1. Introduction
The Polish population has undergone significant shifts in dietary habits in recent years, marked by an increased consumption of ultra-processed foods (UPFs) and added sugars. This study aims to evaluate the prevalence and impact of sweets addiction within this population to inform public health interventions and clinical practice.
Food addiction, particularly to sweets, has garnered substantial research attention due to its strong association with metabolic diseases. The rising global prevalence of conditions such as obesity and type 2 diabetes mellitus (T2DM) represents a major public health challenge, contributing to increased mortality and disability-adjusted life years across all socioeconomic groups [
1]. Among key modifiable risk factors, dietary behavior, such as the habitual consumption of UPFs, has been identified as a primary driver of these conditions [
2,
3]. UPFs, characterized by high levels of added sugars, refined carbohydrates, and saturated fats, and low levels of fiber and micronutrients, are strongly linked to weight gain, systemic inflammation, insulin resistance, and impaired satiety signaling [
4,
5,
6].
While traditional dietary patterns such as the Mediterranean diet are linked to improved metabolic outcomes and reduced chronic disease risk [
7,
8], the Western-style diet high in UPFs has been implicated in the development of metabolic disorders, including metabolic dysfunction-associated steatotic liver disease (MASLD), T2DM, cardiovascular complications [
9,
10], as well as dementia and Alzheimer’s disease [
9,
10,
42]. In particular, excessive intake of sugar-sweetened foods and beverages, such as those high in fructose can promote hepatic fat accumulation, mitochondrial dysfunction, and fibrosis [
11,
12].
Beyond metabolic outcomes, growing evidence suggests that UPFs, particularly those rich in added sugars, may exert addictive-like effects by stimulating reward pathways in the brain, leading to compulsive eating behaviors that mirror substance use disorders [
13,
14]. High consumption of sweet UPFs has also been linked to impaired cognitive function, mood instability, and increased risk of depression and anxiety, which may be mediated by blood glucose fluctuations, gut microbiota dysbiosis, and neuroinflammation [
15,
16,
17]. Moreover, habitual intake of these foods can disrupt sleep quality and circadian rhythms, further aggravating metabolic and mental health issues [
18]. In particular, in children and adolescents, excessive sugar intake has been associated with reduced academic performance, attention deficits, and increased hyperactivity [
19]. These neurobiological and behavioral effects carry serious public health implications, especially in countries like Poland, where average sugar consumption far exceeds recommended levels, contributing to the burden of both physical and mental health conditions [
20].
The FitMIND Foundation, established in 2022, is an organization, in which a group of experts in dietetics and psychology work in order to support patients struggling with a broad spectrum of eating disorders and related unhealthy behaviors. Despite its short history, the foundation has provided help and professional support to hundreds of patients from all over Poland. Practical observations from this experiences support the conclusion according to which there is a need for a tool to quantitatively assess the severity of sweets addiction, which is often a significant component of eating disorders.
In sum, we believe that there is a need for a validated, culturally adapted tool for evaluating problematic habits associated with sugary food consumption, which may be used for early detection of addictive-like behaviors towards sweet foods and inform public health strategies aimed at mitigating the metabolic and neuropsychological risks associated with excessive UPF intake.
Given the limitations of available tools to assess sweet food addiction, this pilot study aims to demonstrate psychometric properties of the scale developed by the experts from the FitMIND Foundation (named the FitMIND Foundation Sweets Addiction Scale (FFSAS)) referring to the structure of the Yale Food Addiction Scale 2.0 (YFAS 2.0) based on external expert validation as well as extensive psychometric analysis.
2. Materials and Methods
2.1. Study Design
The validation of the FFSAS followed a two-phase design that combined expert judgement with psychometric testing.
2.1.1. Phase I: Validation of External Experts
A panel of 11 expert judges was recruited to evaluate all 35 items of the FFSAS. The experts (mean experience = 16.5 years; range = 12–24) represented medicine (psychiatry), psychology, and health sciences. Each item was rated on a five-point Likert scale (1 = “strongly disagree”, 5 = “strongly agree”) across four dimensions: (i) clarity, (ii) content validity, (iii) linguistic appropriateness and (iv) construct representativeness. For every item the highest and lowest scores were discarded, a mean of the remaining nine ratings was calculated and ranked; ties were resolved automatically by averaging the ranks and rounding to one decimal. Items scoring < 3.5 were flagged for future revision (e.g. FFSAS9, 15, 30).
Table 1 present the overview of the recruited expert panel with details on filed of expertise and specialization.
2.1.2. Phase II: Psychometric Analysis
Psychometric analysis was based on data collected from participants and included: (a) internal consistency via Cronbach’s α; (b) construct validity via Spearman correlations between FFSAS scores and sweets-related variables; and (c) factorial validity via exploratory and confirmatory factor analyses (EFA, CFA).
2.2. Study Population
The study population, involved in the Phase II, consisted of adult volunteers (aged ≥18 years), in accordance with Polish legal standards. The online questionnaire was distributed through the FitMIND Foundation’s network. The online survey was conducted from January 13, 2022, to February 10, 2025. No minimum sample size was predetermined; the aim was to collect data from as many participants as possible. The questionnaire included the FFSAS scale items, along with additional questions on demographics and eating behaviors, particularly related to sweets consumption. These questions are provided in Supplementary Material (ST1).
This study was approved by the Ethics Committee of Silesia Medical University (protocol code PCN/CBN/0022/KB/291/21, approved January 01, 2022) and conducted in accordance with the Declaration of Helsinki. All participants provided written informed consent, collected electronically via an online Google Forms questionnaire prior to participation.
2.3. Questionnaire Development
The FFSAS was developed by adapting the YFAS 2.0, a validated tool designed to assess food addiction based on the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) criteria for substance use disorders[
22]. The YFAS 2.0 comprises 35 items scored on an 8-point Likert scale (0 = "never," 7 = "daily"), grouped into 11 addiction symptoms plus a 12th criterion assessing clinical distress or functional impairment. These criteria include: (1) consuming larger amounts of food or for longer than intended, (2) persistent desire or unsuccessful attempts to reduce consumption, (3) excessive time spent obtaining, using, or recovering from food, (4) neglect of important social, occupational, or recreational activities, (5) continued use despite knowledge of adverse consequences, (6) tolerance (increased amounts needed or reduced effect), (7) withdrawal symptoms or use to relieve them, (8) continued use despite social or interpersonal problems, (9) failure to fulfill major role obligations, (10) use in physically hazardous situations, (11) craving or strong urge to consume, and (12) distress or functional impairment caused by eating behavior. Each item has a predefined threshold (e.g., "once a month" to "4–6 times a week") yielding a binary score (0 = not met, 1 = met). The total score, ranging from 0 to 11 (excluding the distress criterion for symptom count), determines food addiction severity: mild (2–3 symptoms), moderate (4–5 symptoms), or severe (≥6 symptoms), with diagnosis requiring the presence of distress [
22].
For the FFSAS, the Polish version of YFAS 2.0, validated by Poprawa et al. (2020) [
23] was used as the template, ensuring adequate translation. This adaptation retained the 35-item structure and 8-point Likert scale but replaced all references to "food" with "sweets" to focus exclusively on sweets-specific addiction-like behaviors.
The FFSAS assesses 12 criteria tailored to sweets consumption, including:
Loss of Control – e.g., "When I started eating sweets, I consumed much more than I planned" (FFSAS1).
Persistent Desire or Unsuccessful Efforts to Cut Down – e.g., "I really wanted to cut down or stop eating sweets but couldn’t" (FFSAS5).
Excessive Time Spent – e.g., "When sweets were unavailable, I went out of my way to get them" (FFSAS10).
Neglect of Activities – e.g., "I ate sweets so often or in such quantities that I ate instead of working or spending time with family or friends" (FFSAS11).
Continued Use Despite Negative Consequences – e.g., "I kept eating sweets despite knowing it harmed my health" (FFSAS29).
Tolerance – e.g., "Over time, I had to eat more and more sweets to achieve satisfaction" (FFSAS18).
Withdrawal Symptoms – e.g., "When I cut down or stopped eating sweets, I felt irritable, nervous, or sad" (FFSAS19).
Overeating Despite Social Problems – e.g., "I had problems with family or friends due to overeating" (FFSAS24).
Failure to Fulfill Roles – e.g., "My overeating interfered with caring for my family or doing household duties" (FFSAS27).
Use in Hazardous Situations – e.g., "I was so distracted by eating sweets that I could have had an accident" (FFSAS30).
Craving – e.g., "I had such an intense craving for sweets that I had to eat them immediately" (FFSAS33).
Distress and Functional Impairment – e.g., "I had serious life problems due to eating, affecting daily organization, work, school, friends, family, or health" (FFSAS35).
Each criterion is measured by 1–4 items (see Annex for full list), with scoring thresholds adapted from YFAS 2.0. A sweets addiction diagnosis requires meeting at least two of the 11 symptom criteria, plus the 12th criterion (distress/impairment), within the past 12 months. The total symptom count (0–11) classifies severity as: no sweets addiction (No SA, 0–1 symptom without distress), mild (2–3 symptoms), moderate (4–5 symptoms), or severe (≥6 symptoms), with distress required for all diagnoses. Participants’ responses classify them into four groups: No SA, Mild SA, Moderate SA, or Severe SA. Additionally, the questionnaire includes items assessing the frequency of emotional responses related to sweets consumption (e.g., remorse, guilt, shame, anger), rated on the same 8-point scale (0 = "never," 7 = "several times a day"), providing supplementary data on psychological correlates of sweets addiction. After Phase 1 data collection, the modified items were externally reviewed by an expert panel of 11 specialists (see Section 2.2.3) to ensure cultural relevance, linguistic clarity, and alignment with the Polish population’s context.
2.4. Statistical Analysis
2.4.1. Descriptive Statistics
All statistical procedures were performed in IBM SPSS Statistics v26 and STATISTICA v13. Two-tailed p < 0.05 indicated significance; where several pairwise tests were run, the Bonferroni correction adjusted α.
2.4.2. Descriptive Statistics
Continuous variables (age, BMI, FFSAS scores) are presented as mean ± SD for data that met the Shapiro–Wilk normality criterion (p > 0.05) or as median [IQR] otherwise. Categorical variables (sex, education, place of residence) are shown as counts and percentages.
2.4.3. Phase I – Expert-Rating Statistics
Eleven experts (mean experience = 16.5 years) rated each of the 35 FFSAS items on a 5-point Likert scale across four dimensions (clarity, content validity, linguistic appropriateness, construct representativeness). The highest and lowest score per item were discarded; trimmed means, SD and ranks were calculated in Excel. Items with a trimmed mean < 3.5 were flagged for revision; ties were resolved arithmetically by averaging consecutive ranks (no manual intervention).
2.4.4. Reliability
Internal consistency was assessed with Cronbach’s α for each of the 12 DSM-5 criteria and for the total FFSAS score (35 items, 8-point scale).
2.4.5. Construct Validity
Spearman’s rank-order correlations examined relationships between FFSAS scores (total and criteria) and sweets-related variables: frequency of sweets intake, negative emotions (remorse, guilt, shame, anger) and BMI.
2.4.6. Group Comparisons
Independent t-tests compared total FFSAS scores across four BMI categories—underweight (< 18.5 kg m⁻²), normal (18.5–24.9), overweight (25–29.9) and obese (≥ 30). Bonferroni-adjusted p values are reported.
2.4.7. Factorial Validity
Exploratory factor analysis (EFA) used principal axis factoring with promax rotation; the number of factors was guided by eigenvalues > 1 and the scree-plot elbow. Sampling adequacy was confirmed with the Kaiser–Meyer–Olkin statistic (> 0.80) and Bartlett’s test of sphericity (p < 0.001). The confirmatory factor analysis (CFA) evaluated the hypothesised three-factor model. Model fit was judged acceptable when CFI and TLI > 0.90, RMSEA < 0.08 and χ²/df < 3.0. The missing data were handled by pairwise deletion for descriptive analyses and listwise deletion for multivariate tests.
