1. Introduction
Traumatic brain injury (TBI) is one of the leading causes of death and disability worldwide, particularly among young and middle-aged adults [
1]. Every year, over 50 million individuals suffer from TBI globally, resulting in severe reductions in quality of life and imposing significant economic burdens on families and society [
2,
3]. Depending on the severity of the injury, TBI can be classified as mild, moderate, or severe, with varying outcomes for each classification. Understanding the molecular events associated with secondary brain injuries across different severities of TBI is critical for advancing precise treatments [
4].
TBI involves both primary and secondary injury phases. Primary injuries are caused by the immediate mechanical forces exerted on the brain, leading to structural damage that occurs instantaneously and is often irreversible. Secondary injuries, however, result from subsequent biochemical changes and are the primary focus of therapeutic interventions. Previous studies have identified multiple pathways for neuronal death following TBI, including necrosis, apoptosis, pyroptosis, and autophagy dysfunction [
5]. Researchers have extensively studied these processes to identify potential therapeutic targets, but clinical interventions targeting these mechanisms have yielded unsatisfactory results.
Ferroptosis, a novel form of programmed cell death that differs from traditional apoptotic mechanisms, was first reported in 2012 by Dixon et al [
6]. It is characterized by the accumulation of lipid reactive oxygen species (ROS) and excessive iron deposition. Subsequent research has demonstrated that the ferroptotic pathway is activated following TBI, contributing to neuronal cell death [
7]. Initial findings of ferroptosis in central nervous system were observed in tumor models, and later studies confirmed its occurrence in models of stroke and spinal cord injury [
8,
9]. However, the relationship between ferroptosis and the degree of neuronal injury following TBI, especially in models of varying injury severity, remains unclear [
10]. Therefore, this study aims to establish a rat model of TBI with different severities (mild, mild-moderate, and severe) to investigate the correlation between cortical ferroptosis and neurological impairment, thereby providing a theoretical basis for ferroptosis research in neurotrauma [
11].
2. Materials and Methods
The Materials and Methods should be described with sufficient details to allow others to replicate and build on the published results. Please note that the publication of your manuscript implicates that you must make all materials, data, computer code, and protocols associated with the publication available to readers. Please disclose at the submission stage any restrictions on the availability of materials or information. New methods and protocols should be described in detail while well-established methods can be briefly described and appropriately cited.
2.1. Experimental Animals
Specific pathogen-free (SPF) grade healthy adult male Sprague-Dawley (SD) rats, weighing between 250 and 300 grams, were used in the experiments. The rats were housed in a standard environment with a controlled temperature of 20-25°C, humidity levels of 40%-55%, and a 12-hour light/dark cycle for one week prior to the experiment. Food and water were provided ad libitum. Twelve hours before surgery, the rats were fasted but allowed access to water. The experimental protocol was approved by the Ethics Committee of Kunming Medical University (Approval number: kmmu20220651), and all efforts were made to minimize the suffering of the experimental animals during the study.
2.2. TBI Animal Model
The TBI model was established using the Feeney free-fall impact method. Rats were anesthetized with an intraperitoneal injection of 3% pentobarbital sodium (30-40 mg/kg). Once anesthetized, the rats’ scalps were shaved and disinfected. The rats were then secured on a stereotaxic frame, and a midline incision of approximately 3 cm was made on the scalp to expose the skull. A dental drill was used to create a 6 mm diameter bone window 2 mm posterior to the coronal suture and 2.5 mm lateral to the sagittal suture on the right side of the skull, ensuring the dura mater remained intact.
For the sham group, only the bone window was drilled without applying any impact. For the TBI groups, a 40-gram weight was dropped vertically onto the exposed dura mater from different heights: 15 cm for the mild TBI group (mTBI), 20 cm for the mild-moderate TBI group (mmTBI), and 25 cm for the severe TBI group (sTBI). This impact resulted in contusion and laceration of the brain tissue. After the injury was induced, hemostasis was ensured, and the scalp was closed with interrupted sutures. Post-surgery, the rats were placed in an incubator to recover from anesthesia before being returned to their cages. Standard postoperative care included routine wound disinfection and antibiotic administration to prevent infection.
Twenty-four hours post-injury, the modified Neurological Severity Score (mNSS) was used to assess the neurological function of the rats. The mNSS evaluates sensorimotor function through five tests: tail suspension, motor function, sensory function, beam balance, and reflexes/abnormal movements. Scores range from 0 (normal) to 18, with higher scores indicating greater neurological impairment. Scores of 1-6 reflect mild injury, 7-12 moderate injury, and scores above 13 indicate severe injury.
2.3. Experimental Groups
The rats were randomly divided into four groups (n=9):
Neurological function was assessed using the mNSS test 24 hours after TBI induction, and rats that met the injury criteria were included in the subsequent experiments.
2.4. Magnetic Resonance Imaging (MRI)
Seven days after inducing TBI, the rats underwent MRI scanning to assess brain tissue injury. The MRI scanner used was a Philips Ingenia 3.0T from the Netherlands. Scanning parameters were as follows:
Coronal T2-weighted imaging (T2WI): Resolution 0.3 × 0.33 × 2 mm, Repetition Time (TR) 2000 ms, Echo Time (TE) 80 ms.
Coronal T2* imaging (T2*WI): Resolution 0.53 × 0.53 × 2 mm, TR 510 ms, TE 16 ms, Flip Angle 18°.
2.5. Prussian Blue Staining
Prussian blue staining was used to detect non-heme iron deposition in the cortical tissue of the rats. Paraffin-embedded tissue sections (3-5 µm thick) were deparaffinized and rehydrated through the following series: xylene I for 20 min, xylene II for 20 min, absolute ethanol I for 5 min, absolute ethanol II for 5 min, and 75% ethanol for 5 min. Sections were rinsed in tap water and washed with distilled water three times. The sections were then stained for 1 hour in a freshly prepared Prussian blue staining solution, which was a mixture of potassium ferrocyanide and hydrochloric acid. After washing twice with distilled water, the sections were counterstained with hematoxylin for 1-5 minutes and rinsed in running water. Finally, the sections were dehydrated through graded ethanol and cleared in xylene before mounting with neutral gum. Iron deposition appears as brown granules, while nuclei stain light blue.
2.6. Transmission Electron Microscopy (TEM)
Seven days post-TBI, the rats were sacrificed, and the brain tissues surrounding the injury site were harvested. The cortex was trimmed into 1 mm³ tissue blocks and preserved in electron microscope fixative. Transmission electron microscopy was outsourced to Wuhan Servicebio Technology Co., Ltd.
