Introduction
Cardiovascular diseases (CVD), particularly coronary artery disease (CAD), is a leading cause of morbidity and mortality worldwide. In Germany, CVD accounts for 40% of all deaths [1] with approximately 7.3% attributable to CAD [
1]. Given these statistics, the improvement of coronary diagnostic modalities has been a continuous focus. While invasive coronary angiography (ICA) has traditionally served as the reference standard for diagnosing CAD, advancements in imaging techniques, particularly coronary computed tomography angiography (CTCA), have demonstrated promising results in terms of safety, and cost-effectiveness.
Clinical trials such as PROMISE [
2], Scot-Heart [
3], and DISCHARGE [
4] have validated the efficacy of CTCA, establishing it as a reliable non-invasive imaging modality for patients with a low to intermediate pre-test probability of CAD. In 2019, the European Society of Cardiology (ESC) updated its guidelines [
5] for stable CAD, recommending CTCA as the preferred imaging tool for patients with chronic CAD.
Despite this, CTCA has not yet been routinely adopted as the primary non-invasive diagnostic modality for patients with stable angina in Germany. Since January 2024, public health insurance companies in Germany have allowed CTCA as a routine diagnostic modality for patients pre-diagnosed with CAD who have intermediate Pretest Probability (PTP) [
6] . However, referring cardiologists still usually recommend an ICA to these patients.
Our study aims to evaluate the safety and reliability of coronary CT angiography as a routine diagnostic modality for patients with low or intermediate risk of coronary artery disease, comparing it to the reference method, invasive coronary angiography (ICA) in a real-life-setting.
