Submitted:
06 May 2025
Posted:
07 May 2025
You are already at the latest version
Abstract
Keywords:
Introduction
Materials and Methods
Study Population
Study Outcomes
Statistical Analysis
Results
| Univariate model | Initial multivariate model | Final multivariate model | ||||
|
Crude HR (IC 95%) |
p |
Adjusted HR (IC 95%) |
p |
Adjusted HR (IC 95%) |
p | |
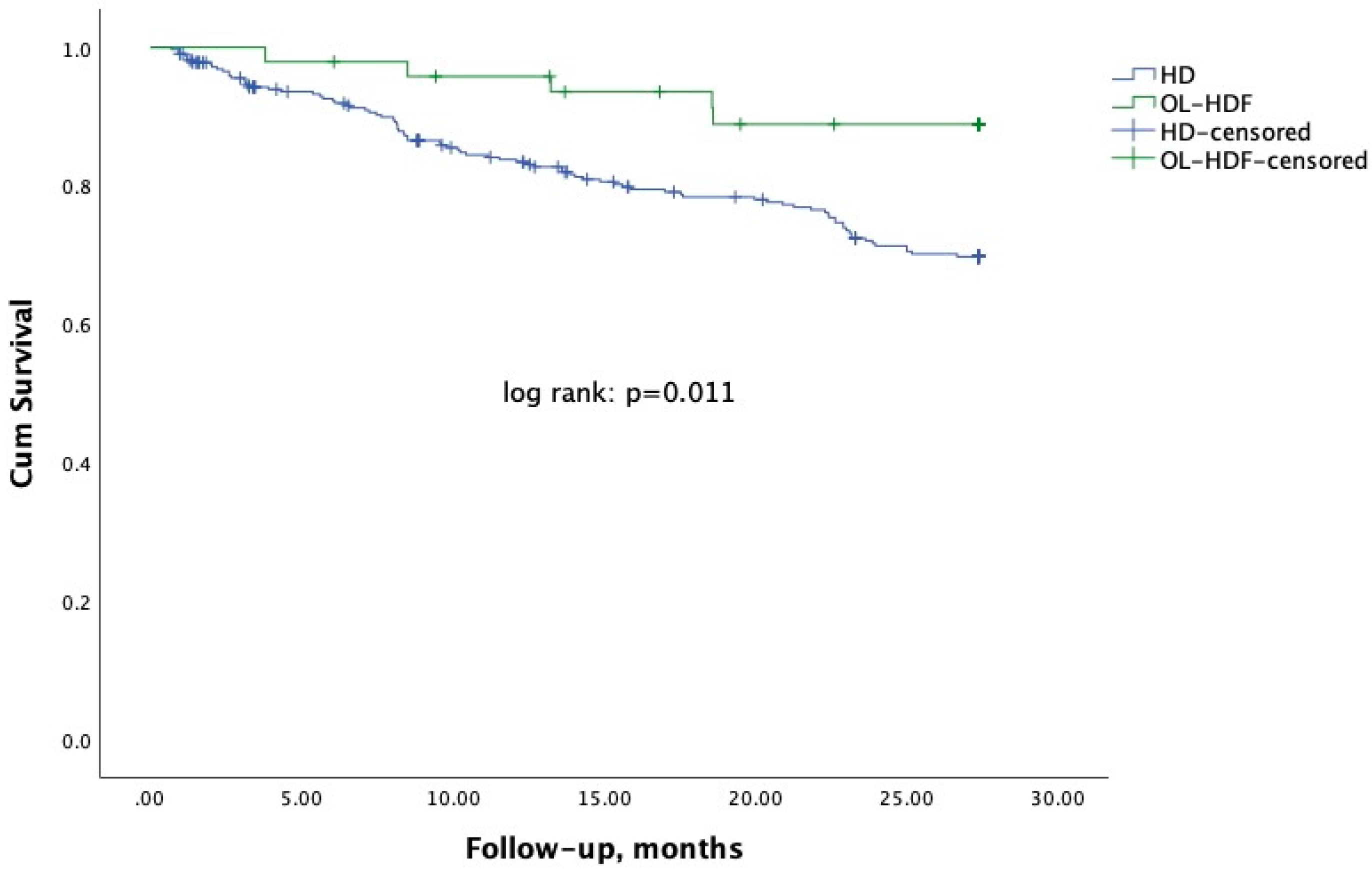
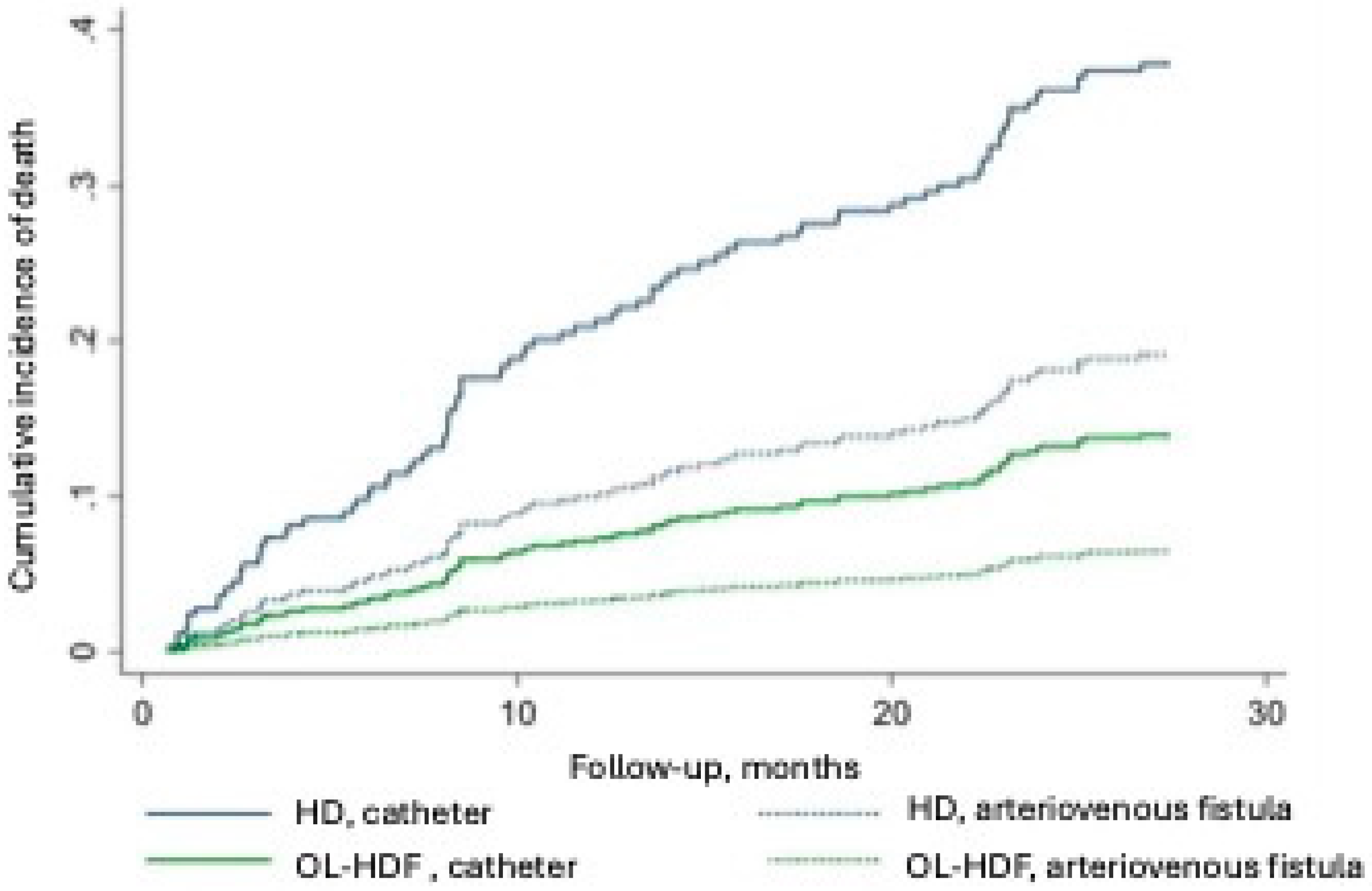
| HD - reference | 0.33 (0.13-0.81) | 0.015 | 0.32 (0.13-0.81) | 0.015 | 0.32 (0.13-0.77) | 0.011 |
| Age, years | 1.01 (1.00-1.03) | 0.104 | 1.01 (0.99-1.03) | 0.234 | - | - |
| Diabetes | 1.47 (0.97-2.23) | 0.068 | 1.36 (0.88-2.09) | 0.167 | - | - |
| Arteriovenous fistula | 0.46 (0.29-0.71) | <0.001 | 0.46 (0.29-0.72) | 0.001 | 0.45 (0.29-0.69) | <0.001 |
| Hours on dialysis/week | 0.95 (0.87-1.05) | 0.339 | 0.93 (0.85-1.03) | 0.177 | ||
Discussion
Data Availability Statement
Funding
Authors’ Contributions
Conflict Interest Statement
References
- Nerbass, F.B.; Lima, H.D.N.; Moura-Neto, J.A.; Lugon, J.R.; Sesso, R. Brazilian Dialysis Survey 2022. Jornal brasileiro de nefrologia : 'orgao oficial de Sociedades Brasileira e Latino-Americana de Nefrologia 2024, 46, e20230062. [CrossRef]
- Bello, A.K.; Okpechi, I.G.; Osman, M.A.; Cho, Y.; Htay, H.; Jha, V.; Wainstein, M.; Johnson, D.W. Epidemiology of haemodialysis outcomes. Nature reviews. Nephrology 2022, 18, 378-395. [CrossRef]
- Ok, E.; Asci, G.; Toz, H.; Ok, E.S.; Kircelli, F.; Yilmaz, M.; Hur, E.; Demirci, M.S.; Demirci, C.; Duman, S.; et al. Mortality and cardiovascular events in online haemodiafiltration (OL-HDF) compared with high-flux dialysis: results from the Turkish OL-HDF Study. Nephrology, dialysis, transplantation : official publication of the European Dialysis and Transplant Association - European Renal Association 2013, 28, 192-202. [CrossRef]
