Submitted:
19 February 2025
Posted:
20 February 2025
You are already at the latest version
Abstract
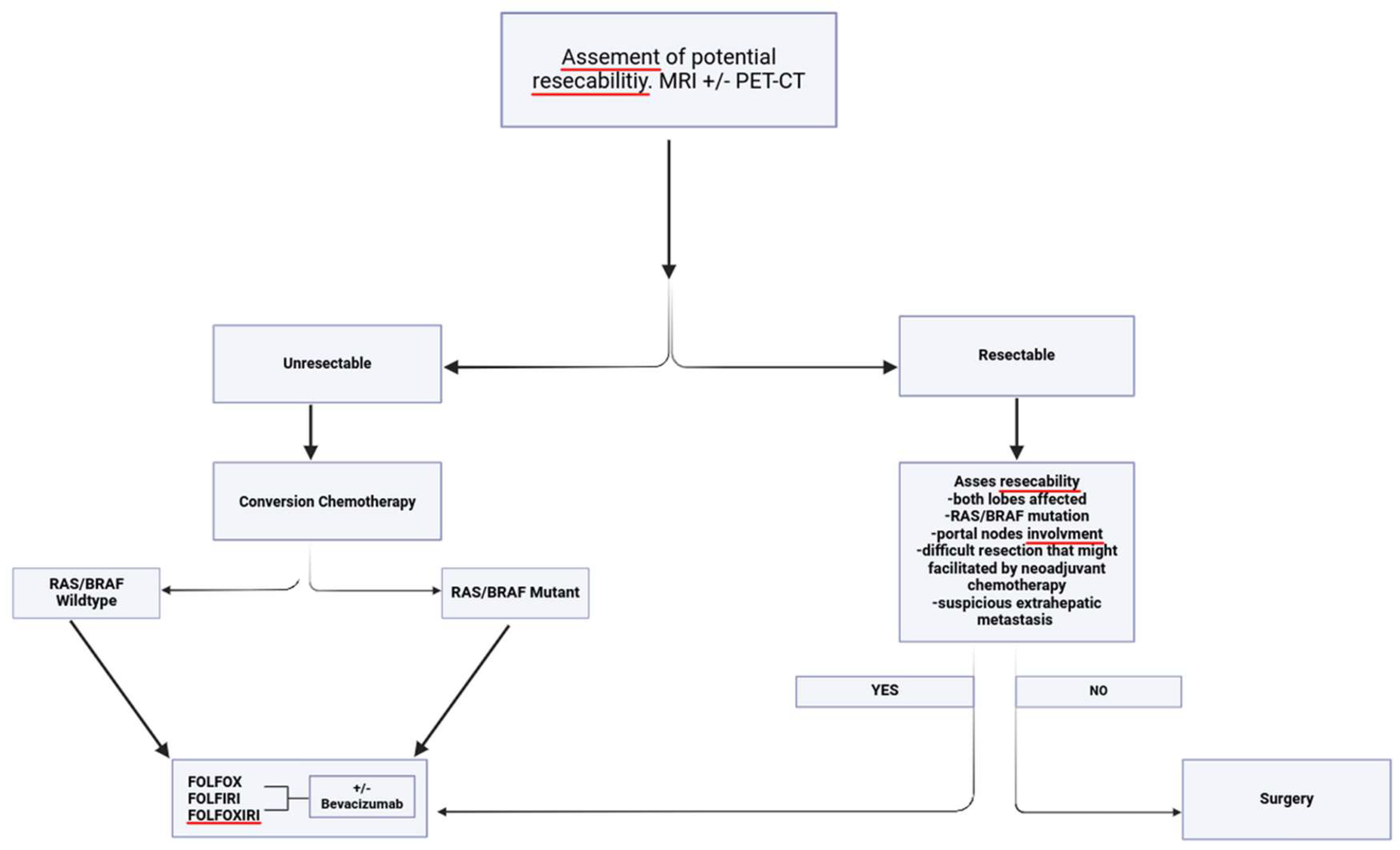
Oligometastatic colorectal cancer (CRC) refers to a state in which distant metastatic spread is limited to a few sites, offering the potential for curative treatment with aggressive local therapies. The surgical management of oligometastatic CRC has gained increasing attention due to its potential to improve survival. This review explores the evolving role of surgery in the treatment of oligometastatic disease, focusing on the criteria for selecting patients, surgical techniques, and outcomes. While systemic therapy remains essential, surgery can offer long-term survival benefits for appropriately selected patients with limited metastatic disease, particularly those with metastases confined to the liver, lungs, or isolated sites in other organs. Advances in imaging technologies, minimally invasive surgical techniques, and perioperative care have enhanced the safety and efficacy of these procedures. The integration of multimodal therapies, such as chemotherapy, targeted therapy, and immunotherapy, in conjunction with surgery, is also discussed, with a focus on optimizing outcomes. This review aims to clarify how and when liver resection first can be chosen, when preoperative systemic treatment is needed and if this is chosen, what is the best approach.
