Introduction
Duodenal ulcers are open sores or break in the mucosal lining in the initial part of the small intestine. These are a subtype of peptic ulcer disease (PUD), which also includes gastric ulcers. PUD occurs due to imbalance between gastric acids and protective mucosal lining of stomach and duodenum. The imbalance is seen commonly in Helicobacter pylori infection and non-steroidal anti-inflammatory use [
1]. Other associated risk factors include smoking and alcohol use.
H. pylori causes chronic gastritis, resulting in increased gastrin production, foveolar hyperplasia, and hence gastric acid release, while NSAIDs via prostaglandin synthesis inhibition lead to altered mucus lining. Studies have shown that these occur independently and presence of both risk factors has even demonstrated dual histological appearance of ulcers [
2]. Mortality in duodenal ulcers is attributed to complications of bleeding [
3]. In a study evaluating risk of mortality from duodenal and gastric ulcers, higher deaths were seen in patients with malignancy directly or leading up to the ulcer [
4].
The prevalence of peptic ulcer disease range between 0·12% and 1·5% reported in recent studies which has significantly lower than 5-15% reported in studies from a decade ago [
5,
6].There has been a concurrent decline in mortality rates of duodenal ulcers in the last decades as well [
7] with men and the elderly being identified at higher risk [
8]
Our study aimed to examine the mortality rates due to duodenal ulcers in the United States from 1999 to 2020. By employing age-adjusted mortality rates (AAMR), we aimed to identify disparities among diverse population groups. Our primary objective was to evaluate temporal trends and geographical variations in duodenal ulcer-related mortality specifically among the elderly U.S. population.
Methods
Study Design
This study utilized mortality data from the Centers for Disease Control and Prevention Wide-Ranging Online Data for Epidemiologic Research (CDC-WONDER) database [
9]. This comprehensive database includes death certificate information from all 50 states of the US and the District of Columbia. Since a publicly available, de-identified dataset was used, institutional review board (IRB) approval was not necessary. Deaths due to duodenal ulcers were examined in individuals aged 35 years and older from 1999 to 2020, identified using International Classification of Diseases Tenth Revision (ICD-10) codes K26– used for mortality coding and classification on death certificates in the USA. The analysis employed multiple cause-of-death data, capturing all deaths where duodenal ulcers were mentioned on the death certificate. This study complied with the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines for reporting observational studies [
10].
Statistical Analysis
The number of deaths attributed to duodenal ulcers was divided by the total population of the specified year to calculate the crude death rate (CR) per 100,000 individuals. To make fair comparisons of diverse populations possible, direct standardization of the death rates was done by applying age-specific mortality rates to the USA 2000 standard population’s age distribution and calculating Age-Adjusted Mortality Rates (AAMRs). AAMRs were used to explore mortality trends based on gender, race or ethnicity, census region, specific states, and urban versus rural areas.
We utilized the Joinpoint Regression Program 5.0.2 (developed by the Statistical Research and Applications Branch, National Cancer Institute) [
11] to calculate Annual Percentage Changes (APCs) and Average Annual Percentage Changes (AAPCs) in AAMRs, with corresponding 95% confidence intervals (95% CIs). This program identifies the most appropriate joinpoint model by testing different numbers of joinpoints and assessing statistical significance through Monte Carlo Permutation Tests [
12]. A two-tailed t-test was used to determine whether the slope indicating shifts in mortality rates differed significantly from zero, with p-values < 0.05 considered statistically significant.
Results
Overall Trend
A total of 52674 individuals with duodenal ulcer died from 1999 to 2020, with an AAPC of -1.6895* (95% CI = -2.4916 to -0.8807). The average AAMR per 1,000,000 was 7.158 (95% CI = 7.097 to 7.22). In 1999, the AAMR was recorded at 10.568 (95% CI =10.182 to 10.954). This rate eventually decreased to 7.938 (95% CI = 7.663 to 8.214) in 2020. The AAMR steadily decreased from 1999 to 2007 with an APC of -6.4723* (95% CI = -7.499 to -5.4338). Thereafter, a comparatively less steep decline in the AAMR was observed till 2014 with an APC of -1.1354 (95% CI = -2.9981 to 0.763). This is followed by a steep rise in AAMR from 2014 to 2020 with an APC of 4.836* (95% CI =2.6656 to 6.1303) but not at the same rate as decline in initial AAMR. We applied the Cuzick test across overall and found a z value of -2.38 (Prob > |z| = 0.017).