2.7. Western Blot Analysis
Western blot analysis was used to assess the expression of ferroptosis-related proteins. The proteins were quantified using the bicinchoninic acid (BCA) method, and 10% SDS-PAGE was used for protein separation. The proteins were transferred to PVDF membranes at 100 V for 1 hour. After transfer, the membranes were washed twice with TBST for 5 minutes each and then blocked with 5% skimmed milk for 2 hours at room temperature with gentle shaking. After blocking, the membranes were washed again with TBST for 5 minutes and then incubated overnight at 4°C with the following primary antibodies diluted in 0.1% TBST: FTH1 (1:1000) and GPX4 (1:1000). The next day, the membranes were washed three times with TBST for 15 minutes each and incubated with a secondary antibody (goat anti-rabbit, 1:5000) for 2 hours at room temperature. After incubation, the membranes were washed three times with TBST, followed by chemiluminescent detection using the Amersham Imager 600 system. Densitometric analysis was performed using ImageJ software.
2.8. MDA (Malondialdehyde) Content Measurement
Lipid peroxidation was assessed by measuring malondialdehyde (MDA) levels using an MDA assay kit (Suzhou Keming, MDA-1-Y). The brain tissue was homogenized in ice-cold extraction buffer at a ratio of 1:5–10 (g tissue: mL buffer). The homogenate was centrifuged at 8000 rpm for 10 minutes at 4°C, and the supernatant was collected. MDA levels were measured at 532 nm and 600 nm using a spectrophotometer, and the MDA concentration was calculated using a standard curve.
2.9. Statistical Analysis
Each experiment was repeated at least three times. Data were expressed as mean ± standard error of the mean (SEM). Pearson correlation analysis was used to analyze the correlation between two groups, and one-way ANOVA was used for comparisons among multiple groups. A p-value of <0.05 was considered statistically significant. Graphs were generated using GraphPad Prism 8.4.3 software.
3. Results
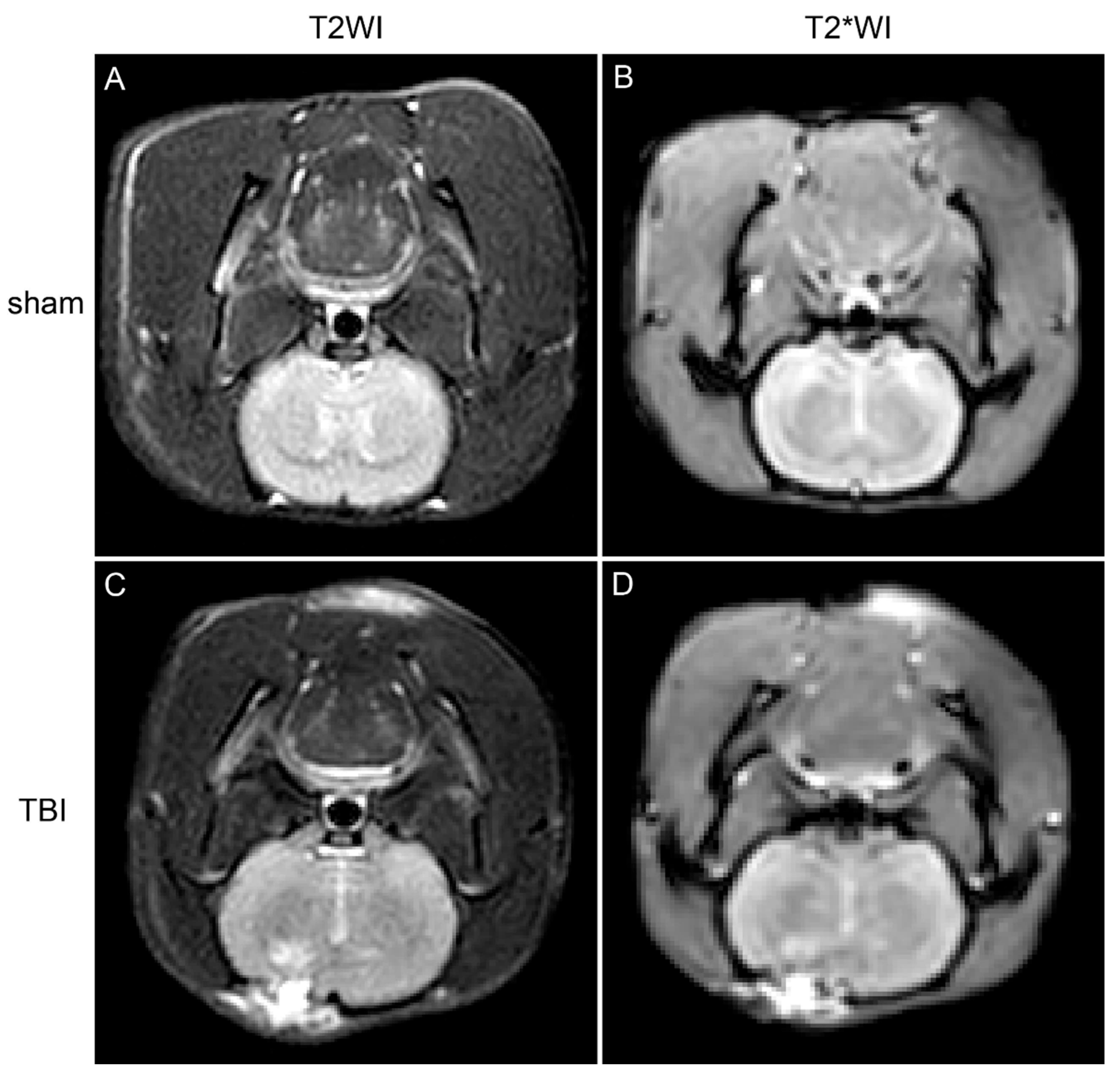
3.1. MRI Shows Iron Deposition in the Brain Tissue Surrounding the Injury Site in TBI Rats
Seven days after TBI induction, magnetic resonance imaging (MRI) was performed on the rats. Compared with the sham group, the brain tissue in the injury region of the TBI groups showed high signal intensity on T2-weighted imaging (T2WI) sequences, indicating brain injury, edema, and hemorrhage (
Figure 1). Additionally, low signal intensity was observed on T2*WI sequences around the injury area, suggesting possible iron deposition in the brain tissue (
Figure 1).
