1. Introduction
Mental foramen (MF) is an oval or circular opening located on the body of the mandible, typically equidistant from its superior and inferior borders. It serves as a passage for the mental nerve, artery and vein, playing a vital role in innervating the lower face, including the lower teeth, lip, labial mucosa and gingiva.
The accessory mental foramen (AMF), when present, is identified as a smaller opening located alongside the MF, typically positioned posterior to it/. The AMF plays a critical role, particularly during operating procedures, making it essential for surgeons to recognize its presence and morphology. Precise knowledge of the variations in the anatomy, shape, size, and position of the MF, along with the presence of the AMF, is invaluable for performing mandibular surgical procedures. These include filling treatments, premolar curettage, root canal therapy, dental implant placement, orthognathic and periapical surgeries, jaw surgeries, and the enucleation of pathologies in the mental region. Given the frequency of dental and maxillofacial procedures involving the mental region, it is imperative for dental practitioners to be well-informed about these anatomical details to prevent postoperative complications such as lip numbness, a significant consequence of improper handling or violation of the AMF [
1].
Saywer et al. demonstrated that the morphology, position, and incidence of AMFs vary among individuals and across ethnic groups [
2]. Additionally, the position of the MF differs between edentulous and dentate subjects [
3]. While many studies focus on dry mandibles, others have utilized data from Cone-Beam Computed Tomography (CBCT) and panoramic radiographs. Notably, linear measurements from CBCT have been shown to align closely with those obtained from dry mandibles using a digital caliper, the gold-standard method [
4]. CBCT measurements of MF size have also been validated for accuracy [
5]. However, comprehensive data on AMFs remain limited.
Although numerous observational studies, case series, and case reports have been published, a systematic review and meta-analysis focusing on dry mandibles has yet to be conducted. This study aims to assess the incidence and perform a morphological and morphometric analysis of AMFs in human dry mandibles from the Greek population, complemented by a systematic review and meta-analysis of available global data.
2. Materials and Methods
The present observational study was conducted on 114 dry adult human mandibles of unknown gender and age, derived from the osteological collection of the Anatomy Department, Democritus University of Thrace, Greece.
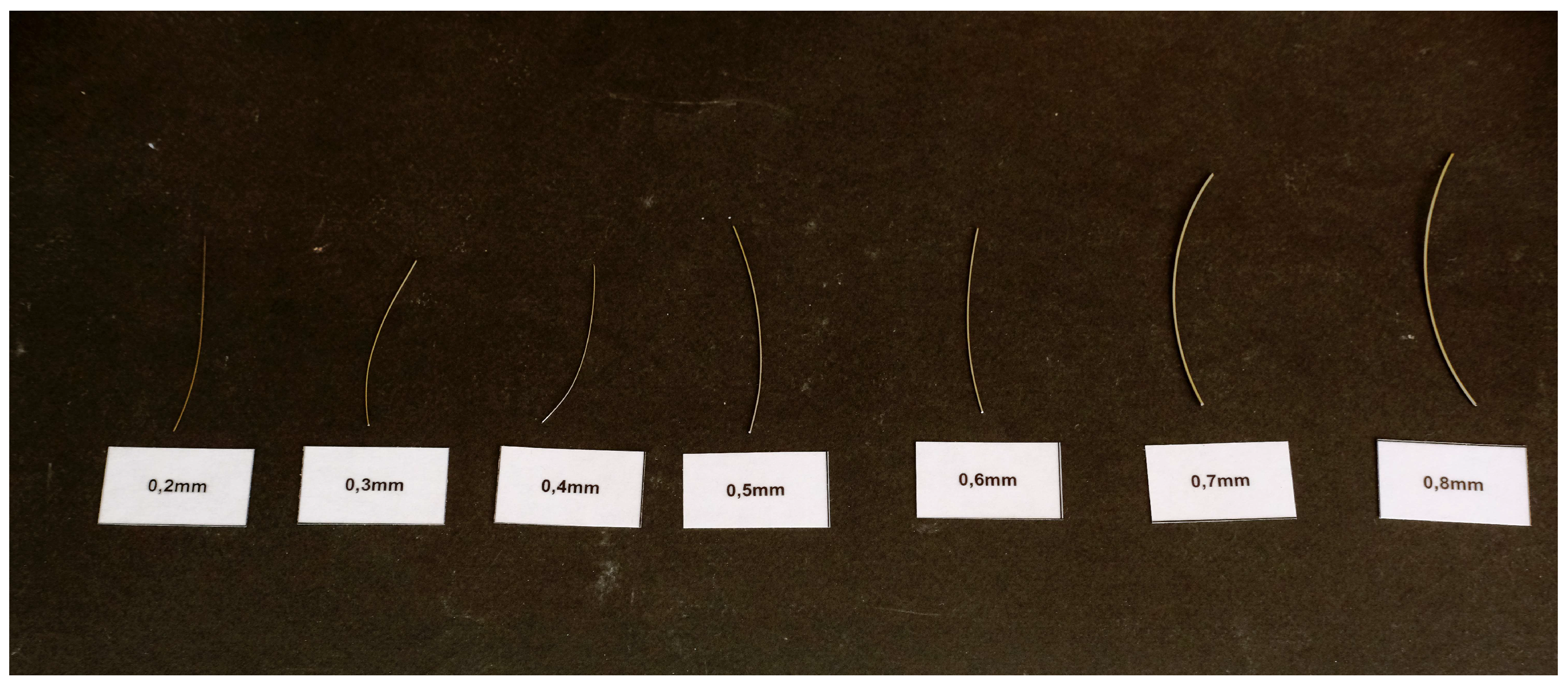
The study objectives were to measure the location, shape, incidence, diameter, as well as the distance between AMFs and MF, AMFs to the alveolar crest and AMFs to the inferior border in each mandible. For that purpose, we used a digimatic caliper (Mitutoyo Co., Japan) of 0.1 mm accuracy. Each distance was measured from the center of each foramen, either MF or AMF. The location of each AMF was determined using two imaginary lines (horizontal and vertical) intersecting at the MF, dividing the area into four quadrants: anterior superior, posterior superior, anterior inferior, and posterior inferior. The diameter of the AMF was measured using a single wire with a diameter ranging from 0.2 mm to 1.4 mm. For oval-shaped foramina, the horizontal distance was measured using up to two wires with diameters ranging from 0.02 mm to 3mm (
Figure 1).
All measurements were performed independently by two investigators. Inter-rater reliability assessment for categorical variables was assessed using the Cohen’s kappa estimates; in case of continuous variables, the intraclass correlation coefficients (ICC) estimates and their 95% confidence intervals (CI) based on a mean rating (n=2), absolute-agreement, two-way random model were alternatively applied. Means are accompanied by the relevant standard deviation (SD). Inter-rater reliability assessment for categorical variables was assessed using the Cohen’s kappa estimates; in case of continuous variables, the intraclass correlation coefficients (ICC) estimates and their 95% confidence intervals (CI) based on a mean rating (n=2), absolute-agreement, two-way random model were alternatively applied [
6]. Based on the 95% confident interval of the ICC estimate, values less than 0.5, between 0.5 and 0.75, between 0.75 and 0.9, and greater than 0.90 are indicative of poor, moderate, good, and excellent reliability, respectively [
7]. The level of statistical significance was set to p=0.05. The SPSS software (version 26.0.0.0) was used for statistical analysis
For the purpose of meta-analysis, we implemented the PRISMA 2020 statement guidelines [
8]. We used the search term “accessory mental foramen” in PubMed, Scopus, and Google Scholar databases to detect all publications reporting prevalence and morphology of AMF in dry mandibles. Inclusion and exclusion criteria followed the PICOTS framework (
Table 1).
Quality assessment was performed with the Johanna Briggs Institute (JBI) Critical Appraisal Checklist for analytical cross-sectional studies tool [
9].
All data regarding author, year of publication, origin of population studied, sample size, number of cases presenting AMF, number of cases presenting unilateral AMF, number of cases presenting bilateral AMF, number of total AMFs detected, number of AMFs detected on the right side, number of AMFs detected on the left side, number of single AMFs, number of multiple AMFs, number of round-shaped AMFs, number of oval-shaped AMFs, diameter in mm (if round) or vertical axis in mm (if oval), distance from MF in mm, distance from alveolar ridge in mm, and distance from mandible lower border were recorded. Quantitative synthesis were performed in case that data were available from ≥5 sources.
All steps including literature search, records screening, and data extraction were performed independently by two authors (Z-M.T., and C.T.). In case of dispute, a third author (V.P.) was responsible for the final judgment.
Data were synthesized using STATA 18 Statistical Software version. Prevalence data were combined using the random-effects REML model after Freeman-Tuckey double arcsine transformation. Combination of means and standard deviations (SDs) were performed using the freely available online tool located at
https://www.statstodo.com/CombineMeansSDs.php.
Heterogeneity was approached using the Q test and I
2 statistic; Q test P value < 0.10 was indicative of a statistically significant result. Furthermore, a value of I
2≤ 25% was indicative of insignificant heterogeneity, 26%-50% of low heterogeneity, 51%-75% of moderate heterogeneity, and > 75% of high heterogeneity [
13,
14]. Sensitivity analysis was performed using the leave-one-out procedure to investigate the effect of each included study on heterogeneity.
