1. Introduction
The clinical and laboratory landscape of COVID-19 has shifted significantly over the course of the pandemic [
1]. Mutations in the SARS-CoV-2 virus have led to the emergence of various antigenic variants, including the EG.5 lineage (Eris), the descendant of the XBB.1.9.2 lineage, as well as XBB.1.16 (Arcturus), XBB.1.5 (Kraken), and other variants of the Omicron coronavirus [
2]. The new variant of the Coronavirus, B.1.1.529, named ’Omicron’, was discovered on November 24, 2021, in South Africa, from a patient’s specimen sample that was collected on November 9, 2021 [
3]. Shortly after its identification, Omicron was detected in several other countries, marking its rapid global spread. In Russia, the Omicron variant began to spread rapidly since December 2021, and it currently completely dominates the territory of Russia (100% of all samples studied) [
5].
With the advent of Omicron, the speed of spread of coronavirus has increased and the incubation period has decreased [
6]. Omicron contains more than 30 mutations in its spike protein, which is significantly higher than in previous variants [
7]. Many of these mutations help Omicron evade the immune response generated by previous infections and vaccinations [
8].
The main danger of this new subtype of the virus is that it can evade the body’s immune system [
9,
10]. Before Omicron, natural immunity provided robust and lasting protection against reinfection [
11]. However, in the Omicron period, protective immunity was only observed among recently recovered people and declined rapidly over the course of a year. This emphasizes the need for continuous monitoring of the virus and its mutations, as well as regular updates to SARS-CoV-2 vaccines to restore immunity and combat ongoing viral immune evasion [
11].
Despite the detected decrease in neutralizing antibody responses to Omicron, vaccines continue to provide significant protection against severe illness [
12]. Epidemiological studies have shown that Omicron infections may result in a variety of symptoms, often associated with mild forms of the illness, especially in vaccinated individuals [
10,
13]. For all ages, the risk of COVID-19-related death, regardless of the number of comorbid conditions, is lower with Omicron than with Delta [
14].
Although the new strains have a milder course of the disease, they can still cause serious complications [
15]. Omicron has demonstrated the highest transmission rate among other variants of SARS-CoV-2 [
4], leading to significant increases in cases, especially among unvaccinated people or those with pre-existing health conditions [
16].
While the S protein of Omicron undergoes substantial changes, promoting transmission and immune evasion, the changes in the N-protein are more modest, primarily relevant to diagnostic considerations and antibody tests [
17]. The N-protein is targeted by the host’s immune response, regulating innate immune responses such as type I interferon (IFN-I) signaling and cytokine production [
18]. Antibodies produced against the N-proteins can be part of an adaptive immune response [
19]. Like other regions of viral genomes, the N-gene can accumulate mutations over time, affecting protein structure and function. These changes can lead to alterations in viral fitness and virulence, as well as the ability to avoid the immune response [
20]. Some SARS-CoV variants may develop mutations in their N-genes that allow them to evade detection by the immune system and impact vaccine effectiveness and natural immunity [
21]. Studying evolutionary changes in SARS-CoV not only in S proteins but also N proteins provide a more complete understanding of its biology, evolution, and interaction with the human immune system.
Since the beginning of SARS-CoV-2 spread, there have been several reports of co-infection with influenza and coronavirus infections [
22]. Since the beginning of the spread of the SARS-CoV-2 virus, there have been quite a few reports of coinfection with influenza viruses and coronavirus infection [
13,
14,
15,
16,
17,
18,
19,
20,
21,
22,
23,
24,
25]. During quarantine and due to the widespread use of personal protective equipment, influenza virus circulation has significantly decreased by 2022. Even influenza B/Yamagata virus disappeared from circulation for the first time in 40 years [
26]. Under such conditions, population immunity against influenza decreases, and the likelihood of emergence of new influenza virus antigenic variants increases.
The purpose of this study is to compare clinical features, inflammatory markers, and adaptive immune parameters in patients with COVID-19 who were hospitalized during first wave of pandemic and at end of 2021 (beginning of ‘Omicron’ era). One of objectives was to evaluate contribution of co-infections with influenza to severity of COVID-19 during these two periods.
2. Materials and Methods
2.1. Ethics Statement
All study participants signed a written informed consent. The study was approved by the Local Ethics Committee of the Federal State Budgetary Scientific Institution ‘IEM’ (protocol 1/23 dated 04/20/2023).
2.2. Study Participants and Samples
In this retrospective cohort study a total of 45 sera from patients with acute COVID-19 obtained at the beginning of the SARS-Cov-2 outbreak (including 28 paired samples), and 53 sera from patients hospitalized at the end of 2021 (including 14 paired samples), were studied. The samples were provided by the Vsevolozhsk Clinical Interdistrict Hospital, Leningrad Region, Russian Federation. The cohort was divided into 3 groups according to the severity of the disease at hospital admission. The severity was assessed according to the Interim recommendations for the prevention, diagnosis, and treatment of coronavirus disease 2019 (COVID-19), version 8. Mild disease is characterized by body temperature <38°C, coughing, weakness, and sore throat without criteria for moderate or severe disease. Moderate disease is characterized by body temperature >38°C, respiratory rate >22/min, dyspnea on exertion (shortness of breath), radiographic changes typical of viral infection (minimal or moderate lesion volume), oxygen saturation <95%, serum C-reactive protein (CRP) >10 mg/l. Severe disease is characterized by respiratory rate >30/min, oxygen saturation <93%, unstable hemodynamics (systolic blood pressure less than 90 mm Hg or diastolic blood pressure below 60 mm Hg, diuresis below 20ml/hour), lung changes on radiograph typical of viral infection (significant or subtotal lesion volume, >75%), arterial lactate >2 mmol/l. Extremely serious disease includes acute respiratory distress syndrome (ARDS). Nasopharyngeal and pharyngeal swabs were tested for real-time PCR upon hospital admission.
2.3. Molecular Genetic Analysis
The nucleotide sequence analysis was performed in the Ugene program. Phylogenetic trees were constructed using the MEGA11 statistical method Maximum likelihood [
27]. Alignment was performed according to the reference genome of Wuhan-Hu-1 (NC_045512.2). The following sequences of the full-length N protein of the SARS-CoV-2 virus were used: BS 016103.1, ON 442223.1, OK 501819.1, PQ 169822.1, OR 275853.1, OR 818056.1, MZ 140764.1, OR 729868.1, PQ 281369.1, PQ 370471.1, OR 457591.1, BS 014763.1, PQ 389522.1, OQ 852551.1, OQ 331796.1, PP215584.1, PQ102435.1, OR958502.1, PQ 515554.1, PP 103560.1, OQ 050741.1, PP 604035.1, OM 247072.1, OP 855515.1, OK 194572.1, LC 573289.2, PQ 437118.1, PQ 210560.1, PQ395243.1, PQ047794.1, PQ508588.1, PQ358595.1, PQ481382.1.
Primers for N-gene study by high-resolution melting curve analysis (HRM analysis) and sequencing were designed using the Primer3Plus online server (
Table 1).
Primers were synthesized by Alcor-Bio (St. Petersburg, Russia). We performed a molecular genetic analysis of SARS-CoV-2 RNA from two nasopharyngeal and pharyngeal swabs from patients with acute COVID -19, obtained in July 2021 (swab 1) and November 2021 (swab 2). The reference RNA for the Wuhan variant of the SARS-CoV-2 virus, kindly provided by the Institute of Influenza, was used as the control sample.
Reverse transcription PCR was performed using Moloney Murine Leukemia Virus Reverse Transcriptase (M-MulV RT), 200,000 units/ml; RNase inhibitor, 40 units/µl; 10X buffer; deoxyribonucleoside triphosphates, SsoFast EvaGreen mixtures on a CF X96 (Biorad, Hercules, USA) device. Melting curves were analyzed using the Precision Melt analysis software as described previously [
28].
