced opioid use, and decreased hospital stays compared to general anesthesia alone [
11]. The blocks were performed at a single level, with a high volume of diluted, short-lasting local anesthetic.
In our case, we expected that blocks performed at the level of the umbilicus only would not provide adequate analgesia across the entire incision, as noted by Visoiu et al [
18]. Therefore, we performed additional bilateral rectus sheath blocks both above and below the umbilicus. Using ultrasound guidance, we were able to visualize the needle placement and medication spread from the xiphoid to the pubis, ensuring effective pain relief across the entire surgical incision.
The patient’s postoperative recovery supports the efficacy of the analgesic approach. To expedite the onset of the nerve block, 1.28 mg/kg of plain bupivacaine was co-administered with liposomal bupivacaine. Given the lack of clear dosage recommendations for liposomal bupivacaine, particularly in the context of ultrasound-guided fascial plane block, we elected to administer 4.23 mg/kg (8.5ml), to prolong the duration of analgesia. This dose approximates the pediatric recommendation for liposomal bupivacaine when used for wound infiltration
To prolong the duration of analgesia, we use 4.24 mg/kg liposomal bupivacaine. This medication, although not FDA-approved for pediatric use, has demonstrated extended analgesia due to its sustained-release properties, lasting up to 72 hours post-injection; warranting further research to establish evidence-based pediatric dosing guidelines [
12,
13,
14,
17].
To further prolong pain relief, we added dexamethasone to the blocks. For our patient, pain scores at the abdominal incision remained consistently low throughout the hospitalization, with no incisional pain reported by postoperative day (POD) 6. It is important to note that the pain scores were in line with the sensory exam findings, which indicated numbness on POD 5, and the presence of bupivacaine in the blood on POD 3. Plasma bupivacaine levels remained well within the safe range, and no signs of local anesthetic systemic toxicity were observed. Monitoring bupivacaine levels allowed us to correlate the duration of analgesia with both the presence of numbness and the anesthetic's blood concentration. This correlation further validates the effectiveness of the pain management strategy and the prolonged analgesia provided by the block. It is possible that dexamethasone contributed to the prolonged numbness (until postoperative day 5) and extended analgesic effect through its anti-inflammatory properties and local anesthetic-sparing effects [
15,
16].
The patient reported mild numbness at the incision site by POD 5, which lasted longer than previously reported in the case report, where dexamethasone was not included in the nerve blocks [
17].
The multimodal analgesic regimen for this patient included scheduled acetaminophen, intermittent methadone doses, a short course of ketamine and ketorolac, and minimal use of short-acting opioids—highlighting the opioid-sparing effect of the block. This approach successfully minimized opioid exposure, which facilitated the resumption of bowel function and helped prevent ileus, a potential complication after surgery. Early mobilization was achieved, with the patient sitting up by POD 1 and ambulating by POD 2.
The patient, family, and surgical team all expressed increased satisfaction with the pain management approach. A few months later, the patient underwent a nephrectomy due to an unresectable aneurysm of the renal artery. For this procedure, the family requested nerve blocks with liposomal bupivacaine for postoperative pain management.
4. Conclusions
This case illustrates the successful use of ultrasound-guided multilevel bilateral rectus sheath blocks (RSBs) with bupivacaine, liposomal bupivacaine, and dexamethasone for postoperative pain management in a pediatric patient undergoing open abdominal aortic aneurysm repair. The approach effectively minimized opioid use, reduced the risk of complications such as ileus, and facilitated early extubation and mobilization. The addition of liposomal bupivacaine and dexamethasone contributed to extended analgesia and enhanced patient comfort. Overall, this pain management strategy was effective in controlling postoperative pain and resulted in high satisfaction from the patient, family, and surgical team. Further studies are warranted to evaluate the long-term safety, optimal dosing strategies of liposomal bupivacaine in children, and the advantages of adding dexamethasone.
Supplementary Materials
The following supporting information can be downloaded at:
https://www.mdpi.com/article/doi/s1, Video S1: Spread of local anesthetic from blocks performed at different levels.
Author Contributions
Conceptualization, M.V.; methodology, M.V.; software, M.V.; validation, M.V.; formal analysis, M.V. and T.A.; investigation, M.V. and T.A.; resources, M.V. and T.A.; data curation, M.V. and T.A.; writing—original draft preparation, T.A.; writing—review and editing, M.V. and T.A.; visualization, T.A.; supervision, M.V.; project administration, M.V. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
All methods used in this article were performed in accordance with the Declaration of Helsinki. The patient and their guardian gave written Health Insurance Portability and Accountability Act (HIPPA) authorization for this case report. This case report does not include any trials, drug use, and/or invasive practice that require approval from the ethics committee.
Informed Consent Statement
Written informed consent was obtained from the child’s parents for the publication of this case report and accompanying images.