3. Results
3.1. Our data
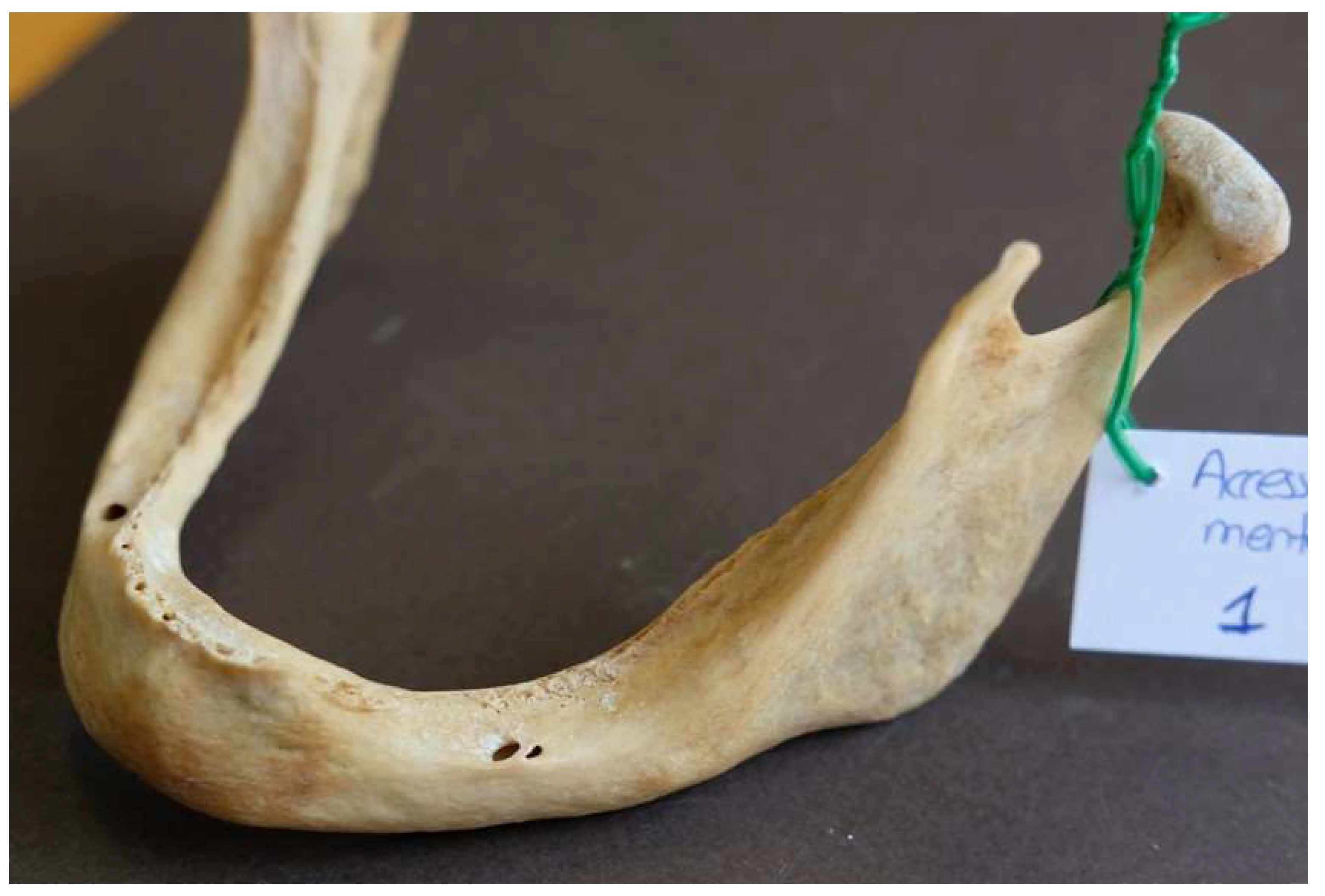
According to our data, the MF was present in all observed mandibles and it was bilateral. Nine AMFs were found in 7 mandibles (5 single, 2 double), all unilateral; 5 AMFs were located at the right hemimandible and 4 at the left (
Figure 2).
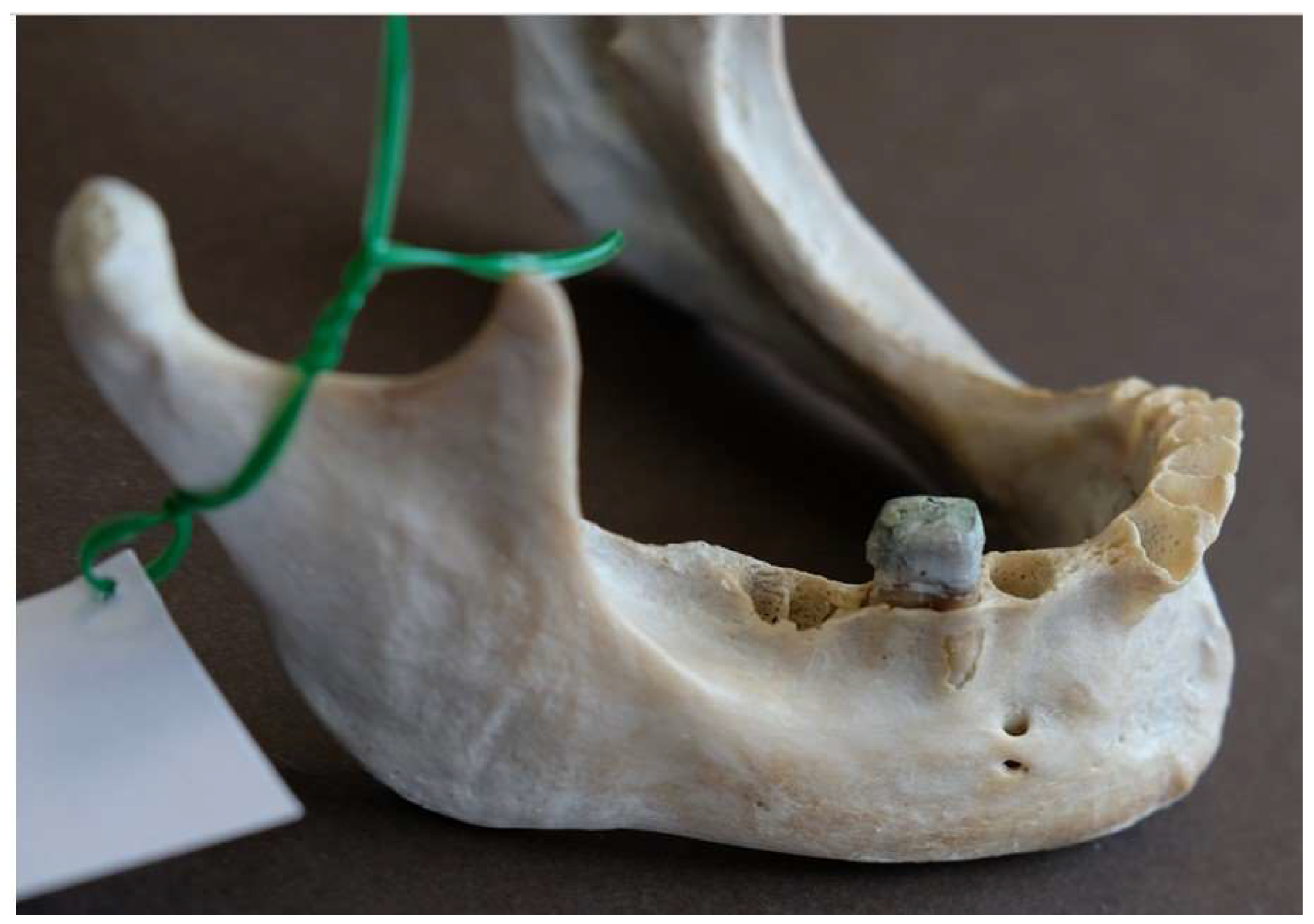
As far as the shape of AMFs is concerned, 5 were round and 4 oval (
Figure 3).
As far as the location of the AMFs is concerned, 6 AMFs were located posterior and 3 anterior to MF (
Figure 4).
Additionally, four AMFs were located inferior to the MF, three superior to it, and two at the same horizontal level as the MF (
Figure 5).
AMFs presented 0.96±0.43 mm mean diameter, ranging from 0.40 to 1.70 mm (
Figure 6).
Additionally, AMFs presented 4.12±2.15 mm mean distance from MF, ranging from 3.20 to 17.72 mm (
Figure 7).
Of note, AMFs were measured to be located 12.68 ± 4.10 mm from alveolar ridge, and 11.92 ± 1.57 mm from mandible lower border (
Table 2).
Lastly, in one mandible, the AMF was located at the same horizontal level as the MF but did not fall within any quadrant (
Table 3).
Considerable interrater agreement was observed for all measurements (
Table 4).
3.2. Meta-analysis
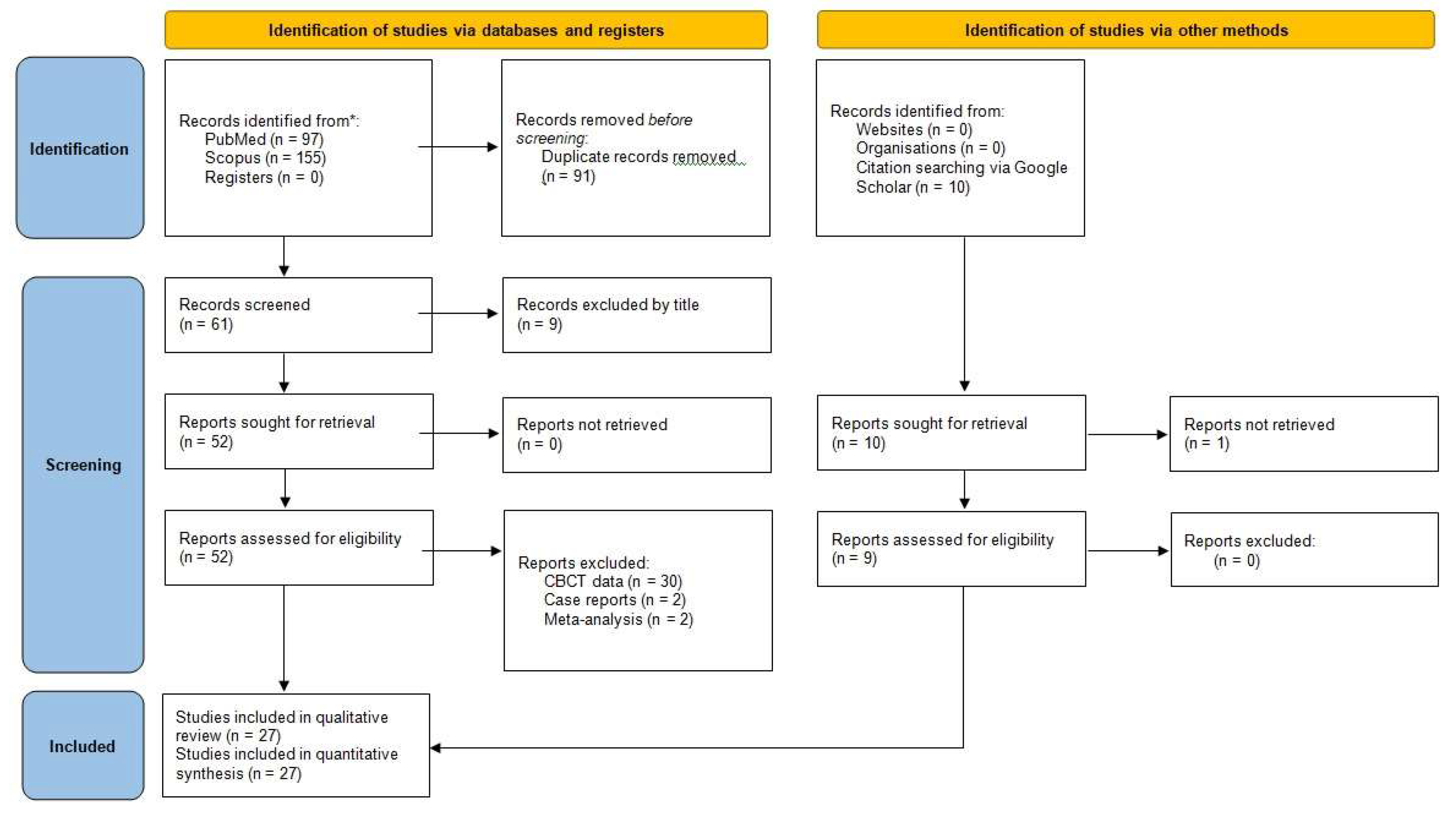
For the purpose of the meta-analysis, 252 publications were identified from search in PubMed and Scopus databases; ten additional publications were retrieved through citation searching (
Figure 8).