- Maduell, F.; Moreso, F.; Pons, M.; Ramos, R.; Mora-Macia, J.; Carreras, J.; Soler, J.; Torres, F.; Campistol, J.M.; Martinez-Castelao, A.; et al. High-efficiency postdilution online hemodiafiltration reduces all-cause mortality in hemodialysis patients. Journal of the American Society of Nephrology : JASN 2013, 24, 487-497. [CrossRef]
- Blankestijn, P.J.; Vernooij, R.W.M.; Hockham, C.; Strippoli, G.F.M.; Canaud, B.; Hegbrant, J.; Barth, C.; Covic, A.; Cromm, K.; Cucui, A.; et al. Effect of Hemodiafiltration or Hemodialysis on Mortality in Kidney Failure. The New England journal of medicine 2023, 389, 700-709. [CrossRef]
- Nefrologia, S.B.d. Censo Brasileiro de Diálise. Available online: http://censo-sbn.org.br/inicio?_gl=1*xyuvlm*_ga*NjkxMDIwMTguMTczMDIxNzY5OA..*_ga_E1HJB87YJ7*MTczMDIxNzY5OC4xLjAuMTczMDIxNzY5OC42MC4wLjA. (accessed on.
- da Rocha, E.P.; Kojima, C.A.; Modelli de Andrade, L.G.; Costa, D.M.; Magalhaes, A.O.; Rocha, W.F.; de Vasconcelos Junior, L.N.; Rosa, M.G.; Wagner Martins, C.S. Comparing Survival Outcomes between Hemodialysis and Hemodiafiltration Using Real-World Data from Brazil. Journal of clinical medicine 2024, 13. [CrossRef]
- Barra, A.B.L.; Roque-da-Silva, A.P.; Canziani, M.E.F.; Lugon, J.R.; Strogoff-de-Matos, J.P. Characteristics and predictors of mortality on haemodialysis in Brazil: a cohort of 5,081 incident patients. BMC nephrology 2022, 23, 77. [CrossRef]
- Canziani, M.E.F.; Strogoff-de-Matos, J.P.; Guedes, M.; Barra, A.B.L.; Canhada, S.; Carvalho, L.; Gemente, D.; Poli-de-Figueiredo, C.E.; Pecoits-Filho, R. High volume online hemodiafiltration: a global perspective and the Brazilian experience. Jornal brasileiro de nefrologia : 'orgao oficial de Sociedades Brasileira e Latino-Americana de Nefrologia 2024, 46, e20230104. [CrossRef]
- Larkin, J.W.; Han, M.; Han, H.; Guedes, M.H.; Goncalves, P.B.; Poli-de-Figueiredo, C.E.; Cuvello-Neto, A.L.; Barra, A.B.L.; de Moraes, T.P.; Usvyat, L.A.; et al. Impact of hemodialysis and post-dialysis period on granular activity levels. BMC nephrology 2020, 21, 197. [CrossRef]