Data Availability Statement
The data presented in this study are available on request from the corresponding author due to privacy reasons.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| AAA |
Abdominal aortic aneurysm |
| RSB |
Rectus sheath block |
| POD |
Postoperative day |
| LD |
Linear dichroism |
References
- Wang, Y.; Tao, Y. , Diagnosis and treatment of congenital abdominal aortic aneurysm: a systematic review of reported cases. Orphanet J Rare Dis 2015, 10, 4. [Google Scholar] [CrossRef] [PubMed]
- Eliason, J.L.; et al. Surgical treatment of abdominal aortic aneurysms in infancy and early childhood. J Vasc Surg 2016, 64, 1252–1261. [Google Scholar] [CrossRef] [PubMed]
- Ye, C.; et al. Abdominal aorta aneurysms in children: single-center experience of six patients. Ann Thorac Surg 2012, 93, 201–205. [Google Scholar] [CrossRef] [PubMed]
- Dueppers, P.; et al. Open Repair for Abdominal Aortic Aneurysm in a Young Boy with Tuberous Sclerosis and Review of the Literature. Ann Vasc Surg 2017, 39, 286.e1–286.e5. [Google Scholar] [CrossRef] [PubMed]
- Kontopodis, N.; et al. Systematic Review With Meta-Analysis of Endovascular Versus Open Repair of Abdominal Aortic Aneurysm Repair in the Young. J Endovasc Ther 2025, 32, 276–289. [Google Scholar] [CrossRef] [PubMed]
- Byun, E.; et al. Quality-adjusted life year comparison at medium-term follow-up of endovascular versus open surgical repair for abdominal aortic aneurysm in young patients. PLoS One 2021, 16, e0260690. [Google Scholar] [CrossRef] [PubMed]
- Kontopodis, N.; et al. Endovascular vs Open Aneurysm Repair in the Young: Systematic Review and Meta-analysis. J Endovasc Ther 2015, 22, 897–904. [Google Scholar] [CrossRef] [PubMed]
- Chaikof, E.L.; et al. The Society for Vascular Surgery practice guidelines on the care of patients with an abdominal aortic aneurysm. J Vasc Surg 2018, 67, 2–77.e2. [Google Scholar] [CrossRef] [PubMed]
- Fairman, A.S.; et al. The evolution of open abdominal aortic aneurysm repair at a tertiary care center. J Vasc Surg 2020, 72, 1367–1374. [Google Scholar] [CrossRef] [PubMed]
- Yoshida, K.; et al. Pain Management in Open Abdominal Aortic Aneurysm Repair: Potential Alternatives to Epidural Anesthesia. J Cardiothorac Vasc Anesth 2025, 39, 785–791. [Google Scholar] [CrossRef] [PubMed]
- Cleary, C.; et al. Rectus Sheath Block Improves Patient Recovery Following Open Aortic Surgery. Ann Vasc Surg 2023, 97, 27–36. [Google Scholar] [PubMed]
- Hamilton, T.W.; et al. Liposomal bupivacaine infiltration at the surgical site for the management of postoperative pain. Cochrane Database Syst Rev 2017, 2, CD011419. [Google Scholar] [PubMed]
- Golembiewski, J. and Dasta, J., Evolving Role of Local Anesthetics in Managing Postsurgical Analgesia. Clin Ther 2015, 37, 1354–1371. [Google Scholar] [PubMed]
- Beiranvand, S. and Moradkhani, M.R., Bupivacaine Versus Liposomal Bupivacaine For Pain Control. Drug Res (Stuttg) 2018, 68, 365–369. [Google Scholar] [PubMed]
- Cohen, B.; et al. Incidence of adverse events attributable to bupivacaine liposome injectable suspension or plain bupivacaine for postoperative pain in pediatric surgical patients: A retrospective matched cohort analysis. Paediatr Anaesth 2019, 29, 169–174. [Google Scholar] [CrossRef] [PubMed]
- Tirotta, C.F.; et al. A multicenter study to evaluate the pharmacokinetics and safety of liposomal bupivacaine for postsurgical analgesia in pediatric patients aged 6 to less than 17 years (PLAY). J Clin Anesth 2021, 75, 110503. [Google Scholar] [CrossRef] [PubMed]
- Bonaroti, R.; Ganoza, A.; Visoiu, M. Liposomal Bupivacaine in Single-Injection Quadratus Lumborum Block for Pediatric Kidney Transplant: Case Report of a Novel Application. Pediatr Transplant 2025, 29, e70112. [Google Scholar] [PubMed]
- Visoiu, M.; Hauber, J.; Scholz, S. Single injection ultrasound-guided rectus sheath blocks for children: Distribution of injected anesthetic. Paediatr Anaesth 2019, 29, 280–285. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).