1. Introduction
Testicular cancer (TC) is a rare tumour (1%), that is mostly diagnosed at a younger age (15 to 35 years)[
1]. Since the advent of the cisplatin-based chemotherapy regimens, the cure rates are reported to be above 95%[
2]. Cisplatin-based multi-drug regimens, first used in 1974, hugely improved the prognosis compared to the pre-cisplatin era [
3,
4]. Moreover, recent decades have seen an increase in the incidence along with an improvement in the survival rate[
1]. Unfortunately, these high cure rates come at a cost of late side effects, particularly in the patients who receive chemotherapy and radiotherapy[
5]. These side effects encompass a list of malignant and non-malignant conditions including late recurrences, second malignant neoplasms, cardiovascular disease, renal insufficiency, pulmonary disease, hypogonadism, infertility, and metabolic syndrome[
6]. On top of these complications, a higher incidence of psychological conditions including anxiety and fear of cancer recurrence has also been reported in this cohort[
7]. As most of the survivors are young at the time of diagnosis, they have to brave these complications for decades to come. These physical and psychological complications have been reported to cause a negative impact on the social, economic, and sexual well-being of TC survivors[
8,
9]. A higher level of disability, unemployment, and sick leave has been reported in recent studies[
8].
An estimated half of patients have abnormal semen analysis at the time of diagnosis before any treatments[
10]. Chemotherapy, radiotherapy, and surgeries can further deteriorate sperm production, motility, and erectile function[
11]. As a result, a reduced rate of paternity is found in TC survivors compared to the normal population, even with pre-treatment semen cryopreservation techniques[
11]. These consequences of treatment also cause the re-entry and readjustment problems for the survivors back into society, as they are nervous and anxious about their fertility [
12]. Many researchers have reported long-term deterioration in sexual health, including erectile dysfunction, sexual dissatisfaction, low sex drive, and orgasmic dysfunction[
13]. This long-term deterioration in sexual health results from multiple factors, including hypogonadism, anxiety, systemic diseases, impaired body image perception, and a sense of loss of masculinity[
13]. These complications, in turn, have a significant effect on the social lives of TC survivors, particularly relationships with their partners. Spouses and partners, especially those who began their relationship after TC diagnosis, are poorly affected in terms of their quality of life and stress response symptoms[
14]. In addition, long-term side effects on career and financial well-being are also reported in TC survivors. Jobs and careers can be affected by late comorbidities like peripheral neuropathy and chronic cancer-related fatigue[
15]. A systematic review by Schepisi et al. painted a grim picture of survivors, revealing a higher incidence of joblessness, absenteeism, and neuroticism, especially in those involved in manual labour[
12]. TC diagnosis and treatments, mainly chemotherapy, have been found to cause financial distress and financial burden on survivors[
9]. In the last few years, we have seen growing interest in cancer survivorship, with numerous studies performed to look at different aspects of survivorship care. This is the first study to give an estimation of these difficulties faced by TC survivors in Ireland. As we believe a multi-team, collaborative model of care will be key to improving the quality of life in survivors, our study aims to identify areas of need for further research and quality improvement initiatives. Our study may also be helpful for other urban populations in the UK and Western Europe.
This article is a revised and expanded version of a paper entitled “Impact of testicular cancer on socio-economic and sexual health of survivors: A questionnaire-based survey”, which was presented at ESMO Sarcoma and Rare Cancer Congress, held in Lugano, Switzerland on 14th March 2024[
16].
2. Materials and Methods
2.1. Study Design and Participants
We requested the patients attending the survivorship clinic in a tertiary care cancer centre in Ireland to participate in the study. A self-reported, completely anonymised survey questionnaire (provided in
supplementary files) was filled out by the participants after verbal consent. All patients who were requested agreed to participate. The study was completely anonymised to encourage participation. Based on our clinic parameters, we know that all participants were known cases of testicular cancer and had successfully completed at least five years of surveillance after treatment.
2.2. Data Assessment
We designed the questionnaire to assess the self-reported impact of testicular cancer and treatment on the fertility, sexual health, and socio-economic aspects, including job and careers of TC survivors.
