Submitted:
04 May 2025
Posted:
06 May 2025
You are already at the latest version
Abstract
Keywords:
1. Introduction
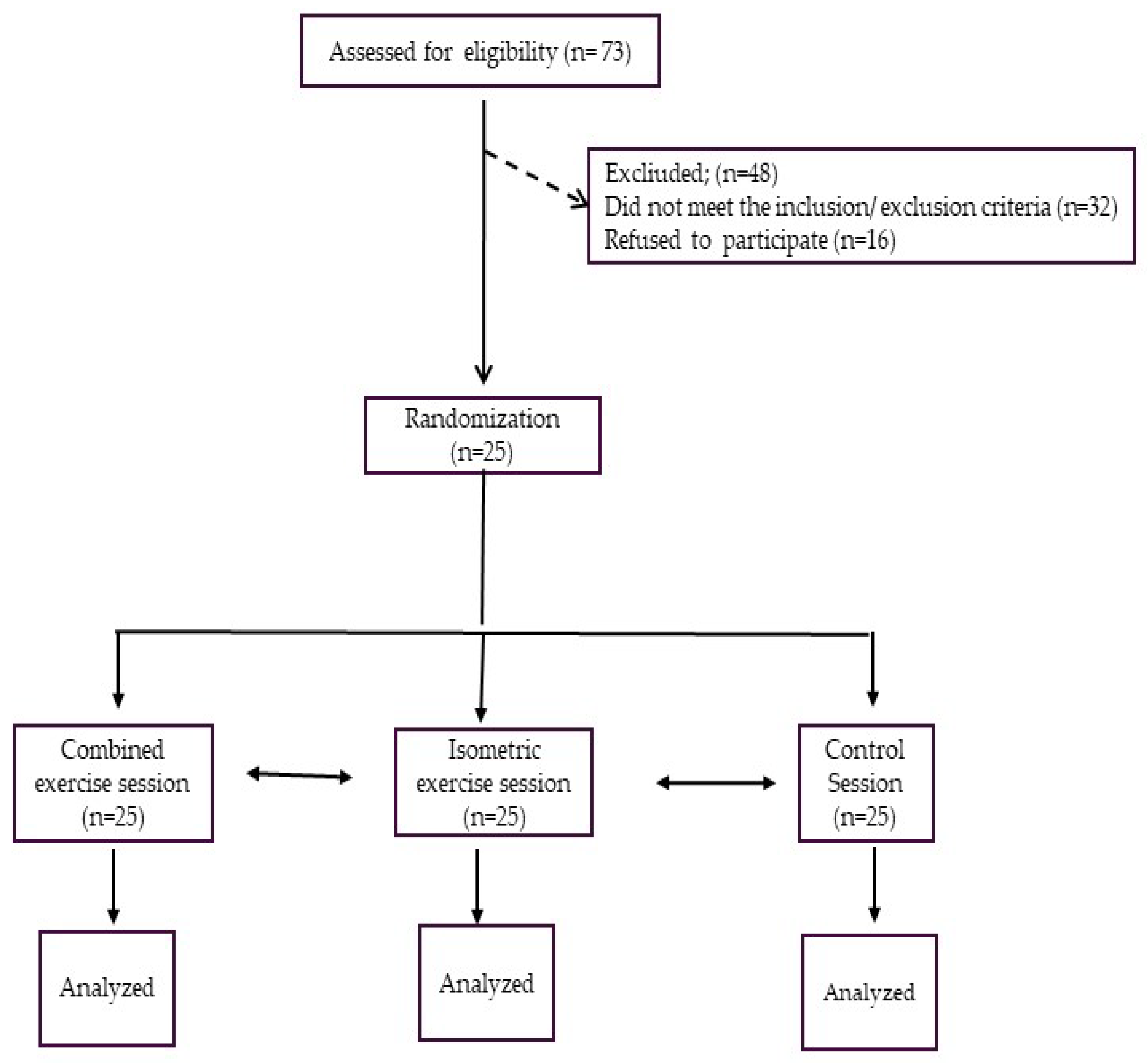
2. Materials and Methods
2.1. Population
2.2. Study Design
2.3. Exercise Settings
2.4. Experimental Sessions
2.5. Statistical Analysis
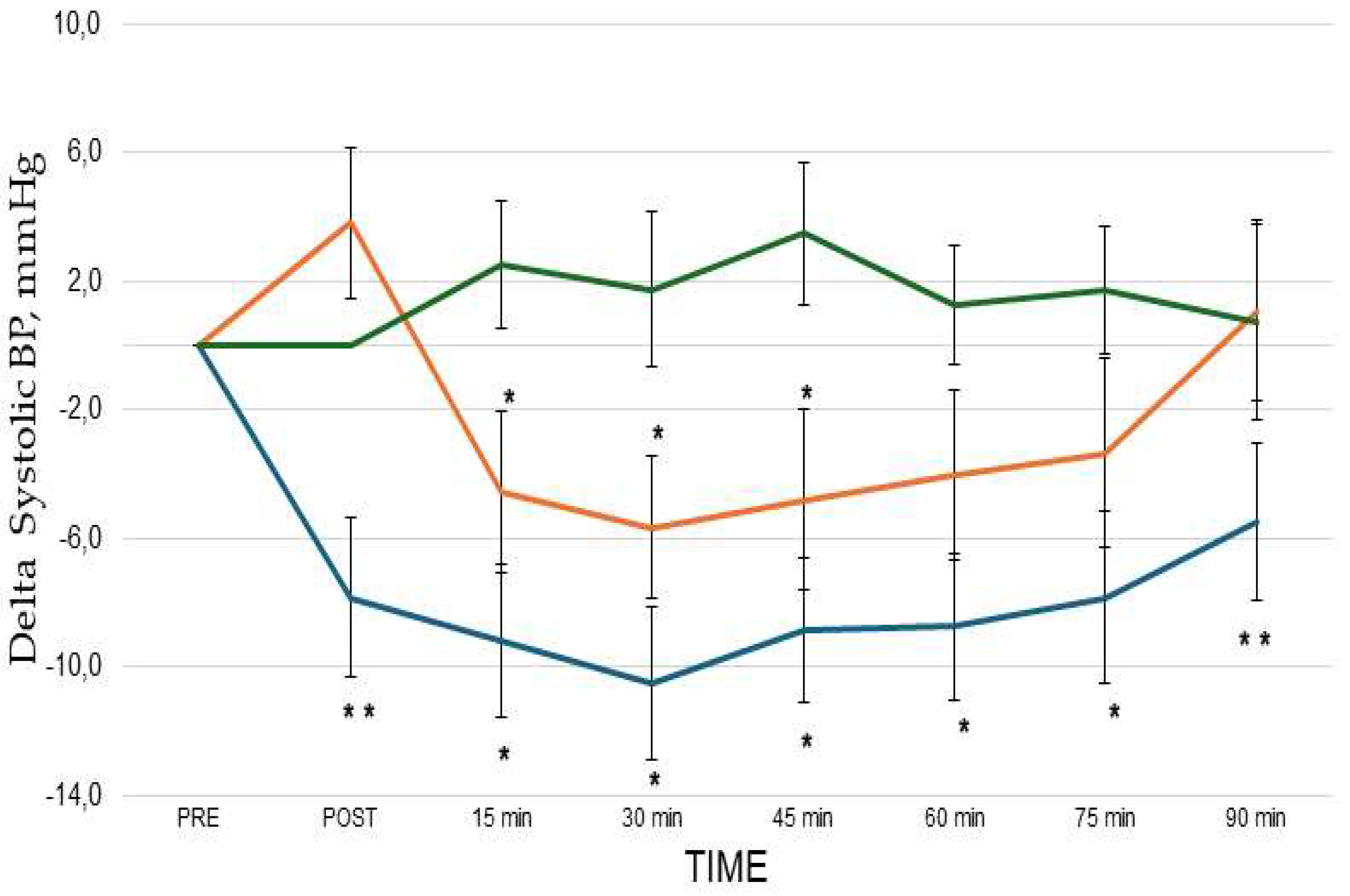
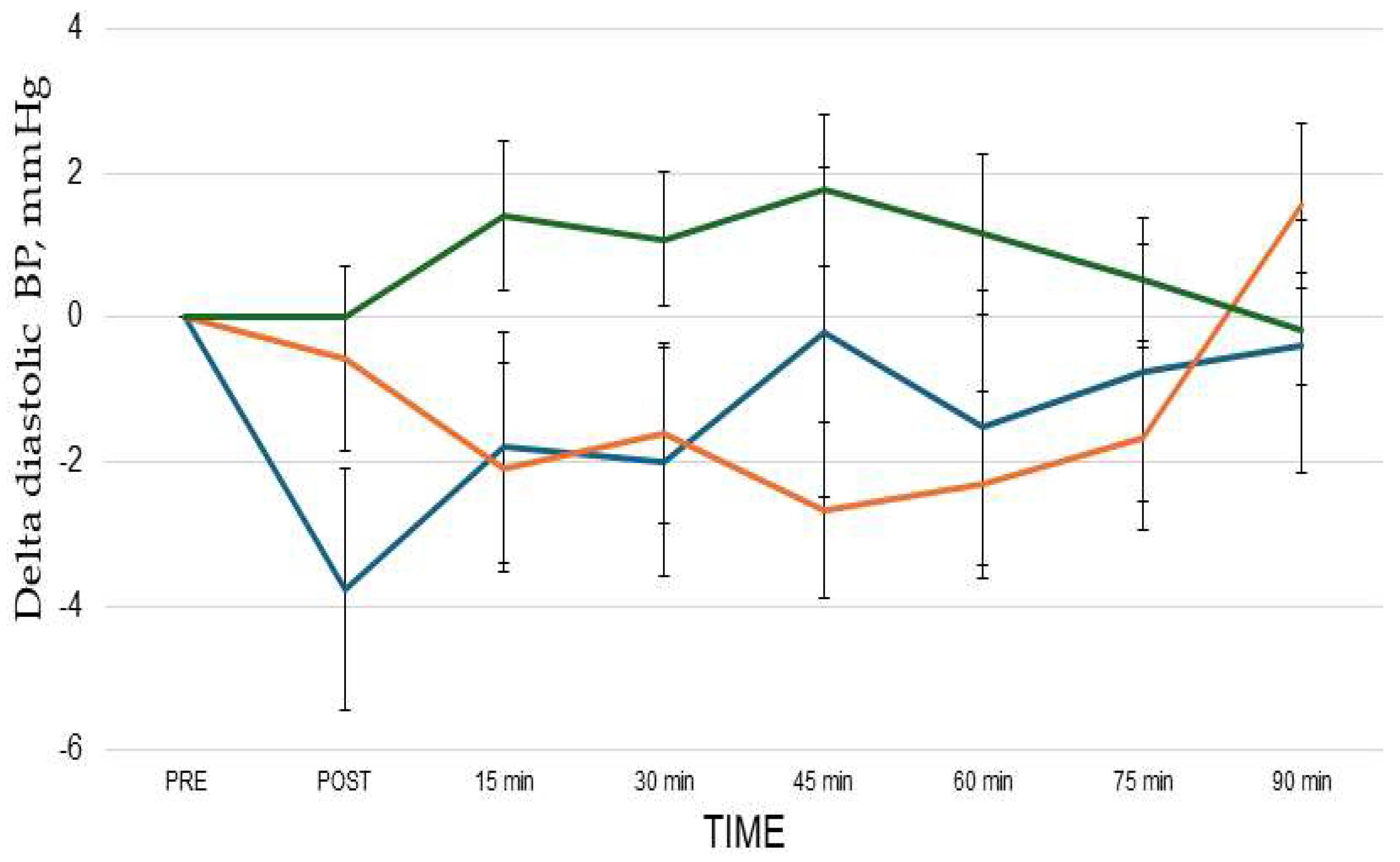
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
References
- Cornelissen VA, Smart NA. Exercise training for blood pressure: a systematic review and meta-analysis. J Am Heart Assoc. 2013 Feb 1;2(1):e004473. [CrossRef]
- Pescatello LS, Buchner DM, Jakicic JM, Powell KE, Kraus WE, Bloodgood B, Campbell WW, Dietz S, Dipietro L, George SM, et al. 2018 PHYSICAL ACTIVITY GUIDELINES ADVISORY COMMITTEE*. Physical