Results
Study Population
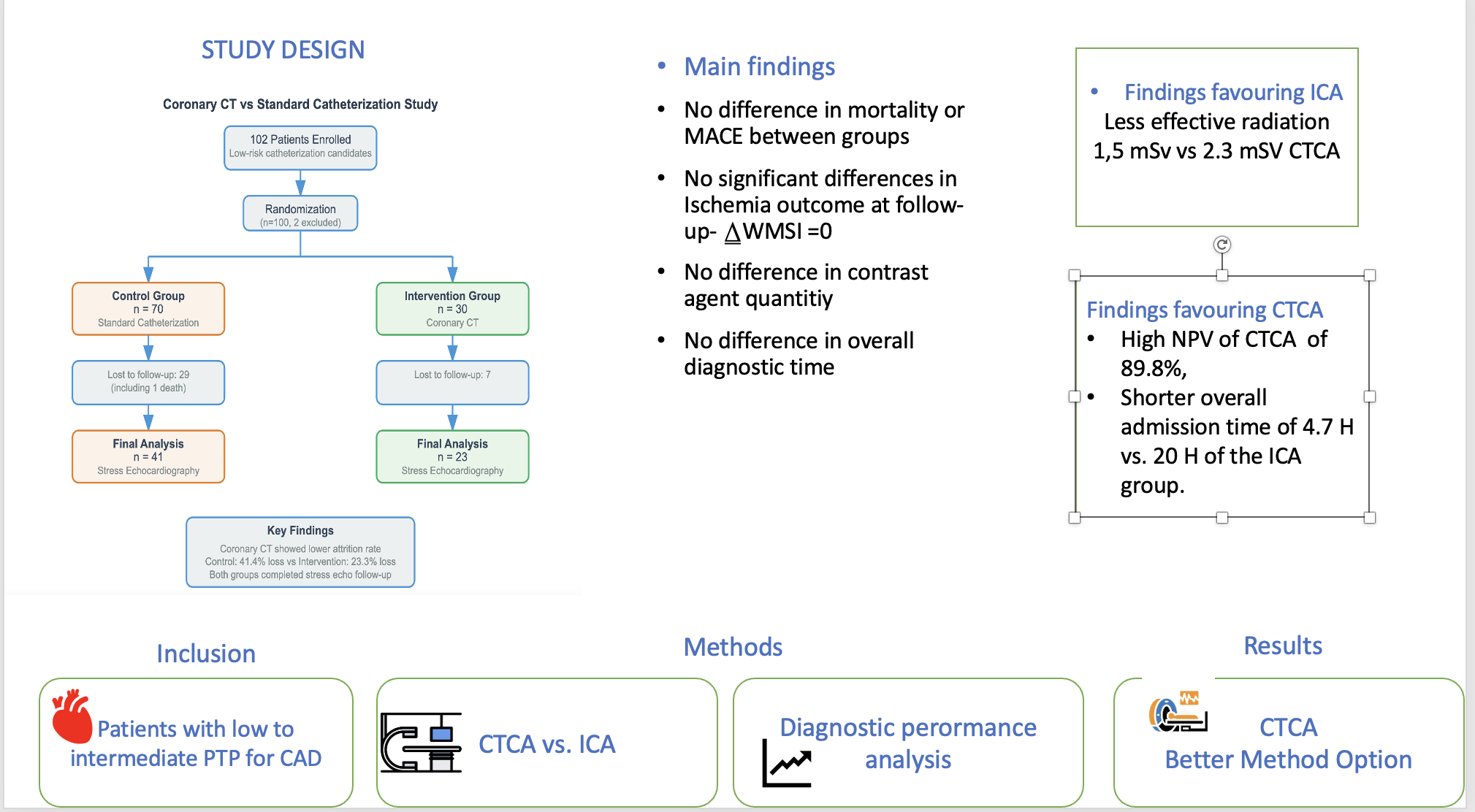
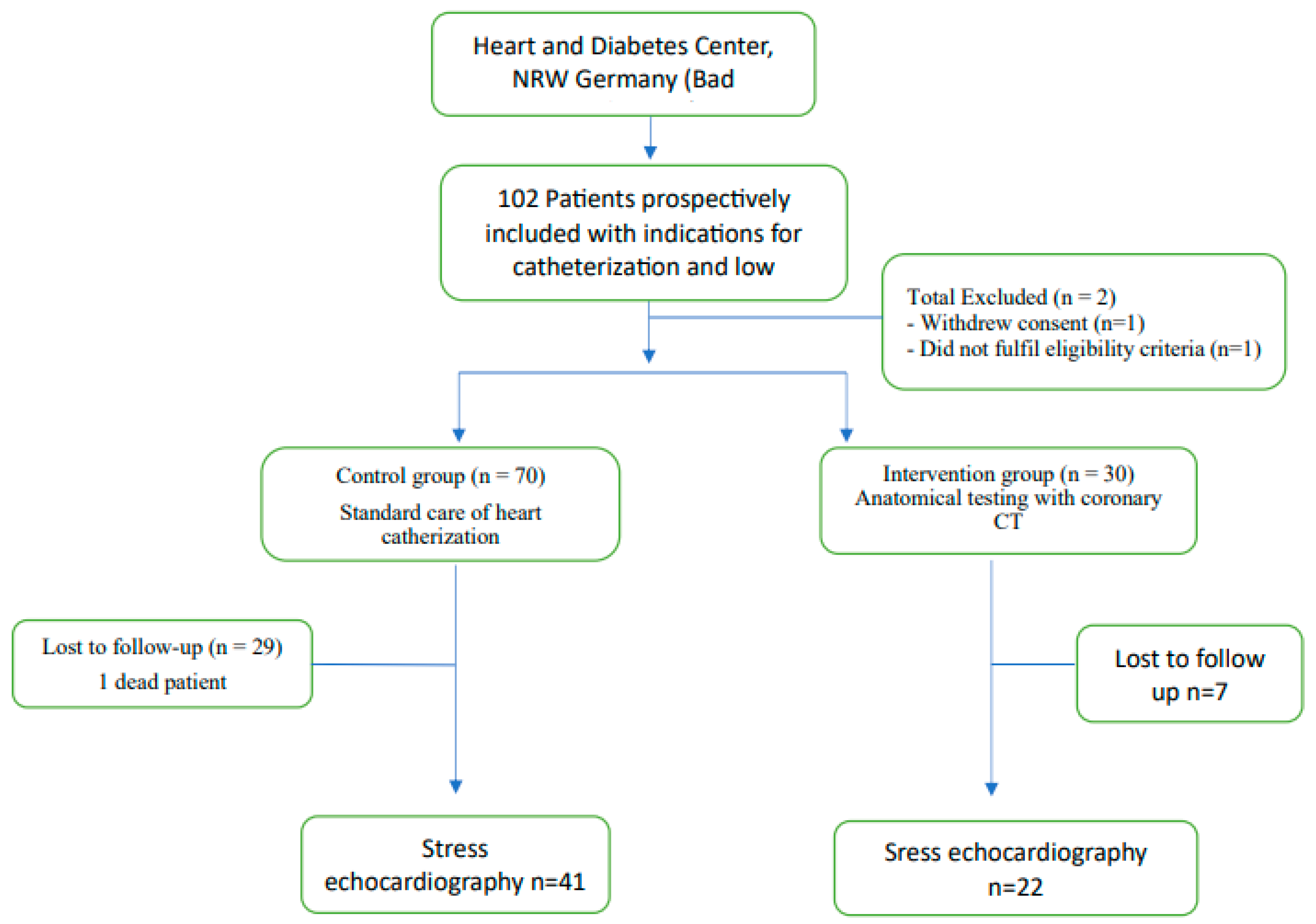
Between November 2019 and April 2022, a total of 102 consecutive patients were enrolled at our center. Of these, two patients withdrew from the study (
Figure 1, Flow Chart). Among the remaining 100 patients, 30 received a diagnosis through computed tomography (CT), while 70 underwent conventional treatment involving invasive coronary angiography (ICA). A total of 63 patients completed the follow-up, which had a median duration of 10 months.
Baseline Characteristics
Table 1 provides an overview of the baseline characteristics and results of the balance tests for the coronary CT and ICA groups. The mean age of patients in the coronary CT group was 63 ± 11.6 years, compared to 65 ± 9.4 years in the ICA group, indicating no statistically significant difference (p = 0.26). The distribution of sex was comparable across both groups, with 67% of the participants being male.
The principal cardiac risk factors, including hypertension, diabetes, and smoking, were similar between the two groups, with hypertension being the most prevalent risk factor noted.
The symptom most frequently reported was angina pectoris, which was observed in 60% of patients in the coronary CT group and in 54.3% of those in the ICA group, again showing no significant difference (p = 0.59). In summary, there were no statistically significant differences identified between the two groups for any of the assessed variables.
Diagnostic Results
CTCA Arm
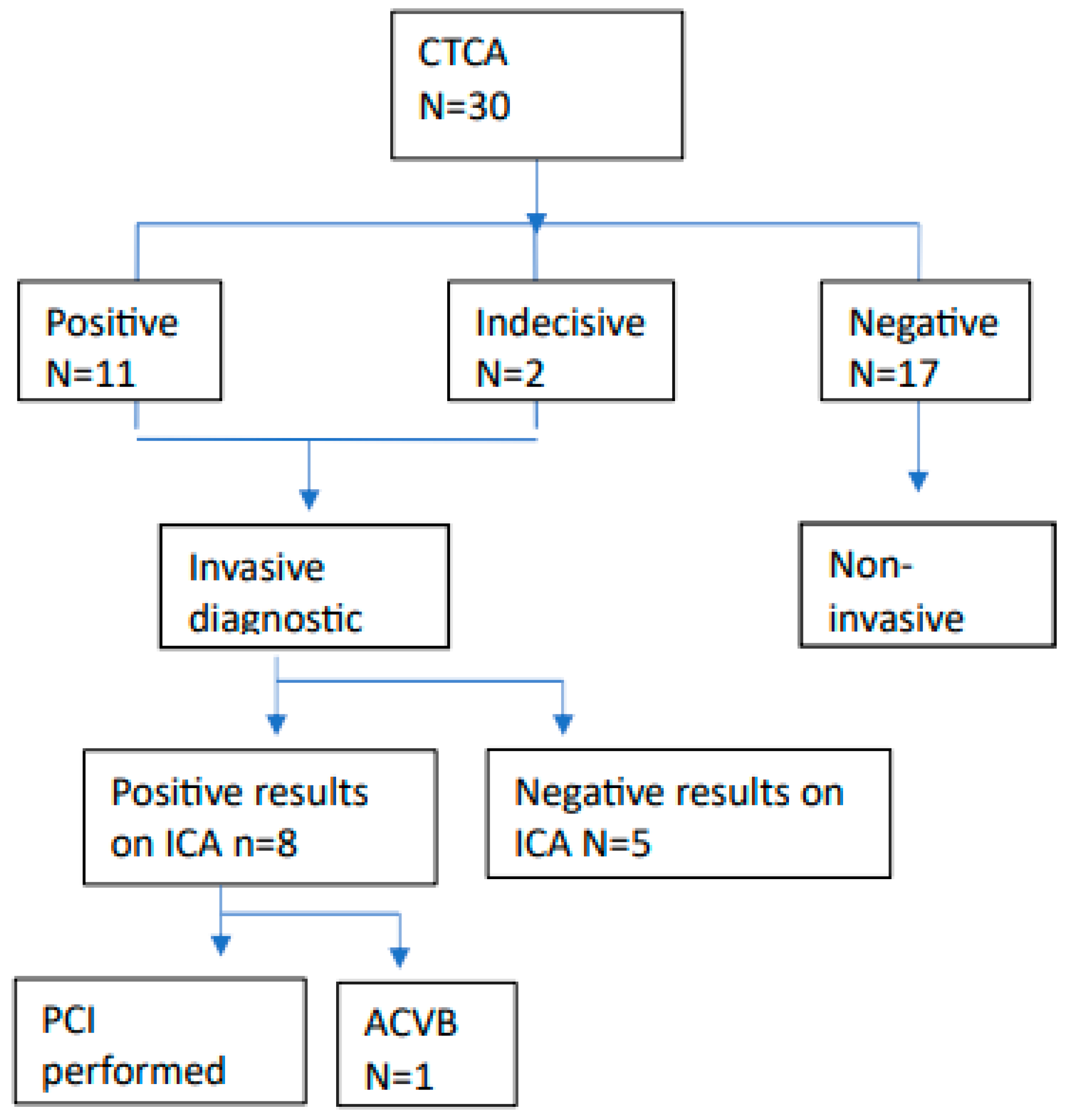
Figure 2 shows the pathological CTCA results and the following diagnostic procedures or treatment.