After screening, 27 publications were included in qualitative review and in quantitative synthesis, along with data obtained from the present observational study (
Table 5;
Table 6).
The quality assessment is presented in detail as depicted in
Table 7. In detail, 8 domains were assessed using respective questions (Q1-Q8), as follows: Q1: “Were the criteria for inclusion in the sample clearly defined?”; Q2: “Were the study subjects and the setting described in detail?”; Q3: “Was the exposure measured in a valid and reliable way?”; Q4: “Were objective, standard criteria used for measurement of the condition?”; Q5: “Were confounding factors identified?”; Q6: “Were strategies to deal with confounding factors stated?”; Q7: “Were the outcomes measured in a valid and reliable way?”; Q8: “Was appropriate statistical analysis used?”. The response options were recorded as “Yes” (Y), “No” (N), “Unclear (U)”, and “Not Applicable” (NA).
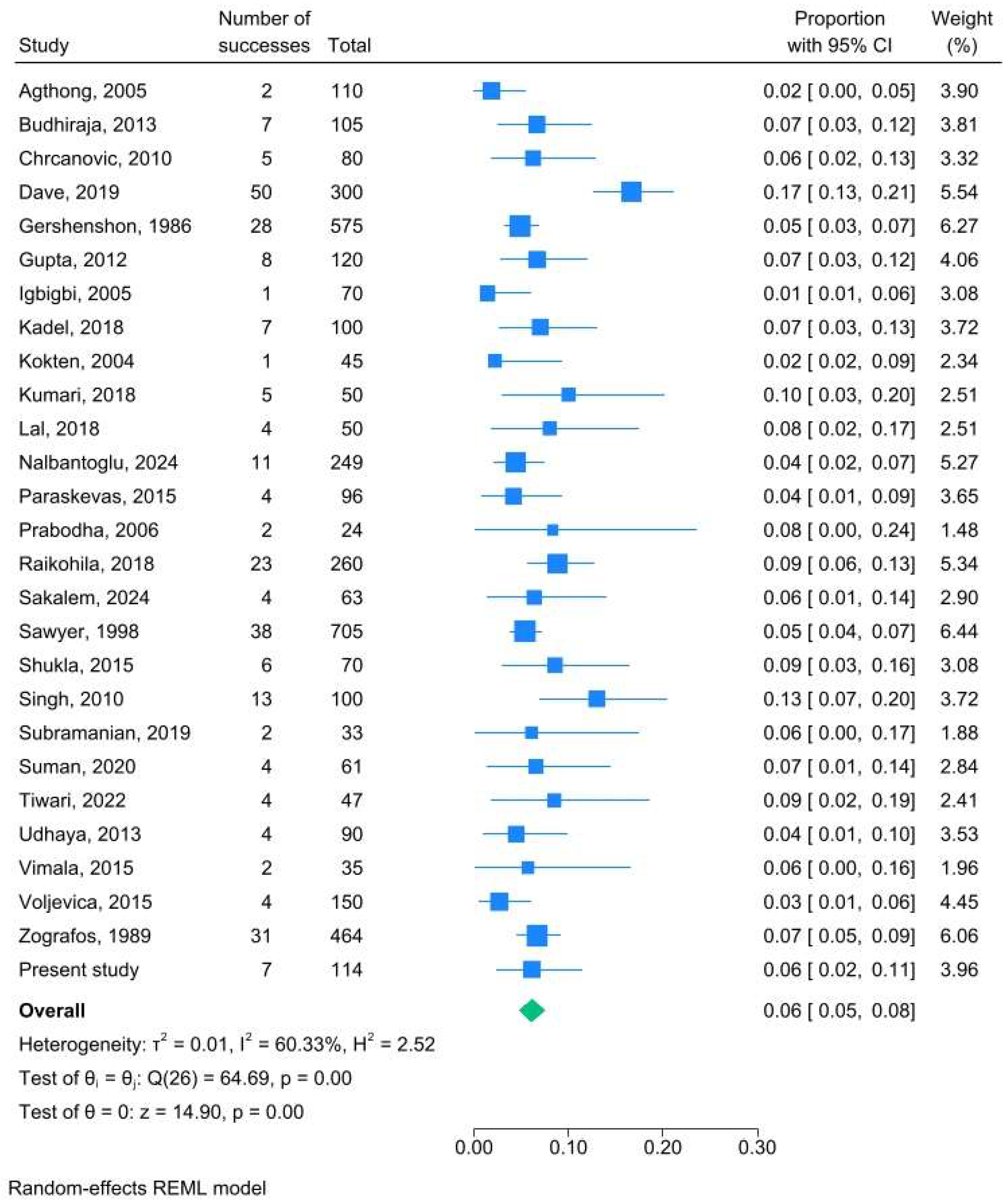
The combined AMF prevalence was 6.1% (95% CI: 4.8% - 7.6%; I
2 60%) (
Figure 9).
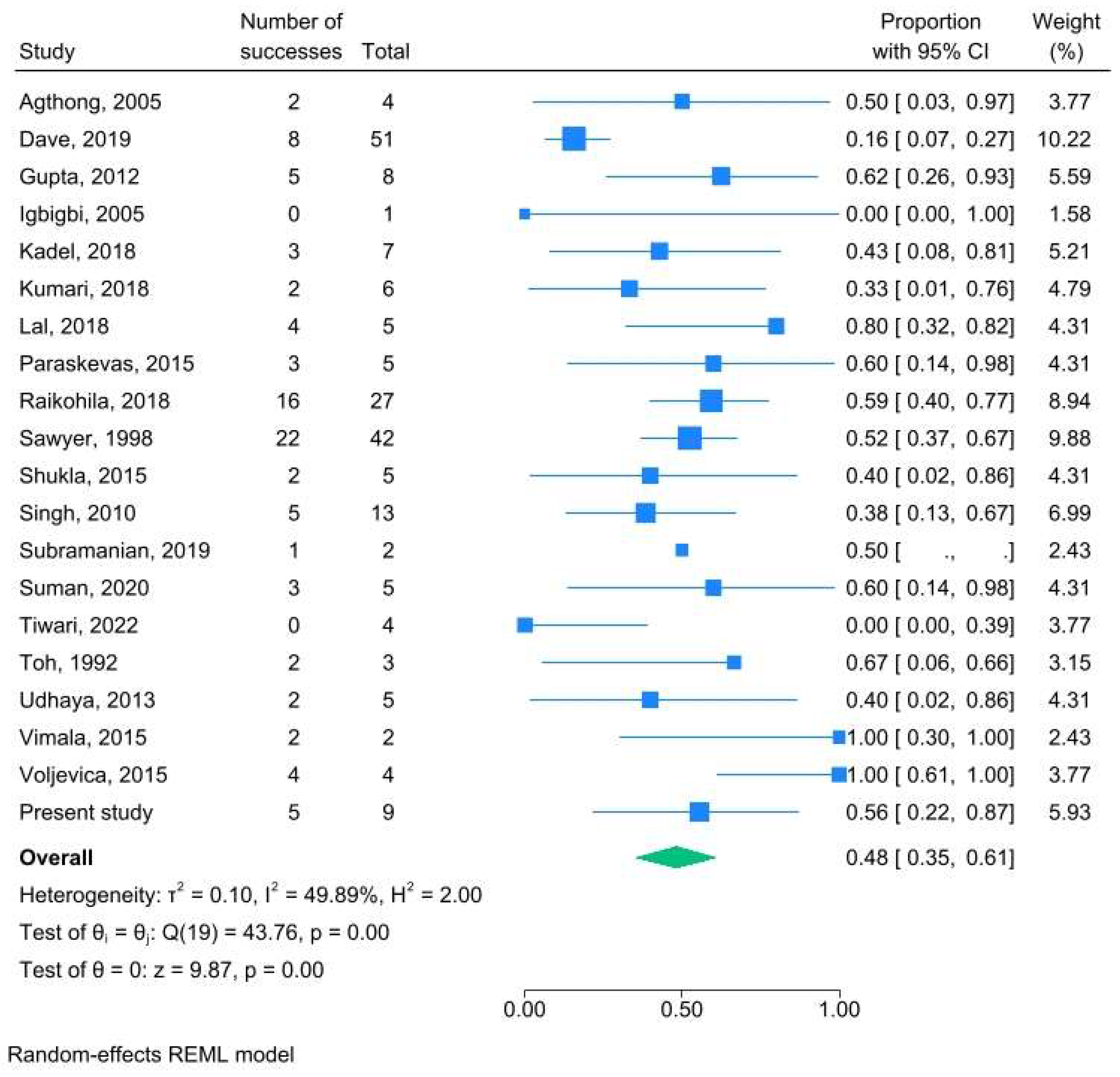
AMF were detected in 48.2% (95% CI: 35.2% - 61.2%; I
2 50%) on the right side (
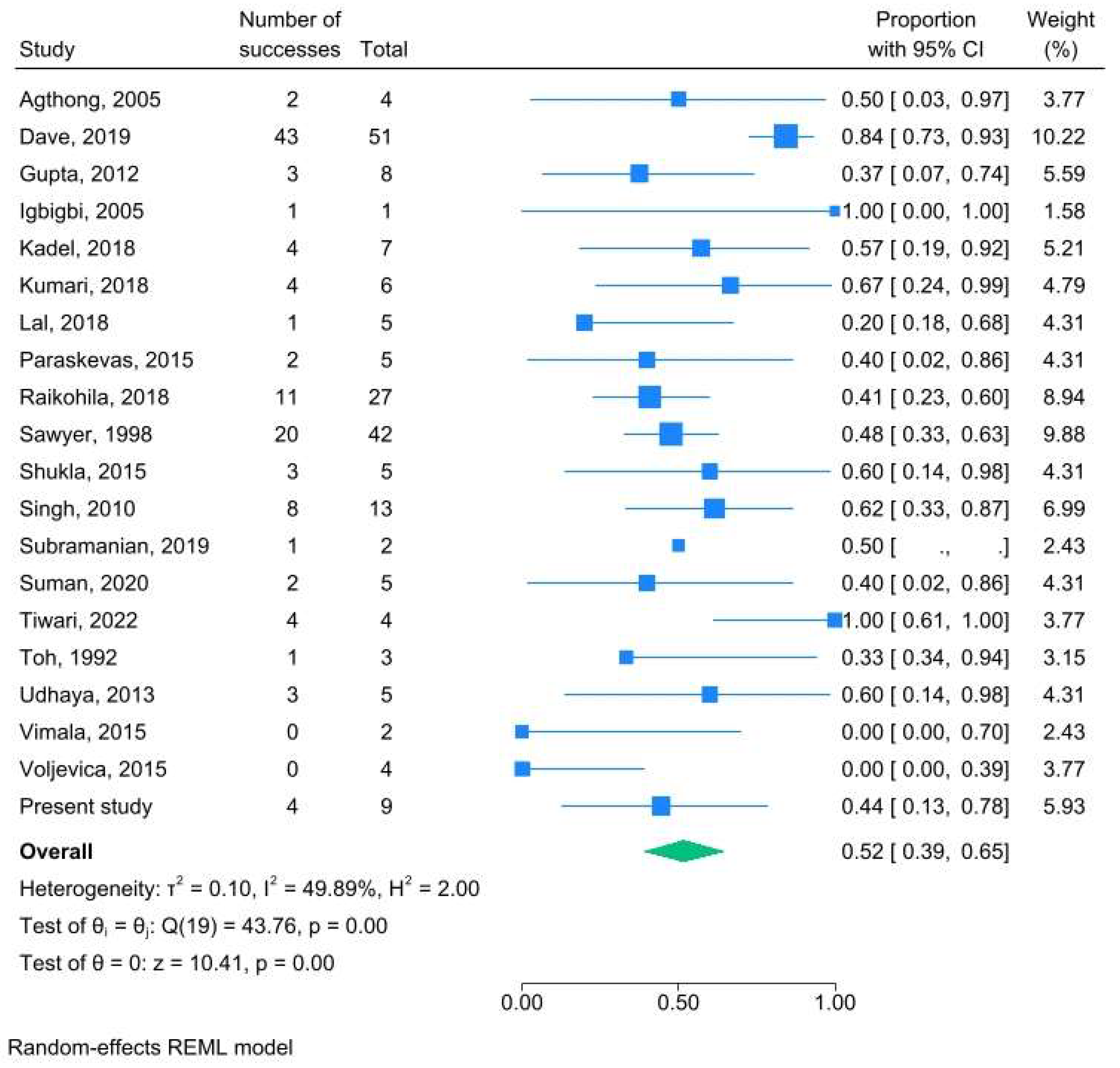
Figure 10), and in 51.8% (95% CI: 38.8% - 64.8%; I
2 50%) on the left side (
Figure 11); no difference was documented as CIs referring to both sides overlapped.
