Submitted:
28 April 2025
Posted:
30 April 2025
Read the latest preprint version here
Abstract
Human psychology has been playing major contributory factors in the calibration of human medicine, as it is cognitive perception that has ultimately shaped the trajectory of medical progress. Such perceptive patterns are dependent upon the integrity of emotional and intellectual levels of intelligence, meaning that good emotional states can significantly contribute to shaping medical and scientific progress. Throughout the paper, the topic of the progressive loss of balance in societal perspectives, attitudes and behaviours will be thoroughly assessed, given that such loss of balance often results in a phenomenon known as “throwing the baby out with the bathwater”, in which good values are rooted out with the bad habits infiltrated into emerged branches. For example, the increasing epidemic of loneliness, isolation and deprivation of affection has resulted in the creation of an inaccurate perception upon the importance of solitude and self-reflection due to a generated excessive emotion of craving for human affection, which has often translated into practices of dependency upon social contexts, attachment to mismatching relationships, promiscuity and unhealthy, unexplained abandonment. Such increasing events have created unprecedented frictions within societies, which resulted in the skyrocketed extent of trust issues and isolation among people and consequently, to a steep decline in the average extent of human mental health and emotional wellbeing. Such societal frictions have significantly manifested even within biological families, which itself represents a direct factor for the recent increase in the number of people registered as “homeless”. It is therefore evident that loneliness and homelessness represent two opposite ends of the same sequence of events, as homelessness is ultimately dependent upon loneliness and isolation. The author will be presenting an extensive set of theoretical and practical solutions against the ongoing and growing problem of the existing frictions within human relationships by encouraging proportional workshops and novel lifestyles aimed at gradually repairing the created damages of human trust, with an emphasis upon distributing existing projects of “mental health first aid”, “cuddle therapy”, “cuddled bed & breakfast”, “artistic expressions aimed at deepening healthy human connection”, consensually “singing lullabies to each other and therapeutically swinging one another to sleep”, as well as other similar practices, even incorporating them into regular housing, which may be regarded as “cuddled renting” or “housing”; as well as workshops in retreat and camping settings, alongside the creation of theoretical and practical courses to help each participating member apprehend the depth of the details covering consent, boundaries, as well as health and safety - offering either low-cost or free courses to members of the general public on creating safe spaces and meaningful, profound and long-lasting connections by widening the availability of such resources in an exponential manner, subsequently reducing the need for significant, localised financial expenditure per initiative and perhaps obtaining funding from specific non-governmental organisations (NGOs), with the overall purpose of ensuring that the UN’s Sustainable Development Goals are met by 2030. Moreover, efforts could also be made to rebuild natural environments in areas where harm has been caused by pollution - given the existence of an interdependent relationship between the integrities of the environment and of life. There could be a gradual evolution from “local cuddled communities” into broad rural and urban areas dedicated to intentional, regular and conscious human connection, potentially perfecting the concept of “Smart Cities” whilst implementing it under real-world conditions. It is known that life emerges from the water and that, immediately after the new-born human is separated from the amniotic water after nine months of pregnancy, is united with the mother in a long and profound hug; hence, affection is as important for human survival as water. Normative levels of human affection should be proportional to the levels observed in animals, as all life forms physically emerge from water, bacteria and soil. Given that Albert Einstein’s Theory of Relativity may apply to human and animal psychology - at the levels of perception and intelligence - it may be important to make differentiations between the speed of animal bonding and the speed of human bonding proportionally with the displayed levels of intelligence and wisdom, given that intelligence may generally be proportional with a perceived speed of time, meaning overall that caution and social selection ultimately occur as significantly in animals as they do in humans, and that boundaries are as essential in animal bonding as they are in human bonding. Scientific evidence indicates that regular practices of “hugging” and “cuddling” are associated with optimised immune systems, lower probabilities to develop various types of illnesses, increased quality and extent of physical, emotional, neuronal and intellectual development during childhood and teenage years, as well as increased duration of life. Overall, platonic intimacy represents the most important, profound and sophisticated form of art that brings all forms of sensorial art into a complete state of “oneness”, reflecting the objective of human existence herself. The objective of extending platonic intimacy to regular life would also implicate the introduction of cuddle-optional safe spaces into settings that include foster care homes, elderly care homes, kindergartens, schools, youth centres, homeless shelters, emergency housing centres and accommodation support networks, centres for suicide prevention, points of mental health crisis alleviation, disability service centres, palliative care centres, hospitals and other medical centres, as well as addiction recovery centres and prisons, with all laws and guidelines on safeguarding children and vulnerable people, respecting personal boundary, informed consent, as well as Health and Safety respected to the letter. It is only when such an importance is theoretically and practically understood, and when numerous people gently and patiently climb through the existing many hierarchies of intimacy that people will successfully find compatibility and thorough fulfilment in their romantic life as well.
Keywords:
Introduction
Methodology
Discussion
Conclusions
References
- Miller G. (2011). Social neuroscience. Why loneliness is hazardous to your health. Science (New York, N.Y.), 331(6014), 138–140. [CrossRef]
- Cacioppo, S., Grippo, A. J., London, S., Goossens, L., & Cacioppo, J. T. (2015). Loneliness: clinical import and interventions. Perspectives on psychological science: a journal of the Association for Psychological Science, 10(2), 238–249. [CrossRef]
- von Känel, R., Weilenmann, S., & Spiller, T. R. (2021). Loneliness Is Associated with Depressive Affect, But Not with Most Other Symptoms of Depression in Community-Dwelling Individuals: A Network Analysis. International journal of environmental research and public health, 18(5), 2408. [CrossRef]
- Tillinghast E. (2024). Selected for Solitude: A Case Report of Loneliness. Psychodynamic psychiatry, 52(2), 206–217. [CrossRef]
- Loboprabhu, S., & Molinari, V. (2012). Severe loneliness in community-dwelling aging adults with mental illness. Journal of psychiatric practice, 18(1), 20–28. [CrossRef]
- Hughes, G., Moore, L., Hennessy, M., Sandset, T., Jentoft, E. E., & Haldar, M. (2024). What kind of a problem is loneliness? Representations of connectedness and participation from a study of telepresence technologies in the UK. Frontiers in Digital Health, 6, 1304085. [CrossRef]
- Krause-Parello C. A. (2012). Pet ownership and older women: the relationships among loneliness, pet attachment support, human social support, and depressed mood. Geriatric nursing (New York, N.Y.), 33(3), 194–203. [CrossRef]
- Krause-Parello C. A. (2008). The mediating effect of pet attachment support between loneliness and general health in older females living in the community. Journal of community health nursing, 25(1), 1–14. [CrossRef]
- Zasloff, R. L., & Kidd, A. H. (1994). Loneliness and pet ownership among single women. Psychological reports, 75(2), 747–752. [CrossRef]
- Jordan, J. V. (2020). Relational-Cultural Theory: Fostering Connection to Heal Trauma. Women & Therapy, 43(3-4), 278–294.
- Kilpatrick, D. G., & Acierno, R. (2020). Mental Health Needs of Homeless Populations. Current Opinion in Psychiatry, 33(3), 231–236. [CrossRef]
- Lynch, M., & LaSala, M. C. (2011). The ethical boundaries of safeguarding in professional and intimate relationships. Journal of Social Work Values and Ethics, 8(1), 14–22.
- Reed, B., & Boddy, J. (2016). Safeguarding boundaries in care: A comprehensive framework for ethical practice. Journal of Ethics and Social Work, 20(4), 433–448.
- Tannen, D. (1990). You just don't understand: Women and men in conversation. Ballantine Books.
- Lundgren, R. E., & Amin, A. (2015). Addressing intimate partner violence and sexual violence: A global health perspective. The Lancet, 385(9977), 155–163.
- Berg, J. H., & McQuinn, C. L. (2009). Platonic intimacy: Interpersonal and relational outcomes of non-sexual physical touch. The Journal of Social and Personal Relationships, 26(1), 52-69.
- Bowen, E. A., & Irish, A. (2021). A Trauma-Informed Approach to Mental Health Services in Homeless Shelters. Social Work, 66(2), 121–130. [CrossRef]
- Brown, B. (2021). Atlas of the Heart: Mapping Meaningful Connection and the Language of Human Experience. Random House. [CrossRef]
- Bryant, J., & Ellard, D. (2020). Boundaries in Psychological Treatment: A Review. Clinical Psychology Review, 81, 101893. [CrossRef]
- Cloitre, M. (2021). Trauma Recovery: Research and Practice. Annual Review of Clinical Psychology, 17, 1–23.