In our cohort, all patients exhibiting a non-zero CalcScore or stenoses classified by the CADRadsScore underwent further evaluation. The CalcScores within this cohort exhibited considerable variability, ranging from a minimum of 0 to a maximum of 1,119. The positive CalcScore results were referred for invasive coronary angiography (ICA). Conversely, patients presenting a CalcScore of 0 or lacking stenotic lesions were classified as non-pathological and subsequently discharged without further recommendations. Notably, one patient presented with a low CADRadsScore of 32 and no evidence of stenoses. This patient underwent myocardial scintigraphy as a functional assessment, which indicated no signs of ischemia.
11 out of 30 patients (37%) exhibited pathological results on their CT scans in the CTCA arm. Furthermore, two patients (6%) presented with image artifacts, resulting in inconclusive findings. Given their typical symptoms indicative of coronary artery disease, we proceeded with invasive coronary angiography (ICA) for both individuals. An invasive coronary angiography (ICA) was conducted for all 13 patients. Among these, eight patients (27%) were later confirmed to have pathological coronary disease through ICA, as illustrated in
Figure 2. Of the eight patients identified with coronary disease, six underwent interventional percutaneous coronary intervention (PCI), one received coronary artery bypass graft surgery (CABG), and one patient was diagnosed with moderate coronary artery stenosis but did not require any intervention. The remaining five patients did not exhibit any coronary pathologies and, consequently, did not necessitate further procedures. Additionally, 17 out of 30 patients (57%) in the CTCA arm either had a coronary calcium score of 0 or did not present with any stenoses as diagnosed by the CTCA. Consequently, these patients were discharged without the need for further procedures or recommendations.
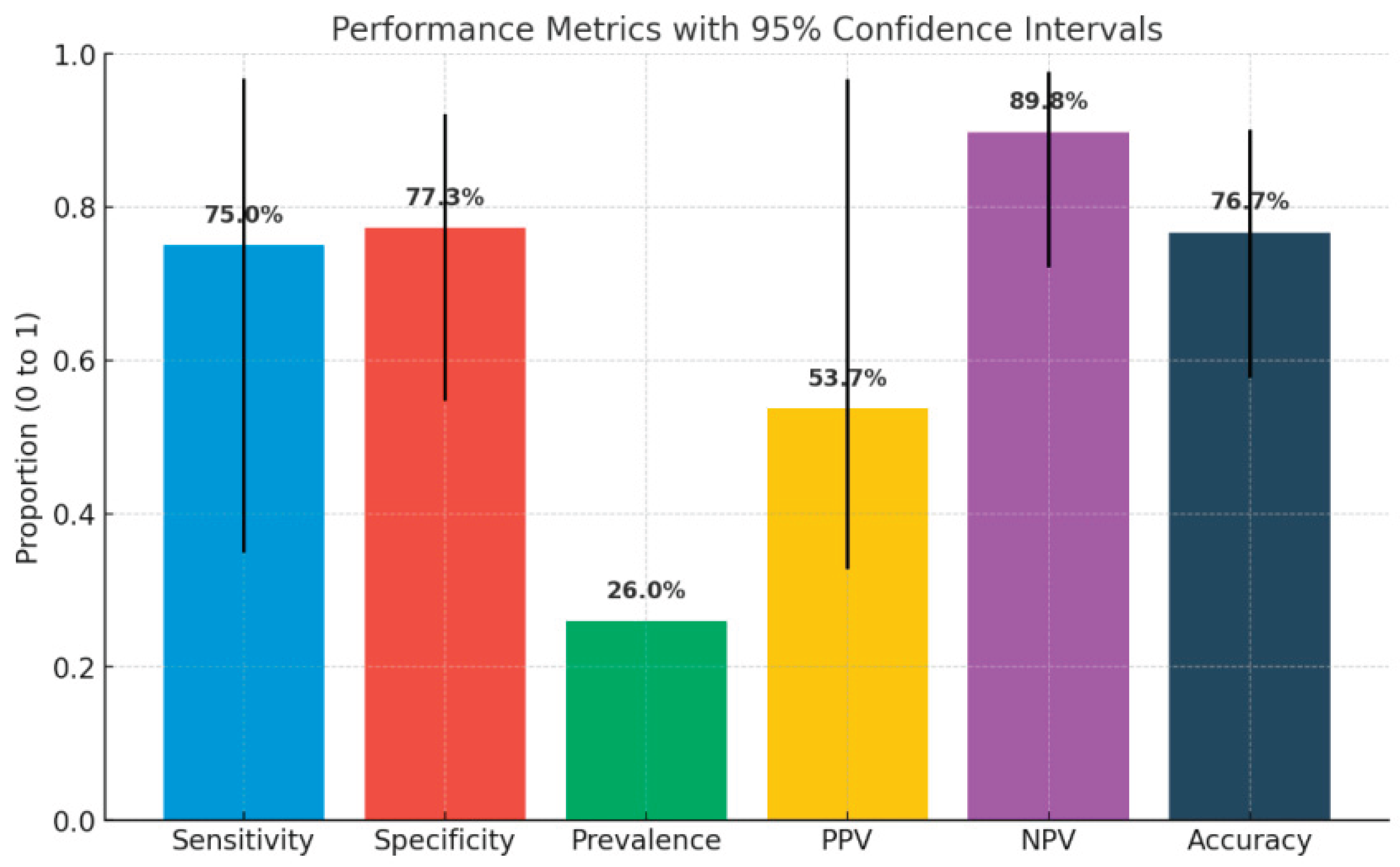
To evaluate the reliability of the CTCA as a non-invasive method we calculated, as presented on
Table 6, the results for sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV). "A diagnostic test evaluation was conducted on a subgroup of patients from the CTCA cohort who demonstrated positive results for CAD, using ICA as the comparative reference standard." According to the data presented in Contingency
Table 5, the sensitivity of computed tomography coronary angiography (CTCA) was recorded at 75%, while the specificity was established at 77.27%. The PPV for CTCA was determined to be 53%, as detailed in
Table 6.
