Submitted:
31 March 2025
Posted:
01 April 2025
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Working Hypothesis and Theory
3. Method of Validation
3.1. Genomic Data
3.2. Rationale
4. Results
4.1. The Three CHS and TLR Genes with the Highest Expression Level (Largest AVE)
4.2. The Three Most Controlled CHS and TLR Genes in Each Profiled Region
4.3. The three least controlled CHS and TLR genes in each profiled region
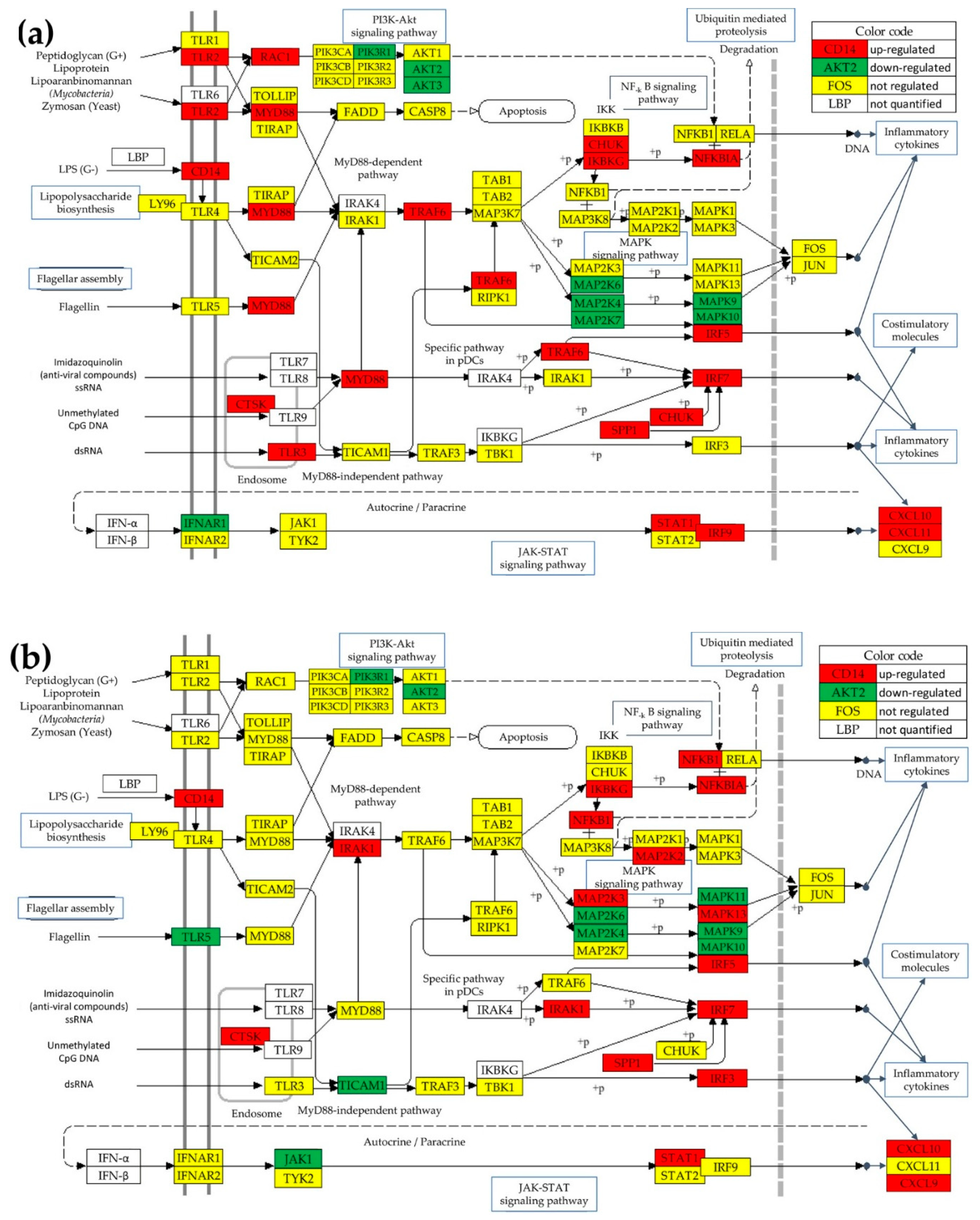
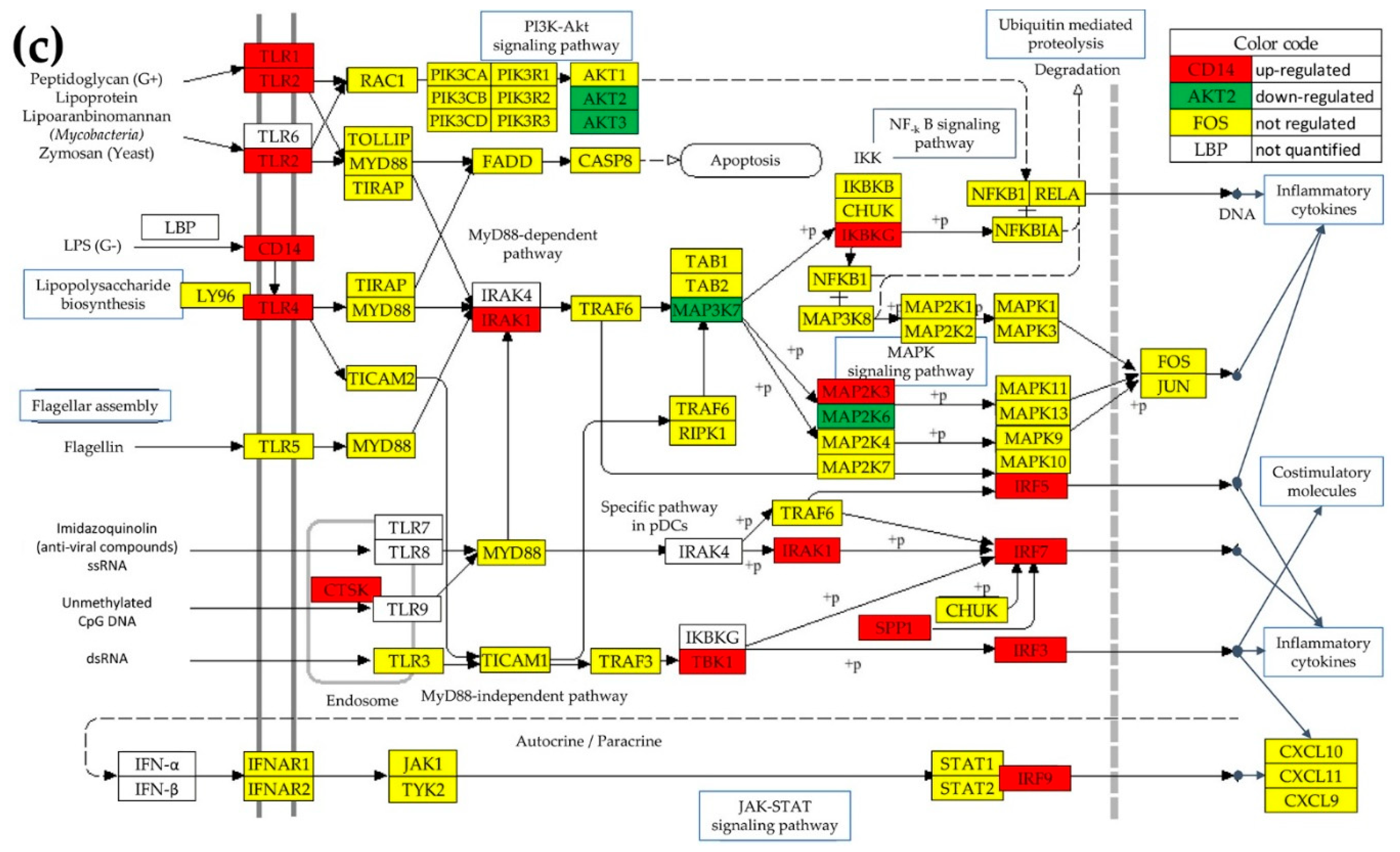
4.4. Regulation of the TLR-Signaling Pathway in the Cancer Nodules
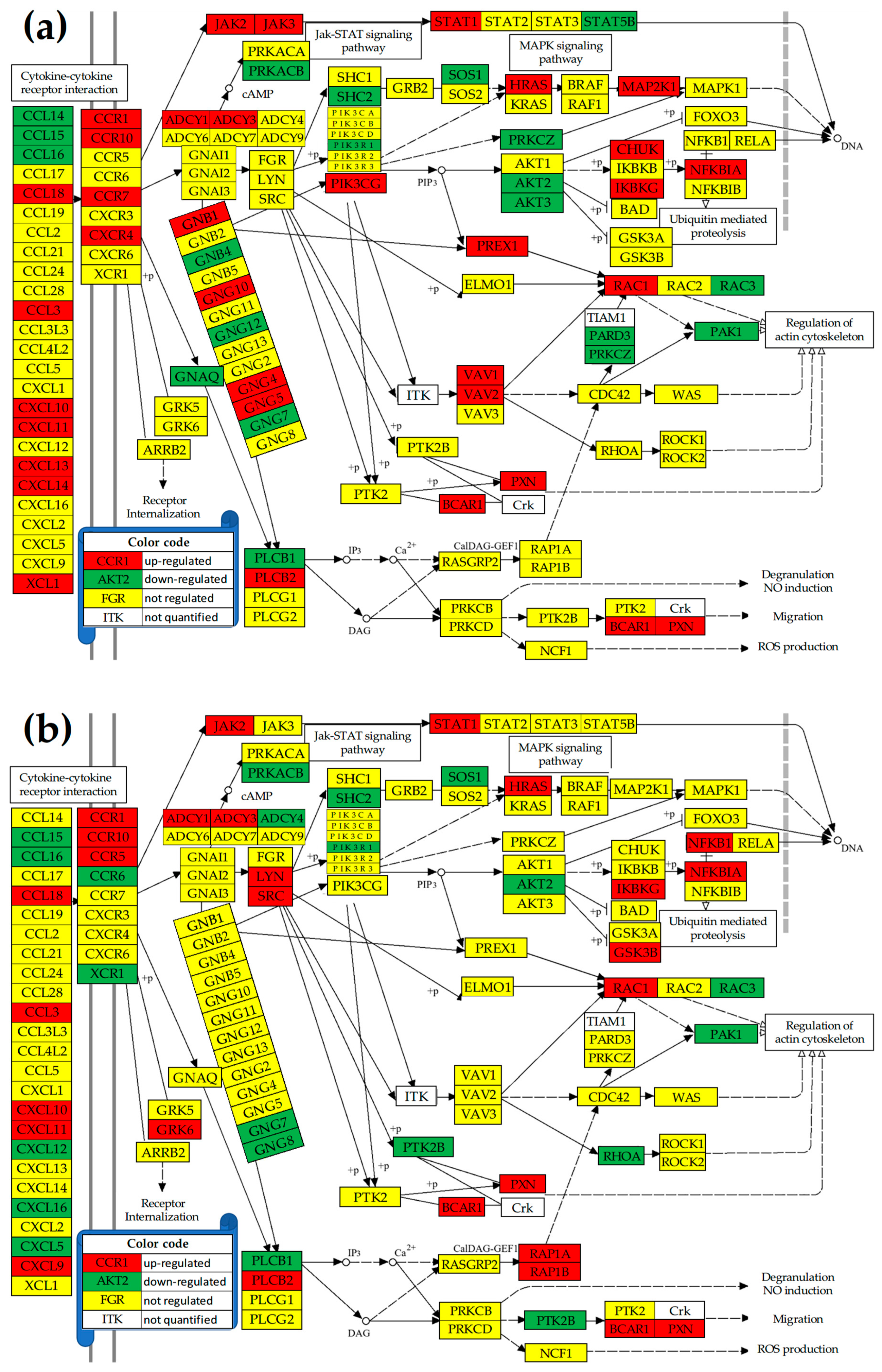
4.5. Regulation of the Chemokine Signaling (CHS) Pathway
4.6. Remodeling of the TLR-CHS Interplay
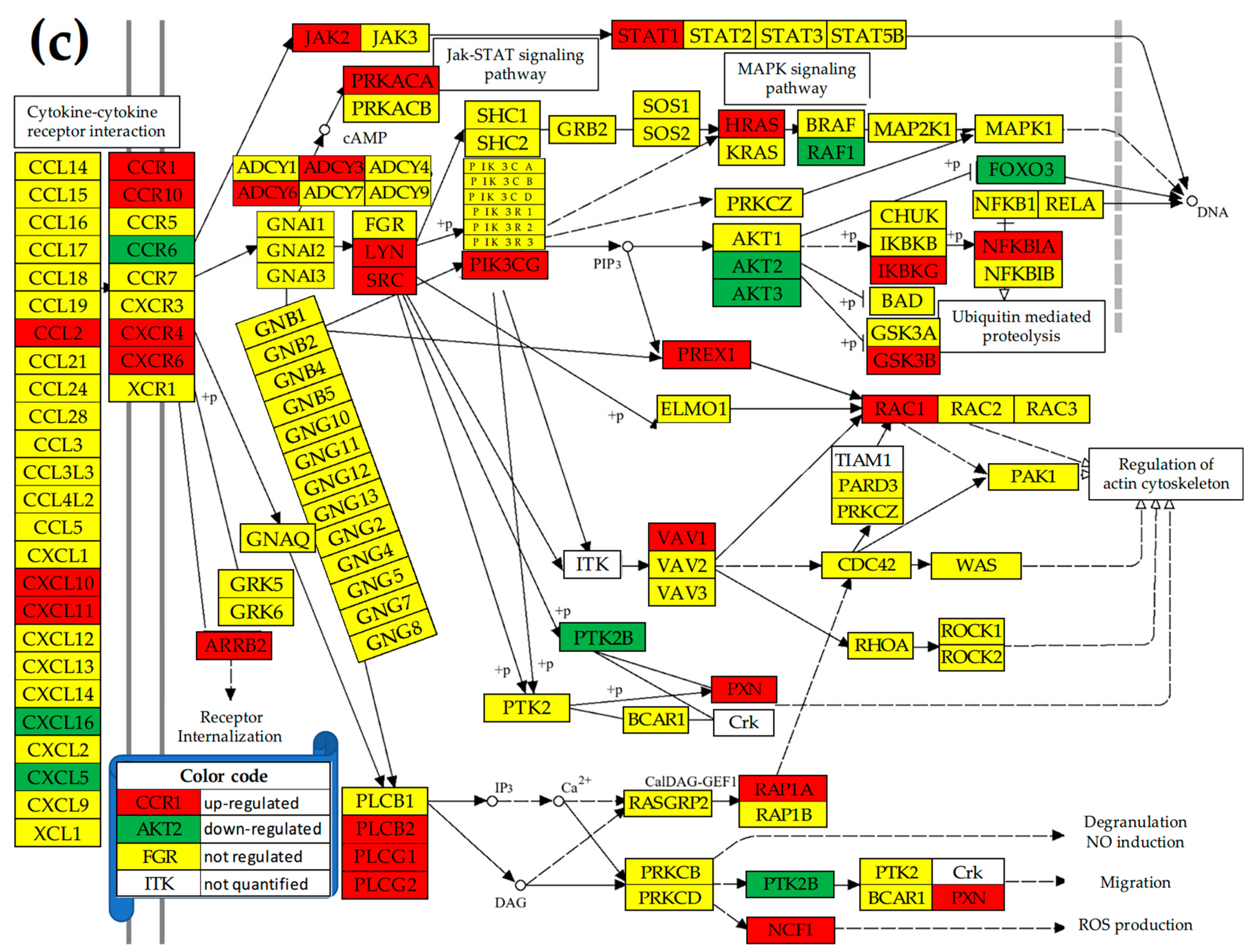
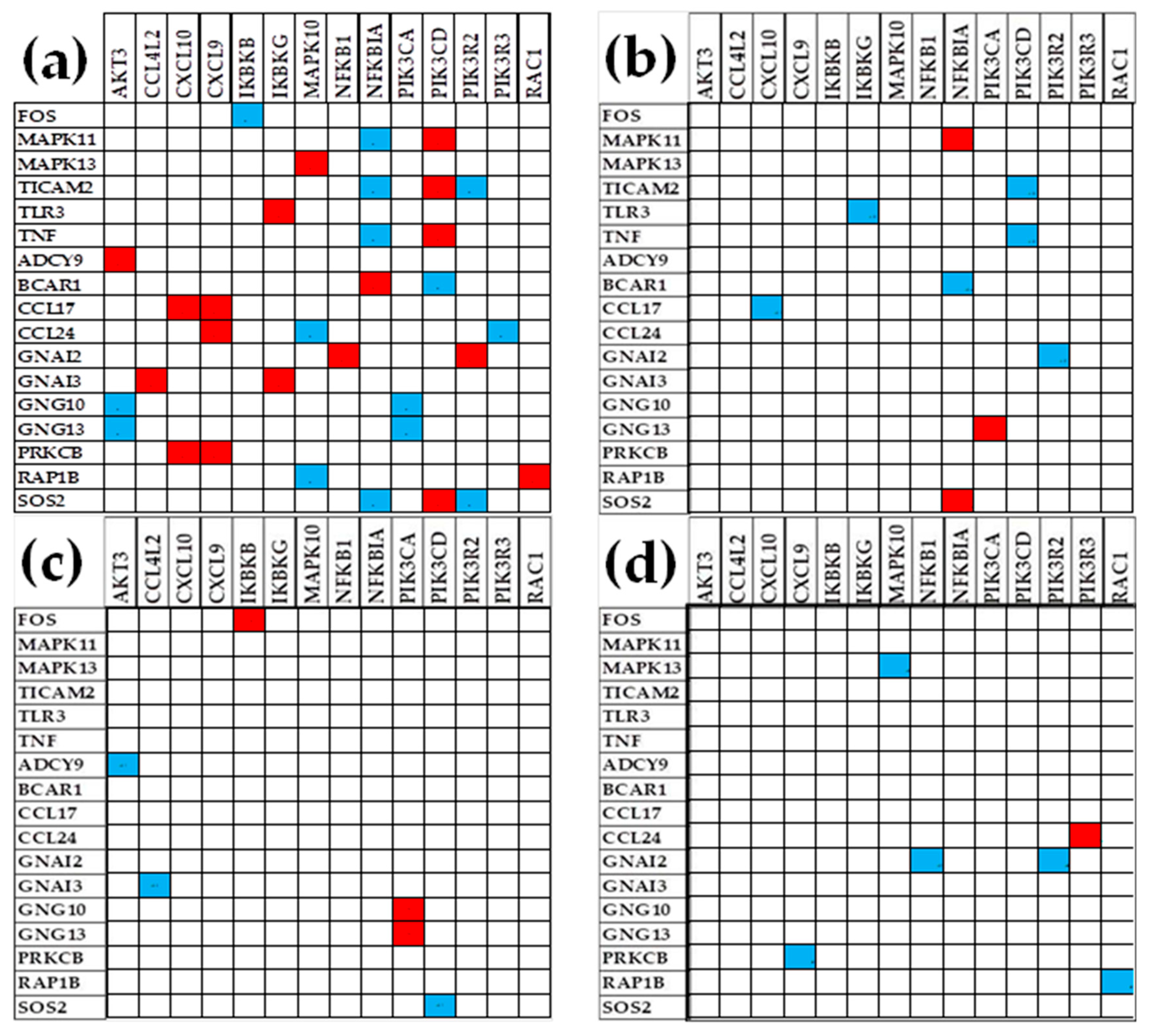
4.6.1. Significant Expression Coordination
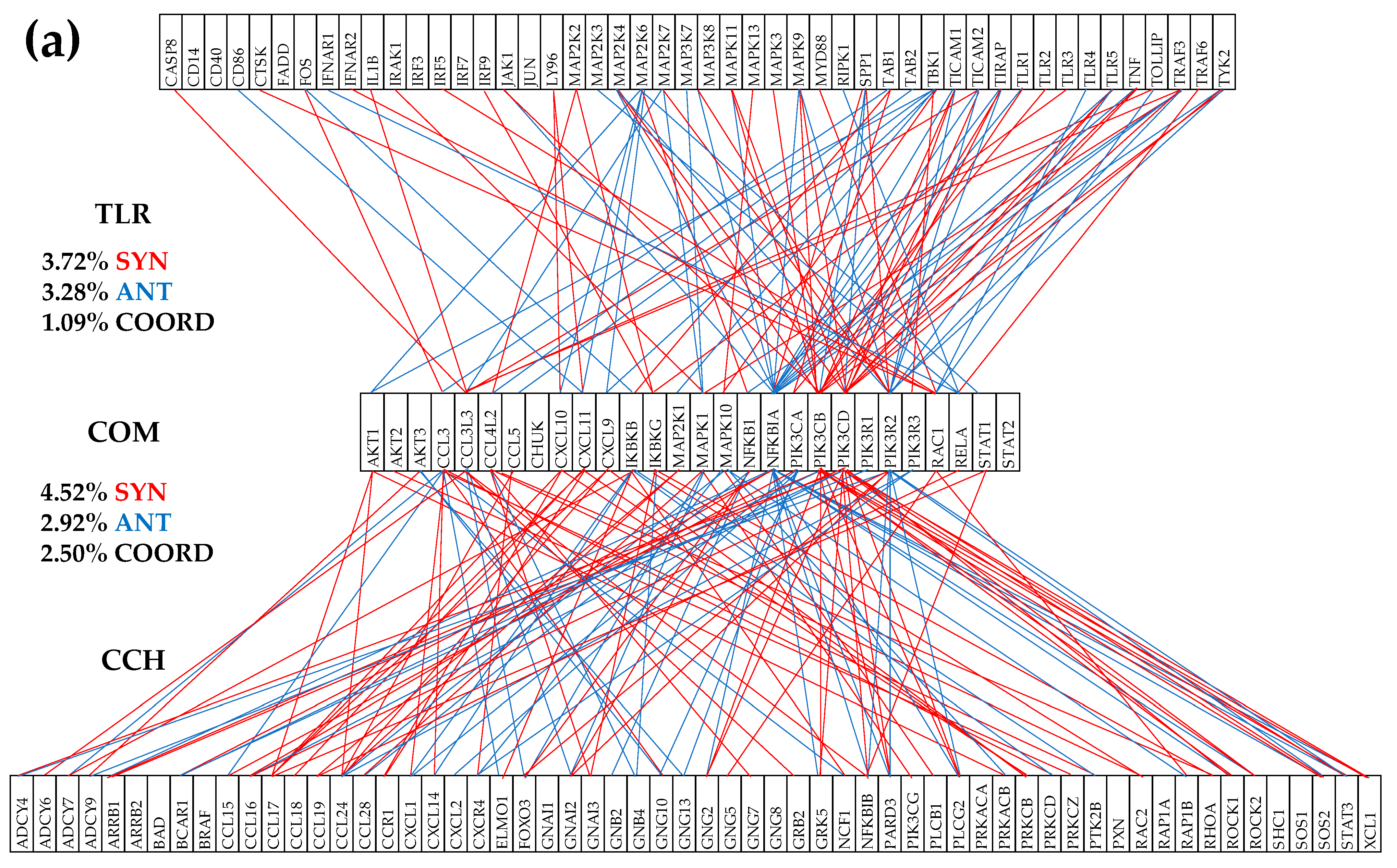
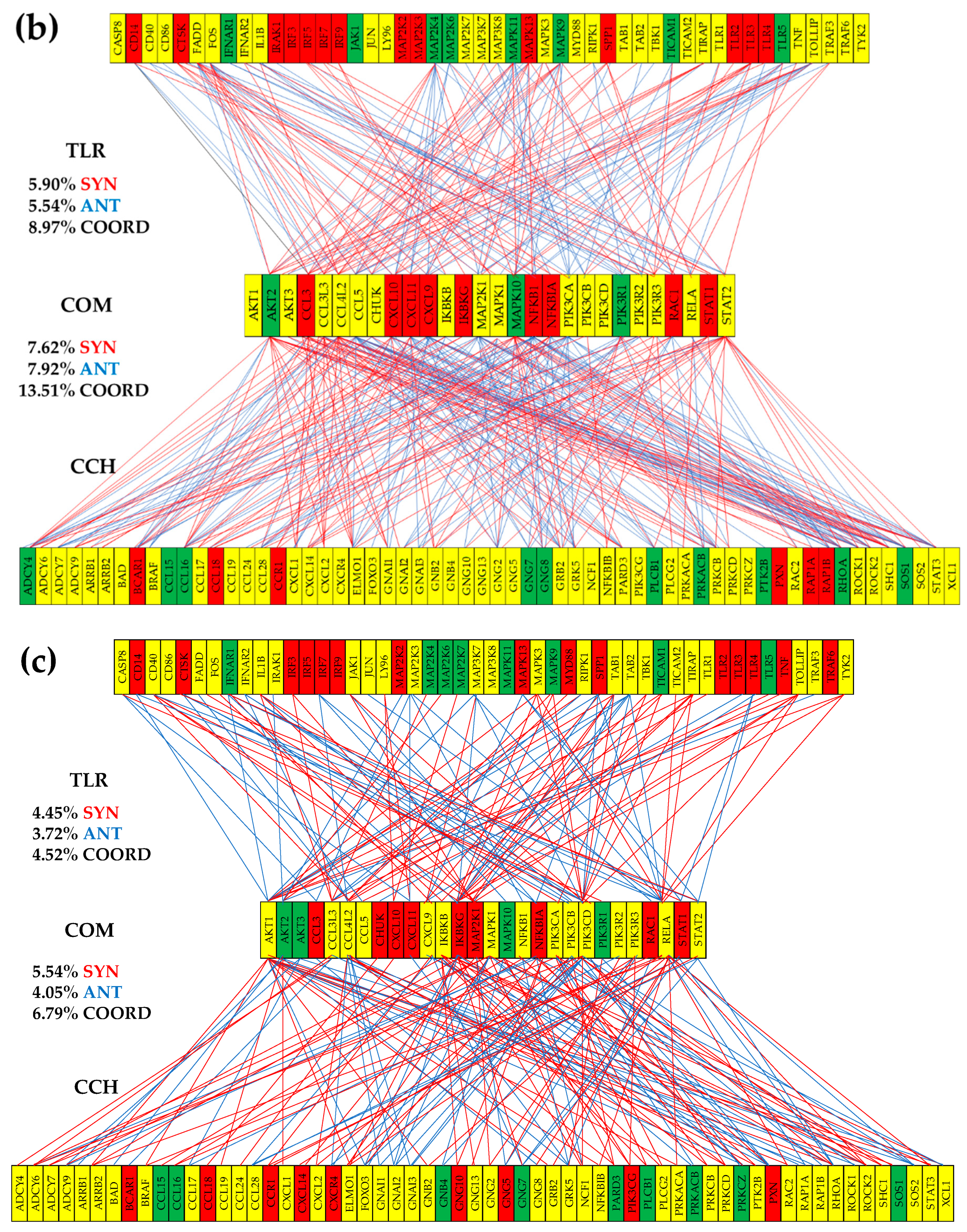
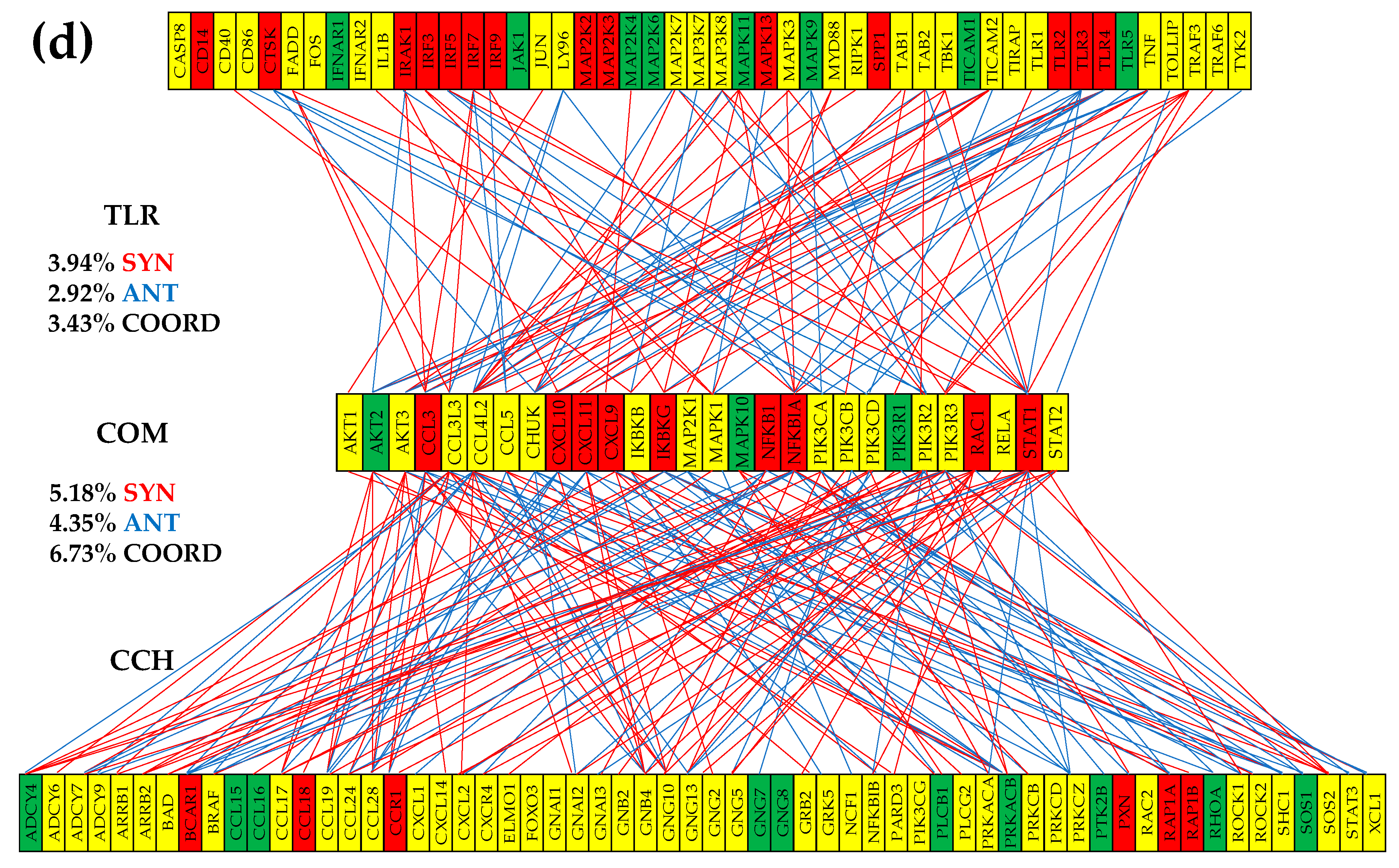
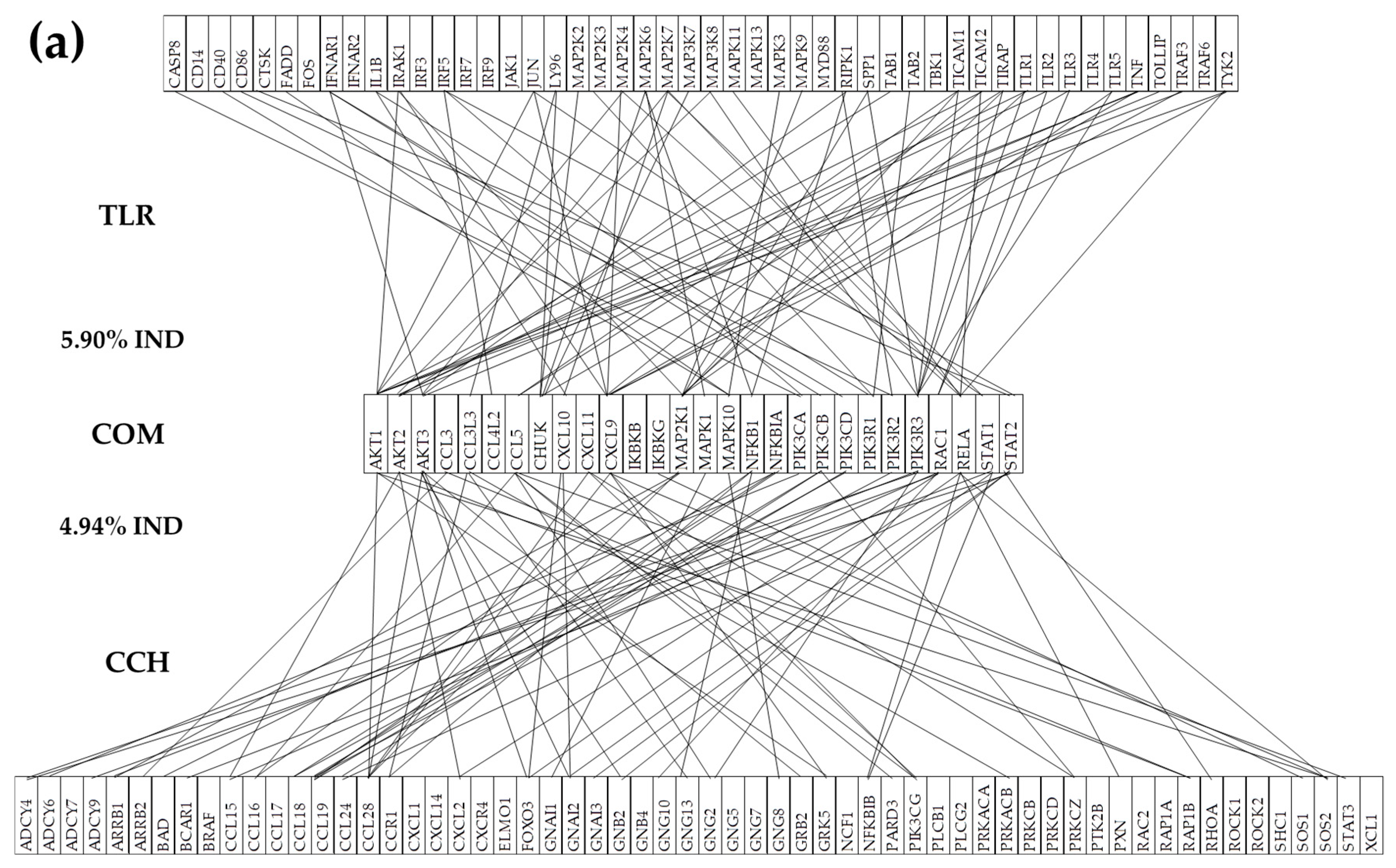
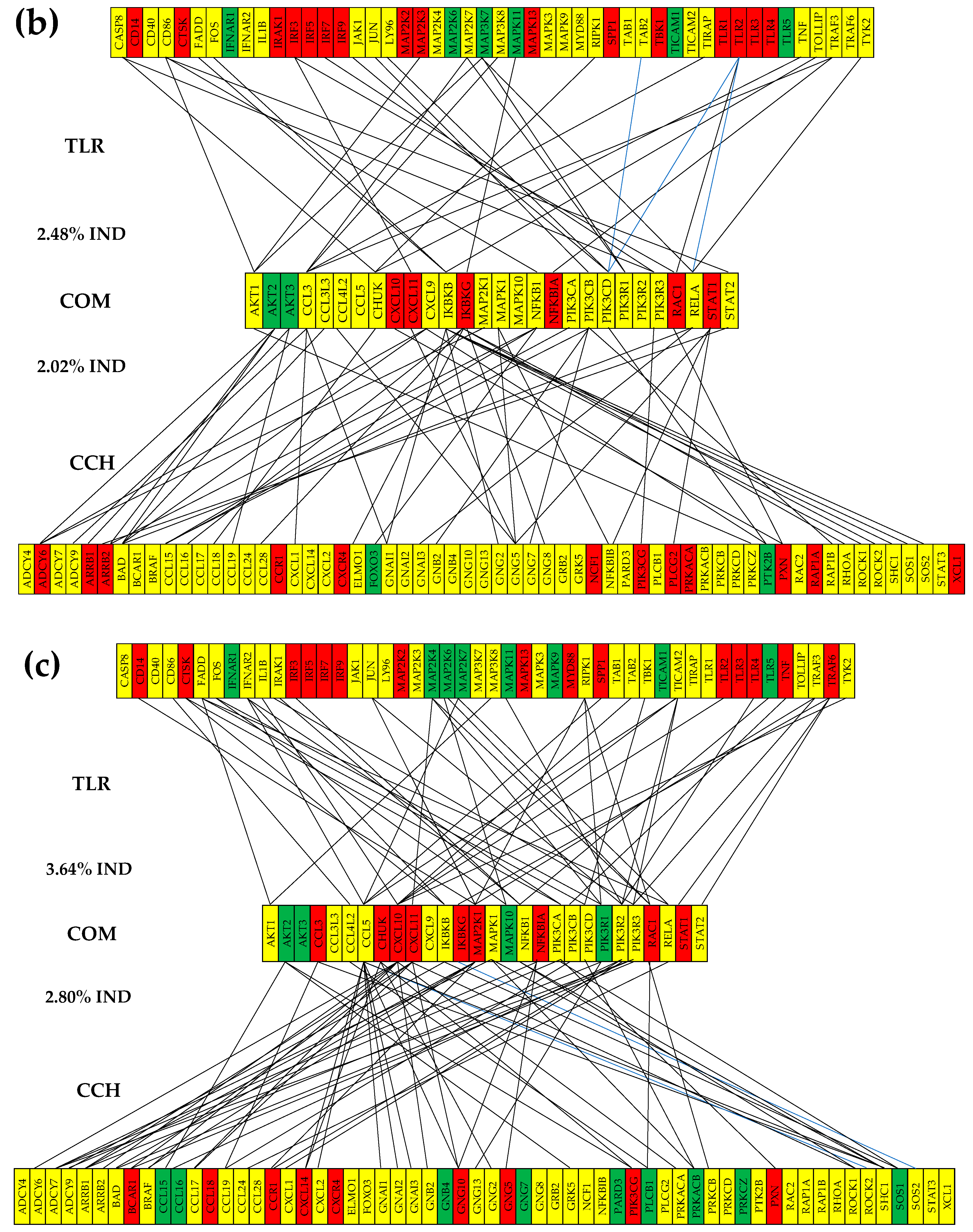
