Submitted:
18 December 2024
Posted:
19 December 2024
You are already at the latest version
Abstract
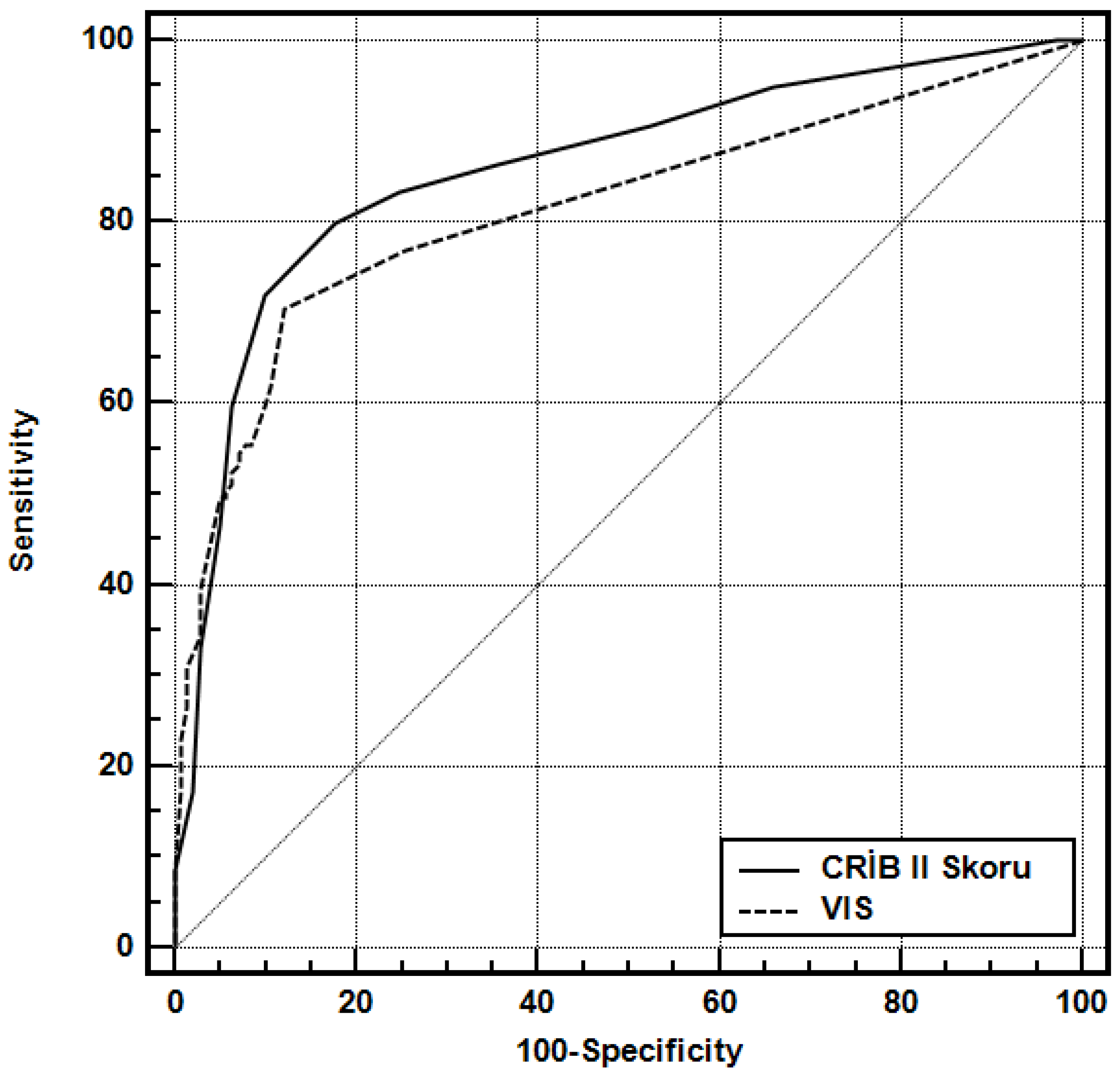
Background: Can vasoactive inotropic score (VIS) be a new mortality score in preterm infants weighing less than 1000 grams? Method:This study was designed as a retrospective study. A total of 280 preterm infants under 1000 grams admitted to the neonatal intensive care unit over a five-year period were included in the study. For each patient, CRIB-II score and VIS were calculated, and their ability to predict mortality was compared. To predict and compare the accuracy of the scoring systems, Receiver Operating Characteristic (ROC) analysis was used, and the area under the curve (AUC) was calculated. Results:In infants who died within the first 28 days postnatally, CRIB-II Score (p=0.0001) and VISmax (p=0.0001) were higher compared to those who survived. The AUC for CRIB-II and VIS in predicting mortality were 0.86/0.81, with cutoffs of >12/>5, sensitivity 79/70, specificity 82/87, positive predictive value (PPV) 81/85, and negative predictive value 80/75, respectively. There was no statistically significant difference between the AUC values of the CRIB-II Score and VIS variables (p=0.160). Conclusion: VIS can predict mortality in very low birth weight preterm infants as accurately as the CRIB-II score.