Figure 5, shows a graphic of all six characteristics of the CTCA as a non-invasive method with 95% confidence intervals.
ICA Arm
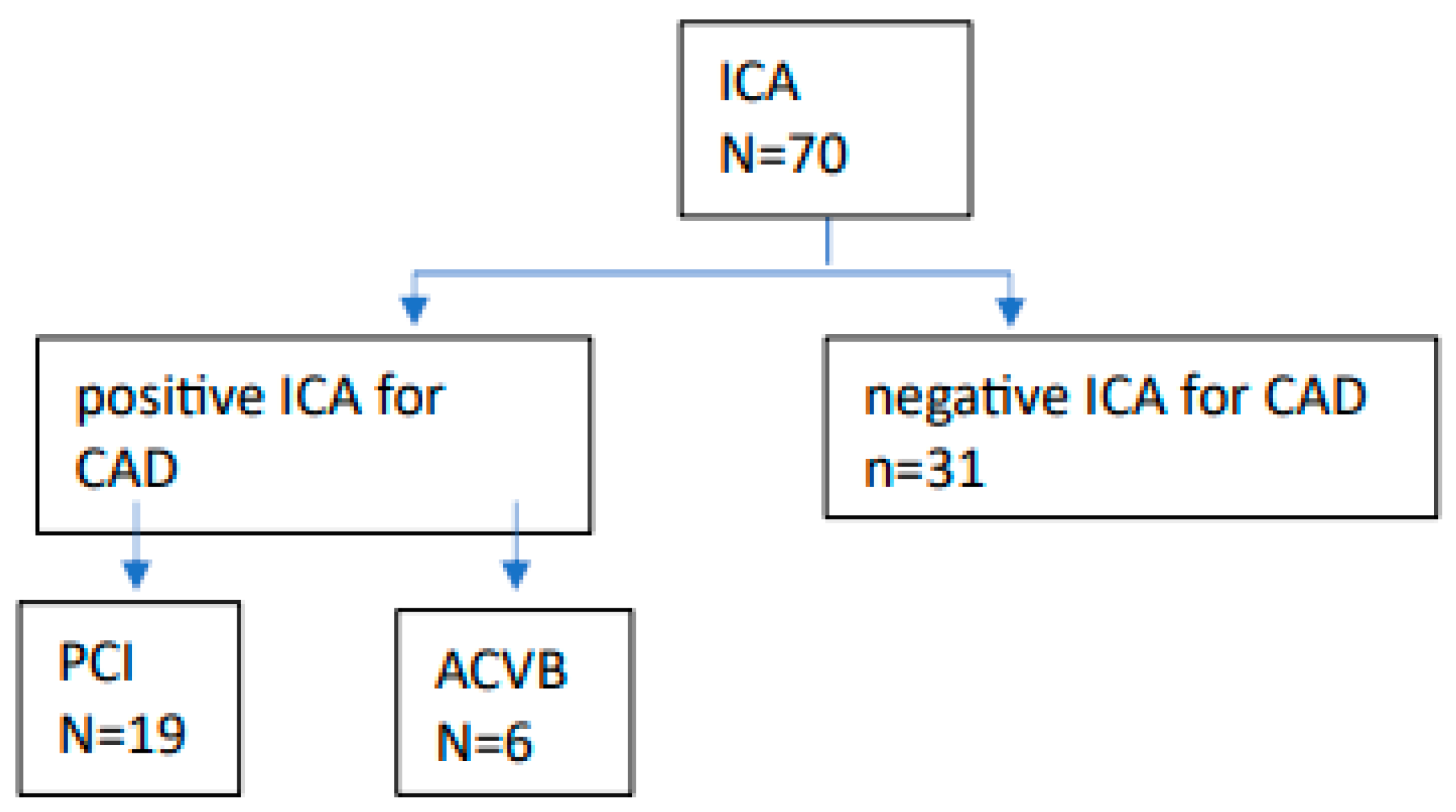
In the control group undergoing invasive coronary angiography (ICA), 39 out of 70 patients (55%) received a diagnosis of coronary artery disease. Among these patients, 19 (27%) proceeded to undergo percutaneous coronary intervention (PCI), while 6 (8%) required cardiac bypass surgery, as illustrated in
Figure 3. The remaining 31 patients exhibited no evidence of coronary pathology and were subsequently discharged without further recommendations.
Follow-Up and Endpoint Measures
Table 3 presents the outcomes observed at the follow-up, which had a median duration of 10 months. There were no significant differences in the outcomes between the two groups.
The primary outcome assessed was the difference in the Wall Motion Score Index (∆WMSI) from stress to rest,1comparing results at follow-up with those at admission. Among the 63 patients available for follow-up, none demonstrated a ∆WMSI exceeding 0.37 or exhibited signs of ischemia based on the findings from the stress echocardiography. The survival analysis of the WMSI is depicted in
Figure 4, indicating a survival rate of 1, which signifies that no changes in WMSI were detected in either group at the time of follow-up.
In relation to secondary outcomes, one patient in the ICA group died. This particular patient had a history of kidney transplantation several years prior, and no conclusive cause of death was determined. Moreover, only one patient in the CT group reported experiencing angina during the follow-up assessment. There were no recorded instances of myocardial infarction or revascularization at the follow-up evaluation.
We conducted a t-test analysis to evaluate further possible differences, based on several parameters like effective radiation dosis, contrast agent quantity, overall diagnostic time, admission time: either inpatient or ambulant care, between two groups.
The diagnostic time was assessed based on the documented records of the respective teams. For the CTCA group, the overall radiation exposure duration was considered as the diagnostic time. Conversely, for the ICA group, the diagnostic time was defined as the interval from puncture to sheath removal. Additionally, the total admission time for each patient was calculated from admission to discharge, as documented in the medical records. Our findings indicated no significant differences between the groups concerning the quantity of contrast dye administered or the overall diagnostic time (
Table 4).