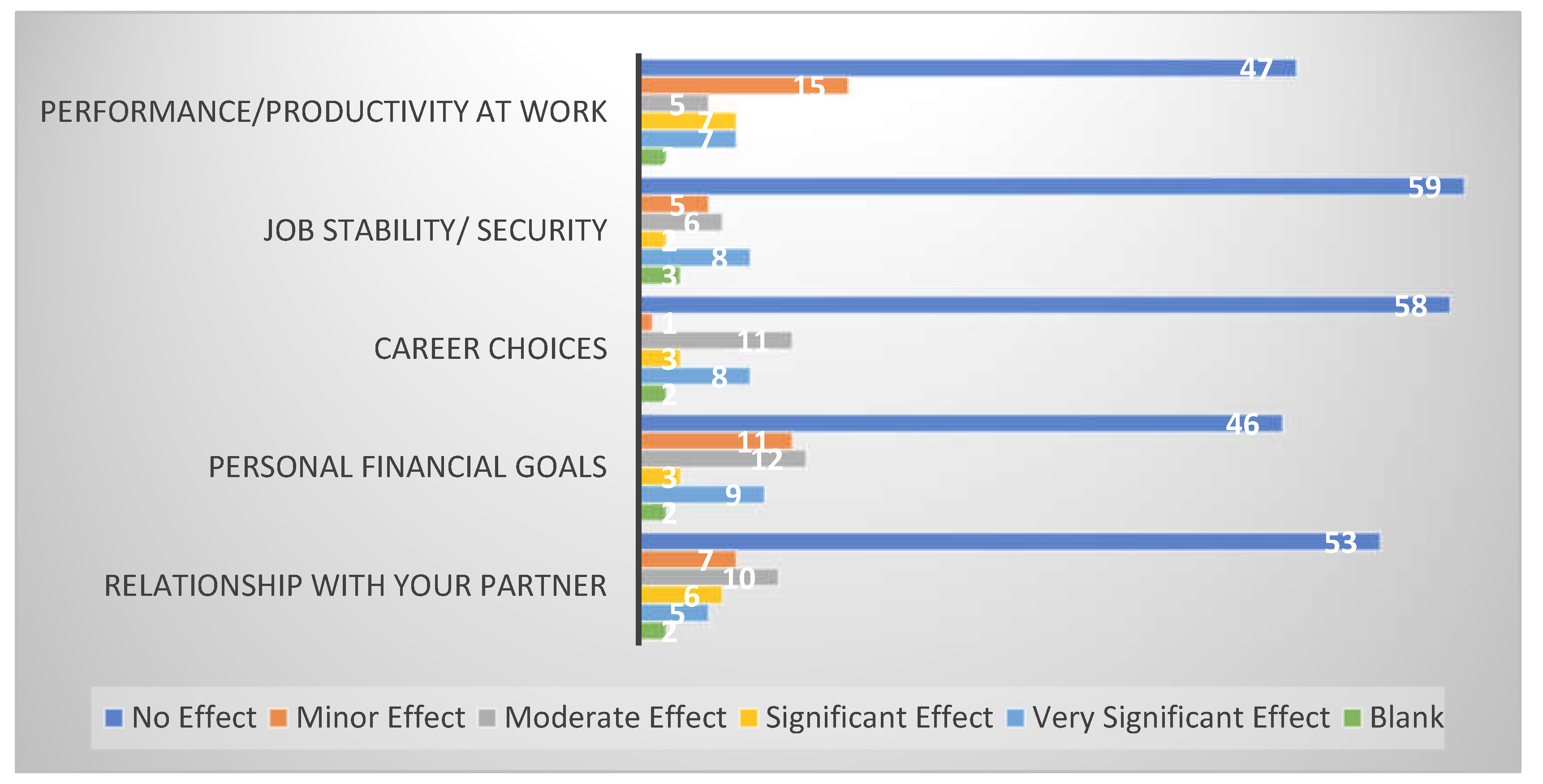
To assess the socio-economic impact, patients were asked to report the negative impact of cancer on their performance/productivity at work, job stability, career choices, personal financial goals, and the relationship with their partner. The responses were recorded as one of the five options on the Likert scale, including no effect, minor effect, moderate effect, significant effect, and very significant effect.
