1. Introduction
Children and youth often have challenges processing and integrating sensory information, that, if left unrecognized and untreated, can result in negative consequences in everyday activities, routines and roles. Often referred to as challenges in sensory integration or sensory processing, these interconnected terms describe the neural processes through which we organize sensory inputs from the body and the environment and use this information to adaptively interact with the world (Lane et al., 2019). These functions are foundational to everyday activities and disruptions can have pervasive effects on behavioral and emotional regulation, motor performance, social interaction, self-care, and learning. While readers may encounter these and various other terms in the literature or the vernacular of families or professionals, to promote clarity and consistency, in this paper we employ two terms: (1) sensory integration as a term that encompasses sensory responsivity, sensory perception, and sensory-motor abilities and (2) occupational therapy using Ayres Sensory Integration™ (ASI) to refer to assessment and intervention.
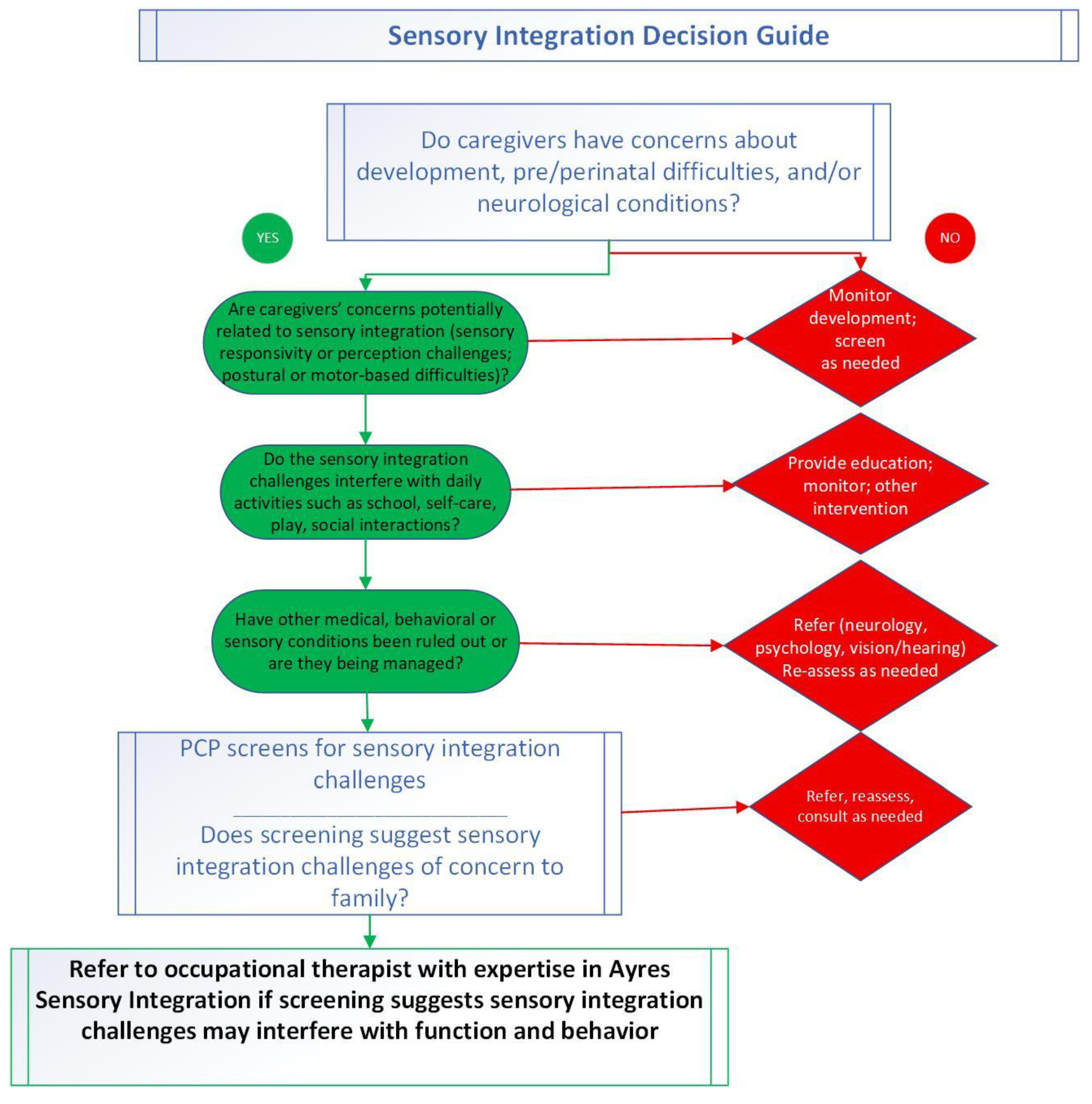
Sensory integration challenges are often comorbid with existing neurodevelopmental or mental health conditions such as autism (e.g. Camino-Alarcon et al., 2024; Schaaf et al., 2023) and attention deficit hyperactivity disorder [ADHD]; e.g. Jurek et al., 2025), as well as some psychiatric disorders. Additionally, these challenges can manifest in children with no other condition (Ahn et al., 2004; Gouze et.al., 2009; Jussila et al., 2020). The high prevalence of sensory integration challenges in children with (50-90%) and without (5-20%) other diagnoses (Ahn et al., 2004; Carter et al., 2011; Galiana et al., 2022; Gouze et al., 2009; Hemant & Ferzandi, 2020; Jussila et al., 2020; Kirby et al., 2022; Klintwall et al., 2011; Leekam et al., 2007; Mulligan et al., 2021;Tomchek & Dunn, 2007; Miller et al., 2017; Verma et al., 2025) highlights the importance of accurate detection and intervention. Since primary care providers (PCPs) play a significant role in the referral process, it is critical to enhance their knowledge and confidence in detection of these problems and appropriate referral for services. Our aim is to assist PCPs in their clinical decision making. We present foundational information to support an understanding of these challenges, and a novel tool, based on an example provided by van Venrooij et al. (2022) that can be used as a clinical decision-making support method.
