1. Introduction
The growing global burden of complex wounds poses significant clinical, economic, and social challenges, particularly in ageing populations and in individuals with chronic diseases. Specialised nursing care in this field has emerged as a cornerstone strategy to promote effective wound healing, reduce hospitalisation rates, and optimise resource allocation within healthcare systems [
1]. International evidence consistently highlights that advanced nursing care models, led by nurses with specific expertise in wound management, contribute to lower complication rates—such as infections, amputations, and unplanned readmissions—and to better clinical outcomes [
2].
Despite this, the implementation and evaluation of specialised wound care nursing services remain uneven across health systems. In the Portuguese context, there is a striking absence of standardised criteria to guide referrals to specialised nursing consultations for complex wounds. Moreover, there is limited evidence concerning the economic impact and cost-effectiveness of such consultations, both in direct and indirect terms [
3].
This gap compromises equity in access, continuity of care, and optimal use of specialised clinical expertise.
In light of these limitations, this study addresses a critical and unmet need: the development and validation of a structured referral model for specialised nursing consultation in complex wound care. This model aims to ensure that individuals who would most benefit from advanced, specialised nursing interventions are identified and referred in a timely and consistent manner.
To this end, we adopted a rigorous consensus-based methodology, combining Focus Group and Delphi techniques, to engage national experts in wound care and systematically develop a set of validated referral criteria. The methodological steps and findings are detailed in the following sections.
2. Materials and Methods
To validate the referral model for specialised nursing consultation in complex wound care, a structured consensus methodology was adopted, incorporating both qualitative and quantitative approaches. Specifically, a sequential design combining Focus Group and Delphi techniques was employed. This mixed-method consensus approach is increasingly recognised as robust in health research, especially when aiming to establish expert agreement on clinical guidelines or referral criteria where empirical evidence is limited or inconsistent [
4,
6].
2.1. Design and Rationale
Given the lack of standardised referral criteria for complex wound care nursing consultations in Portugal [
1], a two-phase consensus process was undertaken. The first phase involved a focus group with national wound care experts to explore, in detail, their views on essential referral indicators. The second phase employed the Delphi method to validate and refine the identified criteria, ensuring wider expert agreement and minimising the influence of dominant voices often seen in face-to-face settings [
5,
6].
This study followed ethical research principles as outlined by the Medical Research Involving Human Subjects Act (WMO). Since it did not involve any physical or psychological interventions, formal approval by a Medical Ethics Review Committee was not necessary. However, all participants gave informed written consent prior to taking part and were assured of confidentiality, voluntariness, and data protection. No financial incentives were offered.
The study was also designed and reported in accordance with the Critical Appraisal Skills Programme (CASP) and the Consolidated Criteria for Reporting Qualitative Research (COREQ) [
7], ensuring methodological transparency and reproducibility.