Keywords:
Introduction
Methods: Literature Search
Results and Discussion
Presurgery Evaluation
Simultaneous Versus Staged Resection
Hepatic Metastases Defined as Unresectable
RAS/RAF Mutated Tumors
RAS/RAF Wild-Type Tumors
Hepatic Metastases Are Defined as Resectable
Conclusion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Berri, R.N.; Abdalla, E.K. Curable metastatic colorectal cancer: Recommended paradigms. Curr. Oncol. Rep. 2009, 11, 200–208. [Google Scholar] [CrossRef] [PubMed]
- Folprecht, G.; Grothey, A.; Alberts, S.; Raab, H.-R.; Köhne, C.-H. Neoadjuvant treatment of unresectable colorectal liver metastases: correlation between tumour response and resection rates. Ann. Oncol. 2005, 16, 1311–1319. [Google Scholar] [CrossRef] [PubMed]
- Grothey A, Hedrick EE, Mass RD, et al. Response-independent survival benefit in metastatic colorectal cancer: a comparative analysis of N9741 and AVF. J Clin Oncol 2008, 26, 183. [CrossRef]
- Bipat S, van Leeuwen MS, Comans EF, et al. Colorectal liver metastases: CT, MR imaging, and PET for diagnosis--meta-analysis. Radiology 2005, 237, 123. [CrossRef]
- Kamel, I.R.; Choti, M.A.; Horton, K.M.; Braga, H.J.V.; Birnbaum, B.A.; Fishman, E.K.; Thompson, R.E.; Bluemke, D.A. Surgically Staged Focal Liver Lesions: Accuracy and Reproducibility of Dual-Phase Helical CT for Detection and Characterization. Radiology 2003, 227, 752–757. [Google Scholar] [CrossRef] [PubMed]
- Floriani, I.; Torri, V.; Rulli, E.; Garavaglia, D.; Compagnoni, A.; Salvolini, L.; Giovagnoni, A. Performance of imaging modalities in diagnosis of liver metastases from colorectal cancer: A systematic review and meta-analysis. J. Magn. Reson. Imaging 2009, 31, 19–31. [Google Scholar] [CrossRef]
- Kulemann V, Schima W, Tamandl D, et al. Preoperative detection of colorectal liver metastases in fatty liver: MDCT or MRI? Eur J Radiol 2011, 79, e1. [CrossRef]
- Scharitzer, M.; Ba-Ssalamah, A.; Ringl, H.; Kölblinger, C.; Grünberger, T.; Weber, M.; Schima, W. Preoperative evaluation of colorectal liver metastases: comparison between gadoxetic acid-enhanced 3.0-T MRI and contrast-enhanced MDCT with histopathological correlation. Eur. Radiol. 2013, 23, 2187–2196. [Google Scholar] [CrossRef]
- Sahani, D.V.; Bajwa, M.A.; Andrabi, Y.; Bajpai, S.; Cusack, J.C. Current Status of Imaging and Emerging Techniques to Evaluate Liver Metastases From Colorectal Carcinoma. Ann. Surg. 2014, 259, 861–872. [Google Scholar] [CrossRef]
- National Comprehensive Cancer Network. Colon Cancer. Version 5.2024 colon.pdf Accesed on 29 Dec 2024.
