1. Introduction
As of March 2025, the COVID-19 resulted in more than 777 million reported cases and more than 7 million confirmed deaths globally [
1]. SARS-CoV-2 high transmission and mutation occurrence in the virus genome result in the emergence of new variants that impact COVID-19 vaccines efficacy and virus transmission by evading the host immune system [
2]. The World Health Organization (WHO) have classified the variants in three groups: variants of concern (VOCs), variants of interest (VOIs) and variants under monitoring (VUMs) [
3].
VUMs are variants with genetic changes that are suspected to affect virus characteristics and spread more than other circulating variants, but evidence of their phenotypic or epidemiological impact remains unclear [
4]. VOIs have genetic changes that are predicted to affect virus transmissibility, virulence, antibody evasion, susceptibility to therapeutics, and detection. VOIs may also show high prevalence in the population, having an epidemiological impact suggestive of an emerging risk to global public health [
4]. P.2 was a VOI first detected in the clinical setting in April 2020 and was widespread in Rio de Janeiro, Brazil [
3,
5]. VOCs are variants associated with a more severe clinical presentation, or changes in COVID-19 epidemiology that cause a substantial impact on the ability of health systems to provide care to patients with COVID-19 or others illness. They represent a burden on the public health system. Additionally, VOCs are variants known to significantly decrease the effectiveness of available vaccines in protecting against severe disease [
4]. The following variants were assigned as VOCs and were first detected in clinical samples: Alpha (B.1.1.7) in the United Kingdom (September 2020), Beta (B.1.351) in South Africa (October 2020), Gamma (P.1) in Brazil (January 2021), Delta (B.1.617.2) in India (December 2020) and Omicron (B.1.1.529) in South Africa (November 2021) [
6,
7,
8,
9,
10]. The Omicron variant has already many sublineages that spread globally [
11].
SARS-CoV-2 variants have many polymorphisms, mostly in the S protein coding gene. The Spike protein comprises an S1 subunit facing the surface of the membrane and an S2 transmembrane subunit. The S1 subunit is responsible for binding to the receptor on the target cell whereas the S2 is involved in the fusion of the viral and host membrane cell, playing a crucial role in the entry of the virus into target cells [
12,
13]. The S1 subunit encompasses the N-terminal domain (NTD) and the receptor binding domain (RBD), both of which harbor numerous polymorphisms [
14]. Since the S gene harbors many mutations and some of them differ among SARS-CoV-2 variants, nucleotide sequencing of the S gene is used for identifying virus variants [
15,
16].
Considering that SARS-CoV-2 RNA has been detected in feces of infected people, wastewater-based epidemiology (WBE) serves as a valuable tool for assessing the prevalence of infections within the population [
17,
18]. Indeed, WBE is effective in monitoring SARS-CoV-2 in the population. This approach has been employed to quantify SARS-CoV-2 and identify variants in sewage [
19,
20]. However, genome detection by WBE is challenging due to the presence of reaction inhibitors and the low concentrations of SARS-CoV-2 in sewage [
21,
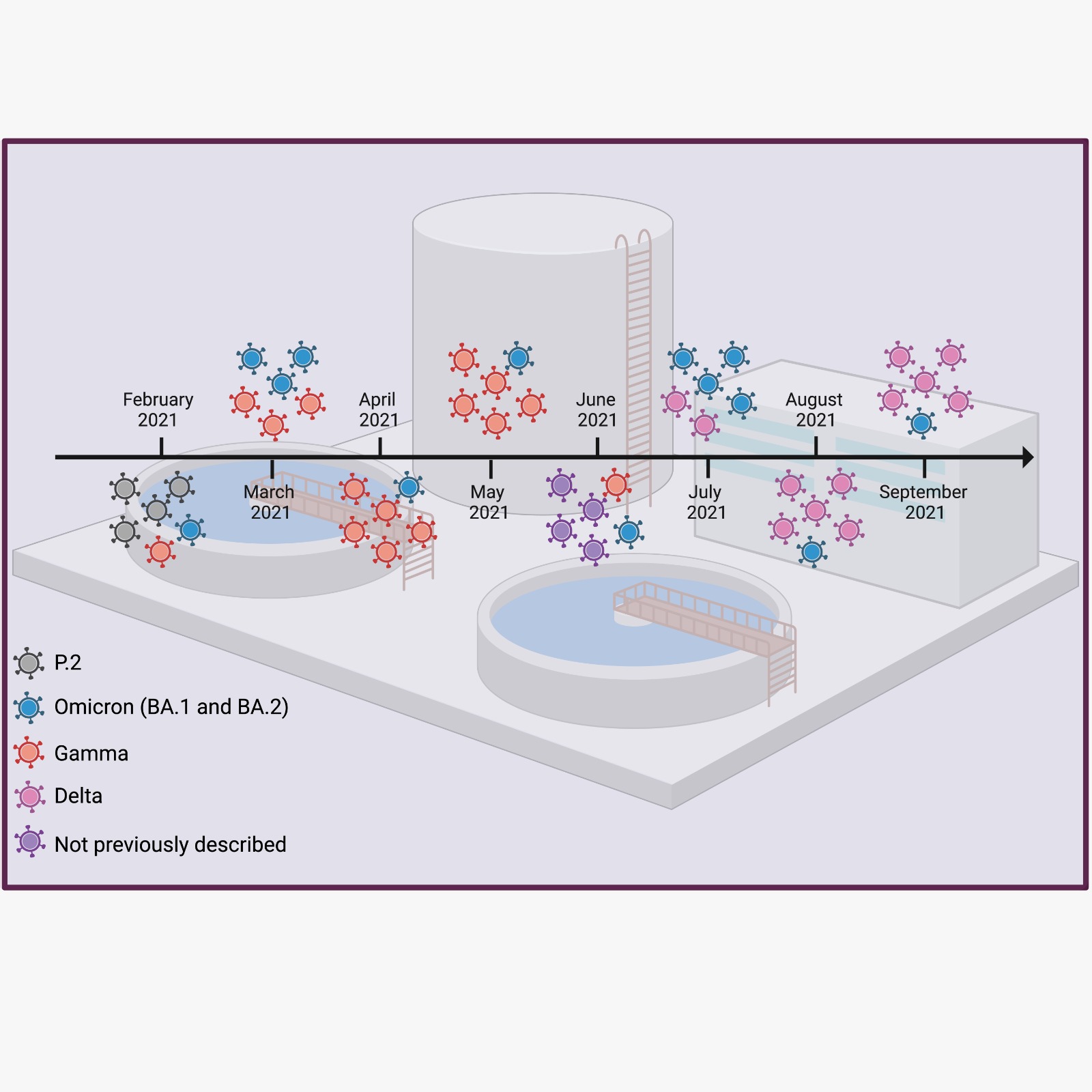
22]. Therefore, the present study aimed to improve SARS-CoV-2 variant detection in wastewater by employing nested-PCR followed by next-generation sequencing of selected small amplicons of the S gene. Samples were collected between February and September 2021 in a major Wastewater Treatment Plant of Rio de Janeiro, Brazil. The results provide valuable insights into the prevalence and spread of the virus in the region. Our analysis identified and estimated the frequency of SARS-CoV-2 variants mutations in wastewater samples, which were then compared to the occurrence of clinical cases at the time. Our approach successfully identified SARS-CoV-2 variants, overcoming challenges posed by reaction inhibitors and low virus concentration.