- DeCandia, C. J., & Guarino, K. (2022). Implementing Trauma-Informed Care in Homeless Shelters: A Practice Framework. Journal of Social Distress and Homelessness, 31(1), 43–55.
- Zerger, S., Bacon, S., & Corneau, S. (2021). Mental Health Care for Homeless People: Challenges and Opportunities. Canadian Journal of Psychiatry, 66(5), 416–425.
- Pfohl, M., & Brown, E. (2014). The role of physical touch in homelessness services: A review of case studies. Journal of Homelessness & Social Work, 6(2), 85-101.
- Hall, L. A., & Williams, R. C. (2017). Effects of nurturing touch in caregiving for the homeless: A field study. Journal of Human Services, 41(2), 93-104.
- Kohrt, B. A., & Mendenhall, E. (2021). Global Mental Health: Anthropological Perspectives. Routledge.
- Levine, P. A. (2020). Trauma and Memory: Brain and Body in a Search for the Living Past. North Atlantic Books. [CrossRef]
- Pinals, D. A. (2020). Correctional Settings and Trauma-Informed Care. Psychiatric Services, 71(2), 123–129.
- Lewis, S. J., & Wainwright, S. P. (2021). Boundaries and Ethical Care in Palliative Settings. Journal of Medical Ethics, 47(9), 630–635. [CrossRef]
- Marmot, M. (2020). Social Determinants of Health Inequalities. The Lancet, 395(10234), 1129–1140.
- Mollica, R. F. (2021). Healing Invisible Wounds: Paths to Hope and Recovery. Harvard University Press.
- Mueser, K. T., & Gingerich, S. (2020). The Recovery Model of Mental Illness: A Comprehensive Guide. Guilford Press. [CrossRef]
- Calati, R., Ferrari, C., Brittner, M., Oasi, O., Olié, E., Carvalho, A. F., & Courtet, P. (2019). Suicidal thoughts and behaviors and social isolation: A narrative review of the literature. Journal of affective disorders, 245, 653–667. [CrossRef]
- McClelland, H., Evans, J. J., & O'Connor, R. C. (2023). The association of family, social and romantic loneliness in relation to suicidal ideation and self-injurious behaviours. Journal of psychiatric research, 158, 330–340. [CrossRef]
- Bertram, F., Heinrich, F., Fröb, D., Wulff, B., Ondruschka, B., Püschel, K., König, H. H., & Hajek, A. (2021). Loneliness among Homeless Individuals during the First Wave of the COVID-19 Pandemic. International journal of environmental research and public health, 18(6), 3035. [CrossRef]
- Cohen, S., & Wills, T. A. (1985). Stress, social support, and the buffering hypothesis. Psychological Bulletin, 98(2), 310–357.
- Baumeister, R. F., & Leary, M. R. (1995). The need to belong: Desire for interpersonal attachments as a fundamental human motivation. Psychological Bulletin, 117(3), 497–529. [CrossRef]
- Lupton, D. (2013). The social worlds of the healthcare professional: Exploring the emotional and relational aspects of healthcare practice. Routledge.
- Hurley, D. M., & McKenna, J. L. (2020). Therapeutic touch in trauma recovery: A review of touch therapies for survivors of trauma. Journal of Traumatic Stress, 33(4), 793–801. [CrossRef]
- Senn, C. Y., & Radtke, L. (2010). Consent and the experience of platonic and sexual intimacy: Perceptions of university students. Journal of Social and Personal Relationships, 27(5), 658–673.
- Lammers, J., Stoker, J. I., Jordan, J., Pollmann, M., & Fischer, A. H. (2011). Power increases infidelity among men and women. Psychological Science, 22(9), 1191–1197. [CrossRef]
- Beck, J. G., & Clapp, J. D. (2011). Posttraumatic stress disorder in survivors of intimate partner violence: Prevalence, correlates, and treatment outcomes. Clinical Psychology Review, 31(3), 389–401. [CrossRef]
- Sullivan, H. S. (1953). The interpersonal theory of psychiatry. Norton & Company.
- Koelsch, S., & Siebel, W. A. (2005). Towards a neuroscience of music and emotion: Implications for music therapy. Music Therapy Perspectives, 23(2), 128–137.
- Seppälä, E. M., Rossomando, T. A., & Doty, J. R. (2013). Social connection and compassion: Important predictors of health and well-being. Social and Personality Psychology Compass, 7(12), 883–894. [CrossRef]
- Radfar, A., Ferreira, M. M., Sosa, J. P., & Filip, I. (2021). Emergent Crisis of COVID-19 Pandemic: Mental Health Challenges and Opportunities. Frontiers in psychiatry, 12, 631008. [CrossRef]
- Saha, K., Torous, J., Caine, E. D., & De Choudhury, M. (2020). Psychosocial Effects of the COVID-19 Pandemic: Large-scale Quasi-Experimental Study on Social Media. Journal of medical Internet research, 22(11), e22600. [CrossRef]
- Adikari, A., Nawaratne, R., De Silva, D., Ranasinghe, S., Alahakoon, O., & Alahakoon, D. (2021). Emotions of COVID-19: Content Analysis of Self-Reported Information Using Artificial Intelligence. Journal of medical Internet research, 23(4), e27341. [CrossRef]
- Huang, Y., Liu, H., Zhang, L., Li, S., Wang, W., Ren, Z., Zhou, Z., & Ma, X. (2021). The Psychological and Behavioral Patterns of Online Psychological Help-Seekers before and during COVID-19 Pandemic: A Text Mining-Based Longitudinal Ecological Study. International journal of environmental research and public health, 18(21), 11525. [CrossRef]
- Bowlby, J. (1988). A secure base: Parent-child attachment and healthy human development. Routledge.
- Bath, H. (2021). The Three Pillars of Trauma-Informed Care. Reclaiming Children and Youth, 30(1), 5–12.
- Eisenberger, N. I., & Lieberman, M. D. (2004). Why rejection hurts: A common neural alarm system for physical and social pain. Trends in Cognitive Sciences, 8(7), 294–300. [CrossRef]
- Perry, B. D., & Szalavitz, M. (2017). The boy who was raised as a dog: And other stories from a child psychiatrist’s notebook—What traumatized children can teach us about loss, love, and healing. Basic Books.
- Meherali, S., Punjani, N., Louie-Poon, S., Abdul Rahim, K., Das, J. K., Salam, R. A., & Lassi, Z. S. (2021). Mental Health of Children and Adolescents Amidst COVID-19 and Past Pandemics: A Rapid Systematic Review. International journal of environmental research and public health, 18(7), 3432. [CrossRef]
- Felitti, V. J., & Anda, R. F. (2020). The Relationship of Adverse Childhood Experiences to Adult Health. American Journal of Preventive Medicine, 58(3), 345–352. [CrossRef]
- Read, J., & Bentall, R. (2020). Negative Childhood Experiences and Adult Mental Health. Psychology and Psychotherapy, 93(1), 20–37. [CrossRef]
- Walker, P. (2021). Complex PTSD: From Surviving to Thriving. Skylight Press. [CrossRef]
- White, R., & Satyen, L. (2020). Cross-Cultural Boundaries in Trauma Practice. International Journal of Stress Management, 27(1), 12–24. [CrossRef]
- Fisher, J. (2021). Transforming the Living Legacy of Trauma: A Workbook for Survivors and Therapists. PESI Publishing. [CrossRef]
- Ghaemi, S. N. (2021). The Importance of Humanistic Care in Modern Psychiatry. Journal of Psychiatric Research, 142, 356–361. [CrossRef]
- Goodman, L. A., Fels Smyth, K., Borges, A. M., & Fallot, R. D. (2022). Advancing Trauma-Informed Care for Marginalized Populations. Traumatology, 28(2), 84–95. [CrossRef]
- Green, B. L., & Engel, C. C. (2020). Trauma-Informed Primary Care: A New Paradigm. Families, Systems, & Health, 38(2), 163–174. [CrossRef]
- Harris, M., & Fallot, R. D. (Eds.). (2021). Using Trauma Theory to Design Service Systems. Jossey-Bass.
- Tronick, E. Z. (2007). The neurobiology of trauma and the role of human connection in healing. International Journal of Psychoanalysis, 88(4), 785–797. [CrossRef]
- Meyer, B., & Luce, K. (2016). The psychology of human touch and its implications for therapy. Journal of Humanistic Psychology, 56(2), 123–135.
- Cloninger, C. R., & Zohar, A. H. (2011). Personality and the perception of well-being: New insights into the relationship between personality traits and well-being. The Journal of Positive Psychology, 6(6), 466–478.