Significant differences were observed in the effective radiation dose, with a mean dose of 2.3 mSv for the CTCA group compared to 1.5 mSv for the ICA group (P=0.03). Furthermore, the mean overall diagnostic time was 4.7 hours for the CTCA group, in contrast to 20.2 hours for the ICA group (P<0.0001).
Table 5.
Contingency table showing multivariate frequency distribution of CT findings versus disease status. This 2x2 contingency table illustrates the diagnostic performance of computed tomography (CT) in detecting coronary artery disease. Patients were categorized based on CT results (positive or negative) and confirmed presence or absence of disease. Frequencies are reported for each combination, enabling calculation of diagnostic accuracy metrics such as sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV).
Table 5.
Contingency table showing multivariate frequency distribution of CT findings versus disease status. This 2x2 contingency table illustrates the diagnostic performance of computed tomography (CT) in detecting coronary artery disease. Patients were categorized based on CT results (positive or negative) and confirmed presence or absence of disease. Frequencies are reported for each combination, enabling calculation of diagnostic accuracy metrics such as sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV).
| |
Disease |
No disease |
|
| CT positiv |
6 |
5 |
11 |
| CT negative |
2 |
17 |
19 |
| |
8 |
22 |
30 |
Table 6.
Diagnostic performance of computed tomography coronary angiography (CTCA). This table summarizes key performance metrics of CTCA in detecting coronary artery disease, including sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), accuracy, and disease prevalence. Values are presented with corresponding 95% confidence intervals, based on the study sample. The findings suggest that CTCA has high negative predictive value and moderate overall accuracy in this patient cohort.
Table 6.
Diagnostic performance of computed tomography coronary angiography (CTCA). This table summarizes key performance metrics of CTCA in detecting coronary artery disease, including sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), accuracy, and disease prevalence. Values are presented with corresponding 95% confidence intervals, based on the study sample. The findings suggest that CTCA has high negative predictive value and moderate overall accuracy in this patient cohort.
Figure 5.
Sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) of coronary computed tomography angiography (CTCA). This figure summarizes the diagnostic performance of CTCA for detecting significant coronary artery disease, using invasive coronary angiography (ICA) as the reference standard.
Figure 5.
Sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) of coronary computed tomography angiography (CTCA). This figure summarizes the diagnostic performance of CTCA for detecting significant coronary artery disease, using invasive coronary angiography (ICA) as the reference standard.
Discussion and Study Limitations
In a real-life setting conducted at an experienced tertiary care center, we evaluated the diagnostic efficacy of less invasive computed tomography coronary angiography (CTCA) in comparison to invasive coronary angiography (ICA). The results of our study indicate no significant differences in adverse cardiovascular events, mortality rates, or clinical manifestations, including the Wall Motion Score Index and reported episodes of angina pectoris, between the two diagnostic modalities.
We performed a survival analysis using Kaplan-Meier Curve comparing the two methods based on the delta WMSI.
We presented this analysis in
Figure 4 indicating no significant (HR 1, CI 95%) differences between the two groups at follow-up, suggesting that routine application of CTCA offers an effective alternative for diagnosing CAD in patients with low to intermediate pre-test probability (PTP). Our findings align with the results from trials such as DISCHARGE [
4]and Scot-Heart [
3], which highlight the non-inferiority of CTCA as a diagnostic tool compared to other non-invasive functional methods and invasive coronary angiography (ICA).
Table 6 indicates that CTCA possesses a strong negative predictive value of 89%, consistent with findings from the PROMISE [
2] trial. This supports the utilization of CTCA as a reliable method for ruling out CAD, thereby meeting the expectations of both healthcare professionals and patients. The subgroup analysis in our study indicated that performance metrics were lower than anticipated, with a sensitivity of 75% and a specificity of 77%. Furthermore, the positive predictive value (PPV) in our study was measured at 53%, which is markedly below the general range of 64-92% documented in existing literature[
10].These variations may be attributed to the relatively small cohort size within the CTCA group.
The average admission time for CTCA was recorded at 4.7 hours, significantly shorter than the 20.2 hours required for Invasive Catheterization Angiography (ICA). Furthermore, CTCA does not necessitate intensive patient monitoring following the procedure, in contrast to ICA. The CTCA group reported no complications, whereas the ICA group experienced a single incident of hematoma at the puncture site, with no subsequent deterioration in the patient’s condition. Additionally, randomized trials, such as DISCHARGE, have revealed that complication rates associated with invasive catheterization angiography are significantly higher when compared to those associated with CTCA. The effective radiation dose was significantly higher calculated at the CTCA group compared to the ICA group. We did not find significant differences between the two groups regarding the amount of contrast agent quantity used or the overall diagnostic time.
All participants in our study had no prior history of coronary artery disease. The most common presenting complaint was typical angina, reported by 60%, while approximately 50% cited dyspnoea as their primary reason for referral. Additionally, 21% were asymptomatic yet demonstrated abnormal electrocardiograms or stress test results, leading to referrals for further evaluation to exclude significant coronary artery disease.
The diagnosis and management of coronary artery disease are crucial topics in cardiology, as they significantly impact prognosis and morbidity. In cases of stable coronary artery disease (CAD), accurate diagnosis relies on patient-reported symptoms. However, variability in symptom reporting presents a challenge, as the absence or presence of atypical symptoms does not exclude significant coronary disease. Studies investigating the screening of asymptomatic patients for CAD have not shown clear advantages.
In light of these uncertainties, non-invasive tests play a vital role, especially for patients with low to intermediate pretest probabilities. Stress tests, such as myocardial perfusion imaging (MPS) and stress echocardiography, are valuable for identifying prognostic indicators, although they have limitations, including the potential for false negative results in balanced ischemia and oversights in left main coronary disease, valvular heart disease or reduced left ventricular function.
The European Society of Cardiology (ESC) has offered recommendations for coronary artery disease (CAD) and CT coronary angiography (CTCA) since 2019. Notably, starting in January 2024, patients in Germany with cardiological indications and public health insurance will be able to undergo CTCA at accredited centers. This change is expected to increase both the number of procedures performed and the certified centers available.
Moreover, it highlights the need for future multicenter trials to evaluate the cost-effectiveness of CTCA compared to invasive coronary angiography (ICA) in Germany. Currently, only 30 cardiac CT centers in Germany are recognized by the German Cardiac Society to train and certify cardiologists and radiologists in cardiac CT.