Activity to Prevent and Treat Hypertension: A Systematic Review. Med Sci Sports Exerc.2019 Jun;51(6):1314-1323. [CrossRef]
- Jabbarzadeh Ganjeh B, Zeraattalab-Motlagh S, Jayedi A, Daneshvar M, Gohari Z, Norouziasl R, Ghaemi S, Selk-Ghaffari M, Moghadam N, Kordi R, Shab-Bidar S. Effects of aerobic exercise on blood pressure in patients with hypertension: a systematic review and dose-response meta-analysis of randomized trials. Hypertens Res. 2024 Feb;47(2):385-398. [CrossRef]
- Cao L, Li X, Yan P, Wang X, Li M, Li R, Shi X, Liu X, Yang K. The effectiveness of aerobic exercise for hypertensive population: A systematic review and meta-analysis. J ClinHypertens (Greenwich). 2019 Jul;21(7):868-876. [CrossRef]
- Hanssen H, Boardman H, Deiseroth A, Moholdt T, Simonenko M, Kränkel N, Niebauer J, Tiberi M, Abreu A, Solberg EE, et al. Personalized exercise prescription in the prevention and treatment of arterial hypertension: a Consensus Document from the European Association of Preventive Cardiology (EAPC) and the ESC Council on Hypertension. Eur J PrevCardiol.2022;19:205-215. [CrossRef]
- Carlson DJ, Dieberg G, Hess NC, Millar PJ, Smart NA. Isometric exercise training for blood pressure management: a systematic review and meta-analysis. Mayo Clin Proc.2014 Mar;89(3):327-34. [CrossRef]
- Edwards JJ, Deenmamode AHP, Griffiths M, Arnold O, Cooper NJ, Wiles JD, O'Driscoll JM. Exercise training and resting blood pressure: a large-scale pairwise and network meta-analysis of randomised controlled trials. Br J Sports Med. 2023 Oct;57(20):1317-1326.