3. Results
The results are presented in the sections below, which were divided into two phases, Phase 1, presenting the outcomes from The FFSAS Validation by Panel of Expert Judges, followed by Phase 2, showing the Workflow of the study along with responses provided on the FFSAS questionnaire in the pilot with volunteering participants. The presented sample sizes in these samples may differ, what is the result of applying a pair-wise deletion to missing data. Consequently, the effective N differs across analyses and has been detailed in each table and figure.
3.1. Phase I: The FFSAS Validation Results by Panel of Expert Judges
The first phase of the presented study analysis was focused on the expert validation of collected through the FFSAS data on behaviors related to food consumption, along with their perception of feelings associated with sugary foods intakes. The evaluation investigated these information by applying the assessment of different criteria.
For Clarity, item scores ranged from 3.33 (FFSAS15, SD = 1.12) to 4.78 (FFSAS4, FFSAS32, SD < 0.47), with FFSAS4 and FFSAS19 scoring particularly high (> 4.67) and exhibiting low variability. However, FFSAS15 and FFSAS30 scored below 3.5, indicating potential comprehension issues. In terms of Content Validity, scores ranged from 3.33 (FFSAS28, SD = 1.03) to 4.56 (FFSAS4, FFSAS19, SD < 0.69), with FFSAS9 and FFSAS30 being the lowest-scoring items. Other parameters, including Linguistic Appropriateness scores varied from 3.22 (FFSAS21, SD = 1.47) to 4.78 (FFSAS32, SD = 0.47), and Construct Representativeness ranged from 3.22 (FFSAS30, SD = 1.10) to 4.67 (FFSAS19, SD = 0.50). Items consistently scoring below 3.5, such as FFSAS9, FFSAS15, and FFSAS30, were flagged for revision in future iterations of the scale. All items from the FFSAS questionnaire can be found in Supplementary Material (ST1).
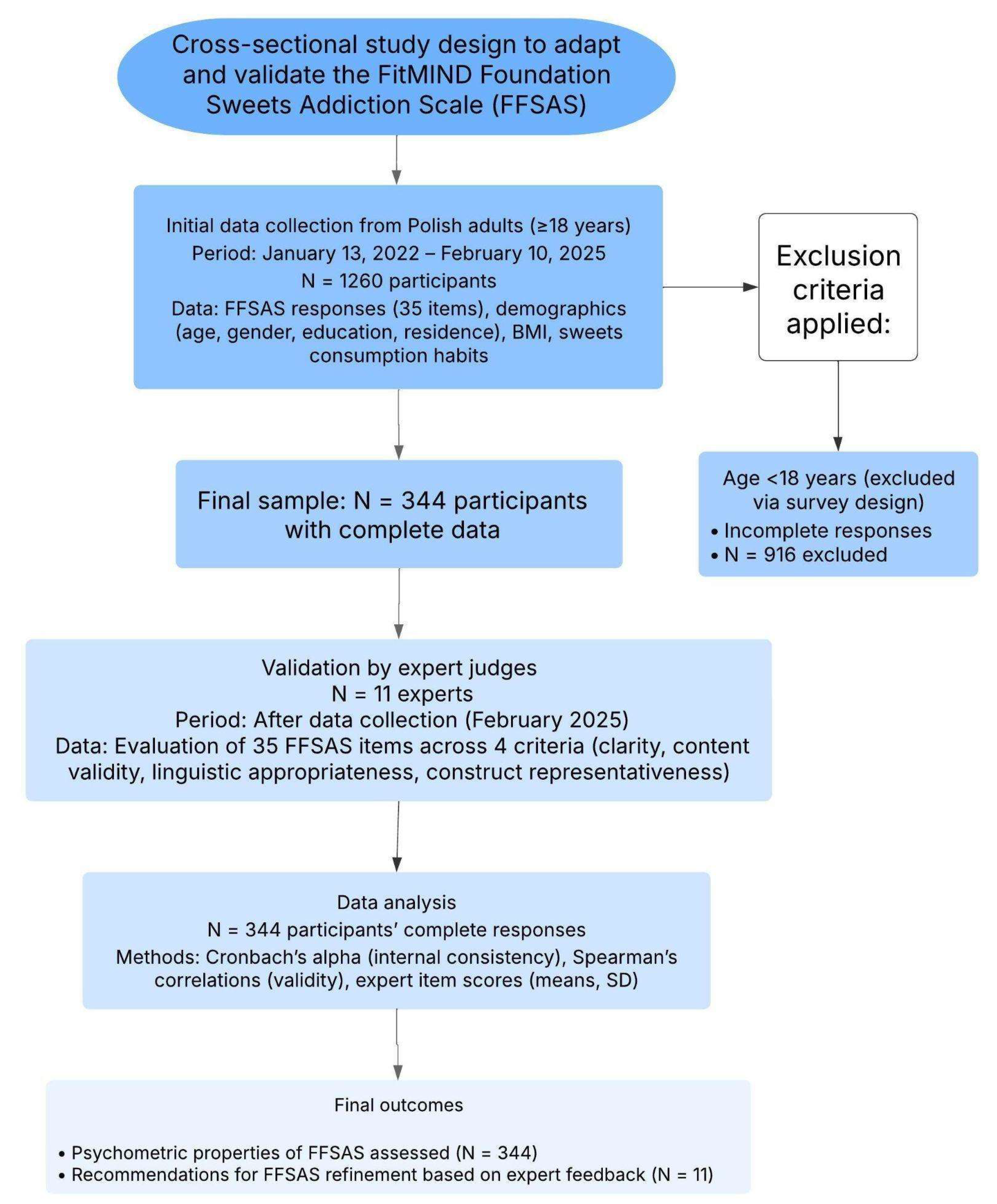
3.2. Phase II: Workflow and Characteristics of Study Participants
Between January 13, 2022, and February 10, 2025, a total of 1260 Polish adults (aged ≥18 years) volunteered to participate in the study by completing the online FFSAS questionnaire via Google Forms. Of these, 916 participants were excluded due to incomplete responses (e.g., missing FFSAS items or demographic data). The study workflow along with the process of participant recruitment is demonstrated in
Figure 1.
The final sample consisted of 344 participants with complete data on demographics, BMI, and sweets consumption habits, which was used for further analysis. This sample size met the requirements for factor analysis, as power calculations estimated a minimum sample size of 100–250 participants [
21].
In this study, a total group of 344 Polish adults, including 270 (78%) women, and a mean age of 40.6 years (range 18-76) voluntarily responded online to the items of the developed FFSAS questionnaire. The demographic and anthropometric characteristics along with sub-group classification of participants are presented in
Table 2.
Briefly, most of the participants in this study had higher education (72%) and resided in large cities with more than 500,000 inhabitants (34%). In this cohort, the mean BMI was 27.86 kg/m2, and 97 people (31%) of responders were classified as obese (BMI ≥ 30 kg/m2).
3.2.1. Self-Reported Responses on Sweets Consumption and Addiction-Like Behaviors
To assess the self-reported behaviors and emotional responses related to sweets consumption, participants responded to items in the FFSAS questionnaire concerning their identification as sweets addicts, admission of addiction, frequency and quantity of sweets intake, cravings or unsuccessful attempts to reduce consumption, and associated feelings of guilt or remorse. These data provide insight into the prevalence and patterns of addiction-like behaviors toward sweets in the total sample (N = 344). Results are summarized in
Table 3.
In this study, most participants perceived their sweets consumption as problematic, with frequent intake and large quantities commonly reported, in contrast to self-reported addiction-like symptoms (e.g., cravings) and emotional distress (e.g., guilt). More than half of responders (62%) identified themselves as addicted to sweets when asked, "Do you identify as addicted to sweets?" while 82 (24%) did not, and 50 (15%) were uncertain ("Don’t know"). When asked directly about admitting addiction (e.g., to themselves or others), 183 (53%) confirmed it, 96 (28%) denied it, 29 (8%) were unsure, and 36 (10%) deemed the question not applicable. In this study, the frequency of sweets consumption was displayed as follows 107 (31%) reported eating sweets several times a day, 64 (19%) once a day, 65 (19%) 3–4 times a week, 37 (11%) 5–6 times a week, 42 (12%) 1–2 times a week, and 29 (8%) less than once a week. In terms of quantity of consumed sweets, 173 participants (50.3%) reported consuming large amounts, and 170 participants (49.4%) reported small amounts.
In contrast, the self-reported behavioral indicators of addiction, such as cravings or unsuccessful attempts to quit, were less frequent in the study as 29 (8%) affirming such experiences, 42 (12%) denying them. The frequency of experiencing emotional states associated with sweets consumption, in particular feelings of guilt or remorse were varied between participants, as 38 (11%) experienced these feelings several times a day, 19 (6%) once a day, 7 (2%) 5–6 times a week, 17 (5%) 3–4 times a week, 21 (6%) 1–2 times a week, 17 (5%) less than once a week, and 7 (2%) never, with 218 (63%) responses missing.
3.2.2. Association Between Sweets Consumption, Sweets Addiction Severity, and Negative Emotions
To further examine whether individuals with high Sweets addiction (SA) severity experience greater emotional distress associated with sweet food intake, the relationship between sweets consumption frequency, SA severity, and negative emotions (e.g., guilt, remorse, shame, or anger) was assessed and results are presented in
Table 2 (sub-sample, N = 126) and
Table 3 (total sample, N = 344). For this analysis, the participants in the total sample were classified into four groups based on the overall FFSAS score: No SA (0–1 symptoms without distress), Mild SA (2–3 symptoms), Moderate SA (4–5 symptoms), and Severe SA (≥6 symptoms, with distress required for SA diagnosis, see
Section 2.1.1). In this analysis two key measures included sweets consumption frequency (
Table 3, total sample, N = 344) and the frequency of negative emotions (
Table 2, sub-sample N = 126), with results displayed in
Figure 2.
3.2.3. Sweets Consumption Frequency and SA Severity
Sweets consumption frequency was assessed in the total sample of 344 participants (
Table 3), in which 62% (n = 213) were classified as No SA, 1% (n = 4) as Mild SA, 1% (n = 4) as Moderate SA, and 36% (n = 123) as Severe SA. Participants with Severe SA had significantly higher consumption rates of sweet foods, with 19% (n = 66) reporting eating sweets ’several times a day’ compared to 12% (n = 40) in the No SA group. In this group was a strong association between sweet food consumption frequency and SA severity (χ² = 85.23, df = 15, p < 0.00001).