Gender Distribution
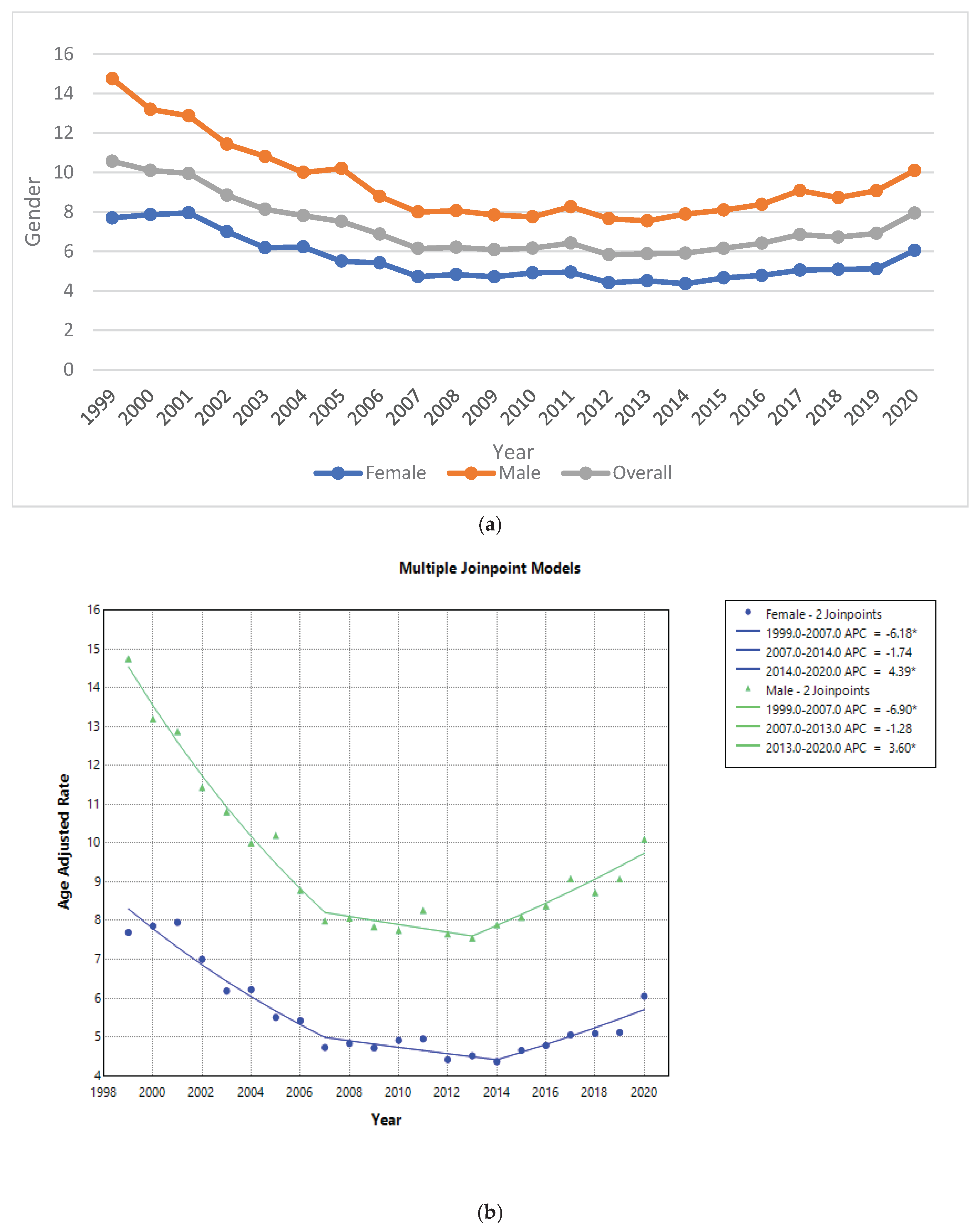
From 1999 to 2020, male population exhibited an AAMR of 9.286 (95% CI = 9.178 to 9.395), while female population exhibited an AAMR of 5.456 (95% CI =5.386 to 5.526). During this period,, the AAMR for male population decreased considerably from 14.755 (95% CI = 14.016 to 15.495) in 1999 to 10.1 (95% CI = 9.634 to 10.567) in 2020, and the AAMR for female population, it only decreased from 7.695 (95% CI = 7.271 to 8.118) in 1999 to 6.049 (95% CI = 5.729 to 6.37) in 2020. The AAMR in female population exhibited a steady declining trend at first from 1999 to 2007, with an APC of -6.18* (95% CI = -7.6843 to -4.648), a shallow decline from 2007 to 2014 with an APC of -1.74 (95%CI = -4.4744 to 1.0703) and then a rise from 2014 to 2020 with APC of 4.39* (95% CI = 1.8025 to 7.0463). Whereas, a steep declining trend with an APC of -6.90* (95% CI = -7.9622 to -5.8188) from 1999 to 2007 for male population was followed by a shallow decrease from 2007-2013 with an APC of -1.28 (95%CI = -3.7938 to 1.303), and then a gentle rise from 2013-2020 with an APC of 3.60* (95%CI = 2.233 to 4.98) was recorded respectively. We applied the Cuzick test across Gender and found a z value of 5.42 (Prob > |z| = 0.000). We applied Mann-Whitney U test across gender as well and found a significant p value of 0.000.
Figure 1.
(a) Age-adjusted mortality rates (AAMRs) for duodenal ulcer per 1,000,000 individuals in the United States, from 1999 to 2020, presented overall and separated by sex. (b) Joinpoint illustration of Duodenal ulcer related AAMRs per 1,000,000 individuals in the United States, from 1999 to 2020.
Figure 1.