- do Nascimento Lima, H.; Monarrez-Espino, J.; Nerbass, F.B.; Moura-Neto, J.A.; Sesso, R.; Lugon, J.R.; Brazilian Dialysis Register, I. Comparison of 1-year survival between patients initiating chronic hemodialysis under public and private health insurance: register-based data analysis from Brazil. International urology and nephrology 2024, 56, 3013-3022. [CrossRef]
- Barra, A.B.L.; Silva, A.; Canziani, M.E.F.; Lugon, J.R.; Matos, J.P.S. Survival in hemodialysis in Brazil according to the source of payment for the treatment: Public Healthcare System (SUS) versus private insurance. Jornal brasileiro de nefrologia : 'orgao oficial de Sociedades Brasileira e Latino-Americana de Nefrologia 2023, 45, 302-309. [CrossRef]
- Aquino, H.B.S.; Canziani, M.E.F.; Barra, A.B.L.; Roque-da-Silva, A.P.; Strogoff-de-Matos, J.P.; Dalboni, M.A.; Moyses, R.M.A.; Elias, R.M. PTH may predict early mortality in incident patients on hemodialysis: results from a large cohort. International urology and nephrology 2025, 57, 545-551. [CrossRef]
- Roetker, N.S.; Gilbertson, D.T.; Weinhandl, E.D. A Brief Introduction to Competing Risks in the Context of Kidney Disease Epidemiology. Kidney360 2022, 3, 740-743. [CrossRef]
- Al-Wahsh, H.; Tangri, N.; Quinn, R.; Liu, P.; Ferguson Ms, T.; Fiocco, M.; Lam Md, M.N.N.; Tonelli, M.; Ravani, P. Accounting for the Competing Risk of Death to Predict Kidney Failure in Adults With Stage 4 Chronic Kidney Disease. JAMA Netw Open 2021, 4, e219225. [CrossRef]
- Di Iorio, B.; Di Micco, L.; Bruzzese, D.; Nardone, L.; Russo, L.; Formisano, P.; D'Esposito, V.; Russo, D. Ultrapure dialysis water obtained with additional ultrafilter may reduce inflammation in patients on hemodialysis. Journal of nephrology 2017, 30, 795-801. [CrossRef]
- Hasegawa, T.; Nakai, S.; Masakane, I.; Watanabe, Y.; Iseki, K.; Tsubakihara, Y.; Akizawa, T. Dialysis fluid endotoxin level and mortality in maintenance hemodialysis: a nationwide cohort study. American journal of kidney diseases : the official journal of the National Kidney Foundation 2015, 65, 899-904. [CrossRef]