2.2. Phase I – Focus Group Procedure
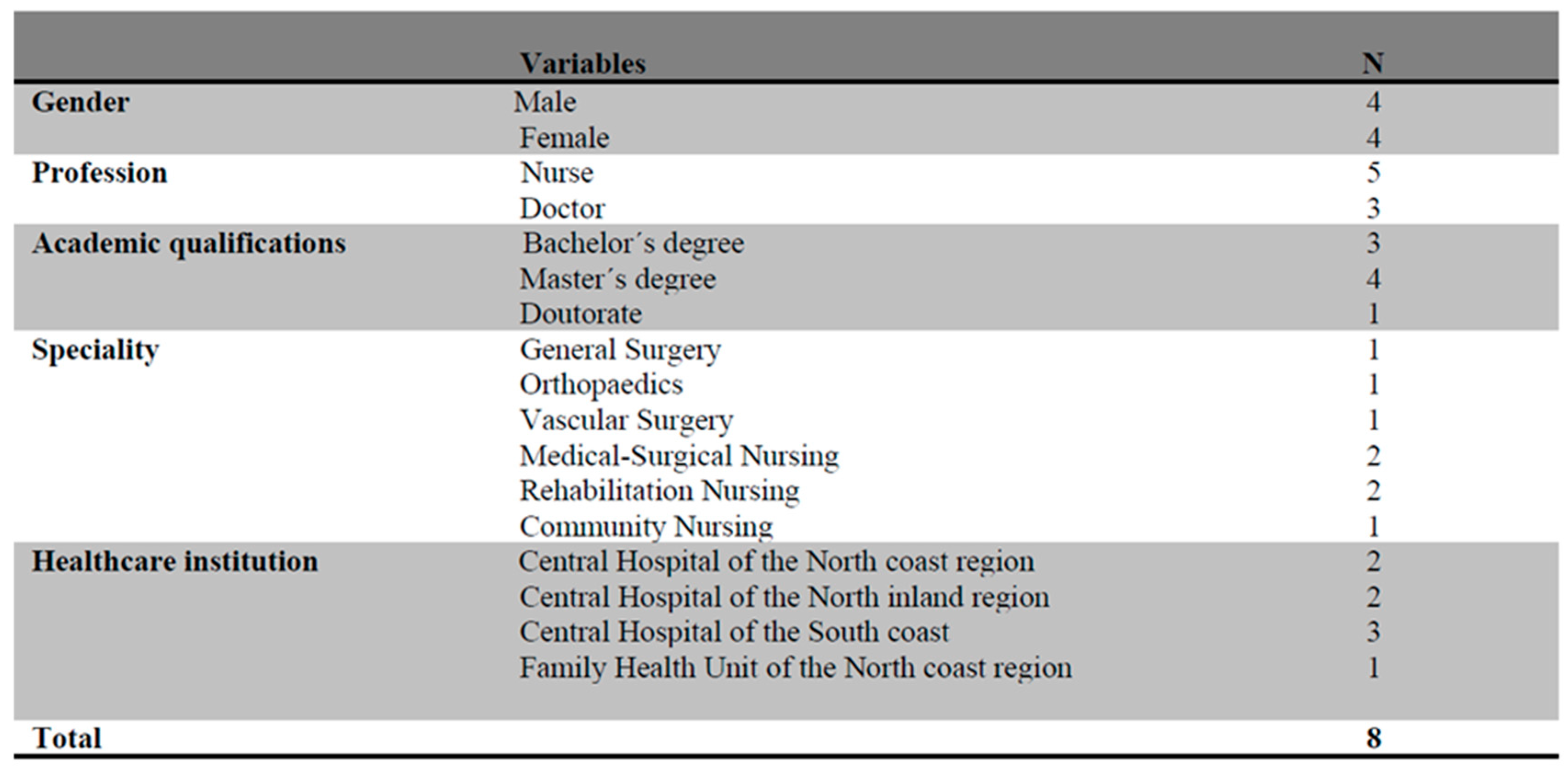
The Focus Group was conducted with a purposive sample of eight professionals (n=8), including three physicians (specialists in general, orthopaedic, and vascular surgery) and five specialist nurses, all recognised nationally for their clinical expertise in complex wound management. Recruitment followed maximum variation sampling to ensure diversity in clinical background and geographic location. Invitations and informed consent forms were distributed electronically.
The session was held online and facilitated by an experienced qualitative researcher. Methodological guidelines proposed by Krueger & Casey (2014) were followed to improve group dynamics and data quality. The discussion focused on defining referral indicators for specialised nursing consultation in complex wound care. The session was audio-recorded and transcribed verbatim by the interviewer. Data from the Focus Group were analysed using thematic content analysis, supported by NVivo 15® software, which enabled systematic coding, categorisation, and identification of recurrent patterns [
8]. Two researchers independently coded the transcripts, and disagreements were resolved through consensus. Constant comparison was employed to iteratively refine emerging themes against the literature, ensuring theoretical sensitivity. Thematic saturation was reached when no new categories emerged during analysis.
2.3. Phase II – Delphi Technique
To validate the referral criteria identified in the Focus Group, a Delphi panel was conducted involving national experts in wound care affiliated with the Portuguese Wound Care Association. The Delphi method is widely used in health research to build expert consensus, especially when recommendations must be made in areas where evidence is limited or practice varies [
4].
Eighty professionals were initially invited through institutional channels. After two rounds of invitations, 36 agreed to participate, and 26 met the eligibility criteria for expert status (e.g., advanced training in tissue viability, clinical experience of at least 10 years, and publications in wound care). These participants completed successive rounds of questionnaires designed to evaluate the relevance and clarity of the proposed referral criteria using a 5-point Likert scale.
Data were analysed using IBM SPSS Statistics®, version 26. Descriptive statistics determined consensus levels, with ≥70% agreement considered indicative of strong consensus, in line with Delphi methodological standards [
6]. One criterion was marginally below this threshold (69.2%) but was retained due to its clinical significance. Considering the high levels of agreement across most items and the risk of attrition in further rounds, a third round was deemed unnecessary.
2.4. Rigor and Validity
To ensure methodological rigour, triangulation was applied through investigator triangulation, data triangulation, and theoretical triangulation. Investigator triangulation involved three independent researchers conducting parallel analyses to promote dependability and confirmability. Data triangulation referred to the integration of qualitative data from the Focus Group and quantitative data from the Delphi panel, enabling a more comprehensive understanding of expert perspectives. Theoretical triangulation was achieved by consistently comparing the findings with current literature throughout the analysis and model refinement process, as supported by the literature [
9,
10]. The transparency of procedures, the independence of analysis, and the achievement of data saturation contributed to the credibility, transferability, and overall trustworthiness of the results.