Our study has several important limitations. First, the small sample size may be underpowered to identify significant differences between groups. Additionally, 37 patients were lost to follow-up, primarily due to the impact of the COVID-19 pandemic. However, all patients were contacted via phone, and their symptoms were evaluated. Moreover, since our study was not randomized, we cannot exclude potential selection bias. The choice of some patients to undergo CT coronary angiography (CTCA) instead of invasive coronary angiography (ICA) may also have introduced a self-selection bias.
Implications for Practice
Our study supports the assertion that CT coronary angiography (CTCA) is a safe and reliable non-invasive modality for the diagnosis or exclusion of coronary artery disease (CAD) when appropriate clinical indications are met. The future of non-invasive diagnostics appears promising for CT coronary angiography (CTCA), especially with the emergence of photon-counting CTCA technology, enabling a substantially higher image resolution. To further validate its effectiveness and its role in detecting atherosclerosis in patients with angina, there is a need for large-scale trials.
Figure 1.
Flow diagram of patient inclusion, group allocation, and follow-up in a prospective comparison of coronary computed tomography angiography (CTCA) versus standard invasive coronary angiography (ICA). A total of 102 patients with clinical indications for coronary catheterization and low to intermediate pre-test probability of coronary artery disease were prospectively enrolled at the Heart and Diabetes Center, NRW, Germany. Two patients were excluded (one withdrew consent, one did not meet eligibility criteria). The remaining 100 patients were allocated to either the control group receiving standard ICA (n = 70) or the intervention group undergoing CTCA-based anatomical testing (n = 30). Follow-up stress echocardiography was completed by 41 patients in the control (ICA) group (29 lost to follow-up, including one death) and 22 patients in the intervention (CTCA) group (8 lost to follow-up).
Figure 1.
Flow diagram of patient inclusion, group allocation, and follow-up in a prospective comparison of coronary computed tomography angiography (CTCA) versus standard invasive coronary angiography (ICA). A total of 102 patients with clinical indications for coronary catheterization and low to intermediate pre-test probability of coronary artery disease were prospectively enrolled at the Heart and Diabetes Center, NRW, Germany. Two patients were excluded (one withdrew consent, one did not meet eligibility criteria). The remaining 100 patients were allocated to either the control group receiving standard ICA (n = 70) or the intervention group undergoing CTCA-based anatomical testing (n = 30). Follow-up stress echocardiography was completed by 41 patients in the control (ICA) group (29 lost to follow-up, including one death) and 22 patients in the intervention (CTCA) group (8 lost to follow-up).
Figure 2.
Diagnostic pathway of patients in the CTCA group. Following coronary computed tomography angiography (CTCA), 11 patients had positive findings, 2 had inconclusive results, and 17 had negative findings. Patients with positive or inconclusive results proceeded to invasive coronary angiography (ICA). Among those, 8 had positive findings on ICA, leading to percutaneous coronary intervention (PCI) in 7 patients and coronary artery bypass grafting (CABG) in 1 patient. Patients with negative CTCA results were managed non-invasively.
Figure 2.
Diagnostic pathway of patients in the CTCA group. Following coronary computed tomography angiography (CTCA), 11 patients had positive findings, 2 had inconclusive results, and 17 had negative findings. Patients with positive or inconclusive results proceeded to invasive coronary angiography (ICA). Among those, 8 had positive findings on ICA, leading to percutaneous coronary intervention (PCI) in 7 patients and coronary artery bypass grafting (CABG) in 1 patient. Patients with negative CTCA results were managed non-invasively.
Figure 3.
Diagnostic pathway of patients in the invasive coronary angiography (ICA) group. All 70 patients underwent ICA as the initial diagnostic approach. Coronary artery disease (CAD) was confirmed in 39 patients, leading to percutaneous coronary intervention (PCI) in 19 patients and coronary artery bypass grafting (CABG) in 6 patients. No significant CAD was found in 31 patients.
Figure 3.
Diagnostic pathway of patients in the invasive coronary angiography (ICA) group. All 70 patients underwent ICA as the initial diagnostic approach. Coronary artery disease (CAD) was confirmed in 39 patients, leading to percutaneous coronary intervention (PCI) in 19 patients and coronary artery bypass grafting (CABG) in 6 patients. No significant CAD was found in 31 patients.
Figure 4.
Kaplan–Meier survival analysis based on the Wall Motion Score Index (WMSI). Patients were stratified according to their ΔWMSI (change in WMSI), with a threshold of 0.37 identified as both statistically and clinically relevant. No significant difference in survival was observed between the groups above and below this cutoff. Both groups demonstrated a survival rate of 1.0 during the follow-up period, indicating no prognostic discrimination by ΔWMSI in this cohort.
Figure 4.
Kaplan–Meier survival analysis based on the Wall Motion Score Index (WMSI). Patients were stratified according to their ΔWMSI (change in WMSI), with a threshold of 0.37 identified as both statistically and clinically relevant. No significant difference in survival was observed between the groups above and below this cutoff. Both groups demonstrated a survival rate of 1.0 during the follow-up period, indicating no prognostic discrimination by ΔWMSI in this cohort.
Table 1.
Baseline characteristics of the study population. This table presents socio-demographic data, cardiovascular risk factors, reported symptoms, and pre-diagnostic test findings of patients assigned to either the CTCA (computed tomography coronary angiography) group or the ICA (invasive coronary angiography) group. Continuous variables are reported as mean and standard deviation (SD), while categorical variables are expressed as number and percentage. Statistical comparisons between groups were performed using Student’s t-test or Chi-square test, as appropriate. No statistically significant differences were observed between the groups across measured parameters, indicating comparable baseline profiles.
Table 1.