2.4. Laboratory Data
Serum C-reactive protein (CRP) and fibrinogen concentrations were determined by turbodimetric method using BioSystem reagents (BioSystems, Barcelona, Spain). Interleukin-6 (IL-6), tumor necrosis factor alpha (TNF-α) or interferon 1 alpha (IFN-α) were determined using ELISAs (Vector-best, Novosibirsk, Russia) according to the manufacturer’s instructions. Serum complement C3 levels were measured using an ELISA kit (Cloud-Clone Corp., Wuhan, China) according to manufacturer’ instructions. All blood samples were tested without heating. The neutrophil/lymphocyte ratio (NLR) was calculated based on clinical data from blood tests using the formula for absolute neutrophils/absolute lymphocytes.
2.5. Hemagglutination Inhibition Test (HI)
To determine the level of HI antibodies to influenza viruses in the blood samples studied, the following influenza viruses obtained from the Department of Virology of the Institute of Experimental Medicine were used: A/New York/61/2015(H1N1)pdm09, A/Hong Kong/4801/2014 (H3N2), B/Colorado/06/2017 (B/Victoria/2/87 lineage) (2020) and A/Guangdong-Maonan/SWL1536/2019(H1N1)pdm09, B/Austria/06/2017 (B/Victoria/2/87 lineage) (2021). Blood sera were pretreated with an enzyme destroying enzyme, RDE (Denka Seiken, Tokyo, Japan), as described previously [
29]. RDE-treated and 1:10 diluted blood sera were titrated in short rows on a 96-well U-bottomed immunoassay plate (’Medpolymer’, St Petersburg, Russia) to obtain a series of 2-fold dilutions (in 25 μl of PBS): 1:10, 1:20, 1:40, and so on. Then, standard doses of virus (8 agglutinating units, AU) in a volume of 25 μl was added to each well. After 30 minutes at room temperature, 50 μl of 0.75% suspension of human red blood cells (RBCs) of group I(0) were added and kept for another 40 minutes under similar conditions for RBC sedimentation. The serum titer was determined as the reciprocal of the dilution of the last well in which no hemagglutination occurred. A fourfold or greater increase in the level of HI antibodies was considered reliable seroconversion.
2.6. Statistical Analysis
Statistical data processing was carried out using the Prism 8 software package (GraphPad software, San Diego, USA). Medians (Me) and lower and upper quartiles (Q1; Q3) were calculated and used to present the antibody response and blood test levels. In cases with normal distribution of the studied characteristics – M±σ, with M being the mean value and σ being the standard deviation. Comparisons between independent groups were made using non-parametric tests: for multiple comparisons, Friedman’s test (F-test (ANOVA) or Kruskall-Wallis (Kruskall-Wallis ANOVA), and Mann-Whitney (Mann-Whitney U test) to assess intragroup differences. A p value of <0.05 is considered statistically significant.
3. Results
3.1. Molecular Genetic Analysis of the N Protein Gene of SARS-CoV-2 Antigenic Variants
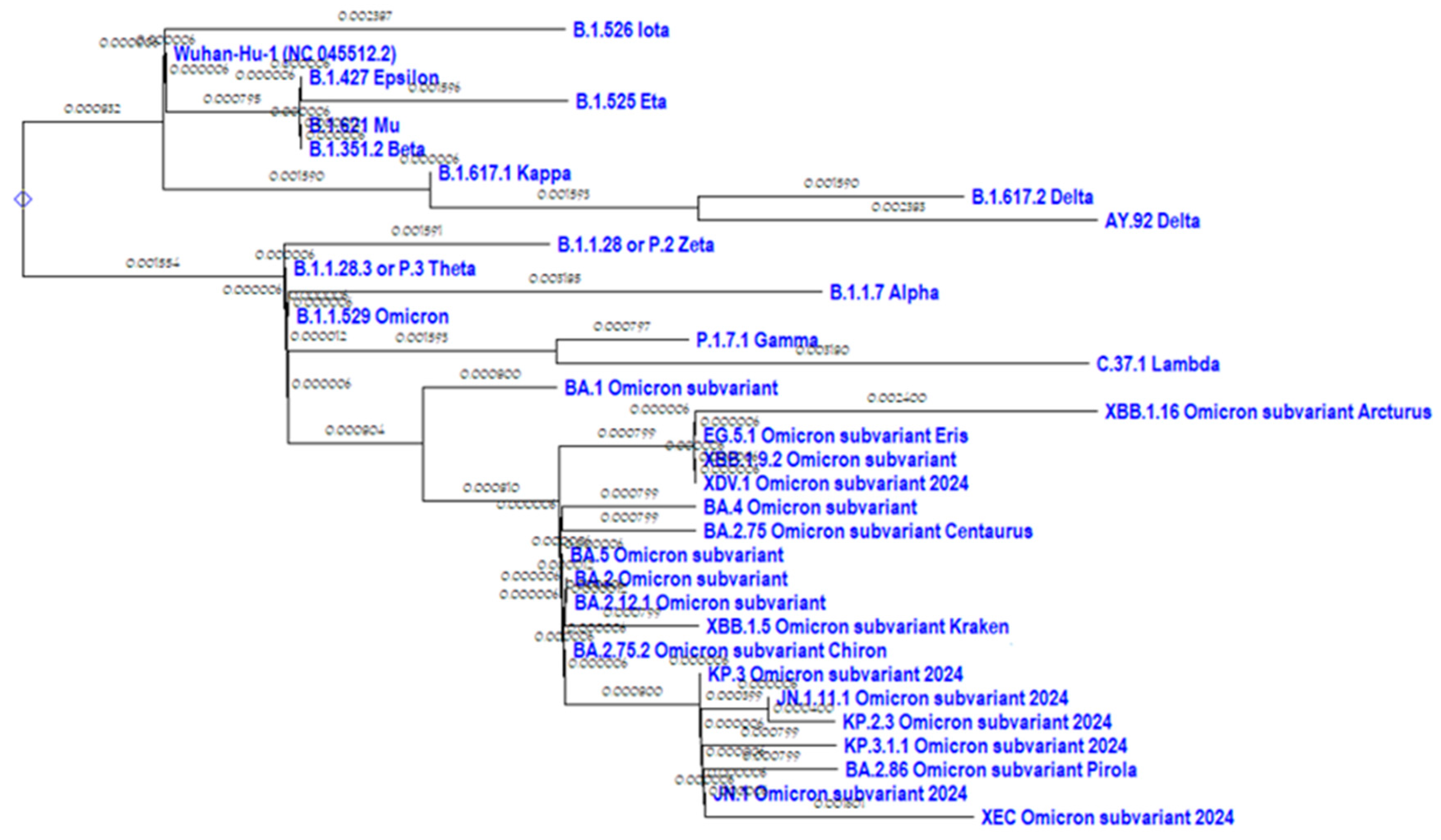
A phylogenetic tree of the N protein of the most representative SARS-CoV-2 variants was constructed in comparison with the original ’Wuhan’ variant (
Figure 1).