3. Results
3.1. Focus Group
Eight health professionals participated in the Focus Group, including three physicians (specialising in general surgery, orthopaedics, and vascular surgery) and five specialist nurses. All participants were affiliated with reference institutions from both northern and southern Portugal (
Table 1).
Recruitment and informed consent procedures were carried out via institutional email, and all participants signed the consent forms prior to enrolment. The meeting was held online and attended by the research team, one of whom was responsible for recording the session.
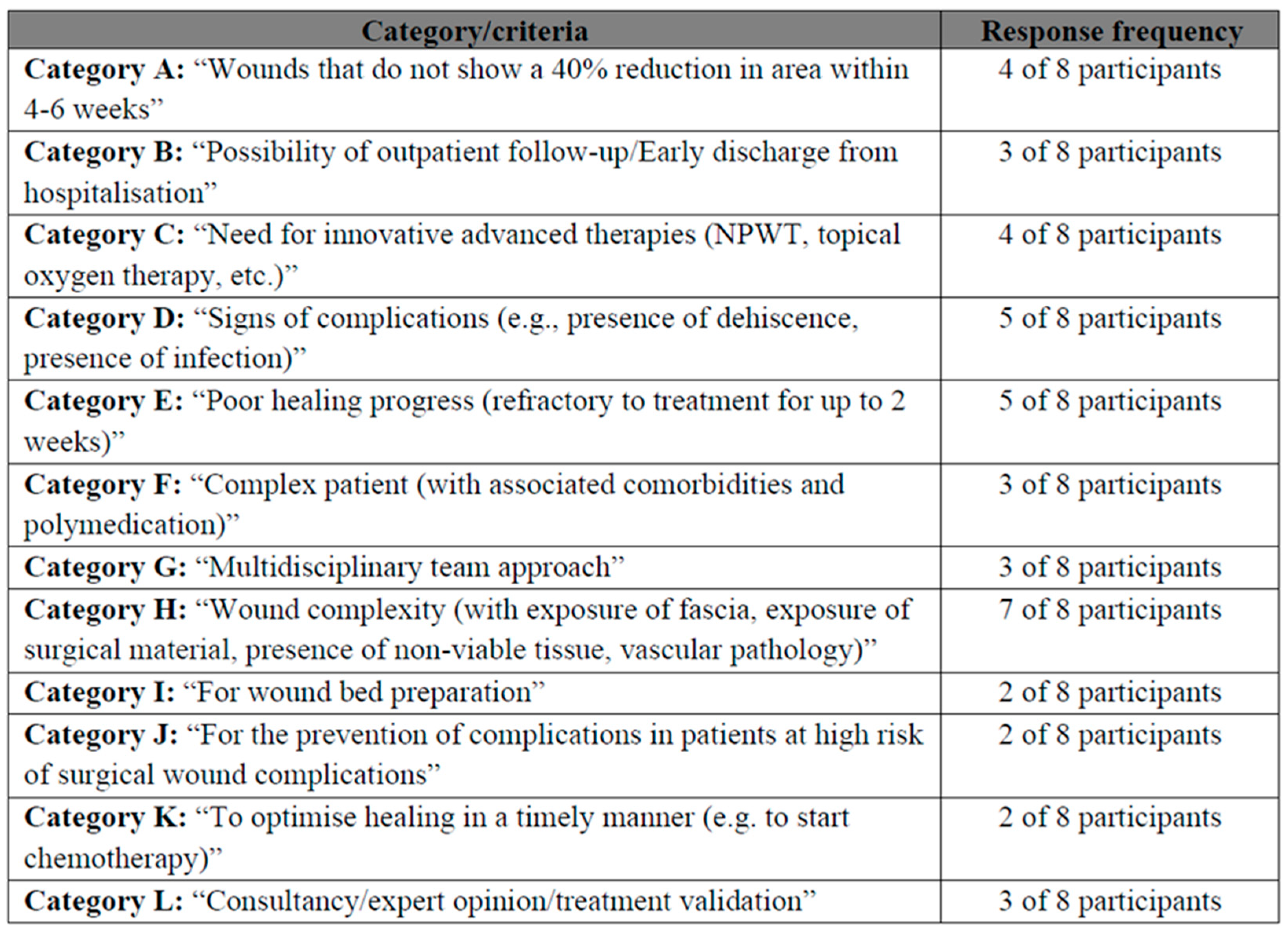
The Focus Group enabled in-depth discussion of referral criteria for specialised nursing consultation. Through systematic content analysis, several thematic categories were identified and subsequently organised (Table 3). Although not all categories had the same level of endorsement, even less frequent contributions were considered valuable, as they reflected specific perspectives grounded in clinical experience.