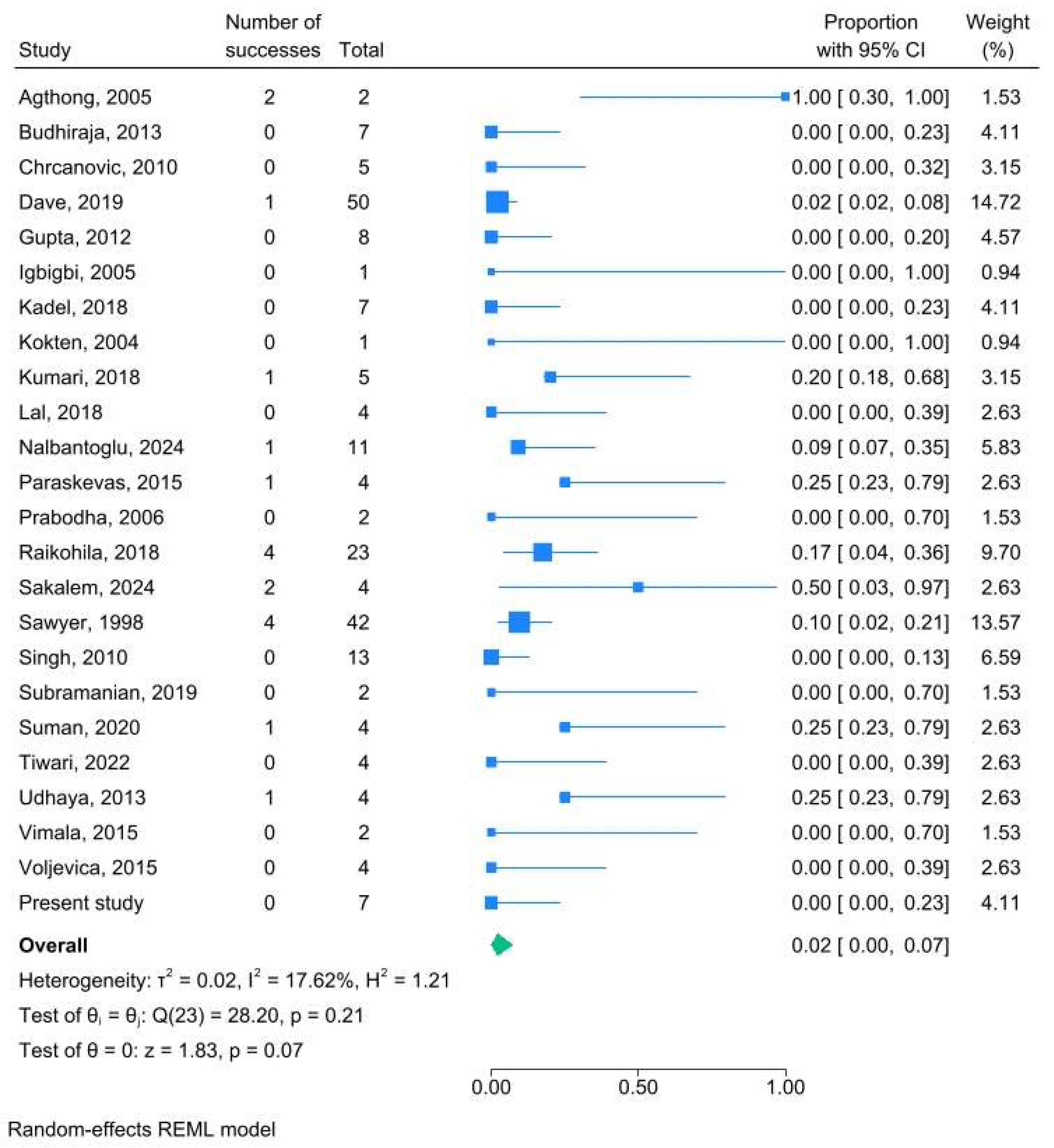
The combined mean vertical axis was 1.18 ± 0.61 mm, and the combined mean distance from MF was 3.64 ± 2.29 mm. Bilateral AMFs were detected in 2.1% of AMF cases (95% CI: 0.0% - 7.3%; I
2 18%) (
Figure 12).
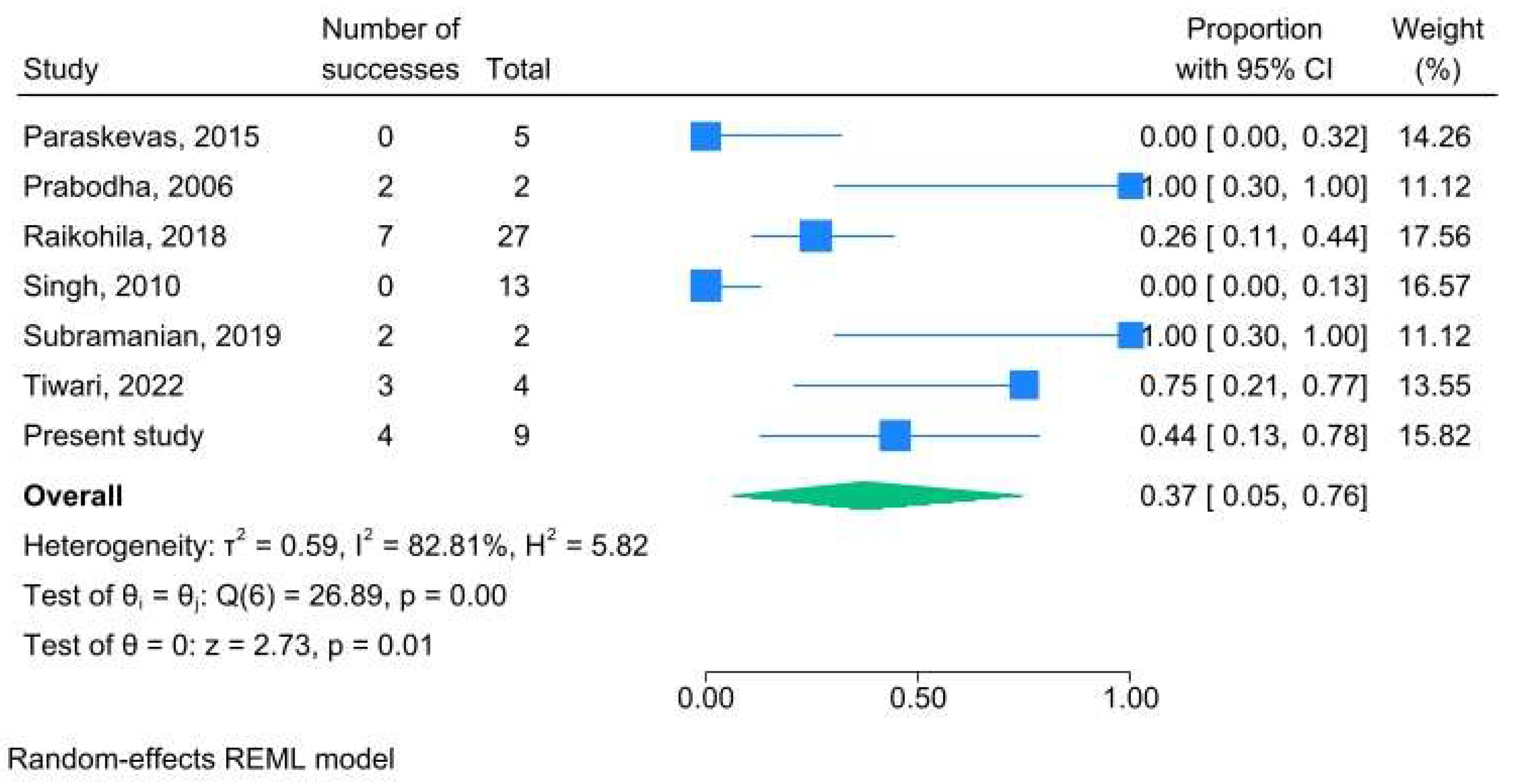
Oval shape was described in 37.0% of AMFs (95% CI: 5.1% - 75.8%; I
2 83%) (
Figure 13).