2. Results
2.1. SARS-CoV-2 S Gene Fragments Are Efficiently Amplified in Wastewater Samples
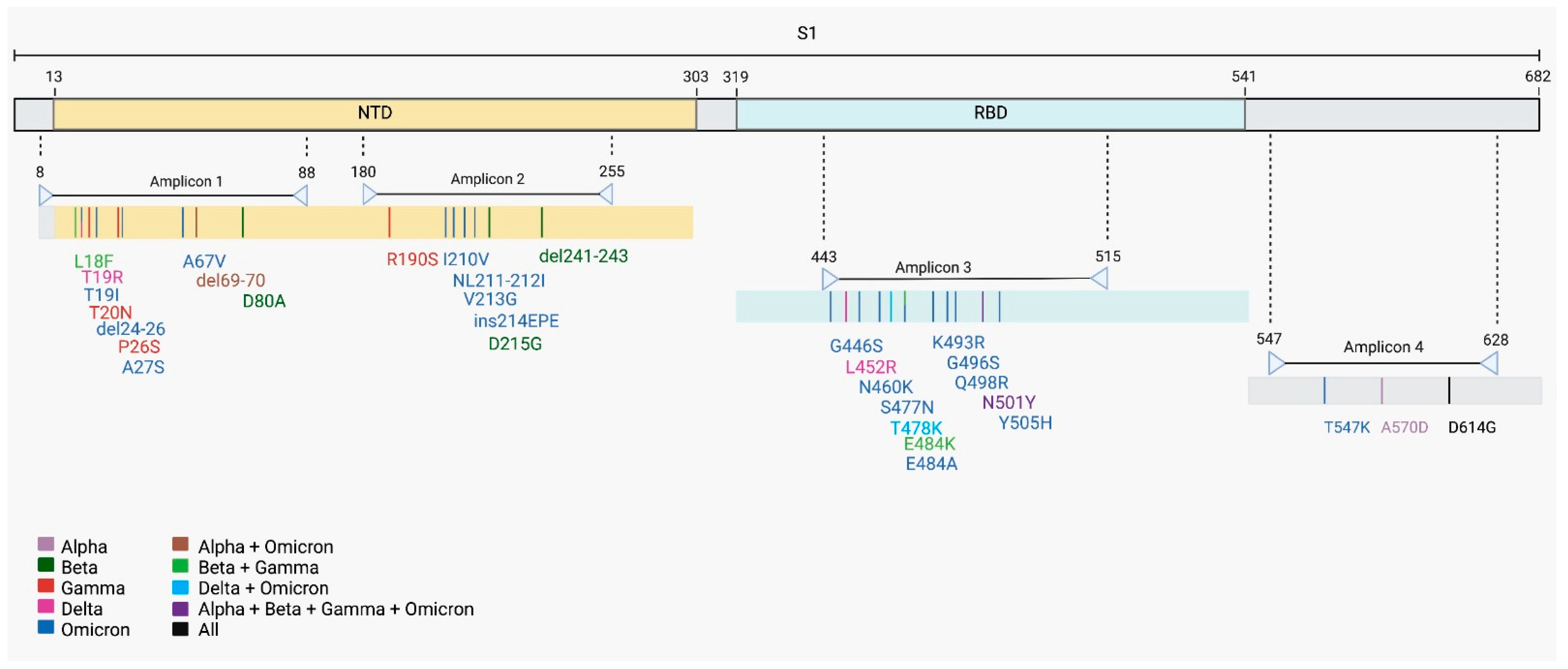
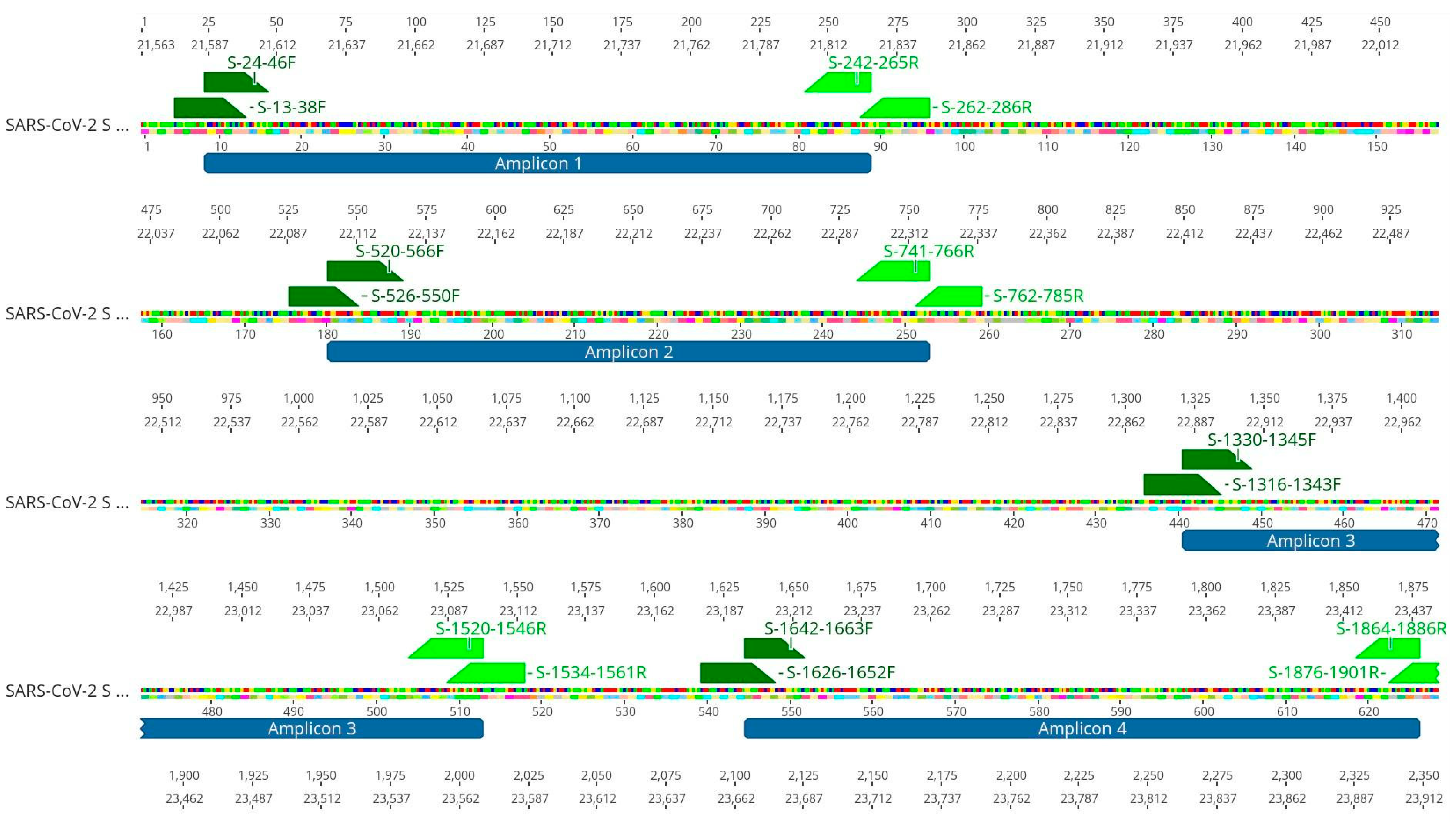
Alegria Wastewater Treatment Plant (WWTP) samples, collected between February and September of 2021, showed a low amount of SARS-CoV-2 genomic RNA, as revealed by the Cts obtained for each sample by the SARS-CoV-2 diagnostics RT-qPCR assay (
Table 1). To increase the amount of SARS-CoV-2 template used for sequencing, we performed a nested-PCR of selected regions in the S gene that generated amplicons of around 230 bp. These regions harbor Spike mutations and indels that were associated with a variant of concern (
Figure 1). All four S regions from the eight wastewater samples were successfully amplified by nested-PCR (
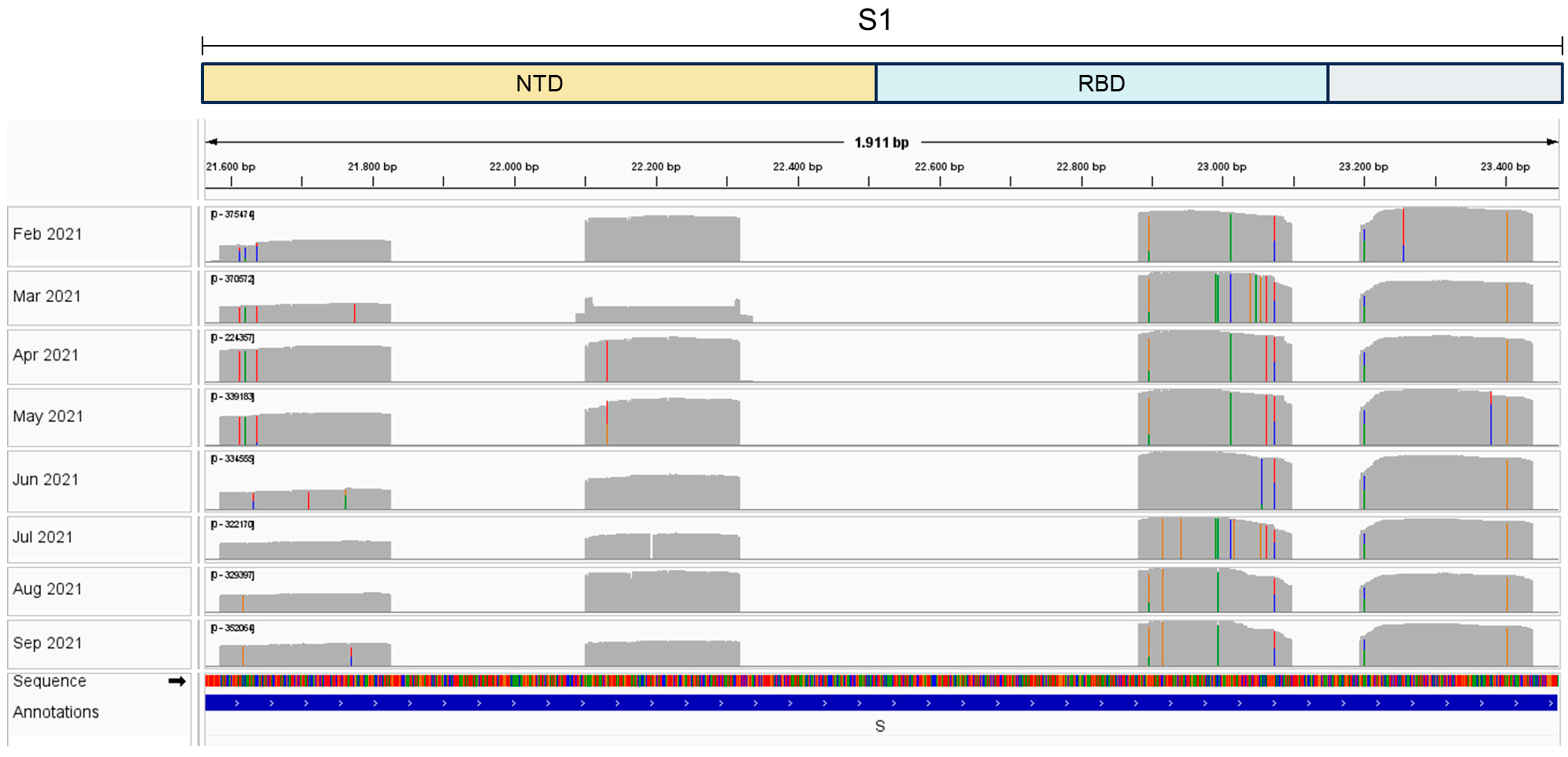
Figure S1) and sequenced using the Ion Torrent Platform (
Figure 2). Results show mutations at different sites over eight months,
each month corresponding to a unique sample collection, that matched virus variants that were considered variants of concern (VOCs) at the time of sample collection (
Figure 2). Our results show that nested-PCR efficiently amplified SARS-CoV-2 S regions that harbor mutation sites, as confirmed by next generation sequencing.
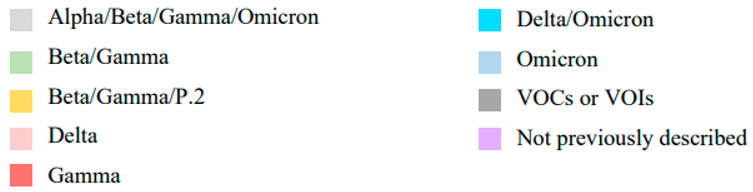
2.2. Identification of 29 Mutations in SARS-CoV-2 S Gene
To investigate the mutations associated with SARS-CoV-2 S variants, we searched for Single Nucleotide Polymorphisms (SNPs) and found 29 different SARS-CoV-2 S mutations in Alegria WWTP samples (
Table 2). Mutations matched those found in SARS-CoV-2 Alpha, Beta, Gamma, Delta, Omicron and P.2 variants. We also identified mutations that were not yet described at the time of sample collection. Mutations E484K and D614G predominated in February, less frequent mutations that match Gamma and Omicron variants were also observed during this period. Mutations found in samples from March matched all variants of concern; Gamma and Omicron mutations predominated during this period. In samples from April and May, we detected five mutations that matched Gamma while three matched Omicron variants. Curiously, Gamma matching mutations were fewer in February, but were abundant in March, April, and May. In June we detected mutations that had not been described at the time of sample collection. In July, August, and September we detected mutations that matched Delta and Omicron variants (