Baseline characteristics of the study population. This table presents socio-demographic data, cardiovascular risk factors, reported symptoms, and pre-diagnostic test findings of patients assigned to either the CTCA (computed tomography coronary angiography) group or the ICA (invasive coronary angiography) group. Continuous variables are reported as mean and standard deviation (SD), while categorical variables are expressed as number and percentage. Statistical comparisons between groups were performed using Student’s t-test or Chi-square test, as appropriate. No statistically significant differences were observed between the groups across measured parameters, indicating comparable baseline profiles.
| Socio-demographic |
| Variable |
Description |
Computed tomography (CT)
n=30
(mean and Std. Dev)
|
Invasive coronary angiography (ICA)
n=70
(mean and Std.Dev)
|
T Test/Chi-square Test
(two- sided P value)
|
| Age |
Self-reported |
63 (11,6) |
65 (9,4) |
0.26 |
| Male |
|
20 (66,7%) |
47(67,1%) |
0,96 |
| Height (cm) |
Self-reported |
174 (6.04) |
174 (9,4) |
0,98 |
| Weight (Kg) |
Self-reported |
87 (18.4) |
88,3 (18,6) |
0,43 |
| Body mass index (BMI) |
Kg/m² |
28.8 (5,7) |
29,1 (5,8) |
0,83 |
| Mean blood pressure (mmHg) |
Measured at the ambulatory care |
98,8 (12.1) |
103 (13,4) |
0,14 |
| Heart Rate (beats per minute) |
Measured at the ambulatory care |
68,3 (10,8) |
68,8 (11,8) |
0,84 |
| Risk factors |
| Cardiac Risk Factors |
Description |
CT n=30 |
ICA n=70 |
T Test/Chi-square Test
(two sided P value)
|
| Hypertension |
Pre-diagnosed
(number,%) |
23 (76%) |
59 (84,3%) |
0,36 |
| Diabetes |
Pre-diagnosed
(number,%) |
8 (26.7%) |
22 (31,4%) |
0,63 |
| Hypercholesterolemia |
Pre-diagnosed
(number,%) |
17 (56,7%) |
42 (60%) |
0,75 |
| Current smoker |
Self-reported
(number,%) |
7 (23.3) |
23 (32,9%) |
0,34 |
| Ex-smoker |
Self-reported
(number,%) |
5 (16.7%) |
16 (22,9%) |
0,48 |
| Myocardial infarction |
Self reported/ pre-diagnosed
(number,%) |
1 (3,3%) |
1 (1,4%) |
0,53 |
| Adiposity |
Evaluated according to BMI
(number, %) |
15 (50%) |
30 (42,9) |
0,51 |
| Apoplexy |
Self-reported/ pre-diagnosed
(number, %) |
3 (10%) |
3 (4,3%) |
0,27 |
| Peripheral artery disease PAD |
Pre-diagnosed
(number, %) |
1 (3,3%) |
4 (5,7%) |
0,61 |
| Family history for CAD |
Self-reported
(number,%) |
8 (26,7%) |
24 (34,3%) |
0,4 |
| Symptoms |
| Symptoms |
Description |
CT
n=30
|
ICA
n=70
|
T Test/Chi-square Test
(two sided P value)
|
| Angina |
Self reported
Evaluated based on CCS 0-IV (Canadian cardiovascular society)
(number, %) |
18 (60%) |
38 (54,3%) |
0,9 |
| Pain radiation |
Self reported
(number, %) |
4 (13,3%) |
12 (17,1%) |
0,63 |
Dyspnea |
Self reported, primary or only symptom |
4(13,3%) |
19 (27,1%) |
0,13 |
| Pre-diagnostic: |
| Symptoms |
Description
|
CT
n=30
|
ICA
n=70
|
T Test/Chi-square Test
(two sided P value)
|
| Pathological ECG of extremity leads |
Performed at the ambulatory care unit of the clinic
(number, %) |
4 (13%) |
11 (15%) |
0,76 |
| Pathological ECG of chest leads |
Performed at the ambulatory care unit of the clinic
(number, %) |
3 (10%) |
5 (7%) |
0,62 |
Pathological echocardiography
(abnorm wall motion) |
Intranet or performed from the referring cardiologist
(number, %) |
2 (6%) |
9 (12%) |
0,36 |
| Performed stress ECG |
Results taken from the referring cardiologist
(number, %) |
9 (30%) |
32 (45%) |
0,14 |
| Pathological stress ECG in extremity leads |
Results taken from the referring cardiologist
(number, %) |
7 (77%) (out of performed stress ECG) |
18 (56%) |
0,8 |
| Pathological stress ECG in chest leads |
Results taken from the referring cardiologist
(number, %) |
4 (44%) (out of performed stress ECG) |
13 (40%) |
0,52 |
| Performed Stress Echocardiography |
Results taken from the referring cardiologist
(number, %) |
3 (10%) |
8 (11%) |
0,83 |
| Pathological stress echocardiography |
Results taken from the referring cardiologist
(number, %) |
3 (100%) out of performed stress echocardiography |
6 (75%) |
0,81 |
| Performed stress myocardial scintigraphy |
Results taken from the referring cardiologist
(number, %) |
11 (36%) |
31 (44%) |
0,47 |
| Pathological stress myocardial scintigraphy |
Results taken from the referring cardiologist
(number, %) |
8 (72%) |
30 (96%) |
0,12 |
Table 2.
Coronary artery diagnostic findings and procedural outcomes. This table summarizes the diagnostic and interventional results obtained during initial hospital admission for patients undergoing either computed tomography coronary angiography (CTCA) or invasive coronary angiography (ICA). Data include the prevalence and severity of coronary artery stenosis, adjunctive diagnostic modalities (IVUS, IFR/FFR), anatomical distribution of disease, and therapeutic interventions such as percutaneous coronary intervention (PCI) and coronary artery bypass grafting (CABG). Radiation exposure and contrast media volume are also reported. Continuous variables are presented as mean ± standard deviation, and categorical variables as number and percentage. Group comparisons were performed using t-tests or Chi-square tests, with corresponding p-values shown.
Table 2.
Coronary artery diagnostic findings and procedural outcomes. This table summarizes the diagnostic and interventional results obtained during initial hospital admission for patients undergoing either computed tomography coronary angiography (CTCA) or invasive coronary angiography (ICA). Data include the prevalence and severity of coronary artery stenosis, adjunctive diagnostic modalities (IVUS, IFR/FFR), anatomical distribution of disease, and therapeutic interventions such as percutaneous coronary intervention (PCI) and coronary artery bypass grafting (CABG). Radiation exposure and contrast media volume are also reported. Continuous variables are presented as mean ± standard deviation, and categorical variables as number and percentage. Group comparisons were performed using t-tests or Chi-square tests, with corresponding p-values shown.