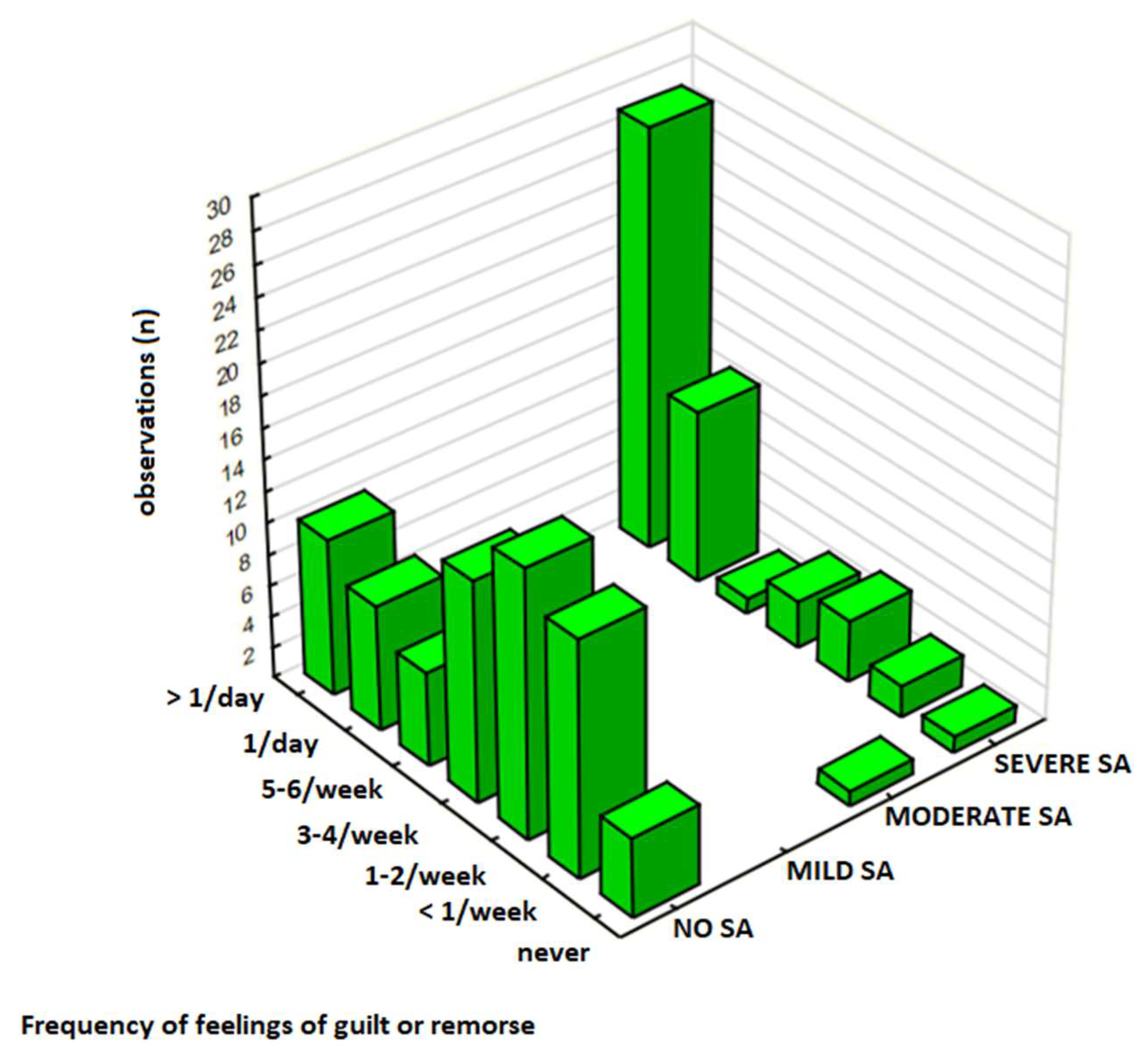
3.2.4. Negative Emotions and SA Severity
The frequency of negative emotions was evaluated in a subgroup of 126 participants (
Table 2), in which 60% (n = 75) were No SA, 1% (n = 1) Mild SA, 1% (n = 1) Moderate SA, and 39% (n = 49) Severe SA. Overall, 30% (n = 38) of participants in this group experienced negative emotions towards sweets consumption ’several times a day,’ including 21% (n = 27) participants with the Severe SA group and 8% (n = 10) in the No SA group. Emotional distress was significantly associated with SA severity (χ², p = 0.00001), particularly among those with Severe SA, as evidenced by a moderate-to-strong positive correlation (γ = 0.629, p < 0.001).
3.3. Association Between Sweets Consumption and Negative Emotions
Participants without SA (No SA) exhibited relatively stable levels of negative emotions across all consumption frequencies, with only 8% (n = 10 out of 75 in the N = 126 subgroup) reporting frequent emotional distress (’several times a day’), even among those consuming sweets daily (10%, n = 36 out of 213 in the N = 344 sample). In contrast, individuals with SA, especially Severe SA, reported a significantly higher prevalence of negative emotions, with the strongest concentration observed among those consuming sweets ’several times a day’. A strong association between frequent sweets intake and emotional distress was observed in this group (χ², p < 0.00001), with 55% (n = 27 out of 49) experiencing negative emotions at the highest frequency.
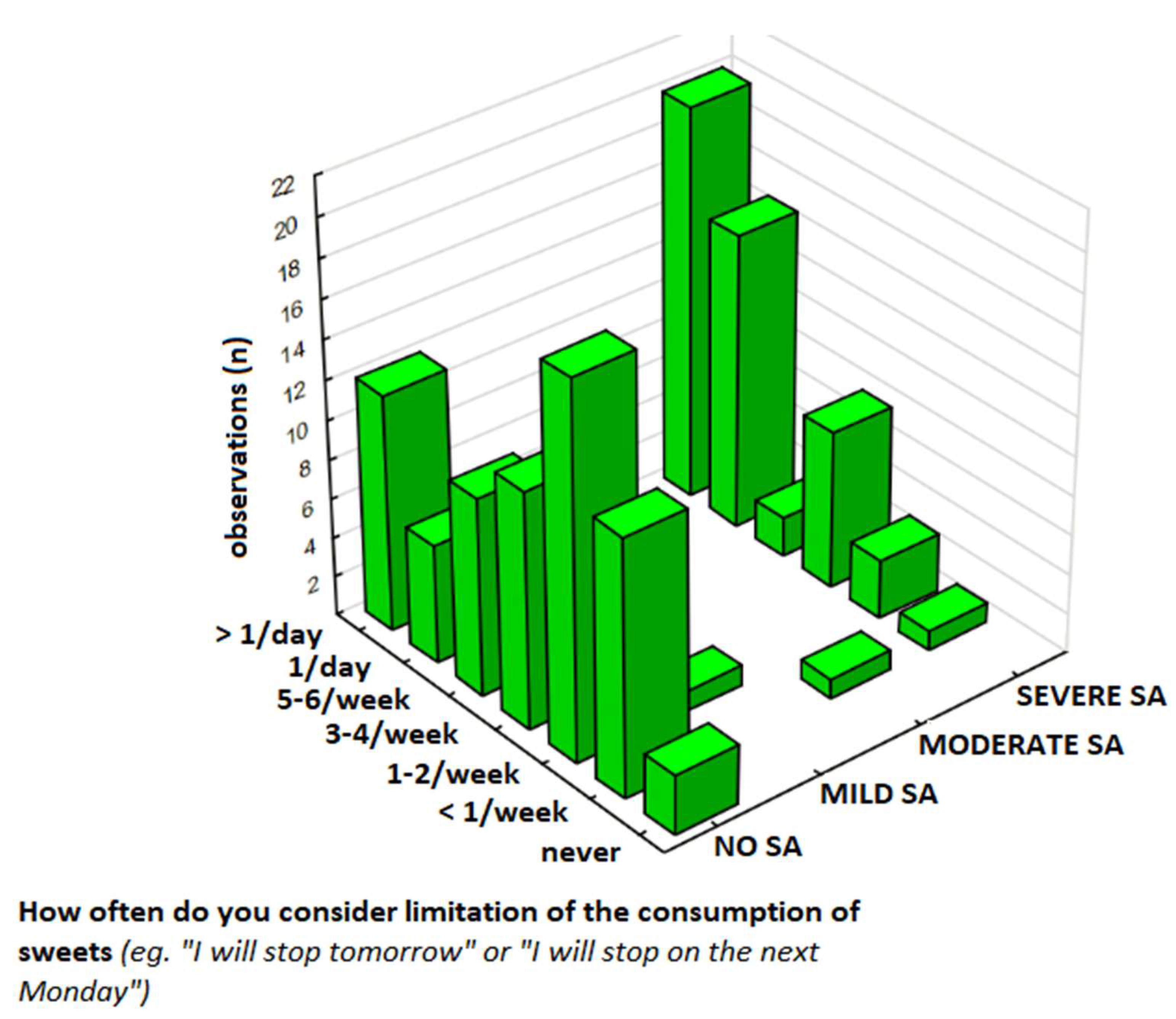
3.4. Patterns of Sweets Restriction Contemplation and Resolution Among Individuals with Sweets Addiction
To assess the individual differences in responses to sweets restriction, including frequency of contemplating sweets restriction, experiencing negative emotions, consumption patterns, and persistent desires or unsuccessful attempts to limit sweets consumption, were compared between the SA and No SA groups based on the scores reported values on a 7-point scale (for frequencies of contemplation, negative emotions, and sweets consumption, 1 = never, 7 = several times a day:
Table 4,
Table 5 and
Table 6) and binary response (for persistent desire or control attempts, Yes/No:
Table 7) in respect to the question on the FFSAS questionnaire, (1) "How often do you experience periods of contemplating restricting sweets? Promise of improvement or resolution ’from tomorrow,’ ’from Monday’?" (contemplation and resolutions) (
Table 4), (2) "How often do you experience remorse, guilt, shame, or anger at yourself related to this?" (negative emotions) (
Table 5), (3) "How often do you eat sweets?" (consumption frequency) (
Table 6), and (4) "Is there a persistent desire or unsuccessful attempts to stop or control eating sweets?" (persistent desire/control attempts) (
Table 7).
The differences in sample sizes across
Table 4,
Table 5,
Table 6 and
Table 7 reflect varying levels of response completeness for specific questionnaire items.
Table 4 and
Table 5 were analyzed in a subgroup of 126 participants who provided full responses to the variables included in these analyses.
Table 6, however, was assessed using the total sample of 344 participants, as all participants responded to the relevant items.
Table 7 was evaluated in a different subgroup of 166 participants who completed all items required for that specific analysis. These variations are due to partial missing data and were handled by conducting each analysis only on participants with complete data for the relevant variables. We recognize that these differences in sample size may be confusing and have now clarified them in the manuscript to ensure transparency and reproducibility.
3.5.1. Contemplation, Resolutions, and Negative Emotions
The frequency of contemplating sweets restriction and making resolutions was analyzed in the subgroup of the sample (N = 126), and the results presented on
Table 4. The results have shown that 60% (n = 75) participants had No SA, 1% (n = 1) as Mild SA, 1% (n = 1) as Moderate SA, and 39% (n = 49) as Severe SA. Notably, 30% of respondents experienced negative emotions ’several times a day,’ predominantly among those with Severe SA (21%, n = 27). The Severe SA group reported the highest frequency of the contemplating sweet restriction, with 16% (n = 20) doing this ’several times a day,’ compared to 10% (n = 12) in the No SA group. In this group the contemplation frequency was positively correlated with SA severity (p < 0.001).
Similarly, the frequency of negative emotions was significantly higher in participants with SA compared to those with No SA (
Table 5). In this subgroup (N = 126), 30% (n = 38) responders experienced feelings of remorse, guilt, shame, or anger ‘several times a day,’ including 21% (n = 27) in the Severe SA group and 8% (n = 10) in the No SA group (
Figure 3). Statistical analysis revealed a strong association between SA severity and the frequency of experiencing negative emotions (p = 0.00001) and a moderate-to-strong correlation between these variables (p < 0.001).