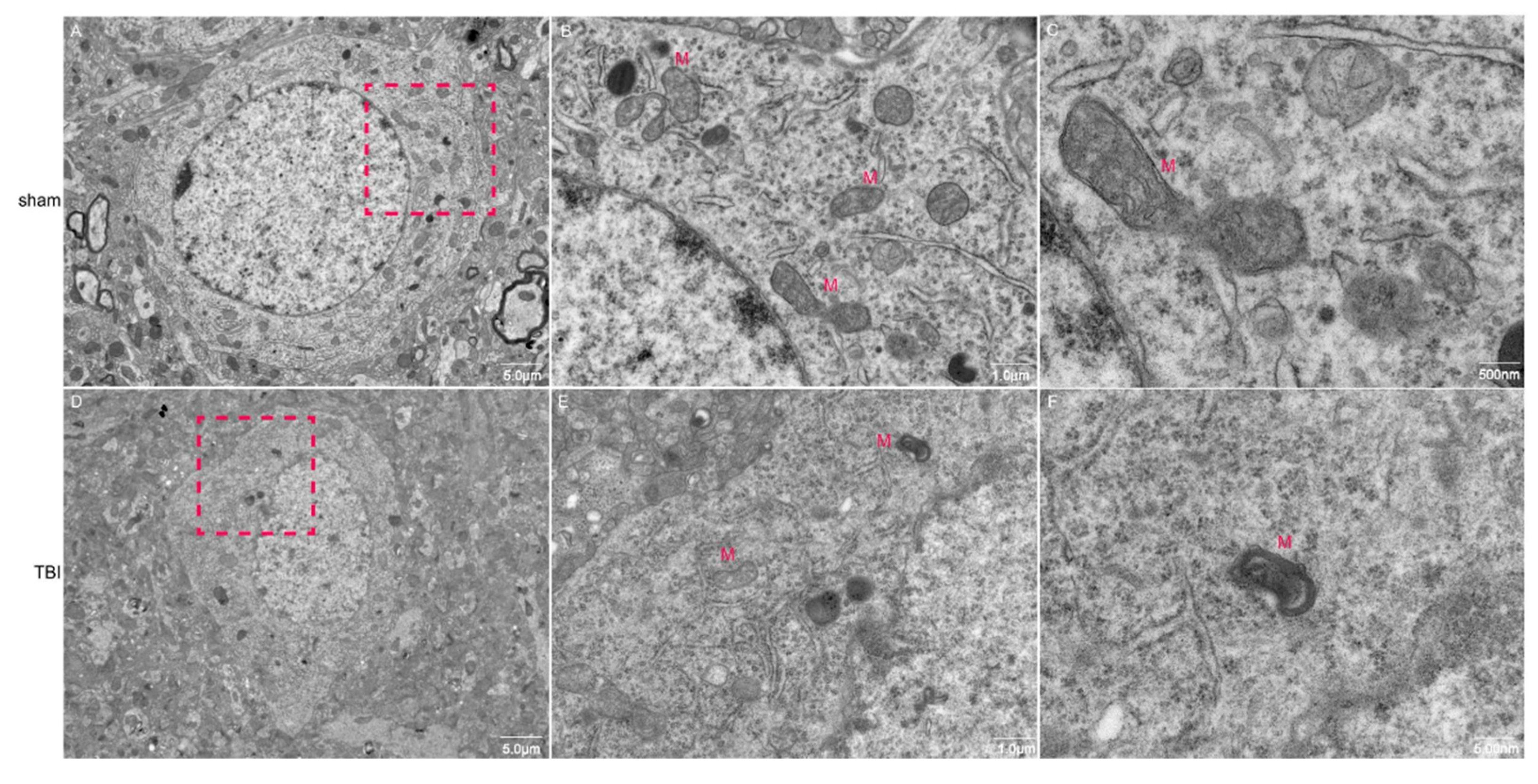
3.2. TEM Shows Evidence of Ferroptosis in Neurons of TBI Rats
Transmission electron microscopy (TEM) was used to observe neuronal mitochondria morphology. The results showed that in the sham group, neurons exhibited normal morphology with intact mitochondrial membranes and normal cristae structure. However, in the TBI group, neurons exhibited significant morphological changes, including mitochondrial atrophy, deepened matrix color, thickened membranes, and some outer membrane rupture accompanied by expansion and reduction of internal cristae (
Figure 2). These findings suggest that ferroptosis occurred in the neurons of the TBI group.
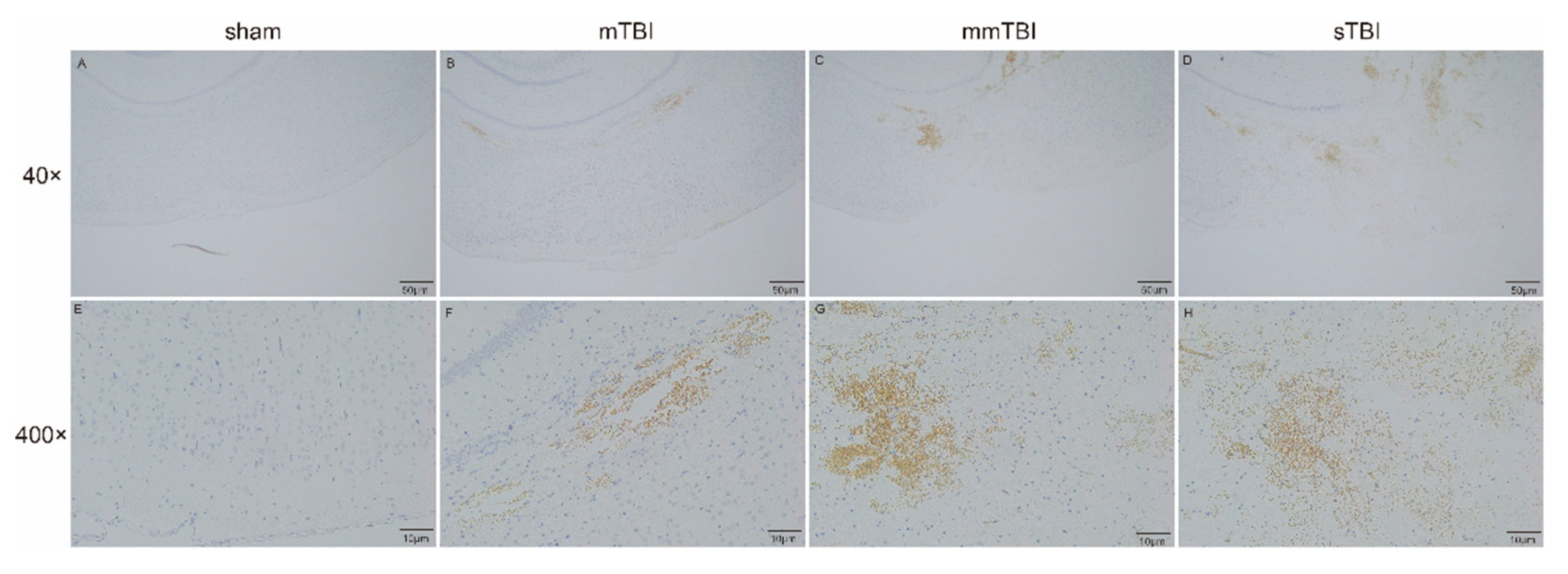
3.3. Prussian Blue Staining Shows Iron Deposition in the Cortex of TBI Rats
Prussian blue staining was used to detect non-heme iron deposition in the cortical tissue surrounding the injury sites in TBI rats. In the sham group, no iron deposition was observed. In the mTBI group, mild iron deposition (brown regions) was observed in the cortex around the injury site. In the mmTBI and sTBI groups, progressively higher levels of iron deposition were observed, with the sTBI group exhibiting the most significant iron accumulation (
Figure 3).