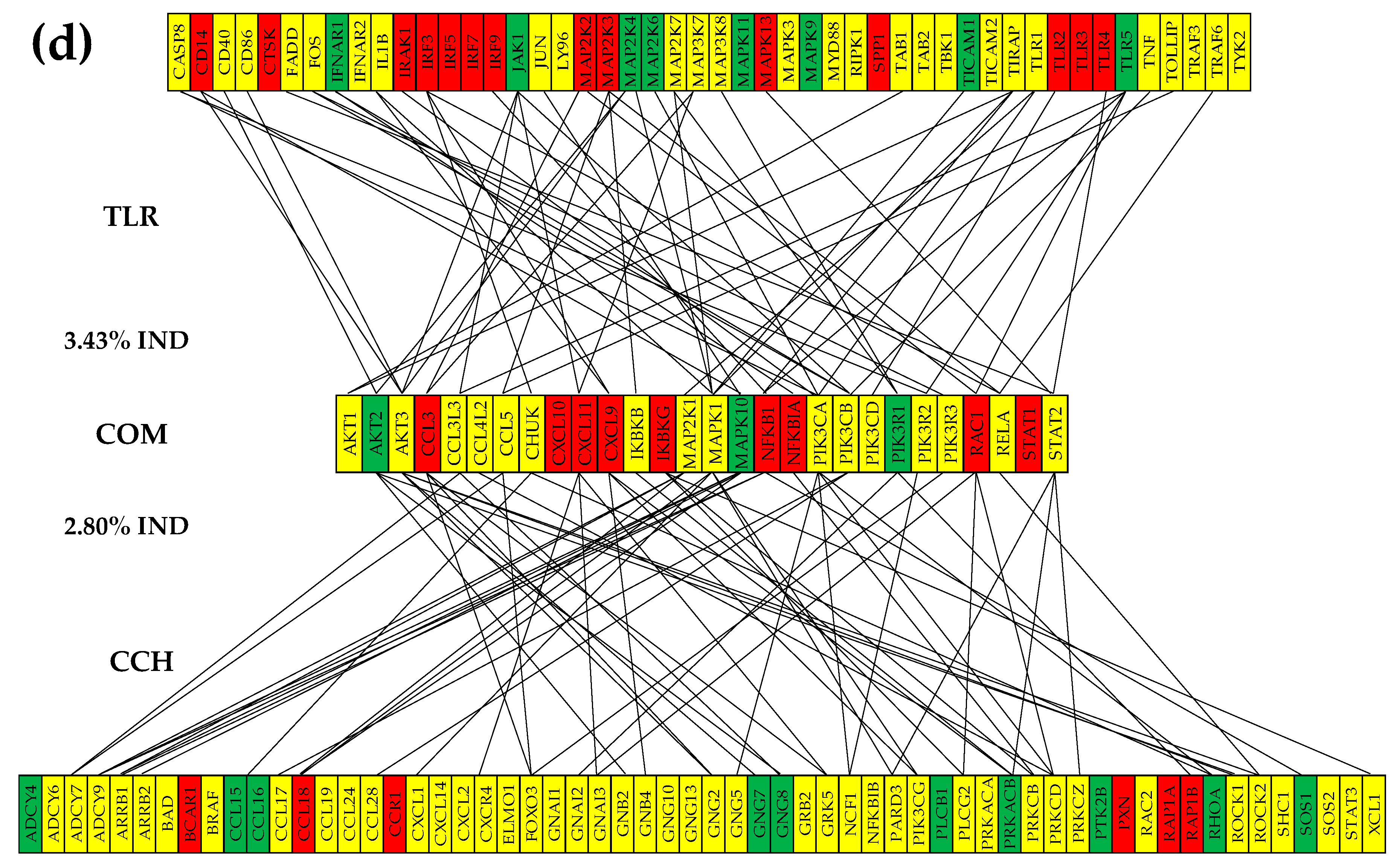
4.6.2. Prostate Cancer Couples Several Normally Independently Expressed TLR and CHS Genes
4.6.3. Cancer Decouples Several Coordinately Expressed TLR and CHS Gene-Pairs in the Normal Tissue
4.6.4. Cancer Switches to the Opposite the Coupling Type of Some Gene Pairs in the Normal Tissue
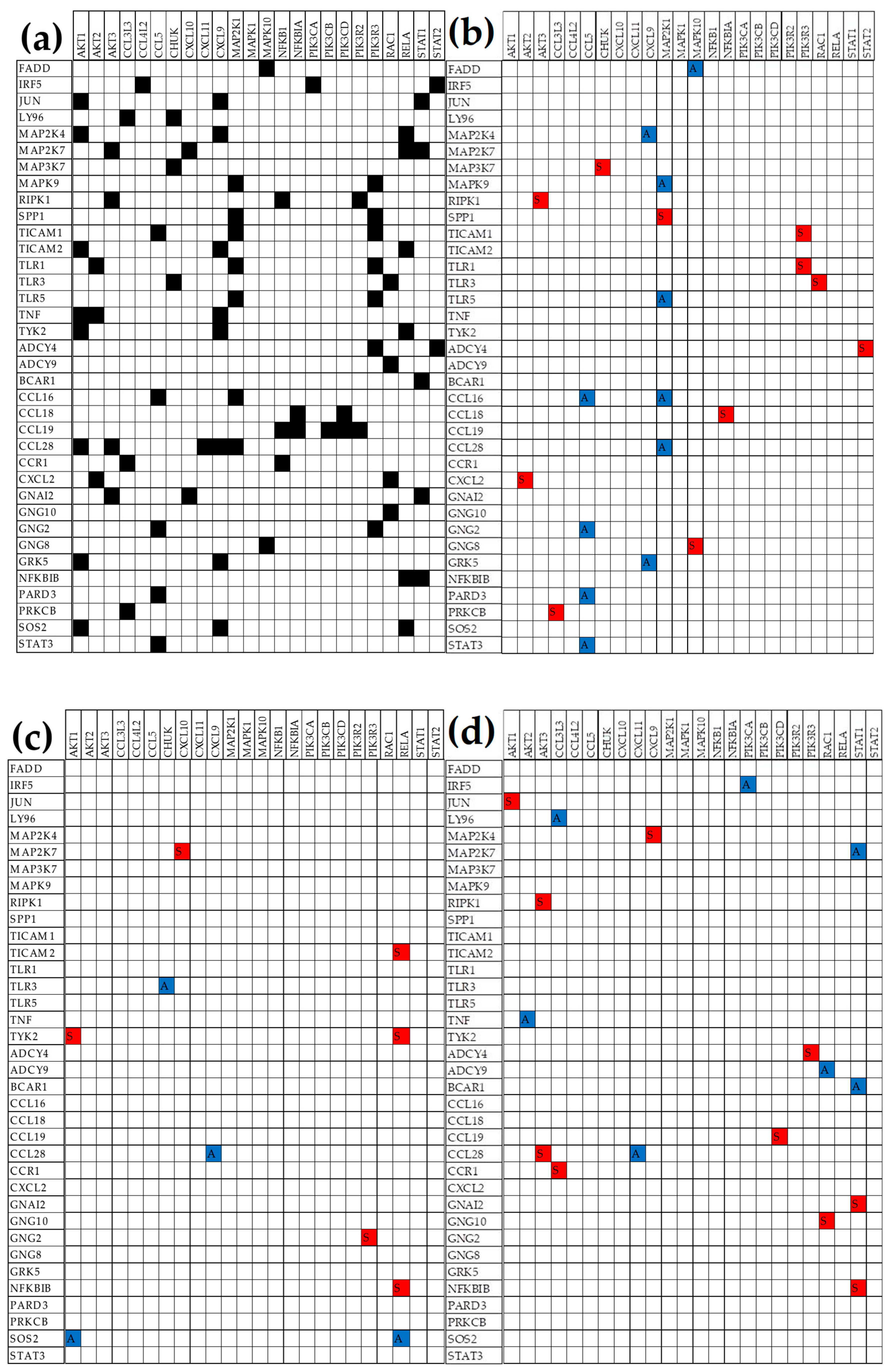
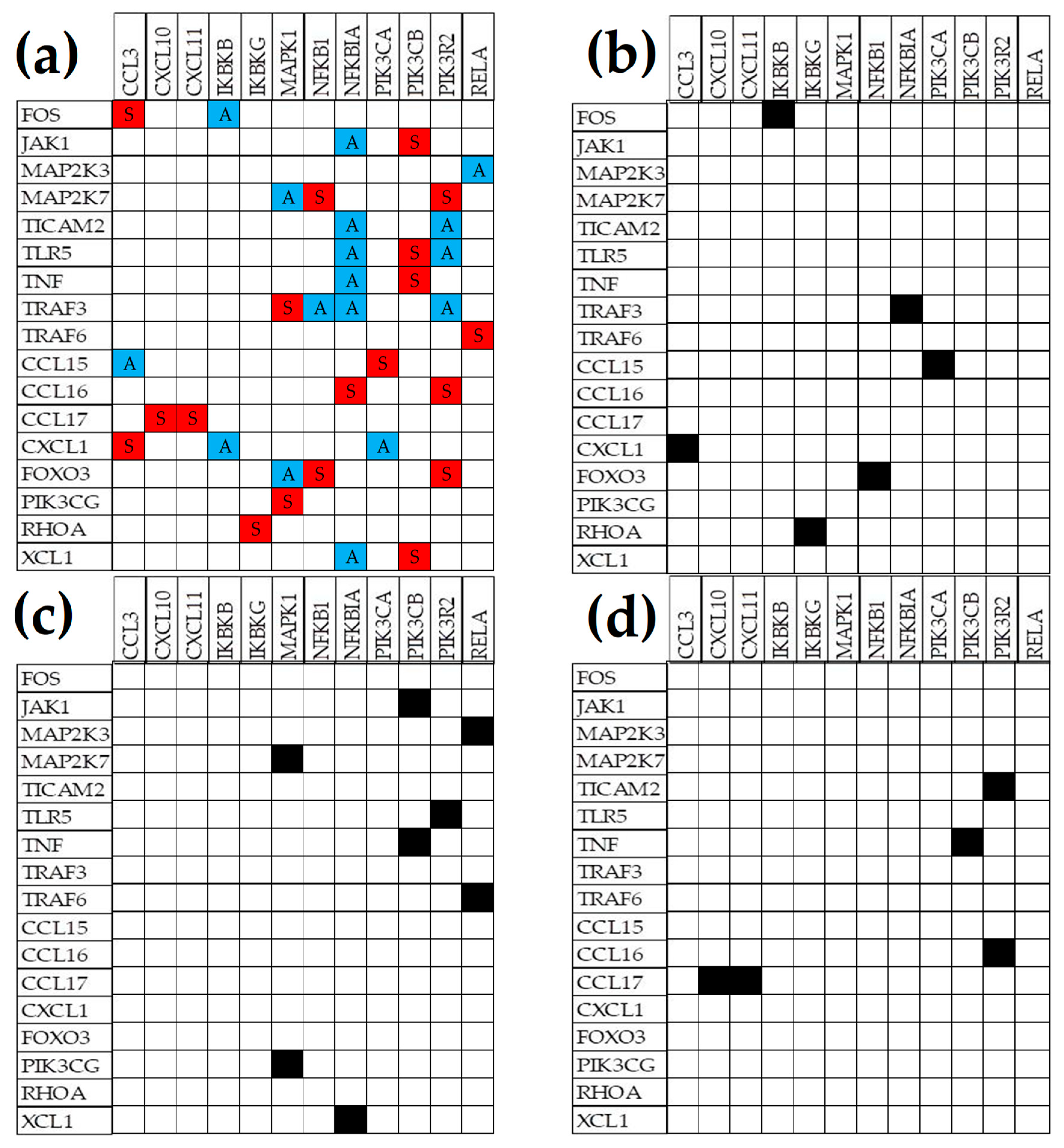
4.7. Key Influential Genes in the CHS and TLR Signaling Pathways
5. Discussion
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
References
- Kohaar, I.; Petrovics, G.; Srivastava, S. A Rich Array of Prostate Cancer Molecular Biomarkers: Opportunities and Challenges. Int J Mol Sci. 2019, 20, 1813. [Google Scholar] [CrossRef] [PubMed]
- Boehm, B.E.; York, M.E.; Petrovics, G.; Kohaar, I.; Chesnut, G.T. Biomarkers of Aggressive Prostate Cancer at Diagnosis. Int. J. Mol. Sci. 2023, 24, 2185. [Google Scholar] [CrossRef] [PubMed]