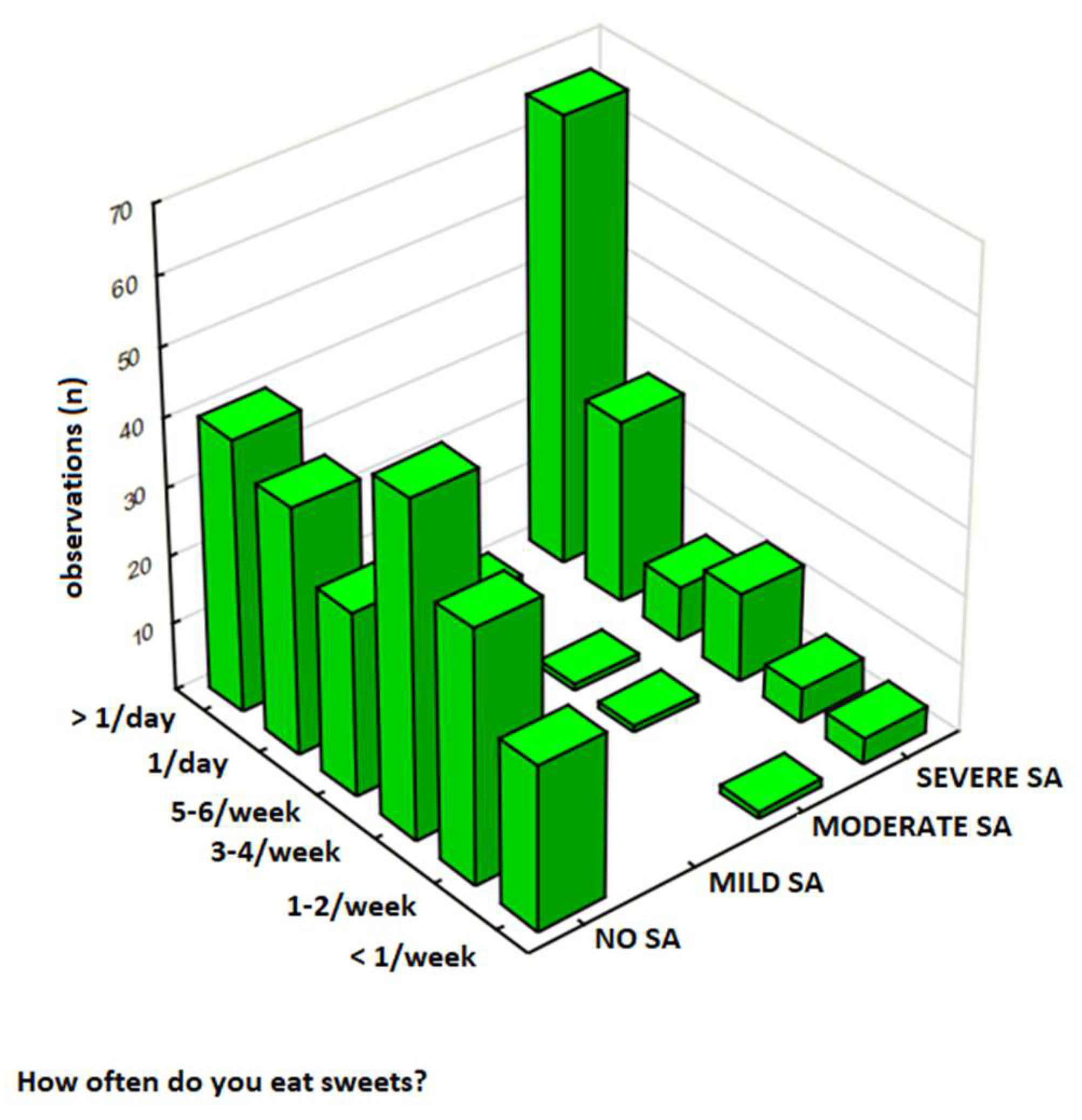
3.4.2. The Frequency of Sweet Food Consumption
The frequency of sweet food consumption was analyzed in a total sample of 344 participants, and results are presented in
Table 6. In this group, 62% (n = 213) of respondents were classified as No SA, 1% (n = 4) as Mild SA, 1% (n = 4) as Moderate SA, and 36% (n = 123) as Severe SA. Participants with Severe SA had significantly higher consumption rates, with 19% (n = 66) eating sweets ‘several times a day’ compared to 12% (n = 40) in the No SA group. Notably, 31% of respondents reported sweet food intake ’several times a day,’ with this behavior most frequent among those with Severe SA (19%, n = 66) compared to No SA (12%, n = 40) (
Figure 4). In this analysis, there was a strong relationship between SA severity and the frequency of sweets consumption (p < 0.00001) and a moderate positive correlation between these variables (γ = 0.544, p < 0.001).
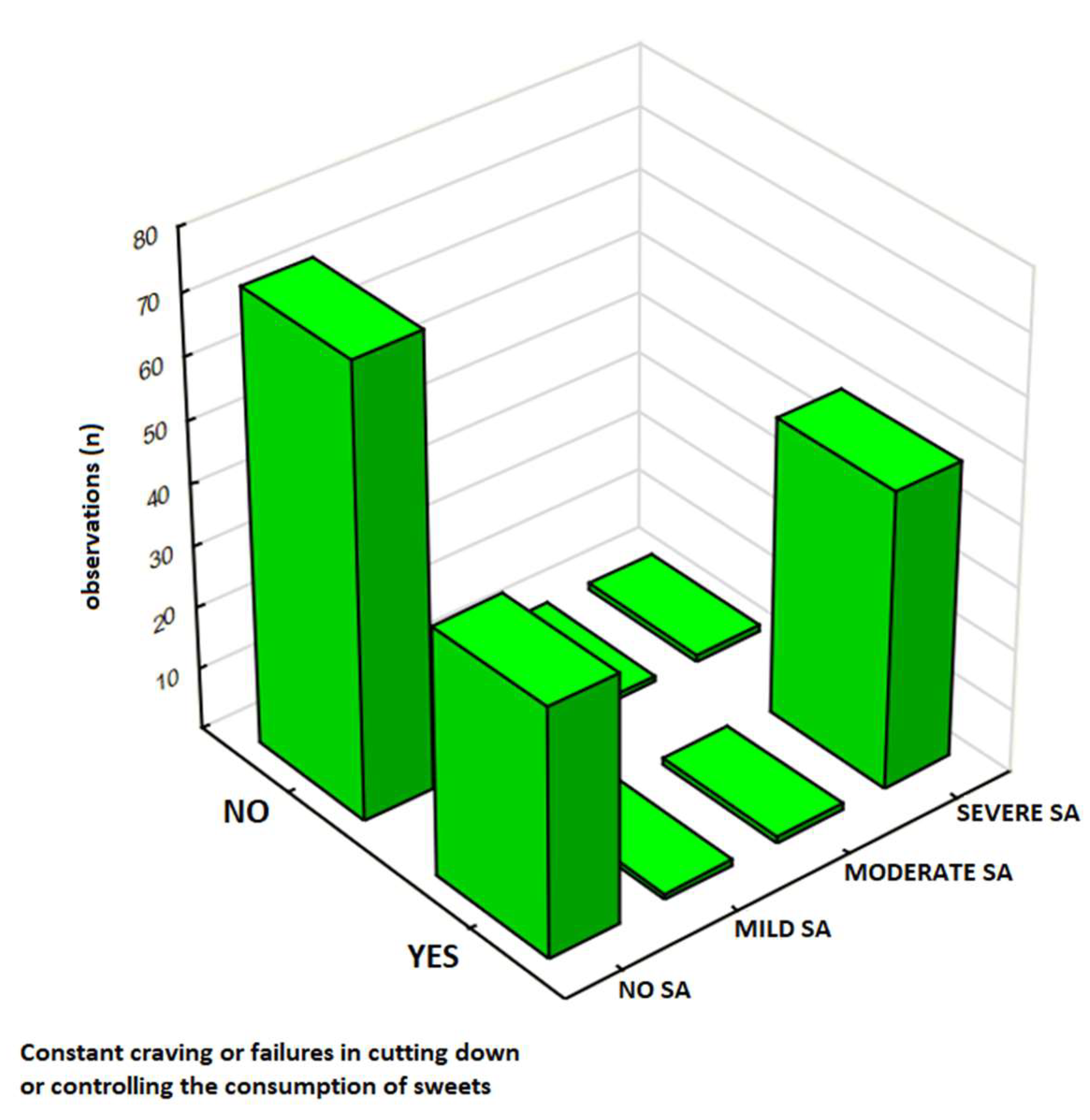
3.4.3. The Persistent Desire and Control Attempts
The persistent desire and unsuccessful attempts to control sweet food consumption was analyzed in a sub-sample of 166 respondents, and results are presented in
Table 7. Participants were classified by SA severity: 68% (n = 113) as No SA, 1% (n = 2) as Mild SA, 1% (n = 2) as Moderate SA, and 30% (n = 49) as Severe SA. The results show that 54% (n = 90) reported ‘Yes,’ including 29% (n = 48) in the Severe SA group compared to 24% (n = 40) in the No SA group. Notably, 54% (n = 90) of respondents in this study agreed to experience persistent desire or unsuccessful attempts to control sweets intake, with this response markedly higher among those with Severe SA (29%, n = 48) compared to No SA (24%, n = 40). In this analysis there was a significant association between SA severity and the presence of persistent desire or unsuccessful control attempts to control eating sweets (p < 0.00001).
3.5. Assessment of the FFSAS Reliability and Internal Consistency
To assess the internal consistency of the FFSAS based on the preliminary data collected from the Polish population, Cronbach’s alpha (α) was computed for each of the 12 criteria evaluated by the questionnaire (
Table 8). Overall, the FFSAS demonstrated strong internal consistency and reliability with the overall α = 0.85, nevertheless, these values varied across different subscales, from 0.43 to 0.92. The high internal consistency was reported for Criterion 3, ’Excessive Time Spent’, which assess the amount of time dedicated to obtaining, consuming, or thinking about sweets, demonstrating particularly high reliability (α = 0.916). This criterion was assessed through items such as “Spędziłem/am dużo czasu na jedzeniu przez cały dzień” (FFSAS9) and “Kiedy słodycze były niedostępne, byłem/am w stanie zrobić wiele, aby je zdobyć” (FFSAS10). Similarly, Criterion 7, ‘Withdrawal Symptoms’, evaluating the physical and emotional symptoms experienced after reducing sweets intake, showed strong internal consistency (α = 0.914). This subscale included five items such as “Kiedy ograniczałem/am lub zaprzestałem/am jedzenia słodyczy, czułem/am się poirytowany/a, nerwowy/a lub smutny/a” (FFSAS19) and “Kiedy ograniczałem/am lub zaprzestałem/am jedzenia słodyczy, miałem/am dolegliwości fizyczne” (FFSAS22).
In contrast, Criterion 10, ’Use in Hazardous Situations’, determining whether participants consume or think about sweets in contexts that could lead to physical harm, showed lower internal consistency (α = 0.430). Items like “Byłem/am tak rozkojarzony/a przez spożywanie jedzenia, że mógłbym/mogłabym ulec wypadkowi” (FFSAS30) and “Byłem/am tak rozkojarzony/a przez myślenie o jedzeniu, że mógłbym/mogłabym ulec wypadkowi” (FFSAS31) yielded a weak alpha value, suggesting that these items may not consistently reflect hazardous behavior in this population. Also, Criterion 11, ‘Craving’, measuring the intensity and frequency of overwhelming urges to consume sweets, demonstrated weak internal consistency (α = 0.520).
Correlation Between the FFSAS Scores and Behavioral and Emotional Indicators of Sweets Addiction
To further explore the associations between the obtained FFSAS scores and self-reported behavioral and emotional measures the series of correlations were executed, and results are presented in
Table 9. In this study, significant positive associations were reported between FFSAS scores and several self-reported behaviors and emotional responses related to sweets consumption. Specifically, FFSAS scores were moderately correlated with self-identified sweets addiction (ρ = 0.38, p < 0.05) and frequency of sweets consumption (ρ = 0.3919, p < 0.05). A similar pattern was observed with feelings of guilt or remorse (ρ = 0.3497, p < 0.05), as higher the FFSAS scores were associated with stronger emotional distress regarding sweets consumption. Furthermore, the number of days per week with sweets consumption was strongly correlated with FFSAS scores (p < 0.05).