- Wasse, H.; Speckman, R.A.; McClellan, W.M. Arteriovenous fistula use is associated with lower cardiovascular mortality compared with catheter use among ESRD patients. Seminars in dialysis 2008, 21, 483-489. [CrossRef]
- Pisoni, R.L.; Arrington, C.J.; Albert, J.M.; Ethier, J.; Kimata, N.; Krishnan, M.; Rayner, H.C.; Saito, A.; Sands, J.J.; Saran, R.; et al. Facility hemodialysis vascular access use and mortality in countries participating in DOPPS: an instrumental variable analysis. American journal of kidney diseases : the official journal of the National Kidney Foundation 2009, 53, 475-491. [CrossRef]
- Lyu, B.; Chan, M.R.; Yevzlin, A.S.; Gardezi, A.; Astor, B.C. Arteriovenous Access Type and Risk of Mortality, Hospitalization, and Sepsis Among Elderly Hemodialysis Patients: A Target Trial Emulation Approach. American journal of kidney diseases : the official journal of the National Kidney Foundation 2022, 79, 69-78. [CrossRef]
- Lok, C.E.; Huber, T.S.; Lee, T.; Shenoy, S.; Yevzlin, A.S.; Abreo, K.; Allon, M.; Asif, A.; Astor, B.C.; Glickman, M.H.; et al. KDOQI Clinical Practice Guideline for Vascular Access: 2019 Update. American journal of kidney diseases : the official journal of the National Kidney Foundation 2020, 75, S1-S164. [CrossRef]
| Variable |
HD N=321 |
OL-HDF N=48 |
p |
| Age, years | 60 ± 14 | 61 ± 14 | 0.676 |
| White race, n (%) | 212 (66.0) | 32 (66.7) | 0.932 |
| Men, n (%) | 176 (54.8) | 30 (62.5) | 0.318 |
| Arteriovenous fistula, n (%) | 152 (47.4) | 21 (43.8) | 0.641 |
| Diabetes, n (%) | 175 (54.5) | 14 (29.2) | 0.001 |
| Dialysis frequency/week, % | <0.001 | ||
| 3 times | 94.1 | 66.7 | |
| 4 or more times | 5.9 | 33.3 | |
| Dialysis vintage, months | 75.1 (33.4. 156.0) | 35.3 (6.2. 68.2) | <0.001 |
| Week dialysis duration, h | 11.2 ± 1.8 | 10.5 ± 1.6 | 0.006 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