- Jiang, C.; Hong, Z.; Liu, S.; Hong, Z.; Dai, B. Roles of CDK12 mutations in PCa development and treatment. Biochim Biophys Acta Rev Cancer. 2024, 1880, 189247. [Google Scholar] [CrossRef]
- Zhou, T.; Feng, Q. Androgen receptor signaling and spatial chromatin organization in castration-resistant prostate cancer. Front Med (Lausanne). 2022, 9, 924087. [Google Scholar] [CrossRef]
- Akele, M.; Iervolino, M.; Van Belle, S.; Christ, F.; Debyser, Z. Role of LEDGF/p75 (PSIP1) in oncogenesis. Insights in molecular mechanism and therapeutic potential. Biochim Biophys Acta Rev Cancer 2024, .1880, 189248. [Google Scholar] [CrossRef]
- Yang, R.K.; Alvarez, H.; Lucas, A.S.; Roy-Chowdhuri, S.; Rashid, A.; Chen, H.; et al. Microsatellite instability and high tumor mutational burden detected by next generation sequencing are concordant with loss of mismatch repair proteins by immunohistochemistry. Cancer Genet. 2024, 290-291, 44-50. Cancer Genet. [CrossRef]
- Diaw, L.; Woodson, K.; Gillespie, J.W. Prostate cancer epigenetics: a review on gene regulation. Gene Regul Syst Bio. 2007, 1, 313–25. [Google Scholar] [CrossRef]
- The Cancer Genome Atlas (TCGA) Research Network. Available at: https://www.cancer.gov/tcga (Accessed on January 4, 2025).
- Harmonized Cancer Datasets Genomic Data Commons Data Portal. Available at: https://portal.gdc.cancer.gov (Accessed January 2, 2025).
- Valencia., I.; Nuzzo, P.V.; Francini, E.; Ravera, F.; Fanelli, G.N.; Bleve, S.; et al. Gene Signature for Predicting Metastasis in Prostate Cancer Using Primary Tumor Expression Profiles. medRxiv [Preprint]. 2024,. [CrossRef]
- Foundation Medicine. Available at: https://www.foundationmedicine.com/genomic-testing (Accessed December 12, 2024).
- Invitae Multi-Cancer Panel. Available at: https://www.invitae.com/us/providers/test-catalog/test-01101 (Accessed December 11, 2024).
- Nanostring nCounter® Panels & Assays. Available at: https://www.nanostring.com/products/gene-expression-panels/gene-expression-panels-overview (Accessed, December 12, 2024).
- TissueScan™ Cancer and Normal Tissue cDNA Arrays. Available at: https://www.origene.com/products/tissues (Accessed December 12, 2024).