Category H, mentioned by seven out of eight participants, emerged as the most prominent criterion, highlighting its central relevance to referral decisions. Other categories such as I, J, and K, although less frequently cited, were considered significant as they provided specific but valuable insights that expanded the scope of discussion.
3.2. Delphi Panel
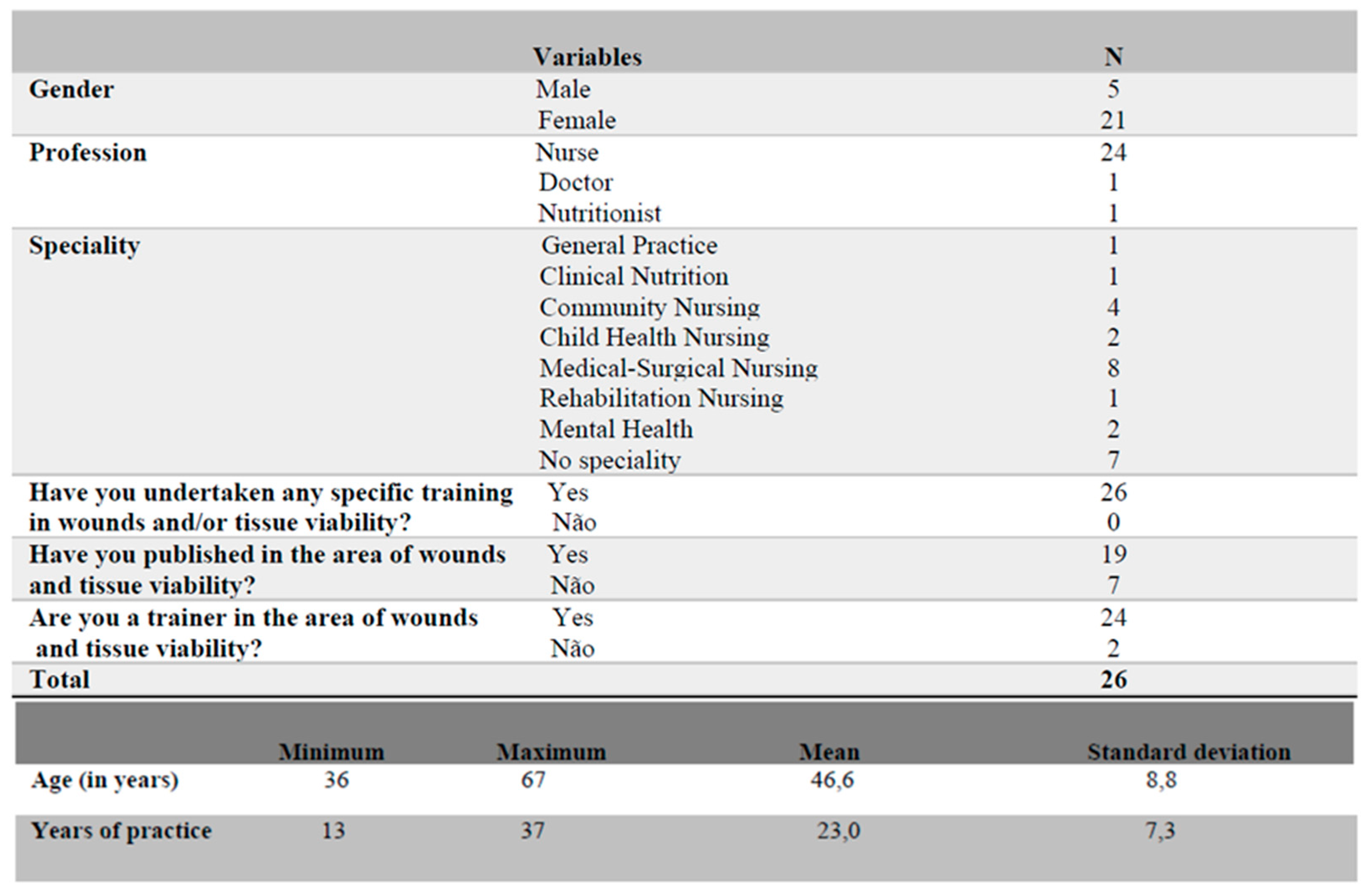
For the Delphi process, an invitation was sent to approximately 80 members of the Portuguese Wound Care Association through the association’s secretariat. After repeated invitations, 36 professionals responded positively, and 26 ultimately met the predefined eligibility criteria for wound care expertise.