Keywords:
Introduction
Materyal - Method
Settings and Study Population
Definitions
Score Calculation
Statistical analysis
Results
Discussion
References
- Baker, S.; Xiang, W.; Atkinson, I. Hybridized neural networks for non-invasive and continuous mortality risk assessment in neonates. Comput. Biol. Med. 2021, 134, 104521. [Google Scholar] [CrossRef] [PubMed]
- The CRIB (clinical risk index for babies) score: a tool for assessing initial neonatal risk and comparing performance of neonatal intensive care units. The International Neonatal Networ. Lancet 1993, 342, 193–198, Erratum in: Lancet 1993, 342, 626. [CrossRef] [PubMed]
- Rahman, A.; Hamid, M.H. Accuracy of CRIB II Score in Predicting the Neonatal Mortality in very Preterm Babies. PJMHS 2022, 16, 564–566. [Google Scholar] [CrossRef]
- Ezz-Eldin, Z.; Hamid, T.; Youssef, M.; Nabil, H. Clinical Risk Index for Babies (CRIB II) Scoring System in Prediction of Mortality in Premature Babies. JCDR 2015, 9. [Google Scholar]
- Marete, I.K.; O Wasunna, A.; A Otieno, P. Clinical risk index for babies (CRIB) II score as a predictor of neonatal mortality among low birth weight babies at Kenyatta National Hospital. East Afr Med J. 2011, 88, 18–23. [Google Scholar]
- Mohkam, M.; Afjeii, A.; Payandeh, P.; Zadkarami, M.; Kazemian, M.; Fakhraii, H. A comparison of CRIB, CRIB II, SNAP, SNAPII and SNAP-PE scores for prediction of mortality in critically ill neonates. Med J Islamic Republ Iran. 2011, 24, 193–199. [Google Scholar]
- Lee, S.M.; Lee, M.H.; Chang, Y.S. The Clinical Risk Index for Babies II for prediction of time-dependent mortality and short-term morbidities in very low birth weight infants. Neonatology 2019, 116, 244–51. [Google Scholar] [CrossRef]
- Faridpour, F.; Farahani, A.S.; Rassouli, M.; Shariat, M.; Nasiri, M.; Ashrafzadeh, M. Clinical risk index for babies (CRIB-II) scoring system in prediction of mortality risk in preterm neonates in the first 24 hour. . Evidence Based Care 2020, 10, 58–63. [Google Scholar]
- Babaei, H.; Jafrasteh, A. The evaluation of CRIB II scoring system in predicting mortality in preterm newborns. Yafteh. 2015, 16, 27–35. [Google Scholar]
- Gagliardi, L.; Cavazza, A.; Brunelli, A.; Battaglioli, M.; Merazzi, D.; Tandoi, F.; Cella, D.; Perotti, G.F.; Pelti, M.; Stucchi, I.; et al. Assessing mortality risk in very low birthweight infants: a comparison of, C.R.I.B.; CRIB-II; SNAPPE-II. Arch Dis Child Fetal Neonatal Ed. 2004, 89, F419–F422. [Google Scholar] [CrossRef]
- EzzEldin, Z.M.; Hamid, T.A.; Youssef, M.R.; Nabil, H.E. Clinical risk index for babies (CRIB II) scoring system in prediction of mortality in premature babies. J Clin Diagn Res. 2015, 9, SC08-11. [Google Scholar]
- Felice C, Del Vecchio A, Latini G. Evaluating illness severity for very low birth weight infants: CRIB or CRIB-II? J Maternal Fetal Neonatal Med. 2005, 7, 257–60.