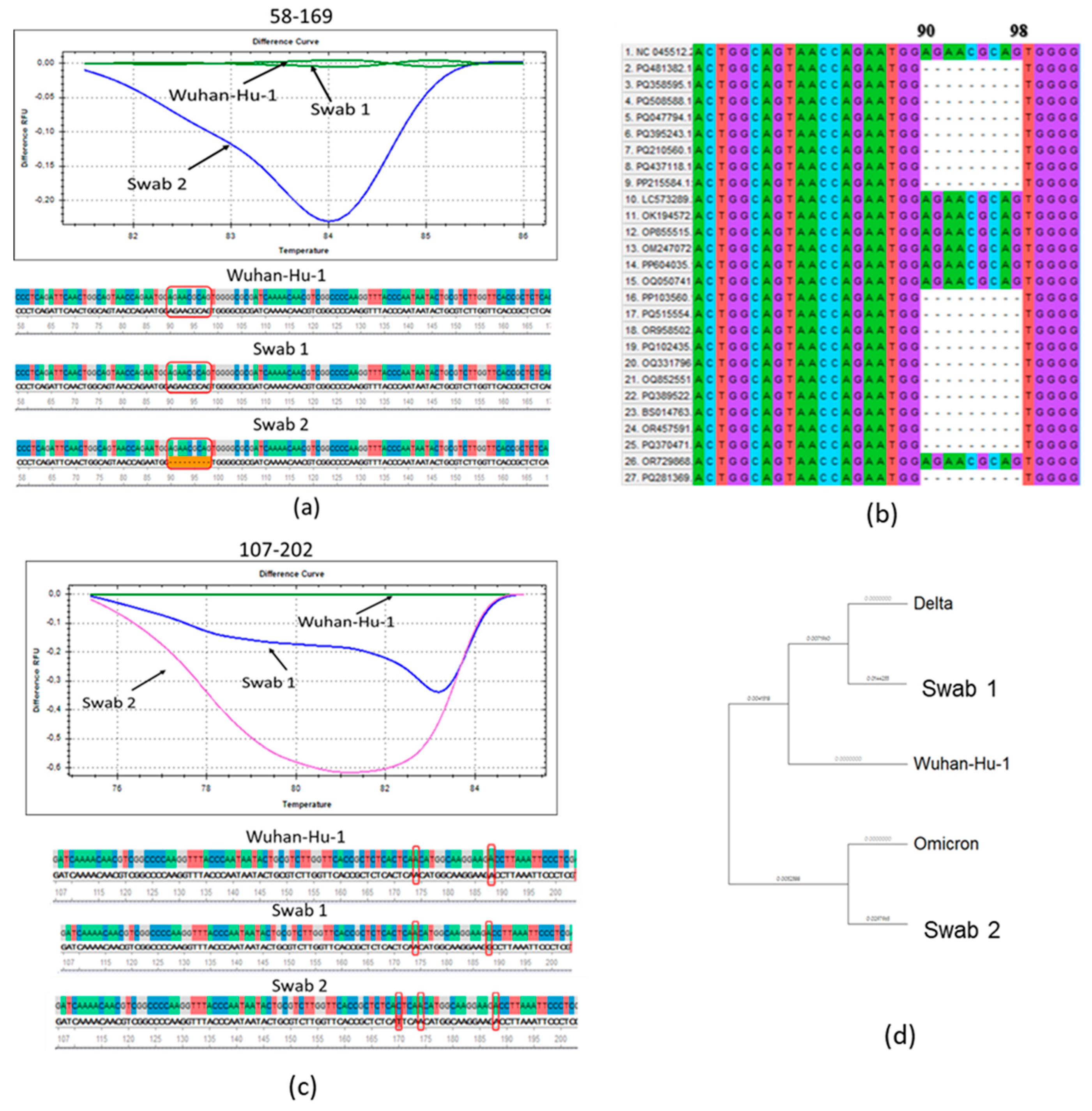
We performed a molecular genetic analysis on N protein RNA from two nasopharyngeal samples from patients with acute COVID -19, obtained in July 2021 (swab 1) and November 2021 (swab 2). The Wuhan reference RNA from the SARS-CoV-2 virus variant was used as a control. The graphs showed a clear difference in the melting patterns for the fragments of swabs 1 and 2 and the reference RNA (
Figure 1, A, B). In swab obtained in November 2021, a characteristic deletion of subvariants from the Omicron lineage was detected (
Figure 1, A). In a multiple alignment analysis of the major SARS-CoV-2 variants, we found that this deletion was also detected in other Omicron variants (
Figure 2B).
When analyzing the fragment flanked by primers 107-202, a single nucleotide substitution 188A→G was identified in swab 1, leading to an amino acid substitution D63G, characteristic of the Delta strain variants B.1.617.2 and AY.9.2 [
32] (
Figure 2, C). Wash 2, as shown by sequencing, has a previously undescribed missense mutation 170C→T in this region, leading to an amino acid substitution T57I (
Figure 2, C).
The multiple alignment of the nucleocapsid proteins of SARS-CoV-2 virus strains and nasopharyngeal swab sequences from patients showed the divergence of the Omicron strain during the evolution of the new coronavirus infection (
Figure 2, D). It was shown that both swabs differ from the original Wuhan variant, while swab 1 belongs to the same phylogenetic branch with the delta variant, and wash 2 is closer to the Omicron variant (
Figure 2, D). Thus, it was shown that by the end of 2021, the SARS-CoV-2 virus had acquired the characteristics of Omicron which had been officially registered in Russia since December 2021 [
2].
3.2. The Main Data on the Observed Patient Cohorts
Table 2 presents the main characteristics of acute COVID-19 patients examined in March 2020 and November 2021. The main differences between the two groups were as follows: the median time from the onset of symptoms to hospitalization was shorter for the second group (P=0.01); the proportion of positive PCR test results for SARS-CoV-2 was greater in the second group than in the first one; in 2021, almost 70 percent of subjects received a coronavirus vaccine, unlike the patients in the first cohort, which were examined prior to the introduction of anti-COVID vaccination. Accordingly, the proportions of individuals possessing serum IgG and IgM antibodies to the SARS-CoV-2 virus were statistically significantly higher in the second cohort of those examined. Additionally, viral RNA was not detected in the blood of patients from the second cohort, in contrast to the first cohort, and there were no fatalities in the second wave, whereas 24.1 percent of cases resulted in death in the first cohort (
Table 2). Аt the same time, there were no significant differences between the two groups in terms of such parameters as frequency of concomitant conditions and bacterial co-infections, as well as age and gender distribution of the studied groups (
Table 2).
There were no significant differences in the main parameters between men and women in the examined cohorts (
Table S1,
Table S2), and also there were almost no statistically significant differences between the parameters studied depending on the age of patients (
Table S3,
Table S4). The exception was that, in the second cohort, the levels of TNF-α and IFN-α were statistically significantly lower in patients younger than 65 compared to older ones (P=0.04 and P=0.001, respectively,
Table S4). There was no significant difference between vaccination statuses among patients examined in 2021 (
Table S5).