- Shen, M.; García-Marqués, F.; Muruganantham, A.; Liu, S.; White, J.R.; Bermudez, A.; et al. Identification of a 5-gene signature panel for the prediction of prostate cancer progression. Br J Cancer. 2024, 131, 1748–1761. [Google Scholar] [CrossRef]
- Iacobas, D.A. Advanced Molecular Solutions for Cancer Therapy-The Good, the Bad, and the Ugly of the Biomarker Paradigm. Curr. Issues Mol. Biol. 2024, 46, 1694–1699. [Google Scholar] [CrossRef]
- Dixcy Jaba Sheeba, J.M.; Hegde, S.; Tamboli, N.; Nadig, N.; Keshavamurthy, R.; Ranganathan, P. Gene expression signature of castrate resistant prostate cancer. Gene. 2024, 925, 148603. [Google Scholar] [CrossRef]
- Garzotto, M.; Kopp, R.P. Gene-expression profiling of localized prostate cancer: still miles to go before we sleep. Future Oncol. 2016, 12, 273–6. [Google Scholar] [CrossRef]
- Li, Y.; Hsu, S.H.; Wang, R.; Theprungsirikul, P.; Neparidze, N.; Chang, S.H.; et al. Associations Between Patient Characteristics and Progression to Multiple Myeloma Among Patients With Monoclonal Gammopathy of Undetermined Significance: A Systematic Review. Clin Lymphoma Myeloma Leuk. 2024, S2152-2650(24)02444-3. [CrossRef]
- Iacobas, S.; Iacobas, D.A. Personalized 3-Gene Panel for Prostate Cancer Target Therapy. Curr. Issues Mol. Biol. 2022, 44, 360–382. [Google Scholar] [CrossRef] [PubMed]
- Iacobas, D.A.; Obiomon, E.A.; Iacobas, S. Genomic Fabrics of the Excretory System’s Functional Pathways Remodeled in Clear Cell Renal Cell Carcinoma. Curr Issues Mol Biol. 2023, 45, 9471–9499. [Google Scholar] [CrossRef] [PubMed]
- Geynisman, D.M.; John, W.S.; Miller, T.A.; Asgarisabet, P.; Guttenplan, S.B.; Yin, X.; et al. Racial differences in real-world outcomes of first-line therapies for advanced renal cell carcinoma. Oncologist. 2024, oyae354. [Google Scholar] [CrossRef] [PubMed]
- Creed, J.H.; Berglund, A.E.; Rounbehler, R.J.; Awasthi, S.; Cleveland, J.L.; Park, J.Y.; Yamoah, K.; Gerke, T.A. Commercial Gene Expression Tests for Prostate Cancer Prognosis Provide Paradoxical Estimates of Race-Specific Risk. Cancer Epidemiol Biomarkers Prev. 2020, 29, 246–253. [Google Scholar] [CrossRef]
- Anbarasu, S.; Anbarasu, A. Cancer-biomarkers associated with sex hormone receptors and recent therapeutic advancements: a comprehensive review. Med Oncol. 2023, 40, 171. [Google Scholar] [CrossRef]
- The Importance of Sex in the Discovery of Colorectal Cancer Prognostic Biomarkers. Int J Mol Sci. 2021, 22, 1354. [CrossRef]
- Lau, C.E.; Robinson, O. DNA methylation age as a biomarker for cancer. Int J Cancer. 2021, 148, 2652–2663. [Google Scholar] [CrossRef]
- Kallai, A.; Ungvari, Z.; Fekete, M.; Maier, A.B.; Mikala, G.; Andrikovics, H.; et al. Genomic instability and genetic heterogeneity in aging: insights from clonal hematopoiesis (CHIP), monoclonal gammopathy (MGUS), and monoclonal B-cell lymphocytosis (MBL). Geroscience. 2025, 47, 703–720. [Google Scholar] [CrossRef]
- Liu, Y.; Hao, H.; Guo, X.; Xu, J.; Kang, L; Zheng, G.; Zhao, H. Rare pancreatic carcinosarcoma in a patient with medical history of esophageal cancer: A case report and literature review. Medicine (Baltimore). 2019, 98, e15238. [CrossRef]
- Clift, K.; Macklin-Mantia, S.; Barnhorst, M. Comparison of a Focused Family Cancer History Questionnaire to Family History Documentation in the Electronic Medical Record. J Prim Care Community Health. 2022, 13, 21501319211069756. [CrossRef]
- Rodríguez-Molinero, J.; Migueláñez-Medrán, B.D.C.; Puente-Gutiérrez, C.; Delgado-Somolinos, E.; Martín Carreras-Presas, C.; Fernández-Farhall, J.; López-Sánchez, A.F. Association between Oral Cancer and Diet: An Update. Nutrients. 2021, 13, 1299. [Google Scholar] [CrossRef]
- Maddineni, G.; Xie, J.J.; Brahmbhatt, B.; Mutha, P. Diet and carcinogenesis of gastric cancer. Curr Opin Gastroenterol. 2022, 38, 588–591. [Google Scholar] [CrossRef]
- Kruk, J.; Aboul-Enein, B.H.; Bernstein, J.; Gronostaj, M. ; Psychological Stress and Cellular Aging in Cancer: A Meta-Analysis. Oxid Med Cell Longev. 2019, 1270397. [Google Scholar] [CrossRef]
- Effects of laughter therapy on improving physical and psychological symptoms among cancer patients: a systematic review and meta-analysis. Support Care Cancer. 2025, 33, 230. [CrossRef]
- Grimes, D.R. Radiofrequency Radiation and Cancer: A Review. JAMA Oncol. 2022, 8, 456–461. [Google Scholar] [CrossRef] [PubMed]
- Holick, M.F. Sunlight, UV Radiation, Vitamin D, and Skin Cancer: How Much Sunlight Do We Need? Adv Exp Med Biol. 2020, 1268, 19–36. [Google Scholar] [CrossRef] [PubMed]
- Gupta, S.; Sharma, R.S.; Singh, R. Non-ionizing radiation as possible carcinogen. Int J Environ Health Res. 2022, 32, 916–940. [Google Scholar] [CrossRef]
- Larsen, K.; Rydz, E.; Peters, C.E. Inequalities in Environmental Cancer Risk and Carcinogen Exposures: A Scoping Review. Int J Environ Res Public Health. 2023, 20, 5718. [Google Scholar] [CrossRef] [PubMed]
- Roje, B.; Zhang, B.; Mastrorilli, E.; Kovačić, A.; Sušak, L.; Ljubenkov, I. et. Gut microbiota carcinogen metabolism causes distal tissue tumours. Nature. 2024, 632, 1137–1144. [Google Scholar] [CrossRef]
- Ge, G.Z.; Xu, T.R.; Chen, C. Tobacco carcinogen NNK-induced lung cancer animal models and associated carcinogenic mechanisms. Acta Biochim Biophys Sin (Shanghai). 2015, 47, 477–87. [Google Scholar] [CrossRef]
- Liu, S.; Saunders, M.; Mak, T.W. Chemical carcinogens: implications for cancer treatment. J Clin Invest. 2023, 133, e174319. [Google Scholar] [CrossRef]
- Lander, E.S.; Linton, L.M.; Birren, B.; Nusbaum, C.; Zody, M.C.; Baldwin, J, et al. Initial sequencing and analysis of the human genome. Nature. 2001. 409 (6822): 860–921.20.
- Bian, P.P.; Zhang, Y.; Jiang, Y. Pan-genome: setting a new standard for high-quality reference genomes. Yi Chuan. 2021, 43, 1023–1037. [Google Scholar] [CrossRef]
- Liao, W.W.; Asri, M.; Ebler, J.; Doerr, D.; Haukness, M.; Hickey, G.; et al. A draft human pangenome reference. Nature. 2023. 617 (7960): 312–324. Bibcode:2023Natur.617..312L. [CrossRef]
- Iacobas, D.A.; Tuli, N.Y.; Iacobas, S.; Rasamny, J.K.; Moscatello, A.; Geliebter, J.; Tiwari, R.K. Gene master regulators of papillary and anaplastic thyroid cancers. Oncotarget. 2017, 9, 2410–2424. [Google Scholar] [CrossRef]
- Liu, Y.; Weber, Z.; San Lucas, F.A.; Deshpande, A.; Jakubek, Y.A.; Sulaiman, R.; et al. Assessing inter-component heterogeneity of biphasic uterine carcinosarcomas. Gynecol Oncol. 2018, 151, 243–249. [Google Scholar] [CrossRef]
- Fujimoto, H.; Saito, Y.; Ohuchida, K.; Kawakami, E.; Fujiki, S.; Watanabe, T et al. Deregulated Mucosal Immune Surveillance through Gut-Associated Regulatory T Cells and PD-1+ T Cells in Human Colorectal Cancer. J. Immunol. 2018, 200, 3291–3303. [CrossRef]
- Yang, C.; Gong, J.; Xu, W.; Liu, Z.; Cui, D. Next-generation sequencing identified somatic alterations that may underlie the etiology of Chinese papillary thyroid carcinoma. Eur. J. Cancer Prev. 2023, 32, 264–274. [Google Scholar] [CrossRef] [PubMed]
- Clark, D.J.; Dhanasekaran, S.M.; Petralia, F.; Pan, J.; Song, X.; et al. Clinical Proteomic Tumor Analysis Consortium. Integrated Proteogenomic Characterization of Clear Cell Renal Cell Carcinoma. Cell 2019, 179, 964–983.e31. [CrossRef]
- Solovyov, A.; Behr, J.M.; Hoyos, D.; Banks, E.; Drong, A.W.; Thornlow, B.; et al. Pan-cancer multi-omic model of LINE-1 activity reveals locus heterogeneity of retrotransposition efficiency. Nat Commun. 2025, 16, 2049. [Google Scholar] [CrossRef] [PubMed]
- Prostate cancer. Available at: https://www.genome.jp/pathway/hsa05215. (Accessed December 12, 2024). 12 December.
- Young, B.; O’Dowd, G.; Woodford, P. Wheater’s functional histology: a text and colour atlas (6th ed.). Philadelphia: Elsevier. 2013. pp. 347–8. ISBN 9780702047473.
- Kulac, I.; Roudier, M.P.; Haffner, M.C. Molecular Pathology of Prostate Cancer. Surg. Pathol. Clin. 2021, 14, 387–401. [Google Scholar] [CrossRef]
- Tolkach, Y.; Kristiansen, G. The Heterogeneity of Prostate Cancer: A Practical Approach. Pathobiology 2018, 85, 108–116. [Google Scholar] [CrossRef]
- Berglund, E.; Maaskola, J.; Schultz, N.; Friedrich, S.; Marklund, M.; Bergenstråhle, J.; et al. Spatial maps of prostate cancer transcriptomes reveal an unexplored landscape of heterogeneity. Nat. Commun. 2018, 9, 2419. [Google Scholar] [CrossRef]
- Brady, L.; Kriner, M.; Coleman, I.; Morrissey, C.; Roudier, M.; True, L.D.; et al. Inter- and intra-tumor heterogeneity of metastatic prostate cancer determined by digital spatial gene expression profiling. Nat. Commun. 2021, 12, 1426. [Google Scholar] [CrossRef]
- Tu, S.M.; Zhang, M.; Wood, C.G.; Pisters, L.L. Stem Cell Theory of Cancer: Origin of Tumor Heterogeneity and Plasticity. Cancers, 2021, 13, 4006. [CrossRef]
- Ankathatti Narayanaswamy, I.; Kattepur, A.K.; Raju, K.; Perumal, V.; Ramalingam, R.; Raavi, V.; et al. Shugoshin 1 expression in various cancers: a potential target for therapy. Clin Transl Oncol. 2024. [CrossRef] [PubMed]
- Frame, G.; Huang, X.; Haas, R.; Khan, K.A.; Leong, H.S.; Kislinger, T.; et al. Accelerated growth and local progression of radiorecurrent prostate cancer in an orthotopic bioluminescent mouse model. Sci Rep. 2024, 14, 31205. [Google Scholar] [CrossRef]
- Wei, X.; Liang, J.; Huang, H.; Yang, D.; Wang, X.; Wang, X.; et al. TMED3 promotes prostate cancer via FOXO1a and FOXO3a phosphorylation. Oncol Res. 2024, 33, 161–169. [Google Scholar] [CrossRef]
- Oliveira-Rizzo, C.; Colantuono, C.L; Fernández-Alvarez, A.J.; Boccaccio, G.L; Garat, B.; Sotelo-Silveira, J.R.; et al. Multi-Omics Study Reveals Nc886/vtRNA2-1 as a Positive Regulator of Prostate Cancer Cell Immunity. J Proteome Res. 2024, 24, 433–448. [Google Scholar] [CrossRef]
- Brunie, M.; Robichaud, M.A.; Touaibia, M.; Martin, L.J. The Activation of the CCND1 Promoter by AP-1 and SOX Transcription Factors in PC3 Prostate Cancer Cells Can Be Prevented by Anacardic Acid Analogs. Cell Biochem Biophys. 2024. [Google Scholar] [CrossRef] [PubMed]
- Iacobas, S.; Iacobas, D.A. Astrocyte proximity modulates the myelination gene fabric of oligodendrocytes. Neuron Glia Biol. 2010, 6, 157–69. [Google Scholar] [CrossRef] [PubMed]
- Iacobas, D.A.; Iacobas, S.; Stout, R.F.; Spray, D.C. Cellular Environment Remodels the Genomic Fabrics of Functional Pathways in Astrocytes. Genes (Basel). 2020, 11, 520. [Google Scholar] [CrossRef] [PubMed]
- Iacobas, S.; Ede, N.; Iacobas, D.A. The Gene Master Regulators (GMR) Approach Provides Legitimate Targets for Per-sonalized, Time-Sensitive Cancer Gene Therapy. Genes, 2019, 10, 560. [CrossRef]
- Toll-like receptor pathway. Available online at: https://www.genome.jp/pathway/hsa04620 (Accessed December 12, 2024). 12 December 0462.
- Chemokine signaling pathway - Homo sapiens. Available online at: https://www.genome.jp/pathway/hsa04062 (Accessed December 12, 2024).
- Agilent-026652 Whole Human Genome Microarray 4x44K v2. Available online at: https://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?acc=GPL10332. (Accessed December 12, 2024).
- Gene Commanding Height (GCH) Hierarchy in the Cancer Nucleus and Cancer-Free Resection Margins from a Surgically Removed Prostatic Adenocarcinoma of a 65y Old Black Man. Available online at: https://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?&acc=GSE133906. (Accessed December 12, 2024).