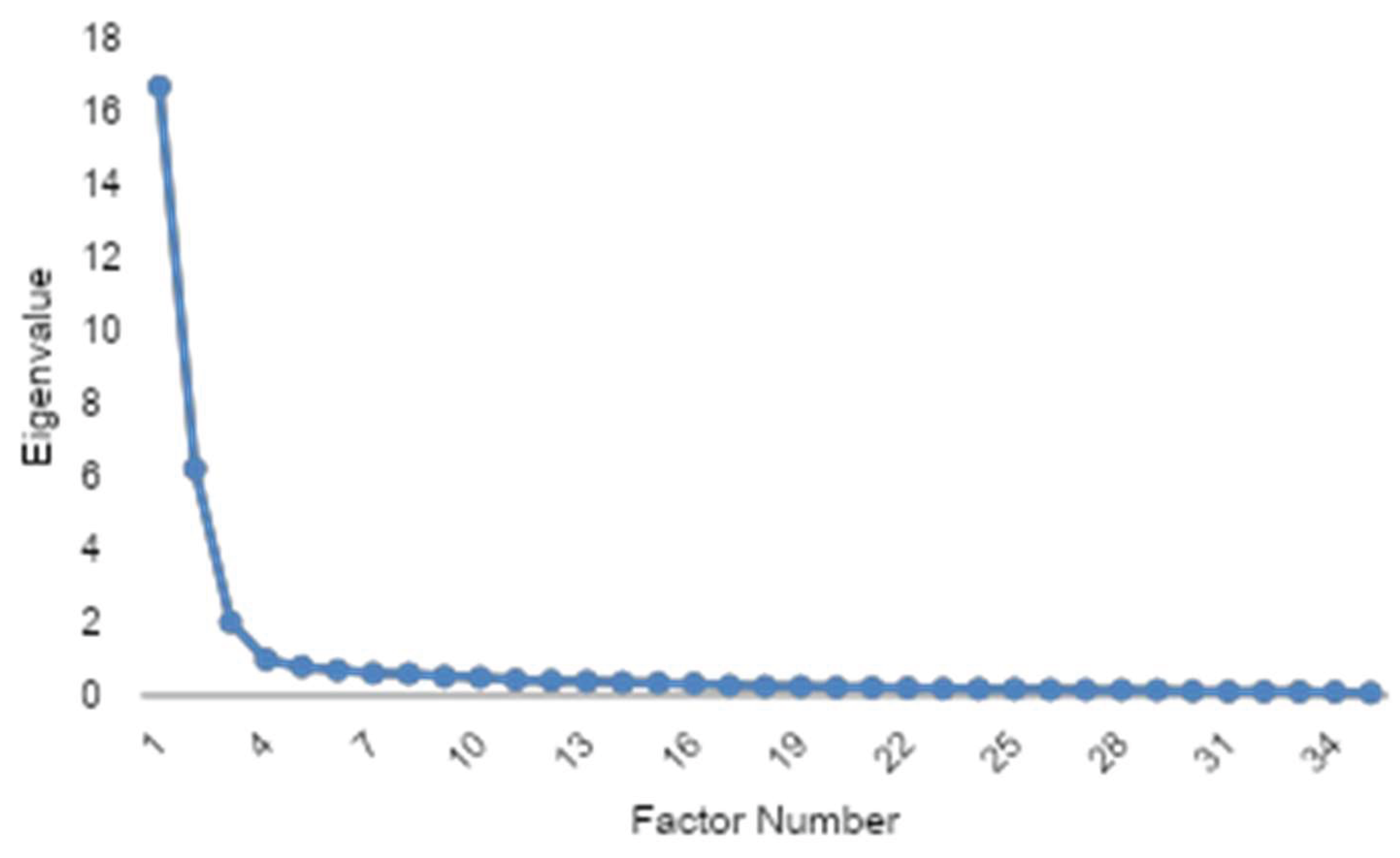
3.6. Preliminary Validation and Factor Extraction of the FFSAS questionnaire
To evaluate the structure of the FFSAS and ensure its psychometric properties, an EFA was conducted. Briefly, applied Kaiser-Meyer-Olkin measure (KMO = 0.956) demonstrated excellent sampling adequacy, and Bartlett’s test of sphericity was highly significant (p < 0.001), confirming robust inter-item correlations and validating the dataset’s suitability for factor analysis. The number of factors was determined via the scree plot elbow criterion, which indicated a three-factor solution as the optimal point where eigenvalues began to level off sharply after the third component (
Figure 6). The communality analysis revealed a high average communality of 0.686, with no variables below the 0.4 threshold and only one variable falling below 0.5, indicating that nearly all items were well-represented by the extracted factors.
The EFA revealed a robust three-factor structure (68.6% variance explained). 37% of items exhibited cross-loadings, primarily between craving and loss-of-control constructs, suggesting nuanced interrelationships in sugar addiction phenotypes (
Table 10). All three factors demonstrated exceptional internal consistency (Cronbach’s α = 0.951–0.962), though the high reliability coefficients and factor loadings above 0.90 for 18-item scales suggest potential item redundancy, necessitating future scale refinement to eliminate overlapping constructs while retaining psychometric robustness.
A CFA was subsequently conducted to validate the hypothesized factor structure, with the model explicitly defined according to the theoretical framework of the FFSAS, which operationalizes 12 diagnostic criteria. The CFA results demonstrated suboptimal fit (CFI = 0.74, TLI = 0.69, RMSEA = 0.14), prompting a potential reassessment of the FFSAS’s theoretical structure and necessitating item-level revisions to address cross-loadings and improve factorial validity. The statistically significant chi-square (χ² = 3761.76, p < 0.001) confirmed model-data misfit, consistent with not perfect fit indices, necessitating post hoc model modifications to better align with the empirical covariance structure (
Table 11). CFA revealed that, while several items loaded strongly onto their intended factors (e.g., FFSAS1 on CR01 and FFSAS5 on CR03 both with loadings of 1.0), some parameters exhibited atypically high values, such as FFSAS12 (loading = 63.44 on CR07) and FFSAS35 (loading = 21.46 on CR08), which may indicate estimation or model specification issues. A few items, including FFSAS9, demonstrated substantial cross-loadings, suggesting some overlap between latent constructs. Additionally, certain items, such as FFSAS33 (loading = 0.39 on CR10) and FFSAS34 (loading = 0.25 on CR10), showed relatively low factor loadings, which could reflect weaker associations with their respective factors. Despite these observations, the overall pattern of loadings provides valuable insights into the factorial structure of the scale and highlights areas for potential refinement. These results suggest that further review of specific items and possible model adjustments may enhance the psychometric properties and theoretical alignment of the instrument [
43].
4. Discussion
Therefore, the primary objective of this study was to evaluate the factor structure, psychometric properties, and external validation of the newly developed FFSAS, aimed at assessing sweets addiction. This scale, as adaptation of the YFAS 2.0 dedicated to identify addictive-like behaviors related to sweet food consumption in the general adult Polish population, demonstrated good overall reliability (α = 0.85) and moderate correlations with self-reported frequency of sweets intake (ρ = 0.39) and feeling of guilt upon their consumption (ρ = 0.35), thereby indicating FFSAS ability to identify the alerted eating habits linked to specifically UPFs rich in added sugar. Results of this pilot study using FFSAS indicated that a higher frequency of contemplating restriction and making resolutions among participants with SA were associated with the cycle of addiction, supporting the validity of FFSAS. Furthermore, the validation identified items of the FFSAS (e.g., FFSAS9, FFSAS15, FFSAS30) for refinement due to weaker subscales (α < 0.60), suggesting future iterations could enhance psychometric properties.
Exploratory factor analysis (EFA) revealed a robust three-factor structure, explaining 68.6% of the variance, with excellent internal consistency (Cronbach’s α = 0.951–0.962) across factors corresponding to constructs such as craving and loss of control. However, 37% of items showed cross-loadings, particularly between craving and loss-of-control constructs, and some items (e.g., FFSAS35, communality = 0.43) exhibited low communality, indicating potential redundancy or weak factor representation. Confirmatory factor analysis (CFA) showed suboptimal model fit (CFI = 0.74, TLI = 0.69, RMSEA = 0.14, χ² = 3761.76, p < 0.001), with some items displaying atypically high loadings (e.g., FFSAS12 = 63.44, FFSAS35 = 21.46) or low loadings (e.g., FFSAS33 = 0.39, FFSAS34 = 0.25), suggesting estimation issues or construct overlap. These findings highlight the need for item-level revisions to improve factorial validity and reduce redundancy, providing a foundation for refining the FFSAS in future studies.
Compared to prior studies, FFSAS aligns with YFAS 2.0 findings, where approximately 15–20% of community samples meet food addiction criteria, with higher rates in females and overweight individuals [
22,
26]. In this study, comprising 78% females with a mean BMI of 27.86 kg/m², reflects these demographics, and the 62% self-identification as sweets-addicted (
Table 2) underscores the scale’s relevance for sugar-focused compulsive eating. While the FFSAS shows promise in capturing sweets-specific addiction behaviors, the variability in item clarity and construct representativeness aligns with challenges seen in validating other food addiction scales, resultant from complexity of defining food addiction and the inconsistencies in scale performance across different populations[
27]. Series of correlation analyses between FFSAS items unraveling moderate associations with self-reported sweet food consumption frequency is consistent with other studies which suggest that food addiction constructs may not directly translate to simple consumption measures [
28]. In addition, significant associations between feeling of guilt and emotional distress related to sweet food intake reported in this study, provides early evidence supporting the notion that psychological factors play a crucial role in addictive-like eating behaviors, linking emotional dysregulation to excessive food intake [
29]. Unlike general food addiction tools, FFSAS’s specificity to UPFs rich in added sugar may detect problematic alerted eating behaviors missed by broader measures, consistent with research highlighting sugar-rich foods as key triggers of addictive-like eating and contributor to metabolic disturbances [
30].
Although the exact mechanisms through which addictive-like behaviors arise from regular consumption of sweet food in large amounts under psychological triggers like negative emotional states and stress—remain unclear, experimental evidence suggests that excessive sweet intake activates dopamine reward pathways, paralleling drug addiction [
19]. Animal studies have shown that sugar bingeing leads to tolerance and withdrawal, with dopamine receptor downregulation resembling substance dependence [
31]. Neuroimaging studies with human participants have supported this, indicating a possible role of reward responses to sweet cues in food-addicted individuals [
22,
32,
33]. These findings collectively support the involvement of neurobiological pathways in certain types of dependence on sugary foods, including urgency of cravings and loss of control [
32,
33,
34].
The FFSAS scale was created based on a combination of psychological theories and eating behavior research, making it essential to evaluate its validity and reliability in non-clinical settings to ensure suitability for general populations [
27]. Given that sweets addiction is associated with various psychological and behavioral factors, including emotional eating, impulsivity, and compulsive consumption [
28,
29,
35,
36], it is crucial to examine how effectively the FFSAS reflects these constructs. Consequently, the second part of this study focused on validation, which confirmed the clarity, content validity, linguistic appropriateness, and construct representativeness of the FFSAS questionnaire. Items FFSAS4 and FFSAS19 received the highest clarity scores, indicating strong conceptual representation, while FFSAS15 and FFSAS30 were rated lower, suggesting a need for revision. Similar trends were observed in content validity and construct representativeness, with items such as FFSAS28 and FFSAS30 scoring lower, highlighting areas for improvement. These findings are consistent with previous food addiction research on tools like the mYFAS 2.0, which also showed variability in factor structures depending on the population and cultural context [
37,
38,
39].
Furthermore, our results indicate that higher FFSAS scores were associated with emotional distress and impulsive eating behaviors, aligning with existing literature linking sweet food addiction to emotional dysregulation and stress [29, 35, [
40]. This supports the scale’s utility in identifying individuals at risk for maladaptive eating patterns, such as compulsive consumption and loss of control over sweets intake [
22]. Notably, items related to behavioral patterns received higher expert ratings than those addressing emotional implications, suggesting that the scale currently places greater emphasis on observable behaviors. This distinction mirrors findings in other research on behavioral versus emotional components of addiction [
40,
41]. Future development of the FFSAS should consider enhancing its capacity to capture both dimensions, thereby improving its diagnostic depth and applicability in diverse psychological contexts.