- Shaver, P. R., & Mikulincer, M. (2012). Attachment theory and research: Reshaping the framework for understanding intimate relationships. Current Directions in Psychological Science, 21(5), 275–279.
- Spence, S. H., & Rapee, R. M. (2010). Social anxiety disorder and emotional regulation. In P. M. Barrett & M. P. Trower (Eds.), The handbook of emotional regulation (pp. 233-246). Oxford University Press.
- Chung, M. C., & Lee, S. Y. (2017). Caring touch, empathy, and healing in clinical settings: A study of nurses and healthcare professionals. Journal of Clinical Nursing, 26(1–2), 52–63. [CrossRef]
- Paluszek, M. M., & Weisberg, R. B. (2014). The impact of social connection on emotional well-being and healing after trauma. Journal of Affective Disorders, 166, 50–58. [CrossRef]
- Neff, K. D. (2011). Self-compassion, self-esteem, and well-being. Social and Personality Psychology Compass, 5(1), 1–12. [CrossRef]
- Freeman, L. C., & Damasio, A. R. (2016). The role of emotional support and connection in the body’s recovery from trauma. Human Brain Mapping, 37(9), 3451–3462. [CrossRef]
- Dunlap, E., & Siegel, A. (2009). Psychological and social factors in trauma recovery: Understanding human connection in healing. Trauma and Recovery, 28(2), 131–145.
- Cox, D., & Brissette, I. (2010). Attachment and healing: Social bonds and recovery from trauma. Journal of Personality and Social Psychology, 99(4), 696–709. [CrossRef]
- Hopper, E. K., Bassuk, E. L., & Olivet, J. (2020). Shelter from the Storm: Trauma-Informed Care in Homelessness Services. Open Health Services and Policy Journal, 13(1), 1–9.
- Rice, C. (2020). Trauma-Informed Leadership in Health and Social Care. Leadership in Health Services, 33(1), 73–83.
- Roper, C., Grey, F., & Cadogan, E. (2021). Co-Production and Trauma-Informed Approaches. Mental Health and Social Inclusion, 25(2), 106–117.
- Sweeney, A., Clement, S., Filson, B., & Kennedy, A. (2022). Trauma-Informed Mental Healthcare in the UK. British Journal of Psychiatry, 220(5), 308–316. [CrossRef]
- Treisman, K. (2020). A Treasure Box for Creating Trauma-Informed Organizations. Jessica Kingsley Publishers. [CrossRef]
- Harlow, H. F., & Harlow, M. K. (1962). The nature of love. American Psychologist, 17(12), 900-909. [CrossRef]
- Barnett, M. A. (2002). Social touch, stress, and health in adult humans: A review. The Journal of Social Psychology, 142(2), 233-245.
- Field, T. (2001). Massage therapy research review. The Journal of Alternative and Complementary Medicine, 7(1), 71-89.
- Field, T., Diego, M., & Hernandez-Reif, M. (2007). Massage therapy reduces anxiety and depression in children with autism. Journal of Autism and Developmental Disorders, 37(4), 647-653.
- McGowan, B., & Kastenbaum, R. (2016). The power of touch in restorative practices: Exploring the role of physical touch in rehabilitation. Journal of Restorative Justice, 4(2), 192-204.
- Yim, E. D., & Scherer, L. D. (2018). The healing touch: Emotional benefits of human touch in vulnerable populations. Psychological Science, 29(12), 1725-1731.
- Coan, J. A., & Schaefer, H. S. (2006). The influence of spouse support on stress and cardiovascular function. Psychological Science, 17(12), 930-937. [CrossRef]
- Hertenstein, M. J., & Keltner, D. (2006). Touch communicates distinct emotions. Emotion, 6(3), 557-561.
- Porges, S. W. (2011). The polyvagal theory: Neurophysiological foundations of emotions, attachment, communication, and self-regulation. Norton & Company.
- Klemm, W. R. (2019). Human touch in clinical practice: A review of studies on physical contact in therapy. The Journal of Clinical Nursing, 28(12), 2153-2161. [CrossRef]
- Kim, Y., & Lee, H. (2016). The impact of physical touch on stress hormones and immune system in patients with chronic illness. Clinical Psychology Review, 46, 25-36. [CrossRef]
- Lee, S., & Choi, J. (2020). Exploring the relationship between physical touch and emotional regulation in clinical settings. Journal of Clinical Psychology, 76(1), 110-117. [CrossRef]
- Fisher, J. B., & Fredrickson, B. L. (2008). The role of social support and touch in maintaining health and wellbeing. Psychosomatic Medicine, 70(7), 840-850.
- Smith, R., & Wadsworth, A. (2017). Effects of cuddling and emotional support on stress and anxiety levels in adults. Journal of Health Psychology, 22(6), 749-758.
- Panksepp, J., & Burgdorf, J. (2003). Neurochemical mechanisms of emotional support: The role of touch in mental health. Psychiatry Research, 120(1), 99-106.
- Porges, S. W. (2011). The polyvagal theory: Neurophysiological foundations of emotions, attachment, communication, and self-regulation. Norton & Company.
- Kim, Y., & Lee, H. (2016). The impact of physical touch on stress hormones and immune system in patients with chronic illness. Clinical Psychology Review, 46, 25-36. [CrossRef]
- Lee, S., & Choi, J. (2020). Exploring the relationship between physical touch and emotional regulation in clinical settings. Journal of Clinical Psychology, 76(1), 110-117. [CrossRef]
- Klemm, W. R. (2019). Human touch in clinical practice: A review of studies on physical contact in therapy. The Journal of Clinical Nursing, 28(12), 2153-2161. [CrossRef]
- Harlow, H. F., & Harlow, M. K. (1962). The nature of love. American Psychologist, 17(12), 900-909. [CrossRef]
- Myers, S., & Snow, B. (2021). Snuggle therapy and the mental health effects of secure physical touch in individuals with trauma histories. Journal of Trauma & Stress Disorders, 34(3), 193-205.
- Kinner, S. A., & Wang, M. L. (2020). Reentry for people released from prison: The role of supportive relationships. Journal of Offender Rehabilitation, 59(5), 401-420.
- O’Donnell, L., & McHugh, P. (2017). Prison reintegration and the role of social bonds in recovery. Journal of Correctional Health Care, 23(4), 351-359.
- Yates, C. (2019). Touch therapy as an adjunct in prison reintegration programs. Journal of Offender Rehabilitation, 58(2), 121-135.
- Spencer, P. G., & Kerr, T. (2018). The healing power of touch in post-incarceration adjustment. Journal of Human Behavior in the Social Environment, 28(7), 801-815.
- Carson, E. A., & Golinelli, D. (2015). Examining the health effects of social touch for vulnerable populations: A longitudinal study. Public Health Reports, 130(6), 582-589. [CrossRef]
- Fink, G., & Blanchard, D. C. (2007). Physical touch and its impact on psychological distress: A meta-analysis of touch therapy studies. Psychoneuroendocrinology, 32(6), 632-638. [CrossRef]
- Gelman, M. A., & Brown, K. (2013). The role of emotional touch in reducing cortisol in traumatized individuals. Traumatology, 19(3), 169-177.
- Silverstein, M., & Williams, J. (2015). Enhancing wellbeing through human connection: The role of touch in therapy for the incarcerated. Journal of Offender Rehabilitation, 53(2), 140-152.
- Ferguson, A. D., & Wong, S. (2020). Exploring how physical comfort and human touch affect post-traumatic stress recovery. Journal of Trauma Recovery, 22(4), 315-325.