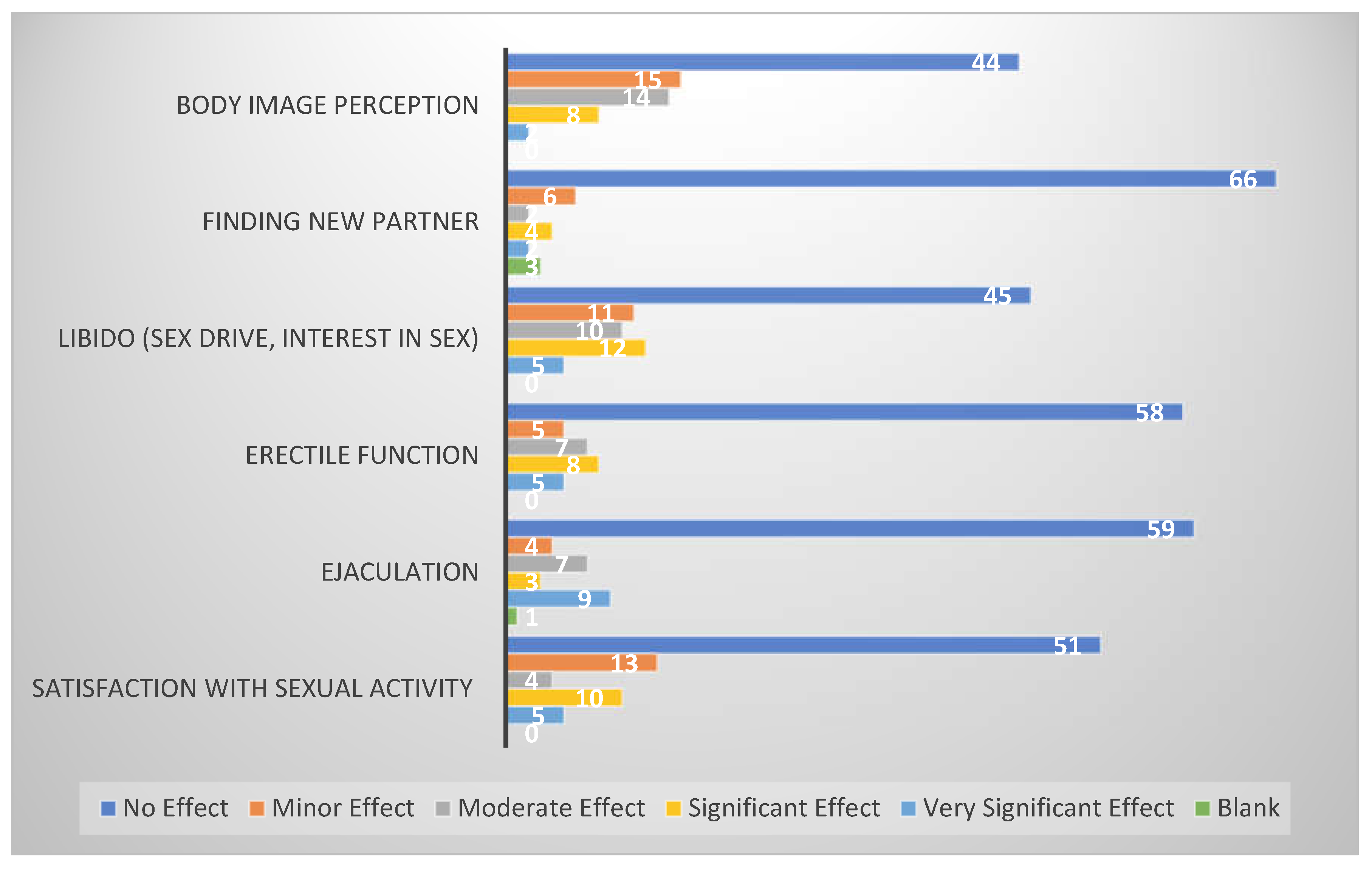
Similar responses were recorded to assess sexual health, where the patients were asked to report the extent to which the cancer and the treatment affected their body image perception, ability to find a new partner, libido, erectile function, ejaculation, and satisfaction with sexual activity.