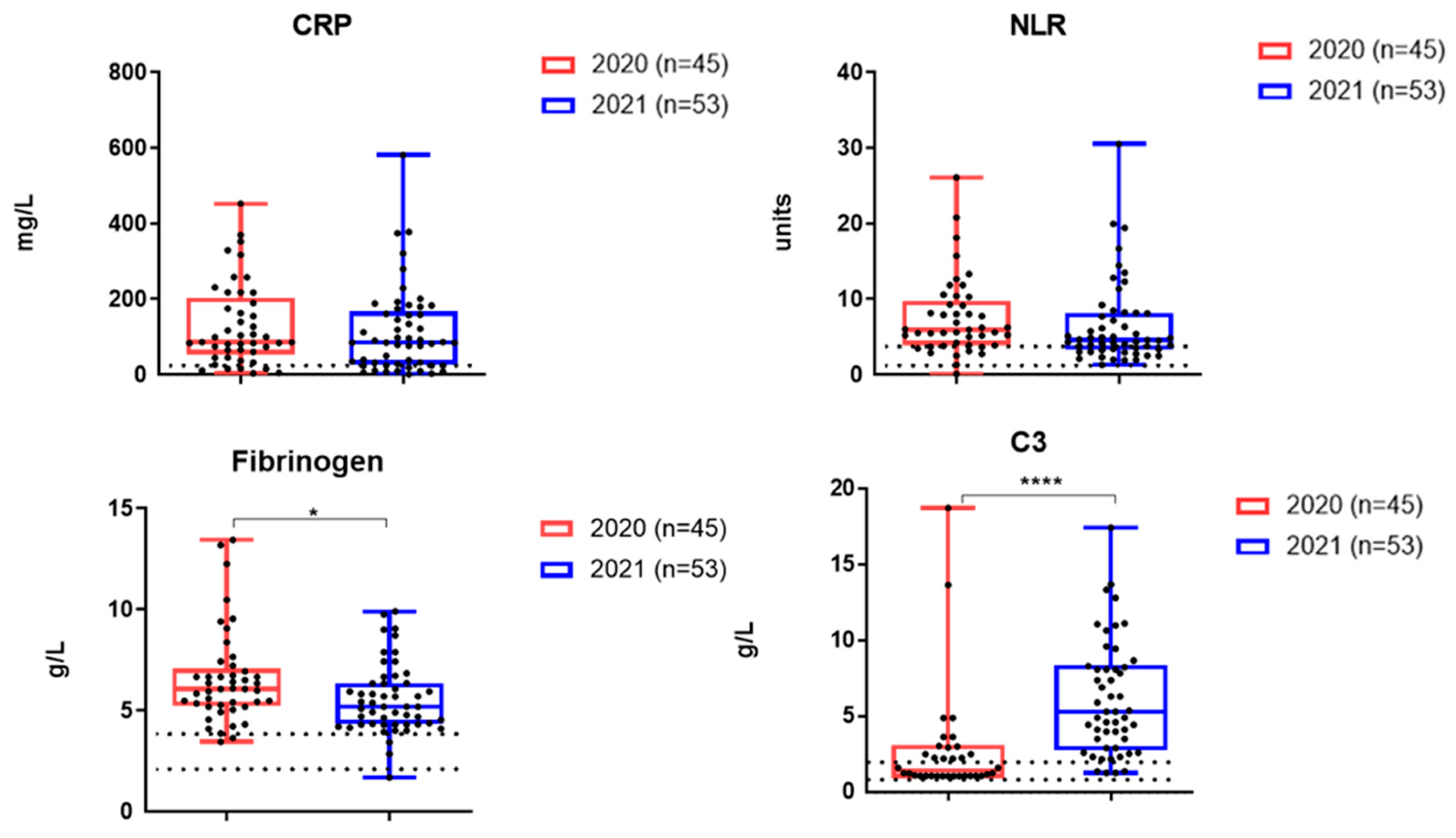
3.3. The Levels of Inflammatory Markers and Cytokines in the Serum Samples of Patients Examined
Figure 3 shows the results of a study on the content of inflammatory markers in hospitalized patients with acute COVID-19 during the two waves of the disease. The levels of CRP and NLR did not differ statistically significantly between the two cohorts examined. At the same time, a statistically significant decrease in fibrinogen was recorded in hospitalized COVID-19 patients during the second wave (
Figure 3).
The mean levels of complement C3 were higher in the second cohort (
Figure 3).
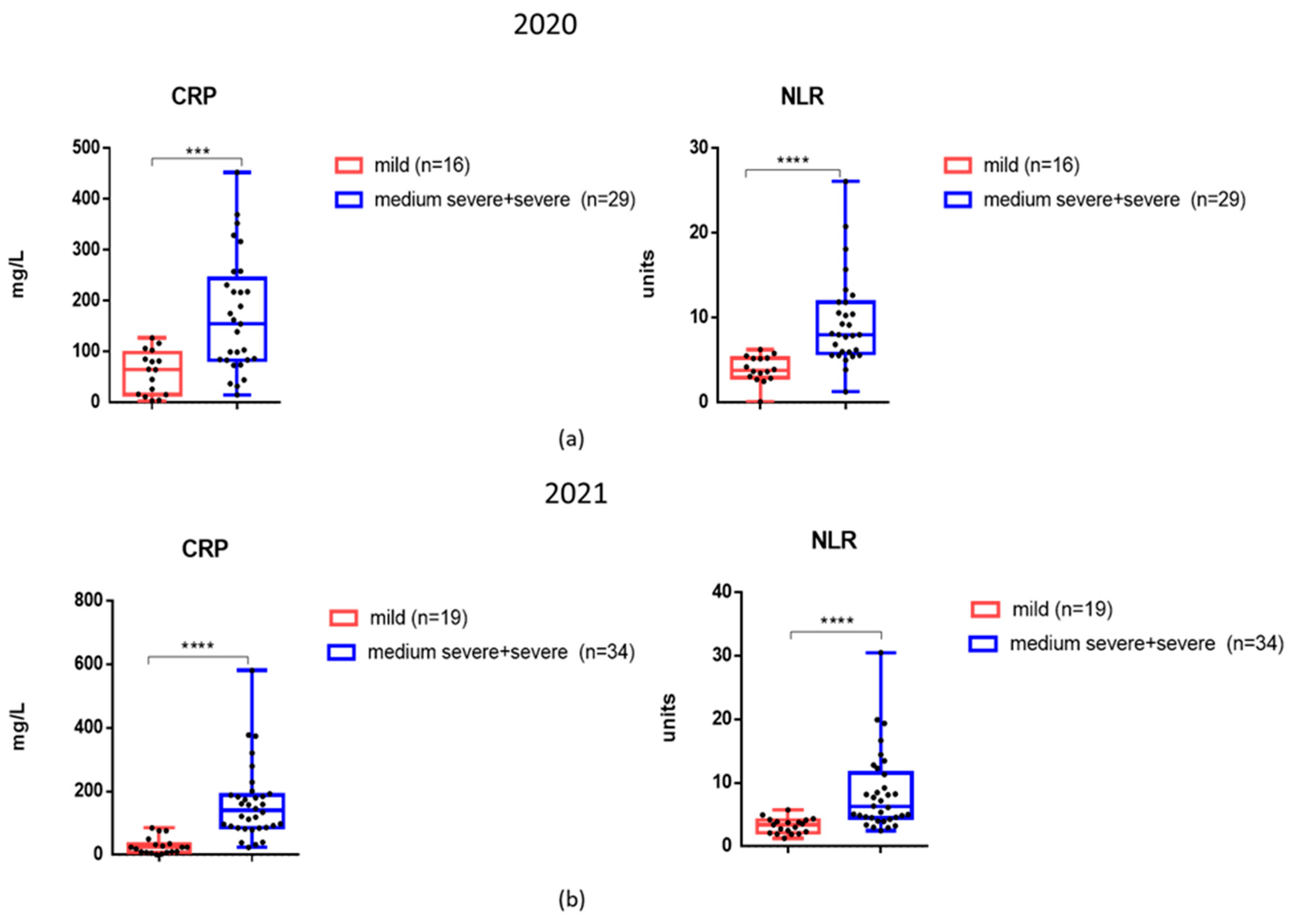
Considering that CRP and NLR levels were elevated in patients not only during the first wave of COVID-19 infection, but also in late 2021, we analyzed these markers among patients with different degrees of severity (
Figure 4, A, B). It was found that in 2021 patients with moderate to severe COVID-19 disease, mean CRP and NLR levels were also significantly higher compared to those with mild disease (
Figure 4, B).