The final panel (n = 26) was predominantly female (n = 21), with a mean age of 46.6 years and an average professional experience of over 13 years. Most participants were nurses (n = 24), of whom 17 held a recognised nursing speciality. The remaining participants included a physician specialised in General Practice (n = 1) and a nutritionist specialised in Clinical Nutrition (n = 1). All participants had formal training in wound management or tissue viability, including master’s degrees (n = 3), advanced training (n = 16), and postgraduate qualifications (n = 7). The majority also reported academic output (publications, n = 19) and experience as trainers in the field (n = 24) (
Table 2).
Two of the criteria for defining the profile of the expert who would continue to take part in Delphi concerned publications and training as a trainer in the area of wounds and tissue viability, the majority of whom had publications (n=19) and were trainers in this area (n=24).
Considering what the literature says about the criteria for referring a person with a wound to a specialised complex wound nursing and based on the clinical experience in wound care of each of the Focus Group participants, putting together a set of statements aimed at the topic under discussion became a very interesting task due to the richness of the sharing and contributions that each participant provided at the meeting.
As soon as all the content analysis had been carried out, were categorised, as shown in
Table 3.
Although not all the categories had the same number of answers, all were taken into consideration in the analysis, because we believe that even the less prevalent ones brought significant contributions and an important perception from each participant on the subject under study.
Category H (7 out of 8 participants) emerged as the most relevant for the participants, being mentioned by almost everyone, which indicates its great importance with regard to referral to this specialised consultation.
Categories I, J and K (2 out of 8 participants), although less addressed by the participants, brought crucial points of view, although more specific, taking into account the practice and clinical experience of the experts who pointed them out, bringing a more specific perception, but which in our opinion deserves to be considered, due to the scope and contribution it brought to the study.
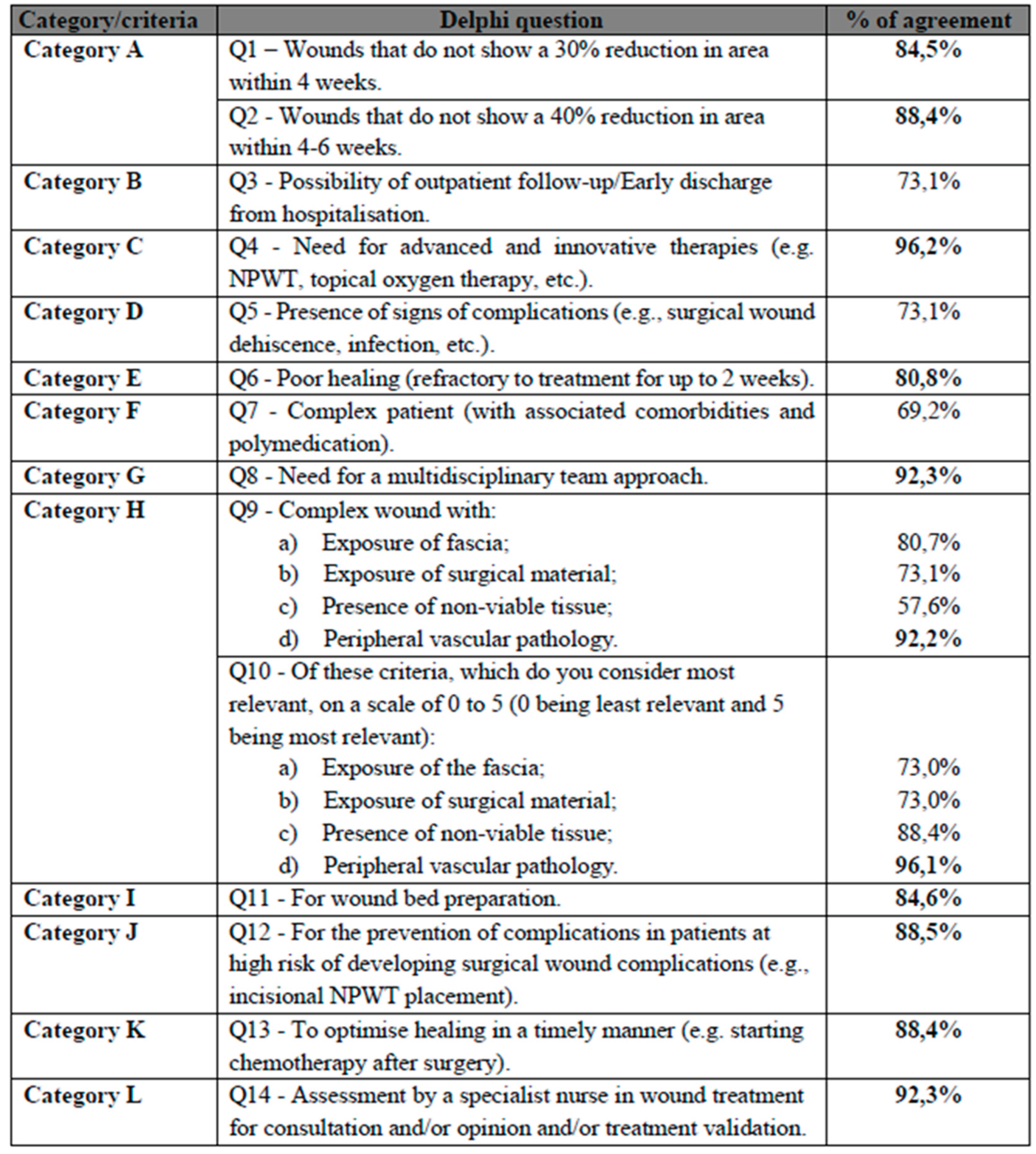
3.3. Validation of Referral Criteria
The statements generated during the Focus Group were refined into a set of potential referral criteria, which were subsequently evaluated in the Delphi rounds. Results from the Delphi process are presented in
Table 4.