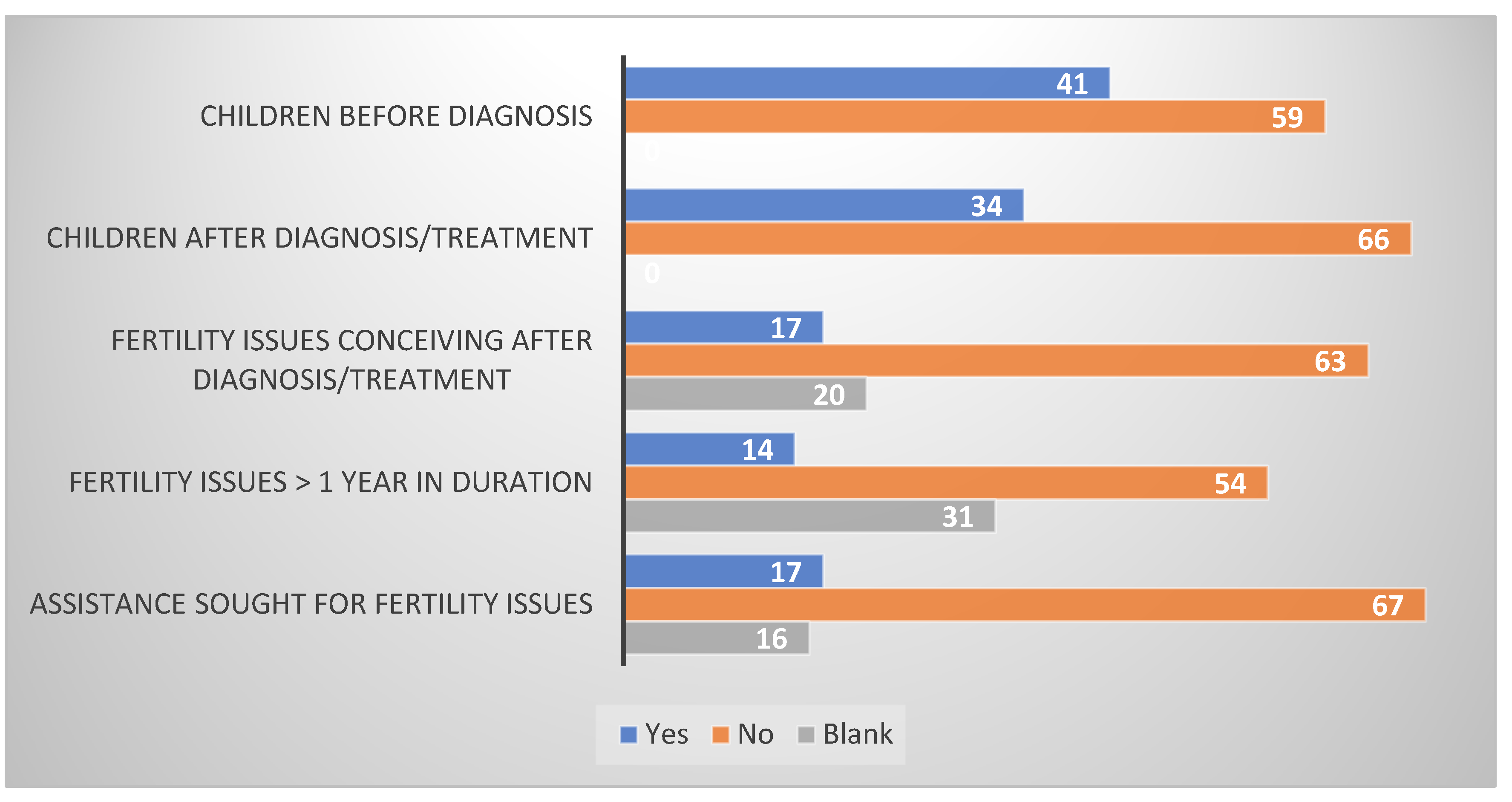
Infertility was defined as the inability to conceive after at least one year of unprotected intercourse with the partner. Participants were also asked if they attempted any medical procedures to assist fertility. We asked patients if they had any children before cancer and after cancer. Also, we inquired if they had any issues with fertility and if the issues lasted more than a year.