- Fouladinejad, M.; Behnampour, N.; Zanjani, A.P.; Gharib, M.H.; Kamrani, M.A. The evaluation of predicting mortality risk of premature infants with very low birthweight by CRIB score. J Gorgan Univ Med Sci. 2009, 10, 40–89. [Google Scholar]
- Davidson, J.; Tong, S.; Hancock, H.; Hauck, A.; da Cruz, E.; Kaufman, J. Pro- spective validation of the vasoactive-inotropic score and correlation to short-term outcomes in neonates and infants after cardiothoracic sur gery. Intensive Care Med 2012, 38, 1184–1190. [Google Scholar] [CrossRef] [PubMed]
- Gaies MG, Gurney JG, Yen AH, Napoli ML, Gajarski RJ, Ohye RG, et al. Vasoactive-inotropic score as a predictor of morbidity and mor- tality in infants after cardiopulmonary bypass. Pediatr Crit Care Med 2010, 11, 234–238. [CrossRef]
- Hari Gopal S, Toy CL, Hanna M, Furtun BY, Hagan JL, Nassr AA, Fernandes CJ, Keswani S and Gowda SH Inotropic score and vasoactive inotropic score as predictors of outcomes in congenital diaphragmatic hernia: A single center retrospective study. Front. Pediatr. 2023, 11, 1101546.
- Demirhan, S.; Topçuoğlu, S.; Karadağ, N.; Özalkaya, E.; Karatekin, G. Vasoactive inotropic score as a predictor of mortality in neonatal septic shock. J Trop Pediatr. 2022, 68. [Google Scholar] [CrossRef]
- Amer, R.; Seshia, M.M.; Elsayed, Y.N. A vasoactive inotropic score predicts the severity of compromised systemic circulation and mortality in preterm infants. J. Neonatal Perinat. Med. 2022, 15, 529–535. [Google Scholar] [CrossRef]
- Aziz, K.B.; Lavilla, O.C.; Wynn, J.L.; Lure, A.C.; Gipson, D.; de la Cruz, D. Maximum vasoactive-inotropic score and mortality in extremely premature, extremely low birth weight infants. J Perinatol 2021, 41, 2337–2344. [Google Scholar] [CrossRef]
- Kliegman, R.M.; Stanton, B.F.; St Gene, J.W.; Schor, N.F.; Behrman, R.E. Nelson textbook of pediatrics. Philadelphia: Saunders Elsevier; 2011.
- Been JV, Rours IG, Kornelisse RF, Lima Passos V, Kramer BW, Schnei- der TA, et al. Histologic chorioamnionitis, fetal involvement, and antena- tal steroids: Effects on neonatal outcome in preterm infants. Am J Obstet Gynecol 2009, 201, 587.e1–8. [CrossRef] [PubMed]
- Romero R, Gomez R, Galasso M, Munoz H, Acosta L, Yoon BH, et al. Macrophage inflammatory protein-1 alpha in term and preterm partu- rition: Effect of microbial invasion of the amniotic cavity. Am J Reprod Immunol 1994, 32, 108–113. [CrossRef]
- Butts, R.J.; Scheurer, M.A.; Atz, A.M.; Zyblewski, S.C.; Hulsey, T.C.; Bradley, S.M.; Graham, E.M. Comparison of maximum vasoactive inotropic score and low cardiac output syndrome as markers of early postoperative outcomes after neonatal cardiac surgery. Pediatr Cardiol. 2012, 33, 6. [Google Scholar] [CrossRef]
- Y Sanil et al Vasoactive-inotropic score after pediatric heart transplant: a marker of adverse outcome. Pediatr Transplant. 2013, 17, 567–72. [CrossRef]
- Friesland-Little, J.M.; et al. Risk factors for requiring extracorporeal membrane oxygenation support after a Norwood operation. J Thorac Cardiovasc Surg. 2019, 122, 428–436.
- Gaies, MG; et al. Vasoactive-inotropic score is associated with outcome after infant cardiac surgery: an analysis from the Pediatric Cardiac Critical Care Consortium and Virtual PICU System Registries. Pediatr Crit Care Med. 2014, 15, 52.