- Yang, X., Yip, B. H. K., Mak, A. D. P., Zhang, D., Lee, E. K. P., & Wong, S. Y. S. (2021). The Differential Effects of Social Media on Depressive Symptoms and Suicidal Ideation Among the Younger and Older Adult Population in Hong Kong During the COVID-19 Pandemic: Population-Based Cross-sectional Survey Study. JMIR public health and surveillance, 7(5), e24623. [CrossRef]
- Hiemke, C., & Härtter, S. (2000). Pharmacokinetics of selective serotonin reuptake inhibitors. Pharmacology & therapeutics, 85(1), 11–28. [CrossRef]
- Casarotto, P. C., Girych, M., Fred, S. M., Kovaleva, V., Moliner, R., Enkavi, G., Biojone, C., Cannarozzo, C., Sahu, M. P., Kaurinkoski, K., Brunello, C. A., Steinzeig, A., Winkel, F., Patil, S., Vestring, S., Serchov, T., Diniz, C. R. A. F., Laukkanen, L., Cardon, I., Antila, H., … Castrén, E. (2021). Antidepressant drugs act by directly binding to TRKB neurotrophin receptors. Cell, 184(5), 1299–1313.e19. [CrossRef]
- Rantamäki T. (2019). TrkB neurotrophin receptor at the core of antidepressant effects, but how?. Cell and tissue research, 377(1), 115–124. [CrossRef]
- Sapolsky R. M. (2005). The influence of social hierarchy on primate health. Science (New York, N.Y.), 308(5722), 648–652. [CrossRef]
- Iyer P. (2018). From rakhi to romance: negotiating 'acceptable' relationships in co-educational secondary schools in New Delhi, India. Culture, health & sexuality, 20(3), 306–320. [CrossRef]
- Twamley K. (2013). Love and desire amongst middle-class Gujarati Indians in the UK and India. Culture, health & sexuality, 15(3), 327–340. [CrossRef]
- Berscheid E. (2010). Love in the fourth dimension. Annual review of psychology, 61, 1–25. [CrossRef]
- Bergner R. M. (2000). Love and barriers to love. An analysis for psychotherapists and others. American journal of psychotherapy, 54(1), 1–17. [CrossRef]
- Lemay, E. P., Jr, & Spongberg, K. (2015). Perceiving and Wanting to Be Valued by Others: Implications for Cognition, Motivation, and Behavior in Romantic Relationships. Journal of personality, 83(4), 464–478. [CrossRef]
- Higginbottom B. (2024). The Nuances of Intimacy: Asexual Perspectives and Experiences with Dating and Relationships. Archives of sexual behavior, 53(5), 1899–1914. [CrossRef]
- Stromberg D. (2018). Good and Bad: Love and Intimacy From Plato to Melanie Klein. American journal of psychoanalysis, 78(2), 159–181. [CrossRef]
- Recht L. (2017). The Wheel and the Ladder: Freudian and Loewaldian Accounts of Individuation. Psychoanalytic review, 104(3), 313–350. [CrossRef]
- Austin, B. A. (1983). Factorial structure of the UCLA Loneliness Scale. Psychological Reports, 53(3), 883-889. [CrossRef]
- Russell, D.W., 1996. UCLA Loneliness Scale (Version 3): Reliability, validity, and factor structure. Journal of personality assessment, 66(1), pp.20-40. [CrossRef]
- Neto, F. (2014). Psychometric analysis of the short-form UCLA Loneliness Scale (ULS-6) in older adults. European journal of ageing, 11, 313-319. [CrossRef]
- Tennant, R., Hiller, L., Fishwick, R., Platt, S., Joseph, S., Weich, S., ... & Stewart-Brown, S. (2007). The Warwick-Edinburgh mental well-being scale (WEMWBS): development and UK validation. Health and Quality of life Outcomes, 5, 1-13. [CrossRef]
- Stewart-Brown, S. L., Platt, S., Tennant, A., Maheswaran, H., Parkinson, J., Weich, S., ... & Clarke, A. (2011). The Warwick-Edinburgh Mental Well-being Scale (WEMWBS): a valid and reliable tool for measuring mental well-being in diverse populations and projects. J Epidemiol Community Health, 65(Suppl 2), A38-A39. https://jech.bmj.com/content/65/Suppl_2/A38.2. [CrossRef]
- Taggart, F., Friede, T., Weich, S., Clarke, A., Johnson, M., & Stewart-Brown, S. (2013). Cross cultural evaluation of the Warwick-Edinburgh mental well-being scale (WEMWBS)-a mixed methods study. Health and Quality of Life Outcomes, 11, 1-12. [CrossRef]
- Keselman, H. J., Huberty, C. J., Lix, L. M., Olejnik, S., Cribbie, R. A., Donahue, B., ... & Levin, J. R. (1998). Statistical practices of educational researchers: An analysis of their ANOVA, MANOVA, and ANCOVA analyses. Review of educational research, 68(3), 350-386. [CrossRef]
- Zhou, Y., & Skidmore, S. T. (2017). A reassessment of ANOVA reporting practices: A review of three APA journals. Journal of Methods and Measurement in the Social Sciences, 8(1), 3-19. [CrossRef]
- Kramer, M., & Schmidhammer, J. (1992). The chi-squared statistic in ethology: use and misuse. Animal Behaviour, 44(5), 833-841. [CrossRef]
- Hélie, S. (2007). Understanding statistical power using noncentral probability distributions: Chi-squared, G-squared, and ANOVA. Tutorials in Quantitative Methods for Psychology, 3(2), 63-69. [CrossRef]
- Wetzels, R., Matzke, D., Lee, M. D., Rouder, J. N., Iverson, G. J., & Wagenmakers, E. J. (2011). Statistical evidence in experimental psychology: An empirical comparison using 855 t tests. Perspectives on Psychological Science, 6(3), 291-298. [CrossRef]
- Delacre, M., Lakens, D., & Leys, C. (2017). Why psychologists should by default use Welch's t-test instead of Student's t-test. International Review of Social Psychology, 30(1), 92-101. [CrossRef]
- Lakens, D. (2017). Equivalence tests: A practical primer for t tests, correlations, and meta-analyses. Social psychological and personality science, 8(4), 355-362. [CrossRef]
- GROSSMAN C. M. (1965). TRANSFERENCE, COUNTERTRANSFERENCE, AND BEING IN LOVE. The Psychoanalytic quarterly, 34, 249–256.
- Karila, L., Wéry, A., Weinstein, A., Cottencin, O., Petit, A., Reynaud, M., & Billieux, J. (2014). Sexual addiction or hypersexual disorder: different terms for the same problem? A review of the literature. Current pharmaceutical design, 20(25), 4012–4020. [CrossRef]
- Kellett, S., Simmonds-Buckley, M., & Totterdell, P. (2017). Testing the Effectiveness of Cognitive Analytic Therapy for Hypersexuality Disorder: An Intensive Time-Series Evaluation. Journal of sex & marital therapy, 43(6), 501–516. [CrossRef]
- Werner, M., Štulhofer, A., Waldorp, L., & Jurin, T. (2018). A Network Approach to Hypersexuality: Insights and Clinical Implications. The journal of sexual medicine, 15(3), 373–386. [CrossRef]
- Stefanska, E. B., Longpré, N., & Rogerson, H. (2024). Relationship Between Atypical Sexual Fantasies, Behavior, and Pornography Consumption. International journal of offender therapy and comparative criminology, 68(9), 915–935. [CrossRef]
- Molen, L. V., Ronis, S. T., & Benoit, A. A. (2023). Paraphilic Interests Versus Behaviors: Factors that Distinguish Individuals Who Act on Paraphilic Interests From Individuals Who Refrain. Sexual abuse : a journal of research and treatment, 35(4), 403–427. [CrossRef]
- Chan, H. C. (2021). Paraphilic interests: The role of psychosocial factors in a sample of young adults in Hong Kong. Sexuality Research and Social Policy, 1-20. [CrossRef]
- Bergmann M. S. (1982). Platonic love, transference love, and love in real life. Journal of the American Psychoanalytic Association, 30(1), 87–111. [CrossRef]
- Bergmann M. S. (1985). Transference love and love in real life. International journal of psychoanalytic psychotherapy, 11, 27–51.
- Benayah, C., & Stern, M. (1994). Transference-countertransference: realizing a love by not actualizing it. The Israel journal of psychiatry and related sciences, 31(2), 94–105.