We selected a narrative review as an appropriate methodology for describing and examining the body of literature specific to sensory integration (Sukhera, 2022). The intent is to facilitate accurate detection of children with sensory integration challenges in need of referral to an occupational therapist specializing in Ayres Sensory Integration ® assessment and intervention. As such, we present 1) a synthesis of the research evidence to support an understanding of sensory integrative challenges; and 2) the Sensory Integration Decision Guide.
2. Materials and Methods
Our narrative review of literature focused on the prevalence and needs of children with sensory integration challenges. To facilitate accurate detection, referral, and management of these challenges that put children at risk for difficulty with everyday life activities, we propose a way of thinking about child behaviors that reflects how they process and integrate sensation.
GenAI was not used in the preparation of this manuscript.
3. Results
Outcomes from our review are presented below, beginning with the impact of sensory integrative challenges on children and families, underscoring the importance of recognizing these challenges. The subsequent sections provide information for the PCP on screening and considerations for referral to occupational therapy and provides a brief description of sensory integration intervention.
3.1. Impact
Differences in how we process and integrate sensation impact many facets of life. Researchers have shown that children with sensory integration challenges experience behavioral difficulties that interfere with their ability to engage in social interaction, play with peers (Brady & Brown, 2023; Schaaf et al., 2011), benefit from learning environments (Gigliotti et al., 2024), sleep adequately (Hartman et al., 2022; Lane et al., 2022), and engage in other routine childhood activities (Loh et al., 2023). In addition, evidence indicates that parenting stress is high when a child has sensory integration challenges and that families often make accommodations for their child, limiting participation in family routines and community activities (Ben-Sasson et al, 2022; Gourley et al., 2013; Kirby et al., 2015; Little et al., 2022).