There are several limitations to this study. Firstly, the sample was limited in size and dominated by females and overweight individuals, which may affect the generalizability of the findings to a broader population. We acknowledge that a larger sample could enhance result interpretation. Additionally, relying on self-reported data for sweets consumption, emotional responses, and body measurements may lead to recall bias, as participants might misreport their behaviors or characteristics due to memory errors or social desirability. Future research should aim to include more diverse samples, including individuals of different ages, genders, and cultural backgrounds, to ensure the scale’s applicability across different populations. Additionally, the expert panel validation revealed variability in ratings for several items, which indicates that some items may need revision to enhance their clarity and relevance. The low clarity scores for items such as FFSAS15 and FFSAS30 suggest that future iterations of the FFSAS should focus on improving these items to ensure better comprehension. Moreover, the sampling method, which was based on expert evaluations, may introduce selection bias, limiting the generalizability of the results. The cross-sectional design limits causal inferences, and focusing solely on sweets excludes other food categories. Lastly, although the FFSAS scale was externally validated by an expert panel, further confirmatory factor analyses (CFA) and reliability testing in larger and more diverse samples are necessary to fully assess its construct validity and internal consistency. Future research should employ longitudinal designs to assess predictive validity, validate FFSAS in clinical populations (e.g., obesity, eating disorders), and conduct factor analysis to confirm its structure.
In summary, the FFSAS offers a promising tool for assessing sweets-specific addiction in particularly overweight women with good initial validity. Future research should refine the scale’s structure and its usability in the larger and diverse populations. Clinically, the FFSAS can aid in identifying individuals at risk, enabling tailored interventions like psychodietetics counseling and behavioral therapy for sugar cravings, contributing to improved patient outcomes and public health strategies.
5. Conclusions
In summary, this pilot study presents strong preliminary evidence supporting the validity and reliability of the FFSAS, as Polish adaptation of the YFAS 2.0 tailored to assess addiction-like behaviors specifically related to sweets consumption. The scale demonstrated solid internal consistency and construct validity, with clear associations to self-reported patterns of excessive intake, intense cravings, and guilt. Its targeted focus on sweet foods offers a distinct advantage over broader food addiction instruments, enabling more precise identification of individuals particularly vulnerable to high-sugar dietary patterns. These findings position the FFSAS as a valuable and contextually relevant tool for both research and early intervention in the field of eating psychology. Nevertheless, continued validation in larger, more diverse, and clinical populations will be essential to fully establish its utility across settings and to inform public health strategies addressing the growing burden of ultra-processed, sugar-rich food consumption.
Supplementary Materials
The following supporting information can be downloaded at the website of this paper posted on Preprints.org.
Author Contributions
Conceptualization, M.C.; methodology, M.C. and A.S.; software, A.S. and S.M.; validation, A.S, K.H and S.M.; formal analysis, J.J., A.S, K.H. and S.M.; investigation, M.C.; resources, M.C., J.J and A.S.; data curation, M.C. and A.S.; writing—original draft preparation, M.C.; writing—review and editing, J.J., H.C-M., T.A.; visualization, A.S., J.J.; supervision, A.S. J.J.; project administration, M.C. and J.J. All authors have read and agreed to the published version of the manuscript.
Funding
This research was partially supported by the internal Wroclaw Medical University Grant, number: SUBK.E140.25.016
Institutional Review Board Statement
This study was approved by the Ethics Committee of Silesia Medical University (protocol code PCN/CBN/0022/KB/291/21, approved January 01, 2022) and conducted in accordance with the Declaration of Helsinki.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The dataset used during the current study is available from the corresponding author on reasonable request.
Acknowledgments
We express our gratitude to the panel of 11 expert judges for their valuable time and expertise in evaluating the FFSAS items, contributing to the refinement of the scale. We also sincerely thank all participants who voluntarily completed the online questionnaires, making this study possible through their generous involvement.
Conflicts of Interest
Mikołaj Choroszyński is the author of the book Uzależnienie od słodyczy (Sweets Addiction) (2020), which discusses the concept of sweets addiction. He did not receive any additional financial support for this publication. The other authors (J.J., T.A., S.M., A.S., H.C-M.) declare no conflicts of interest. The research was conducted independently, and the book did not influence the study design, data collection, or interpretation of results.
References
- N. W. S. Chew et al., ‘The global burden of metabolic disease: Data from 2000 to 2019’, Cell Metabolism, vol. 35, no. 3, pp. 414-428.e3, Mar. 2023. [CrossRef]
- A. Monda et al., ‘Ultra-Processed Food Intake and Increased Risk of Obesity: A Narrative Review’, Foods, vol. 13, no. 16, p. 2627, Aug. 2024. [CrossRef]
- S. J. Dicken and R. L. Batterham, ‘The Role of Diet Quality in Mediating the Association between Ultra-Processed Food Intake, Obesity and Health-Related Outcomes: A Review of Prospective Cohort Studies’, Nutrients, vol. 14, no. 1, p. 23, Dec. 2021. [CrossRef]
- L. C. Tapsell, E. P. Neale, A. Satija, and F. B. Hu, ‘Foods, Nutrients, and Dietary Patterns: Interconnections and Implications for Dietary Guidelines’, Advances in Nutrition, vol. 7, no. 3, pp. 445–454, May 2016. [CrossRef]
- L. Schwingshackl, J. Morze, and G. Hoffmann, ‘Mediterranean diet and health status: Active ingredients and pharmacological mechanisms’, British J Pharmacology, vol. 177, no. 6, pp. 1241–1257, Mar. 2020. [CrossRef]
- A. Nani, B. Murtaza, A. Sayed Khan, N. A. Khan, and A. Hichami, ‘Antioxidant and Anti-Inflammatory Potential of Polyphenols Contained in Mediterranean Diet in Obesity: Molecular Mechanisms’, Molecules, vol. 26, no. 4, p. 985, Feb. 2021. [CrossRef]
- G. Augimeri et al., ‘Potential Antioxidant and Anti-Inflammatory Properties of Serum from Healthy Adolescents with Optimal Mediterranean Diet Adherence: Findings from DIMENU Cross-Sectional Study’, Antioxidants, vol. 10, no. 8, p. 1172, Jul. 2021. [CrossRef]
- M. Bucciantini, M. Leri, P. Nardiello, F. Casamenti, and M. Stefani, ‘Olive Polyphenols: Antioxidant and Anti-Inflammatory Properties’, Antioxidants, vol. 10, no. 7, p. 1044, Jun. 2021. [CrossRef]
- J. Ferreira, M. Bicho, and F. Serejo, ‘ABCA1 Polymorphism R1587K in Chronic Hepatitis C Is Gender-Specific and Modulates Liver Disease Severity through Its Influence on Cholesterol Metabolism and Liver Function: A Preliminary Study’, Genes, vol. 13, no. 11, p. 2095, Nov. 2022. [CrossRef]
- L. Maldonado-Pereira, C. Barnaba, and I. G. Medina-Meza, ‘Oxidative Status of Ultra-Processed Foods in the Western Diet’, Nutrients, vol. 15, no. 23, p. 4873, Nov. 2023. [CrossRef]
- V. J. Clemente-Suárez, A. I. Beltrán-Velasco, L. Redondo-Flórez, A. Martín-Rodríguez, and J. F. Tornero-Aguilera, ‘Global Impacts of Western Diet and Its Effects on Metabolism and Health: A Narrative Review’, Nutrients, vol. 15, no. 12, p. 2749, Jun. 2023. [CrossRef]
- J.-S. Shim, ‘Ultra-Processed Food Consumption and Obesity: A Narrative Review of Their Association and Potential Mechanisms’, Journal of Obesity & Metabolic Syndrome, vol. 34, no. 1, pp. 27–40, Jan. 2025. [CrossRef]
- L. S. Grinshpan, S. Eilat-Adar, D. Ivancovsky-Wajcman, R. Kariv, M. Gillon-Keren, and S. Zelber-Sagi, ‘Ultra-processed food consumption and non-alcoholic fatty liver disease, metabolic syndrome and insulin resistance: A systematic review’, JHEP Reports, vol. 6, no. 1, p. 100964, Jan. 2024. [CrossRef]
- F. A. Shahatah, T. R. Hill, A. Fairley, and A. W. Watson, ‘Ultra-Processed Food Intakes and Health Outcomes in Adults Older Than 60 Years: A Systematic Review’, Nutrition Reviews, p. nuae223, Jan. 2025. [CrossRef]
- M. M. Lane et al., ‘Ultra-processed food exposure and adverse health outcomes: umbrella review of epidemiological meta-analyses’, BMJ, p. e077310, Feb. 2024. [CrossRef]
- C. Li et al., ‘High dietary Fructose Drives Metabolic Dysfunction-Associated Steatotic Liver Disease via Activating ubiquitin-specific peptidase 2/11β-hydroxysteroid dehydrogenase type 1 Pathway in Mice’, Int. J. Biol. Sci., vol. 20, no. 9, pp. 3480–3496, 2024. [CrossRef]
- B. Geidl-Flueck and P. A. Gerber, ‘Fructose drives de novo lipogenesis affecting metabolic health’, Journal of Endocrinology, vol. 257, no. 2, p. e220270, Feb. 2023. [CrossRef]
- D. A. Wiss and E. M. LaFata, ‘Ultra-Processed Foods and Mental Health: Where Do Eating Disorders Fit into the Puzzle?’, Nutrients, vol. 16, no. 12, p. 1955, Jun. 2024. [CrossRef]
- S.-J. Leigh and M. J. Morris, ‘The role of reward circuitry and food addiction in the obesity epidemic: An update’, Biological Psychology, vol. 131, pp. 31–42, Jan. 2018. [CrossRef]
- D. Olczak-Kowalczyk, A. Turska, D. Gozdowski, and U. Kaczmarek, ‘Dental caries level and sugar consumption in 12-year-old children from Poland’, Adv Clin Exp Med, vol. 25, no. 3, pp. 545–550, Jun. 2016. [CrossRef]
- E. Anthoine, L. Moret, A. Regnault, V. Sébille, and J.-B. Hardouin, ‘Sample size used to validate a scale: a review of publications on newly-developed patient reported outcomes measures’, Health Qual Life Outcomes, vol. 12, no. 1, p. 2, Dec. 2014. [CrossRef]
- A. N. Gearhardt, W. R. Corbin, and K. D. Brownell, ‘Development of the Yale Food Addiction Scale Version 2.0.’, Psychology of Addictive Behaviors, vol. 30, no. 1, pp. 113–121, Feb. 2016. [CrossRef]
- R. Wojciech Poprawa, B. Lewandowska, M. Włodarczyk, and K. Tutka, ‘A Polish adaptation and validation of the Yale Food Addiction Scale 2.0’, ain, vol. 33, no. 4, pp. 283–312, 2020. [CrossRef]