- Cohen Y. (2006). Loving the patient as the basis for treatment. American journal of psychoanalysis, 66(2), 139–155. [CrossRef]
- Nordmo, M., Næss, J. Ø., Husøy, M. F., & Arnestad, M. N. (2020). Friends, Lovers or Nothing: Men and Women Differ in Their Perceptions of Sex Robots and Platonic Love Robots. Frontiers in psychology, 11, 355. [CrossRef]
- Fitzroy, A. F., Kemp, C. L., & Burgess, E. O. (2022). "I'm not terribly lonely": Advancing the understanding of intimacy among older adults. Journal of aging studies, 61, 101005. [CrossRef]
- Marshall W. L. (1989). Intimacy, loneliness and sexual offenders. Behaviour research and therapy, 27(5), 491–503. [CrossRef]
- Lau, W. K., Ngan, L. H., Chan, R. C., Wu, W. K., & Lau, B. W. (2021). Impact of COVID-19 on pornography use: Evidence from big data analyses. PloS one, 16(12), e0260386. [CrossRef]
- Zattoni, F., Gül, M., Soligo, M., Morlacco, A., Motterle, G., Collavino, J., Barneschi, A. C., Moschini, M., & Moro, F. D. (2020). The impact of COVID-19 pandemic on pornography habits: a global analysis of Google Trends. International journal of impotence research, 33(8), 824–831. [CrossRef]
- Gazzard Kerr, L., & Human, L. J. (2024). Like yourself, and others will follow: The role of target self-esteem in the association between being seen accurately and being liked in platonic and romantic first impressions. Journal of personality and social psychology, 127(4), 936–948. [CrossRef]
- Tissera, H., Gazzard Kerr, L., Carlson, E. N., & Human, L. J. (2021). Social anxiety and liking: Towards understanding the role of metaperceptions in first impressions. Journal of personality and social psychology, 121(4), 948–968. [CrossRef]
- Tissera, H., Mignault, M. C., & Human, L. J. (2023). "Zooming" in on positive and accurate metaperceptions in first impressions: Examining the links with social anxiety and liking in online video interactions. Journal of personality and social psychology, 125(4), 852–873. [CrossRef]
- Watson J. (2003). Love and caring. Ethics of face and hand--an invitation to return to the heart and soul of nursing and our deep humanity. Nursing administration quarterly, 27(3), 197–202. [CrossRef]
- Bernick L. (2004). Caring for older adults: practice guided by Watson's caring-healing model. Nursing science quarterly, 17(2), 128–134. [CrossRef]
- Helin, K., & Lindström, U. A. (2003). Sacrifice: an ethical dimension of caring that makes suffering meaningful. Nursing ethics, 10(4), 414–427. [CrossRef]
- Fredriksson, L., & Eriksson, K. (2003). The ethics of the caring conversation. Nursing ethics, 10(2), 138–148. [CrossRef]
- Fealy G. M. (1995). Professional caring: the moral dimension. Journal of advanced nursing, 22(6), 1135–1140. [CrossRef]
- Wiklund Gustin L. (2021). " Being mutually involved in recovery". A hermeneutic exploration of nurses' experiences of patient participation in psychiatric care. International journal of qualitative studies on health and well-being, 16(1), 2001893. [CrossRef]
- Jordan W. (2023). Philosophisch-psychiatrische Reflexionen zur Liebe. Psychiatrische Praxis, 50(S 01), S7–S14. [CrossRef]
- Schäfer M. L. (2005). Die gegenwärtigen Geist-Gehirn-Theorien in der Analytischen Philosophie des Geistes und ihre epistemische Bedeutung für die Psychiatrie [The current mind-brain theories in analytical philosophy of mind and their epistemic significance for psychiatry]. Fortschritte der Neurologie-Psychiatrie, 73(3), 129–142. [CrossRef]
- Estany A. (2013). La filosofia en el marco de las neurociencias [Philosophy within the context of neurosciences]. Revista de neurologia, 56(6), 344–348.
- Van Oudenhove, L., & Cuypers, S. E. (2010). The philosophical "mind-body problem" and its relevance for the relationship between psychiatry and the neurosciences. Perspectives in biology and medicine, 53(4), 545–557. [CrossRef]
- Telles-Correia D. (2018). The mind-brain gap and the neuroscience-psychiatry gap. Journal of evaluation in clinical practice, 24(4), 797–802. [CrossRef]
- Brinkmann S. (2011). Towards an expansive hybrid psychology: integrating theories of the mediated mind. Integrative psychological & behavioral science, 45(1), 1–20. [CrossRef]
- Gaete, A., & Cornejo, C. (2014). The brain is not a tool. Integrative psychological & behavioral science, 48(1), 100–109. [CrossRef]
- Harstad, E., Hanson, E., Brewster, S. J., DePillis, R., Milliken, A. L., Aberbach, G., Sideridis, G., & Barbaresi, W. J. (2023). Persistence of Autism Spectrum Disorder From Early Childhood Through School Age. JAMA pediatrics, 177(11), 1197–1205. [CrossRef]
- Mottron, L., & Bzdok, D. (2020). Autism spectrum heterogeneity: fact or artifact?. Molecular psychiatry, 25(12), 3178–3185. [CrossRef]
- de Giambattista, C., Ventura, P., Trerotoli, P., Margari, M., Palumbi, R., & Margari, L. (2019). Subtyping the Autism Spectrum Disorder: Comparison of Children with High Functioning Autism and Asperger Syndrome. Journal of autism and developmental disorders, 49(1), 138–150. [CrossRef]
- Riccioni, A., Pro, S., Di Criscio, L., Terribili, M., Siracusano, M., Moavero, R., Valeriani, M., & Mazzone, L. (2021). High Intellectual Potential and High Functioning Autism: Clinical and Neurophysiological Features in a Pediatric Sample. Brain sciences, 11(12), 1607. [CrossRef]
- Mikami, K., & Matsumoto, H. (2007). Nihon rinsho. Japanese journal of clinical medicine, 65(3), 487–491.
- Pinciotti, C. M., Riemann, B. C., & Abramowitz, J. S. (2021). Intolerance of uncertainty and obsessive-compulsive disorder dimensions. Journal of anxiety disorders, 81, 102417. [CrossRef]
- Boelen, P. A., & Carleton, R. N. (2012). Intolerance of uncertainty, hypochondriacal concerns, obsessive-compulsive symptoms, and worry. The Journal of nervous and mental disease, 200(3), 208–213. [CrossRef]
- Gentes, E. L., & Ruscio, A. M. (2011). A meta-analysis of the relation of intolerance of uncertainty to symptoms of generalized anxiety disorder, major depressive disorder, and obsessive-compulsive disorder. Clinical psychology review, 31(6), 923–933. [CrossRef]
- Segal, S. C., & Carmona, N. E. (2022). A systematic review of sleep problems in children and adolescents with obsessive compulsive disorder. Journal of anxiety disorders, 90, 102591. [CrossRef]
- Skjold, S. H., Hagen, K., Wheaton, M. G., Kallestad, H., Hjelle, K. M., Björgvinsson, T., & Hansen, B. (2024). Insomnia as a predictor of treatment outcomes in adolescents receiving concentrated exposure treatment for OCD. BMC psychiatry, 24(1), 702. [CrossRef]
- Kramer, D. J., & Johnson, A. A. (2024). Apigenin: a natural molecule at the intersection of sleep and aging. Frontiers in nutrition, 11, 1359176. [CrossRef]
- Charrière, K., Schneider, V., Perrignon-Sommet, M., Lizard, G., Benani, A., Jacquin-Piques, A., & Vejux, A. (2024). Exploring the Role of Apigenin in Neuroinflammation: Insights and Implications. International journal of molecular sciences, 25(9), 5041. [CrossRef]
- Olasehinde, T. A., & Olaokun, O. O. (2024). Apigenin and inflammation in the brain: can apigenin inhibit neuroinflammation in preclinical models?. Inflammopharmacology, 32(5), 3099–3108. [CrossRef]
- Kasiri, N., Rahmati, M., Ahmadi, L., & Eskandari, N. (2018). The significant impact of apigenin on different aspects of autoimmune disease. Inflammopharmacology, 26(6), 1359–1373. [CrossRef]
- Taylor S. (2011). Early versus late onset obsessive-compulsive disorder: evidence for distinct subtypes. Clinical psychology review, 31(7), 1083–1100. [CrossRef]
- Fibbe, L. A., Cath, D. C., & van Balkom, A. J. (2011). Obsessieve-compulsieve stoornis met tics: een nieuw subtype? [Obsessive compulsive disorder with tics: a new subtype?]. Tijdschrift voor psychiatrie, 53(5), 275–285.
- Gordon, O. M., Salkovskis, P. M., Oldfield, V. B., & Carter, N. (2013). The association between obsessive compulsive disorder and obsessive compulsive personality disorder: prevalence and clinical presentation. The British journal of clinical psychology, 52(3), 300–315. [CrossRef]
- Eisen, J. L., Coles, M. E., Shea, M. T., Pagano, M. E., Stout, R. L., Yen, S., Grilo, C. M., & Rasmussen, S. A. (2006). Clarifying the convergence between obsessive compulsive personality disorder criteria and obsessive compulsive disorder. Journal of personality disorders, 20(3), 294–305. [CrossRef]
- Boelen, P. A., & Reijntjes, A. (2009). Intolerance of uncertainty and social anxiety. Journal of anxiety disorders, 23(1), 130–135. [CrossRef]
- Clark, L. A., Watson, D., & Mineka, S. (1994). Temperament, personality, and the mood and anxiety disorders. Journal of abnormal psychology, 103(1), 103–116.