Table 2). Omicron matching mutations were detected in all months at varied frequencies. Interestingly, we first detected an Omicron matching mutation in February 2021, although the Omicron variant was first documented in a clinical sample months later, in November 2021 [
3]. Since in June we detected four mutations that had not been described at the time that this article was under preparation, while in March and July many Omicron matching mutations were detected, we performed Sanger sequencing to check their sequences. Sanger results confirmed the NGS results. Together, these results indicate that it is possible to monitor SARS-CoV-2 variant changes through wastewater using next generation sequencing of selected small fragments of the S gene.
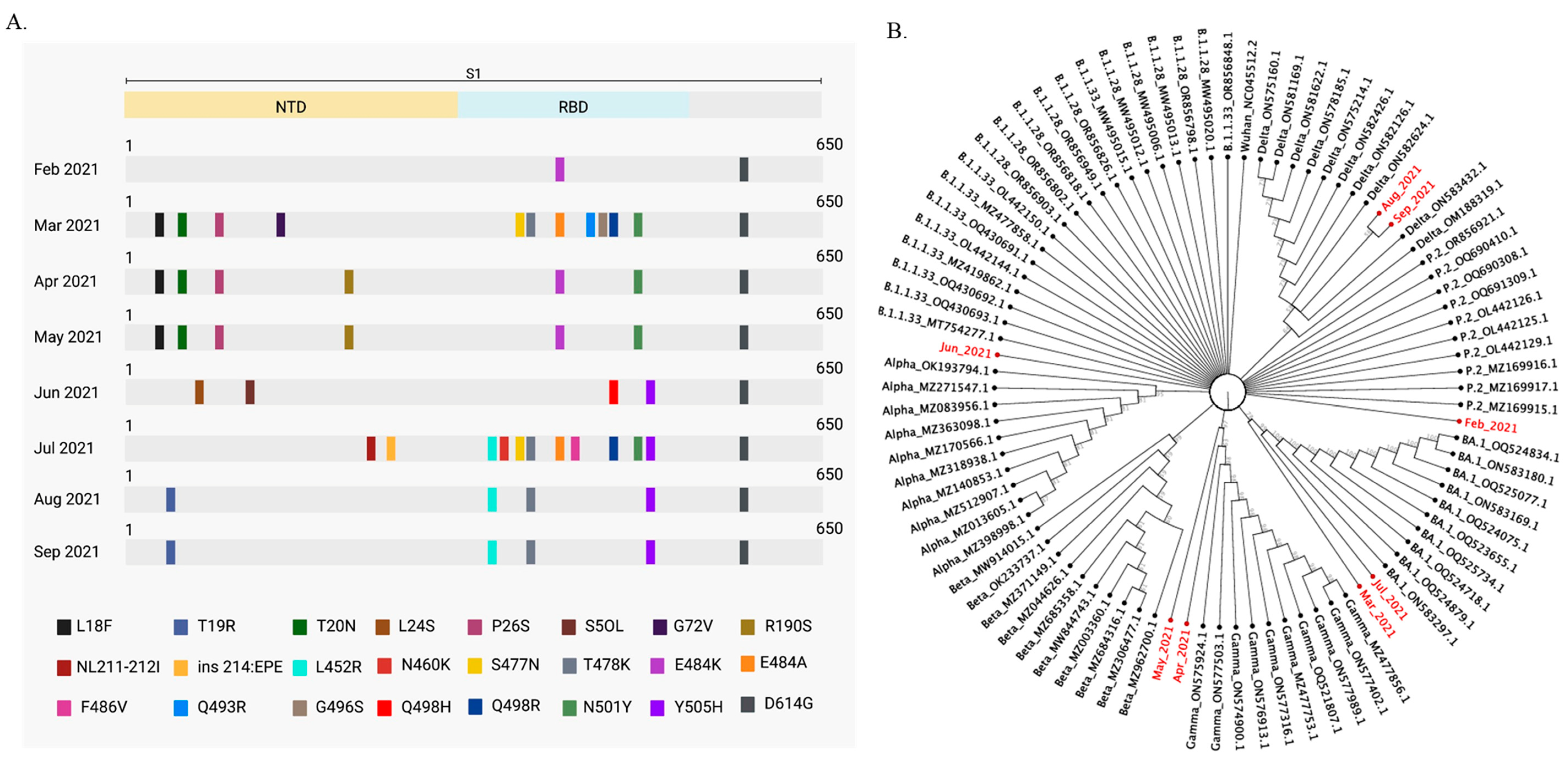
2.3. SARS-CoV-2 Variants Classification in Wastewater
To identify SARS-CoV-2 predominant variants circulating in wastewater from February to September 2021 in Rio de Janeiro, we aligned our sequenced samples to SARS-CoV-2 variant sequences from 2021, available at the Virus Variation Resource at the National Center for Biotechnology Information [
25]. A phylogenetic tree was built based on this alignment that contemplated only mutations with frequencies above 55%. March and July were the months when we found the greater number of mutations. Omicron mutations were in high frequency during these months (
Figure 3). Mutations previously associated with VOCs were identified in all months (
Figure 3A). Sequenced samples were compared to B.1.1.33, B.1.1.28, Alpha, Beta, Delta, Gamma, Omicron (BA.1) and P.2 sequences. We analyzed all VOCs circulating in Brazil in 2021 and the P.2 variant. P.2 was a SARS-CoV-2 variant of interest (VOI), that emerged in April 2020 and had high circulation in Rio de Janeiro [
3,
5]. The Wuhan SARS-CoV-2 reference sequence and the early lineages B.1.1.33 and B.1.1.28 were also included in the analysis. SARS-CoV-2 sequence clusters are shown in
Figure 3B. As expected, April and May wastewater samples clustered with Gamma sequences, while August and September samples clustered with Delta sequences. On the other hand, March and July wastewater samples clustered with Omicron (BA.1) sequences, although Omicron became a VOC only in November 2021. Together, these results show that the dynamics of SARS-CoV-2 variants circulation may be inferred by phylogenetic analysis that included the wastewater predominant mutations found in clinical sequences available on the database [
26].