(a) Age-adjusted mortality rates (AAMRs) for duodenal ulcer per 1,000,000 individuals in the United States, from 1999 to 2020, presented overall and separated by sex. (b) Joinpoint illustration of Duodenal ulcer related AAMRs per 1,000,000 individuals in the United States, from 1999 to 2020.
Trends by Race or Ethnicity
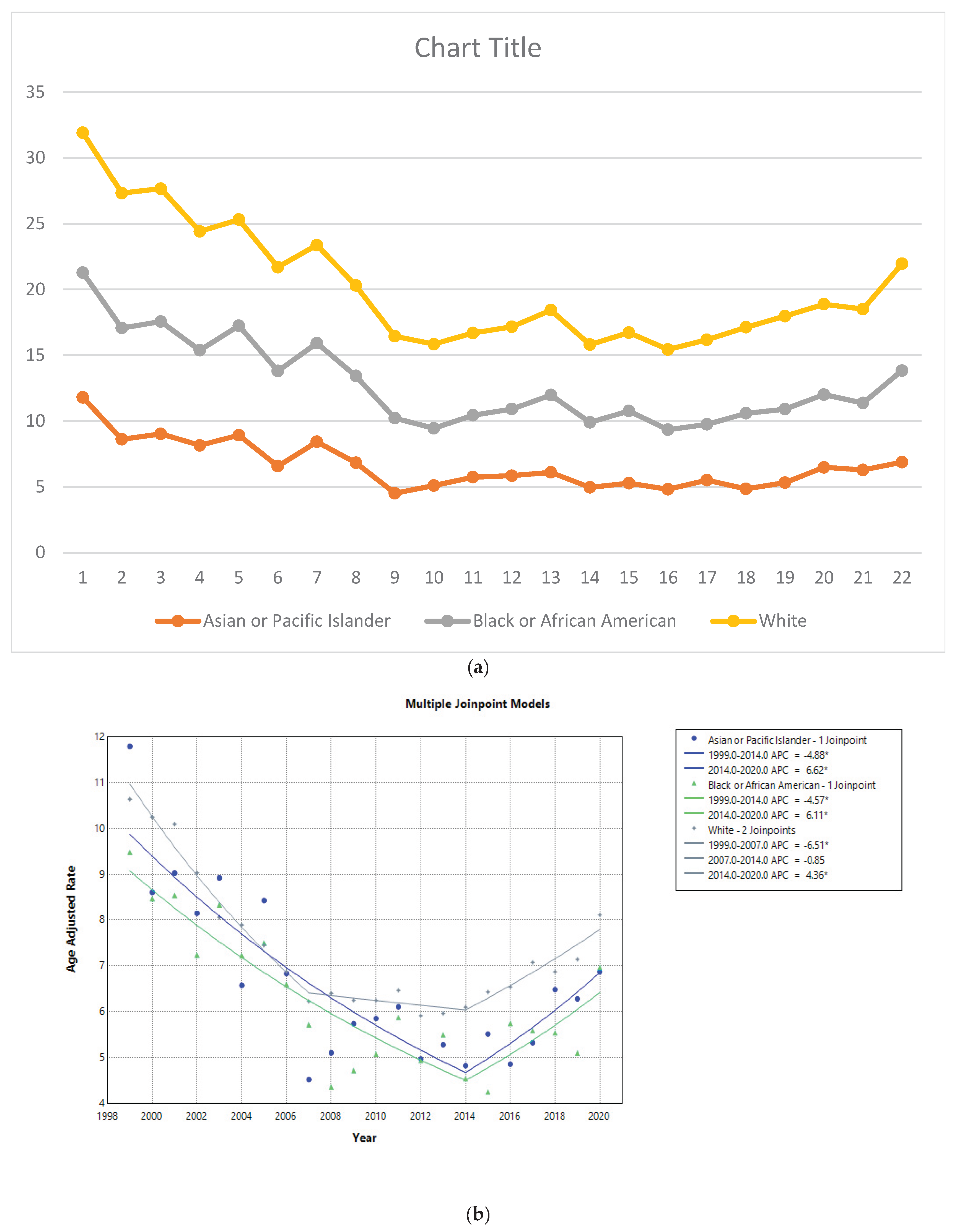
From 1999 to 2020, caucasian population exhibited the highest AAMR of 7.267 (95 % CI = 7.201 to 7.334), followed by Black or African American population with an AAMR of 6.083 (95% CI =5.899 to 6.266) and then an Asian or Pacific Islander population with an AAMR of 6.201 (95% CI = 5.901 to 6.502). The caucasian or white population showed the recurring trajectory – an initial steady decline in AAMR from 1999 to 2007 marked by an APC of -6.5088 (95% CI =-7.538 to -5.4681), a shallow decline till 2014 with an APC of -0.8536 (95% CI= -2.7248 to 1.0537), and an increase till 2020 with an APC of 4.3619 (95% CI = 2.6287 to 6.1244). Whereas the other two population groups showed almost the same trend; a decline from 1999-2014 with an APC of -4.8785(95% CI =-6.4563 to -3.274) in Asian or Pacific Islander group and -4.574*(95% CI= -6.0138 to -3.1121) for Black or African American group followed by an increase till 2020 with an APC of 6.6202* (95% CI = 1.3409 to 12.174) and 6.1135(95% CI = 0.2461 to 12.324) respectively. We applied the Cuzick test across race and found a z value of 1.87 (Prob > |z| = 0.062). We applied Kruskal-Wallis test across race as well and found a significant p value of 0.000.
Figure 2.
a: Age-adjusted mortality rates (AAMRs) for duodenal ulcer per 1,000,000 individuals in the United States, from 1999 to 2020, presented by race. b: Joinpoint illustrated model of duodenal ulcer related AAMRs per 1,000,000 individuals in the United States, from 1999 to 2020, categorized by race.