2.3. Statistical Analysis
All responses were recorded on the Excel-based spreadsheets. To analyse and report the responses, we calculated the percentages of total participants. Unanswered questions were reported as a blank response.
2.4. Ethics and Good Clinical Practice
The study was granted approval in full by JREC (Joint Research and Ethics Committee) of Tallaght University Hospital, Dublin. Survey questionnaires were completely anonymised to protect patient identities. All staff involved in the study were trained in ethics, data protection, and Good Clinical Practice. This study was conducted in compliance with EU and Irish ethics and data protection guidelines. Complete anonymity was maintained during data collection, processing, and analysis. Informed verbal consent was taken from participants, since written consent was not required as the questionnaires were completely anonymised without any identifiers. All authors had complete access to the data and have contributed to conceptualisation, research methodology, writing, and editing. The initial draft was written by the first and last author.
3. Results
The study was conducted from January 2023 to November 2023 in the testicular cancer survivorship clinic of Tallaght University Hospital, Dublin, Ireland. A total of 83 patients completed our survey questionnaire.
3.1. Socio-Economic Impact
To investigate the socio-economic impact on the testicular cancer survivors, we asked the participants about changes in five aspects of their livelihood since the diagnosis of cancer. These five parameters included performance/productivity at work, job security/stability, career choices, personal financial goals, and relationship with their partners (
Figure 1). When asked about performance or productivity at work, 58% reported no effect, 18% reported a minor effect, 6% a moderate effect, while 8% reported a significant and very significant effect. Regarding their job security or stability, the responses showed 72% reporting no effect, 6% a minor effect, 7% a moderate effect, 2% a significant effect, and 10% a very significant effect.
Moreover, we gauged the impact of cancer on their career choices as the majority of patients are diagnosed in the early years of their career. On one hand, 13% reported the effect as moderate and 10% reported as very significant, on the other hand, 71% of patients did not report any effect on their careers. With respect to the financial implications of cancer diagnosis and treatment, 57% of responders noted no effect on their personal financial goals. On the contrary, 11% reported very significant, 4% significant, 14% moderate and 13% minor effect.
Participants were asked if cancer had any effect on their relationship with their partners. 64% reported no effect, while the rest reported some effect. Of those who reported some effect, 27% reported a minor effect, 33% a moderate effect, 19% a significant effect, and 16% a very significant effect. 96% of participants responded to the question asking about any difficulty in finding a new partner since the diagnosis of cancer. The responses revealed that 80% of respondents did not notice any issues in this regard. Among those who experienced any difference, 43% had a minor effect, 31% a moderate effect, 31% a significant effect, while only 12% had a very significant effect.
3.2. Sexual Health
In this survey, the impact on sexual health was assessed in five different categories, including libido, erectile function, ejaculation, satisfaction with sexual activity, and body image perception (
Figure 2). Almost half of our patients (54%) did not report any effect on their libido. Although the rest of the participants stated otherwise, with 6% stating a very significant effect, 14% a significant effect, 12% a moderate effect, and 13% a minor effect. Erectile function reportedly remained intact in more than two-thirds of the respondents (70%), while it was affected very significantly in 6% and significantly in 10%. Moreover, 6% reported a minor and 8% a moderate effect. Similar to erectile function, ejaculation remained intact in 71% of patients. Conversely, 11% described the impact as very significant, 4% as significant, 8% as moderate, and 5% as minor. 39% of our testicular cancer survivors revealed an adverse impact on satisfaction with sexual activity. Of these, the majority stated only a minor to moderate effect (54%), and the rest (46%) experienced a significant or very significant effect. Almost half of patients (53%) reported that cancer didn’t affect their body image perception. At the same time, it was affected to a minor extent in 18%, moderate in 17%, significant in 10%, and very significant in 2% of participants.