- Kerstis, B., Aarts, C., Tillman, C., Persson, H., Engström, G., Edlund, B., Öhrvik, J., Sylvén, S., & Skalkidou, A. (2016). Association between parental depressive symptoms and impaired bonding with the infant. Archives of women's mental health, 19(1), 87–94. [CrossRef]
- Edhborg, M., Matthiesen, A. S., Lundh, W., & Widström, A. M. (2005). Some early indicators for depressive symptoms and bonding 2 months postpartum--a study of new mothers and fathers. Archives of women's mental health, 8(4), 221–231. [CrossRef]
- Nasreen, H. E., Pasi, H. B., Aris, M. A. M., Rahman, J. A., Rus, R. M., & Edhborg, M. (2022). Impact of parental perinatal depressive and anxiety symptoms trajectories on early parent-infant impaired bonding: a cohort study in east and west coasts of Malaysia. Archives of women's mental health, 25(2), 377–387. [CrossRef]
- Ivarsson, T., & Melin, K. (2008). Autism spectrum traits in children and adolescents with obsessive-compulsive disorder (OCD). Journal of anxiety disorders, 22(6), 969–978. [CrossRef]
- Rutgers, A. H., Bakermans-Kranenburg, M. J., van Ijzendoorn, M. H., & van Berckelaer-Onnes, I. A. (2004). Autism and attachment: a meta-analytic review. Journal of child psychology and psychiatry, and allied disciplines, 45(6), 1123–1134. [CrossRef]
- Lukas, M., & Neumann, I. D. (2013). Oxytocin and vasopressin in rodent behaviors related to social dysfunctions in autism spectrum disorders. Behavioural brain research, 251, 85–94. [CrossRef]
- Zhang, R., Zhang, H. F., Han, J. S., & Han, S. P. (2017). Genes Related to Oxytocin and Arginine-Vasopressin Pathways: Associations with Autism Spectrum Disorders. Neuroscience bulletin, 33(2), 238–246. [CrossRef]
- Ebstein, R. P., Knafo, A., Mankuta, D., Chew, S. H., & Lai, P. S. (2012). The contributions of oxytocin and vasopressin pathway genes to human behavior. Hormones and behavior, 61(3), 359–379. [CrossRef]
- Ebstein, R. P., Israel, S., Lerer, E., Uzefovsky, F., Shalev, I., Gritsenko, I., Riebold, M., Salomon, S., & Yirmiya, N. (2009). Arginine vasopressin and oxytocin modulate human social behavior. Annals of the New York Academy of Sciences, 1167, 87–102. [CrossRef]
- Comparan-Meza, M., Vargas de la Cruz, I., Jauregui-Huerta, F., Gonzalez-Castañeda, R. E., Gonzalez-Perez, O., & Galvez-Contreras, A. Y. (2021). Biopsychological correlates of repetitive and restricted behaviors in autism spectrum disorders. Brain and behavior, 11(10), e2341. [CrossRef]
- Schneider, E., Hopf, D., Aguilar-Raab, C., Scheele, D., Neubauer, A. B., Sailer, U., Hurlemann, R., Eckstein, M., & Ditzen, B. (2023). Affectionate touch and diurnal oxytocin levels: An ecological momentary assessment study. eLife, 12, e81241. [CrossRef]
- Seale, J., Murphy, J., Mantle, A., & Chan, B. (2020). The Beneficence of Cuddle Therapy in Hyperekplexia: A Case Report. Advances in neonatal care : official journal of the National Association of Neonatal Nurses, 20(1), 33–37. [CrossRef]
- Molinari, E. (2020). Intimacy and autism: an apparent paradox. The Psychoanalytic Quarterly, 89(3), 483-502. [CrossRef]
- Martin, A. (2008). Autism, Empathy, and Existentialism. Raritan, 27(3), 89. https://search.proquest.com/openview/a9ea9130f177f79c3536182b25bf829b/1?pq-origsite=gscholar&cbl=30927.
- Sala, G., Hooley, M., & Stokes, M. A. (2020). Romantic intimacy in autism: A qualitative analysis. Journal of autism and developmental disorders, 50(11), 4133-4147. [CrossRef]
- Landon, S. (2016). Romantic Relationships: An Exploration of the Lived Experiences of Young Women who identify with a Diagnosis of Autism Spectrum Disorder (Doctoral dissertation, University of East London). [CrossRef]
- Ibrahimagic, A., Patkovic, N., Radic, B., & Hadzic, S. (2021). Communication and Language Skills of Autistic Spectrum Disorders in Children and Their Parents' Emotions. Materia socio-medica, 33(4), 250–256. [CrossRef]
- Ingram, J., Beasant, L., Odd, D., & Chakkarapani, E. (2022). 'Opportunity to bond and a sense of normality': Parent and staff views of cuddling babies undergoing therapeutic hypothermia in neonatal intensive care: 'CoolCuddle'. Health expectations : an international journal of public participation in health care and health policy, 25(4), 1384–1392. [CrossRef]
- Odd, D., Okano, S., Ingram, J., Blair, P. S., Billietop, A., Fleming, P. J., Thoresen, M., & Chakkarapani, E. (2021). Physiological responses to cuddling babies with hypoxic-ischaemic encephalopathy during therapeutic hypothermia: an observational study. BMJ paediatrics open, 5(1), e001280. [CrossRef]
- Sanders, M. R., & Hall, S. L. (2018). Trauma-informed care in the newborn intensive care unit: promoting safety, security and connectedness. Journal of perinatology : official journal of the California Perinatal Association, 38(1), 3–10. [CrossRef]
- Feary A. M. (2002). Touching the fragile baby: looking at touch in the special care nursery (SCN). The Australian journal of holistic nursing, 9(1), 44–48.
- Gueroult P. (2019). Pratique du peau à peau et attachement en réanimation néonatale [Skin-to-skin practice and bonding in neonatal intensive care]. Soins. Pediatrie, puericulture, 40(308), 44–46. [CrossRef]
- Flacking, R., Lehtonen, L., Thomson, G., Axelin, A., Ahlqvist, S., Moran, V. H., Ewald, U., Dykes, F., & Separation and Closeness Experiences in the Neonatal Environment (SCENE) group (2012). Closeness and separation in neonatal intensive care. Acta paediatrica (Oslo, Norway : 1992), 101(10), 1032–1037. [CrossRef]
- Cullen, L., & Barlow, J. (2002). 'Kiss, cuddle, squeeze': the experiences and meaning of touch among parents of children with autism attending a Touch Therapy Programme. Journal of child health care : for professionals working with children in the hospital and community, 6(3), 171–181. [CrossRef]
- Cullen, L. A., Barlow, J. H., & Cushway, D. (2005). Positive touch, the implications for parents and their children with autism: an exploratory study. Complementary therapies in clinical practice, 11(3), 182–189. [CrossRef]
- Powell, L., & Stapley, J. (2008). Training parents of children with life-long and life-limiting conditions in the art of massage. Complementary therapies in clinical practice, 14(4), 237–243. [CrossRef]
- Rao, M. R., Brenner, R. A., Schisterman, E. F., Vik, T., & Mills, J. L. (2004). Long term cognitive development in children with prolonged crying. Archives of disease in childhood, 89(11), 989–992. [CrossRef]
- Murphy M. A. (1975). The crying infant. Pediatric nursing, 1(1), 15–17.
- Schmitt B. D. (1985). Colic: excessive crying in newborns. Clinics in perinatology, 12(2), 441–451.
- Schmitt B. D. (1986). The prevention of sleep problems and colic. Pediatric clinics of North America, 33(4), 763–774. [CrossRef]
- Santos P. (2023). Decoupling touch from sex: gender(ed) representations of physical intimacy in the cuddle industry. Frontiers in sociology, 8, 998037. [CrossRef]
- van Anders, S. M., Edelstein, R. S., Wade, R. M., & Samples-Steele, C. R. (2013). Descriptive experiences and sexual vs. nurturant aspects of cuddling between adult romantic partners. Archives of sexual behavior, 42(4), 553–560. [CrossRef]
- Yamada K. (2016). Masui. The Japanese journal of anesthesiology, 65(3), 255–261.
- Bashor, P. S. (1968). Plato and Aristotle on friendship. J. Value Inquiry, 2, 269. https://heinonline.org/HOL/Page?handle=hein.journals/jrnlvi2&div=30&g_sent=1&casa_token=woVb5B-XjQYAAAAA:nj0sQgHJdyaEEJxwtjDFk1l_zYMop07xE7gFu1BZRMP8jiQ47GhvoQIALmr5XUFtZxaRN-ljG4I&collection=journals.