- Crow, SS; et al. Duration and magnitude of vasopressor support predicts poor outcome after infant cardiac operations. Ann Thorac Surg. 2014, 98, 655–61. [CrossRef]
- Dilli D, et.al. Predictive Value of Vasoactive-inotropic Score for Mortality in Newborns Undergoing Cardiac Surgery. Indian Pediatr. 2019, 56, 735–740. [CrossRef]
- Koponen, T.; Karttunen, J.; Musialowicz, T.; Pietiläinen, L.; Uusaro, A.; Laht- inen, P. Vasoactive-inotropic score and the prediction of morbidity and mortality after cardiac surgery. Br J Anaesth 2019, 122, 428–436. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.; Li, J.; Wei, Y.; Wang, Y.; Zhang, H.; Ma, L. Preliminary study on the predictive value of the vasoactive-inotropic score for the prognosis of neonatal congenital diaphragmatic hernia. BMC Surg. 2023, 23, 69. [Google Scholar] [CrossRef]
- Haque, A.; Siddiqui, N.R.; Munir, O.; Saleem, S.; Mian, A. Association between vasoactive-inotropic score and mortality in pediatric septic shock. Indian Pediatr 2015, 52, 311–313. [Google Scholar] [CrossRef]
- Kallekkattu, D.; Rameshkumar, R.; Chidambaram, M.; Krishnamurthy, K.; Selvan, T.; Mahadevan, S. Threshold of inotropic score and vasoac- tive-inotropic score for predicting mortality in pediatric septic shock. Indian J Pediatr 2022, 89, 432–437. [Google Scholar] [CrossRef] [PubMed]
- Kharrat, A.; Ripstein, G.; Baczynski, M.; Zhu, F.; Ye, X.Y.; Joye, S.; Jain, A. VAlidity of the vasoactive-inotropic score in preterm neonates receiving cardioactive therapies. Early Hum Dev. 2022, 173, 105657. [Google Scholar] [CrossRef]
| Bİrth weight | mean±SD | 684,49±193,21 | |
| Bİrth weeks | mean±SD | 25,39±2,93 | |
| Resuscitation | none | 33 | %11,79 |
| 1 | 241 | %86,07 | |
| >2 | 6 | %2,14 | |
| Gender | female | 159 | %56,79 |
| male | 121 | %43,21 | |
| Preeclampsia | 51 | %18,21 | |
| Chorioamnionitis | 39 | %13,93 | |
| Antenatal steroid dose |
none | 85 | %30,36 |
| 1 | 46 | %16,43 | |
| >2 | 149 | %53,21 | |
| Mode of delivery | vaginal delivery | 95 | %33,93 |
| C/S | 185 | %66,07 | |
| CRİB II Score | mean±SD | 12,32±4,08 | |
| median (IQR | 12 (9-16) | ||
| VIS | mean±SD | 53,75±89,57 | |
| median (IQR | 5 (0-110) | ||
| BE | mean±SD | -6,5±5,7 | |
| Median (IQR | -6 (-9,75--2) | ||
| Dopamin in first hour 24 | 79 | %28,21 | |
| Dobutamin in first hour 24 | 130 | %46,43 | |
| Adrenalin in first hour 24 | 58 | %20,71 | |
| Noradrenalin in first hour 24 | 57 | %20,36 | |
| Milrinon in first hour 24 | 3 | %1,07 | |
| Mortality in postnatal 28 days | 139 | %49,64 | |
| Mortalite (-) n:141 |
Mortalite (+) n:139 |
p | ||||
| Bİrth week | mean±SD | 26,99±2,36 | 23,77±2,55 | 0,0001 | ||
| Bİrth weight | mean±SD | 797,25±160,27 | 570,11±152,47 | 0,0001 | ||