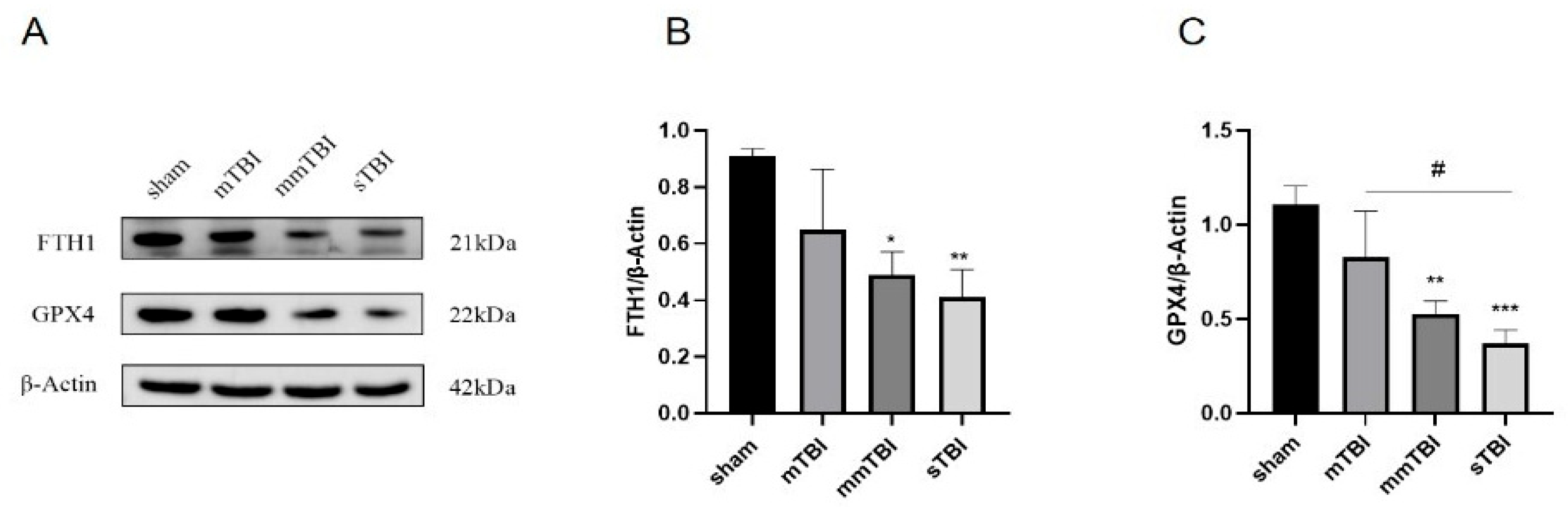
3.4. Decreased Expression of Ferroptosis Negative Regulators in the Cortex Corresponds to Increased Neurological Damage
Twenty-four hours post-TBI induction, the expression levels of ferroptosis negative regulators FTH1 and GPX4 in the cortical tissue surrounding the injury area were assessed by Western blot. Compared to the sham group, the expression levels of FTH1 and GPX4 showed a decreasing trend in the mTBI group, though the differences were not statistically significant. However, in the mmTBI and sTBI groups, the expression levels of FTH1 and GPX4 were significantly reduced compared to the sham group (P < 0.05). Additionally, GPX4 expression in the sTBI group was significantly lower than in the mTBI group (P < 0.05) (
Figure 4).
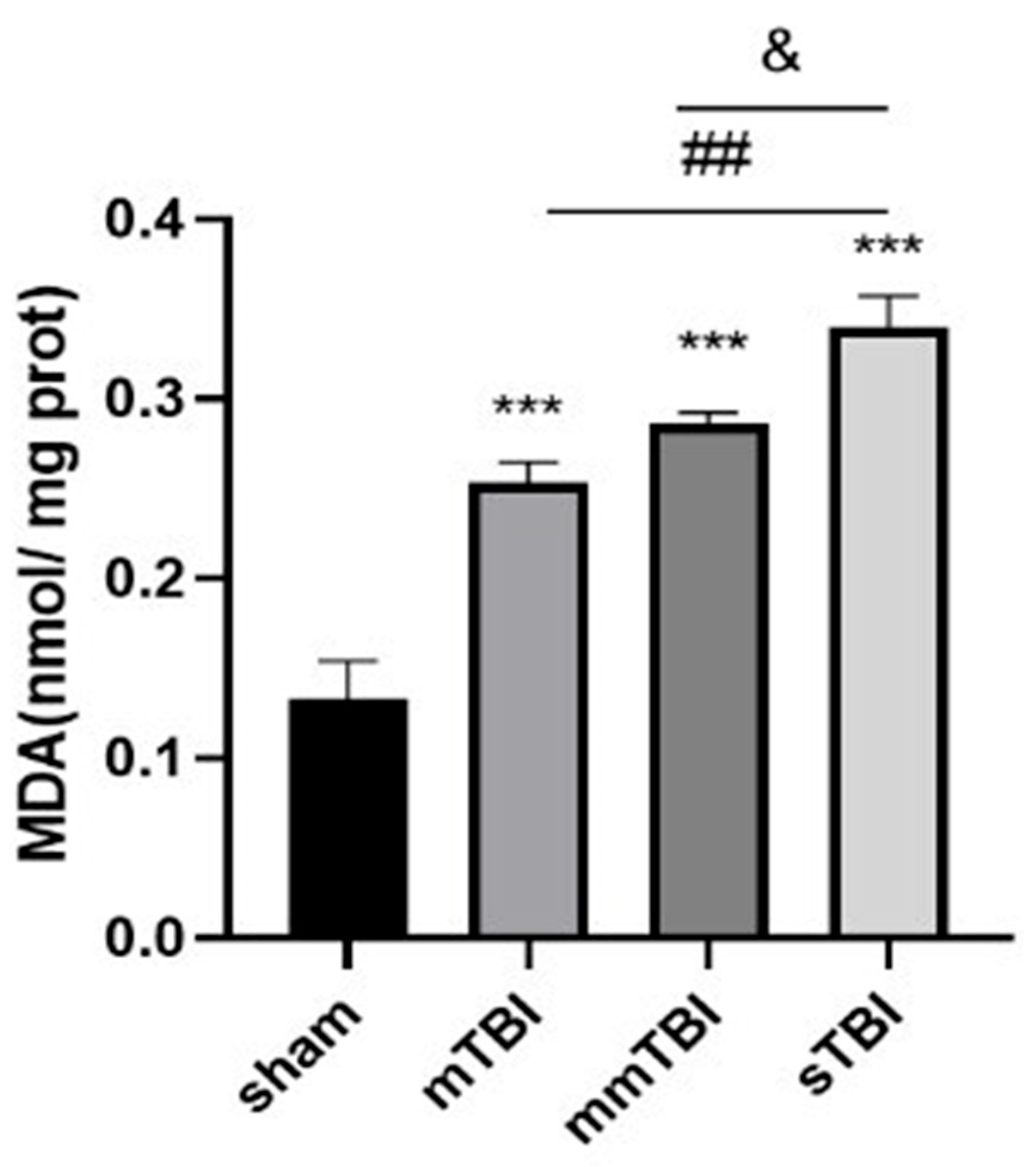
3.5. Increased Lipid Peroxidation in the Cortex Corresponds to Greater Neurological Damage