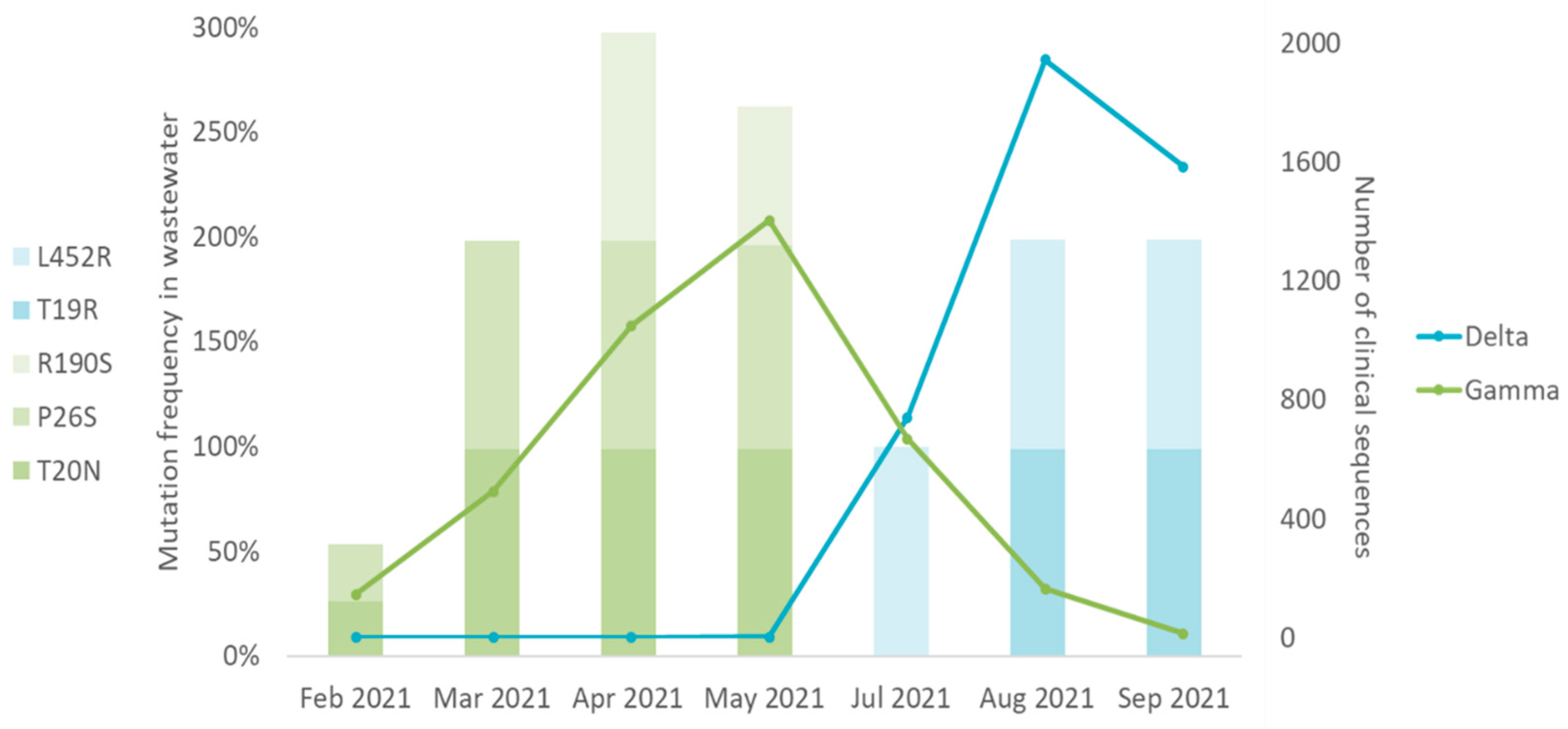
2.4. SARS-CoV-2 Mutations Found in Wastewater Samples Match SARS-CoV-2 Variants in Clinical Samples
To investigate if the SARS-CoV-2 variant in wastewater reflected the findings obtained from clinical samples in the same period, we compared the frequency of the variant-matching mutation detected in wastewater with clinical SARS-CoV-2 variant sequences. Only mutations that were unique to a single variant were considered. SARS-CoV-2 clinical sequences were obtained in [
26] enabled by data from GISAID. Omicron matching mutations detected in wastewater samples were omitted in the analysis, since there were no clinical sequences available during the corresponding period - February to September 2021. Data analyses showed that Gamma and Delta variants were the prevalent variants circulating in Rio de Janeiro between February and September 2021 (
Figure 4). Gamma matching mutations were prevalent between February and May 2021, the period when Gamma was the major variant identified in clinical samples. Delta matching mutations were prevalent between July and September 2021, the period when Delta was prevalent in clinical samples (
Figure 4). These results suggest that wastewater samples reflect the distribution profile of SARS-CoV-2 variants found in clinical samples through time.
3. Discussion
We were able to identify mutation matching SARS-CoV-2 variants and estimate their frequencies in wastewater samples. Alegria Wastewater Treatment Plant (WWTP) samples from Rio de Janeiro, Brazil yielded a low amount of SARS-CoV-2 genomic RNA (
Table 1), which could compromise the whole genome sequencing. In these situations, previous amplification of target regions, such as of a gene or part of a gene, can improve the sequencing performance [
27,
28]. The number and genome location of target regions need to be carefully selected to detect sufficient mutations to identify variants. Thus, we carried out nested-PCR based on four SARS-CoV-2 S gene regions (
Figure 1 and
Figure 5). The small size of the amplicons (around 230 bp) lets us prepare the libraries for sequencing without the need to perform any fragmentation step. The removal of the fragmentation step reduces sequencing artifacts and enzymatic bias, such as insertion and deletion of nucleotides resulting from physical and enzymatic shearing. This strategy improves library construction and the quality of the next generation sequencing (NGS) [
29,
30].