- Iacobas, S.; Iacobas, D.A. A Personalized Genomics Approach of the Prostate Cancer. Cells, 2021, 10, 1644. [CrossRef]
- Carpenter, S.; O’Neill, L.A.J. From periphery to center stage: 50 years of advancements in innate immunity. Cell. 2024, 187, 2030–2051. [Google Scholar] [CrossRef]
- Janeway, C.A. Jr. Pillars article: approaching the asymptote? Evolution and revolution in immunology. Cold spring harb symp quant biol. 1989. 54, 1-13. J Immunol. 2013, 191, 4475-87. [PubMed]
- Matzinger, P. Tolerance, danger, and the extended family. Annu Rev Immunol. 1994, 12, 991–1045. [Google Scholar] [CrossRef] [PubMed]
- Medzhitov, R.; Iwasaki, A. Exploring new perspectives in immunology. Cell. 2024, 187, 2079–2094. [Google Scholar] [CrossRef]
- De Nunzio, C.; Lombardo, R. Best of 2022 in prostate cancer and prostatic diseases. Prostate Cancer Prostatic Dis. 2023, 26, 5–7. [Google Scholar] [CrossRef]
- Liang, H.; Zhang, L.; Liu, Z.; Hoden, B.; DeRubeis, D.; Zhang, Y.; et al. Upregulation of TLR5 indicates a favorable prognosis in prostate cancer. Prostate. 2023, 83, 1035–1045. [Google Scholar] [CrossRef]
- Gambara, G.; De Cesaris, P.; De Nunzio, C.; Ziparo, E.; Tubaro, A.; Filippini, A.; et al. Toll-like receptors in prostate infection and cancer between bench and bedside. J Cell Mol Med. 2013, 17, 713–22. [Google Scholar] [CrossRef]
- Park, S.; Kim, G.; Choi, A.; Kim, S.; Yum, J.S.; Chun, E.; et al. Comparative network-based analysis of toll-like recep-tor agonist, L-pampo signaling pathways in immune and cancer cells. Sci Rep. 2024, 14, 17173. [Google Scholar] [CrossRef]
- Borziak, K.; Finkelstein, J. Gene Expression Markers of Prognostic Importance for Prostate Cancer Risk in Patients with Benign Prostate Hyperplasia. Annu Int Conf IEEE Eng Med Biol Soc. 2022, 2022, 73–76. [Google Scholar] [CrossRef] [PubMed]
- Cheng, C.; Song, D.; Wu, Y.; Liu, B. RAC3 Promotes Proliferation, Migration and Invasion via PYCR1/JAK/STAT Signaling in Bladder Cancer. Front Mol Biosci 2020, 7, 218. [Google Scholar] [CrossRef] [PubMed]
- Engers, R.; Ziegler, S.; Mueller, M.; Walter, A.; Willers, R.; Gabbert, H.E. Prognostic relevance of increased Rac GTPase expression in prostate carcinomas. Endocr Relat Cancer. 2007, 14, 245–56. [Google Scholar] [CrossRef] [PubMed]
- Kudryavtseva, A.V.; Lukyanova, E.N.; Kharitonov, S.L.; Nyushko, K.M.; Krasheninnikov, A.A.; Pudova, E.A.; et al. Bioinformatic identification of differentially expressed genes associated with prognosis of locally advanced lymph node-positive prostate cancer. J Bioinform Comput Biol. 2019, 17, 1950003. [Google Scholar] [CrossRef]
- Tang, L.; Chen, X.; Hou, J.; Wei, X. CXCL14 in prostate cancer: complex interactions in the tumor microenvironment and future prospects. J Transl Med. 2025, 23, 9. [Google Scholar] [CrossRef]
- Chen, J.; Ying, X.M.; Huang, X.M.; Huang, P.; Yan, S.C. Association between polymorphisms in selected inflammatory response genes and the risk of prostate cancer. Onco Targets Ther. 2016, 9, 223–9. [Google Scholar] [CrossRef]
- Qi, F.; Gao, N.; Li, J.; Zhou, C.; Jiang, J.; Zhou, B.; et al. A multidimensional recommendation framework for identifying biological targets to aid the diagnosis and treatment of liver metastasis in patients with colorectal cancer. Mol Cancer. 2024, 23, 239. [Google Scholar] [CrossRef]
- Kalungi, F.; Nsubuga, A.; Anywar, G. Network analysis and molecular docking studies of quercetin as a potential treatment for prostate cancer. In Silico Pharmacol. 2023, 11, 24. [Google Scholar] [CrossRef]
- Chi, H.C.; Lin, Y.H.; Wu, Y.H.; Chang, C.C.; Wu, C.H.; Yeh, C.T.; et al. CCL16 is a pro-tumor chemokine that recruits monocytes and macrophages to promote hepatocellular carcinoma progression. Am J Cancer Res. 2024, 14, 3600–3613. [Google Scholar] [CrossRef]
- Ni, D.; Wu, J.; Pan, J.; Liang, Y.; Xu, Z.; Yan, Z.; et al. The value of a metabolic and immune-related gene signature and adjuvant therapeutic response in pancreatic cancer. Front Genet. 2025, 15, 1475378. [Google Scholar] [CrossRef]
- Kowalewski, A.; Jaworski, D.; Borowczak, J.; Maniewski, M.; Szczerbowski, K.; Antosik, P.; et al. TOLLIP Protein Expression Predicts Unfavorable Outcome in Renal Cell Carcinoma. Int J Mol Sci. 2022, 23, 14702. [Google Scholar] [CrossRef] [PubMed]
- Yao, L.; Chen, X.; Fang, Y.; Huang, Y.; Wu, K.; Huang, X. et. Multi-Omics Analysis of Aberrances and Functional Implications of IRF5 in Digestive Tract Tumours. J Cell Mol Med. 2025, 29, e70433. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Dong, D.; Zhao, N.; Liu, Y.; Bai, C.; Hua, J.; et al. Tumor-derived CCL15 regulates RNA m6A methylation in cancer-associated fibroblasts to promote hepatocellular carcinoma growth. Cancer Lett. 2024, 611, 217420. [Google Scholar] [CrossRef] [PubMed]
- Ahmat Amin, M.K.B.; Shimizu, A.; Zankov, D.P.; Sato, A.; Kurita, S.; Ito, M.; et al. Epithelial membrane protein 1 promotes tumor metastasis by enhancing cell migration via copine-III and Rac1. Oncogene. 2018, 37, 5416–5434. [Google Scholar] [CrossRef]
- Skoulidis, F.; Li, B.T.; Dy, G.K.; Price, T.J.; Falchook, G.S.; Wolf, J.; et al. Sotorasib for Lung Cancers with KRAS p.G12C Mutation. N Engl J Med. 2021, 384, 2371–2381. [Google Scholar] [CrossRef] [PubMed]
- Sutera, P.; Kim, J.; Kumar, R.; Deek, R.A.; Stephenson, R.; Mayer, T.; et al. PIK3/Akt/mTOR pathway alterations in metastatic castration-sensitive prostate cancer. Prostate. 2024, 84, 1301–1308. [Google Scholar] [CrossRef]
- Kim, J.K.; Jung, Y.; Wang, J.; Joseph, J.; Mishra, A.; Hill, E.E.; et al. TBK1 regulates prostate cancer dormancy through mTOR inhibition. Neoplasia. 2013, 15, 1064–74. [Google Scholar] [CrossRef]
- Tang, K.D.; Ling, M.T. Targeting drug-resistant prostate cancer with dual PI3K/mTOR inhibition. Curr Med Chem. 2014, 21, 3048–56. [Google Scholar] [CrossRef]
- Cui, K.; Song, N.; Fan, Y.; Zeng, L.; Shi, P.; Wang, Z.; et al. A two-sample Mendelian randomization analysis: causal association between chemokines and pan-carcinoma. Front Genet. 2023, 14, 1285274. [Google Scholar] [CrossRef]
- Qian, D.; He, L.; Zhang, Q.; Li, W.; Tang, D.; Wu, C.; et al. Cathepsin K: A Versatile Potential Biomarker and Therapeutic Target for Various Cancers. Curr Oncol. 2022, 29, 5963–5987. [Google Scholar] [CrossRef]
- Ye, Z.; Deng, X.; Zhang, J.; Shao, R.; Song, C.; Zhao, J.; et al. Causal relationship between immune cells and prostate cancer: a Mendelian randomization study. Front Cell Dev Biol. 2024, 12, 1381920. [Google Scholar] [CrossRef] [PubMed]
- Iacobas, D.A. Powerful Quantifiers for Cancer Transcriptomics. World J Clinical Oncology 2020, 11, 679-704 https://www.wjgnet.com/2218-4333/full/v11/i9/679.htm.
- Horoszewicz, J.S.; Leong, S.S.; Kawinski, E.; Karr, J.P.; Rosenthal, H.; Chu, T.M.; et al. LNCaP model of human prostatic carcinoma. Cancer Res. 1983, 43, 1809–1818. [Google Scholar]
- Alimirah, F.; Chen, J.; Basrawala, Z.; Xin, H.; Choubey, D. DU-145 and PC-3 human prostate cancer cell lines express androgen receptor: Implications for the androgen receptor functions and regulation. FEBS Lett. 2006, 580, 2294–2300. [Google Scholar] [CrossRef] [PubMed]
- Remodeling of DNA Transcription Genomic Fabric in Capridine-Treated LNCaP Human Prostate Cancer Cell Line. Available online at: https://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?acc=GSE72414 (Accessed December 12, 2024).
- Remodeling of Major Genomic Fabrics and Their Interplay in Capridine-Treated DU145 Classic Human Prostate Cancer. Available online at: https://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?acc=GSE72333 (Accessed December 12, 2024).
- Iacobas, D.A.; Mgbemena, V.; Iacobas, S.; Menezes, K.M.; Wang, H.; Saganti, P.B. Genomic fabric remodeling in metastatic clear cell renal cell carcinoma (ccRCC): A new paradigm and proposal for a personalized gene therapy approach. Cancers, 2020, 12, 3678. [CrossRef]
- Zhong, M.; Clarke, S.; Vo, B.T.; Khan, S.A. The essential role of Giα2 in prostate cancer cell migration. Mol Cancer Res. 2012, 10, 1380–8. [Google Scholar] [CrossRef] [PubMed]
- Raymond, J.R. Jr.; Appleton, K.M.; Pierce, J.Y.; Peterson, Y.K. Suppression of GNAI2 message in ovarian cancer. J Ovarian Res. 2014, 7, 6. [Google Scholar] [CrossRef]
- Sena, L.A.; Salles, D.C.; Engle, E.L.; Zhu, Q.; Tukachinsky, H.; Lotan, T.L.; et al. Mismatch repair-deficient prostate cancer with parenchymal brain metastases treated with immune checkpoint blockade. Cold Spring Harb Mol Case Stud. 2021, 7, a006094. [Google Scholar] [CrossRef]
- Schwarze, S.R.; Luo, J.; Isaacs, W.B.; Jarrard, D.F. Modulation of CXCL14 (BRAK) expression in prostate cancer. Prostate, 2005, 64, 67-74. [CrossRef]
- Mak, P.; Li, J.; Samanta, S.; Mercurio, A.M. ERβ regulation of NF-kB activation in prostate cancer is mediated by HIF-1. Oncotarget. 2015, 6, 40247–54. [Google Scholar] [CrossRef]
- Zhao, Y.; Chen, W.; Zhu, W.; Meng, H.; Chen, J.; Zhang, J. Overexpression of Interferon Regulatory Factor 7 (IRF7) Reduces Bone Metastasis of Prostate Cancer Cells in Mice. Oncol Res. 2017, 25, 511–522. [Google Scholar] [CrossRef]
- Deveci Ozkan, A.; Kaleli, S.; Onen, H.I.; Sarihan, M.; Guney Eskiler, G.; Kalayci Yigin, A.; et al. Anti-inflammatory effects of nobiletin on TLR4/TRIF/IRF3 and TLR9/IRF7 signaling pathways in prostate cancer cells. Immunopharmacol Immunotoxicol. 2020, 42, 93–100. [Google Scholar] [CrossRef]
- Mohite, P.; Lokwani, D.K.; Sakle, N.S. Exploring the therapeutic potential of SGLT2 inhibitors in cancer treatment: integrating in silico and in vitro investigations. Naunyn Schmiedebergs Arch Pharmacol. 2024, 397, 6107–6119. [Google Scholar] [CrossRef]
- Mauri, G.; Chiodoni, C.; Parenza, M.; Arioli, I.; Tripodo, C.; Colombo, M.P. Ultrasound-guided intra-tumor injection of combined immunotherapy cures mice from orthotopic prostate cancer. Cancer Immunol Immunother. 2013, 62, 1811–9. [Google Scholar] [CrossRef] [PubMed]
- Chakraborty, P.K.; Zhang, Y.; Coomes, A.S.; Kim, W.J.; Stupay, R.; Lynch, L.D.; et al. G protein-coupled receptor kinase GRK5 phosphorylates moesin and regulates metastasis in prostate cancer. Cancer Res 2014, 74, 3489–3500. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Chen, Y.; Dong, Y.; Ma, Z.; Zheng, W.; Lin, Y. Prediction of immune infiltration and prognosis for patients with gastric cancer based on the immune-related genes signature. Heliyon. 2023, 9, e22433. [Google Scholar] [CrossRef]
- Mundra, V.; Yang, Y.; von Itzstein, M.S.; Fattah, F.; Gonugunta, A.S.; Hannan, R.; et al. Systemic immune parameters after prior radiation therapy in patients receiving immune checkpoint inhibitors. Transl Oncol. 2023, 34, 101689. [Google Scholar] [CrossRef]
- Ide, H.; Nakagawa, T.; Terado, Y.; Kamiyama, Y.; Muto, S.; Horie, S. Tyk2 expression and its signaling enhances the invasiveness of prostate cancer cells. Biochem Biophys Res Commun, 2008, 369, 292-296. [CrossRef]
- Yuan, S.; Wang, L.; Zhang, H.; Xu, F.; Zhou, X.; Yu, L.; et al. Mendelian randomization and clinical trial evidence supports TYK2 inhibition as a therapeutic target for autoimmune diseases. EBioMedicine. 2023, 89, 104488. [Google Scholar] [CrossRef]
- Zhang, X.; Dong, K.; Zhang, J.; Kuang, T.; Luo, Y.; Yu, J.; et al. GNB1 promotes hepatocellular carcinoma progression by targeting BAG2 to activate P38/MAPK signaling. Cancer Sci. 2023, 114, 2001–2013. [Google Scholar] [CrossRef]
- Vindrieux, D.; Escobar, P.; Lazennec, G. Emerging roles of chemokines in prostate cancer. Endocr Relat Cancer, 2009, 16, 663-673. [CrossRef]
- Goleij, P.; Tabari, M.A.K.; Khandan, M.; Poudineh, M.; Rezaee, A.; Sadreddini, S.; et al. Genistein in focus: pharmacological effects and immune pathway modulation in cancer. Naunyn Schmiedebergs Arch Pharmacol. 2024. [Google Scholar] [CrossRef]
- Vuk-Pavlovic, S., Bulur, P.A., Lin, Y., Qin, R., Szumlanski, C.L., Zhao, X. et al. Immunosuppressive CD14+HLA-DRlow/- monocytes in prostate cancer. Prostate, 2010, 70, 443-455. [CrossRef]
- Takahashi, I.; Takagi, K.; Yamaguchi-Tanaka, M.; Sato, A.; Sato, M.; Miki, Y.; et al. Toll-like receptor (TLR) 4 is a potent prognostic factor in prostate cancer associated with proliferation and invasion. Pathol Res Pract. 2024, 260, 155379. [Google Scholar] [CrossRef]
- Nickols, N.G.; Nazarian, R.; Zhao, S.G.; Tan, V.; Uzunangelov, V.; Xia, Z.; et al. MEK-ERK signaling is a therapeutic target in metastatic castration resistant prostate cancer. Prostate Cancer Prostatic Dis, 2019, 22, 531-538. [CrossRef]
- Emelyanova, A.; Zolotovskaia, M.; Poddubskaya, E.; Modestov, A.; Buzdin, A.; Kuzmin, D. Activation of P38 MAPK Signaling Cascade is Linked with Clinical Outcomes and Therapeutic Responses in Human Cancers. Biochemistry (Mosc). 2024, 89, 2155–2173. [Google Scholar] [CrossRef]
- Iacobas, D.A.; Iacobas, S.; Lee, P.R.; Cohen, J.E.; Fields, R.D. Coordinated Activity of Transcriptional Networks Responding to the Pattern of Action Potential Firing in Neurons. Genes, 2019, 10, 754. [CrossRef]
- Basic Laws of Chemistry–Theories–Principles. Available online at: https://azchemistry.com/basic-laws-of-chemistry. (Accessed October 10, 2024.