Consensus was defined as ≥70% agreement. This decision balanced methodological rigour with practical concerns, namely time constraints and the risk of reduced participation in subsequent rounds.
Overall, the majority of referral criteria surpassed this benchmark, with most achieving robust agreement levels above 80%. Particularly noteworthy were the criteria concerning the need for advanced and innovative therapies (Category C, 96.2%), the need for a multidisciplinary team approach (Category G, 92.3%), the presence of peripheral vascular pathology (Category H, 92.2%), and the role of specialist nursing assessment (Category L, 92.3%). These results highlight the strong consensus among experts regarding the complexity and severity of clinical situations that justify referral to specialised nursing consultation.
Only one item (Category F – complex patient with multiple comorbidities and polymedication) fell slightly below the predefined threshold (69.2%). Despite its borderline result, this criterion was not considered central to the core objectives of the referral model and was therefore not subjected to an additional Delphi round. This decision balanced methodological rigour with feasibility, given the potential disadvantages of extending the process, such as participant attrition and reduced engagement in subsequent rounds.
Importantly, the high levels of agreement across most categories underscore the clinical relevance and applicability of the proposed model. The Delphi validation not only confirmed the criteria identified during the Focus Group but also provided a prioritisation of referral indicators, with wound complexity, advanced therapeutic needs, and vascular involvement emerging as the strongest determinants for specialised nursing consultation in complex wound care.
3.4. Additional Contributions
In addition to closed responses, participants had the opportunity to provide free-text observations. A minority (n = 8) contributed in this section, generally reinforcing criteria already included in the questionnaire. Examples included references to stalled healing beyond four weeks, clinical infection, exposure of delicate anatomical structures, need for advanced therapeutic modalities (e.g., negative pressure therapy, topical oxygen), and the optimisation of healing prior to initiating chemotherapy. These repeated statements were interpreted as further confirmation of the relevance and consistency of the selected referral criteria.
The integration of Focus Group and Delphi results yielded a validated set of referral criteria for specialised nursing consultation in complex wound care. The high level of agreement among experts, particularly in categories related to wound complexity, advanced therapies, and risk of deterioration, underscores their clinical importance. Even less prevalent categories were retained, given their potential to inform comprehensive and patient-centred referral practices.
4. Discussion
This study presents a major advance in establishing evidence-informed and consensus-driven referral criteria for specialist nursing consultation in complex wound care—an area marked by fragmented clinical pathways and variable practices. The integration of expert insights through the Focus Group and their systematic validation via the Delphi process offers methodological rigour and clinical relevance.
Key findings and their meaning: The convergence around core criteria — particularly
wound complexity (Category H),
presence of complications (Category D),
and poor healing trajectories (Category E) — reflects a shared clinical perception that these factors critically determine the need for escalation of care. These align with international approaches, such as the Taiwanese Society of Cardiology and Plastic Surgery’s 2024 consensus on advanced vascular wounds, which emphasize multidisciplinary evaluation and structured referral protocols [
11,
12,
13].
The near-unanimous agreement on the need for advanced and innovative therapies (Category C, 96.2%) underscores the specialist nature of such interventions. This mirrors evidence demonstrating that modalities like NPWT and topical oxygen therapy deliver optimal outcomes only when implemented within specialist, protocol-based frameworks [
14,
15].
High consensus regarding a multidisciplinary team approach (Category G, 92.3%) and the role of specialist nursing assessment (Category L, 92.3%) resonates with integrated care models shown to reduce complications, hospital stays, and amputations [
9]. It further mirrors findings from integrative reviews advocating for structured interdisciplinary referral pathways in maintaining and non-healable wound management [
10,
16].