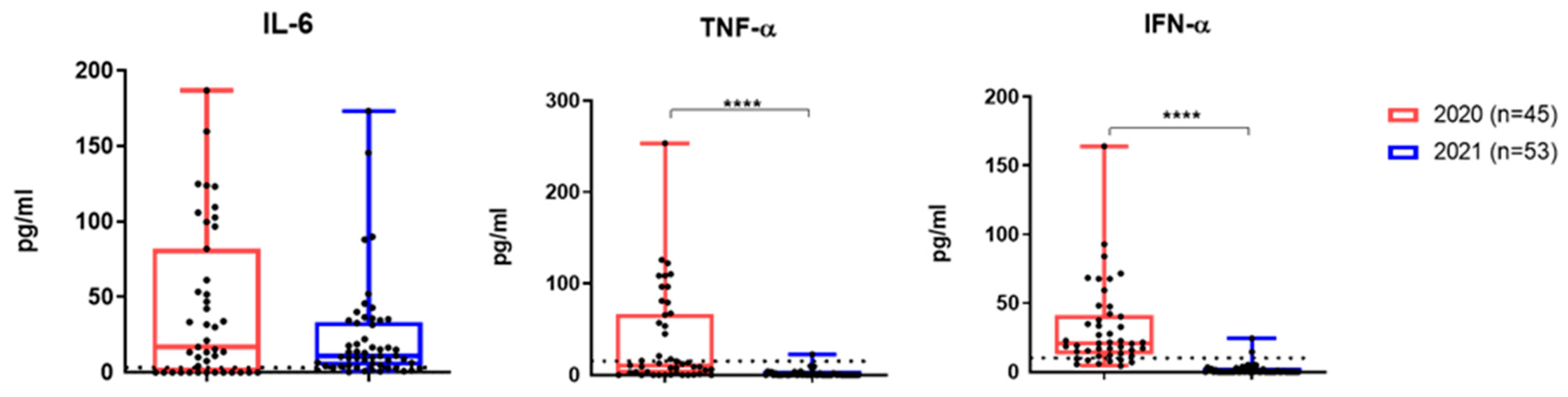
TNF-α and IFN- α levels were significantly lower among patients from the second cohort (
Figure 5). However, IL-6 did not differ significantly between the two groups, and in most patients in second group still significantly exceeded the reference levels (
Figure 5).
3.4. Antibodies to SARS-CoV-2 Analyzed Patient Cohorts
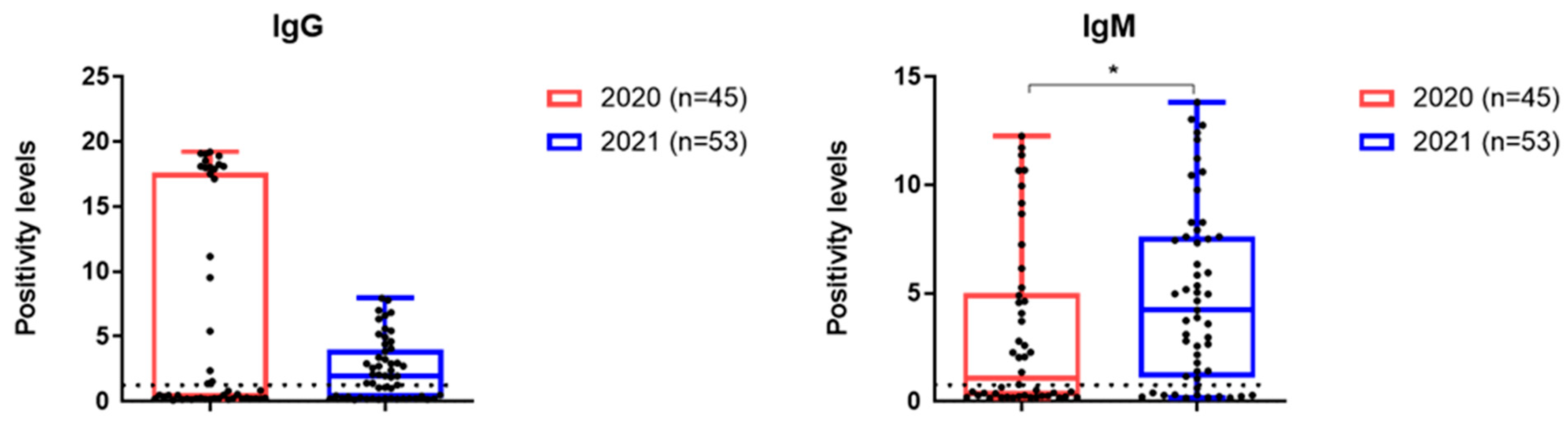
IgG seropositive rates were higher in group 1, while IgM levels were higher in group 2 (
Figure 6).
3.5. Increases in Serum HI Antibodies to Influenza Viruses in Paired Blood Sera
Fourfold or more increases in HI antibody levels to influenza viruses in pairs of serum samples were determined, as there was previous evidence of coinfection with these viruses in acute COVID-19. The main characteristics of the examined patients are presented in
Table 3.
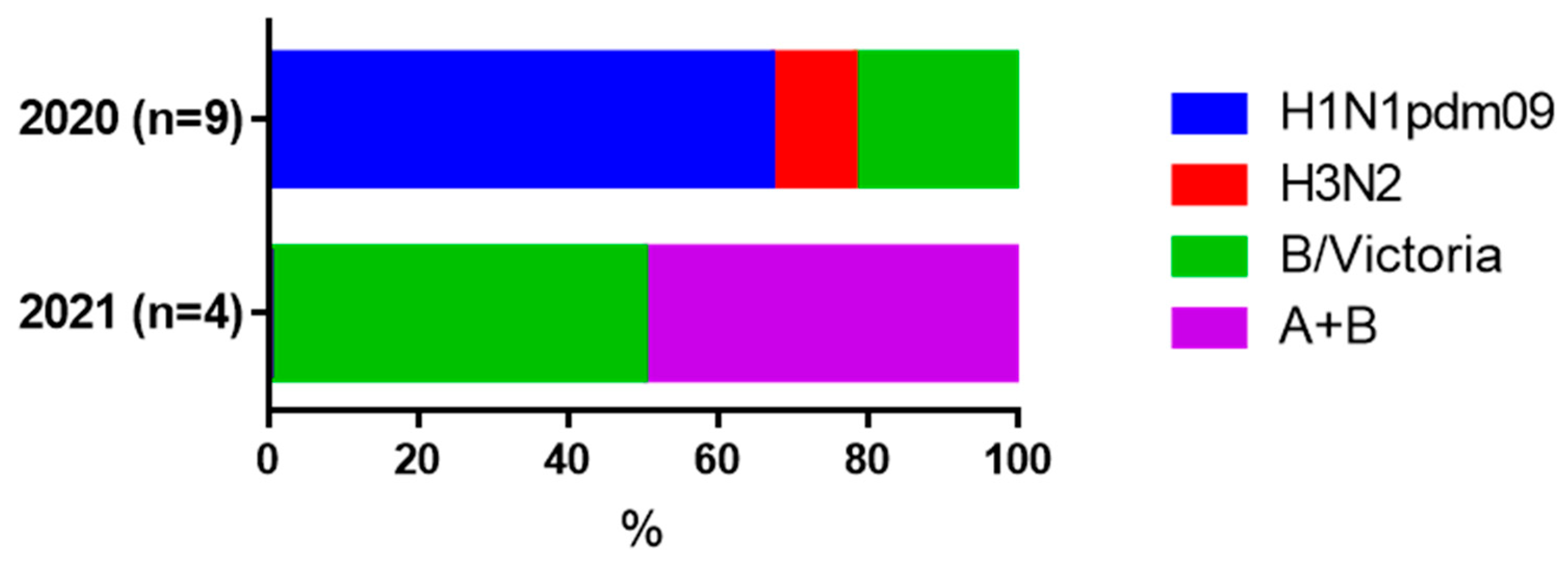
It was shown that in both moderate and severe COVID-19 cases, fourfold or more increases in HI antibodies to influenza A and B viruses were observed in both cohorts (
Table 3). In groups with milder COVID-19, seroconversion to influenza viruses were not detected. In 2020 and 2021 most of the increases in antibody levels were seen for the influenza A/H1N1pdm09 and B/Victoria viruses, respectively. (
Figure 7).