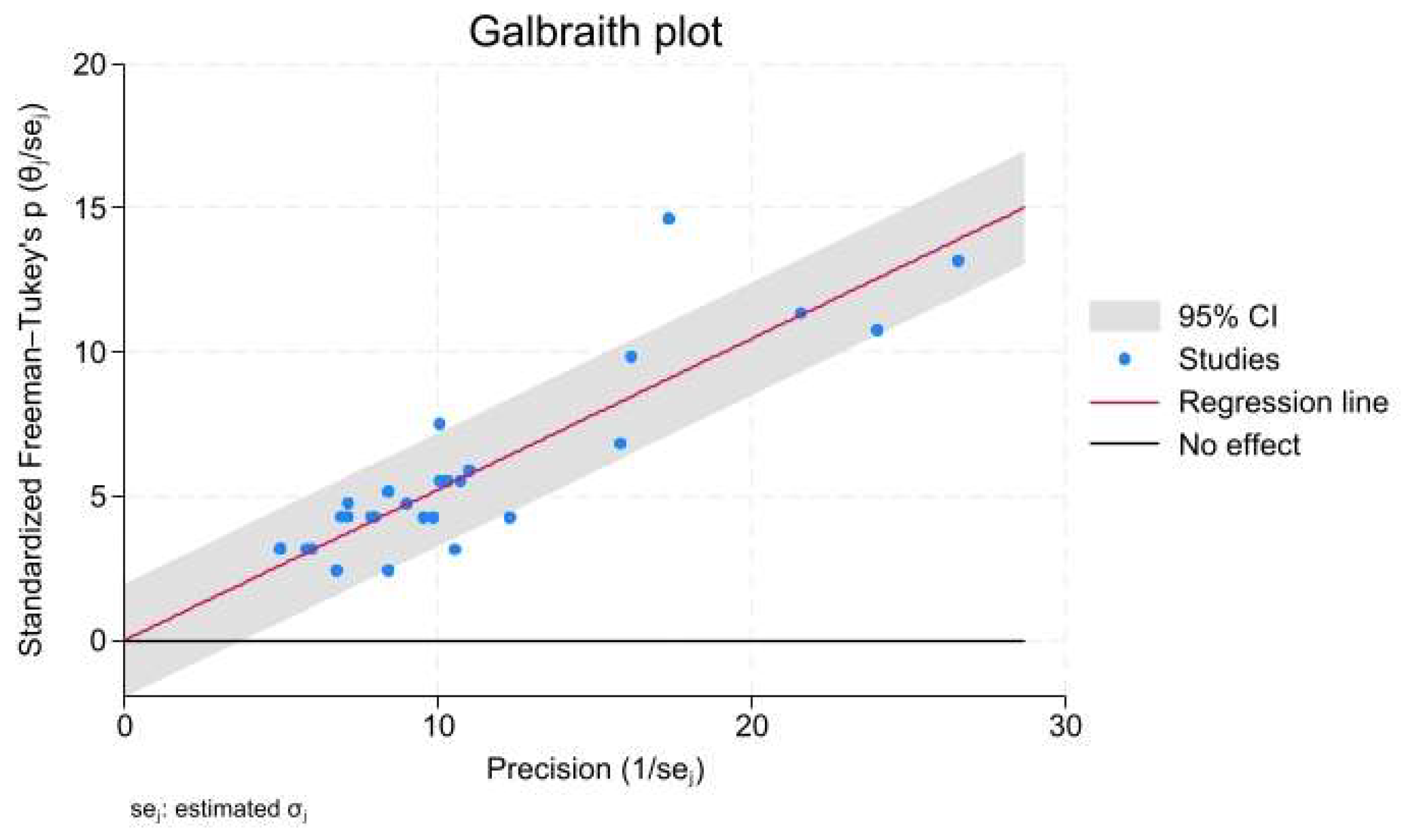
All but one study were close to the 95% confidence intervals of the Galbraith plot (
Figure 14).
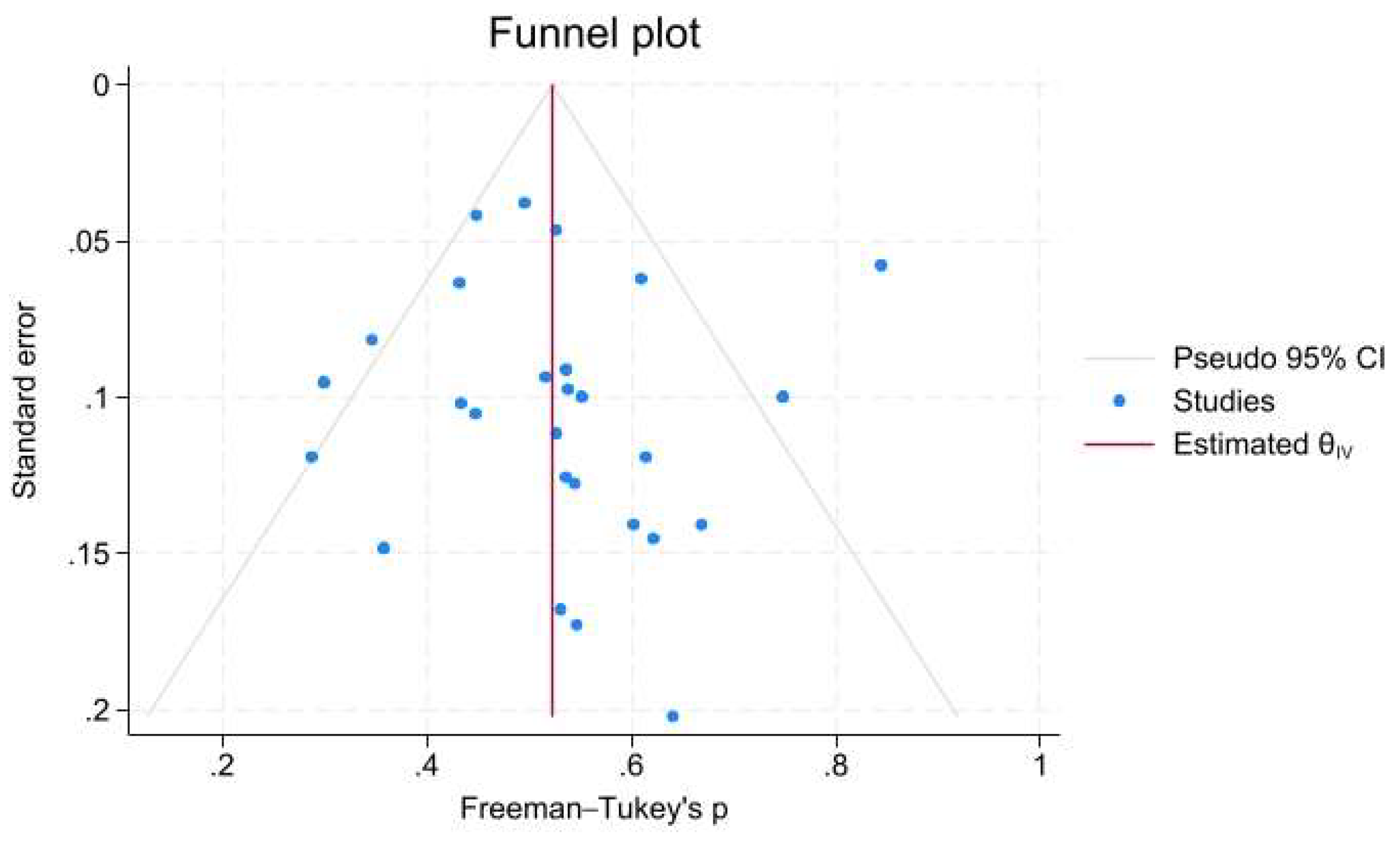
No significant publication bias was detected; the funnel plot was symmetrical by visual inspection. Moreover, no additional study was imputed using the trim-and-fill method on either side (
Figure 15); both Egger’s and Begg’s test yielded a non-significant result (p=0.914, and 0.234, respectively).
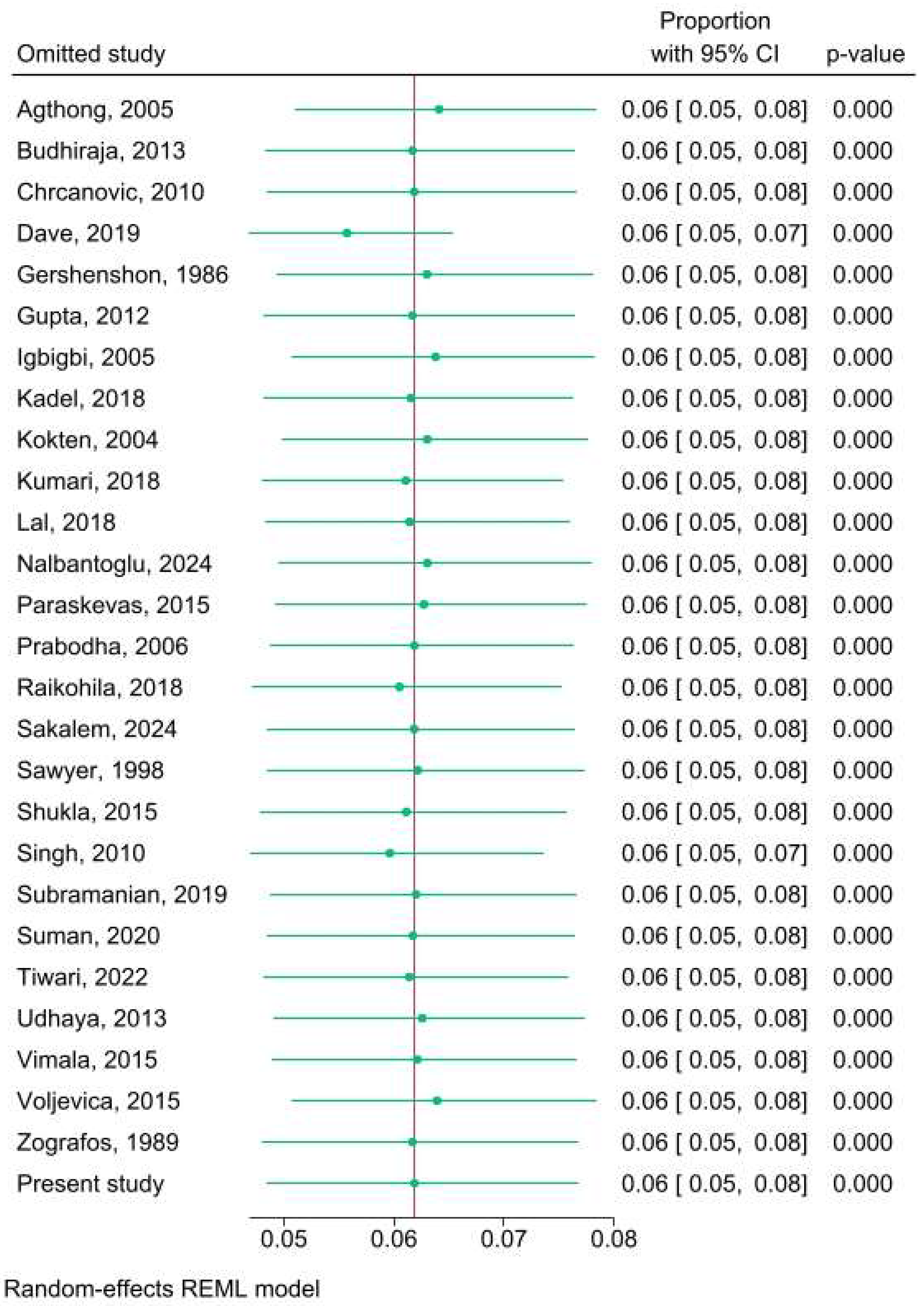
The leave-one-out sensitivity analysis revealed no critical effect on combined mean prevalence due to single publications (
Figure 16).
4. Discussion
This observational study investigates the location, shape, and dimensions of AMFs in dry adult human mandibles and, apart from the presentation of our own data, includes a systematic review and meta-analysis of worldwide data. Notably, this is the first meta-analysis focusing on AMF data obtained exclusively from dry mandibles. In contrast, three previously published meta-analyses primarily rely on CBCT data [41-43].