- Gadamer, H. G. (1986). The idea of the good in Platonic-Aristotelian philosophy. Yale University Press.
- Fistioc, M. C. (2002). The beautiful shape of the good: platonic and pythagorean themes in Kant's critique of the power of judgment. Psychology Press.
- Lam, M., Lam, C., Lam, J., Works, W. C. T., Balance, Y. H., & Closing, I. Cuddle Therapy: How This Underrated Practice Boosts Your Feel-Good Hormones and Health. https://www.drlamcoaching.com/blog/cuddle-therapy/.
- Häusser, J. A., Junker, N. M., & van Dick, R. (2020). The how and the when of the social cure: A conceptual model of group-and individual-level mechanisms linking social identity to health and well-being. European Journal of Social Psychology, 50(4), 721-732. [CrossRef]
- Morrison, I. (2016). Keep calm and cuddle on: social touch as a stress buffer. Adaptive Human Behavior and Physiology, 2, 344-362. [CrossRef]
- Cohen, S., Janicki-Deverts, D., Turner, R. B., & Doyle, W. J. (2015). Does hugging provide stress-buffering social support? A study of susceptibility to upper respiratory infection and illness. Psychological science, 26(2), 135–147. [CrossRef]
- Neff, K. (2003). Self-compassion: An alternative conceptualization of a healthy attitude toward oneself. Self and identity, 2(2), 85-101. [CrossRef]
- Dreisoerner, A., Junker, N. M., Schlotz, W., Heimrich, J., Bloemeke, S., Ditzen, B., & van Dick, R. (2021). Self-soothing touch and being hugged reduce cortisol responses to stress: A randomized controlled trial on stress, physical touch, and social identity. Comprehensive psychoneuroendocrinology, 8, 100091. [CrossRef]
- Packheiser, J., Hartmann, H., Fredriksen, K., Gazzola, V., Keysers, C., & Michon, F. (2024). A systematic review and multivariate meta-analysis of the physical and mental health benefits of touch interventions. Nature human behaviour, 8(6), 1088-1107. [CrossRef]
- Van Raalte, L. J. (2017). The influence of cuddling on relational health for cohabitating couples. Arizona State University. https://www.proquest.com/openview/d202fffca01033b84fbc646ccaaa8a2a/1?casa_token=SsEZErOzDPsAAAAA:ffNdKJKQ7r4QWXAM8o66KXuGKafWo2V6xneyBVX-FPySy4HzmA6oKMwWg99rK8BRw9LehPraaCA&cbl=18750&pq-origsite=gscholar.
- Van Raalte, L. J., Floyd, K., & Mongeau, P. A. (2021). The effects of cuddling on relational quality for married couples: A longitudinal investigation. Western Journal of Communication, 85(1), 61-82.
- Grewen, K. M., Anderson, B. J., Girdler, S. S., & Light, K. C. (2003). Warm partner contact is related to lower cardiovascular reactivity. Behavioral medicine (Washington, D.C.), 29(3), 123–130. [CrossRef]
- Light, K. C., Grewen, K. M., & Amico, J. A. (2005). More frequent partner hugs and higher oxytocin levels are linked to lower blood pressure and heart rate in premenopausal women. Biological psychology, 69(1), 5–21. [CrossRef]
- Field, T., Hernandez-Reif, M., Hart, S., Theakston, H., Schanberg, S., & Kuhn, C. (1999). Pregnant women benefit from massage therapy. Journal of psychosomatic obstetrics and gynaecology, 20(1), 31–38. [CrossRef]
- Field, T., Diego, M. A., Hernandez-Reif, M., Schanberg, S., & Kuhn, C. (2004). Massage therapy effects on depressed pregnant women. Journal of psychosomatic obstetrics and gynaecology, 25(2), 115–122. [CrossRef]
- Hernandez-Reif, M., Field, T., Ironson, G., Beutler, J., Vera, Y., Hurley, J., Fletcher, M. A., Schanberg, S., Kuhn, C., & Fraser, M. (2005). Natural killer cells and lymphocytes increase in women with breast cancer following massage therapy. The International journal of neuroscience, 115(4), 495–510. [CrossRef]
- Ferrell-Torry, A. T., & Glick, O. J. (1993). The use of therapeutic massage as a nursing intervention to modify anxiety and the perception of cancer pain. Cancer nursing, 16(2), 93–101.
- Okvat, H. A., Oz, M. C., Ting, W., & Namerow, P. B. (2002). Massage therapy for patients undergoing cardiac catheterization. Alternative therapies in health and medicine, 8(3), 68–75.
- McNamara, M. E., Burnham, D. C., Smith, C., & Carroll, D. L. (2003). The effects of back massage before diagnostic cardiac catheterization. Alternative therapies in health and medicine, 9(1), 50–57.
- de Boer, A., van Buel, E. M., & Ter Horst, G. J. (2012). Love is more than just a kiss: a neurobiological perspective on love and affection. Neuroscience, 201, 114–124. [CrossRef]
- Kurup, R. K., & Kurup, P. A. (2003). Hypothalamic digoxin, hemispheric dominance, and neurobiology of love and affection. The International journal of neuroscience, 113(5), 721–729. [CrossRef]
- Kurup, R. K., & Kurup, P. A. (2002). Central role of hypothalamic digoxin in conscious perception, neuroimmunoendocrine integration, and coordination of cellular function: relation to hemispheric dominance. The International journal of neuroscience, 112(6), 705–739. [CrossRef]
- Saffer, B. Y., Glenn, C. R., & David Klonsky, E. (2015). Clarifying the Relationship of Parental Bonding to Suicide Ideation and Attempts. Suicide & life-threatening behavior, 45(4), 518–528. [CrossRef]
- Goschin, S., Briggs, J., Blanco-Lutzen, S., Cohen, L. J., & Galynker, I. (2013). Parental affectionless control and suicidality. Journal of affective disorders, 151(1), 1–6. [CrossRef]
- Zaborskis, A., Sirvyte, D., & Zemaitiene, N. (2016). Prevalence and familial predictors of suicidal behaviour among adolescents in Lithuania: a cross-sectional survey 2014. BMC public health, 16, 554. [CrossRef]
- Patient, B. A., Fasting, I., Feelings, G., & Love, B. I. Health Benefits of Cuddling. https://drwillcole.com/autoimmune-health/8-reasons-to-cuddle-more-according-to-science.
- Cikara, A. (2019). Big spoon or little spoon: Relations of couples’ attachment styles to cuddling, affection, sleep, and relationship satisfaction (Doctoral dissertation, Auburn University). https://www.proquest.com/openview/b2c3d201191f76efd59bd3d38199c26e/1?casa_token=OQnSXz29WkIAAAAA:Yi7fnZ3Yn6-binz8DWEvSv_W_6gzaKemSu1-V9ulmzpG3Dx1CLrEeZmMpzQhduR2b5wn9IjQMRk&cbl=18750&diss=y&pq-origsite=gscholar.
- Tidmarsh, C. C. (2024). An Exploratory Study on the Effects of the Infant Cuddling Program on Prenatally Exposed and Institutionalized Infants in Hong Kong (Doctoral dissertation, Fielding Graduate University). https://www.proquest.com/openview/a8c6f557a025229b746bc49e8c4b6550/1?casa_token=1Uh9wQ3M1OcAAAAA:Rt-kLvHl_bLXmyfaJOmLp6JA2ME1T2AMuRCgRbLFpGp5wjR0VhqRXEdzKOU_qZyfi7TSIoLZjXI&cbl=18750&diss=y&pq-origsite=gscholar.