Nested-PCR efficiently amplified the four SARS-CoV-2 S regions from Alegria WWTP samples (
Figure S1). Additionally, amplicons harboring virus mutation sites were efficiently sequenced in the Ion Torrent Platform (
Figure 2), showing that sequencing of small fragments of the S gene previously amplified is a successful approach to adopt when working with wastewater samples that have low amounts of SARS-CoV-2 genomic RNA.
Between February and September 2021, we found 29 SARS-CoV-2 S mutations in Alegria WWTP samples that matched P.2 and were considered VOCs at the time. (
Table 2). Studies have shown that the frequency of the Alpha mutation varied in wastewaters in England and Japan, between October 2020 and January 2021 [
31]. Similarly, we detected Gamma mutations at various frequencies between February and May 2021 in Rio de Janeiro wastewater samples. Gamma mutations were detected at low frequency in February 2021, and then at increasing frequencies in the following months, being the predominant variant found in April and May 2021 (
Table 2,
Figure 3). Our finding indicates that by adopting next generation sequencing of selected small fragments of the S gene, it is possible to identify SARS-CoV-2 variant mutations that appear at low frequencies in wastewater before they become predominant in the population.
Studies have shown that VOCs and mutations associated with VOCs can be identified in wastewater in periods between 2 months to two weeks before it is detected in clinical samples [
32,
33,
34]. We identified mutations matching those found in the Omicron variant (BA.1 and BA.2 sublineages) nine months before they were described in the first clinical sample, suggesting the potential of wastewater surveillance to anticipate variant’s detection (
Table 2) [
3]. Omicron matching mutations were detected in high frequency in wastewater samples in March and July 2021. At the same time, Gamma and Delta matching mutations were also detected in high frequency, and the latter were the ones that became predominant in April and August 2021, respectively, while Omicron was later established in December 2021 (
Table 2;
Figure 3) [
3]. Shempela and co-worker demonstrated that B.1.1.529, the first Omicron lineage described, may not have been completely replaced by newer Omicron subvariants and thus could be circulating and possibly contributing to the community transmission of SARS-CoV-2 [
35]. So, SARS-CoV-2 variants and subvariants co-circulation seem to be common.
Studies show that Omicron replication and infectivity in Caco-2 cells, an epithelial cell derived from colon tissue, is lower than that observed in Gamma and Delta variants [
36]. Gamma and Delta high kinetic replication in colon tissue may explain the prevalence of these variants in wastewater, which is an environment known to be predominated by feces. It is possible that Omicron emerged at the same time as Gamma and Delta variants, but the latter variants initially predominated. The vaccination program that started in March 2021 in Brazil could have contributed to further establish Omicrons as a major variant circulating in Brazil, since vaccination was more effective against Gamma and Delta [
37,
38,
39].
Phylogenetic analysis of SARS-CoV-2 mutations detected in wastewater samples and SARS-CoV-2 sequences from Virus Variation Resource hosted by the National Center for Biotechnology Information allowed us to infer about variant circulation in wastewater between February and September 2021 (
Figure 3B). Wastewater samples from February clustered with P.2 sequences (
Figure 3B). Indeed, the P.2 variant was prevalent during this period in Rio de Janeiro [
40]. Wastewater samples collected between April and May 2021 clustered with Gamma sequences, and wastewater samples from August to September clustered with Delta sequences, which agreed with the variants more prevalent in clinical samples during these periods (
Figure 4), indicating that wastewater samples reflect the distribution of SARS-CoV-2 variants in the population.
While this article was under preparation, new Omicron subvariants emerged that could not be investigated by our approach, because it would require the amplification and sequencing of additional genomic regions [
41]. In fact, we were not able to predict which one would be the next variant to be established in the population because the spread of a new variant depends on many factors that cannot be inferred based solely on the frequency of a given mutation at a given time. Nevertheless, we did detect Omicron (BA.1 and BA.2) mutations in March of 2021, and the variant was established later, in December of the same year (
Figure 3A) [
3].
The approach used in this study may be applied to detect SARS-CoV-2 mutation-matching variants in wastewater samples with low amounts of genomic RNA. The approach may be expanded by designing customized primers for additional genomic regions to identify new variants, contributing to SARS-CoV-2 wastewater monitoring. New sublineage of SARS-CoV-2 are continuously emerging and another pandemic caused by other pathogens is a real threat. Therefore, approaches that allow us to learn how variants emerge and how they relate to clinical outcomes are crucial for our understanding of the pathogen circulation, providing valuable data for public health management.
4. Materials and Methods
4.1. Samples Information
Eight SARS-CoV-2 positive wastewater samples were obtained from Estudo Monitora Corona coordinated by Professor Isaac Volshan Jr. from the Department of Water Resources and Environment from Polytechnic Institute of Federal University of Rio de Janeiro, Brazil. Single samples were manually collected monthly on a timely basis between February 2021 and September 2021 from Alegria Wastewater Treatment Plant (WWTP) located in the metropolitan area of Rio de Janeiro, Brazil. Alegria was the biggest WWTPs operated by Companhia Estadual de Águas e Esgotos (CEDAE), the major city’s sanitation company at the time of this study. Alegria WWTP receives sewage from 1,165,042 people living in 45 neighborhoods. Wastewater samples were kept at 4°C and were processed up to 72 hours.
4.2. Virus Concentration
Wastewater samples were pasteurized at 60°C for 90 minutes to ensure safety for the laboratory personnel [
42,
43]. After inactivation, 40 ml of samples were filtered in 0.22 µm polyethersulfone membrane (ref. K18-230, Kasvi) to remove bacterial cells and debris. Filtered samples were precipitated with polyethylene glycol 8000 (10% [wt/vol]; Promega) and NaCl (0.4 M; Isofar). The mixtures were shaken at room temperature until polyethylene glycol was fully dissolved and centrifuged at 9,000 x g for 2 hours. The viral pellet was resuspended in 1.0 ml of PBS and proceeded to RNA extraction.
4.3. RNA Extraction and SARS-CoV-2 RT-qPCR
Viral RNA was extracted from 0.2 ml of viral concentrate with Bio Gene Viral DNA/RNA Extraction (ref. K204-4, Bioclin) following manufacturer’s protocol. RNA was eluted in 50 µl of DNAse/RNAse free water and quantified by RT-qPCR using primers and probes targeting the SARS-CoV-2 N gene. Primers and probes were obtained from a previous study “
Estudo Monitora Corona”shown in
Table S1. Reactions were performed with 5 µl of extracted RNA (total RNA range of 14 to 25 ng) in a final volume of 25 µl using AgPath-ID™ One-Step RT-PCR Reagents (ThermoFisher Scientific, Massachusetts, USA) following manufacturer’s instructions. Quality controls included a positive control (SARS-CoV-2 clinical positive sample) and a negative control (DNAse/RNAse free water). The RT-qPCR was carried out for 40 cycles on ViiA 7 Real-Time PCR System (ThermoFisher Scientific, Massachusetts, USA) based on the following program: 45°C for 10 min; 95°C for 10 min; and 40 cycles of 95°C for 15 s and 60°C for 45 s.
4.4. SARS-CoV-2 S Gene Targeted Amplification
Nested-PCR was performed to amplify four selected Spike regions. The selected regions for amplification cover mutation and indels present in major variants of concern that circulated in 2021. Primers for SARS-CoV-2 S gene were designed using the S gene from Wuhan reference genome (GenBank: NC_045512.2) using Geneious Prime Software v. 2022.2 (
Figure 1). Primers sequences are shown in
Table 1.
