Submitted:
17 September 2025
Posted:
19 September 2025
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
2.1. Sample and Study Area Description
2.2. Experimental Design and Control Setup
2.3. Measurement Methods and Quality Control
2.4. Data Processing and Model Formulation
3. Results and Discussion
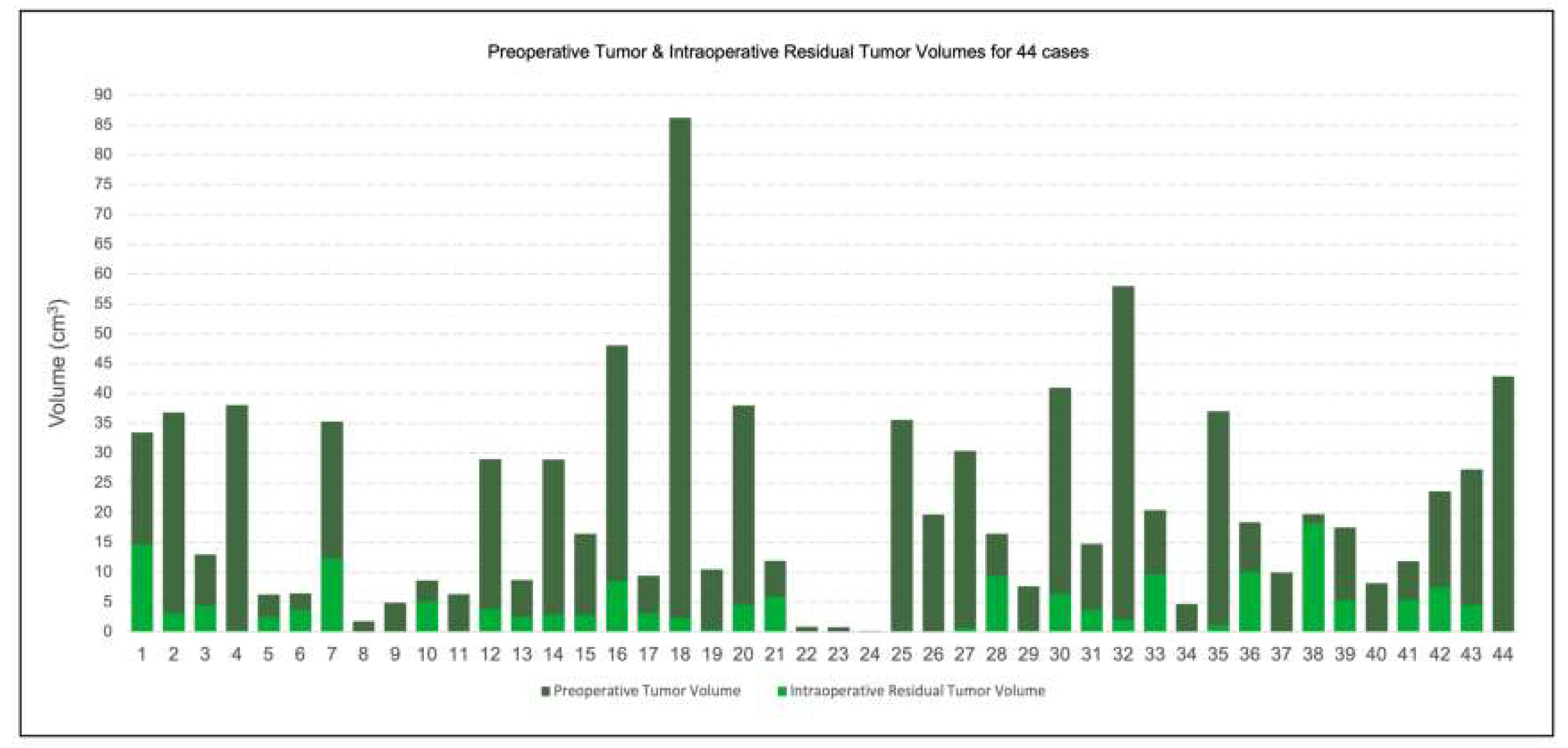
3.1. Margin Accuracy and Residual Tumor Volume
3.2. Latency and Resection Efficiency
3.3. Comparison with Previous Studies
3.4. Clinical Implications and Future Perspectives
4. Conclusion
References
- Gavaghan, K. , Oliveira-Santos, T., Peterhans, M., Reyes, M., Kim, H., Anderegg, S., & Weber, S. (2012). Evaluation of a portable image overlay projector for the visualisation of surgical navigation data: phantom studies. International journal of computer assisted radiology and surgery, 7(4), 547-556.