3.3. Fertility
One third of the participants experienced biological parenthood after the diagnosis of cancer, whereas two thirds of them reported no children since the testicular cancer diagnosis and treatment (
Figure 3). It is important to note that nearly half of them (41%) had children before the diagnosis as per survey responses. 17% of the participants reported having trouble with conception; however, 63% did not report any issues and 20% didn’t respond. When asked if the fertility issues stayed for more than a year, 54% of them responded in the negative, but 14% were affirmative. Approximately one-third of the respondents (31%) refrained from providing an answer to the question. We asked our participants if they sought any medical assistance for fertility issues; only 17% of them stated yes, while 67% stated no and 16% chose not to answer.
4. Discussion
The majority of our patients didn’t report any major effect on their sexual and socio-economic health. Even the fertility rates after TC diagnosis and treatment were similar to the general population, as discussed below.
Spermon MD reported paternity after cancer in Norwegian TC survivors as 43% in 2003[
17], which is higher than the findings in this study (34%). This difference could be due to a general decline in fertility rates witnessed in Europe in the last couple of decades[
18]. This study is not able to identify participants who didn’t want any children. Also, a better overview can be obtained through more studies comparing paternity rates within different treatment modalities. The percentage of patients seeking medical assistance for fertility (17%) in this study is the same as reported by Spermon. The infertility rate (failure to conceive for more than 1 year) reported in our cohort of TC survivors (17%) is closer to the general population (16%)[
18].
In this study, 6% of patients reported a very significant effect on their relationship with their partner. These findings are comparable to 5-10% divorce and break-up rates reported in a study by Schepisi et al.[
12]. Another similar study at Yale University, USA, reported on the subjective impact of cancer on personal finances in survivors[
19]. 8.6% of participants reported impact as “a lot” compared to 11% in our study who reported the effect as “very significant”. However, the study at Yale was not confined to TC and included all cancer survivors.
Regarding the effect on career and job, 8-10% of responders revealed a very significant effect. Again, these findings are comparable to similar studies performed previously[
8,
19]. For instance, a major survey-based study conducted in Texas, USA, encompassing 4,363 cancer survivors, revealed that 8.5% of survivors considered themselves unable to work since diagnosis[
20]. This study included all cancer survivors, yet the results are similar to those in this study. Another study reported 67% of cancer survivors working full-time jobs after 5-7 years post-diagnosis, although some of them reported difficulties in carrying out their responsibilities[
21]. Kerns et al. also reported similar outcomes after studying 1,815 TC survivors in 2020[
8]. 10% of TC survivors were reported to be out of work, with a higher risk of unemployment compared to the age-adjusted general population (odds ratio 2.67)[
8]. They also reported a relatively higher impact on survivors who received chemotherapy[
8].
As most TC survivors are young at the age of diagnosis[
1], body image perception has a major influence on their emotional, sexual, and social well-being[
22]. Rossen et al. reported that 17% of TC survivors experienced altered body image, which was associated with all parameters of sexual dysfunction as well[
22]. However, among our cohort of survivors, only 53% reported no effect, while the rest reported some degree of effect. In the same study, 24.4% of survivors reported reduced sexual interest, which is comparable to our finding of 20% reporting a significant and very significant effect on libido[
22]. A similar trend was seen with the erectile function and satisfaction with sexual activity. Our results show 18% reporting significant or very significant effect on erectile function compared to 17% reported by Rossen et. al. With regards to satisfaction with sexual activity, 18% of our participants disclosed major effectt, compared to 14% in their study. Our participants response on the Likert scale regarding ejaculation shows a worse impact than reported in other studies. Among the respondents 15% describe the effect as significant or very significant, whereas, only 7% reported ejaculatory problems in the survey discussed above[
22]. However, a systemic review by Schesipi et. al. estimates the proportion between 29-44%[
12]. In TC survivors, ejaculatory problems are mostly related to retroperitoneal lymph node dissection and outcomes can be improved with nerve sparing techniques[
23]. This variation could possibly be due to different trends of the surgical treatments in different countries and cancer centres.
A majority (80%) of patients didn’t report any difficulties in finding a new partner, but unfortunately our survey failed to identify participants already in stable relationships.