- Wang, J.; Ouyang, X.; Zhu, W.; Yi, Q.; Zhong, J. The Role of CXCL11 and its Receptors in Cancer: Prospective but Challenging Clinical Targets. Cancer Control, 2024, 10732748241241162. [CrossRef]
- Ullah, A.; Jiao, W.; Shen, B. The role of proinflammatory cytokines and CXC chemokines (CXCL1-CXCL16) in the progression of prostate cancer: insights on their therapeutic management. Cell Mol Biol Lett, 2024, 29, 73. [CrossRef]
- Iacobas, D.; Wen, J.; Iacobas, S.; Schwartz, N.; Putterman, C. Remodeling of Neurotransmission, Chemokine, and PI3K-AKT Signaling Genomic Fabrics in Neuropsychiatric Systemic Lupus Erythematosus. Genes (Basel). 2021, 12, 251. [Google Scholar] [CrossRef]
- Zhao, S.; Zhang, Y.; Zhang, Q.; Wang, F.; Zhang, D. Toll-like receptors and prostate cancer. Front Immunol, 2014, 5, 352. [CrossRef]
- Michalaki, V., Syrigos, K., Charles, P., Waxman, J. Serum levels of IL-6 and TNF-alpha correlate with clinicopathological features and patient survival in patients with prostate cancer. Br J Cancer, 2004, 90, 2312-2316. [CrossRef]
- Bak, S.P.; Barnkob, M.S.; Bai, A.; Higham, E.M.; Wittrup, K.D.; Chen, J. Differential requirement for CD70 and CD80/CD86 in dendritic cell-mediated activation of tumor-tolerized CD8 T cells. J Immunol, 2012, 189, 1708-1716. [CrossRef]
- Chen, S.; Deng, B.; Zhao, F.; You, H.; Liu, Y.; Xie, L.; et al. Silencing SPP1 in M2 macrophages inhibits the progression of castration-resistant prostate cancer via the MMP9/TGFbeta1 axis. Transl Androl Urol, 2024, 13, 1239-1255. [CrossRef]
- Messex, J.K.; Byrd, C.J.; Thomas, M.U.; Liou, G.Y. Macrophages Cytokine Spp1 Increases Growth of Prostate Intraepithelial Neoplasia to Promote Prostate Tumor Progression. Int J Mol Sci, 2022, 23. [CrossRef]
- KEGG: Kyoto Encyclopedia of Genes and Genomes. Available online at: www.kegg.jp. (Accessed December 12, 2024).
- Krämer, A. , Green, J., Pollard, J, Jr., Tugendreich, S. Causal analysis approaches in Ingenuity Pathway Analysis. Bioinformatics. 2014, 30, 523–30. [Google Scholar] [CrossRef] [PubMed]
- Mulholland, D.J.; Kobayashi, N.; Ruscetti, M.; Zhi, A.; Tran, L.M.; Huang, J.; et al. Pten loss and RAS/MAPK activation cooperate to promote EMT and metastasis initiated from prostate cancer stem/progenitor cells. Cancer Res, 2012, 72, 1878-1889. [CrossRef]
- KEGG-designed functional pathways of the excretory system. Available online at: https://www.kegg.jp/pathway/hsa04960 / 04961 / 04962 / 04964 / 04964 / 04966. (Accessed December 12, 2024).
- Iacobas, D.A.; Iacobas, S. Towards a Personalized Cancer Gene Therapy: A Case of Clear Cell Renal Cell Carcinoma. Cancer & Oncol Res. 2017, 5, 45-52. [CrossRef]
- Iacobas, D.A.; Iacobas, S. Papillary Thyroid Cancer Remodels the Genetic Information Processing Path-ways. Genes, 2024, 15, 621. [CrossRef]
- Iacobas, D.A. Biomarkers, Master Regulators and Genomic Fabric Remodeling in a Case of Papillary Thyroid Carcinoma. Genes, 2020, 11, 1030. [CrossRef]
- Iacobas, D.A.; Tuli, N.Y.; Iacobas, S.; Rasamny, J.K.; Moscatello, A.; Geliebter, J.; et al. Gene master regulators of papillary and anaplastic thyroid cancers. Oncotarget. 2017, 9, 2410–2424. [Google Scholar] [CrossRef] [PubMed]
- Hierarchal gene master regulators of papillary (BCPAP) and anaplastic (8505C) thyroid cancer cell lines. Available online at: https://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?acc=GSE97002 (Accessed December 12, 2024).
- Hierarchal gene master regulators of adenocarcinomic human alveolar basal epithelial cells A549. Available online at: https://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?acc=GSE116361 (Accessed December 12, 2024).
- Transcriptomic effects of Capridine on the acute promyelocytic leukemia HL-60 cell line. Available online at: https://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?acc=GSE72415 (Accessed December 12, 2024).
- Qiu, X.; Guo, D.; Du, J.; Bai, Y.; Wang, F. A novel biomarker, MRPS12 functions as a potential oncogene in ovarian cancer and is a promising prognostic candidate. Medicine (Baltimore). 2021, 100, e24898. [Google Scholar] [CrossRef] [PubMed]
- Wu, L.H.; Wang, X.X.; Wang, Y.; Wei, J.; Liang, Z.R.; Yan, X.; et al. Construction and validation of a prognosis signature based on the immune microenvironment in gastric cancer. Front Surg. 2023, 10, 1088292. [Google Scholar] [CrossRef]
- Muthu, M.; Chun, S.; Gopal, J.; Park, G.-S.; Nile, A.; Shin, J.; et al. The MUDENG Augmentation: A Genesis in Anti-Cancer Therapy? Int. J. Mol. Sci. 2020, 21, 5583. [Google Scholar] [CrossRef]
- Cui, X.; Shang, X.; Xie, J.; Xie, C.; Tang, Z.; Luo, Q.; et al. Cooperation between IRTKS and deubiquitinase OTUD4 enhances the SETDB1-mediated H3K9 trimethylation that promotes tumor metastasis via suppressing E-cadherin expression. Cancer Lett. 2023, 575, 216404. [Google Scholar] [CrossRef]
- de Almeida, F.N.; Vasciaveo, A.; Antao, A.M.; Zou, M.; Di Bernardo, M.; de Brot, S.; et al. A forward genetic screen identifies Sirtuin1 as a driver of neuroendocrine prostate cancer. bioRxiv [Preprint]. 2024,. [CrossRef]
- German, B.; Alaiwi, S.A.; Ho, K.L.; Nanda, J.S.; Fonseca, M.A.; Burkhart, D.L.; et al. MYBL2 Drives Prostate Cancer Plasticity: Inhibiting Its Transcriptional Target CDK2 for RB1-Deficient Neuroendocrine Prostate Cancer. Cancer Res Commun. 2024, 4, 2295–2307. [Google Scholar] [CrossRef]
- Kim, M.; Tamukong, P.; Galvan, G.C.; Yang, Q.; De Hoedt, A.; Freeman, M.R.; et al. Prostate cancers with distinct transcriptional programs in Black and White men. Genome Med. 2024, 16, 92. [Google Scholar] [CrossRef]
- Moran, B.; Rahman, A.; Palonen, K.; Lanigan, F.T.; Gallagher, W.M. Master transcriptional regulators in cancer: discov-ery via reverse engineering approaches and subsequent validation. Cancer Res. 2017, 77, 2186–90. [Google Scholar] [CrossRef]
- Sledziona, J.; Burikhanov, R.; Araujo, N.; Jiang, J.; Hebbar, N.; Rangnekar, V.M. The Tumor Suppressor Par-4 Regulates Adipogenesis by Transcriptional Repression of PPARγ. Cells 2024, 13, 1495. [Google Scholar] [CrossRef]
- Zhou, Q.; Wu, F.; Chen, Y.; Fu, J.; Zhou, L.; Xu, Y.; et al. (2024) Reynoutria multiflora (Thunb.) Moldenke and its ingredient suppress lethal prostate cancer growth by inducing CDC25B-CDK1 mediated cell cycle arrest. Bioorg Chem. 152, 107731. [CrossRef]
- Batson, J.; Maccarthy-Morrogh, L.; Archer, A.; Tanton, H.; Nobes, C.D. EphA receptors regulate prostate cancer cell dis-semination through Vav2-RhoA mediated cell-cell repulsion. Biol Open. 2014, 3, 453–62. [Google Scholar] [CrossRef] [PubMed]
- Batson, J.; Astin, J.W.; Nobes, C.D. Regulation of contact inhibition of locomotion by Ephephrin signalling. J. Microsc. 2013, 251, 232–241.
- Wang, C.; Jiang, X.; Zhao, Q.; Xie, Z.; Cai, H. The diagnostic or prognostic values of FADD in cancers based on pan-cancer analysis. Biomed Rep. 2023, 19, 77. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.; Zhang, F.; Xie, W.; Niu, Y.; Wang, H.; Li, G.; et al. Induced Necroptosis and Its Role in Cancer Immunotherapy. Int. J. Mol. 2024, Sci. 25, 10760. [Google Scholar] [CrossRef]
- McCann, C.; Crawford, N.; Majkut, J.; Holohan, C.; Armstrong, C.W.D.; Maxwell, P.J.; et al. Cytoplasmic FLIP(S) and nuclear FLIP(L) mediate resistance of castrate-resistant prostate cancer to apoptosis induced by IAP antagonists. Cell Death Dis. 2018, 9, 1081. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, M.; Lai, T.H.; Zada, S.; Hwang, J.S.; Pham, T.M.; Yun, M.; et al. Functional Linkage of RKIP to the Epithelial to Mesenchymal Transition and Autophagy during the Development of Prostate Cancer. Cancers 2018, 10, 273. [Google Scholar] [CrossRef]
- Lu, Z.; Wu, C.; Zhu, M.; Song, W.; Wang, H.; Wang, J.; et al. Ophiopogonin D’ induces RIPK1 dependent necroptosis in androgen dependent LNCaP prostate cancer cells. Int J Oncol, 2020, 56, 439-447. [CrossRef]
- Sabater, A.; Sanchis, P.; Seniuk, R.; Pascual, G.; Anselmino, N.; Alonso, D.F.; et al. Unmasking Neuroendocrine Prostate Cancer with a Machine Learning-Driven Seven-Gene Stemness Signature That Predicts Progression. Int. J. Mol. Sci. 2024, 25, 11356. [Google Scholar] [CrossRef]
- Manceau, C.; Fromont, G.; Beauval, J.-B.; Barret, E.; Brureau, L.; Créhange, G.; et al. Biomarker in Active Surveillance for Prostate Cancer: A Systematic Review. Cancers 2021, 13, 4251. [Google Scholar] [CrossRef]
- Moghaddam, S.; Jalali, A.; O’Neill, A.; Murphy, L.; Gorman, L.; Reilly, A.-M.; et al. Integrating Serum Biomarkers into Prediction Models for Biochemical Recurrence Following Radical Prostatectomy. Cancers, 2021, 13, 4162. [CrossRef]
- Hongo, H.; Kosaka, T.; Takayama, K.I.; Baba, Y.; Yasumizu, Y.; Ueda, K.; et al. G-protein signaling of oxytocin receptor as a potential target for cabazitaxel-resistant prostate cancer. PNAS Nexus, 2024. 3, pgae002. [CrossRef]
- Liu, H.; Yin, J.; Wang, H.; Jiang, G.; Deng, M.; Zhang, G.; et al. FOXO3a modulates WNT/beta-catenin signaling and suppresses epithelial-to-mesenchymal transition in prostate cancer cells. Cell Signal, 2015, 27, 510-518. [CrossRef]
- Huang, R.; Guo, L.; Gao, M.; Li, J.; Xiang, S. Research Trends and Regulation of CCL5 in Prostate Cancer. Onco Targets Ther, 2021, 14, 1417-1427. [CrossRef]
- Aldinucci, D.; Borghese, C.; Casagrande, N. The CCL5/CCR5 Axis in Cancer Progression. Cancers (Basel), 2020, 12. [CrossRef]
- Maeda, S.; Motegi, T.; Iio, A. Kaji, K.; Goto-Koshino, Y.; Eto, S. et al. Anti-CCR4 treatment depletes regulatory T cells and leads to clinical activity in a canine model of advanced prostate cancer. J Immunother Cancer, 2022, 10. [CrossRef]
- Rogers, E.N.; Jones, D.Z.; Kidd, N.C.; Yeyeodu, S.; Brock, G.; Ragin, C.; et al. Toll-like receptor-associated sequence variants and prostate cancer risk among men of African descent. Genes Immun, 2013, 14, 347-355. [CrossRef]
- Iacobas, D.A. The Genomic Fabric Perspective on the Transcriptome Between Universal Quantifiers and Personalized Genomic Medicine. Biol Theory 2016, 11, 123–137. [Google Scholar] [CrossRef]
- Tu, S.-M.; Trikannad, A.K.; Vellanki, S.; Hussain, M.; Malik, N.; Singh, S.R.; et al. Stem Cell Origin of Cancer: Clinical Implications beyond Immunotherapy for Drug versus Therapy Develop-ment in Cancer Care. Cancers, 2024, 16, 1151. [CrossRef]