Figure 2.
a: Age-adjusted mortality rates (AAMRs) for duodenal ulcer per 1,000,000 individuals in the United States, from 1999 to 2020, presented by race. b: Joinpoint illustrated model of duodenal ulcer related AAMRs per 1,000,000 individuals in the United States, from 1999 to 2020, categorized by race.
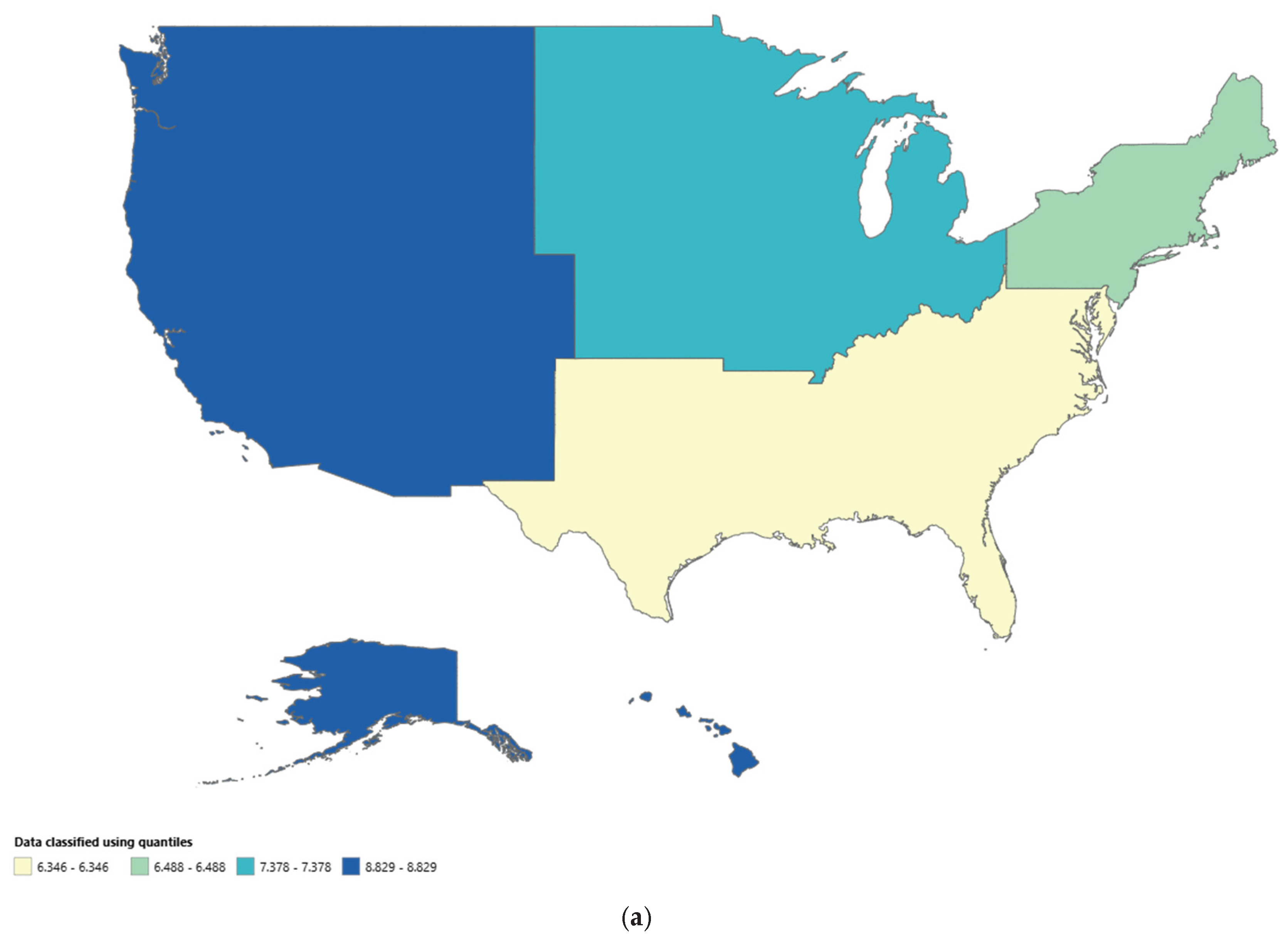
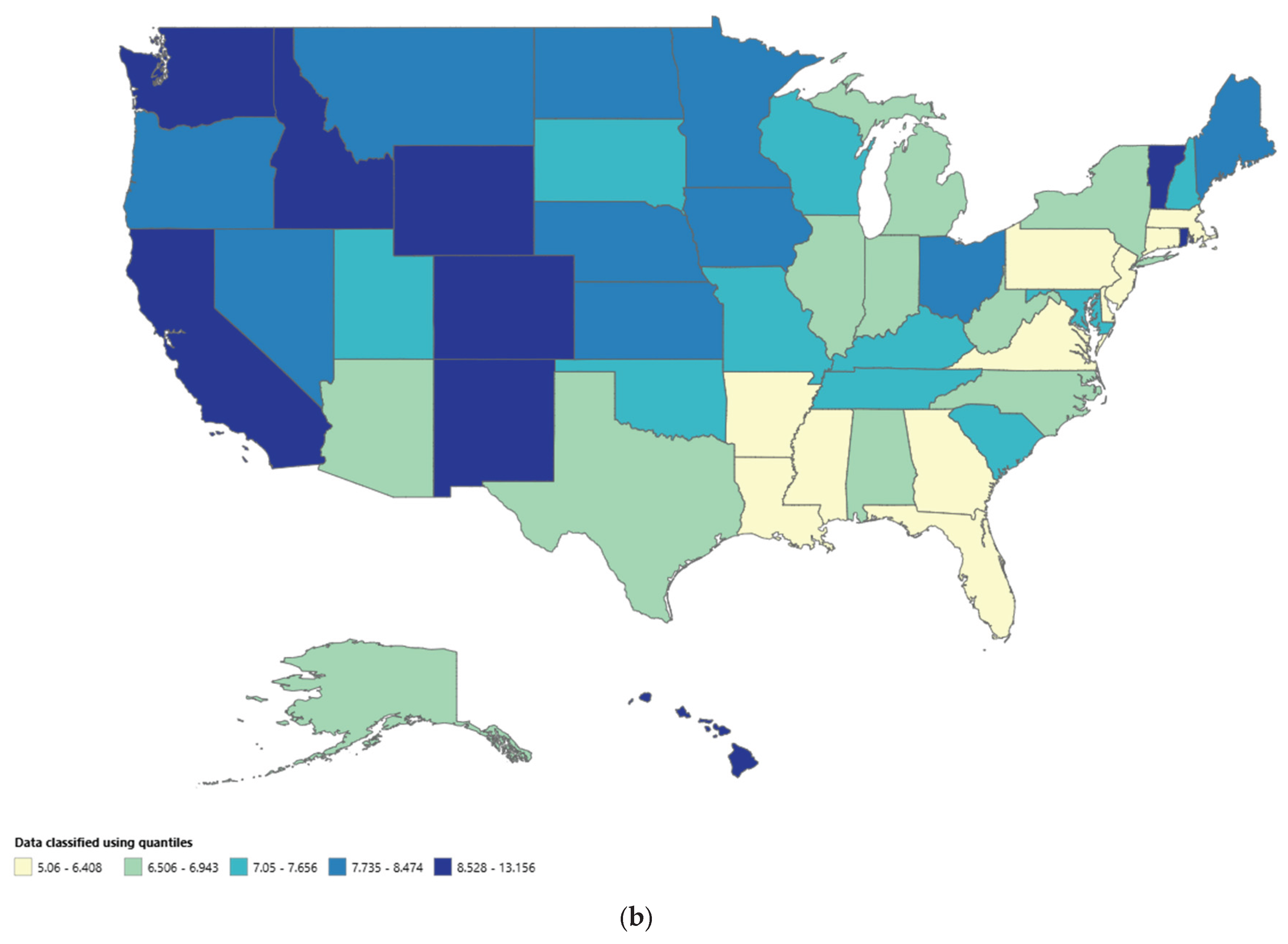
Trends by Place of Death, Region, and State
From 1999 to 2020, 76.2% of the deaths due to duodenal ulcer occurred in medical facilities-Inpatient, 6.7% in the Nursing / Long Term Care, 10.9% in Descendant’s home, 3.7% in medical facilities-Outpatient or ER, and 2.5% in other places. The West region displayed the highest AAMR of 8.829 (95% CI = 8.682 to 8.976), followed by the Midwest with an AAMR of 7.378(95% CI =7.246 to 7.509). The South and Northeast regions displayed almost the same AAMR with the AAMR of 6.346 (95% CI = 6.25 to 6.442) for South and for Northeast the AAMR was 6.488 (95% CI = 6.356 to 6.62). Differences in AAMRs were prominent across different states. The states with the highest AAMRs included California (AAMR 9.67; 95% CI = 8.64 to 10.69), Washington (AAMR = 9.54; 95% CI = 7.36 to 12.15), Colorado (AAMR = 8.82; 95% CI = 6.29 to 12.04),and Oregon (AAMR = 8.42; 95% CI = 5.93 to 11.63). These states showed rates that were approximately double the AAMRs of states on the lower end of the spectrum like Virginia (AAMR = 5.66; 95% CI = 4.12.56 to 7.59), New Jersey (AAMR =5.66; 95% CI = 4.28 to 7.34), Florida (AAMR = 5.816; 95% CI =4.87 to 6.76) and Georgia (AAMR = 5.901; 95% CI = 4.34 to 7.833).