The participation in this study was phenomenal as all the survivors we approached agreed to be a part of the study. We believe one of the main reasons for the high recruitment was the complete anonymisation of questionnaires. However, this anonymisation also proved to be a major limitation of our study. Due to anonymisation, we were not able to stratify our data based on age at diagnosis, treatment types, stage of cancer at diagnosis, co-morbidities, and social parameters, e.g., employment status, relationship status, and education level. This stratification could have been very useful to identify the risk factors for the major implications in the survivorship phase. The size of the cohort in this study was small; a multi-centre study with a larger cohort of patients could give us more significant and impactful data.
Another considerable limitation comes from the absence of any comparative cohort as a control arm. A comparable control arm of the general population could help us better define the effect of testicular cancer on these parameters.
Given the small scale of study and limitations described above, we strongly believe that more research in this area is needed. We recommend multicentre, pseudonymised and case-control studies for further insight into the subject of TC survivorship.
5. Conclusions
In this study, we have highlighted the issues being faced by the testicular cancer survivors as a result of late side-effects of cancer and its treatments. Although most of the TC survivors reported no significant effect on their socio-economic and sexual health, some of them struggle with the negative impacts. In regards to sexual health, most of the repercussions were seen on body image perception and libido while social sequelae mainly included deterioration in relationship with partner. The economic health was affected in some TCS due to job instability and reduced performance at work. Survivorship care should include these aspects of well-being and should be designed to provide support where needed.
Supplementary Materials
The following supporting information can be downloaded at the website of this paper posted on Preprints.org.
Author Contributions
Conceptualization, MRK, PKS, AB, CL, LC, RMcD.; methodology MRK, PKS, AB, CL, LC, RMcD.; software, MRK, PKS, AB, CL, LC, RMcD.; validation MRK, PKS, AB, CL, LC, RMcD.; formal analysis, MRK, PKS, AB, CL, LC, RMcD.; investigation, MRK, PKS, AB, CL, LC, RMcD.; resources, MRK, PKS, AB, CL, LC, RMcD.; data curation, MRK, PKS, AB, RMcD.; writing—original draft preparation, MRK, PKS, RMcD.; writing—review and editing, MRK, PKS, AB, CL, LC, RMcD; visualization, MRK, PKS, AB, CL, LC, RMcD.; supervision, MRK, PKS, AB, CL, LC, RMcD.; project administration, MRK, PKS, AB, CL, LC, RMcD; funding acquisition, MRK, PKS, AB, CL, LC, RMcD. All authors have read and agreed to the published version of the manuscript
Funding
This research received no external funding
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Joint Research and Ethics Committee of Tallaght University Hospital, Dublin (submission no. 2524, date of approval 14th March 2023
Informed Consent Statement
Informed verbal consent was obtained from all subjects involved in the study. Written consent was not required as the study was completely anonymised.
Data Availability Statement
In this section, please provide details regarding where data supporting reported results can be found, including links to publicly archived datasets analyzed or generated during the study. Please refer to suggested Data Availability Statements in section “MDPI Research Data Policies” at
https://www.mdpi.com/ethics. If the study did not report any data, you might add “Not applicable” here.