First-strand cDNA was synthesized using SuperScript III Reverse Transcriptase (ThermoFisher Scientific, Massachusetts, USA) with random primer and using 5.0μl of RNA (total RNA range of 14 to 25 ng). First PCR reaction was performed using 4.0μl of cDNA in a final volume of 25 μl, using 2mM MgCl
2, 0.2mM dNTP, 0.2µM of primers, 5% DMSO and 1.25 U DNA Polymerase (Go Taq Flexi DNA Polymerase, Promega, Wisconsin, USA). The PCR conditions were as follows: 95 °C for 2 min; 15 cycles of 95 °C for 30 s, 50 °C for 30 s and 72 °C for 30 s; 20 cycles of 95 °C for 30 s, 53 °C for 30 s and 72 °C for 30 s; and final extension 72 °C for 5 min. Nested-PCR was performed using 2μl of first PCR product in a final volume of 25 μl, using 2mM MgCl
2, 0.2mM dNTP, 0.2µM of primers and 1.25 U DNA Polymerase (Go Taq Flexi DNA Polymerase, Promega, Wisconsin, USA). The nested-PCR conditions were as follows: 95 °C for 2 min; 35 cycles of 95 °C for 30 s, 53 °C for 30 s and 72 °C for 30 s; and final extension 72 °C for 5 min. DNAse/RNAse free water was used as the negative control. The amplified PCR product quality was visualized in 4150 TapeStation System (Agilent Technology, California, USA) using the Agilent High Sensitivity D1000 ScreenTape Kit following manufacturer’s instructions.
Table 3
4.5. Next Generation Sequencing (NGS)
Nested-PCR amplicons were purified using Agencourt AMPure XP Reagent (Beckman Coulter, California, USA) and quantified by QubitTM dsDNA BR Assay (Invitrogen, Massachusetts, USA). A total of 25 ng of the purified amplicons corresponding to each of the four S gene regions of the same sample were combined to a final concentration of 100 ng. NGS was achieved using the Ion Plus Fragment Library Kit (ThermoFisher Scientific, Massachusetts, USA), following manufacturing instructions (MAN0006846). Quantification of the libraries was obtained using the Ion Library TaqMan™ Quantitation Kit (ThermoFisher Scientific, Massachusetts, USA). The libraries were pooled at a concentration of 40 pM, and run on the Ion Chef™ system (ThermoFisher Scientific, Massachusetts, USA) using Ion 510, 520 & 530 Kits (ThermoFisher Scientific, Massachusetts, USA) and run into a 530 chip in an Ion S5™ System genetic sequencer (ThermoFisher Scientific, Massachusetts, USA).
4.6. Data Analysis
The sequencing reads generated were mapped to a SARS-CoV-2 reference genome Wuhan (GenBank: MN908947) using the Ion Browser software included in the Torrent Suite 5.18.1. and visualized in Integrative Genomics Viewer (IGV Version 2.16.2) (Broad Institute, Cambridge, USA) (Robinson, J. et al., 2011). Reads were trimmed using BBDuk Adapter/Quality Trimming Version 38.84 (by Brian Bushnell) available in Geneious Prime Software v.2023.2. The trim parameter was minimum quality = 20; minimum length = 200 bp. Trimmed reads were mapped to a SARS-CoV-2 S gene reference genome (GenBank: NC_045512.2) and Single Nucleotide Polymorphisms (SNP
S) achieved using Geneious Prime Workflow “Map reads then find variations/SNPs''. The parameter setting was: Bowtie2 mapper v. 7.2.2 with a highest sensitivity local alignment type; minimum variant frequency = 0.1, find variants only inside CDS, standard analyze effect of variants on translations, assumed quality of bases without quality = 20 [
44]. Consensus sequences were aligned using MAFFT alignment v7.490 with Geneious Prime default [
45,
46]. The four amplicons sequenced were manually concatenated for each sample.
4.7. Phylogenetic Tree
A total of 80 SARS-CoV-2 nucleotide sequences from B.1.1.33, B.1.1.28, Alpha, Beta, Gamma, Delta and Omicron BA.1 variants were downloaded from Virus Variation Resource hosted by the National Center for Biotechnology Information [
25]. We used filters: Geographic Region: Brazil; Nucleotide Completeness: complete. Selected sequences are: NC_045512.2; ON583297.1; OQ524879.1; OQ524718.1; OQ525734.1; OQ523655.1; OQ524075.1; ON583169.1; OQ525077.1; ON583180.1; OQ524834.1; MZ685358.1; MW844743.1; MZ003360.1; MZ684316.1; MZ306477.1; MW914015.1; OK233737.1; MZ371149.1; MZ044626.1; MZ962700.1; OK193794.1; MZ271547.1; MZ083956.1; MZ363098.1; MZ170566.1; MZ318938.1; MZ140853.1; MZ512907.1; MZ013605.1; MZ398998.1; ON575924.1; ON577503.1; ON574900.1; ON576913.1 ; ON577316.1; MZ477753.1; OQ521807.1; ON577989.1; ON577402.1; MZ477856.1; MW495020.1; OR856798.1; MW495013.1; MW495006.1; MW495012.1; MW495015.1; OR856826.1; OR856949.1; OR856818.1; OR856802.1; OR856903.1; OL442150.1; MZ477858.1; OQ430691.1; OL442144.1; MZ419862.1; OQ430692.1; OQ430693.1; MT754277.1; OR856848.1; MZ169915.1; MZ169917.1; MZ169916.1; OL442129.1; OL442125.1; OL442126.1; OQ691309.1; OQ690308.1; OQ690410.1; OR856921.1; ON582624.1; ON583432.1; OM188319.1; ON582126.1; ON582426.1; ON575214.1; ON578185.1; ON581622.1; ON581169.1; ON575160.1.
Sequences were aligned using MAFFT alignment, followed by S gene extraction and realignment. Sequences were cut and concatenated to harbor only the four regions of Spike that correspond to our approach of small S amplicons and used to build a phylogenetic tree. Mutations above 55% frequency were contemplated for tree analyses. A modeltest was run in CLC Genomic Workbench v.24.0.1, and the HKY model was recommended. Phylogenetic tree was built in CLC Genomic Workbench v.24.0.1 with parameters as follow: Neighbor Joining construction method, HKY nucleotide substitution model, number of substitution rate categories equal 4, gamma distribution parameter equal 1, and 1000 replicates of bootstrap.
5. Conclusions
Nested-PCR followed by next-generation sequencing of selected small amplicons of the S gene improves SARS-CoV-2 variant detection in wastewater and allows monitoring of SARS-CoV-2 variant changes through time. Our approach allowed us to detect Omicron matched mutations nine months before they were described in the first clinical sample, suggesting the potential of wastewater surveillance to anticipate variant’s detection. Furthermore, wastewater samples reflect the distribution profile of SARS-CoV-2 variants found in clinical samples. Therefore, SARS-CoV-2 genome monitoring in wastewater contributes to our understanding of the virus dynamic circulation in the population, providing helpful data for the public health system.
Supplementary Materials
The following supporting information can be downloaded at the website of this paper posted on Preprints.org.
Author Contributions
Conceptualization, S.M.C, M.C.d.C.S, L.J.d.C and R.S; Methodology, S.M.C, M.C.d.C.S, L.J.d.C and R.S; Validation, S.M.C, M.C.d.C.S, L.J.d.C and R.S; Formal Analysis, S.M.C, M.C.d.C.S and R.S; Investigation, S.M.C, M.C.d.C.S, L.J.d.C and R.S; Resources, S.M.C, M.C.d.C.S, L.J.d.C and R.S; Data curation, S.M.C, M.C.d.C.S, L.J.d.C and R.S; Writing - Original Draft Preparation, S.M.C, M.C.d.C.S, L.J.d.C and R.S; Writing - Review & Editing, S.M.C, M.C.d.C.S, L.J.d.C and R.S; Visualization, S.M.C, M.C.d.C.S, L.J.d.C and R.S; Supervision, L.J.d.C and R.S; Project Administration, L.J.d.C and R.S; Funding Acquisition, L.J.d.C and R.S.
Funding
This work was supported by Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES), 88887.647891/2021-00; CAPES, 88887.511767/2020-00; Fundação de Amparo à Pesquisa do Estado do Rio de Janeiro (FAPERJ), SEI-260003/012994/2021 Ref.:211.116/2021; FAPERJ, E-26/200.999/2022; Conselho Nacional de Conselho Científico e Tecnológico (CNPQ), 303829/2019-2.
Data Availability Statement
DNA sequences generated during this study are available in the NCBI database (
https://www.ncbi.nlm.nih.gov/nuccore/) under the following accession IDs: PP579733, PP579734, PP579735, PP579736, PP579737, PP579738, PP579739, PP579740.