Twenty-four hours post-TBI, malondialdehyde (MDA), a marker of lipid peroxidation and oxidative stress, was measured in the cortical tissue surrounding the injury site. Compared with the sham group, MDA levels were significantly elevated in the mTBI, mmTBI, and sTBI groups (P < 0.001). There was a trend toward increased MDA levels in the mmTBI group compared to the mTBI group, and MDA levels were significantly higher in the sTBI group compared to both the mmTBI and mTBI groups (P < 0.05) (
Table 1,
Figure 5).
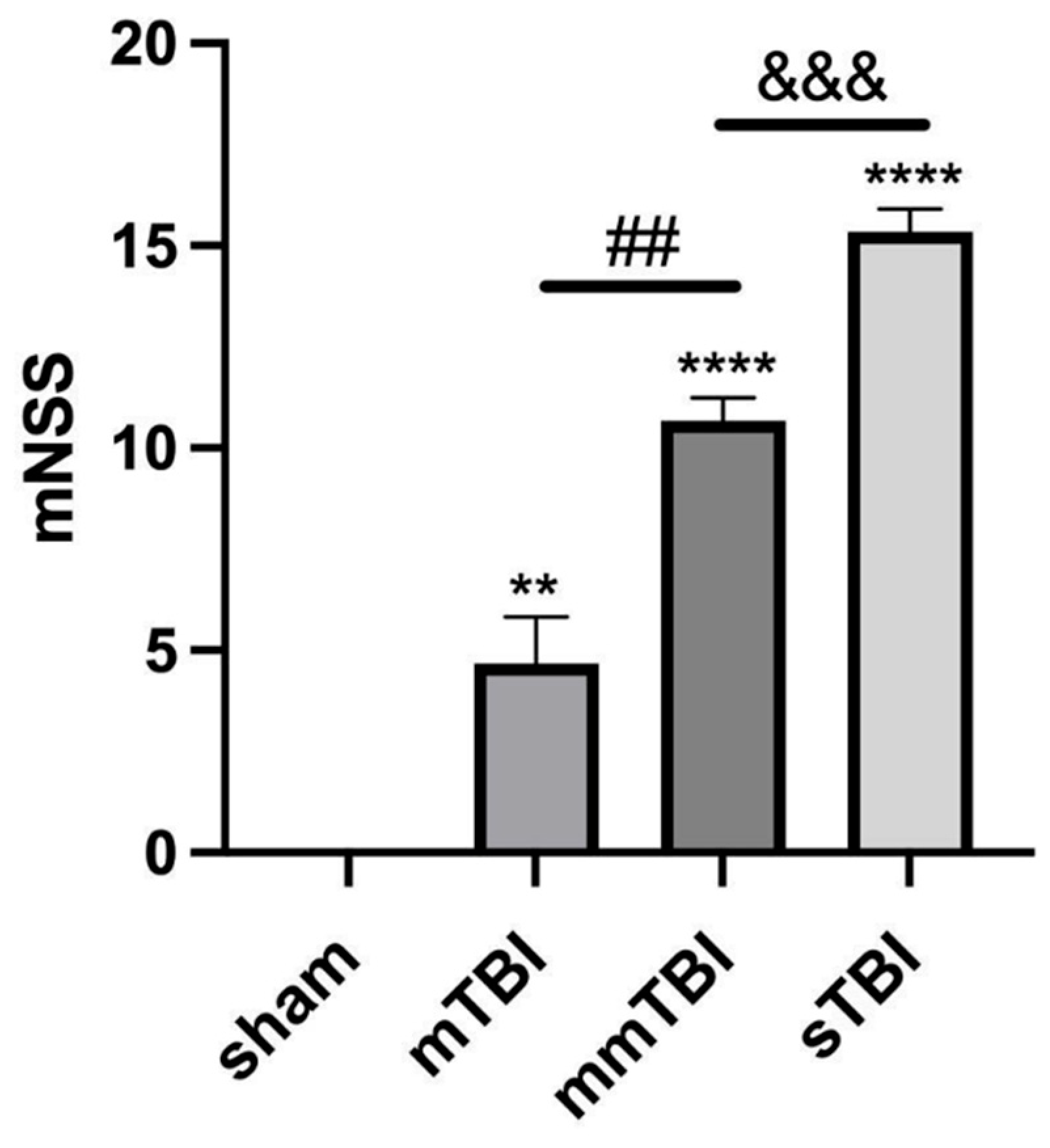
3.6. Increased mNSS Scores Correlate with Increased Ferroptosis and Oxidative Stress
Twenty-four hours post-TBI, neurological function was assessed using the mNSS scale. The mNSS scores, indicating neurological impairment, were significantly higher in the mTBI, mmTBI, and sTBI groups compared to the sham group (P < 0.001) (
Table 2,
Figure 6).