Figure 3.
a: CDC-WONDER Heat map of AAMRs of duodenal ulcer stratified by Census Region. b: CDC-WONDER Heat map of AAMRs of duodenal ulcer stratified by States.
Figure 3.
a: CDC-WONDER Heat map of AAMRs of duodenal ulcer stratified by Census Region. b: CDC-WONDER Heat map of AAMRs of duodenal ulcer stratified by States.
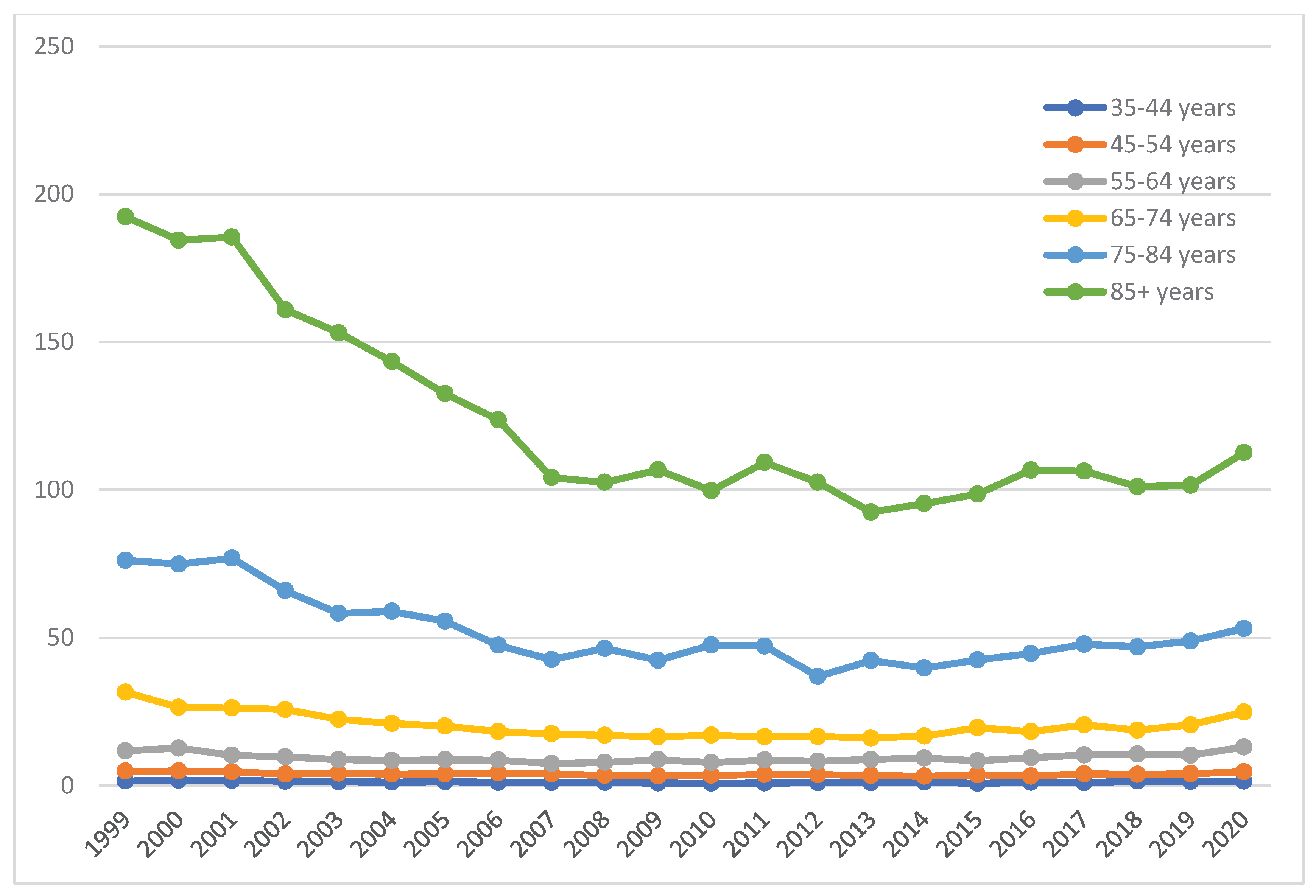
Trends by Age Groups
The most vulnerable population comprised individuals above 85+ years of age, with the highest CR of 119.425 (95% CI = 117.466 to 121.385). The CR exhibited by the age groups of 75 to 84 years and 65 to 74 years were 51.644 (95% CI = 50.829 to 52.459) and 20.223 (95% CI = 19.833 to 20.613) respectively. Next, a CR of 9.493 (95%CI = 9.275 to 9.712) by age group 55-64 years and a CR of 3.964 (95% CI = 3.836 to 4.092) by age group 45-54 years. The least CR of 1.298 (95%CI = 1.225 to 1.371) was exhibited by age group 35-44 years. Males had higher crude death rates as compared to females. We applied the Cuzick test across age groups and found a z value of 11.29 (Prob > |z| = 0.000). We applied Kruskal-Wallis test across Age groups as well and found a significant p value of 0.000.
Figure 4.
Duodenal Ulcer-Related Age-Adjusted Mortality Rates (AAMRs) per 1,000,000 Individuals, Stratified by age groups in the United States, 1999 to 2020.