- C. E. Gasser, F. K. Mensah, M. Russell, S. E. Dunn, and M. Wake, ‘Confectionery consumption and overweight, obesity, and related outcomes in children and adolescents: a systematic review and meta-analysis’, The American Journal of Clinical Nutrition, vol. 103, no. 5, pp. 1344–1356, May 2016. [CrossRef]
- M. Czarnecki, ‘Metodyka pracy z sędziami kompetentnymi w procesie opracowywania skali do pomiaru konstruktów: rekomendacje i egzemplifikacja’, PO, pp. 13–18, Dec. 2020. [CrossRef]
- K. Pursey, P. Stanwell, A. Gearhardt, C. Collins, and T. Burrows, ‘The Prevalence of Food Addiction as Assessed by the Yale Food Addiction Scale: A Systematic Review’, Nutrients, vol. 6, no. 10, pp. 4552–4590, Oct. 2014. [CrossRef]
- E. Van Hagen, ‘“A Salisbury steak is not a steak, it’s ground beef.” The significance, messages and symbolism of final meals on death row’, Appetite, vol. 144, p. 104445, Jan. 2020. [CrossRef]
- A. J. Burnett, K. E. Lamb, A. C. Spence, K. E. Lacy, and A. Worsley, ‘Associations between feeding practices and child dietary quality, and the moderating effect of child eating behaviours on these associations’, Eating Behaviors, vol. 43, p. 101569, Dec. 2021. [CrossRef]
- A. Hammami et al., ‘Social modeling of vegetarian food choices’, Appetite, vol. 157, p. 104867, Feb. 2021. [CrossRef]
- K. J. Melanson, T. J. Angelopoulos, V. Nguyen, L. Zukley, J. Lowndes, and J. M. Rippe, ‘High-fructose corn syrup, energy intake, and appetite regulation’, The American Journal of Clinical Nutrition, vol. 88, no. 6, pp. 1738S-1744S, Dec. 2008. [CrossRef]
- N. M. Avena, ‘The study of food addiction using animal models of binge eating’, Appetite, vol. 55, no. 3, pp. 734–737, Dec. 2010. [CrossRef]
- X. Meng, D. Huang, H. Ao, X. Wang, and X. Gao, ‘Food cue recruits increased reward processing and decreased inhibitory control processing in the obese/overweight: An activation likelihood estimation meta-analysis of fMRI studies’, Obesity Research & Clinical Practice, vol. 14, no. 2, pp. 127–135, Mar. 2020. [CrossRef]
- E. M. Schulte, S. Yokum, A. Jahn, and A. N. Gearhardt, ‘Food cue reactivity in food addiction: A functional magnetic resonance imaging study’, Physiology & Behavior, vol. 208, p. 112574, Sep. 2019. [CrossRef]
- S. Lewis, ‘Melatonin influence on circadian rhythms’, Nat Rev Neurosci, vol. 17, no. 1, pp. 4–4, Jan. 2016. [CrossRef]
- P. Premkumar, J. Onwumere, L. Betts, F. Kibowski, and E. Kuipers, ‘Schizotypal traits and their relation to rejection sensitivity in the general population: Their mediation by quality of life, agreeableness and neuroticism’, Psychiatry Research, vol. 267, pp. 201–209, Sep. 2018. [CrossRef]
- P. Sweeney, R. Levack, J. Watters, Z. Xu, and Y. Yang, ‘Caffeine increases food intake while reducing anxiety-related behaviors’, Appetite, vol. 101, pp. 171–177, Jun. 2016. [CrossRef]
- N. R. Fisher, B. R. Mead, P. Lattimore, and P. Malinowski, ‘Dispositional mindfulness and reward motivated eating: The role of emotion regulation and mental habit’, Appetite, vol. 118, pp. 41–48, Nov. 2017. [CrossRef]
- J. L. P. Chia, M. Fuller-Tyszkiewicz, K. Buck, K. Chamari, B. Richardson, and I. Krug, ‘An ecological momentary assessment of the effect of fasting during Ramadan on disordered eating behaviors’, Appetite, vol. 127, pp. 44–51, Aug. 2018. [CrossRef]
- M. A. Thomas, ‘Are vegans the same as vegetarians? The effect of diet on perceptions of masculinity’, Appetite, vol. 97, pp. 79–86, Feb. 2016. [CrossRef]
- A. M. Monge, D. Ferriday, S. Heckenmueller, J. M. Brunstrom, and P. J. Rogers, ‘Consumption of low-calorie sweeteners is associated with “sweet satiation” (sensory-specific satiety) but not “sweet-taste confusion”’, Appetite, vol. 169, p. 105492, Feb. 2022. [CrossRef]
- K. A. Faust and J. J. Prochaska, ‘Internet gaming disorder: A sign of the times, or time for our attention?’, Addictive Behaviors, vol. 77, pp. 272–274, Feb. 2018. [CrossRef]
- doi.org/10.1007/s00415-023-12033-1.
- Brown, T. A. (2015). Confirmatory factor analysis for applied research (2nd ed.). The Guilford Press.
Figure 1.
Workflow of the Study Methodology for the Development and Validation of the FFS.
Figure 1.
Workflow of the Study Methodology for the Development and Validation of the FFS.
Figure 2.
The frequency of Contemplating Sweets Restriction by Sweets Addiction Severity (SA) in the sub-sample (N = 126).
Figure 2.
The frequency of Contemplating Sweets Restriction by Sweets Addiction Severity (SA) in the sub-sample (N = 126).
Figure 3.
The frequency of Experiencing Negative Emotions by Sweets Addiction Severity in the sub-sample (N = 126).
Figure 3.
The frequency of Experiencing Negative Emotions by Sweets Addiction Severity in the sub-sample (N = 126).
Figure 4.
The frequency of sweet food consumption by Sweets Addiction Severity in the total sample (N = 344).
Figure 4.
The frequency of sweet food consumption by Sweets Addiction Severity in the total sample (N = 344).
Figure 5.
persistent desire or unsuccessful attempts to control sweet food consumption in Participants Without Sweets Addiction (No SA) and participants with Any Degree of Sweets Addiction (SA) in the sub-sample (N = 166).
Figure 5.
persistent desire or unsuccessful attempts to control sweet food consumption in Participants Without Sweets Addiction (No SA) and participants with Any Degree of Sweets Addiction (SA) in the sub-sample (N = 166).
Figure 6.
Based on the scree plot, a three-factor structure was identified.
Figure 6.
Based on the scree plot, a three-factor structure was identified.
Table 1.
Composition of the expert panel validating the FFSAS.
Table 1.
Composition of the expert panel validating the FFSAS.
| Degree |
Field |
Specialization |
Experience (Years) |
| Prof. |
Medicine |
Psychiatry; eating, anxiety & personality disorders |
24 |
| PhD |
Psychology |
Self-regulation; behavioural addictions; psychometrics |
20 |
| PhD |
Psychology |
Research, business training, coaching, change management |
20 |
| MSc |
Psychology |
Psychometrics; organisational psychology |
20 |
| PhD |
Psychology |
Mental health; EMDR; consumer behaviour |
20 |
| Dr hab. |
Health Sciences |
Clinical dietetics; obesity; MAFLD; CKD |
18 |
| PhD |
Medicine |
Psychiatry; psychotherapy; suicidology |
15 |
| PhD |
Psychology |
Psychodietetics, eating disorders |
15 |
| Dr hab. |
Health Sciences |
Clinical dietetics, psychodietetics, eating disorders |
14 |
| PhD |
Psychology |
Behavioral addictions, research methodology, psychometrics, statistics, mindfulness |
12.5 |
| PhD |
Health Sciences |
Public health, e-health, m-health, data analysis |
12 |
Table 2.
Demographic and anthropometric characteristics of study participants (total sample N=344).
Table 2.
Demographic and anthropometric characteristics of study participants (total sample N=344).
| Characteristics |
N |
Values |
| Age |
344 |
40.6 ± 10.7 (18–76) |
| Gender |
| Women |
270 |
78% |
| Men |
74 |
22% |
| Education |
| Primary |
1 |
0% |
| Vocational |
9 |
3% |
| Secondary |
68 |
20% |
| During studies |
18 |
5% |
| Higher Degree |
248 |
72% |
| Place of Residence |
| Village (up to 2,000 residents) |
45 |
13% |
| Town (2,000 to 50,000 residents) |
76 |
22% |
| City (50,000 to 250,000 residents) |
72 |
21% |
| City (250,000 to 500,000 residents) |
34 |
10% |
| City (over 500,000 residents) |
117 |
34% |
| BMI (kg/m²) |
336 |
27.86 ± 6.6 |
| Underweight (<18.5) |
8 |
2% |
| Normal weight (18.5–24.9) |
111 |
32% |
| Overweight (25–29.9) |
120 |
35% |
| Obese (≥30) |
97 |
31% |
Table 3.
Reported Sweet Food Consumption and Addiction in the total sample (N = 344).
Table 3.
Reported Sweet Food Consumption and Addiction in the total sample (N = 344).
| Criterion |
Response |
N |
% |
| Sweets addiction self-identification: |
Yes |
212 |
62 |
| No |
82 |
24 |
| Don’t know |
50 |
15 |
| Admission of addiction: |
Yes |
183 |
53 |
| No |
96 |
28 |
| Don’t know |
29 |
8 |
| Not applicable |
36 |
10 |
| Frequency of sweets consumption: |
Less than 1 time a week: |
29 |
8 |
| 1-2 times a week: |
42 |
12 |
| 3-4 times a week: |
65 |
19 |
| 5-6 times a week: |
37 |
11 |
| Once a day: |
64 |
19 |
| Several times a day: |
107 |
31 |
| Quantity of sweets consumed: |
Small: |
170 |
49 |
| Large: |
173 |
50 |
| Missing data: |
1 |
0 |
| Craving or unsuccessful attempts to quit: |
Yes |
29 |
8 |
| No |
42 |
12 |
| Missing data: |
65 |
19 |
| Frequency of sweets cravings: |
Never |
3 |
1 |
| Less than 1 time a week: |
15 |
4 |
| 1-2 times a week: |
23 |
7 |
| 3-4 times a week: |
20 |
6 |
| 5-6 times a week: |
12 |
3 |
| Once a day: |
21 |
6 |
| Several times a day: |
32 |
9 |
| Missing data: |
218 |
63 |
| Feelings of guilt or remorse: |
Never |
7 |
2 |
| Less than 1 time a week: |
17 |
5 |
| 1-2 times a week: |
21 |
6 |
| 3-4 times a week: |
17 |
5 |
| 5-6 times a week: |
7 |
2 |
| Once a day: |
19 |
6 |
| Several times a day: |
38 |
11 |
| Missing data: |
218 |
63 |
Table 4.
Comparison of the Frequency of Contemplating Sweets Restriction between Participants Without Sweets Addiction (No SA) and participants with Any Degree of Sweets Addiction (SA) in the sub-sample (N = 126).
Table 4.
Comparison of the Frequency of Contemplating Sweets Restriction between Participants Without Sweets Addiction (No SA) and participants with Any Degree of Sweets Addiction (SA) in the sub-sample (N = 126).
| How often do you experience periods of contemplating restriction? Promise of improvement or resolution "from tomorrow," "from Monday"? |
Classification SA |
| No SA |
Mild SA |
Moderate SA |
Severe SA |
Total |
| Never |
2 (3) |
0 (0) |
0 (0) |
0 (0) |
2 (3) |
| Less than once a week |
10 (13) |
0 (0) |
1 (1) |
1 (1) |
12 (15) |
| 1-2 times a week |
15 (19) |
1 (1) |
0 (0) |
2 (3) |
18 (23) |
| 3-4 times a week |
10 (12) |
0 (0) |
0 (0) |
6 (8) |
16 (20) |
| 5-6 times a week |
8 (10) |
0 (0) |
0 (0) |
2 (3) |
10 (12) |
| Once a day |
5 (6) |
0 (0) |
0 (0) |
12 (15) |
17 (21) |
| Several times a day |
10 (12) |
0 (0) |
0 (0) |
16 (20) |
25 (32) |
| Total |
60 (75) |
1 (1) |
1 (1) |
39 (49) |
100 (126) |
| χ², p = 0.00046 |
| γ = 0,573, p < 0.001 |
Table 5.
Comparison of the Frequency of experiencing negative emotions between Participants Without Sweets Addiction (No SA) and participants with Any Degree of Sweets Addiction (SA) in the sub-sample (N = 126).
Table 5.