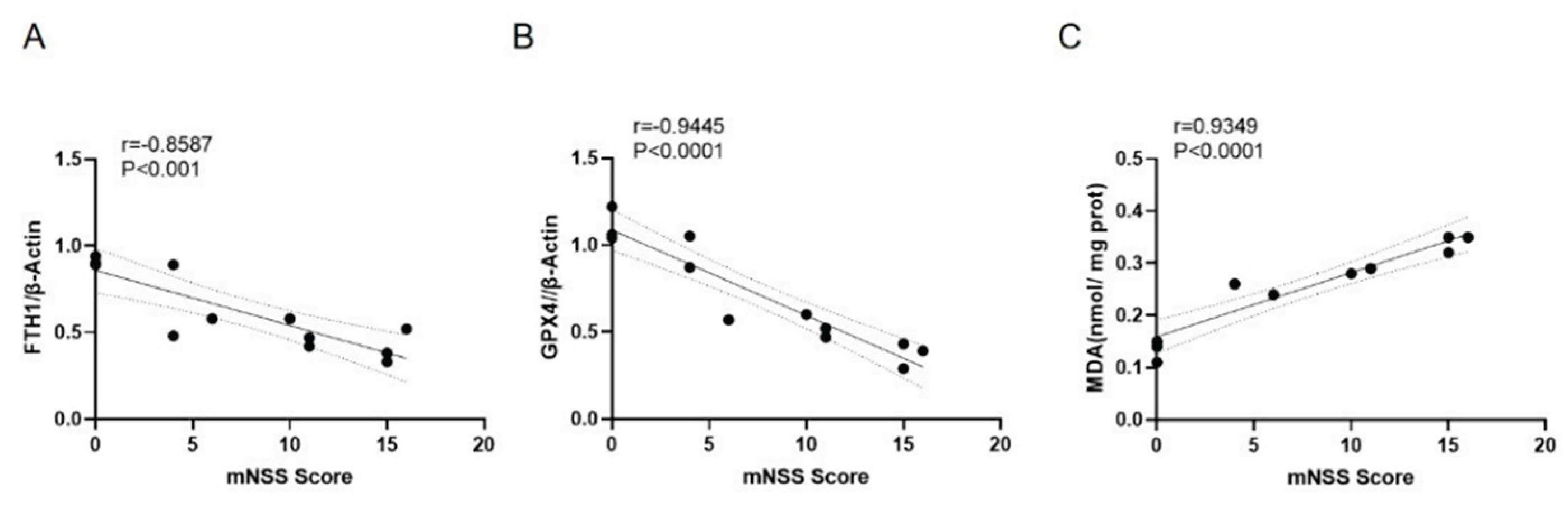
Correlation analysis showed a significant negative correlation between mNSS scores and the relative expression levels of the ferroptosis negative regulators FTH1 and GPX4 (r = -0.8587 and -0.9445, P < 0.001), and a significant positive correlation between mNSS scores and MDA content (r = 0.9349, P < 0.0001) (
Figure 7).
4. Discussion
Traumatic brain injury (TBI) is a leading cause of death and disability worldwide, particularly in young adults, imposing significant economic and societal burdens. The primary causes of TBI include traffic accidents, falls from heights, violent assaults, and slip-and-fall accidents. TBI can be categorized into primary and secondary injuries based on the timing and nature of the damage. Primary injury results from external mechanical forces that cause immediate and irreversible damage to brain structures, such as disruption of the blood-brain barrier, axonal injury, and neuronal death. Current clinical treatments for TBI primarily focus on decompressive craniectomy and hypothermia therapy; however, these treatments only address immediate concerns and fail to significantly reduce mortality and disability rates.
Secondary injury refers to a series of biochemical changes that occur following primary injury, leading to further tissue damage. Traditionally, it was believed that secondary injury involved mechanisms such as excitotoxicity from the release of glutamate, oxidative stress from the accumulation of reactive oxygen species (ROS), inflammatory cascades triggered by cytokines and chemokines, vasogenic and cytotoxic edema resulting in brain swelling, blood-brain barrier disruption, and mitochondrial dysfunction leading to abnormal energy metabolism [
12]. These mechanisms have been extensively studied to identify potential therapeutic targets. However, clinical treatments targeting these pathways have shown limited success in preventing the progression of TBI.
Ferroptosis, a newly discovered form of regulated cell death, was first reported in 2012 by Dixon et al. It is a type of programmed, non-apoptotic cell death characterized by the accumulation of lipid reactive oxygen species (ROS) and iron deposition. Research has shown that the ferroptosis pathway is activated following TBI and contributes to neuronal cell death. In 2017, ferroptosis was first observed in central nervous system tumor models, and it has since been reported in animal models of stroke and spinal cord injury. Ferroptosis is distinct from other forms of cell death, such as apoptosis, necrosis, and autophagy, in that it cannot be inhibited by traditional inhibitors of these pathways but can be suppressed by antioxidants and iron chelators [
13].
In this study, we aimed to investigate the role of ferroptosis in TBI and its correlation with the severity of neurological impairment. Using a rat model of TBI, we induced brain injuries of varying severity and assessed iron deposition, ferroptosis markers, and neurological function. The results demonstrated that iron deposition and ferroptosis occurred in the cortical tissue of TBI rats and were associated with the degree of neuronal damage. Our findings support the hypothesis that ferroptosis plays a critical role in secondary injury following TBI and that its severity is directly correlated with the extent of neurological impairment [
14].
Iron is an essential trace element involved in many physiological and biochemical processes, including oxygen transport, DNA synthesis, and energy metabolism [
15]. However, excess iron accumulation is a key factor in triggering ferroptosis [
16]. Normally, extracellular iron ions bind to transferrin receptors and are internalized by cells through clathrin-mediated endocytosis. Within endosomes, iron is reduced to ferrous ions (Fe²⁺) and transported into the cytosol, where it is stored in the labile iron pool or sequestered in ferritin complexes. Under normal conditions, iron homeostasis is tightly regulated to prevent oxidative damage. However, in conditions such as TBI, disrupted cellular metabolism and hypoxia can lead to excessive accumulation of ferrous ions, which catalyze the Fenton reaction, generating highly reactive hydroxyl radicals. These radicals initiate lipid peroxidation, damaging cell membranes and eventually causing cell death.
Our MRI results showed that TBI-induced brain tissue damage and iron deposition were evident seven days after injury. This was further supported by transmission electron microscopy (TEM), which revealed mitochondrial atrophy, membrane thickening, and rupture in neurons, characteristic features of ferroptosis. Prussian blue staining also confirmed that iron accumulation increased with the severity of brain injury. These results indicate that ferroptosis plays a significant role in TBI-related neuronal damage and that iron deposition is closely linked to the extent of injury.
Lipid peroxidation is a hallmark of ferroptosis, characterized by the accumulation of lipid ROS and malondialdehyde (MDA), a byproduct of lipid peroxidation [
17]. In this study, we found that MDA levels were significantly elevated in the cortical tissue of TBI rats, and the severity of TBI was positively correlated with MDA levels. This suggests that oxidative stress and lipid peroxidation are key contributors to ferroptosis in TBI.