- Tu, S.-M.; Chen, J.Z.; Singh, S.R.; Maraboyina, S.; Gokden, N.; Hsu, P.-C.; et al. Stem Cell Theory of Cancer: Clinical Implications for Cellular Metabolism and Anti-Cancer Metabolomics. Cancers, 2024, 16, 624. [CrossRef]
- San-Jose Manso, L.; Alfranca, A.; Moreno-Pérez, I.; Ruiz-Vico, M.; Velasco, C.; Toquero, P.; et al. Immunome profiling in prostate cancer: a guide for clinicians. Front Immunol. 2024, 15, 1398109. [Google Scholar] [CrossRef]
- Beer, T.M.; Kwon, E.D.; Drake, C.G.; Fizazi, K.; Logothetis, C.; Gravis, G.; et al. Randomized, double-blind, phase III trial of ipilimumab versus placebo in asymptomatic or minimally symptomatic patients with metastatic chemotherapy-naive castration-resistant prostate cancer. J Clin Oncol Off J Am Soc Clin Oncol. 2017, 35, 40–7. [Google Scholar] [CrossRef]
- Antonarakis, E.S.; Piulats, J.M.; Gross-Goupil, M.; Goh, J.; Ojamaa, K.; Hoimes, C.J.; et al. Pembrolizumab for treatment-refractory metastatic castration-resistant prostate cancer: multicohort, open-label phase II KEYNOTE-199 study. J Clin Oncol Off J Am Soc Clin Oncol. 2020, 38, 395–405. [Google Scholar] [CrossRef] [PubMed]
- Schwehn, P.M.; Falter-Braun, P. Inferring protein from transcript abundances using convolutional neural networks. BioData Mining 2025, 18, 18. [Google Scholar] [CrossRef] [PubMed]
- Mekic, R.; Zolotovskaia, M.A.; Sorokin, M.; Mohammad, T.; Shaban, N.; Musatov, I.; Tkachev, V.; et al. Number of human protein interactions correlates with structural, but not regulatory conservation of the respective genes. Front Genet. 2024, 15, 1472638. [Google Scholar] [CrossRef] [PubMed]
- Iacobas, D.A.; Zhang, D. Prostate cancer-induced remodeling of the topologies and in-terplay of the TLR (toll-like receptor) and chemokine signaling pathways, 2024,. [CrossRef]
| CHEMOKINE SIGNALING | |||||
|---|---|---|---|---|---|
| Gene | Description | N | A | B | C |
| GNAI2 | guanine nucleotide-binding protein (G protein), alpha inhibiting activity polypeptide 2 | 58 | 69 | 96 | 68 |
| RAC3 | ras-related C3 botulinum toxin substrate 3 (rho family, small GTP binding protein | 23 | 11 | 15 | 17 |
| STAT2 | signal transducer and activator of transcription 2 | 18 | 16 | 22 | 24 |
| GNAI2 | guanine nucleotide-binding protein (G protein), alpha inhibiting activity polypeptide 2 | 58 | 69 | 96 | 68 |
| CXCL14 | chemokine (C-X-C motif) ligand 14 | 5 | 33 | 36 | 23 |
| NFKBIA | nuclear factor of kappa light polypeptide gene enhancer in B-cells inhibitor, alpha | 15 | 32 | 42 | 23 |
| GNAI2 | guanine nucleotide-binding protein (G protein), alpha inhibiting activity polypeptide 2 | 58 | 69 | 96 | 68 |
| NFKBIA | nuclear factor of kappa light polypeptide gene enhancer in B-cells inhibitor, alpha | 15 | 32 | 42 | 23 |
| CXCL14 | chemokine (C-X-C motif) ligand 14 | 5 | 33 | 36 | 23 |
| GNAI2 | guanine nucleotide binding protein (G protein), alpha inhibiting activity polypeptide 2 | 58 | 69 | 96 | 68 |
| STAT2 | signal transducer and activator of transcription 2 | 18 | 16 | 22 | 24 |
| NFKBIA | nuclear factor of kappa light polypeptide gene enhancer in B-cells inhibitor, alpha | 15 | 32 | 42 | 23 |
| TOLL-LIKE RECEPTOR SIGNALING | |||||
| STAT2 | signal transducer and activator of transcription 2 | 18 | 16 | 22 | 24 |
| MAP2K7 | mitogen-activated protein kinase kinase 7 | 17 | 12 | 16 | 14 |
| PIK3R2 | phosphoinositide-3-kinase, regulatory subunit 2 (beta) | 15 | 16 | 16 | 13 |
| NFKBIA | nuclear factor of kappa light polypeptide gene enhancer in B-cells inhibitor, alpha | 15 | 32 | 42 | 23 |
| IRF7 | interferon regulatory factor 7 | 10 | 31 | 42 | 21 |
| PIK3R2 | phosphoinositide-3-kinase, regulatory subunit 2 (beta) | 15 | 16 | 16 | 13 |
| NFKBIA | nuclear factor of kappa light polypeptide gene enhancer in B-cells inhibitor, alpha | 15 | 32 | 42 | 23 |
| IRF7 | interferon regulatory factor 7 | 10 | 31 | 42 | 21 |
| STAT2 | signal transducer and activator of transcription 2 | 18 | 16 | 22 | 24 |
| STAT2 | signal transducer and activator of transcription 2 | 18 | 16 | 22 | 24 |
| NFKBIA | nuclear factor of kappa light polypeptide gene enhancer in B-cells inhibitor, alpha | 15 | 32 | 42 | 23 |
| IRF7 | interferon regulatory factor 7 | 10 | 31 | 42 | 21 |
| CHEMOKINE SIGNALING | Region | ||||
|---|---|---|---|---|---|
| Gene | Description | N | A | B | C |
| CCL15 | chemokine (C-C motif) ligand 15 | 2.75 | -1.91 | 0.37 | 0.10 |
| VAV2 | vav 2 guanine nucleotide exchange factor | 2.39 | -0.65 | -0.59 | 2.37 |
| KRAS | Kirsten rat sarcoma viral oncogene homolog | 1.73 | 0.01 | -1.00 | 0.35 |
| GNB1 | guanine nucleotide-binding protein (G protein), beta polypeptide 1 | -0.40 | 4.18 | 0.06 | 0.63 |
| CXCL16 | chemokine (C-X-C motif) ligand 16 | 0.18 | 2.06 | 0.06 | -1.01 |
| FOXO3 | forkhead box O3 | 0.49 | 2.02 | 0.76 | -0.51 |
| MAPK1 | mitogen-activated protein kinase 1 | -0.72 | 0.38 | 2.59 | 0.33 |
| GRK5 | G protein-coupled receptor kinase 5 | -1.24 | 0.26 | 1.55 | -1.07 |
| CCL16 | chemokine (C-C motif) ligand 16 | 0.40 | 0.25 | 1.46 | 3.65 |
| CCL16 | chemokine (C-C motif) ligand 16 | 0.40 | 0.25 | 1.46 | 3.65 |
| VAV2 | vav 2 guanine nucleotide exchange factor | 2.39 | -0.65 | -0.59 | 2.37 |
| PLCB1 | phospholipase C, beta 1 (phosphoinositide-specific) | -0.69 | -0.53 | 0.13 | 2.29 |
| TOLL-LIKE RECEPTOR SIGNALING | |||||
| PIK3R1 | phosphoinositide-3-kinase, regulatory subunit 1 (alpha) | 1.56 | -0.24 | 1.09 | 1.34 |
| TBK1 | TANK-binding kinase 1 | 1.34 | 1.46 | -0.30 | 0.05 |
| PIK3CA | phosphatidylinositol-4,5-bisphosphate 3-kinase, catalytic subunit alpha | 1.30 | 0.62 | 0.10 | -0.31 |
| TYK2 | tyrosine kinase 2 | -1.85 | 2.95 | 0.74 | -1.71 |
| RIPK1 | receptor (TNFRSF)-interacting serine-threonine kinase 1 | 1.05 | 2.79 | 0.96 | 0.94 |
| CD14 | CD14 molecule | -0.41 | 1.83 | 1.76 | 0.66 |
| TOLLIP | toll interacting protein | -1.05 | 1.29 | 2.67 | -1.19 |
| MAPK1 | mitogen-activated protein kinase 1 | -0.72 | 0.38 | 2.59 | 0.33 |
| IRF3 | interferon regulatory factor 3 | 0.87 | 0.74 | 2.20 | -0.36 |
| IRF5 | interferon regulatory factor 5 | -0.11 | 1.02 | 0.43 | 2.66 |
| MAP2K3 | mitogen-activated protein kinase kinase 3 | 0.75 | 1.34 | 0.54 | 1.83 |
| CCL5 | chemokine (C-C motif) ligand 5 | -1.87 | -0.52 | -0.76 | 1.66 |
| CHEMOKINE SIGNALING | Region | ||||
|---|---|---|---|---|---|
| Gene | Description | N | A | B | C |
| GNG13 | guanine nucleotide-binding protein (G protein), gamma 13 | -2.90 | -0.81 | -1.12 | -0.25 |
| FGR | FGR proto-oncogene, Src family tyrosine kinase | -2.82 | 0.11 | -0.02 | -0.23 |
| CXCL9 | chemokine (C-X-C motif) ligand 9 | -2.48 | -1.37 | 0.76 | -1.50 |
| CCL15 | chemokine (C-C motif) ligand 15 | 2.75 | -1.91 | 0.37 | 0.10 |
| CCL14 | chemokine (C-C motif) ligand 14 | -1.66 | -1.54 | -1.13 | -1.47 |
| CXCL11 | chemokine (C-X-C motif) ligand 11 | -2.18 | -1.44 | -1.62 | -0.88 |
| CCL19 | chemokine (C-C motif) ligand 19 | -1.99 | 0.90 | -1.91 | -2.41 |
| CCL17 | chemokine (C-C motif) ligand 17 | -0.38 | -0.15 | -1.75 | 0.54 |
| CXCL11 | chemokine (C-X-C motif) ligand 11 | -2.18 | -1.44 | -1.62 | -0.88 |
| CCL19 | chemokine (C-C motif) ligand 19 | -1.99 | 0.90 | -1.91 | -2.41 |
| NFKB1 | nuclear factor of kappa light polypeptide gene enhancer in B-cells 1 | 0.91 | -0.82 | 0.64 | -2.23 |
| CXCL9 | chemokine (C-X-C motif) ligand 9 | -2.48 | -1.37 | 0.76 | -1.50 |
| TOLL-LIKE RECEPTOR SIGNALING | |||||
| CD86 | CD86 molecule | -3.10 | -0.49 | -1.12 | -1.41 |
| FOS | FBJ murine osteosarcoma viral oncogene homolog | -2.70 | -1.56 | -0.83 | -1.92 |
| CXCL9 | chemokine (C-X-C motif) ligand 9 | -2.48 | -1.37 | 0.76 | -1.50 |
| TICAM2 | TICAM2 – TIR domain-containing adaptor molecule 2 | -0.83 | -2.27 | -0.63 | 0.17 |
| SPP1 | secreted phosphoprotein 1 | -1.22 | -1.61 | -0.28 | 0.28 |
| FOS | FBJ murine osteosarcoma viral oncogene homolog | -2.70 | -1.56 | -0.83 | -1.92 |
| CXCL11 | chemokine (C-X-C motif) ligand 11 | -2.18 | -1.44 | -1.62 | -0.88 |
| TNF | tumor necrosis factor | -0.89 | -0.39 | -1.60 | -0.49 |
| CD86 | CD86 molecule | -3.10 | -0.49 | -1.12 | -1.41 |
| NFKB1 | nuclear factor of kappa light polypeptide gene enhancer in B-cells 1 | 0.91 | -0.82 | 0.64 | -2.23 |
| FOS | FBJ murine osteosarcoma viral oncogene homolog | -2.70 | -1.56 | -0.83 | -1.92 |
| TLR4 | toll-like receptor 4 | 0.15 | 1.34 | 0.64 | -1.90 |
| CHEMOKINE SIGNALING | ||||||
|---|---|---|---|---|---|---|
| Gene | Description | N | A | B | C | |
| CCL15 | chemokine (C-C motif) ligand 15 | 16.84 | 0.14 | 1.36 | 1.58 | |
| PRKCD | protein kinase C, delta | 9.96 | 2.26 | 1.62 | 3.66 | |
| VAV2 | vav 2 guanine nucleotide exchange factor | 9.22 | 2.32 | 1.57 | 3.79 | |
| GNB1 | guanine nucleotide binding protein (G protein), beta polypeptide 1 | 1.94 | 34.15 | 1.51 | 4.54 | |
| JAK2 | Janus kinase 2 | 1.93 | 9.99 | 4.50 | 3.21 | |
| TYK2 | tyrosine kinase 2 | 0.79 | 8.75 | 3.13 | 1.07 | |
| CCR6 | chemokine (C-C motif) receptor 6 | 1.36 | 4.07 | 5.46 | 1.22 | |
| CCR1 | chemokine (C-C motif) receptor 1 | 1.98 | 4.40 | 4.88 | 3.32 | |
| BCAR1 | BCAR1 scaffold protein, Cas family member | 1.94 | 3.30 | 4.81 | 4.51 | |
| CCL16 | chemokine (C-C motif) ligand 16 | 4.03 | 4.20 | 2.63 | 14.72 | |
| PLCB1 | phospholipase C, beta 1 (phosphoinositide-specific) | 1.13 | 2.48 | 1.47 | 9.67 | |
| PREX1 | phosphatidylinositol-3,4,5-trisphosphate-dependent Rac exchange factor 1 | 2.14 | 1.87 | 2.03 | 8.07 | |
| TOLL-LIKE RECEPTOR SIGNALING | ||||||
| FADD | Fas (TNFRSF6)-associated via death domain | 7.28 | 5.03 | 2.24 | 0.42 | |
| IKBKB | inhibitor of kappa light polypeptide gene enhancer in B-cells, kinase beta | 5.86 | 1.04 | 0.91 | 1.21 | |
| MAP2K4 | mitogen-activated protein kinase kinase 4 | 5.80 | 2.35 | 2.23 | 3.08 | |
| RIPK1 | receptor (TNFRSF)-interacting serine-threonine kinase 1 | 2.60 | 11.86 | 3.01 | 5.31 | |
| CD14 | CD14 molecule | 1.20 | 9.79 | 2.58 | 5.27 | |
| TOLLIP | toll interacting protein | 1.08 | 9.03 | 7.21 | 1.45 | |
| TOLLIP | toll interacting protein | 1.08 | 9.03 | 7.21 | 1.45 | |
| MAPK1 | mitogen-activated protein kinase 1 | 1.50 | 2.69 | 6.40 | 3.53 | |
| MAP3K7 | mitogen-activated protein kinase kinase kinase 7 | 4.33 | 4.40 | 6.02 | 2.77 | |
| IRF5 | interferon regulatory factor 5 | 1.83 | 4.40 | 2.99 | 11.34 | |
| IL1B | interleukin 1, beta | 0.76 | 2.60 | 1.17 | 5.48 | |
| RIPK1 | receptor (TNFRSF)-interacting serine-threonine kinase 1 | 2.60 | 11.86 | 3.01 | 5.31 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).