4. Discussion
Analysis of the genomic diversity of SARS-CoV-2 revealed several stages in the spread of the most representative strains of the virus during the pandemic [
16]. Periods with homogeneity of the pathogen population, where the Alpha, Delta or Omicron variants dominated, were followed by more complex stages involving the simultaneous circulation of several strains. This was due to the adaptation of the virus. The Alpha variant, with its high transmissibility and virulence at the beginning of the pandemic, contributed to the emergence of Delta, which caused a sharp increase in the incidence rate. Active vaccination in Russia began in 2021 and led to a rise in seroprevalence up to 50% [
2,
4]. Gradually, Delta adapted to a greater proportion of people who were not susceptible, leading to the formation of Omicron. Delta-Omicron recombinant strains were also found, with the N-terminal portion of the N gene being identical to that of the Omicron sequence. [
17]. We used HRM analysis to compare two SARS-CoV-2 viruses isolated in 2021.
We used HRM-analysis to determine differences between the N protein RNA of two SARS-CoV-2 isolates obtained during 2021. The isolate obtained in late 2021 acquired Omicron features, as a deletion of nucleotides 90–98 was detected, which leads, as previously shown, to the loss of ERS31 amino acids without a frameshift [
32]. Given the low cost and ease of implementation, HRM-analysis is suitable for rapid screening of large numbers of isolates for genotyping purposes.
The study of inflammation markers and cytokines in relation to Omicron and other SARS-CoV-2 variants is an important area of research which can help us understand viral pathogenicity, influence clinical practice and public health policies, as well as therapeutic development.
In our study, about 70% of the patients examined in the late 2021 were vaccinated against COVID-19 and, in general, despite the presence of severe cases, no mortality was observed. Indeed, the proportion of seropositive patients is significantly higher in the second cohort compared with the first cohort (
Table 2). In 2021, no viremia was recorded using the detection of SARS-CoV-2 virus RNA in the blood of patients, and some blood parameters were lower compared to hospitalized patients in 2020. Thus, fibrinogen levels as well as TNF-α and IFN-α levels were statistically significantly lower in patients from the second cohort. It has been shown previously that elevated fibrinogen levels can serve as a marker of inflammation and severity of COVID-19 [
33]. Our study showed that in all patients examined during the first wave of COVID-19, fibrinogen levels were elevated. During Omicron in 2021, some hospitalized patients had fibrinogen levels within the reference values, and the average level was significantly lower compared to 2020 (
Figure 3). The reduction in TNF-α and IFN-α levels in the second cohort shown in our study may reflect a reduction in the overall burden on the immune system with Omicron. However, in hospitalized patients, Omicron still may cause significant systemic inflammation. And indeed, the levels of CRP, NLR and IL-6 did not differ significantly between two groups of patients and remained significantly above reference values both in 2020 and 2021 groups. In 2021, individuals with moderate to severe COVID-19 experienced elevated levels of CRP and NLR compared to those with mild COVID-19 (
Figure 4), just like during the first wave of the disease. The observation that certain pro-inflammatory markers become lower in hospitalized patients during the Omicron wave, while IL-6 remains high, reflects a combination of reduced viral pathogenicity, differences in immune responses, and the distinct roles of specific cytokines in inflammation.
In addition, among patients from the second cohort, the level of serum complement C3 was significantly higher than that in patients examined in 2020 (
Figure 3). Complement component C3 is a protein in the complement system, which is part of the body’s immune response. In the context of COVID-19, complement activation has been observed as a significant part of the immune response to the virus [
34]. The population’s level of immunity due to vaccination or prior infection can affect the immune response to a new variant. Omicron’s impact on serum complement levels may also reflect differences in how people with pre-existing immunity respond compared to those who were infected during the first wave. The increased complement C3 content in 2021 compared to 2020 may confirm the activation of the complement system in response to breakthrough infection with Omicron. This evasion could lead to a more pronounced reliance on the complement system as the immune system attempts to mount a defense [
35]. Nevertheless, some studies suggest that complementary dysregulation, including the involvement of C3, may play a role in the development of long COVID. Previously, it was shown that activation of complement system leading to the formation of the membrane attack complex plays a role in COVID-19 pathogenesis [
36]. This can lead to the release of self-antigens from damaged tissues and trigger an autoimmune response, as the immune system begins to target these self-antigens, leading to tissue inflammation and symptomatology associated with autoimmunity [
36,
37,
38]. Persistent complement activation could contribute to ongoing inflammation and immune dysregulation that characterizes long COVID symptoms. Markers of complement activation, including elevated levels of C3 may provide insights into the underlying mechanisms contributing to prolonged COVID-19 symptoms.
A separate issue is the aggravation of the clinical picture of COVID-19 due to coinfection with influenza viruses. In this regard, there was great similarity between the two examined cohorts. Since 4-fold increases in HI antibodies is the ‘gold standard’ of seroconversion to influenza [
29], the data obtained suggest that in moderate cases of COVID-19, coinfection with influenza viruses could possibly be present. The fact that in 2020 there were increases in the influenza A/H1N1pdm09 virus, and in 2021 - in the B/Victoria virus may coincide with the pattern of circulation of influenza viruses in the indicated epidemic seasons [
39]. The problem of influenza and other respiratory infections in COVID-19 has been repeatedly discussed in the scientific literature. The fact that the incidence of seasonal influenza often coincides with an increase in the incidence of COVID-19 may negatively contribute to the clinical picture of coronavirus infection [
40,
41]
This indicates the need for increased attention to influenza vaccination in the context of preventing severe forms of coronavirus infection. Thus, it has been shown that vaccination with a quadrivalent influenza vaccine not only prevents severe cases of COVID-19, but also helps to ’pre-stimulate’ the immune system for faster and earlier responses to the pathogen [
42].
5. Conclusions
Thus, the analysis of clinical isolates of the SARS-CoV-2 virus using HRM analysis showed the deletion characteristic of the Omicron variant in the N-protein RNA at the end of 2021. HRM analysis allows for the differentiation of changes in the antigenic structure of SARS-CoV variants.
Patients hospitalized both in the first wave of the disease and in 2021 showed a significant increase in CRP, NLR and IL-6. The data that IL-6 and inflammatory markers are significantly increased in Omicron, and average complement levels are higher in 2021 compared to the first wave, it can be assumed that the high transmission capacity of new coronavirus variants may lead to the fact that severe consequences may be observed in a larger number of people.
IgG and IgM to SARS-CoV-2 were detected statistically significantly more often at the beginning of hospitalization during the second wave COVID-19, which may indicate a more rapid immune response due to the formation of memory B cells after previous infections or immunizations.
And finally, the fact that seroconversions to influenza viruses were detected in moderate and severe cases of COVID-19 indicates an additional negative contribution of influenza to the pathogenesis of coronavirus infection.
Further studies are needed to determine whether clinical presentation and blood parameters change in response to changes in the SARS-CoV-2 virus in breakthrough infections and in patients with post-COVID syndrome.
Supplementary Materials
The following supporting information can be downloaded at website of this paper posted on Preprints.org, Table S1: Characteristics of patients with COVID-19 depending on the gender of participants, cohort 1.; Table S2: Characteristics of patients with COVID-19 depending on the gender of participants, cohort 2; Table S3: Characteristics of patients with COVID-19 depending on the age of participants, cohort 1.; Table S4: Characteristics of patients with COVID-19 depending on the age of participants, cohort 2; Table S5: Characteristics of patients with COVID-19 depending on the presence of vaccination, for 2021.