Acknowledgements
We thank the groups from Estudo Monitora Corona for collaborating to produce this work. We thank Claudio Nunes Pereira for technical support and Polyana Silva Pereira from Plataforma de Sequenciamento de DNA (PSEQDNA-UFRJ) for DNA sequencing analyses. We thank Marcia Triunfol at Publicase International for her comments and for editing this manuscript. We acknowledge the anonymous researchers, whose constructive comments and suggestions improved the quality of the paper.
Conflicts of Interest
The authors declare no conflict of interest.
References
- WHO WHO COVID-19 Dashboard Available online: https://data.who.int/dashboards/covid19/cases?n=c. acessed on March 6, 2025.
- Mistry, P.; Barmania, F.; Mellet, J.; Peta, K.; Strydom, A.; Viljoen, I.M.; James, W.; Gordon, S.; Pepper, M.S. SARS-CoV-2 Variants, Vaccines, and Host Immunity. Front. Immunol. 2022, 12, 809244. [Google Scholar] [CrossRef] [PubMed]
- Organization, W.W.H. Updated Working Definitions and Primary Actions for SARSCoV2 Variants. (n.d.-g) Available online: https://www.who.int/publications/m/item/historical-working-definitions-and-primary-actions-for-sars-cov-2-variants.
- WHO; Organization, W.H. Updated Working Definitions and Primary Actions for SARSCoV2 Variants. (n.d.-d). Available online: https://www.who.int/publications/m/item/updated-working-definitions-and-primary-actions-for--sars-cov-2-variants. (accessed on 6 February 2024).
- Voloch, C.M.; Francisco, R. da S.; Almeida, L.G.P. de; Cardoso, C.C.; Brustolini, O.J.; Gerber, A.L.; Guimarães, A.P. de C.; Mariani, D.; Costa, R.M. da; Ferreira, O.C.; et al. Genomic Characterization of a Novel SARS-CoV-2 Lineage from Rio de Janeiro, Brazil. J Virol 2021, 95, e00119–21. [Google Scholar] [CrossRef] [PubMed]
- Rambaut, A.; Loman, N.; Pybus, O.; Barclay, W.; Barrett, J.; Carabelli, A.; Connor, T.; Peacock, T.; Robertson, D.L.; Volz, E.; et al. Preliminary Genomic Characterisation of an Emergent SARS-CoV-2 Lineage in the UK Defined by a Novel Set of Spike Mutations, 2020.
- Tegally, H.; Wilkinson, E.; Giovanetti, M.; Iranzadeh, A.; Fonseca, V.; Giandhari, J.; Doolabh, D.; Pillay, S.; San, E.J.; Msomi, N.; et al. Detection of a SARS-CoV-2 Variant of Concern in South Africa. Nature 2021, 592, 438–443. [Google Scholar] [CrossRef] [PubMed]
- Fujino, T.; Nomoto, H.; Kutsuna, S.; Ujiie, M.; Suzuki, T.; Sato, R.; Fujimoto, T.; Kuroda, M.; Wakita, T.; Ohmagari, N. Novel SARS-CoV-2 Variant in Travelers from Brazil to Japan - Volume 27, Number 4—April 2021 - Emerging Infectious Diseases Journal - CDC. Emerg. Infect. Dis. 2021, 27, 1243–1245. [Google Scholar] [CrossRef]
- Cherian, S.; Potdar, V.; Jadhav, S.; Yadav, P.; Gupta, N.; Das, M.; Rakshit, P.; Singh, S.; Abraham, P.; Panda, S.; et al. SARS-CoV-2 Spike Mutations, L452R, T478K, E484Q and P681R, in the Second Wave of COVID-19 in Maharashtra, India. Microorganisms 2021, 9, 1542. [Google Scholar] [CrossRef]
- Wang, L.; Cheng, G. Sequence Analysis of the Emerging SARS-CoV-2 Variant Omicron in South Africa. J. Méd. Virol. 2022, 94, 1728–1733. [Google Scholar] [CrossRef]
- Parums, D.V. Editorial: A Rapid Global Increase in COVID-19 Is Due to the Emergence of the EG.5 (Eris) Subvariant of Omicron SARS-CoV-2. Méd. Sci. Monit. : Int. Méd. J. Exp. Clin. Res. 2023, 29, e942244–1. [Google Scholar] [CrossRef]
- Hoffmann, M.; Kleine-Weber, H.; Pöhlmann, S. A Multibasic Cleavage Site in the Spike Protein of SARS-CoV-2 Is Essential for Infection of Human Lung Cells. Mol. Cell 2020, 78, 779–784.e5. [Google Scholar] [CrossRef]
- Huang, Y.; Yang, C.; Xu, X.; Xu, W.; Liu, S. Structural and Functional Properties of SARS-CoV-2 Spike Protein: Potential Antivirus Drug Development for COVID-19. Acta Pharmacol. Sin. 2020, 41, 1141–1149. [Google Scholar] [CrossRef]
- Arora, P.; Sidarovich, A.; Graichen, L.; Hörnich, B.; Hahn, A.; Hoffmann, M.; Pöhlmann, S. Functional Analysis of Polymorphisms at the S1/S2 Site of SARS-CoV-2 Spike Protein. PLoS ONE 2022, 17, e0265453. [Google Scholar] [CrossRef]
- Liao, Y.-C.; Chen, F.-J.; Chuang, M.-C.; Wu, H.-C.; Ji, W.-C.; Yu, G.-Y.; Huang, T.-S. High-Integrity Sequencing of Spike Gene for SARS-CoV-2 Variant Determination. Int. J. Mol. Sci. 2022, 23, 3257. [Google Scholar] [CrossRef] [PubMed]
- Salles, T.S.; Cavalcanti, A.C.; Costa, F.B. da; Dias, V.Z.; Souza, L.M. de; Meneses, M.D.F. de; Silva, J.A.S. da; Amaral, C.D.; Felix, J.R.; Pereira, D.A.; et al. Genomic Surveillance of SARS-CoV-2 Spike Gene by Sanger Sequencing. PLoS ONE 2022, 17, e0262170. [Google Scholar] [CrossRef]
- Agrawal, S.; Orschler, L.; Schubert, S.; Zachmann, K.; Heijnen, L.; Tavazzi, S.; Gawlik, B.M.; Graaf, M. de; Medema, G.; Lackner, S. Prevalence and Circulation Patterns of SARS-CoV-2 Variants in European Sewage Mirror Clinical Data of 54 European Cities. Water Res. 2022, 214, 118162. [Google Scholar] [CrossRef] [PubMed]
- Wang, W.; Xu, Y.; Gao, R.; Lu, R.; Han, K.; Wu, G.; Tan, W. Detection of SARS-CoV-2 in Different Types of Clinical Specimens. JAMA 2020, 323, 1843–1844. [Google Scholar] [CrossRef]
- Ahmed, W.; Angel, N.; Edson, J.; Bibby, K.; Bivins, A.; O’Brien, J.W.; Choi, P.M.; Kitajima, M.; Simpson, S.L.; Li, J.; et al. First Confirmed Detection of SARS-CoV-2 in Untreated Wastewater in Australia: A Proof of Concept for the Wastewater Surveillance of COVID-19 in the Community. Sci. Total Environ. 2020, 728, 138764. [Google Scholar] [CrossRef]
- Crits-Christoph, A.; Kantor, R.S.; Olm, M.R.; Whitney, O.N.; Al-Shayeb, B.; Lou, Y.C.; Flamholz, A.; Kennedy, L.C.; Greenwald, H.; Hinkle, A.; et al. Genome Sequencing of Sewage Detects Regionally Prevalent SARS-CoV-2 Variants. mBio 2021, 12, 10.1128–mbio.02703. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, W.; Bertsch, P.M.; Bivins, A.; Bibby, K.; Farkas, K.; Gathercole, A.; Haramoto, E.; Gyawali, P.; Korajkic, A.; McMinn, B.R.; et al. Comparison of Virus Concentration Methods for the RT-QPCR-Based Recovery of Murine Hepatitis Virus, a Surrogate for SARS-CoV-2 from Untreated Wastewater. Sci. Total Environ. 2020, 739, 139960. [Google Scholar] [CrossRef]
- Sims, N.; Kasprzyk-Hordern, B. Future Perspectives of Wastewater-Based Epidemiology: Monitoring Infectious Disease Spread and Resistance to the Community Level. Environ. Int. 2020, 139, 105689. [Google Scholar] [CrossRef]
- Shrestha, L.B.; Tedla, N.; Bull, R.A. Broadly-Neutralizing Antibodies Against Emerging SARS-CoV-2 Variants. Front. Immunol. 2021, 12, 752003. [Google Scholar] [CrossRef]
- Mercier, P.L.; Hulo, C.; Masson, P.; Castro, E. de SARS-CoV-2 Variants ~ ViralZone Available online: https://viralzone.expasy.org/9556.