Sensory integration challenges manifest as difficulties in sensory perception, hypo- or hyper-responsivity, and engagement in sensory-motor activities. Sensory-motor difficulties include poor postural control and coordination of eye movements, and challenges with motor planning /execution of movements (Bundy & Lane, 2020). Functionally, these differences are seen as motor clumsiness, challenges with balance, and difficulty with age-appropriate motor skill attainment (Cermak & May-Benson, 2020). Ultimately, these sensory integration challenges interfere with children’s ability to engage in everyday occupations such as self-care, play, leisure and school activities. Parents report that such challenges are among the most challenging issues they face in managing their child’s behavior and engagement in everyday activities. Consequently, parents rate occupational therapy intervention as a top priority for remediating these challenges (Goin-Kochel et al., 2009; Green et al., 2006; Robertson et al., 2017).
3.2. Screening by the PCP
Children with sensory integration challenges may present to their PCP with a variety of concerns including functional problems such as delays in self care, dressing, eating, motor coordination challenges, sensory sensitivities and/or challenging behaviors (Wood, 2020). As there is a high co-morbidity of these behaviors with autism, ADHD, and other neurodevelopmental or mental health conditions, PCPs may initially screen for these conditions. However, regardless of whether a comorbid condition exists, if parental concerns or child history suggest challenges in sensory and motor abilities, PCPs should consider the potential impact on the child’s performance of everyday activities.
There are myriad checklists available to screen for sensory integration challenges available through occupational therapy clinics; several can be found by searching on the web. Some examples of these checklists include those available from the Spiral Foundation(
http://bit.ly/4pc0nY2), links to checklists for infants – school aged children;
https://www.thespiralfoundation.org/ash, a tool for adolescents and adults), and the STAR Center (
https://sensoryhealth.org/basic/symptoms-checklist). These non-standardized tools provide initial information as to the nature of the challenges but do not provide standard scores or scoring guidelines. They are simply a place to begin exploring sensory integration challenges and gaining an initial understanding of reported concerns. Importantly, the most useful checklists include questions related to sensory perception, sensory responsivity, and sensory-motor abilities. Standardized tools are recommended when available. For example, the Sensory Processing Measure-2 (SPM-2; Parham et al., 2021) is a standardized screening tool that provides both insight into sensory integration challenges and standard scores. If screening suggests sensory integration impairments referral to an occupational therapist for a comprehensive assessment is a recommended next step.
3.3. Referral to Occupational Therapy
When considering referral to occupational therapy, it is important to obtain information from the family regarding needs, priorities, and preferences for their child as well as the contexts in which the child’s participation is compromised. If a referral to occupational therapy is agreed upon, it is essential to select a therapist with appropriate training in the evidence-based approach to sensory integration challenges, namely occupational therapy using Ayres Sensory Integration® (ASI) intervention. Therapists trained in this approach have the advanced knowledge necessary to ensure appropriate assessment and provision of this intervention (Ayres, 2005; Parham et al, 2011).
Occupational therapy using ASI is distinguished from other sensory-based interventions such as “sensory diets,” or specific sensory strategies such as a brushing protocol or listening to music on headphones (Bundy & Lane, 2020). Occupational therapy using ASI is the only evidence-based occupational therapy treatment for sensory integration differences. There is good evidence for its efficacy for autistic children (Schaaf et al., 2015; Steinbrenner et al., 2020; Schoen et al., 2019; Omairi,et al, 2020) and emerging evidence for its efficacy with other populations of children such as cerebral palsy and cortical visual impairment (Cemali et al., 2022), ADHD (Hermant & Ferzandi, 2018), as well as for children with no specific diagnosis (Andelin et al., 2021; Chan, 2023; Lecuona et al., 2017; McQuiddy, et al., 2024; et al., 2007; Whiting et al. 2022). As an evidence-based intervention, some insurance carriers may cover occupational therapy using ASI as a neurodevelopmental concern.