Figure 4.
Duodenal Ulcer-Related Age-Adjusted Mortality Rates (AAMRs) per 1,000,000 Individuals, Stratified by age groups in the United States, 1999 to 2020.
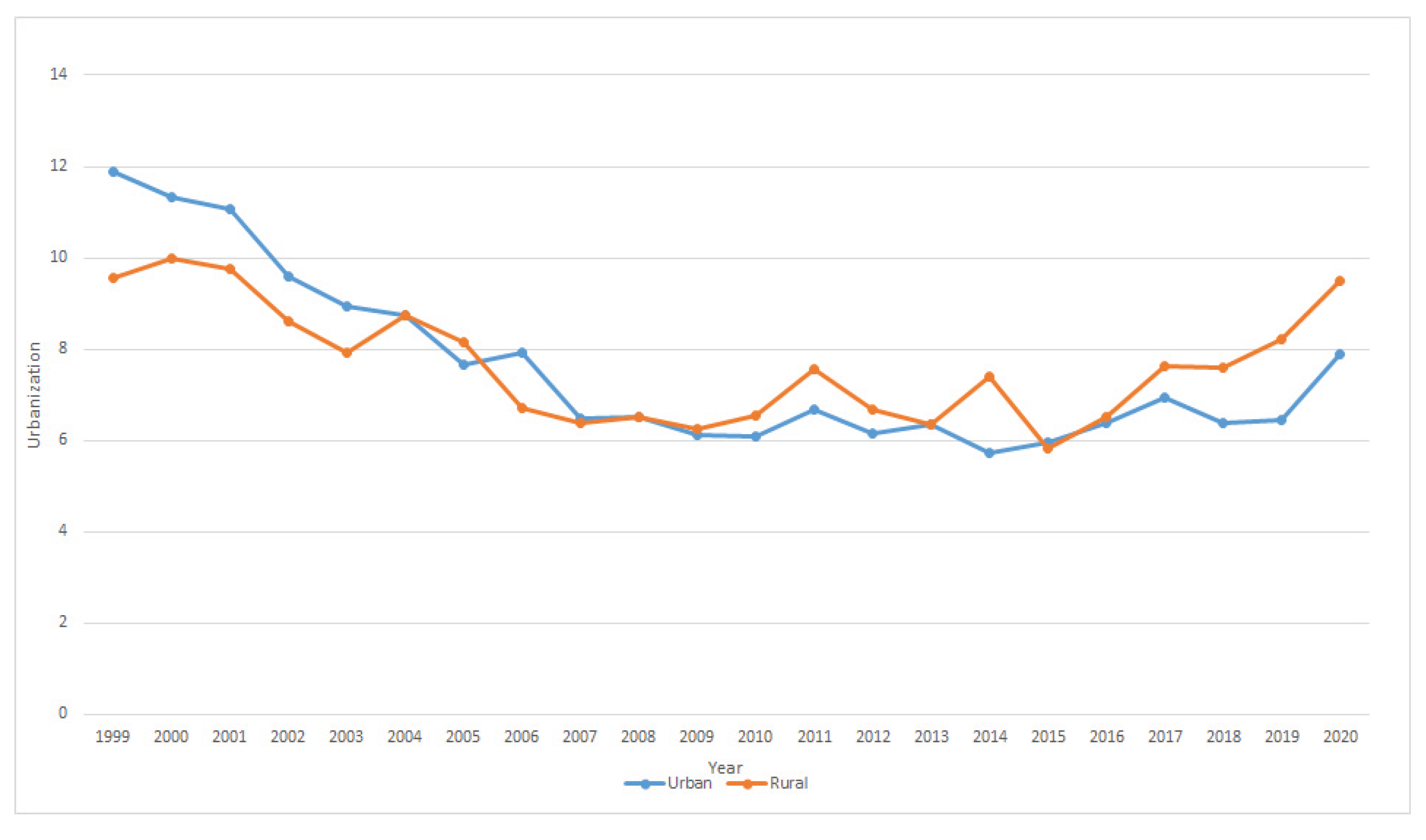
Trends by Urbanization
According to 2013 urbanization, a non-parallel trend (P=0.01) was observed in which the AAPC in the urban population was -2.63 (95%-CI: -3.49 to -1.76) while the AAPC in the rural population was -0.07 (95%-CI: -1.56 to -1.41). The Mann-Whitney U test gave the p-value of 0.014 while the Cuzick’s test gave a z-value of 1.41.
Figure 5.
Duodenal Ulcer-Related Age-Adjusted Mortality Rates (AAMRs) per 1,000,000 Individuals, Stratified by Urbanization in the United States, 1999 to 2020.
Figure 5.
Duodenal Ulcer-Related Age-Adjusted Mortality Rates (AAMRs) per 1,000,000 Individuals, Stratified by Urbanization in the United States, 1999 to 2020.
Table 1.
Demographic Characteristics of Deaths due to Infective Endocarditis Among the Geriatric in the USA from 1999 to 2020.
Table 1.
Demographic Characteristics of Deaths due to Infective Endocarditis Among the Geriatric in the USA from 1999 to 2020.
| Variable |
Duodenal Ulcer related Deaths (n) |
Age Adjusted Mortality Rate (AAMR) per 1,000,000 |
| Overall Population |
52674 |
7.158 |
| Sex |
|
|
Male
Female |
28974
23700 |
9.286
5.456 |
| US Census Region |
|
|
Northeast
Midwest
South
West |
9471
12281
16962
13960 |
6.488
7.378
6.346
8.829 |
| Race / Ethnicity |
|
|
Asian or Pacific Islander
Black or African American
White |
1701
4430
46267 |
6.201
6.083
7.267 |
| Age a |
|
|
35-44 years
45-54 years
55-64 years
65-74 years
75-84 years
85+ years |
1209
3677
7276
10323
15416
14273 |
1.298
3.964
9.493
20.223
51.644
119.425 |
| Place of Death b |
|
|
Medical facilities-Inpatient
Medical facility-Outpatient or ER
Decedent’s Home
Nursing / Long Term Care
Others |
38623
1868
5540
3413
1244 |
-
-
-
-
- |
| Urbanization |
|
|
Urban
Rural |
43683
9076 |
7.47
7.61 |
Table 2.