Our data is in keeping with the results of the consequent meta-analysis, thus rendering them credible and representative. Of note, we reported that the combined AMF prevalence is 6.1% (95% CI: 4.8% - 7.6%), and that there is no difference between right and left side. Moreover, AMFs were mostly rounded, while oval shape was described in 37.0% of cases; the combined mean AMF vertical axis was 1.18 ± 0.61 mm, and the combined mean distance from MF was 3.64 ± 2.29 mm. Lastly, AMFs were detected bilaterally in 2.1% of cases. The heterogeneity of our results, measured as I2, ranged from unimportant to considerable, reaching 83% in case of AMF shape determination.
In this study, we assessed AMF locations by measuring distances from the AMFs to both the alveolar crest and the inferior border of the mandible. The latter measurement is considered more reliable, as it remains consistent regardless of whether the mandible is dentate or edentulous. In contrast, the distance between the AMF and the alveolar ridge can change due to resorption of the alveolar ridge with age [
3].
The presence of AMF is a critical consideration in surgical procedures involving the mental region. These additional foramina house nerves and blood vessels that, if damaged during surgery, can result in complications such as lower lip numbness or bleeding. Consequently, understanding the location and content of AMFs is essential for planning and executing safe and effective surgical interventions. In their hallmark paper, Rahpeyma and Khajehahmadi have highlighted the impact of AMFs on the outcomes of various surgical procedures, including orthognathic, periapical, implant, inferior alveolar nerve repositioning, and trauma surgeries. This underscores the importance of incorporating AMF considerations into surgical planning to minimize complications and optimize patient outcomes [
44].
The influence of AMFs on local anesthesia is another important aspect to consider. Their presence can affect the success of mental nerve blocks. If an AMF is located near the main mental foramen, a single anesthetic injection into the main foramen may suffice, as the anesthetic can diffuse into the AMF. However, if an AMF is located farther from the main foramen, an additional injection may be necessary to ensure effective anesthesia. Recognizing these anatomical variations allows dental professionals and anesthesiologists to tailor their techniques, ensuring patient comfort and procedural success.
The major strength of this study is its integration of primary data from the well-established osteological collection of the Anatomy Department at Democritus University of Thrace, Greece, with data from a systematic review and meta-analysis. To our knowledge, this is the first study of its kind. However, a certain limitation of the study is that the total heterogeneity, mostly attributable to ethnic-related variation, could not be further assessed, due to the lack of gender-specific information. Future research incorporating subgroup analyses or meta-regression could explore potential gender-related differences in AMF anatomy.
5. Conclusions
Dental surgeons must have a comprehensive understanding of the anatomical variations in the mental foramen (MF) and the potential presence of accessory mental foramina (AMFs). This knowledge is essential to prevent or mitigate the risk of postoperative complications such as pain, anesthesia, injury, and other adverse outcomes. By incorporating this anatomical insight into surgical and anesthetic planning, clinicians can enhance patient safety and procedural success.
Author Contributions
Conceptualization, Z-M.T., and V.P.; methodology, Z-M.T., C.T., and V.P.; software, V.P.; validation, Z-M.T., C.T., and V.P.; formal analysis, V.P.; investigation, Z-M.T., C.T., and V.P.; resources, Z-M.T., C.T., and V.P.; data curation, V.P.; writing—original draft preparation, Z-M.T., and V.P.; writing—review and editing, Z-M.T., C.T., and V.P.; visualization, Z-M.T., C.T., and V.P.; supervision, V.P.; project administration, V.P.. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Ethical review and approval were waived due to the use of cadaveric material.
Informed Consent Statement
Not applicable.
Data Availability Statement
Acknowledgments
Not applicable.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Montagu, MF. The direction and position of the mental foramen in the great apes and man. Am J Phys Anthropol. 1954, 12, 503–18. [Google Scholar] [CrossRef] [PubMed]
- Sawyer DR, Kiely ML, Pyle MA. The frequency of accessory mental foramina in four ethnic groups. Arch Oral Biol. 1998, 43, 417–20. [Google Scholar] [CrossRef] [PubMed]
- Charalampakis A, Kourkoumelis G, Psari C, Antoniou V, Piagkou M, Demesticha T, Kotsiomitis E, Troupis T. The position of the mental foramen in dentate and edentulous mandibles: clinical and surgical relevance. Folia Morphol (Warsz). 2017, 76, 709–714. [Google Scholar] [CrossRef]
- Almeida VSM, Bomfim RT, Sobreira ACR, Barbosa IDS, Leite-Ribeiro PM, Rubira-Bullen IR, Sarmento VA. Linear measurement accuracy of CBCT panoramic reconstructions: experimental study with dry human mandibles. Oral Radiol. 2021, 37, 421–426. [Google Scholar] [CrossRef]
- Ahmed AA, Ahmed RM, Jamleh A, Spagnuolo G. Morphometric Analysis of the Mandibular Canal, Anterior Loop, and Mental Foramen: A Cone-Beam Computed Tomography Evaluation. Int J Environ Res Public Health. 2021, 18, 3365. [Google Scholar] [CrossRef]
- Hallgren, KA. Computing Inter-Rater Reliability for Observational Data: An Overview and Tutorial. Tutor Quant Methods Psychol. 2012, 8, 23–34. [Google Scholar] [CrossRef] [PubMed]
- Koo TK, Li MY. A Guideline of Selecting and Reporting Intraclass Correlation Coefficients for Reliability Research. J Chiropr Med. 2016, 15, 155–63. [Google Scholar] [CrossRef]
- Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P, Moher D. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021, 372, n71. [Google Scholar]
- Ma LL, Wang YY, Yang ZH, Huang D, Weng H, Zeng XT. Methodological quality (risk of bias) assessment tools for primary and secondary medical studies: what are they and which is better? Mil Med Res. 2020, 7, 7. [Google Scholar]
- Wan X, Wang W, Liu J, Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. 2014, 14, 135. [Google Scholar]
- Luo D, Wan X, Liu J, Tong T. Optimally estimating the sample mean from the sample size, median, mid-range, and/or mid-quartile range. Stat Methods Med Res. 2018, 27, 1785–1805. [Google Scholar] [CrossRef] [PubMed]
- Shi J, Luo D, Weng H, Zeng XT, Lin L, Chu H, Tong T. Optimally estimating the sample standard deviation from the five-number summary. Res Synth Methods. 2020, 11, 641–654. [Google Scholar] [CrossRef] [PubMed]
- Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002, 21, 1539–1558. [Google Scholar] [CrossRef] [PubMed]
- Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003, 327, 557–560. [Google Scholar] [CrossRef] [PubMed]
- Agthong S, Huanmanop T, Chentanez V. Anatomical variations of the supraorbital, infraorbital, and mental foramina related to gender and side. J Oral Maxillofac Surg. 2005, 63, 800–4. [Google Scholar] [CrossRef]
- Βudhiraja V, Rastogi R, Lalwani R, Goel P, Bose SC. Study of position, shape, and size of mental foramen utilizing various parameters in dry adult human mandibles from north India. ISRN Anat. 2012, 2013, 961429. [Google Scholar]
- Chrcanovic BR, Abreu MH, Custódio AL. Morphological variation in dentate and edentulous human mandibles. Surg Radiol Anat. 2011, 33, 203–13. [Google Scholar] [CrossRef]
- Dave UH, Gupta S, Astik R. Cross sectional analysis of positional and numerical variations of mental foramina in dry human mandibles. Indian J Clin Anat Physiol. 2019, 6, 81–84. [Google Scholar] [CrossRef]
- Gershenson A, Nathan H, Luchansky E. Mental foramen and mental nerve: changes with age. Acta Anat (Basel). 1986, 126, 21–8. [Google Scholar] [CrossRef]
- Gupta S, Soni JS. Study of anatomical variations and incidence of mental foramen and accessory mental foramen in dry human mandibles. Natl J Med Res. 2012, 2, 28–30. [Google Scholar]
- Igbigbi PS, Lebona S. The position and dimensions of the mental foramen in adult Malawian mandibles. West Afr J Med. 2005, 24, 184–9. [Google Scholar]
- Kadel M, Sedhain BP. Morphometric Analysis of Accessory Mental Foramen in Human Dry Mandibles. J Nepal Dent Assoc. 2018, 18, 17–20. [Google Scholar]
- Kokten G, Buyukanten M, Balcioglu HA (2004) Comparison of the diameter and the location of mental foramen in dry mandible and panoramic. J Istanbul Univ Fac Dent. 2024, 38, 65–71.
- Kumari R, Panchal P, Prasad A, Prasad B, Britto J. International Journal of Scientific Research. 2018, 7. Available at: https://www.worldwidejournals.com/international-journal-of-scientific-research-(IJSR)/article/incidence-of-accessory-mental-foramen-in-mandible-and-its-clinical-significance/MTM4MDQ=/?is=1&b1=61&k=16.