3.3. Treatment of Sensory Integration Challenges
Occupational therapy using ASI begins with a comprehensive evaluation of children and their sensory needs using administered standardized assessments designed for this purpose. Treatment is guided by evaluation findings, family and child priorities, and the child’s specific needs. The underlying sensory and motor factors impacting the child’s participation in everyday activities are the targets of intervention.
Occupational therapy intervention using ASI should be “ individualized, developmentally appropriate, intensive and include performance data relevant to treatment goals to evaluate and adjust interventions . . . based on sound theoretical constructs, rigorous methodologies and objective scientific evidence” (Hyman et al., 2020, pg. 20). Schaaf and Mailloux (2015) developed a clinical guide/manualized approach for practitioners that meet these criteria and support clinical reasoning through the intervention process.
Parent education is an integral component of treatment (Bundy & Smith Roley, 2020; Schaaf & Mailloux, 2015). Parents learn to reframe their child’s behavior by understanding their child’s sensory needs and working with the therapist to modify daily activities to facilitate success. For example, a therapist may recommend clothing that is better tolerated by a tactilely sensitive child who refuses to get dressed every morning or changes to evening routines to promote calming in preparation for sleep for a child who gets overstimulated/overwhelmed by the sensory environment.
In addition to direct intervention and parent education, occupational therapists collaborate with other stakeholders (e.g., teachers, other family members) to identify activity, routine and/or physical and social environmental modifications to support optimal performance (Schaaf & Mailloux, 2015) and participation. For instance, the therapist may collaborate with the parents to change the sleep environment for a child with tactile sensitivity by recommending sleeping on smooth microfiber (rather than cotton) sheets. Collaborations with the school personnel for a child with challenges in praxis might involve planning for the child to arrive at school a few minutes early so the child can find their cubby, hang up their jacket, and put away their lunch before the classroom becomes busy with other children.
3.4. Family Centered Goals Inform Expected Outcomes
Outcome measurement and progress reports are integral components of occupational therapy using ASI (Bundy & Lane, 2020; Schaaf et al., 2014). Family goals are often used to measure outcomes; goals frequently include improved participation in daily living, learning, play, sleep, eating, behavioral or emotional regulation and social interaction. Through a systematic process of assessment, goal setting, intervention implementation and outcome measurement, sensory integration challenges can be addressed effectively in occupational therapy using ASI. Randomized trials of this intervention report positive outcomes in independence in daily activities, improved participation in social situations and better regulated behavior (Schaaf et al., 2014; Steinbrenner et al., 2020; Schoen et al., 2019; Whiting et al. 2022). Other researchers have found improvements in receptive communication and fine and gross motor skills (Andelin, et al.,2021; Lecuona et al, 2017), functional regulation and participation in school (Whiting et al 2022) as well as gains in individually established family centered goal attainment scaled goals (Schaaf et al. 2015; Miller et al, 2007).
4. Sensory Integration Decision Guide
Based on this narrative review of the literature and clinical expertise, we created the
Sensory Integration Decision Guide (
Figure 1) designed to help PCPs make appropriate referrals for occupational therapy assessment and intervention for children with sensory integration challenges. The
Guide includes statements about sensory integration challenges and childhood occupations that may be disrupted by these concerns. We present two pathways, one leading to referral to occupational therapy and the other to screenings for other conditions and ongoing monitoring or referral to other professionals.
5. Conclusions and Future Directions
The prevalence of sensory integration challenges is high in children with and without other diagnosed conditions. When signs and symptoms of difficulties with sensory integration are detected during screening procedures and found to impact everyday life, assessment by a trained occupational therapist may be warranted, and the child may require treatment. When treatment is recommended, the use of evidence-based occupational therapy intervention is an important consideration for referral. Future study is suggested that evaluates the accuracy and usefulness of the Sensory Integration Decision Guide in the clinical decision-making process of primary care professionals.