- Ruers, T.J.; Wiering, B.; van der Sijp, J.R.; Roumen, R.M.; de Jong, K.P.; Comans, E.F.; Pruim, J.; Dekker, H.M.; Krabbe, P.F.; Oyen, W.J. Improved Selection of Patients for Hepatic Surgery of Colorectal Liver Metastases with 18F-FDG PET: A Randomized Study. J. Nucl. Med. 2009, 50, 1036–1041. [Google Scholar] [CrossRef]
- Akhurst, T.; Gönen, M.; Baser, R.E.; Schwartz, L.H.; Tuorto, S.; Brody, L.A.; Covey, A.; Brown, K.T.; Larson, S.M.; Fong, Y. Prospective evaluation of 18F-FDG positron emission tomography in the preoperative staging of patients with hepatic colorectal metastases. HepatoBiliary Surg. Nutr. 2021, 11, 539–554. [Google Scholar] [CrossRef] [PubMed]
- Lai, D.T.M.; Fulham, M.; Stephen, M.S.; Chu, K.-M.; Thompson, J.F.; Sheldon, D.M.; Storey, D.W. The Role of Whole-Body Positron Emission Tomography With [18F]Fluorodeoxyglucose in Identifying Operable Colorectal Cancer Metastases to the Liver. Arch. Surg. 1996, 131, 703–707. [Google Scholar] [CrossRef] [PubMed]
- Delbeke, D.; Vitola, J.V.; Sandler, M.P.; Arildsen, R.C.; A Powers, T.; Wright, J.K.; Chapman, W.C.; Pinson, C.W. Staging recurrent metastatic colorectal carcinoma with PET. J Nucl Med. 1997, 38, 1196–201. [Google Scholar]
- Mekenkamp, L.J.M.; Koopman, M.; Teerenstra, S.; van Krieken, J.H.J.M.; Mol, L.; Nagtegaal, I.D.; A Punt, C.J. Clinicopathological features and outcome in advanced colorectal cancer patients with synchronous vs metachronous metastases. Br. J. Cancer 2010, 103, 159–164. [Google Scholar] [CrossRef]
- Tsai, M.-S.; Su, Y.-H.; Ho, M.-C.; Liang, J.-T.; Chen, T.-P.; Lai, H.-S.; Lee, P.-H. Clinicopathological Features and Prognosis in Resectable Synchronous and Metachronous Colorectal Liver Metastasis. Ann. Surg. Oncol. 2006, 14, 786–794. [Google Scholar] [CrossRef]
- Driedger, M.R.; Yamashita, T.S.; Starlinger, P.; Mathis, K.L.; Smoot, R.L.; Cleary, S.P.; Nagorney, D.M. Synchronous resection of colorectal cancer primary and liver metastases: an outcomes analysis. HPB 2021, 23, 1277–1284. [Google Scholar] [CrossRef]
- McCahill LE, Yothers G, Sharif S, et al. Primary mFOLFOX6 plus bevacizumab without resection of the primary tumor for patients presenting with surgically unresectable metastatic colon cancer and an intact asymptomatic colon cancer: definitive analysis of NSABP trial C. J Clin Oncol 2012, 30, 3223.
- Shimada, H.; Tanaka, K.; Masui, H.; Nagano, Y.; Matsuo, K.; Kijima, M.; Ichikawa, Y.; Ike, H.; Ooki, S.; Togo, S. Results of surgical treatment for multiple (> or =5 nodules) bi-lobar hepatic metastases from colorectal cancer. Langenbeck's Arch. Surg. 2004, 389, 114–121. [Google Scholar] [CrossRef]
- Gruenberger, T.; Morris, D.L. Staged Treatment of Bilobar Hepatic Metastases from Colorectal Cancer. Eur. J. Surg. 2002, 168, 516–518. [Google Scholar] [CrossRef] [PubMed]
- Birrer, D.L.; Tschuor, C.; Reiner, C.S.; Fritsch, R.; Pfammatter, T.; Schüler, H.G.; Pavic, M.; De Oliveira, M.; Petrowsky, H.; Dutkowski, P.; et al. Multimodal treatment strategies for colorectal liver metastases. Swiss Med Wkly. 2021, 151, w20390. [Google Scholar] [CrossRef] [PubMed]
- Boudiaf Z, Bouzid C, Ait-Arab MR, Cherchar K, Kheloufi M, Chibane A, Boutekedjiret IH, Hattou Z, Gouaref F, Bentabak K. La chirurgie laparoscopique de downstaging pour cancer colorectal avec métastases hépatiques synchrones: quel intérêt dans les hépatectomies en deux temps? à propos d’une série de 6 cas [Laparoscopic downstaging surgery for colorectal cancer with synchronous liver metastases: what value in two-stage hepatectomies?]. Pan Afr Med J. 2023, 27, 46:38.