| Results |
| Diagnostic run on the admission day |
Description |
CT
n =30
|
ICA
n=70
|
T-Test, chi square,
(p-value)
|
| Coronary stenoses all degrees |
Number of patients with coronary stenoses (%) |
13 (43%) |
41 (58%) |
0.16 |
| Minimal stenosis |
Number and % of patients with coronary stenoses <50% |
3 (10%) |
18 (26%) |
0.07 |
| Mild stenosis |
Number and % of patients with coronary stenoses 50-74% |
6 (20%) |
5 (7%) |
0.06 |
| Moderate stenosis |
Number of patients with coronary stenoses 75-90% (%) |
3 (10 %) |
16 (2,2%) |
0.13 |
| Severe stenosis |
Number and % of patients with coronary stenoses >90% |
3 (10%) |
18 (26%) |
0.07 |
Chronic total occlusion
(CTO) |
Number and % of patients with chronic total occlusion |
2 (6,6%) |
7 (10%) |
0.59 |
Intravascular ultrasound
(IVUS) |
Number and % of patients diagnosed with IVUS |
2 (6%) |
2 (2.8%) |
0.37 |
| Pathological IVUS |
Number and % of patients with pathological IVUS result |
2 (6%) |
2 (2.8%) |
0.37 |
Instantaneous flow reserve/fractional flow reserve
(IFR/FFR) |
Number and % of patients diagnosed either with iFR or FFR |
4 (13%) |
20 (28%) |
0.1 |
Pathological IFR/FFR
|
Number and % of patients with pathological IFFR/FFR result |
3 (10%) |
5 (7%) |
0.62 |
| Right coronary artery stenosis (RCA) |
Number and % of patients diagnosed through ICA |
6 (46%) |
22 (53%) |
0.24 |
| Ramus circumflexus artery stenosis (RCX) |
Number and % of patients diagnosed through ICA |
5 (38%) |
24 (58%) |
0.07 |
| Left anterior descending artery stenosis (LAD) |
Number and % of patients diagnosed through ICA |
11 (84%) |
29 (70%) |
0.65 |
| Common trunk artery stenosis |
Number and % of patients diagnosed through ICA |
1 (3%) |
1 (2%) |
0.53 |
| Hemodynamic significant stenosis |
Number and % of patients diagnosed through ICA |
8 (27%) |
28 (40%) |
0.2 |
| PCI performed |
Performed from the interventional cardiologists |
5 (16%) |
18 (25%) |
0.32 |
| ACVB |
Performed from surgeons of the clinic |
1 (3%) |
7 (1%) |
|
| Right coronary artery (RCA) percutaneous coronary intervention (PCI) |
Performed from the interventional cardiologists of the clinic |
3 (10%) |
9 (12%) |
0.68 |
| Ramus circumflexus PCI |
Performed from the interventional cardiologists of the clinic |
0 |
9 (12%) |
0.04 |
| Left anterior descendens artery PCI |
Performed from the interventional cardiologists of the clinic |
4 (13%) |
11 (15%) |
0.76 |
| Common trunk artery PCI |
Performed from the interventional cardiologists of the clinic |
1 (3%) |
1 (1%) |
0.53 |
| Effective dosis of radiation (mSV) |
milli Sievert |
Mean:2.33
Std. Dev. 1.26 |
Mean 1.70
Std. Dev. 1.68 |
0.04 |
| Contrast agent volume (ml) |
milliliter |
Mean=55,5 ml
Std.Dev. 6,06
Max. 50 ml
Min. 70 ml |
Mean=76,71 ml
Std.dev.=35,44
Max. 164 ml, Min. 29 ml |
<0,01 |
Table 3.
Clinical outcomes during follow-up. This table presents follow-up outcomes (range: 6–31 months) for patients initially assessed via computed tomography coronary angiography (CTCA) or invasive coronary angiography (ICA). Outcomes include cardiovascular mortality, rehospitalization due to angina, stress echocardiography results, symptoms under stress (angina and dyspnea), and changes in wall motion score index (ΔWMSI). Continuous variables are expressed as mean ± standard deviation, and categorical outcomes are presented as number and percentage. Group comparisons were performed using t-tests or Chi-square tests as appropriate, with p-values reported.
Table 3.
Clinical outcomes during follow-up. This table presents follow-up outcomes (range: 6–31 months) for patients initially assessed via computed tomography coronary angiography (CTCA) or invasive coronary angiography (ICA). Outcomes include cardiovascular mortality, rehospitalization due to angina, stress echocardiography results, symptoms under stress (angina and dyspnea), and changes in wall motion score index (ΔWMSI). Continuous variables are expressed as mean ± standard deviation, and categorical outcomes are presented as number and percentage. Group comparisons were performed using t-tests or Chi-square tests as appropriate, with p-values reported.
| Outcomes |
| Variable |
Description |
Computed tomography
n=30
|
Invasive coronary angiography
n=70
|
T Test/Chi-square Test
(two-sided P value)
|
Outcomes at follow up
(6-31 months) |
Months to follow up (mean and Std. Dev) |
8.57
(2.72) |
12.2
(4.83) |
0.002 |
| Cardiovascular deaths |
Clinically diagnosed |
0 |
0 from Angina
1 other causes |
No statistics |
| Rehospitalization coming from angina |
Clinically diagnosed |
1 (3,3%) |
1 (1,4%) |
0,9 |
| Follow up with stress echocardiography |
Clinically diagnosed |
22 (73%) |
41 (58%) |
0.16 |
| Angina under Stress |
Clinically diagnosed |
1 (4%) |
0 |
0,19 |
| Dyspnea under Stress |
Clinically diagnosed after NYHA classification (I-IV) |
14 (60%) |
21 (51%) |
0,72 |
| Wall Motion Score Index (ΔWMSI=0) |
calculated |
22 (73%) |
41 (58%) |
0,27 |
Table 4.
Subgroup analysis comparing contrast dye volume, radiation exposure, and procedural time between CTCA and ICA. This table presents a comparative analysis between patients undergoing computed tomography coronary angiography (CTCA) and those receiving exclusive invasive coronary angiography (ICA). Variables assessed include contrast agent volume (ml), effective radiation dose (mSv), total admission time (hours), and diagnostic procedure time (minutes). Mean values are reported with standard deviations where applicable. Statistical comparisons were made using two-sided t-tests.
Table 4.
Subgroup analysis comparing contrast dye volume, radiation exposure, and procedural time between CTCA and ICA. This table presents a comparative analysis between patients undergoing computed tomography coronary angiography (CTCA) and those receiving exclusive invasive coronary angiography (ICA). Variables assessed include contrast agent volume (ml), effective radiation dose (mSv), total admission time (hours), and diagnostic procedure time (minutes). Mean values are reported with standard deviations where applicable. Statistical comparisons were made using two-sided t-tests.
| |
CTCA (mean) |
Exclusively ICA (mean) |
T-test- two sided p-Value |
| Contrast dye |
55 ml |
66 ml |
0.09 |
| Effective radiation dosis |
2,3 mSv |
1,5 mSv |
0.03 |
| Admission time |
4,76H (std. dev. 0.24) |
20,2h(std, dev. 11.05) |
<0.0001 |
| Diagnostic time |
23,5 min |
25,5 min |
0.6 |