- Edwards JJ, Coleman DA, Ritti-Dias RM, Farah BQ, Stensel DJ, Lucas SJE, Millar PJ, Gordon BDH, Cornelissen V, Smart NA, et al. Isometric Exercise Training and Arterial Hypertension: An Updated Review. Sports Med. 2024 Jun;54(6):1459-1497. [CrossRef]
- Miura, S. Evidence for exercise therapies including isometric handgrip training for hypertensive patients. Hypertens. Res. 2024, 48, 846–848. [CrossRef]
- MacDougall J.D., McKelvie R.S., Moroz D.E., Sale D.G., McCartney N., Buick F. Factors affecting blood pressure during heavy weight lifting and static contractions. J ApplPhysiol (1985) 1992;73(4):1590–1597. [CrossRef]
- Taylor K.A., Wiles J.D., Coleman D.D., Sharma R., O'driscoll J.M. Continuous cardiac autonomic hemodynamic responses to isometric exercise. Med Sci Sports Exerc.2017;49(8):1511–1519.
- Hanson P, Nagle F. Isometric exercise: cardiovascular responses in normal and cardiac populations. CardiolClin.1987 May;5(2):157-70. [CrossRef]
- Goessler, K.; Buys, R.; Cornelissen, V.A. Low-intensity isometric handgrip exercise has no transient effect on blood pressure in patients with coronary artery disease. J. Am. Soc. Hypertens. 2016, 10, 633–639. [Google Scholar] [CrossRef] [PubMed]
- Caminiti, G.; Marazzi, G.; Volterrani, M.; D’Antoni, V.; Fecondo, S.; Vadalà, S.; Sposato, B.; Giamundo, D.M.; Vitarelli, M.; Morsella, V.; et al. Effect of Different Isometric Exercise Modalities on Myocardial Work in Trained Hypertensive Patients with Ischemic Heart Disease: A Randomized Pilot Study. J. Funct. Morphol. Kinesiol. 2025, 10, 108. [Google Scholar] [CrossRef]
- Pagonas N, Vlatsas S, Bauer F, Seibert FS, Zidek W, Babel N, Schlattmann P, Westhoff TH. Aerobic versus isometric handgrip exercise in hypertension: a randomized controlled trial. J Hypertens.2017 Nov;35(11):2199-2206.
- Goessler K, Buys R, Cornelissen VA. Low-intensity isometric handgrip exercise has no transient effect on blood pressure in patients with coronary artery disease. J Am SocHypertens. 2016 Aug;10(8):633-9.
- Oliveira-Silva L, Fecchio RY, Silva Junior NDD, Pio-Abreu A, Silva GVD, Drager LF, Silva de Sousa JC, Forjaz CLM. Post-dynamic, isometric and combined resistance exercise responses in medicated hypertensive men. J Hum Hypertens. 2024;;38:52-61. [CrossRef]
- Aly K, Yeung PK. Post-Exercise Hypotension: An Alternative Management Strategy for Hypertension and Cardiovascular Disease? J Clin Med. 2023 Jul 3;12(13):4456.