- Ono, Y.; Inoue, Y.; Kobayashi, K.; Sato, S.; Kitano, Y.; Oba, A.; Sato, T.; Ito, H.; Takahashi, Y. Laparoscopic Portal Vein Ligation and Embolization During First-Stage Hepatectomy for Initially Unresectable Colorectal Liver Metastases. Ann. Surg. Oncol. 2024, 31, 1–2. [Google Scholar] [CrossRef] [PubMed]
- Adam R, Wicherts DA, de Haas RJ, et al. Complete pathologic response after preoperative chemotherapy for colorectal liver metastases: myth or reality? J Clin Oncol 2008, 26, 1635. [CrossRef]
- Blazer DG 3rd, Kishi Y, Maru DM, et al. Pathologic response to preoperative chemotherapy: a new outcome end point after resection of hepatic colorectal metastases. J Clin Oncol 2008, 26, 5344. [CrossRef]
- Benoist S, Brouquet A, Penna C, et al. Complete response of colorectal liver metastases after chemotherapy: does it mean cure? J Clin Oncol 2006, 24, 3939. [CrossRef]
- Kim SS, Song KD, Kim YK, Kim HC, Huh JW, Park YS, Park JO, Kim ST. Disappearing or residual tiny (≤5 mm) colorectal liver metastases after chemotherapy on gadoxetic acid-enhanced liver MRI and diffusion-weighted imaging: Is local treatment required? Eur Radiol. 2017, 27, 3088–3096. [CrossRef]
- Kepenekian, V.; Muller, A.; Valette, P.J.; Rousset, P.; Chauvenet, M.; Phelip, G.; Walter, T.; Adham, M.; Glehen, O.; Passot, G. Evaluation of a strategy using pretherapeutic fiducial marker placement to avoid missing liver metastases. BJS Open 2018, 3, 344–353. [Google Scholar] [CrossRef]
- Tsilimigras, D.I.; Ntanasis-Stathopoulos, I.; Paredes, A.Z.; Moris, D.; Gavriatopoulou, M.; Cloyd, J.M.; Pawlik, T.M. Disappearing liver metastases: A systematic review of the current evidence. Surg. Oncol. 2019, 29, 7–13. [Google Scholar] [CrossRef]
- Alberts SR, Horvath WL, Sternfeld WC, et al. Oxaliplatin, fluorouracil, and leucovorin for patients with unresectable liver-only metastases from colorectal cancer: a North Central Cancer Treatment Group phase II study. J Clin Oncol 2005, 23, 9243. [CrossRef]
- Hayashi, H.; Miyamoto, Y.; Higashi, T.; Hiyoshi, Y.; Yamao, T.; Uemura, N.; Matsumura, K.; Imai, K.; Yamashita, Y.-I.; Baba, H. CD44 expression enhances chemoresistance and implies occult micrometastases after conversion hepatectomy for initially unresectable colorectal liver metastases. Am J Transl Res. 2020, 15, 5955–5966. [Google Scholar]
- A Bridgewater, J.; A Pugh, S.; Maishman, T.; Eminton, Z.; Mellor, J.; Whitehead, A.; Stanton, L.; Radford, M.; Corkhill, A.; O Griffiths, G.; et al. Systemic chemotherapy with or without cetuximab in patients with resectable colorectal liver metastasis (New EPOC): long-term results of a multicentre, randomised, controlled, phase 3 trial. Lancet Oncol. 2020, 21, 398–411. [Google Scholar] [CrossRef] [PubMed]
- Stintzing S, Modest DP, Rossius L, Lerch MM, von Weikersthal LF, Decker T, Kiani A, Vehling-Kaiser U, Al-Batran SE, Heintges T, Lerchenmüller C, Kahl C, Seipelt G, Kullmann F, Stauch M, Scheithauer W, Held S, Giessen-Jung C, Moehler M, Jagenburg A, Kirchner T, Jung A, Heinemann V; FIRE-3 investigators. FOLFIRI plus cetuximab versus FOLFIRI plus bevacizumab for metastatic colorectal cancer (FIRE-3): a post-hoc analysis of tumour dynamics in the final RAS wild-type subgroup of this randomised open-label phase 3 trial. Lancet Oncol. 2016, 17, 1426–1434.