Clinical and system-level implications: This validated referral model offers Portugal a locally adapted, scalable, and scientifically grounded approach—addressing a critical gap in national wound care standards. It aligns with global best practices, such as the Wound Care Pathway and wound-type specific pathways (e.g., for diabetic foot and venous leg ulcers), which facilitate consistent, evidence-based care even for generalist clinicians [
17].
At the professional level, the study reinforces the leadership role of specialist wound care nurses. Literature consistently shows that advanced nursing practice in wound care enhances healing outcomes, supports cost-effectiveness through reduced readmissions, and elevates patient quality of life [
10,
18]. This referral framework empowers nurses as decision-makers, key gatekeepers, and system-level innovators.
Comparison with guidelines: NICE guidance, for example, indicates that wounds not improving after 2–4 weeks or those with complicating factors warrant specialist referral, aligning closely with several criteria validated here—especially in terms of healing trajectory, infection, and complex comorbidities [
10,
17,
19,
20,
21,
22].
Strategic value and generalisability: While similar referral tools exist internationally, our study’s tailored model offers relevance and validity specifically for the Portuguese NHS, mindful of local context, workflows, and professional scopes. These criteria can serve as policy anchors, support training curricula for wound care nurses, and facilitate auditing and quality assurance in specialist referral pathways.
Limitations and directions for future research include that, although the sample sizes (Focus Group n=8; Delphi n=26) are typical for consensus methods, testing the findings across different healthcare settings and institutions would improve external validity. Future research could investigate how the model influences patient outcomes, resource use, and fair access to specialised consultations.
5. Conclusions
The validated referral model marks a significant advance in standardising complex wound management, reinforcing the role of specialist nursing and ensuring that individuals with complex wounds receive timely and appropriate care.
This study makes a vital contribution to nursing science and clinical practice by providing, for the first time in Portugal, a validated set of referral criteria for specialised nursing consultation in complex wound care. In a context where evidence has been limited and referral practices often vary, the developed model offers an innovative, structured, and scientifically robust approach to guide clinical decision-making.
The validated criteria highlight the importance of wound complexity, poor healing progress, presence of complications, and the need for advanced therapies as key factors for referral. By incorporating expert consensus, this model strengthens the capacity of specialist nurses to act as primary decision-makers, ensuring prompt access to specialised care, reducing practice variation, and ultimately improving outcomes for patients with complex wounds. Although the main limitation was variable adherence to the Delphi process, the high level of consensus achieved suggests that the robustness and relevance of the findings were not compromised.
Beyond its immediate clinical relevance, this study provides a foundation for future research to test the model in different care settings, assess its impact on patient outcomes and healthcare costs, and explore its integration into digital decision-support tools. The criteria may also inform policy development and professional training, fostering more equitable, efficient, and person-centred wound care.
Acknowledgments
We would like to thank all the wound care experts who participated in the consensus groups.
Conflicts of Interest
We have no conflict of interest or financial interest to declare.
Abbreviations
The following abbreviations are used in this manuscript:
| CASP |
Critical Appraisal Skills Programme |
| COREQ |
COnsolidated criteria for REporting Qualitative |
| NPWT |
Negative Pressure Wound Therapy |
| NICE |
National Institute for Health and Care Excellence |
| NHS |
National Health Service |
| WMO |
Medical Research Involving Human Subjects Act |
References
- Heerschap, C. , & Duff, V. (2021). The Value of Nurses Specialized in Wound, Ostomy, and Continence: A Systematic Review. Advances in Skin & Wound Care. [CrossRef]
- Olsson, M. , Järbrink, K., Divakar, U., Bajpai, R., Upton, Z., Schmidtchen, A. and Car, J. (2019), The humanistic and economic burden of chronic wounds: A systematic review. Wound Rep Reg. [CrossRef]
- Guest, J. F. , Fuller, G. W., & Vowden, P. (2020). Wound care in the UK: Burden, treatment, and costs. International Wound Journal, 17(4), 899–906. [CrossRef]
- Boulkedid, R. , Abdoul, H., Loustau, M., Sibony, O., & Alberti, C. (2011). Using and reporting the Delphi method for selecting healthcare quality indicators: a systematic review. PloS ONE. [CrossRef]
- Krueger, R. A. & Casey, M. A. (2014). Focus groups: A practical guide for applied research.(5th ed.) Sage publications.
- Keeney, S., Hasson, F., & McKenna, H. P. (2001). A critical review of the Delphi technique as a research methodology for nursing. International Journal of Nursing Studies 2001, 38(2), 195–200. [CrossRef]
- Tong, A. , Sainsbury, P., & Craig, J. (2007). Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. International Journal for Quality in Health Care. [CrossRef]
- Bardin, L. (2018). Análise de conteúdo. (Edição revista e atualizada). Edições 70.