- Oliveira PC, Dipp T, Waclawovsky G, Lehnen AM. Post-isometric exercise hypotension occurs irrespective of muscle mass in adults with hypertension: A randomized clinical trial. Clinics (Sao Paulo). 2025 Apr 16;80:100612. [CrossRef]
- Borg, G.A. Psychophysical bases of perceived exertion. Med. Sci. Sports Exerc. 1982, 14, 377–381. [Google Scholar] [CrossRef] [PubMed]
- Meldrum D, Cahalane E, Conroy R, Fitzgerald D, Hardiman O. Maximum voluntary isometric contraction: reference values and clinical application. AmyotrophLateralScler. 2007 Feb;8(1):47-55. [CrossRef]
- Niewiadomski W, Laskowska D, Gąsiorowska A, Cybulski G, Strasz A, Józef Langfort J. Determination and Prediction of One Repetition Maximum (1RM): Safety Considerations. Journal of Human Kinetics. 2008;19:109-120. [CrossRef]
- Wiles, J. D., Goldring, N., & Coleman, D. Home-based isometric exercise training induced reductions resting blood pressure. European journal of applied physiology. 2017;117(1), 83–93. [CrossRef]
- Javidi M, Ahmadizad S, Argani H, Najafi A, Ebrahim K, Salehi N, Javidi Y, Pescatello LS, Jowhari A, Hackett DA. Effect of Lower- versus Higher-Intensity Isometric Handgrip Training in Adults with Hypertension: A Randomized Controlled Trial. J Cardiovasc Dev Dis.2022 Aug 30;9(9):287. [CrossRef]
- Caminiti, G.; Volterrani, M.; Iellamo, F.; Marazzi, G.; D’Antoni, V.; Calandri, C.; Vadalà, S.; Catena, M.; Di Biasio, D.; Manzi, V.; et al. Acute Changes in Myocardial Work during Isometric Exercise in Hypertensive Patients with Ischemic Heart Disease: A Case–Control Study. J. Clin. Med. 2024, 13, 5955. [Google Scholar] [CrossRef] [PubMed]
- Inder, J. D., Carlson, D. J., Dieberg, G., McFarlane, J. R., Hess, N. C., & Smart, N. A. (2016). Isometric exercise training for blood pressure management: A systematic review and meta-analysis to optimize benefit. Hypertension Research2016; 39(2):88-94. [CrossRef]
- Loaiza-Betancur AF, Pérez Bedoya E, Montoya Dávila J, Chulvi-Medrano I. Effect of Isometric Resistance Training on Blood Pressure Values in a Group of Normotensive Participants: A Systematic Review and Meta-analysis. Sports Health.2020 May/Jun;12(3):256-262. [CrossRef]
- Baross, A. W., Wiles, J. D., & Swaine, I. L. (2012). Effects of the intensity of leg isometric training on the vasculature of trained and untrained limbs and resting blood pressure in middle-aged men. International journal of vascular medicine, 2012, 964697. [CrossRef]
- Baross AW, Wiles JD, Swaine IL. Double-leg isometric exercise training in older men. Open Access J Sports Med. 2013 Jan 30;4:33-40. [CrossRef]
- Wiles JD, Coleman DA, Swaine IL. The effects of performing isometric training at two exercise intensities in healthy young males. Eur J Appl Physiol. 2010 ;108(3):419-28. [CrossRef]
- Ash GI, Taylor BA, Thompson PD, MacDonald HV, Lamberti L, Chen MH, Farinatti P, Kraemer WJ, Panza GA, Zaleski AL, et al. The antihypertensive effects of aerobic versus isometric handgrip resistance exercise. J Hypertens. 2017 Feb;35(2):291-299. [CrossRef]
- Somani YB, Baross AW, Brook RD, Milne KJ, McGowan CL, Swaine IL. Acute response to a 2-minute isometric exercise test predicts the blood pressure-lowering efficacy of isometric resistance training in young adults. Am J Hypertens [Internet]. 2018;31:362–8. [CrossRef]
| Age, years | 65.9±8.2. |
| BMI, kg/m2 | 28.1±8.2 |
| Waist circumference, cm | 106.2±31.6 |
| Male/female, n | 23/2 |
| Previous PCI/CABG, n | 19/10 |
| EF, (%) | 52.7± 6.7 |
| NT-proBNP, ng/pl | 124.2±31.6 |
| Comorbidities | |
| Carotid artery disease, n (%) | 14 (56) |
| Diabetes, n (%) | 7 (24) |
| Hypercholesterolemia, n (%) | 22 (88) |
| Previous Smoke habit, n (%) | 15 (60) |
| Treatment | |
| Anti-platelets agents, n (%) | 25 (100) |
| ACE-Is/ARBs, n (%) | 22 (88) |
| Betablockers, n (%) | 21 (84) |
| CCBs, n (%) | 11 (44) |
| SGLT2-I, n (%) | 7 (28) |
| Diuretics, n (%) | 8 (32) |
| Statins, n (%) | 25 (100) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