| Resuscitation | none | 26 | %18,44 | 7 | %5,04 | 0,0001 |
| 1 | 115 | %81,56 | 126 | %90,65 | ||
| >2 | 0 | %0,00 | 6 | %4,32 | ||
| Gender | Male | 66 | %46,81 | 93 | %66,91 | 0,001 |
| Female | 75 | %53,19 | 46 | %33,09 | ||
| Preeclampsia | 37 | %26,24 | 14 | %10,07 | 0,0001 | |
| Chorioamnionitis | 12 | %8,51 | 27 | %19,42 | 0,008 | |
| Antenatal steroid dose |
none | 24 | %17,02 | 61 | %43,88 | 0,0001 |
| 1 | 19 | %13,48 | 27 | %19,42 | ||
| >2 | 98 | %69,50 | 51 | %36,69 | ||
| Mode of delivery | vaginal delivery | 24 | %17,02 | 71 | %51,08 | 0,0001 |
| C/S | 117 | %82,98 | 68 | %48,92 | ||
| CRİB II Score | mean±SD | 9,85±3,01 | 14,82±3,46 | 0,0001 | ||
| Median (IQR) | 10 (8-11,5) | 15 (13-17) | ||||
| VIS | mean±SD | 10,07±33,04 | 98,05±105,76 | 0,0001 | ||
| Median (IQR) | 0 (0-5) | 100 (5-140) | ||||
| BE | mean±SD | -5±5,12 | -8,01±5,87 | 0,0001 | ||
| Median (IQR) | -4 (-7--1,5) | -6,5 (-11,5--4) | ||||
| Dopamin | 17 | %12,06 | 62 | %44,60 | 0,0001 | |
| Dopamin dose in postnatal 24h | Ort±SS | 10,59±5,83 | 15,24±5,78 | 0,004 | ||
| Median (IQR) | 10 (5-15) | 20 (10-20) | ||||
| Dobutamin | 31 | %21,99 | 99 | %71,22 | 0,0001 | |
| Dobutamin dose in postnatal 24h | Ort±SS | 8,71±4,83 | 13,81±5,47 | 0,0001 | ||
| Median (IQR) | 5 (5-10) | 10 (10-20) | ||||
| Adrenalin | 5 | %3,55 | 53 | %38,13 | 0,0001 | |
| Adrenalin dose in postnatal 24h | Ort±SS | 0,64±0,49 | 1,07±0,47 | 0,061 | ||
| Median (IQR) | 1 (0,1-1) | 1 (1-1) | ||||
| Noradrenalin | 6 | %4,26 | 51 | %36,69 | 0,0001 | |
| Noradrenalin dose in postnatal 24h | Ort±SS | 0,93±0,19 | 1,06±0,27 | 0,156 | ||
| Median (IQR) | 1 (1-1) | 1 (1-1) | ||||
| Milrinon | 0 | %0,00 | 3 | %2,16 | 0,079 | |
| OR (%95 G.A) | p | |
| Bİrth week | 1,05 (0,75-1,48) | 0,786 |
| Birth weight | 1 (0,99-1,01) | 0,155 |
| Resuscitation | 1,42 (0,39-5,11) | 0,594 |
| Gender | 0,48 (0,21-1,07) | 0,074 |
| Preeclempsia | 0,42 (0,15-1,20) | 0,104 |
| Chorioamnionitis | 0,81 (0,27-2,38) | 0,699 |
| Antenatal steroid | 0,853 | |
| 1 | 0,83 (0,25-2,74) | 0,758 |
| >2 | 0,77 (0,31-1,9) | 0,573 |
| Mode of delivery | 0,87 (0,35-2,12) | 0,753 |
| Dopamin | 0,44 (0,14-1,36) | 0,154 |
| Dobutamin | 1,89 (0,76-4,71) | 0,173 |
| Adrenalin | 0,37 (0,03-5,07) | 0,456 |
| Noradrenalin | 0,17 (0,01-3,84) | 0,267 |
| CRİB II Score | 1,55 (1,38-1,73) | 0,0001 |
| VIS | 1,02 (1,01-1,02) | 0,0001 |
| BE | 1,04 (0,94-1,15) | 0,416 |
| AUC | SE | 95% CI | ||||
|---|---|---|---|---|---|---|
| CRİB II Skoru | 0,860 | 0,023 | 0,814 - 0,898 | |||
| VIS | 0,816 | 0,026 | 0,765 - 0,859 | |||
| Cut-off | Sensitivity | Specificity | PPV | NPV | LR (+) | |
| CRIB II Skoru | >12 | 79,86 | 82,27 | 81,60 | 80,60 | 4,50 |
| VIS | >5 | 70,50 | 87,94 | 85,20 | 75,20 | 5,85 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