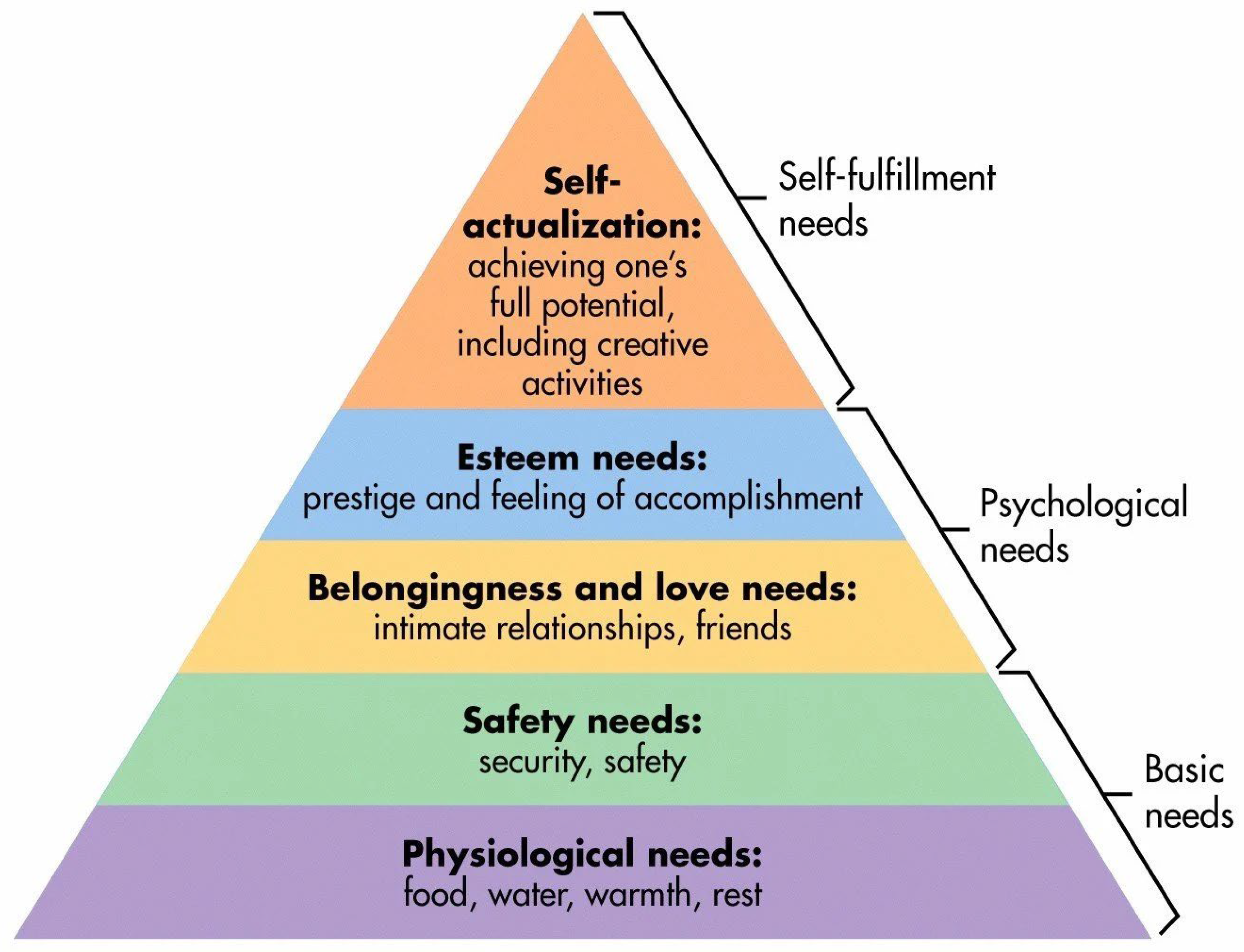
- McLeod, S. (2007). Maslow's hierarchy of needs. Simply psychology, 1(1-18). https://www.researchgate.net/publication/383241976_Maslow's_Hierarchy_of_Needs.
- Mikulović, S. C. (2020). The Hierarchy of Needs from the'Urge for Motherhood'Perspective. Journal of Experiential Psychotherapy/Revista de PSIHOterapie Experientiala, 23(4).https://www.researchgate.net/profile/Carmen-Mikulovic/publication/357535315_The_Hierarchy_of_Needs_from_the_'Urge_for_Motherhood'_Perspective/links/61d30059b6b5667157c5900c/The-Hierarchy-of-Needs-from-the-Urge-for-Motherhood-Perspective.pdf.
- Cabanas, E., & Sánchez-González, J. C. (2016). Inverting the pyramid of needs: Positive psychology's new order for labor success. Psicothema, 107-113. https://reunido.uniovi.es/index.php/PST/article/view/11165.
- Kenrick, D. T., Griskevicius, V., Neuberg, S. L., & Schaller, M. (2010). Renovating the Pyramid of Needs: Contemporary Extensions Built Upon Ancient Foundations. Perspectives on psychological science : a journal of the Association for Psychological Science, 5(3), 292–314. [CrossRef]
- Lam, M., Lam, C., Lam, J., Works, W. C. T., Balance, Y. H., & Closing, I. Cuddle Therapy: How This Underrated Practice Boosts Your Feel-Good Hormones and Health. https://www.drlamcoaching.com/blog/cuddle-therapy/.
- Carp, T. N. (2025). Did the Natural Selection of Humans and of Animals Occur During a “Pregnancy” of Time, Space, Matter and Life?. Preprints. [CrossRef]
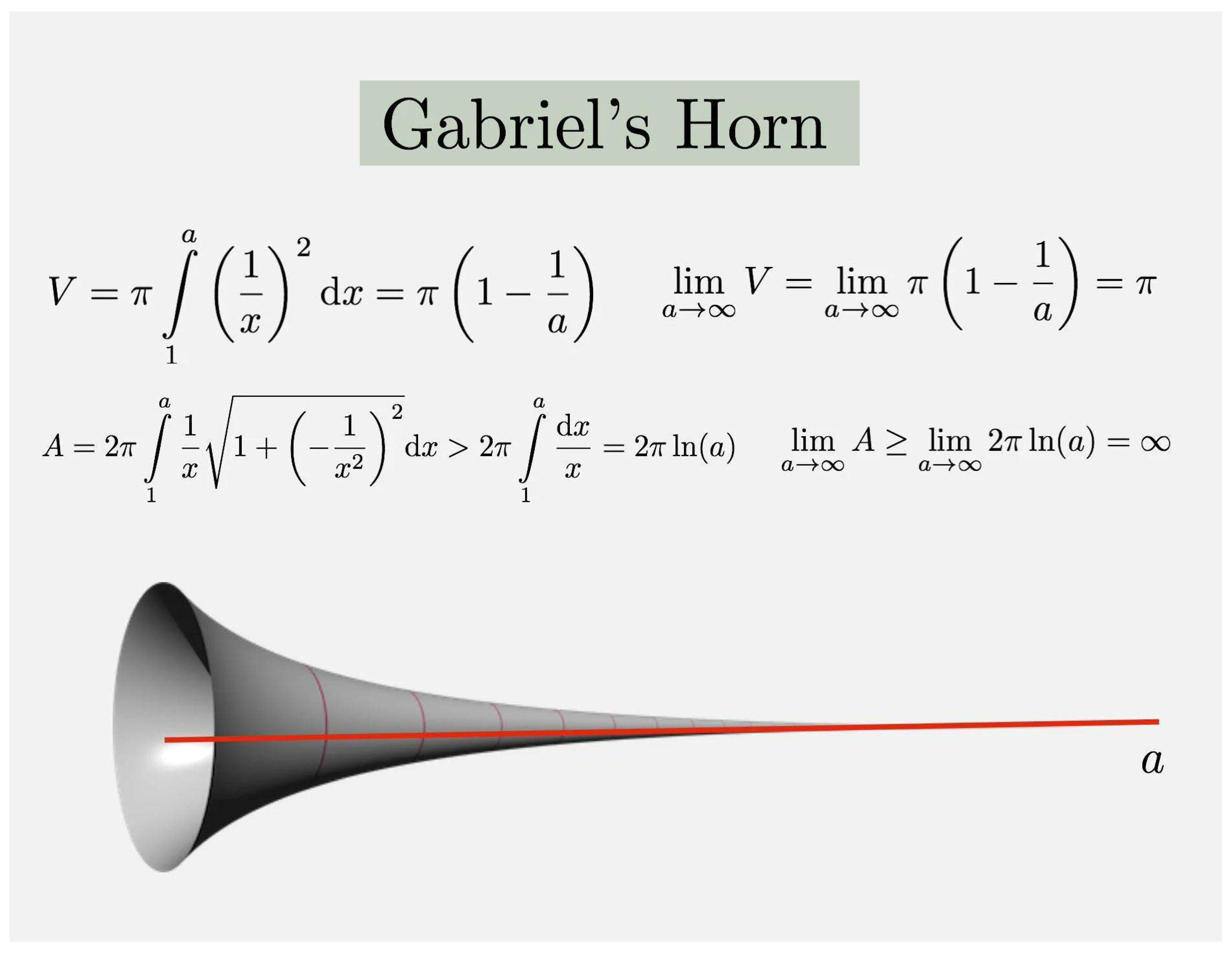
- Math is Visual (2024). https://www.facebook.com/photo/?fbid=1422147295368865&set=a.1042809029969362.
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).