- A Adams, R.; Meade, A.M.; Seymour, M.T.; Wilson, R.H.; Madi, A.; Fisher, D.; Kenny, S.L.; Kay, E.; Hodgkinson, E.; Pope, M.; et al. Intermittent versus continuous oxaliplatin and fluoropyrimidine combination chemotherapy for first-line treatment of advanced colorectal cancer: results of the randomised phase 3 MRC COIN trial. Lancet Oncol. 2011, 12, 642–653. [Google Scholar] [CrossRef]
- Van Cutsem, E.; Lang, I.; Folprecht, G.; Nowacki, M.; Barone, C.; Shchepotin, I.; Maurel, J.; Cunningham, D.; Celik, I.; Kohne, C. Cetuximab plus FOLFIRI: Final data from the CRYSTAL study on the association of KRAS and BRAF biomarker status with treatment outcome. J. Clin. Oncol. 2010, 28, 3570–3570. [Google Scholar] [CrossRef]
- Tournigand, C.; Cervantes, A.; Figer, A.; Lledo, G.; Flesch, M.; Buyse, M.; Mineur, L.; Carola, E.; Etienne, P.-L.; Rivera, F.; et al. OPTIMOX1: A Randomized Study of FOLFOX4 or FOLFOX7 With Oxaliplatin in a Stop-and-Go Fashion in Advanced Colorectal Cancer—A GERCOR Study. J. Clin. Oncol. 2006, 24, 394–400. [Google Scholar] [CrossRef]
- Schwartzberg, L.S.; Rivera, F.; Karthaus, M.; Fasola, G.; Canon, J.-L.; Hecht, J.R.; Yu, H.; Oliner, K.S.; Go, W.Y. PEAK: A Randomized, Multicenter Phase II Study of Panitumumab Plus Modified Fluorouracil, Leucovorin, and Oxaliplatin (mFOLFOX6) or Bevacizumab Plus mFOLFOX6 in Patients With Previously Untreated, Unresectable, Wild-Type KRAS Exon 2 Metastatic Colorectal Cancer. J. Clin. Oncol. 2014, 32, 2240–2247. [Google Scholar] [CrossRef]
- Mise Y, Hasegawa K, Saiura A, et al. A Multicenter Phase 2 Trial to Evaluate the Efficacy of mFOLFOX6 + Cetuximab as Induction Chemotherapy to Achieve R0 Surgical Resection for Advanced Colorectal Liver Metastases (NEXTO Trial). Ann Surg Oncol 2020, 27, 4188. [CrossRef]
- Masi, G.; Loupakis, F.; Pollina, L.; Vasile, E.; Cupini, S.; Ricci, S.; Brunetti, I.M.; Ferraldeschi, R.; Naso, G.; Filipponi, F.; et al. Long-Term Outcome of Initially Unresectable Metastatic Colorectal Cancer Patients Treated with 5-Fluorouracil/Leucovorin, Oxaliplatin, and Irinotecan (FOLFOXIRI) Followed by Radical Surgery of Metastases. Ann. Surg. 2009, 249, 420–425. [Google Scholar] [CrossRef]
- Ychou, M.; Viret, F.; Kramar, A.; Desseigne, F.; Mitry, E.; Guimbaud, R.; Delpero, J.R.; Rivoire, M.; Quénet, F.; Portier, G.; et al. Tritherapy with fluorouracil/leucovorin, irinotecan and oxaliplatin (FOLFIRINOX): a phase II study in colorectal cancer patients with non-resectable liver metastases. Cancer Chemother. Pharmacol. 2007, 62, 195–201. [Google Scholar] [CrossRef]
- Chrabaszcz, S.; Rajeev, R.M.; Witmer, H.D.M.; Dhiman, A.M.; Klooster, B.; Gamblin, T.C.M.; Banerjee, A.; Johnston, F.M.M.; Turaga, K.K. A Systematic Review of Conversion to Resectability in Unresectable Metastatic Colorectal Cancer Chemotherapy Trials. Am. J. Clin. Oncol. 2022, 45, 366–372. [Google Scholar] [CrossRef] [PubMed]
- Karaoğlan, B.B.; Öz, D.K.; Araz, M.S.; Akyol, C.; Utkan, G. Advancements in the Management of Synchronous Colorectal Liver Metastases: A Comprehensive Review of Surgical, Systemic, and Local Treatment Modalities. Curr. Oncol. Rep. 2024, 26, 791–803. [Google Scholar] [CrossRef] [PubMed]
- Wagman, L.D. Importance of Response to Neoadjuvant Therapy in Patients With Liver-Limited mCRC When the Intent Is Resection and/or Ablation. Clin. Color. Cancer 2013, 12, 223–232. [Google Scholar] [CrossRef]