Annual Percentage Changes (APCs) and Average Annual Percentage Changes (AAPCs) in Infective Endocarditis Mortality Rate Among the Geriatrics in the USA from 1999 to 2020.
Table 2.
Annual Percentage Changes (APCs) and Average Annual Percentage Changes (AAPCs) in Infective Endocarditis Mortality Rate Among the Geriatrics in the USA from 1999 to 2020.
| Variable |
AAPC (95% CI) |
Trend segment |
Year |
APC (95% CI) |
| Overall Population |
-1.6895* |
1
2
3 |
1999-2007
2007-2014
2011-2020 |
-6.4723*
-1.1354
4.3836* |
| Sex |
|
|
|
|
| Female |
-1.7713* |
1
2
3 |
1999-2007
2007-2014
2014-2020 |
-6.1786*
-1.7412
4.3915* |
| Male |
1.8915* |
1
2
3 |
1999-2007
2007-2013
2013-2020 |
-6.8966*
-1.2762
-3.6024*
|
| US Census Region |
|
|
|
|
| Northeast |
-2.578* |
1
2 |
1999-2008
2008-2020 |
-6.6583*
0.5981 |
| Midwest |
-1.5386* |
1
2
|
1999-2012
2012-2020 |
-5.044*
4.4366* |
| South |
-1.4645* |
1
2
3 |
1999-2007
2007-2013
2013-2020 |
-5.924*
-1.515
3.9386* |
| West |
-1.5512* |
1
2
3 |
1999-2008
2008-2016
2016-2020
|
-6.754*
0.7309
6.259* |
| Race / Ethnicity |
|
|
|
|
| Asian or Pacific Islander |
-1.7259 |
1
2 |
1999-2014
2014-2020 |
-4.8785*
6.6202* |
| Black or African American |
-1.6535 |
1
2 |
1999-2014
2014-2020 |
-4.5740*
6.1135* |
| White |
-1.6166* |
1
2
3 |
1999-2007
2007-2014
2014-2020 |
-6.5088*
-0.8536
4.3619* |
| Urbanization |
|
|
|
|
Urban
Rural |
-2.63*
-0.07 |
1
2
1
2 |
1999-2009
2009-2015
1999-2015
2015-2020 |
-6.88*
1.40*
-2.80*
9.13* |
Discussion
Our analysis of mortality trends due to duodenal ulcer-related deaths in the United States based upon CDC WONDER database evidence from 1999 to 2020 revealed an overall decline in age-adjusted mortality rates (AAMRs) along with a decreasing trend for annual percentage change (APC) as well. This decline was particularly pronounced between 1999 and 2007, followed by a less steep decrease until 2014. However, from 2014 to 2020, we observed a slight increase in AAMR and APC values, though it did not exceed the initial rate. This finding is consistent with the decreasing trend seen for the same disease in previous studies as well [
13,
14]. Our study does a deep dive into different factors responsible for the duodenal ulcer-related deaths in the USA and also highlights the fact that previously it was believed conventionally that Black african-americans were the high-risk population, but statistically caucasian white population has higher mortality rates, as shown by our study.
When we analyzed the data specifically for gender, we found out that the AAMR for duodenal ulcer-related death was higher in men as compared to women which proves that gender differences are evident in the mortality trends. A previous study conducted by Xie et al. also found out that deaths for the mentioned disease were more in case of men than women [
15]. The analysis for trend of mortality showed that while both genders experienced a decline in mortality, the decrease was more substantial among males. This can be attributed to risk factors like tobacco smoking and alcohol abuse being more prevalent in men than in women [
16,
17] which increases the predisposition to not only acquiring a duodenal ulcer but also resulting in death. Significant disparities in mortality rates were observed across racial and ethnic groups. White population consistently had higher AAMRs compared to Black or African American and Asian or Pacific Islander individuals. The white although showed a peculiar trajectory with an initial decline up till 2007 then a lesser steeper decline till 2014 and then a slight increase in mortality up to 2020 while Black or African American and Asian or Pacific Islander showed an almost same trend; a decline until 2014 and then an increase until 2020. This racial disparity has been previously reported as well [
18,
19] which tells us that race has a significant correlation. The genetic variations in genes involved in inflammation and immune function, such as those in interleukin(IL)-1B and interleukin(IL)-RN families, have been linked to increased risk of duodenal ulcers. Furthermore, blood group O, smoking, alcohol, positive family history and stress also contribute positively to formation of ulcers.
Regional variations in mortality rates were also apparent. The West region consistently had higher AAMRs than the Midwest, South, and Northeast. Furthermore, substantial differences were observed among states within these regions with California, Washington, Colorado and Oregon existing on the upper end of spectrum while New Jersey, Virginia, Florida and Georgia on the lower end of the spectrum [
20,
21].
For the category of age, it was found that the highest mortality rates were concentrated among individuals aged 85 and older, followed by those aged 75-84. Mortality rates decreased progressively with younger age groups as also documented previously [
22]. This is attributed mainly to more complications in older age groups and a higher chance of perforation of the ulcer leading to death of the patient [
23].
The observed decline in duodenal cancer mortality is likely attributable to several factors, including advances in medical treatments, improved screening practices, and changes in lifestyle factors. However, the reasons for the recent uptick in mortality rates require further investigation [
24]. One of the attributing factors is the increased use of Direct Oral Anticoagulants (DOACs) in the latter half of 2010s; increasing tendency for ulcer to hemorrhage and thus increased mortality. Future studies should explore the underlying causes of these trends, identify factors contributing to disparities among different groups, and evaluate the effectiveness of current prevention and treatment strategies. Additionally, research on the impact of socioeconomic factors, environmental exposures, and genetic variations on duodenal cancer risk is warranted.
Conclusions
An overall decline was found out regarding the duodenal-ulcer related mortality rate with this effect being significant from 1990-2007, less steep till 2014 and a slight increase till 2020. It was further investigated that older people, male gender and white race are at a higher risk than people of younger age group, female gender and African- American or black and Asian or pacific islander. Regional distribution showed that the West region had a higher mortality rate. Better steps and measures should be taken to form policies and provide facilities to further decrease the mortality associated with duodenal ulcer.