- Lal N, Mathur S, Joshi P. A study on incidence of Accessory Mental Foramen in Dry Human Mandibles of Rajasthan State. J Med Sci Clin Res. 2018, 6, 1049–1053. [Google Scholar]
- Nalbantoglu AM, Yanik D, Albay S. Location and Anatomic Characteristics of Mental Foramen in Dry Adult Human Mandibles. ADO Klinik Bilimler Dergisi. 2024, 13, 51–8. [Google Scholar] [CrossRef]
- Paraskevas G, Mavrodi A, Natsis K. Accessory mental foramen: an anatomical study on dry mandibles and review of the literature. Oral Maxillofac Surg. 2015, 19, 177–81. [Google Scholar] [CrossRef]
- Prabodha LBL, Nanayakkara BG. The position, dimensions and morphological variations of mental foramen in mandibles. Galle Med J. 2006, 11, 13–15. [Google Scholar]
- Rajkohila J, Daniel P, Ambikaipakan S, Rabi S. Morphological and morphometric analysis of accessory mental foramen in dry human mandibles of south indian population. Indian J Dent Res. 2018, 29, 56–60. [Google Scholar] [CrossRef]
- Sakalem ME, Sestario CS, Motta AL, Quintilhano D, Myszynski SL, Sato VAH. Anatomical variations of the human mandible and prevalence of duplicated mental and mandibular foramina in the collection of the State University of Londrina. Transl Res Anat. 2024, 37, 100357. [Google Scholar]
- Shukla RK, Gupta P, Hussein M, Hussain F, Singh AB. Morphometric measurement of mental foramen in dry human mandible in north Indian population. Int J Anat Res. 2015, 3, 899–905. [Google Scholar] [CrossRef]
- Singh R, Srivastav AK. Study of position, shape, size and incidence of mental foramen and accessory mental foramen in Indian adult human skulls. Int J Morphol. 2010, 28, 1141–1146. [Google Scholar] [CrossRef]
- Subramanian B, Anthony SN, Mubbunu L, Hachombwa C, Mlawa MS, Majambo MM, Sasi RM. Anthropometrics Analysis of Mental Foramen and Accessory Mental Foramen in Zambian Adult Human Mandibles. Scientific World Journal. 2019, 2019, 9093474. [Google Scholar]
- Suman P, Singh S, Mahato RK. Mental foramen and accessory mental foramen: a dry human mandibles study in South Indian population. Nat J Clin Anat 2018, 7, 182–189. [CrossRef]
- Tiwari, N. Left Accessory Mental Foramen in Dry Mandibles in Department of Anatomy in a Medical College: A Descriptive Cross-sectional Study. JNMA J Nepal Med Assoc. 2022, 60, 805–807. [Google Scholar] [CrossRef]
- Toh H, Kodama J, Yanagisako M, Ohmori T. Anatomical study of the accessory mental foramen and the distribution of its nerve. Okajimas Folia Anat Jpn. 1992, 69, 85–8. [Google Scholar] [CrossRef]
- Udhaya K, Saraladevi KV, Sridhar J. The morphometric analysis of the mental foramen in adult dry human mandibles: a study on the South Indian population. J Clin Diagn Res. 2013, 7, 1547–51. [Google Scholar]
- Vimala V, Rohinidevi M, Mekala D. Study of Anatomical Variations of Mental Foramen in Dry Adult Human Mandibles and its clinical importance. J Dent Med Sci. 2015, 14, 40–44. [Google Scholar]
- Voljevica A, Talović E, Hasanović A. Morphological and morphometric analysis of the shape, position, number and size of mental foramen on human mandibles. Acta Med Acad. 2015, 44, 31–8. [Google Scholar] [CrossRef]
- Zografos J, Mutzuri A. E sychnoteta yparxes diplou geneiakou trematos se deigma tou Ellenikou plethysmou [Incidence of double mental foramen in a sample of Greek population]. Odontostomatol Proodos. 1989, 43, 521–3. [Google Scholar]
- Muinelo-Lorenzo J, Rodríguez-Pato R, Martínez-Reglero C, Salgado-Barreira A, Suárez-Cunqueiro MM. Detection of the Accessory Mental Foramina on Human Mandibles Using Cone-beam Computed Tomography: A Systematic Review and Meta-analysis. J Endod. 2021, 47, 1215–1228. [Google Scholar] [CrossRef]
- Shan S, Zhong S, Li J, Wang T. Systematic review and meta-analysis of mandibular canal variations on cone beam computed tomography. Oral Radiol. 2022, 38, 445–451. [Google Scholar] [CrossRef] [PubMed]
- Βruna-Mejias A, Nova-Baeza P, Torres-Riquelme F, Delgado-Retamal MF, Orellana-Donoso M, Suazo-Santibañez A, Sepulveda-Loyola W, Valdés-Orrego I, Sanchis-Gimeno J, Valenzuela-Fuenzalida JJ. Morphological Characteristics of the Double Mental Foramen and Its Relevance in Clinical Practice: An Observational Study. Diagnostics. 2024, 14, 1277.
- Rahpeyma A, Khajehahmadi S. Accessory Mental Foramen and Maxillofacial Surgery. J Craniofac Surg. 2018, 29, e216–e217.
Figure 1.
Wires used to additionally determine the diameter of AMFs.
Figure 1.
Wires used to additionally determine the diameter of AMFs.
Figure 2.
Two small accessory mental foramina located the one very close to the main mental foramen and the other one in a far distance from it anterosuperiorly.
Figure 2.
Two small accessory mental foramina located the one very close to the main mental foramen and the other one in a far distance from it anterosuperiorly.
Figure 3.
Double accessory mental foramina, round and oval, found superior and antero-superior to the main mental foramen.
Figure 3.
Double accessory mental foramina, round and oval, found superior and antero-superior to the main mental foramen.
Figure 4.
Accessory mental foramen located immediately posterior to the main mental foramen.
Figure 4.
Accessory mental foramen located immediately posterior to the main mental foramen.
Figure 5.
Accessory mental foramen located postero-inferior to the main mental foramen.
Figure 5.
Accessory mental foramen located postero-inferior to the main mental foramen.
Figure 6.
A wide accessory mental foramen located inferiorly to the main mental foramen.
Figure 6.
A wide accessory mental foramen located inferiorly to the main mental foramen.
Figure 7.
Accessory mental foramen very close to the main mental foramen.
Figure 7.
Accessory mental foramen very close to the main mental foramen.
Figure 8.
Meta-analysis: PRISMA 2020 flow diagram.
Figure 8.
Meta-analysis: PRISMA 2020 flow diagram.
Figure 9.
AMF prevalence meta-analysis; the combined prevalence of AMF in dry mandibles is 6.1% (95% CI: 4.8% - 7.6%;) with I2 60%.
Figure 9.
AMF prevalence meta-analysis; the combined prevalence of AMF in dry mandibles is 6.1% (95% CI: 4.8% - 7.6%;) with I2 60%.
Figure 10.
Right AMF prevalence meta-analysis; the combined prevalence of AMF in dry mandibles is 48.2% (95% CI: 35.2% - 61.2%) with I2 50%
Figure 10.
Right AMF prevalence meta-analysis; the combined prevalence of AMF in dry mandibles is 48.2% (95% CI: 35.2% - 61.2%) with I2 50%
Figure 11.
Left AMF prevalence meta-analysis; the combined prevalence of AMF in dry mandibles is 51.8% (95% CI: 38.8% - 64.8%) with I2 50%.
Figure 11.
Left AMF prevalence meta-analysis; the combined prevalence of AMF in dry mandibles is 51.8% (95% CI: 38.8% - 64.8%) with I2 50%.
Figure 12.
Bilateral AMF prevalence meta-analysis; the combined prevalence of AMF in dry mandibles is 2.1% (95% CI: 0.0% - 7.3%) with I2 18%.
Figure 12.
Bilateral AMF prevalence meta-analysis; the combined prevalence of AMF in dry mandibles is 2.1% (95% CI: 0.0% - 7.3%) with I2 18%.
Figure 13.
Oval-shaped AMF prevalence meta-analysis; the combined prevalence of AMF in dry mandibles is 37.3% (95% CI: 5.1% - 75.8%) with I2 83%.
Figure 13.
Oval-shaped AMF prevalence meta-analysis; the combined prevalence of AMF in dry mandibles is 37.3% (95% CI: 5.1% - 75.8%) with I2 83%.
Figure 14.
AMF prevalence meta-analysis; Galbraith plot.
Figure 14.
AMF prevalence meta-analysis; Galbraith plot.
Figure 15.
AMF prevalence meta-analysis; Funnel plot. Trim-and-fill analysis does not impute any studies on either side. Egger’s p = 0.914; Begg’s p = 0.234.
Figure 15.
AMF prevalence meta-analysis; Funnel plot. Trim-and-fill analysis does not impute any studies on either side. Egger’s p = 0.914; Begg’s p = 0.234.
Figure 16.
AMF prevalence meta-analysis; sensitivity analysis (leave-one-out analysis).
Figure 16.
AMF prevalence meta-analysis; sensitivity analysis (leave-one-out analysis).
Table 1.
A synopsis of the inclusion criteria using the PICOTS framework.
Table 1.
A synopsis of the inclusion criteria using the PICOTS framework.
| Parameters |
Inclusion criteria |
Exclusion criteria |
| (P) Population |
Human dry mandibles |
Cone-Beam Computed tomography; panoramic Rx |
| (I) Intervention |
Measurements with digital caliper and wires |
|
| (C) Comparison |
Heterogeneity assessment; publication bias assessment |
|
| (O) Outcome |
AMF prevalence, location, shape, size, and distance from MF, alveolar ridge, and mandible lower border |
Cases involving mandible pathology (fracture, tumor) |
| (T) Time |
Papers published over the last 50 years (from 1974) |
Previously published duplicates |
| (S) Setting |
Universities (dissection rooms; osteological collections) |
|
Table 2.
Characteristics of accessory mental foramen (AMF) cases of the present study.
Table 2.
Characteristics of accessory mental foramen (AMF) cases of the present study.
| Sample size |
|
| Mandibles |
114 |
| Sides |
228 |
| Mental Foramens |
228 |
| Accessory Mental Foramens |
9 |
| AMF cases (per mandible) |
|
| Absent |
107/114 (93.9%) |
| Present; Total |
7/114 (6.1%) |
| Present; Unilateral |
7/114 (6.1%) |
| Present; Bilateral |
0/114 (0%) |
| Location |
|
| Right side |
5/9 (55.6%) |
| Left side |
4/9 (44.4%) |
| Anterior to mental foramen |
3/9 (33.3%) |
| Posterior to mental foramen |
6/9 (66.7%) |
| Shape |
|
| Round |
5/9 (55.6%) |
| Oval |
4/9 (44.4%) |
| Dimensions (mean ± SD) |
|
| Diameter / Vertical axis1 (mm) |
0.96 ± 0.43 |
| Horizontal axis (mm)† |
1.33 ± 0.55 |
| Area (mm2) |
0.94 ± 0.87 |
| Dimensions (mean ± SD) |
|
| from mental foramen (mm) |
4.12 ± 2.15 |
| from alveolar ridge (mm) |
12.68 ± 4.10 |
| from lower border of mandible (mm) |
11.92 ± 1.57 |
Table 3.
Inter-rater reliability assessment for categorical variables; Cohen’s kappa estimates.
Table 3.
Inter-rater reliability assessment for categorical variables; Cohen’s kappa estimates.
| Samples |
Side;
1st rater |
Side;
2nd rater |
Position regarding MF;
1st rater |
Position regarding MF;
2nd rater |
Shape;
1st rater |
Shape;
2nd rater |
| 1 |
left |
left |
posterior; same horizontal level |
posterior; same horizontal level |
oval |
oval |
| 2 |
right |
right |
posterior inferior |
posterior inferior |
circle |
circle |
| 3 |
right |
right |
posterior inferior |
posterior inferior |
oval |
oval |
| 4 |
left |
left |
posterior inferior |
posterior inferior |
oval |
oval |
| 5A |
right |
right |
posterior inferior |
posterior inferior |
oval |
oval |
| 5B |
right |
right |
anterior superior |
anterior superior |
circle |
circle |
| 6 |
right |
right |
posterior inferior |
posterior; same horizontal level |
circle |
circle |
| 7A |
left |
left |
anterior superior |
anterior superior |
circle |
circle |
| 7B |
left |
left |
anterior superior |
anterior superior |
circle |
circle |
| Cohen’s kappa |
1.000 |
0.805 |
1.000 |
| p-value |
0.008 |
0.001 |
0.008 |
Table 4.
Inter-rater reliability assessment for continuous variables; intraclass correlation coefficients (ICC) estimates and their 95% confidence intervals (CI) based on a mean rating (n=2), absolute-agreement, two-way random model.
Table 4.