Author Contributions
All authors contributed to the conceptualization and methodology. Writing—original draft preparation, S.J.L., S.A.S., R.S., and A.B. Writing—review and editing was done by all authors. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study did not require ethical approval.
Conflicts of Interest
ZM and SSR are co-authors of the Evaluation in Ayres Sensory Integration (EASI), a set of tests which measure sensory and motor functions in children, which are freely available and for which they receive no royalties. Both authors are instructors for a non-profit organization, the Collaborative for Leadership in Ayres Sensory Integration which offers continuing education programs related to sensory integration and receives teaching honoraria and royalties related to these programs. LDP is co-author of the Sensory Processing MeasureTM-2 for which she receives royalties.
References
- Ahn, R.R.; Miller, L.J.; Milberger, S.; McIntosh, D.N. Prevalence of parents' perceptions of sensory processing disorders among kindergarten children. American Journal of Occupational Therapy 2004, 58, 287–293. [Google Scholar] [CrossRef]
- Andelin, L.; Reynolds, S.; Schoen, S. Effectiveness of occupational therapy using a sensory integration approach: A multiple-baseline design study. American Journal of Occupational 2021, 75, 7506205030. [Google Scholar] [CrossRef]
- Ayres, A. J. Sensory integration and the child; Western Psychological Services, 2005. [Google Scholar]
- Ben-Sasson, A.; Zisserman, A. Sensory family accommodation for autistic and sensory overresponsive children: The mediating role of parenting distress tolerance. American Journal of Occupational Therapy 2025, 79, 7903205110. [Google Scholar] [CrossRef] [PubMed]
- Brady, E.; Brown, T. An investigation of the association between school-aged children’s sensory processing and their self-reported leisure activity participation and preferences. Journal of Occupational Therapy, Schools, & Early Intervention 2022, 16, 51–77. [Google Scholar] [CrossRef]
- Bundy, A.; Lane, S.J. (2020). Sensory integration: A. Jean Ayres theory revisited. In A. Bundy & S. J. Lane (eds.), Sensory integration theory and practice, 3rd ed (pp. 2–20). F. A. Davis.
- Bundy, A.; Smith Roley, S. (2020). Planning and implementing intervention using sensory integration theory. In A. Bundy & S. J. Lane (eds.), Sensory integration theory and practice, 3rd ed (pp. 532–547). F. A. Davis.
- Camino-Alarcón, J.; Robles-Bello, M.A.; Valencia-Naranjo, N.; Sarhani-Robles, A.A. Systematic review of treatment for children with Autism Spectrum Disorder: The sensory processing and sensory integration approach. Children 2024, 11, 1222. [Google Scholar] [CrossRef]
- Carter, A.S.; Ben-Sasson, A.; Briggs-Gowan, M.J. Sensory over-responsivity, psychopathology, and family impairment in school-aged children. Journal of the American Academy of Child and Adolescent Psychiatry 2011, 50, 1210–1219. [Google Scholar] [CrossRef]
- Cemali, M.; Pekçetin, S.; Akı, E. The effectiveness of sensory integration interventions on motor and sensory functions in infants with cortical vision impairment and cerebral palsy: A single blind randomized controlled trial. Children (Basel, Switzerland) 2022, 9, 1123. [Google Scholar] [CrossRef]
- Cermak, S.A.; May-Benson, T. (2020). Praxis and dyspraxia. In A. Bundy & S. J. Lane (eds.), Sensory integration theory and practice, 3rd ed (pp. 115–150). F.A. Davis.