Author Contributions
Conceptualization, B.S., M.K., M.H.,I.Q.,M.S.,M.A.; methodology, B.S.,L.M., A.K.; investigation, B.S., M.K., M.H.,I.Q.,M.S.,M.A.; resources, B.S., M.K., M.H.,I.Q.,M.S.,M.A.; data curation, B.S., L.M., A.K.; writing—original draft preparation, B.S..; writing—review and editing, B.S., L.M., A.K..; visualization, B.S..; supervision, L.M., All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding
References
- Malik TF, Gnanapandithan K, Singh K. Peptic Ulcer Disease. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 [cited 2024 Sep 11]. Available from: http://www.ncbi.nlm.nih.gov/books/NBK534792/.
- The relation between Helicobacter pylori and nonsteroidal anti-inflammatory drugs.
- Barkin, Jamie; The American Journal of Medicine, Volume 105, Issue 5, 22S - 27S.
- Sung, Joseph J Y MD, PhD, FRCP1; Tsoi, Kelvin K F PhD1; Ma, Terry K W MBChB1; Yung, Man-Yee BN1; Lau, James Y W MD, FRCS1; Chiu, Philip W Y MD, FRCS1. Causes of Mortality in Patients With Peptic Ulcer Bleeding: A Prospective Cohort Study of 10,428 Cases. American Journal of Gastroenterology 105(1):p 84-89, January 2010. |. [CrossRef]
- Odat, R.M., Idrees, M., Marsool, M.D.M. et al. Stomach and duodenal ulcer as a cause of death in patients with cancer: a cohort study. Int J Emerg Med 17, 199 (2024). [CrossRef]
- Cave DR. Transmission and epidemiology of Helicobacter pylori. Am J Med. 1996 May 20;100(5A):12S-17S; discussion 17S-18S.
- Peptic ulcer disease Almadi, Majid A et al. The Lancet, Volume 404, Issue 10447, 68 - 81.
- Groenen MJ, Kuipers EJ, Hansen BE, Ouwendijk RJT. Incidence of duodenal ulcers and gastric ulcers in a Western population: Back to where it started. Can J Gastroenterol. 2009 Sep;23(9):604–8.
- Sun J, Huang L, Li R, Wang T, Wang S, Yu C, et al. Comparison of Secular Trends in Peptic Ulcer Diseases Mortality in China, Brazil and India during 1990–2019: An Age-Period-Cohort Analysis. Healthcare. 2023 Apr 11;11(8):1085.
- Centers for Disease Control and Prevention. National Center for Health Statistics. Multiple Cause of Death 1999-2019 on CDC WONDER Online Database, Released in 2020. Data are from the Multiple Cause of Death Files, 1999-2019, as Compiled from Data Provided by the 57 Vital Statistics Jurisdictions through the Vital Statistics Cooperative Program; 2021. Accessed May 21 http://wonder.cdc.gov/mcd-icd10.html.
- Von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008 Apr;61(4):344–9.
- Joinpoint Regression Program, Version 5.0.2 - May 2023; Statistical Methodology and Applications Branch, Surveillance Research Program, National Cancer Institute.
- Kim HJ, Fay MP, Feuer EJ, Midthune DN. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med. 2000;19(3):335–351. Available from: https://onlinelibrary.wiley.com/.
- Elashoff JD, Grossman MI. Trends in hospital admissions and death rates for peptic ulcer in the United States from 1970 to 1978. Gastroenterology. 1980 Feb;78(2):280–5.
- Feinstein LB, Holman RC, Christensen KLY, Steiner CA, Swerdlow DL. Trends in Hospitalizations for Peptic Ulcer Disease, United States, 1998–2005. Emerg Infect Dis. 2010 Sep;16(9):1410–8.
- Xie X, Ren K, Zhou Z, Dang C, Zhang H. The global, regional and national burden of peptic ulcer disease from 1990 to 2019: a population-based study. BMC Gastroenterol. 2022 Feb 10;22(1):58.
- Garrow D, Delegge MH. Risk Factors for Gastrointestinal Ulcer Disease in the US Population. Dig Dis Sci. 2010 Jan 1;55(1):66–72.
- Idris M, Smiley A, Patel S, Latifi R. Risk Factors for Mortality in Emergently Admitted Patients with Acute Gastric Ulcer: An Analysis of 15,538 Patients in National Inpatient Sample, 2005–2014. Int J Environ Res Public Health. 2022 Dec 5;19(23):16263.
- Bazargan-Hejazi S, Ambriz M, Ullah S, Khan S, Bangash M, Dehghan K, et al. Trends and racial disparity in primary pressure ulcer hospitalizations outcomes in the US from 2005 to 2014. Medicine (Baltimore). 2023 Oct 6;102(40):e35307.
- Jennings D. PERFORATED PEPTIC ULCER: CHANGES IN AGE-INCIDENCE AND SEX-DISTRIBUTION IN THE LAST 150 YEARS. The Lancet. 1940 Mar 9;235(6080):444–7.
- Kurata JH, Elashoff JD, Haile BM, Honda GD. A reappraisal of time trends in ulcer disease: factors related to changes in ulcer hospitalization and mortality rates. Am J Public Health. 1983 Sep;73(9):1066–72.
- Everhart JE, Kruszon-Moran D, Perez-Perez GI, Tralka TS, McQuillan G. Seroprevalence and ethnic differences in Helicobacter pylori infection among adults in the United States. J Infect Dis. 2000 Apr;181(4):1359–63.
- Susser M, Stein Z. Civilization and peptic ulcer*. Int J Epidemiol. 2002 Feb 1;31(1):13–7.
- Higham J, Kang JY, Majeed A. Recent trends in admissions and mortality due to peptic ulcer in England: increasing frequency of haemorrhage among older subjects. Gut. 2002 Apr;50(4):460–4.
- Havens JM, Castillo-Angeles M, Nitzschke SL, Salim A. Disparities in peptic ulcer disease: A nationwide study. Am J Surg. 2018 Dec 1;216(6):1127–8.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).