- Furman, A. A. , & Hsu, W. K. (2021). Augmented reality (AR) in orthopedics: current applications and future directions. Current reviews in musculoskeletal medicine, 14(6), 397-405.
- Yang, Y. , Leuze, C., Hargreaves, B., Daniel, B., & Baik, F. (2025). EasyREG: Easy Depth-Based Markerless Registration and Tracking using Augmented Reality Device for Surgical Guidance. arXiv:2504.09498.
- Mago, V. (2021). Augmented reality in plastic surgery education. The Egyptian Journal of Plastic and Reconstructive Surgery, 45(1), 19-25.
- Xu, J. (2025). Semantic Representation of Fuzzy Ethical Boundaries in AI.
- Yang, Y. , Leuze, C., Hargreaves, B., Daniel, B., & Baik, F. (2025). EasyREG: Easy Depth-Based Markerless Registration and Tracking using Augmented Reality Device for Surgical Guidance. arXiv:2504.09498.
- Wu, C. , Chen, H., Zhu, J., & Yao, Y. (2025). Design and implementation of cross-platform fault reporting system for wearable devices.
- Ji, A. , & Shang, P. (2019). Analysis of financial time series through forbidden patterns. Physica A: Statistical Mechanics and its Applications, 534, 122038.
- Yao, Y. (2024, May). Design of neural network-based smart city security monitoring system. In Proceedings of the 2024 International Conference on Computer and Multimedia Technology (pp. 275-279). [Google Scholar]
- Chen, F. , Li, S., Liang, H., Xu, P., & Yue, L. (2025). Optimization Study of Thermal Management of Domestic SiC Power Semiconductor Based on Improved Genetic Algorithm.
- Li, W., Xu, Y., Zheng, X., Han, S., Wang, J., & Sun, X. (2024, October). Dual advancement of representation learning and clustering for sparse and noisy images. In Proceedings of the 32nd ACM International Conference on Multimedia (pp. 1934-1942).
- Sun, X. , Meng, K., Wang, W., & Wang, Q. (2025, March). Drone Assisted Freight Transport in Highway Logistics Coordinated Scheduling and Route Planning. In 2025 4th International Symposium on Computer Applications and Information Technology (ISCAIT) (pp. 1254-1257). IEEE.
- Li, C. , Yuan, M., Han, Z., Faircloth, B., Anderson, J. S., King, N., & Stuart-Smith, R. (2022). Smart branching. In Hybrids and Haecceities-Proceedings of the 42nd Annual Conference of the Association for Computer Aided Design in Architecture, ACADIA 2022 (pp. 90-97). ACADIA.
- Chen, H., Li, J., Ma, X., & Mao, Y. (2025). Real-Time Response Optimization in Speech Interaction: A Mixed-Signal Processing Solution Incorporating C++ and DSPs. Available at SSRN 5343716.
- Chan, H. H. , Haerle, S. K., Daly, M. J., Zheng, J., Philp, L., Ferrari, M.,... & Irish, J. C. (2021). An integrated augmented reality surgical navigation platform using multi-modality imaging for guidance. PLoS One, 16(4), e0250558.
- Guo, L. , Wu, Y., Zhao, J., Yang, Z., Tian, Z., Yin, Y., & Dong, S. (2025, May). Rice Disease Detection Based on Improved YOLOv8n. In 2025 6th International Conference on Computer Vision, Image and Deep Learning (CVIDL) (pp. 123-132). IEEE.

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).