- Chan, P.L.C.; Poon, M.Y.C.; Bux, V.; Wong, S.K.F.; Chu, A.W.Y.; Louie, F.T.M.; Wang, A.Q.L.; Yang, H.L.C.; Yu, E.L.M.; Fong, S.S. Occupational therapy using an Ayres Sensory integration® approach for school-age children–a randomized controlled trial. World Federation of Occupational Therapists Bulletin 2023, 79, 228–235. [Google Scholar] [CrossRef]
- Galiana, A.; Flores-Ripoll, J.M.; Benito-Castellanos, P.J.; Villar-Rodriguez, C.; Vela-Romero, M. Prevalence and severity-based classification of sensory processing issues. An exploratory study with neuropsychological implications. Applied Neuropsychology Child 2022, 11, 850–862. [Google Scholar] [CrossRef]
- Gigliotti, F.; Giovannone, F.; Belli, A.; Sogos, C. Atypical sensory processing in neurodevelopmental disorders: Clinical phenotypes in preschool-aged children. Children 2024, 11, 875. [Google Scholar] [CrossRef]
- Goin-Kochel, R.P.; Mackintosh, V.H.; Myers, B.J. Parental reports on the efficacy of treatments and therapies for their children with autism spectrum disorders. Research in Autism Spectrum Disorder 2009, 3, 528–537. [Google Scholar] [CrossRef]
- Gourley, L.; Wind, C.; Henninger, E.M.; Chinitz, S. Sensory processing difficulties, behavioral problems, and parental stress in a clinical population of young children. Journal of Child and Family Studies 2013, 22, 912–921. [Google Scholar] [CrossRef]
- Gouze, K.R.; Hopkins, J.; LeBailly, S.A.; Lavigne, J.V. Re-examining the epidemiology of sensory regulation dysfunction and comorbid psychopathology. Journal of Abnormal Child Psychology 2009, 37, 1077–1087. [Google Scholar] [CrossRef]
- Green, V.A.; Pituch, K.A.; Itchon, J.; Choi, A.; O'Reilly, M.; Sigafoos, J. Internet survey of treatments used by parents of children with autism. Research in Developmental Disabilities 2006, 27, 70–84. [Google Scholar] [CrossRef]
- Hartman, A.G.; McKendry, S.; Soehner, A.; Bodison, S.; Akcakaya, M.; DeAlmeida, D.; Bendixen, R. Characterizing sleep differences in children with and without sensory sensitivities. Frontiers in Psychology 2022, 13, 875766. [Google Scholar] [CrossRef] [PubMed]
- Hemant, P.; Ferzandi, Z. Ayres sensory integration for children with attention deficit and hyperactivity disorder (ADHD): A mixed method study. International Journal of Advanced Research 2020, 8, 1034–1042. [Google Scholar] [CrossRef] [PubMed]
- Hyman, S.L.; Levy, S.E.; Myers, S.M. ; Council on Children with Disabilities, Section on Developmental and Behavioral Pediatrics Identification, evaluation, and management of children with autism spectrum disorder. Pediatrics 2020, 145, e20193447. [Google Scholar] [CrossRef]
- Jurek, L.; Duchier, A.; Gauld, C.; Hénault, L.; Giroudon, C.; Fourneret, P.; Cortese, S.; Nourredine, M. (2025). Sensory processing in individuals with Attention-Deficit/Hyperactivity Disorder compared with control populations: A systematic review and meta-analysis. Journal of the American Academy of Child and Adolescent Psychiatry 2025. [Google Scholar] [CrossRef]
- Jussila, K.; Junttila, M.; Kielinen, M.; Ebeling, H.; Joskitt, L.; Moilanen, I.; Mattila, M.L. Sensory abnormality and quantitative autism traits in children with and without autism spectrum disorder in an epidemiological population. Journal of Autism and Developmental Disorders 2020, 50, 180–188. [Google Scholar] [CrossRef] [PubMed]