Ferroptosis is regulated by key proteins, including ferritin heavy chain 1 (FTH1) and glutathione peroxidase 4 (GPX4). FTH1 plays a critical role in iron storage and detoxification by sequestering excess iron, thereby preventing iron-mediated oxidative damage. GPX4 is an essential enzyme that protects cells from lipid peroxidation by reducing lipid hydroperoxides to non-toxic lipid alcohols [
18]. In our study, the expression levels of FTH1 and GPX4 were significantly reduced in the brain tissue of TBI rats, particularly in the groups with more severe injuries. This reduction in FTH1 and GPX4 expression suggests that the protective mechanisms against ferroptosis are compromised in TBI, leading to increased oxidative stress and neuronal death.
The modified Neurological Severity Score (mNSS) was used to assess the degree of neurological impairment in TBI rats. The mNSS scores were significantly higher in rats with more severe injuries, indicating greater neurological dysfunction. Correlation analysis revealed a significant negative correlation between mNSS scores and the expression levels of FTH1 and GPX4, and a positive correlation between mNSS scores and MDA levels. These findings further support the hypothesis that ferroptosis contributes to neurological deficits following TBI and that the severity of ferroptosis is closely associated with the degree of brain injury [
19].
5. Conclusions
In conclusion, this study demonstrates that ferroptosis plays a crucial role in secondary brain injury following TBI. Iron deposition, lipid peroxidation, and the downregulation of ferroptosis inhibitors FTH1 and GPX4 are all closely associated with the extent of neuronal damage and neurological impairment. Targeting ferroptosis may represent a novel therapeutic approach for reducing neuronal death and improving outcomes in TBI patients. Further research is needed to explore potential interventions that can modulate ferroptosis and mitigate its effects on brain injury.
Author Contributions
LY: conceived and designed the experiments, Writing review and editing. JL: Conceptualization, Methodology, Investigation, Writing – original draft, Writing – review & editing. YY and HZ: Investigation, Methodology, and Validation. XZ and QZ: Conceptualization, Methodology, Investigation. CQ and HW: Investigation. QD: Conceptualization, Writing – review & editing, Supervision. All authors have read and approved the final manuscript.
Funding
This research was funded by the National Natural Science Foundation of China (82260384); Science and Technology Plan Project of Yunnan Science and Technology Department (202301AU070164); Doctoral Research Fund Project of the First Affiliated Hospital of Kunming Medical University (2022BS026); Scientific Research Fund Project of Yunnan Provincial Department of Education (2023Y0597).
Data Availability Statement
We encourage all authors of articles published in MDPI journals to share their research data. In this section, please provide details regarding where data supporting reported results can be found, including links to publicly archived datasets analyzed or generated during the study. Where no new data were created, or where data is unavailable due to privacy or ethical restrictions, a statement is still required. Suggested Data Availability Statements are available in section “MDPI Research Data Policies” at
https://www.mdpi.com/ethics.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Reddi, S.; Thakker-Varia, S.; Alder, J.; Giarratana, A.O. Status of precision medicine approaches to traumatic brain injury. Neural Regen Res 2022, 17, 2166–2171. [Google Scholar] [CrossRef]
- Martinez, B.; Peplow, P.V. Biomaterial and tissue-engineering strategies for the treatment of brain neurodegeneration. Neural Regen Res 2022, 17, 2108–2116. [Google Scholar] [CrossRef]
- Scarboro, M.; McQuillan, K.A. Traumatic Brain Injury Update. AACN Adv Crit Care 2021, 32, 29–50. [Google Scholar] [CrossRef] [PubMed]
- Muhammad, S.A.; Abbas, A.Y.; Imam, M.U.; Saidu, Y.; Bilbis, L.S. Efficacy of stem cell secretome in the treatment of traumatic brain injury: A systematic review and meta-analysis of preclinical studies. Mol Neurobiol 2022, 59, 2894–2909. [Google Scholar] [CrossRef]
- Zhou, C.; Zheng, J.; Fan, Y.; Wu, J. TI: NLRP3 Inflammasome-Dependent Pyroptosis in CNS Trauma: A Potential Therapeutic Target. Front Cell Dev Biol 2022, 10, 821225. [Google Scholar] [CrossRef] [PubMed]
- Dixon, S.J.; Lemberg, K.M.; Lamprecht, M.R.; Skouta, R.; Zaitsev, E.M.; Gleason, C.E.; Patel, D.N.; Bauer, A.J.; Cantley, A.M.; Yang, W.S.; et al. Ferroptosis: an iron-dependent form of nonapoptotic cell death. Cell 2012, 149, 1060–1072. [Google Scholar] [CrossRef]
- Chen, D.; Fan, Z.; Rauh, M.; Buchfelder, M.; Eyupoglu, I.Y.; Savaskan, N. ATF4 promotes angiogenesis and neuronal cell death and confers ferroptosis in a xCT-dependent manner. Oncogene 2017, 36, 5593–5608. [Google Scholar] [CrossRef]
- Alim, I.; Caulfield, J.T.; Chen, Y.; Swarup, V.; Geschwind, D.H.; Ivanova, E.; Seravalli, J.; Ai, Y.; Sansing, L.H.; Ste Marie, E.J.; et al. Selenium Drives a Transcriptional Adaptive Program to Block Ferroptosis and Treat Stroke. Cell 2019, 177, 1262–1279.e1225. [Google Scholar] [CrossRef] [PubMed]
- Kenny, E.M.; Fidan, E.; Yang, Q.; Anthonymuthu, T.S.; New, L.A.; Meyer, E.A.; Wang, H.; Kochanek, P.M.; Dixon, C.E.; Kagan, V.E.; et al. Ferroptosis Contributes to Neuronal Death and Functional Outcome After Traumatic Brain Injury. Crit Care Med 2019, 47, 410–418. [Google Scholar] [CrossRef]
- Xie, B.S.; Wang, Y.Q.; Lin, Y.; Mao, Q.; Feng, J.F.; Gao, G.Y.; Jiang, J.Y. Inhibition of ferroptosis attenuates tissue damage and improves long-term outcomes after traumatic brain injury in mice. CNS Neurosci Ther 2019, 25, 465–475. [Google Scholar] [CrossRef]