Acknowledgments
Cancer Trials Ireland, Tallaght University Hospital
Conflicts of Interest
The authors declare no conflict of interest
References
- Kusler, K.A. and J.N. Poynter, International testicular cancer incidence rates in children, adolescents and young adults. Cancer Epidemiology, 2018. 56: p. 106-111. [CrossRef]
- Gillessen, S. , et al., Predicting Outcomes in Men With Metastatic Nonseminomatous Germ Cell Tumors (NSGCT): Results From the IGCCCG Update Consortium. J Clin Oncol, 2021. 39(14): p. 1563-1574. [CrossRef]
- LAWRENCE, H. EINHORN, M.D., F.A.C.P., Cis-Diamminedichloroplatinum, Vinblastine, and Bleomycin Combination Chemotherapy in Disseminated Testicular Cancer. Annals of Internal Medicine, 1977. 87(3): p. 293-298. [CrossRef]
- Hanna, N. and L.H. Einhorn, Testicular Cancer: A Reflection on 50 Years of Discovery. Journal of Clinical Oncology, 2014. 32(28): p. 3085-3092. [CrossRef]
- Agrawal, V. , et al., Adverse Health Outcomes Among US Testicular Cancer Survivors After Cisplatin-Based Chemotherapy vs Surgical Management. JNCI Cancer Spectr, 2020. 4(2): p. pkz079. [CrossRef]
- Kerns, S.L. , et al., Cumulative Burden of Morbidity Among Testicular Cancer Survivors After Standard Cisplatin-Based Chemotherapy: A Multi-Institutional Study. J Clin Oncol, 2018. 36(15): p. 1505-1512. [CrossRef]
- Smith, A.B. , et al., A systematic review of quantitative observational studies investigating psychological distress in testicular cancer survivors. Psychooncology, 2018. 27(4): p. 1129-1137. [CrossRef]
- Kerns, S.L. , et al., Relationship of Cisplatin-Related Adverse Health Outcomes With Disability and Unemployment Among Testicular Cancer Survivors. JNCI Cancer Spectr, 2020. 4(4): p. pkaa022. [CrossRef]
- Nezu, K. , et al., Association of financial toxicity with quality of life in testicular cancer survivors. International Journal of Urology, 2022. 29(12): p. 1526-1534. [CrossRef]
- Fosså, S.D. , T. Åbyholm, and A. Aakvaag, Spermatogenesis and Hormonal Status after Orchiectomy for Cancer and before Supplementary Treatment. European Urology, 2017. 10(3): p. 173-177. [CrossRef]
- Jacobs, L.A. and D.J. Vaughn, Hypogonadism and Infertility in Testicular Cancer Survivors. Journal of the National Comprehensive Cancer Network J Natl Compr Canc Netw, 2012. 10(4): p. 558-563. [CrossRef]
- Schepisi, G. , et al., Psychosocial Issues in Long-Term Survivors of Testicular Cancer. Frontiers in Endocrinology, 2019. 10. [CrossRef]
- Capogrosso, P. , et al., Long-term recovery of normal sexual function in testicular cancer survivors. Asian Journal of Andrology, 2016. 18(1): p. 85-89. [CrossRef]
- Tuinman, M.A. , et al., Quality of life and stress response symptoms in long-term and recent spouses of testicular cancer survivors. European Journal of Cancer, 2004. 40(11): p. 1696-1703. [CrossRef]
- Fung, C. , et al., Testicular Cancer Survivorship. Journal of the National Comprehensive Cancer Network J Natl Compr Canc Netw, 2019. 17(12): p. 1557-1568. [CrossRef]
- Khan, M.R. , et al., 11P Impact of testicular cancer on socio-economic and sexual health of survivors: A questionnaire-based survey. ESMO Open, 2024. 9. [CrossRef]
- Spermon, J.R. , et al., Fertility in men with testicular germ cell tumors. Fertil Steril, 2003. 79 Suppl 3: p. 1543-9. [CrossRef]
- Executive, H.S. Fertility Problems. 2023 [cited 2024 25th April 2024]. Available online: https://www2.hse.ie/conditions/fertility/#:~:text=Around%201%20in%206%20heterosexual%20couples%20in%20Ireland%20have%20fertility%20problems.
- Fenn, K.M. , et al., Impact of financial burden of cancer on survivors’ quality of life. J Oncol Pract, 2014. 10(5): p. 332-8. [CrossRef]
- Schultz, P.N. , et al., Cancer survivors. Work related issues. Aaohn j, 2002. 50(5): p. 220-6. [CrossRef]
- Bradley, C.J. and H.L. Bednarek, Employment patterns of long-term cancer survivors. Psycho-Oncology, 2002. 11(3): p. 188-198. [CrossRef]
- Rossen, P. , et al., Sexuality and body image in long-term survivors of testicular cancer. European Journal of Cancer, 2012. 48(4): p. 571-578. [CrossRef]
- Pettus, J.A. , et al., Preservation of ejaculation in patients undergoing nerve-sparing postchemotherapy retroperitoneal lymph node dissection for metastatic testicular cancer. Urology, 2009. 73(2): p. 328-31; discussion 331-2. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).