Inter-rater reliability assessment for continuous variables; intraclass correlation coefficients (ICC) estimates and their 95% confidence intervals (CI) based on a mean rating (n=2), absolute-agreement, two-way random model.
| Parameter |
Mean ±SD
(average) |
Mean ±SD
(1st rater) |
Mean ±SD
(2nd rater) |
ICC; 95% CI |
ICC
p-value |
| Diameter / Vertical axis† (mm) |
0.96 ± 0.43 |
0.97 ± 0.42 |
0.94 ± 0.43 |
0.997; 0.987 – 0.999 |
<0.001 |
| Horizontal axis (mm)† |
1.33 ± 0.55 |
1.34 ± 0.56 |
1.32 ± 0.53 |
0.997; 0.970 – 1.000 |
<0.001 |
| Area (mm2) |
0.94 ± 0.87 |
0.96 ± 0.87 |
0.93 ± 0.86 |
1.000; 0.996 – 1.000 |
<0.001 |
| Distance from mental foramen (mm) |
4.12 ± 2.15 |
4.09 ± 2.15 |
4.14 ± 2.15 |
1.000; 0.998 – 1.000 |
<0.001 |
| Distance from alveolar ridge (mm) |
12.68 ± 4.10 |
12.66 ± 4.03 |
12.69 ± 4.17 |
0.999; 0.998 – 1.000 |
<0.001 |
| Distance from lower border of mandible (mm) |
11.92 ± 1.57 |
11.90 ± 1.56 |
11.93 ± 1.58 |
0.998; 0.991 – 1.000 |
<0.001 |
| Diameter / Vertical axis† (mm) |
0.96 ± 0.43 |
0.97 ± 0.42 |
0.94 ± 0.43 |
0.997; 0.987 – 0.999 |
<0.001 |
Table 5.
Prevalence meta-analysis; included studies.
Table 5.
Prevalence meta-analysis; included studies.
| Study |
Origin |
Size |
Cases with AMF |
Total AMF |
Right AMF |
Left AMF |
Unilateral AMF |
Bilateral AMF |
Single AMF |
Multiple AMFs |
| Agthong, 2005 [15] |
Thailand |
110 |
2 |
4 |
2 |
2 |
0 |
2 |
4 |
0 |
| Budhiraja, 2013 [16] |
India |
105 |
7 |
7 |
|
|
7 |
0 |
|
|
| Chrcanovic, 2010 [17] |
Brazil |
80 |
5 |
5 |
|
|
5 |
0 |
5 |
0 |
| Dave, 2019 [18] |
India |
300 |
50 |
51 |
8 |
43 |
49 |
1 |
|
|
| Gershenshon, 1986 [19] |
Israel; India |
575 |
28 |
39 |
|
|
|
|
23 |
5 |
| Gupta, 2012 [20] |
India |
120 |
8 |
8 |
5 |
3 |
8 |
0 |
8 |
0 |
| Igbigbi, 2005 [21] |
Malawi |
70 |
1 |
1 |
0 |
1 |
1 |
0 |
1 |
0 |
| Kadel, 2018 [22] |
Nepal |
100 |
7 |
7 |
3 |
4 |
7 |
0 |
|
|
| Kokten, 2004 [23] |
Turkey |
45 |
1 |
1 |
|
|
1 |
0 |
1 |
0 |
| Kumari, 2018 [24] |
India |
50 |
5 |
6 |
2 |
4 |
3 |
1 |
|
|
| Lal, 2018 [25] |
India |
50 |
4 |
5 |
4 |
1 |
5 |
0 |
5 |
0 |
| Nalbantoglu, 2024 [26] |
Turkey |
249 |
11 |
12 |
|
|
10 |
1 |
|
|
| Paraskevas, 2015 [27] |
Greece |
96 |
4 |
5 |
3 |
2 |
3 |
1 |
5 |
0 |
| Prabodha, 2006 [28] |
Sri Lanka |
24 |
2 |
2 |
|
|
2 |
0 |
2 |
0 |
| Raikohila, 2018 [29] |
India |
260 |
23 |
27 |
16 |
11 |
19 |
4 |
27 |
0 |
| Sakalem, 2024 [30] |
Brazil |
63 |
4 |
6 |
|
|
2 |
2 |
|
|
| Sawyer, 1998 [2] |
USA |
705 |
42 |
46 |
22 |
20 |
38 |
4 |
|
|
| Shukla, 2015 [31] |
India |
70 |
6 |
5 |
2 |
3 |
|
|
|
|
| Singh, 2010 [32] |
India |
100 |
13 |
13 |
5 |
8 |
13 |
0 |
13 |
0 |
| Subramanian, 2019 [33] |
Zambia |
33 |
2 |
2 |
1 |
1 |
2 |
0 |
2 |
0 |
| Suman, 2020 [34] |
India |
61 |
4 |
5 |
3 |
2 |
3 |
1 |
|
|
| Tiwari, 2022 [35] |
Nepal |
47 |
4 |
4 |
0 |
4 |
4 |
0 |
|
|
| Toh, 1992 [36] |
Japan |
|
|
3 |
2 |
1 |
3 |
0 |
3 |
0 |
| Udhaya, 2013 [37] |
India |
90 |
4 |
5 |
2 |
3 |
3 |
1 |
|
|
| Vimala, 2015 [38] |
India |
35 |
2 |
2 |
2 |
0 |
2 |
0 |
2 |
0 |
| Voljevica, 2015 [39] |
Bosnia-Herz. |
150 |
4 |
4 |
4 |
0 |
4 |
0 |
4 |
0 |
| Zografos, 1989 [40] |
Greece |
464 |
31 |
|
|
|
|
|
|
|
| Present study |
Greece |
114 |
7 |
9 |
5 |
4 |
7 |
0 |
5 |
2 |
Table 6.
Meta-analysis of shape, size, and distance from mental foramen; included studies. Combined mean vertical axis is 1.18 ± 0.61 mm, while combined mean distance from MF 3.64 ± 2.29 mm.
Table 6.
Meta-analysis of shape, size, and distance from mental foramen; included studies. Combined mean vertical axis is 1.18 ± 0.61 mm, while combined mean distance from MF 3.64 ± 2.29 mm.
| Study |
Origin |
Total AMF |
Round |
Oval |
Vertical axis
(mean) |
Vertical axis
(SD) |
Distance from MF
(mean) |
Distance from MF
(SD) |
| Paraskevas, 2015 [27] |
Greece |
5 |
5 |
0 |
1.09 |
0.15 |
5.24 |
3.21 |
| Prabodha, 2006 [28] |
Sri Lanka |
2 |
0 |
2 |
1.70 |
0.28 |
|
|
| Raikohila, 2018 [29] |
India |
27 |
20 |
7 |
1.27 |
0.77 |
2.96 |
2.07 |
| Singh, 2010 [32] |
India |
13 |
13 |
0 |
|
|
|
|
| Subramanian, 2019 [33] |
Zambia |
2 |
0 |
2 |
1.53 |
0.35 |
|
|
| Tiwari, 2022 [35] |
Nepal |
4 |
1 |
3 |
1.02 |
0.03 |
5.72 |
0.40 |
| Toh, 1992 [36] |
Japan |
3 |
|
|
0.84 |
0.12 |
2.84 |
2.13 |
| Present study |
Greece |
9 |
5 |
4 |
0.96 |
0.43 |
4.12 |
2.15 |
Table 7.
Quality assessment of the included studies using the Joanna Briggs Institute (JBI) Critical Appraisal Checklist for analytical cross-sectional study.
Table 7.
Quality assessment of the included studies using the Joanna Briggs Institute (JBI) Critical Appraisal Checklist for analytical cross-sectional study.
| Study |
Q1 |
Q2 |
Q3 |
Q4 |
Q5 |
Q6 |
Q7 |
Q8 |
Overall appraisal |
| Agthong, 2005 [15] |
Y |
Y |
NA |
Y |
N |
N |
Y |
Y |
Include |
| Budhiraja, 2013 [16] |
Y |
Y |
NA |
Y |
N |
N |
Y |
NA |
Include |
| Chrcanovic, 2010 [17] |
Y |
Y |
NA |
Y |
N |
N |
Y |
Y |
Include |
| Dave, 2019 [18] |
Y |
Y |
NA |
Y |
N |
N |
Y |
NA |
Include |
| Gershenshon, 1986 [19] |
Y |
Y |
NA |
Y |
N |
N |
Y |
NA |
Include |
| Gupta, 2012 [20] |
Y |
Y |
NA |
Y |
N |
N |
Y |
NA |
Include |
| Igbigbi, 2005 [21] |
Y |
Y |
NA |
Y |
N |
N |
Y |
Y |
Include |
| Kadel, 2018 [22] |
Y |
Y |
NA |
Y |
N |
N |
Y |
NA |
Include |
| Kokten, 2004 [23] |
Y |
Y |
NA |
Y |
N |
N |
Y |
NA |
Include |
| Kumari, 2018 [24] |
Y |
Y |
NA |
Y |
N |
N |
Y |
NA |
Include |
| Lal, 2018 [25] |
Y |
Y |
NA |
Y |
N |
N |
Y |
NA |
Include |
| Nalbantoglu, 2024 [26] |
Y |
Y |
NA |
Y |
N |
N |
Y |
Y |
Include |
| Paraskevas, 2015 [27] |
Y |
Y |
NA |
Y |
N |
N |
Y |
NA |
Include |
| Prabodha, 2006 [28] |
Y |
Y |
NA |
Y |
N |
N |
Y |
NA |
Include |
| Raikohila, 2018 [29] |
Y |
Y |
NA |
Y |
N |
N |
Y |
NA |
Include |
| Sakalem, 2024 [30] |
Y |
Y |
NA |
Y |
N |
N |
Y |
Y |
Include |
| Sawyer, 1998 [2] |
Y |
Y |
NA |
Y |
Y |
Y |
Y |
Y |
Include |
| Shukla, 2015 [31] |
Y |
Y |
NA |
Y |
N |
N |
Y |
NA |
Include |
| Singh, 2010 [32] |
Y |
Y |
NA |
Y |
N |
N |
Y |
NA |
Include |
| Subramanian, 2019 [33] |
Y |
Y |
NA |
Y |
N |
N |
Y |
Y |
Include |
| Suman, 2020 [34] |
Y |
Y |
NA |
Y |
N |
N |
Y |
NA |
Include |
| Tiwari, 2022 [35] |
Y |
Y |
NA |
Y |
N |
N |
Y |
Y |
Include |
| Toh, 1992 [36] |
Y |
Y |
NA |
Y |
N |
N |
Y |
Y |
Include |
| Udhaya, 2013 [37] |
Y |
Y |
NA |
Y |
N |
N |
Y |
NA |
Include |
| Vimala, 2015 [38] |
Y |
Y |
NA |
Y |
N |
N |
Y |
NA |
Include |
| Voljevica, 2015 [39] |
Y |
Y |
NA |
Y |
N |
N |
Y |
Y |
Include |
| Zografos, 1989 [40] |
Y |
Y |
NA |
Y |
N |
N |
Y |
U |
Include |
| Present study |
Y |
Y |
NA |
Y |
Y |
Y |
Y |
Y |
Include |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).