- Hatcher, E.L.; Zhdanov, S.A.; Bao, Y.; Blinkova, O.; Nawrocki, E.P.; Ostapchuck, Y.; Schäffer, A.A.; Brister, J.R. Virus Variation Resource – Improved Response to Emergent Viral Outbreaks. Nucleic Acids Res. 2017, 45, D482–D490. [Google Scholar] [CrossRef]
- Fiocruz. Dashboard-Pt. (n.d.). Available online: https://www.genomahcov.fiocruz.br/dashboard-pt/. (accessed on 13 December 2023).
- Rosa, G.L.; Mancini, P.; Ferraro, G.B.; Veneri, C.; Iaconelli, M.; Lucentini, L.; Bonadonna, L.; Brusaferro, S.; Brandtner, D.; Fasanella, A.; et al. Rapid Screening for SARS-CoV-2 Variants of Concern in Clinical and Environmental Samples Using Nested RT-PCR Assays Targeting Key Mutations of the Spike Protein. Water Res. 2021, 197, 117104. [Google Scholar] [CrossRef] [PubMed]
- Carcereny, A.; Garcia-Pedemonte, D.; Martínez-Velázquez, A.; Quer, J.; Garcia-Cehic, D.; Gregori, J.; Antón, A.; Andrés, C.; Pumarola, T.; Chacón-Villanueva, C.; et al. Dynamics of SARS-CoV-2 Alpha (B.1.1.7) Variant Spread: The Wastewater Surveillance Approach. Environ. Res. 2022, 208, 112720. [Google Scholar] [CrossRef]
- Knierim, E.; Lucke, B.; Schwarz, J.M.; Schuelke, M.; Seelow, D. Systematic Comparison of Three Methods for Fragmentation of Long-Range PCR Products for Next Generation Sequencing. PLoS ONE 2011, 6, e28240. [Google Scholar] [CrossRef] [PubMed]
- Costello, M.; Pugh, T.J.; Fennell, T.J.; Stewart, C.; Lichtenstein, L.; Meldrim, J.C.; Fostel, J.L.; Friedrich, D.C.; Perrin, D.; Dionne, D.; et al. Discovery and Characterization of Artifactual Mutations in Deep Coverage Targeted Capture Sequencing Data Due to Oxidative DNA Damage during Sample Preparation. Nucleic Acids Res. 2013, 41, e67–e67. [Google Scholar] [CrossRef] [PubMed]
- Wilton, T.; Bujaki, E.; Klapsa, D.; Majumdar, M.; Zambon, M.; Fritzsche, M.; Mate, R.; Martin, J. Rapid Increase of SARS-CoV-2 Variant B.1.1.7 Detected in Sewage Samples from England between October 2020 and January 2021. mSystems 2021, 6, 10.1128–msystems.00353. [Google Scholar] [CrossRef]
- Karthikeyan, S.; Levy, J.I.; Hoff, P.D.; Humphrey, G.; Birmingham, A.; Jepsen, K.; Farmer, S.; Tubb, H.M.; Valles, T.; Tribelhorn, C.E.; et al. Wastewater Sequencing Reveals Early Cryptic SARS-CoV-2 Variant Transmission. Nature 2022, 609, 101–108. [Google Scholar] [CrossRef]
- Barnes, K.G.; Levy, J.I.; Gauld, J.; Rigby, J.; Kanjerwa, O.; Uzzell, C.B.; Chilupsya, C.; Anscombe, C.; Tomkins-Tinch, C.; Mbeti, O.; et al. Utilizing River and Wastewater as a SARS-CoV-2 Surveillance Tool in Settings with Limited Formal Sewage Systems. Nat. Commun. 2023, 14, 7883. [Google Scholar] [CrossRef]
- Iwamoto, R.; Yamaguchi, K.; Katayama, K.; Ando, H.; Setsukinai, K.; Kobayashi, H.; Okabe, S.; Imoto, S.; Kitajima, M. Identification of SARS-CoV-2 Variants in Wastewater Using Targeted Amplicon Sequencing during a Low COVID-19 Prevalence Period in Japan. Sci. Total Environ. 2023, 887, 163706. [Google Scholar] [CrossRef]
- Shempela, D.M.; Muleya, W.; Mudenda, S.; Daka, V.; Sikalima, J.; Kamayani, M.; Sandala, D.; Chipango, C.; Muzala, K.; Musonda, K.; et al. Wastewater Surveillance of SARS-CoV-2 in Zambia: An Early Warning Tool. Int. J. Mol. Sci. 2024, 25, 8839. [Google Scholar] [CrossRef]
- Mautner, L.; Hoyos, M.; Dangel, A.; Berger, C.; Ehrhardt, A.; Baiker, A. Replication Kinetics and Infectivity of SARS-CoV-2 Variants of Concern in Common Cell Culture Models. Virol. J. 2022, 19, 76. [Google Scholar] [CrossRef]
- Organization., P. Organization., P.| P.A.H. Brazil Will Receive the First Vaccines against COVID-19 through the COVAX Mechanism. (n.d.). Available online: https://www.paho.org/en/news/21-3-2021-brazil-will-receive-first-vaccines-against-covid-19-through-covax-mechanism.
- Andrews, N.; Stowe, J.; Kirsebom, F.; Toffa, S.; Rickeard, T.; Gallagher, E.; Gower, C.; Kall, M.; Groves, N.; O’Connell, A.-M.; et al. Covid-19 Vaccine Effectiveness against the Omicron (B.1.1.529) Variant. N. Engl. J. Med. 2022, 386, 1532–1546. [Google Scholar] [CrossRef] [PubMed]
- Zeng, B.; Gao, L.; Zhou, Q.; Yu, K.; Sun, F. Effectiveness of COVID-19 Vaccines against SARS-CoV-2 Variants of Concern: A Systematic Review and Meta-Analysis. BMC Med. 2022, 20, 200. [Google Scholar] [CrossRef]
- Giovanetti, M.; Slavov, S.N.; Fonseca, V.; Wilkinson, E.; Tegally, H.; Patané, J.S.L.; Viala, V.L.; San, E.J.; Rodrigues, E.S.; Santos, E.V.; et al. Genomic Epidemiology of the SARS-CoV-2 Epidemic in Brazil. Nat. Microbiol. 2022, 7, 1490–1500. [Google Scholar] [CrossRef] [PubMed]
- Tracking SARS-CoV-2 Variants. (2023b, March 16 Available online:. Available online: https://www.who.int/activities/tracking-SARS-CoV-2-variants (accessed on 12 March 2024).
- Pastorino, B.; Touret, F.; Gilles, M.; Luciani, L.; Lamballerie, X. de; Charrel, R.N. Evaluation of Chemical Protocols for Inactivating SARS-CoV-2 Infectious Samples. Viruses 2020, 12, 624. [Google Scholar] [CrossRef] [PubMed]
- Batéjat, C.; Grassin, Q.; Manuguerra, J.-C.; Leclercq, I. Heat Inactivation of the Severe Acute Respiratory Syndrome Coronavirus 2. J. Biosaf. Biosecurity 2021, 3, 1–3. [Google Scholar] [CrossRef]
- Langmead, B.; Salzberg, S.L. Fast Gapped-Read Alignment with Bowtie 2. Nat. Methods 2012, 9, 357–359. [Google Scholar] [CrossRef] [PubMed]
- Katoh, K.; Standley, D.M. MAFFT Multiple Sequence Alignment Software Version 7: Improvements in Performance and Usability. Mol. Biol. Evol. 2013, 30, 772–780. [Google Scholar] [CrossRef]
- Katoh, K.; Misawa, K.; Kuma, K.; Miyata, T. MAFFT: A Novel Method for Rapid Multiple Sequence Alignment Based on Fast Fourier Transform. Nucleic Acids Res. 2002, 30, 3059–3066. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).