- Damato, A.; Ghidini, M.; Dottorini, L.; Tomasello, G.; Iaculli, A.; Ghidini, A.; Luciani, A.; Petrelli, F. Chemotherapy Duration for Various Indications in Colorectal Cancer: a Review. Curr. Oncol. Rep. 2023, 25, 341–352. [Google Scholar] [CrossRef]
- Bond, M.J.G.; Bolhuis, K.; Loosveld, O.J.L.; de Groot, J.W.B.; Droogendijk, H.; Helgason, H.H.; Hendriks, M.P.; Klaase, J.M.; Kazemier, G.; Liem, M.S.L.; et al. First-line systemic treatment strategies in patients with initially unresectable colorectal cancer liver metastases (CAIRO5): an open-label, multicentre, randomised, controlled, phase 3 study from the Dutch Colorectal Cancer Group. Lancet Oncol. 2023, 24, 757–771. [Google Scholar] [CrossRef]
- D’angelica, M.; Kornprat, P.; Gonen, M.; Chung, K.-Y.; Jarnagin, W.R.; DeMatteo, R.P.; Fong, Y.; Kemeny, N.; Blumgart, L.H.; Saltz, L.B. Lack of Evidence for Increased Operative Morbidity After Hepatectomy with Perioperative Use of Bevacizumab: A Matched Case-Control Study. Ann. Surg. Oncol. 2006, 14, 759–765. [Google Scholar] [CrossRef]
- Reddy, S.K.; Morse, M.A.; Hurwitz, H.I.; Bendell, J.C.; Gan, T.J.; Hill, S.E.; Clary, B.M. Addition of Bevacizumab to Irinotecan- and Oxaliplatin-Based Preoperative Chemotherapy Regimens Does Not Increase Morbidity after Resection of Colorectal Liver Metastases. J. Am. Coll. Surg. 2008, 206, 96–106. [Google Scholar] [CrossRef]
- Okines, A.; del Puerto, O.; Cunningham, D.; Chau, I.; Van Cutsem, E.; Saltz, L.; Cassidy, J. Surgery with curative-intent in patients treated with first-line chemotherapy plus bevacizumab for metastatic colorectal cancer First BEAT and the randomised phase-III NO16966 trial. Br. J. Cancer 2009, 101, 1033–1038. [Google Scholar] [CrossRef]
- Kesmodel, S.B.; Ellis, L.M.; Lin, E.; Chang, G.J.; Abdalla, E.K.; Kopetz, S.; Vauthey, J.-N.; Rodriguez-Bigas, M.A.; Curley, S.A.; Feig, B.W. Preoperative Bevacizumab Does Not Significantly Increase Postoperative Complication Rates in Patients Undergoing Hepatic Surgery for Colorectal Cancer Liver Metastases. J. Clin. Oncol. 2008, 26, 5254–5260. [Google Scholar] [CrossRef]
- Tamandl D, Gruenberger B, Klinger M, et al. Liver resection remains a safe procedure after neoadjuvant chemotherapy including bevacizumab: a case-controlled study. Ann Surg 2010, 252, 124. [CrossRef]
- A Wicherts, D.; de Haas, R.J.; Sebagh, M.; Corrales, E.S.; Gorden, D.L.; Lévi, F.; Paule, B.; Azoulay, D.; Castaing, D.; Adam, R. Impact of bevacizumab on functional recovery and histology of the liver after resection of colorectal metastases. Br. J. Surg. 2010, 98, 399–407. [Google Scholar] [CrossRef] [PubMed]
- Van Der Pool, A.E.; Marsman, H.A.; Verheij, J.; Ten Kate, F.J.; Eggermont, A.M.; Ijzermans, J.N.; Verhoef, C. Effect of bevacizumab added preoperatively to oxaliplatin on liver injury and complications after resection of colorectal liver metastases. J. Surg. Oncol. 2012, 106, 892–897. [Google Scholar] [CrossRef] [PubMed]
- A Wicherts, D.; de Haas, R.J.; Andreani, P.; Sotirov, D.; Salloum, C.; Castaing, D.; Adam, R.; Azoulay, D. Impact of portal vein embolization on long-term survival of patients with primarily unresectable colorectal liver metastases. Br. J. Surg. 2010, 97, 240–250. [Google Scholar] [CrossRef]