Author Contributions
Conceptualization, Yu.D.; methodology, O.S. and P.K; software, D.P.; validation, T.S., A.L. and T.K.; formal analysis, E.G.; investigation, P.K.; data curation, T.S.; writing—original draft preparation, Yu.D. and D.G.; writing—review and editing, Yu.D.; visualization, O.K.; supervision, S.P. All authors have read and agreed to the published version of the manuscript.
Funding
Please add: The work was supported by budget funds of the Federal State Budgetary Scientific Institution “Institute of Experimental Medicine”, topic FGWG-2003-0002.
Institutional Review Board Statement
The study was approved by the Local Ethics Committee of the Federal State Budgetary Scientific Institution ‘IEM’ (protocol 1/23 dated 04/20/2023).
Informed Consent Statement
All study participants signed a written informed consent.
Data Availability Statement
All data is contained in the text of the paper and in the supplementary files..
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| COVID-19 |
coronavirus disease-19 |
| CRP |
C-reactive protein |
| HI |
Hemagglutination Inhibition |
| HRM |
High-Resolution Melting |
| IFN-α |
Interferon 1 alpha |
| IL-6 |
Interleukin-6 |
| Me |
Medians |
| M-MulV RT |
Moloney Murine Leukemia Virus Reverse Transcriptase |
| NLR |
NLR neutrophil/lymphocyte ratio |
| Q1; Q3 |
Lower and upper quartiles |
| RBCs |
Red Blood Cells |
| SARS-CoV-2 |
Severe acute respiratory syndrome coronavirus 2 () |
| TNF-α |
Tumor Necrosis Factor alpha |
References
- Kawamura, S.; Yamaguchi, F.; Kusakado, R.; Go, Y.; Nohmi, S.; Yoshizaki, C.; Yoshida, Y.; Izumizaki, K.; Saito, Y.; Kobayashi, H.; et al. Changes in Clinical Features and Severity of COVID-19 with the Emergence of Omicron Variants: A Shift Towards a Common Disease. Infect. Drug Resist. 2024, ume 17, 5595–5603. [CrossRef]
- Akimkin V., et al. COVID-19 epidemic process and evolution of SARS-CoV-2 genetic variants in the Russian Federation // Microbiology Research. – 2024. – Т. 15, № 1. – С. 213–224.
- Meo, S.A.; Meo, A.S.; Al-Jassir, F.F.; Klonoff, D.C. Omicron SARS-CoV-2 new variant: global prevalence and biological and clinical characteristics. European Review for Medical & Pharmacological Sciences 2021, 25, 8012–8018. [CrossRef]
- Long, B.; Carius, B.M.; Chavez, S.; Liang, S.Y.; Brady, W.J.; Koyfman, A.; Gottlieb, M. Clinical update on COVID-19 for the emergency clinician: Presentation and evaluation. Am. J. Emerg. Med. 2022, 54, 46–57. [CrossRef]
- Akimkin, V.G.; Popova, A.Y.; Khafizov, K.F.; Dubodelov, D.V.; Ugleva, S.V.; Semenenko, T.A.; Ploskireva, A.A.; Gorelov, A.V.; Pshenichnaya, N.Y.; Yezhlova, E.; et al. COVID-19: evolution of the pandemic in Russia. Report II: dynamics of the circulation of SARS-CoV-2 genetic variants. J. Microbiol. epidemiology Immunobiol. 2022, 99, 381–396. [CrossRef]
- Park, S.W.; Sun, K.; Abbott, S.; Sender, R.; Bar-On, Y.M.; Weitz, J.S.; Funk, S.; Grenfell, B.T.; Backer, J.A.; Wallinga, J.; et al. Inferring the differences in incubation-period and generation-interval distributions of the Delta and Omicron variants of SARS-CoV-2. Proc. Natl. Acad. Sci. 2023, 120. [CrossRef]
- Hui, K.P.Y.; Ho, J.C.W.; Cheung, M.-C.; Ng, K.-C.; Ching, R.H.H.; Lai, K.-L.; Kam, T.T.; Gu, H.; Sit, K.-Y.; Hsin, M.K.Y.; et al. SARS-CoV-2 Omicron variant replication in human bronchus and lung ex vivo. Nature 2022, 603, 715–720. [CrossRef]
- Ren, S. Y., Wang, W. B., Gao, R. D., & Zhou, A. M. (2022). Omicron variant (B. 1.1. 529) of SARS-CoV-2: Mutation, infectivity, transmission, and vaccine resistance. World journal of clinical cases, 10(1), 1.
- Xia, S.; Wang, L.; Zhu, Y.; Lu, L.; Jiang, S. Origin, virological features, immune evasion and intervention of SARS-CoV-2 Omicron sublineages. Signal Transduct. Target. Ther. 2022, 7, 1–7. [CrossRef]
- Liu, Y.; Huang, X.; Li, P.; Wang, D.; Yin, H.; Wang, N.; Luo, Y.; Li, H.; Sun, S. Clinical Profile and Outcome Analysis of Ear-Nose-Throat Symptoms in SARS-CoV-2 Omicron Subvariant Infections. Int. J. Public Heal. 2023, 68, 1606403. [CrossRef]
- Chemaitelly, H.; Ayoub, H.H.; Coyle, P.; Tang, P.; Hasan, M.R.; Yassine, H.M.; Al Thani, A.A.; Al-Kanaani, Z.; Al-Kuwari, E.; Jeremijenko, A.; et al. Differential protection against SARS-CoV-2 reinfection pre- and post-Omicron. Nature 2025, 639, 1–8. [CrossRef]
- Ao, D., Lan, T., He, X., Liu, J., Chen, L., Baptista-Hon, D. T., ... & Wei, X. (2022). SARS-CoV-2 Omicron variant: immune escape and vaccine development. MedComm, 3(1), e126.
- Chatterjee, S.; Bhattacharya, M.; Nag, S.; Dhama, K.; Chakraborty, C. A Detailed Overview of SARS-CoV-2 Omicron: Its Sub-Variants, Mutations and Pathophysiology, Clinical Characteristics, Immunological Landscape, Immune Escape, and Therapies. Viruses 2023, 15, 167. [CrossRef]
- M Hussein, A., Majeed, H. A., Majeed, N. R., Ali, N. H., Saeed, D. A., & Ali, N. A. (2024). An Overview of Signs and Symptoms to Determine Coronavirus and Omicron Patients in Primary Care and Hospitals. Cihan University-Erbil Scientific Journal, 8(1), 8-17.
- Hansen, P.R. Relative contagiousness of emerging virus variants: An analysis of the Alpha, Delta, and Omicron SARS-CoV-2 variants. Econ. J. 2022, 25, 739–761. [CrossRef]
- Malik, Y.A. Covid-19 variants: Impact on transmissibility and virulence. The Malaysian journal of pathology 2022, 44, 387–396.