- Kirby, A.V.; Bilder, D.A.; Wiggins, L.D.; Hughes, M.M.; Davis, J.; Hall-Lande, J.A.; Lee, L.C.; McMahon, W.M.; Bakian, A.V. Sensory features in autism: Findings from a large population-based surveillance system. Autism Research 2022, 15, 751–760. [Google Scholar] [CrossRef]
- Kirby, A.V.; Dickie, V.A.; Baranek, G.T. Sensory experiences of children with autism spectrum disorder: in their own words. Autism 2015, 19, 316–326. [Google Scholar] [CrossRef] [PubMed]
- Klintwall, L.; Holm, A.; Eriksson, M.; Carlsson, L.H.; Olsson, M.B.; Hedvall, A.; Gillberg, C.; Fernell, E. Sensory abnormalities in autism. A brief report. Research in Developmental Disabilities 2011, 32, 795–800. [Google Scholar] [CrossRef]
- Lane, S.J.; Leão, M.A.; Spielmann, V. Sleep, sensory integration/processing, and autism: A scoping review. Frontiers in Psychology 2022, 13, 877527. [Google Scholar] [CrossRef] [PubMed]
- Lane, S.J.; Mailloux, Z.; Schoen, S.; Bundy, A.; May-Benson, T.A.; Parham, L.D.; Smith Roley, S.; Schaaf, R.C. Neural Foundations of Ayres Sensory Integration®. Brain sciences 2019, 9, 153. [Google Scholar] [CrossRef] [PubMed]
- Lecuona, E.; Van Jaarsveld, A.; Raubenheimer, J.; Van Heerden, R. Sensory integration intervention and the development of the premature infant: A controlled trial. South African Medical Journal 2017, 107, 976–982. [Google Scholar] [CrossRef]
- Leekam, S.R.; Nieto, C.; Libby, S.J.; Wing, L.; Gould, J. Describing the sensory abnormalities of children and adults with autism. Journal of Autism and Developmental Disorders 2007, 37, 894–910. [Google Scholar] [CrossRef]
- Little, L.M.; Ausderau, K.; Freuler, A.; Sideris, J.; Baranek, G.T. Caregiver strategies to sensory features for children with autism and developmental disabilities. Frontiers in Psychology 2022, 13, 905154. [Google Scholar] [CrossRef]
- Loh, S.Y.; Ee, S.I.; Marret, M.J. Sensory processing and its relationship to participation among childhood occupations in children with autism spectrum disorder: Exploring the profile of differences. International Journal of Developmental Disabilities 2021, 69, 226–237. [Google Scholar] [CrossRef]
- Miller, L.J.; Anzalone, M.E.; Lane, S.J.; Cermak, S.A.; Osten, E.T. Concept evolution in sensory integration: A proposed nosology for diagnosis. American Journal of Occupational Therapy 2007, 61, 135–140. [Google Scholar] [CrossRef]
- Miller, L.J.; Schoen, S.A.; Mulligan, S.; Sullivan, J. Identification of sensory processing and integration symptom clusters: A preliminary study. Occupational Therapy International 2017, 2876080. [Google Scholar] [CrossRef]
- Mulligan, S.; Douglas, S.; Armstrong, C. Characteristics of idiopathic sensory processing disorder in young children. Frontiers in Integrative Neuroscience 2021, 15, 647928. [Google Scholar] [CrossRef]
- McQuiddy, V.A.; Ingram, M.; Vines, M.; Teeters, S.; Ramstetter, A. & Strain-Roggs, S. Long-term impact of an occupational therapy intervention for children with challenges in sensory processing and integration. American Journal of Occupational Therapy 2024, 78, 7804185060. [Google Scholar] [CrossRef]
- Omairi, C.; Mailloux, Z.; Antoniuk, S.A.; Schaaf, R. Occupational therapy using Ayres Sensory Integration®: A randomized controlled trial in Brazil. American Journal of Occupational Therapy 2022, 76, 7604205160. [Google Scholar] [CrossRef]
- Parham, L.D.; Ecker, C.L.; Kuhaneck, H.; Henry, D.A.; Glennon, T.J. (2021). Sensory processing measure, second edition (SPM-2). Western Psychological Services.