- Zorzi, D.; Chun, Y.S.; Madoff, D.C.; Abdalla, E.K.; Vauthey, J.-N. Chemotherapy With Bevacizumab Does Not Affect Liver Regeneration After Portal Vein Embolization in the Treatment of Colorectal Liver Metastases. Ann. Surg. Oncol. 2008, 15, 2765–2772. [Google Scholar] [CrossRef]
- O’connell, R.M.; Hoti, E. Challenges and Opportunities for Precision Surgery for Colorectal Liver Metastases. Cancers 2024, 16, 2379. [Google Scholar] [CrossRef]
- Folprecht, G.; Grothey, A.; Alberts, S.; Raab, H.-R.; Köhne, C.-H. Neoadjuvant treatment of unresectable colorectal liver metastases: correlation between tumour response and resection rates. Ann. Oncol. 2005, 16, 1311–1319. [Google Scholar] [CrossRef]
- Chrabaszcz, S.; Rajeev, R.M.; Witmer, H.D.M.; Dhiman, A.M.; Klooster, B.; Gamblin, T.C.M.; Banerjee, A.; Johnston, F.M.M.; Turaga, K.K. A Systematic Review of Conversion to Resectability in Unresectable Metastatic Colorectal Cancer Chemotherapy Trials. Am. J. Clin. Oncol. 2022, 45, 366–372. [Google Scholar] [CrossRef]
- Ychou, M.; Rivoire, M.; Thezenas, S.; Guimbaud, R.; Ghiringhelli, F.; Mercier-Blas, A.; Mineur, L.; Francois, E.; Khemissa, F.; Chauvenet, M.; et al. Chemotherapy (doublet or triplet) plus targeted therapy by RAS status as conversion therapy in colorectal cancer patients with initially unresectable liver-only metastases. The UNICANCER PRODIGE-14 randomised clinical trial. Br. J. Cancer 2022, 126, 1264–1270. [Google Scholar] [CrossRef]
- Tournigand, C.; André, T.; Achille, E.; Lledo, G.; Flesh, M.; Mery-Mignard, D.; Quinaux, E.; Couteau, C.; Buyse, M.; Ganem, G.; et al. FOLFIRI Followed by FOLFOX6 or the Reverse Sequence in Advanced Colorectal Cancer: A Randomized GERCOR Study. J. Clin. Oncol. 2004, 22, 229–237. [Google Scholar] [CrossRef]
- Yamazaki, K.; Nagase, M.; Tamagawa, H.; Ueda, S.; Tamura, T.; Murata, K.; Nakajima, T.E.; Baba, E.; Tsuda, M.; Moriwaki, T.; et al. Randomized phase III study of bevacizumab plus FOLFIRI and bevacizumab plus mFOLFOX6 as first-line treatment for patients with metastatic colorectal cancer (WJOG4407G). Ann. Oncol. 2016, 27, 1539–1546. [Google Scholar] [CrossRef]
- Bokemeyer, C.; Van Cutsem, E.; Rougier, P.; Ciardiello, F.; Heeger, S.; Schlichting, M.; Celik, I.; Köhne, C.-H. Addition of cetuximab to chemotherapy as first-line treatment for KRAS wild-type metastatic colorectal cancer: Pooled analysis of the CRYSTAL and OPUS randomised clinical trials. Eur. J. Cancer 2012, 48, 1466–1475. [Google Scholar] [CrossRef] [PubMed]
- Van Cutsem, E.; Köhne, C.-H.; Hitre, E.; Zaluski, J.; Chien, C.-R.C.; Makhson, A.; D’Haens, G.; Pintér, T.; Lim, R.; Bodoky, G.; et al. Cetuximab and Chemotherapy as Initial Treatment for Metastatic Colorectal Cancer. N. Engl. J. Med. 2009, 360, 1408–1417. [Google Scholar] [CrossRef] [PubMed]
- Bokemeyer C, Bondarenko I, Makhson A, et al. Fluorouracil, leucovorin, and oxaliplatin with and without cetuximab in the first-line treatment of metastatic col orectal cancer. J Clin Oncol 2009, 27, 663. [CrossRef] [PubMed]
- Primrose, J.; Falk, S.; Finch-Jones, M.; Valle, J.; O'Reilly, D.; Siriwardena, A.; Hornbuckle, J.; Peterson, M.; Rees, M.; Iveson, T.; et al. Systemic chemotherapy with or without cetuximab in patients with resectable colorectal liver metastasis: the New EPOC randomised controlled trial. Lancet Oncol. 2014, 15, 601–611. [Google Scholar] [CrossRef]