- Zabidi, N.Z.; Liew, H.L.; Farouk, I.A.; Puniyamurti, A.; Yip, A.J.W.; Wijesinghe, V.N.; Low, Z.Y.; Tang, J.W.; Chow, V.T.K.; Lal, S.K. Evolution of SARS-CoV-2 Variants: Implications on Immune Escape, Vaccination, Therapeutic and Diagnostic Strategies. Viruses 2023, 15, 944. [CrossRef]
- Fan, H.; Tian, M.; Liu, S.; Ye, C.; Li, Z.; Wu, K.; Zhu, C. Strategies Used by SARS-CoV-2 to Evade the Innate Immune System in an Evolutionary Perspective. Pathogens 2024, 13, 1117. [CrossRef]
- Afridonova, Z.E.; Toptygina, A.P.; Mikhaylov, I.S. Humoral and Cellular Immune Response to SARS-CoV-2 S and N Proteins. Biochem. (Moscow) 2024, 89, 872–882. [CrossRef]
- El-Maradny, Y.A.; Badawy, M.A.; Mohamed, K.I.; Ragab, R.F.; Moharm, H.M.; Abdallah, N.A.; Elgammal, E.M.; Rubio-Casillas, A.; Uversky, V.N.; Redwan, E.M. Unraveling the role of the nucleocapsid protein in SARS-CoV-2 pathogenesis: From viral life cycle to vaccine development. Int. J. Biol. Macromol. 2024, 279, 135201. [CrossRef]
- Rahman, M.S.; Islam, M.R.; Alam, A.S.M.R.U.; Islam, I.; Hoque, M.N.; Akter, S.; Rahaman, M.; Sultana, M.; Hossain, M.A. Evolutionary dynamics of SARS-CoV-2 nucleocapsid protein and its consequences. J. Med Virol. 2020, 93, 2177–2195. [CrossRef]
- Alosaimi, B.; Naeem, A.; Hamed, M.E.; Alkadi, H.S.; Alanazi, T.; Al Rehily, S.S.; Almutairi, A.Z.; Zafar, A. Influenza co-infection associated with severity and mortality in COVID-19 patients. Virol. J. 2021, 18, 1–9. [CrossRef]
- Wu, X.; Cai, Y.; Huang, X.; Yu, X.; Zhao, L.; Wang, F.; Li, Q.; Gu, S.; Xu, T.; Li, Y.; et al. Co-infection with SARS-CoV-2 and Influenza A Virus in Patient with Pneumonia, China. Emerg. Infect. Dis. 2020, 26, 1324–1326. [CrossRef]
- Cuadrado-Payán, E., Montagud-Marrahi, E., Torres-Elorza, M., Bodro, M., Blasco, M., Poch, E., ... & Piñeiro, G. J. (2020). SARS-CoV-2 and influenza virus co-infection. Lancet (London, England), 395(10236), e84.
- Shvedova, T.N.; Kopteva, O.S.; Kudar, P.A.; Lerner, A.A.; Desheva, Y.A. The role of coinfection with influenza viruses in the pathogenesis of severe infection in patients with COVID-19. Med Acad. J. 2021, 21, 159–164. [CrossRef]
- Dhanasekaran, V.; Sullivan, S.; Edwards, K.M.; Xie, R.; Khvorov, A.; Valkenburg, S.A.; Cowling, B.J.; Barr, I.G. Human seasonal influenza under COVID-19 and the potential consequences of influenza lineage elimination. Nat. Commun. 2022, 13, 1–11. [CrossRef]
- Tamura, K.; Stecher, G.; Kumar, S. MEGA11: Molecular Evolutionary Genetics Analysis Version 11. Mol. Biol. Evol. 2021, 38, 3022–3027. [CrossRef]
- Desheva, Y.A.; Smolonogina, T.A.; Landgraf, G.O.; Rudenko, L.G. Development of the A/H6N1 influenza vaccine candidate based on A/Leningrad/134/17/57 (H2N2) master donor virus and the genome composition analysis using high resolution melting (HRM). Microbiol. Indep. Res. J. 2016, 3. [CrossRef]
- Katz, J.M.; Hancock, K.; Xu, X. Serologic assays for influenza surveillance, diagnosis and vaccine evaluation. Expert Rev. Anti-infective Ther. 2011, 9, 669–683. [CrossRef]
- Sharma, R., & Dubey, S. K. (2020). Computational Management of Alignment of Multiple Protein Sequences Using ClustalW. In First International Conference on Sustainable Technologies for Computational Intelligence: Proceedings of ICTSCI 2019 (pp. 177-186). Springer Singapore.
- O’toole, Á.; Pybus, O.G.; Abram, M.E.; Kelly, E.J.; Rambaut, A. Pango lineage designation and assignment using SARS-CoV-2 spike gene nucleotide sequences. BMC Genom. 2022, 23, 1–13. [CrossRef]
- Liang, F. Quantitative Mutation Analysis of Genes and Proteins of Major SARS-CoV-2 Variants of Concern and Interest. Viruses 2023, 15, 1193. PMID: 37243278; PMCID: PMC10222255. [CrossRef]
- Sui, J.; Noubouossie, D.F.; Gandotra, S.; Cao, L. Elevated Plasma Fibrinogen Is Associated With Excessive Inflammation and Disease Severity in COVID-19 Patients. Front. Cell. Infect. Microbiol. 2021, 11, 734005. [CrossRef]
- Xiao, M.T.; Ellsworth, C.R.; Qin, X. Emerging role of complement in COVID-19 and other respiratory virus diseases. Cell. Mol. Life Sci. 2024, 81, 1–18. [CrossRef]
- Mellors, J.; Dhaliwal, R.; Longet, S.; Tipton, T.; Barnes, E.; Dunachie, S.J.; Klenerman, P.; Hiscox, J.; Carroll, M. Complement-mediated enhancement of SARS-CoV-2 antibody neutralisation potency in vaccinated individuals. Nat. Commun. 2025, 16, 1–15. [CrossRef]
- Ellsworth, C.R.; Chen, Z.; Xiao, M.T.; Qian, C.; Wang, C.; Khatun, M.S.; Liu, S.; Islamuddin, M.; Maness, N.J.; Halperin, J.A.; et al. Enhanced complement activation and MAC formation accelerates severe COVID-19. Cell. Mol. Life Sci. 2024, 81, 1–14. [CrossRef]
- Detsika, M.G.; Palamaris, K.; Dimopoulou, I.; Kotanidou, A.; Orfanos, S.E. The complement cascade in lung injury and disease. Respir. Res. 2024, 25, 1–16. [CrossRef]
- Dumitrescu, G.; Antovic, J.; Soutari, N.; Gran, C.; Antovic, A.; Al-Abani, K.; Grip, J.; Rooyackers, O.; Taxiarchis, A. The role of complement and extracellular vesicles in the development of pulmonary embolism in severe COVID-19 cases. PLOS ONE 2024, 19, e0309112. [CrossRef]
- Yatsyshina, S.B.; Artamonova, A.A.; Elkina, M.A.; Valdokhina, A.V.; Bulanenko, V.P.; Berseneva, A.A.; Akimkin, V.G. Genetic characteristics of influenza A and B viruses circulating in Russia in 2019–2023. J. Microbiol. epidemiology Immunobiol. 2024, 101, 719–734. [CrossRef]
- Pawlowski, C.; Silvert, E.; O'Horo, J.C.; Lenehan, P.J.; Challener, D.; Gnass, E.; Murugadoss, K.; Ross, J.; Speicher, L.; Geyer, H.; et al. SARS-CoV-2 and influenza coinfection throughout the COVID-19 pandemic: an assessment of coinfection rates, cohort characteristics, and clinical outcomes. PNAS Nexus 2022, 1, pgac071. [CrossRef]
- Varshney, K.; Pillay, P.; Mustafa, A.D.; Shen, D.; Adalbert, J.R.; Mahmood, M.Q. A systematic review of the clinical characteristics of influenza-COVID-19 co-infection. Clin. Exp. Med. 2023, 23, 3265–3275. [CrossRef]
- Debisarun, P.A.; Gössling, K.L.; Bulut, O.; Kilic, G.; Zoodsma, M.; Liu, Z.; Oldenburg, M.; Rüchel, N.; Zhang, B.; Xu, C.-J.; et al. Induction of trained immunity by influenza vaccination - impact on COVID-19. PLOS Pathog. 2021, 17, e1009928. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).