- Constant, J. , & Reed, J. (2022). Designing a new community lower limb haematoma pathway to prevent hospital admission and reduce cost. Wounds UK.
- Boersema, G. C. , Smart, H., Giaquinto-Cilliers, M. G. C., Mulder, M., Weir, G. R., Bruwer, F. A., Idensohn, P. J., Sander, J. E., Stavast, A., Swart, M., Thiart, S., & Van der Merwe, Z. (2021). Management of Nonhealable and Maintenance Wounds: A Systematic Integrative Review and Referral Pathway. Advances in Skin & Wound Care. [CrossRef]
- Frykberg, R. G., & Banks, J. (2015). Challenges in the Treatment of Chronic Wounds. Advances in wound care. 4(9), 560–582. [CrossRef]
- Gefen, A. , Alves, P., Ciprandi, G., Coyer, F., Milne, C., Ousey, K., Ohura, N., Waters, N., Worsley, P., Black, J., Barakat-Johnson, M., Beeckman, D., Fletcher, J., Kirkland-Kyhn, H., Lahmann, N. A., Moore, Z., Payan, Y., & Schlüer, A. B. (2020). An international consensus on device-related pressure ulcers: SECURE prevention. British Journal of Nursing. [CrossRef]
- Deschepper, M. , Labeau, S. O., Waegeman, W., Blot, S. I., DecubICUs study Team, & Eu-ropean Society of Intensive Care Medicine (ESICM) Trials Group collaborators (2021). Pressure injury prediction models for critically-ill patients should consider both the case-mix and local factors. Intensive & Critical Care Nursing. [CrossRef]
- Atkin, L. , Bućko, Z., Conde Montero, E., Cutting, K., Moffatt, C., Probst, A., Romanelli, M., Schultz, G. S., & Tettelbach, W. (2019). Implementing TIMERS: the race against hard-to-heal wounds. Journal of Wound Care, 23(Sup3a), S1–S50. [CrossRef]
- Gefen, A. , Alves, P., Creehan, S., Call, E., & Santamaria, N. (2019). Computer Modeling of Prophylactic Dressings: An Indispensable Guide for Healthcare Professionals. Advances in Skin & Wound Care. [CrossRef]
- Beeckman, D. , Cooper, M., Greenstein, E., Idensohn, P., Klein, R. J., Kolbig, N., LeBlanc, K., Milne, C., Treadwell, T., Weir, D., & White, W. (2024). The role community-based healthcare providers play in managing hard-to-heal wounds. International Wound Journal, 21, e14402. [CrossRef]
- World Union of Wound Healing Societies (2025) Implementing Wound Balance: Outcomes and future recommendations. London: Wounds International. Available at: www.woundsinternational.com.
- Ribeiro, O. M. P. L. , Martins, M. M. F. P. da S., & Tronchin, D. M. R. (2016). Modelos de prática profissional de enfermagem: revisão integrativa da literatura. Revista de Enfermagem Referência. [CrossRef]
- van Rijswijk, L. , & Beitz, J. M. (2025). Updating Wound Care Algorithms: A Systematic, Focused Review. Journal of Wound, Ostomy, and Continence Nursing. [CrossRef]
- Ahmajärvi, K., Isoherranen, K., & Venermo, M. (2022). Cohort study of diagnostic delay in the clinical pathway of patients with chronic wounds in the primary care setting. BMJ open 12(11), e062673. [CrossRef]
- Berti-Hearn, L. (2022). Back to the Basics: Wound Assessment, Management, and Documentation. Home healthcare now, 40(5), 245–251. [CrossRef]
- Buckley, K. M. , Adelson, L. K., & Agazio, J. G. (2009). Reducing the risks of wound consultation: adding digital images to verbal reports. Journal of Wound, Ostomy, and Continence Nursing. [CrossRef]
Table 1.
Sociodemographic characterisation of Focus Group participants.
Table 1.
Sociodemographic characterisation of Focus Group participants.
Table 2.
Sociodemographic characteristics of participants in the Delphi.
Table 2.
Sociodemographic characteristics of participants in the Delphi.
Table 3.
Categorisation of referral criteria for specialist nursing consultations in the treatment of complex wounds.
Table 3.
Categorisation of referral criteria for specialist nursing consultations in the treatment of complex wounds.
Table 4.
Validation of the referral criteria for the specialised nursing consultation for the treatment of complex wounds.
Table 4.
Validation of the referral criteria for the specialised nursing consultation for the treatment of complex wounds.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).