- Bridgewater JA, Pugh SA, Maishman T, et al. Systemic chemotherapy with or without cetuximab in patients with resectable colorectal liver metastasis (New EPOC): long-term results of a multicentre, randomised, controlled, phase 3 trial. Lancet Oncol 2020, 21, 398. [CrossRef]
- Nordlinger, B.; Sorbye, H.; Glimelius, B.; Poston, G.J.; Schlag, P.M.; Rougier, P.; Bechstein, W.O.; Primrose, J.N.; Walpole, E.T.; Finch-Jones, M.; et al. Perioperative chemotherapy with FOLFOX4 and surgery versus surgery alone for resectable liver metastases from colorectal cancer (EORTC Intergroup trial 40983): a randomised controlled trial. Lancet 2008, 371, 1007–1016. [Google Scholar] [CrossRef]
- Morris, V.K.; Kennedy, E.B.; Baxter, N.N.; Benson, A.B.; Cercek, A.; Cho, M.; Ciombor, K.K.; Cremolini, C.; Davis, A.; Deming, D.A.; et al. Treatment of Metastatic Colorectal Cancer: ASCO Guideline. J. Clin. Oncol. 2023, 41, 678–700. [Google Scholar] [CrossRef]
- Kanemitsu, Y.; Mizusawa, J.; Inaba, Y.; Hamaguchi, T.; Shida, D.; Ohue, M.; Komori, K.; Shiomi, A.; Shiozawa, M.; Watanabe, J.; et al. Hepatectomy Followed by mFOLFOX6 Versus Hepatectomy Alone for Liver-Only Metastatic Colorectal Cancer (JCOG0603): A Phase II or III Randomized Controlled Trial. J. Clin. Oncol. 2021, 39, 3789–3799. [Google Scholar] [CrossRef]
| Trial Name | Authors | Publication Year | Key Findings/Important Data |
| New EPOC | Bridgewater JA, et al. [32] | 2020 | The multicenter, open label, randomized study found a detrimental effect on overall survival in patients with metastatic colorectal cancer, RAS wild type with resectable or suboptimal resectable liver metastases who received perioperative cetuximab. |
| FIRE-3 | Stintzing S, et al. [33] | 2015 | Comparison of FOLFIRI plus cetuximab vs. FOLFIRI plus bevacizumab in mCRC. The study highlighted that cetuximab significantly increased the rate of conversion to resectability compared to bevacizumab, especially in patients with RAS wild-type tumors. |
| COIN (Chemotherapy versus Chemotherapy plus Cetuximab) | Seymour MT, et al. [34] | 2007 | This trial assessed the addition of cetuximab to standard chemotherapy (FOLFOX) in mCRC patients. It demonstrated an improvement in progression-free survival (PFS) but did not show a major increase in resection rates for liver metastases. It highlighted the challenge in using cetuximab for conversion. |
| CRISTAL | Van Cutsem, et al. [35] | 2010 | Studied FOLFIRI plus cetuximab in RAS wild-type mCRC patients. It found that cetuximab improved overall survival and response rates and supported its role in conversion strategies for patients with limited metastatic spread. |
| OPTIMOX | Tournigand C, et al. [36] | 2006 | Investigated the use of oxaliplatin-based chemotherapy in mCRC, showing that alternating chemotherapy (OXALIPLATIN/FOLFOX) regimens led to significant tumor reduction, aiding in conversion to resectability in some patients. |
| PEAK | Schwartzberg LS, et al. [37] | 2014 | Focused on the combination of FOLFOX and bevacizumab in patients with liver-limited mCRC. It demonstrated that a high response rate with this regimen increased the likelihood of achieving resectability, especially in patients with isolated liver metastases. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