Comparison of the Frequency of experiencing negative emotions between Participants Without Sweets Addiction (No SA) and participants with Any Degree of Sweets Addiction (SA) in the sub-sample (N = 126).
| How often do you experience remorse, guilt, shame, or anger at yourself related to this? |
Classification SA |
| No SA |
Mild SA |
Moderate SA |
Severe SA |
Total |
| Never |
4 (5) |
0 (0) |
1 (1) |
1 (1) |
6 (7) |
| Less than once a week |
12 (15) |
0 (0) |
0 (0) |
2 (2) |
13 (17) |
| 1-2 times a week |
13 (17) |
0 (0) |
0 (0) |
3 (4) |
17 (21) |
| 3-4 times a week |
11 (14) |
0 (0) |
0 (0) |
2 (3) |
13 (17) |
| 5-6 times a week |
5 (6) |
0 (0) |
0 (0) |
1 (1) |
6 (7) |
| Once a day |
6 (8) |
0 (0) |
0 (0) |
9 (11) |
15 (19) |
| Several times a day |
8 (10) |
1 (1) |
0 (0) |
21 (27) |
30 (38) |
| Total |
60 (75) |
1 (1) |
1 (1) |
39 (49) |
100 (126) |
| χ², p=0,00001 |
| γ = 0.629, p < 0,001 |
Table 6.
Comparison of the Frequency of the sweet food consumption between Participants Without Sweets Addiction (No SA) and participants with Any Degree of Sweets Addiction (SA) in the total sample (N = 344).
Table 6.
Comparison of the Frequency of the sweet food consumption between Participants Without Sweets Addiction (No SA) and participants with Any Degree of Sweets Addiction (SA) in the total sample (N = 344).
| How often do you eat sweets? |
Classification SA |
| No SA |
Mild SA |
Moderate SA |
Severe SA |
Total |
| Never |
7 (24) |
0 (0) |
0 (0) |
1 (4) |
8 (29) |
| Less than once a week |
11 (37) |
0 (0) |
0 (0) |
1 (5) |
12 (42) |
| 1-2 times a week |
14 (49) |
1 (2) |
0 (1) |
4 (13) |
19 (65) |
| 3-4 times a week |
8 (27) |
0 (1) |
0 (1) |
2 (8) |
11 (37) |
| 5-6 times a week |
10 (36) |
0 (1) |
0 (0) |
8 (27) |
19 (64) |
| Once a day |
12 (40) |
0 (0) |
0 (1) |
19 (66) |
31 (107) |
| Several times a day |
62 (213) |
1 (4) |
1 (4) |
36 (123) |
100 (344) |
| χ², p < 0.00001 |
| γ = 0.544, p < 0.001 |
Table 7.
Reported persistent desire or unsuccessful attempts to control sweet food consumption in Participants Without Sweets Addiction (No SA) and participants with Any Degree of Sweets Addiction (SA) in the sub-sample (N = 166).
Table 7.
Reported persistent desire or unsuccessful attempts to control sweet food consumption in Participants Without Sweets Addiction (No SA) and participants with Any Degree of Sweets Addiction (SA) in the sub-sample (N = 166).
| Is there a persistent desire or unsuccessful attempts to stop or control eating sweets? |
Classification SA |
| No SA |
Mild SA |
Moderate SA |
Severe SA |
Total |
| Yes |
24 (40) |
1 (1) |
1 (1) |
29 (48) |
54 (90) |
| No |
44 (73) |
1 (1) |
1 (1) |
1 (1) |
46 (76) |
| Total |
68 (113) |
1 (2) |
1 (2) |
30 (49) |
100 (166) |
| χ², p<0.00001 |
Table 8.
The computed Cronbach’s Alpha (α) for all FFSAS Criteria.
Table 8.
The computed Cronbach’s Alpha (α) for all FFSAS Criteria.
| Criterion |
Number of Items |
Sum of Item Variances |
Variance of Summed Items |
Cronbach’s Alpha |
| 1 |
3 |
13.68815682 |
32.31926741 |
0.864706044 |
| 2 |
4 |
25.82650221 |
75.678207 |
0.878310181 |
| 3 |
3 |
18.20527663 |
46.77292528 |
0.916159781 |
| 4 |
4 |
22.29518103 |
38.16421452 |
0.554412336 |
| 5 |
2 |
12.16105329 |
19.50280527 |
0.752891892 |
| 6 |
2 |
10.85493084 |
19.04643535 |
0.860161427 |
| 7 |
5 |
26.24855922 |
97.68957217 |
0.914133046 |
| 8 |
3 |
14.63365313 |
29.18580921 |
0.747905736 |
| 9 |
2 |
9.778273103 |
14.89375551 |
0.686929821 |
| 10 |
3 |
19.74027053 |
27.6627568 |
0.429593098 |
| 11 |
2 |
11.89428944 |
16.06928436 |
0.51962425 |
| 12 |
2 |
10.59159943 |
16.29869822 |
0.70031345 |
Table 9.
The associations between FFSAS Scores and Self-Reported Behavioral and Emotional Measures of Sweets Consumption.
Table 9.
The associations between FFSAS Scores and Self-Reported Behavioral and Emotional Measures of Sweets Consumption.
| FFSAS Score |
Variables |
ρ |
p value |
| 1 |
Self-identified sweets addiction |
0.38 |
< 0.05 |
| 2 |
Admission of addiction to loved ones |
0.28 |
< 0.05 |
| 3 |
Frequency of sweets consumption |
0.39 |
< 0.05 |
| 4 |
Quantity of sweets consumed |
0.23 |
< 0.05 |
| 5 |
Frequency of thoughts about limiting sweets |
0.39 |
< 0.05 |
| 6 |
Frequency of feelings of guilt or remorse |
0.35 |
< 0.05 |
| 7 |
Frequency of evening snacking |
0.44 |
< 0.05 |
| 8 |
Number of days per week with sweets consumption |
0.48 |
< 0.05 |
Table 10.
EFA rotated loadings matrix of EFA.
Table 10.
EFA rotated loadings matrix of EFA.
| |
Factor 1 |
Factor 2 |
Factor 3 |
Comunality |
| YFAS 1 |
0,28 |
0,36 |
0,67 |
0,66 |
| YFAS 2 |
0,30 |
0,34 |
0,71 |
0,72 |
| YFAS 3 |
0,36 |
0,44 |
0,43 |
0,51 |
| YFAS 4 |
0,29 |
0,40 |
0,76 |
0,83 |
| YFAS 5 |
0,49 |
0,25 |
0,67 |
0,76 |
| YFAS 6 |
0,70 |
0,03 |
0,53 |
0,77 |
| YFAS 7 |
0,59 |
0,13 |
0,60 |
0,72 |
| YFAS 8 |
0,78 |
0,06 |
0,16 |
0,64 |
| YFAS 9 |
0,77 |
0,18 |
0,08 |
0,63 |
| YFAS 10 |
0,79 |
-0,02 |
0,22 |
0,68 |
| YFAS 11 |
0,17 |
0,79 |
0,19 |
0,70 |
| YFAS 12 |
0,06 |
0,87 |
0,12 |
0,77 |
| YFAS 13 |
0,18 |
0,85 |
0,17 |
0,78 |
| YFAS 14 |
0,21 |
0,75 |
0,05 |
0,62 |
| YFAS 15 |
0,32 |
0,59 |
0,50 |
0,69 |
| YFAS 16 |
0,43 |
0,52 |
0,46 |
0,67 |
| YFAS 17 |
0,71 |
0,29 |
0,18 |
0,62 |
| YFAS 18 |
0,72 |
0,32 |
0,17 |
0,65 |
| YFAS 19 |
0,83 |
0,06 |
0,24 |
0,74 |
| YFAS 20 |
0,84 |
-0,01 |
0,29 |
0,79 |
| YFAS 21 |
0,86 |
-0,05 |
0,25 |
0,81 |
| YFAS 22 |
0,26 |
0,66 |
0,33 |
0,61 |
| YFAS 23 |
0,54 |
0,27 |
0,58 |
0,69 |
| YFAS 24 |
0,34 |
0,71 |
0,11 |
0,63 |
| YFAS 25 |
-0,18 |
0,87 |
0,23 |
0,85 |
| YFAS 26 |
0,30 |
0,68 |
0,17 |
0,58 |
| YFAS 27 |
0,63 |
0,47 |
-0,03 |
0,63 |
| YFAS 28 |
-0,17 |
0,88 |
0,21 |
0,84 |
| YFAS 29 |
0,55 |
0,25 |
0,52 |
0,64 |
| YFAS 30 |
-0,05 |
0,79 |
0,26 |
0,70 |
| YFAS 31 |
-0,12 |
0,64 |
0,45 |
0,62 |
| YFAS 32 |
0,17 |
0,61 |
0,54 |
0,69 |
| YFAS 33 |
0,78 |
0,05 |
0,27 |
0,69 |
| YFAS 34 |
0,78 |
0,10 |
0,16 |
0,65 |
| YFAS 35 |
0,46 |
0,47 |
0,02 |
0,43 |
Table 11.
CFA loadings matrix.
Table 11.
CFA loadings matrix.
| |
CR01 |
CR02 |
CR03 |
CR04 |
CR05 |
CR06 |
CR07 |
CR08 |
CR09 |
CR10 |
CR11 |
CR12 |
| YFAS1 |
1,00 |
|
|
|
|
|
|
|
|
|
|
|
| YFAS2 |
1,04 |
|
|
|
|
|
|
|
|
|
|
|
| YFAS3 |
0,86 |
|
|
|
|
|
|
|
|
|
|
|
| YFAS4 |
|
1,00 |
|
|
|
|
|
|
|
|
|
|
| YFAS5 |
|
|
1,00 |
|
|
|
|
|
|
|
|
|
| YFAS6 |
|
|
1,02 |
|
|
|
|
|
|
|
|
|
| YFAS7 |
|
|
1,00 |
|
|
|
1,00 |
|
|
|
|
|
| YFAS8 |
|
|
|
1,00 |
|
|
|
|
|
|
|
|
| YFAS9 |
|
|
|
|
|
|
|
1,00 |
1,00 |
|
|
|
| YFAS10 |
|
|
|
1,03 |
|
|
|
|
|
|
|
|
| YFAS11 |
|
|
|
|
|
|
61,85 |
|
|
|
|
|
| YFAS12 |
|
|
|
|
|
|
63,44 |
|
|
|
|
|
| YFAS13 |
|
|
|
|
|
|
64,35 |
|
|
|
|
|
| YFAS14 |
|
|
|
|
|
|
56,25 |
|
|
|
|
|
| YFAS15 |
|
|
|
|
|
|
52,44 |
|
|
|
|
|
| YFAS16 |
|
|
|
|
|
|
|
|
|
|
|
1,00 |
| YFAS17 |
|
|
|
|
|
|
|
|
|
|
|
0,95 |
| YFAS18 |
|
|
|
0,98 |
|
|
|
|
|
|
|
|
| YFAS19 |
|
|
|
|
|
|
|
|
1,17 |
|
|
|
| YFAS20 |
|
|
|
1,20 |
|
|
|
|
|
|
|
|
| YFAS21 |
|
|
|
|
|
|
|
45,32 |
|
|
|
|
| YFAS22 |
|
|
|
|
1,00 |
|
|
|
|
|
|
|
| YFAS23 |
|
|
|
|
1,18 |
|
|
|
|
|
|
|
| YFAS24 |
|
|
|
|
|
1,00 |
|
|
|
|
|
|
| YFAS25 |
|
1,10 |
|
|
|
|
|
|
|
|
|
|
| YFAS26 |
|
|
|
|
|
0,99 |
|
|
|
|
|
|
| YFAS27 |
|
|
|
|
|
|
|
|
0,94 |
|
|
|
| YFAS28 |
|
|
|
|
|
|
|
|
|
1,00 |
|
|
| YFAS29 |
|
|
|
|
|
|
|
|
|
|
1,00 |
|
| YFAS30 |
|
|
|
|
|
|
|
|
|
|
1,26 |
|
| YFAS31 |
|
1,05 |
|
|
|
|
|
|
|
|
|
|
| YFAS32 |
|
1,13 |
|
|
|
|
|
|
|
|
|
|
| YFAS33 |
|
|
|
|
|
|
|
|
|
0,39 |
|
|
| YFAS34 |
|
|
|
|
|
|
|
|
|
0,25 |
|
|
| YFAS35 |
|
|
|
|
|
|
|
21,46 |
|
|
|
|
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).