- Parham, L.D.; Roley, S.S.; May-Benson, T.A.; Koomar, J.; Brett-Green, B.; Burke, J.P.; Cohn, E.S.; Mailloux, Z.; Miller, L.J.; Schaaf, R.C. Development of a fidelity measure for research on the effectiveness of the Ayres sensory Integration intervention. American Journal of Occupational Therapy 2011, 65, 133–142. [Google Scholar] [CrossRef]
- Robertson, C.E.; Baron-Cohen, S. Sensory perception in autism. Nature Reviews Neuroscience 2017, 18, 671–684. [Google Scholar] [CrossRef]
- Schaaf, R.C.; Benevides, T.; Mailloux, Z.; Faller, P.; Hunt, J.; van Hooydonk, E.; Freeman, R.; Leiby, B.; Sendecki, J.; Kelly, D. An intervention for sensory difficulties in children with autism: A randomized trial. Journal of Autism and Developmental Disorders 2014, 44, 1493–1506. [Google Scholar] [CrossRef]
- Schaaf, R.C.; Mailloux, Z. (2015). A clinician’s guide for implementing Ayres sensory integration: Promoting participation for children with autism. AOTA Press.
- Schaaf, R.C.; Mailloux, Z.; Ridgway, E.; Berruti, A.S.; Dumont, R.L.; Jones, E.A.; Leiby, B.E.; Sancimino, C.; Yi, M.; Molholm, S. Sensory phenotypes in autism: Making a case for the inclusion of sensory integration functions. Journal of Autism and Developmental Disorders 2023, 53, 4759–4771. [Google Scholar] [CrossRef] [PubMed]
- Schaaf, R.C.; Toth-Cohen, S.; Johnson, S.L.; Outten, G.; Benevides, T.W. The everyday routines of families of children with autism: Examining the impact of sensory processing difficulties on the family. Autism 2011, 15, 373–389. [Google Scholar] [CrossRef] [PubMed]
- Schoen, S.A.; Lane, S.J.; Mailloux, Z.; May-Benson, T.; Parham, L.D.; Smith Roley, S.; Schaaf, R.C. A systematic review of Ayres sensory integration intervention for children with autism. Autism Research 2019, 12, 6–19. [Google Scholar] [CrossRef]
- Steinbrenner, J.R.; Hume, K.; Odom, S.L.; Morin, K.L.; Nowell, S.W.; Tomaszewski, B.; Szendrey, S.; McIntyre, N.S.; Yucesoy-Ozkan, S.; Savage, M.N. (2020). Evidence-based practices for children, youth, and young adults with autism. The University of North Carolina at Chapel Hill, Frank Porter Graham Child Development Institute.
- Sukhera, J. Narrative reviews: Flexible, rigorous, and practical. Journal of Graduate Medical Education 2022, 14, 414–417. [Google Scholar] [CrossRef] [PubMed]
- Tomchek, S.D.; Dunn, W. Sensory processing in children with and without autism: A comparative study using the Short Sensory Profile. American Journal of Occupational Therapy 2007, 61, 190–200. [Google Scholar] [CrossRef]
- van Venrooij, L.T.; Rusu, V.; Vermeiren, R.R.J.M.; Koposov, R.A.; Skokauskas, N.; Crone, M.R. Clinical decision support methods for children and youths with mental health disorders in primary care. Family Practice 2022, 39, 1135–1143. [Google Scholar] [CrossRef] [PubMed]
- Verma, B.; Madhumita, D.; Sehgal, R. Exploring prevalence of sensory patterns among children with developmental disabilities: A cross-sectional study. International Journal of Contemporary Pediatrics 2025, 12, 471–478. [Google Scholar] [CrossRef]
- Whiting, C.C.; Schoen, S.A.; Schaaf, R.C.; Auld-Wright, K.; McKeon, M.C. Guidelines for occupational therapy using Ayres Sensory Integration® in school-based practice: A validation study. American Journal of Occupational Therapy 2025, 79, 7904205190. [Google Scholar] [CrossRef] [PubMed]
- Wood, J.K. Sensory processing disorder: Implications for primary care nurse practitioners. Journal for Nurse Practitioners 2020, 16, 514–516. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).