- Roth, T.L.; Nayak, D.; Atanasijevic, T.; Koretsky, A.P.; Latour, L.L.; McGavern, D.B. Transcranial amelioration of inflammation and cell death after brain injury. Nature 2014, 505, 223–228. [Google Scholar] [CrossRef] [PubMed]
- Sulhan, S.; Lyon, K.A.; Shapiro, L.A.; Huang, J.H. Neuroinflammation and blood-brain barrier disruption following traumatic brain injury: Pathophysiology and potential therapeutic targets. J Neurosci Res 2020, 98, 19–28. [Google Scholar] [CrossRef] [PubMed]
- Yan, H.F.; Zou, T.; Tuo, Q.Z.; Xu, S.; Li, H.; Belaidi, A.A.; Lei, P. Ferroptosis: mechanisms and links with diseases. Signal Transduct Target Ther 2021, 6, 49. [Google Scholar] [CrossRef]
- Geeraerts, T.; Velly, L.; Abdennour, L.; Asehnoune, K.; Audibert, G.; Bouzat, P.; Bruder, N.; Carrillon, R.; Cottenceau, V.; Cotton, F.; et al. Management of severe traumatic brain injury (first 24hours). Anaesth Crit Care Pain Med 2018, 37, 171–186. [Google Scholar] [CrossRef] [PubMed]
- Yang, W.S.; Stockwell, B.R. Synthetic lethal screening identifies compounds activating iron-dependent, nonapoptotic cell death in oncogenic-RAS-harboring cancer cells. Chem Biol 2008, 15, 234–245. [Google Scholar] [CrossRef] [PubMed]
- Gao, M.; Monian, P.; Quadri, N.; Ramasamy, R.; Jiang, X. Glutaminolysis and Transferrin Regulate Ferroptosis. Mol Cell 2015, 59, 298–308. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Cao, F.; Yin, H.L.; Huang, Z.J.; Lin, Z.T.; Mao, N.; Sun, B.; Wang, G. Ferroptosis: past, present and future. Cell Death Dis 2020, 11, 88. [Google Scholar] [CrossRef] [PubMed]
- Liang, D.; Feng, Y.; Zandkarimi, F.; Wang, H.; Zhang, Z.; Kim, J.; Cai, Y.; Gu, W.; Stockwell, B.R.; Jiang, X. Ferroptosis surveillance independent of GPX4 and differentially regulated by sex hormones. Cell 2023, 186, 2748–2764.e2722. [Google Scholar] [CrossRef] [PubMed]
- Awasthi, D.; Church, D.F.; Torbati, D.; Carey, M.E.; Pryor, W.A. Oxidative stress following traumatic brain injury in rats. Surg Neurol 1997, 47, 575-581; discussion 581-572. [Google Scholar] [CrossRef] [PubMed]
Figure 1.
Coronal MRI scans of rat brain tissue, with images A and B representing the sham group (T2WI and T2WI sequences), and images C and D representing the TBI group (T2WI and T2WI sequences).
Figure 1.
Coronal MRI scans of rat brain tissue, with images A and B representing the sham group (T2WI and T2WI sequences), and images C and D representing the TBI group (T2WI and T2WI sequences).
Figure 2.
Transmission electron microscopy images of neurons. Images A-C represent sham group neurons, and images D-F represent neurons from the TBI group. The scale bars in A, D are 5.0 μm; in B, E, 5.0 μm; in C, F, 500 nm.
Figure 2.
Transmission electron microscopy images of neurons. Images A-C represent sham group neurons, and images D-F represent neurons from the TBI group. The scale bars in A, D are 5.0 μm; in B, E, 5.0 μm; in C, F, 500 nm.
Figure 3.
Prussian blue staining images showing iron deposition in the cortical tissue surrounding the injury area. Images A, E represent the sham group, B, F the mTBI group, C, G the mmTBI group, and D, H the sTBI group. The scale bars in A-D are 50 μm, and in E-H are 10 μm.
Figure 3.
Prussian blue staining images showing iron deposition in the cortical tissue surrounding the injury area. Images A, E represent the sham group, B, F the mTBI group, C, G the mmTBI group, and D, H the sTBI group. The scale bars in A-D are 50 μm, and in E-H are 10 μm.
Figure 4.
Western blot analysis of ferroptosis negative regulators FTH1 and GPX4 in the cortex of TBI rats. A: Immunoblot showing protein levels; B, C: Relative quantification of FTH1 and GPX4 protein expression. *P < 0.05 vs. sham, **P < 0.01 vs. sham, #P < 0.05 vs. mTBI.
Figure 4.
Western blot analysis of ferroptosis negative regulators FTH1 and GPX4 in the cortex of TBI rats. A: Immunoblot showing protein levels; B, C: Relative quantification of FTH1 and GPX4 protein expression. *P < 0.05 vs. sham, **P < 0.01 vs. sham, #P < 0.05 vs. mTBI.
Figure 5.
MDA levels in the cortical tissue of TBI rats. ***P < 0.001 vs. sham, ##P < 0.01 vs. mTBI, &P < 0.05 vs. mmTBI.
Figure 5.
MDA levels in the cortical tissue of TBI rats. ***P < 0.001 vs. sham, ##P < 0.01 vs. mTBI, &P < 0.05 vs. mmTBI.
Figure 6.
mNSS scores in TBI rats. **P < 0.01 vs. sham, ****P < 0.0001 vs. sham, ##P < 0.01 vs. mTBI, &&&P < 0.001 vs. mmTBI.
Figure 6.
mNSS scores in TBI rats. **P < 0.01 vs. sham, ****P < 0.0001 vs. sham, ##P < 0.01 vs. mTBI, &&&P < 0.001 vs. mmTBI.
Figure 7.
Correlation between mNSS scores and the relative expression levels of ferroptosis markers in the cortex of TBI rats. A: Correlation between mNSS score and FTH1 protein expression; B: Correlation between mNSS score and GPX4 protein expression; C: Correlation between mNSS score and MDA levels.
Figure 7.
Correlation between mNSS scores and the relative expression levels of ferroptosis markers in the cortex of TBI rats. A: Correlation between mNSS score and FTH1 protein expression; B: Correlation between mNSS score and GPX4 protein expression; C: Correlation between mNSS score and MDA levels.
Table 1.
Changes in malondialdehyde (MDA) levels in cortical tissue (nmol/mg prot).
Table 1.
Changes in malondialdehyde (MDA) levels in cortical tissue (nmol/mg prot).
| Group |
MDA (nmol/mg prot) |
| sham |
0.13±0.02 |
| mTBI |
0.25±0.01 |
| mmTBI |
0.29±0.01 |
| sTBI |
0.34±0.02 |
Table 2.
Modified Neurological Severity Scores (mNSS).
Table 2.
Modified Neurological Severity Scores (mNSS).
| Group |
mNSS |
| sham |
0.00±0.00 |
| mTBI |
4.67±1.15 |
| mmTBI |
10.67±0.58 |
| sTBI |
15.33±0.58 |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).