1. Introduction
Eye diseases are quite common in animals and humans. For example, in Russia, 20–45% of people over 40 have eye diseases [
1]. Neoplasms of the eye and its appendages are rare in the general etiology of neoplasms [
2]. The tumor process has a comprehensive effect on the body, more pronounced in malignant neoplasms consisting of moderately or poorly differentiated cells [
3]. In both humans and mammals, “paraneoplastic” syndromes are clinical and laboratory manifestations of the tumor process caused by the release of a large number of biologically active substances by tumor cells, such as cytokines, interleukins, hormone-like peptides, growth factors, and antigens [
4]. They present with hematological, endocrine, dermatological, neurological disorders, gastrointestinal changes, cancer-associated ophthalmopathy [
4,
5,
6,
7,
8,
9]. To date, the collection of cytological samples from or near the human eye is underused. Ocular cytology is relatively simple to perform and its use is informative in making a diagnosis [
10,
11,
12,
13]. Great variability in the cytological characteristics of the visual organs of animals affected by ophthalmological diseases has been found [
14]. The most common indications for ocular cytology include: scrapings or cleaning of the conjunctiva and cornea to determine the type and etiology of conjunctivitis and keratitis; aspirates of aqueous fluid or vitreous body if septic uveitis or “endophthalmitis” is suspected; and aspiration of solid tissue or cystic masses on the surface of, in, or around the eyeball [
15]. Pathological examination of the eyes when making a diagnosis during organ-preserving or liquidating surgical intervention is carried out quite rarely [
16]. Since modeling malignant neoplasms is a complex task, cytological-morphological study of the development of existing malignant neoplasms in animals can make it possible to clarify the causes of the occurrence and pathogenesis of the tumor process, and to develop effective methods for its prevention and treatment.
The aim of the work: to study the “morphological-functional indices” (MFIs) of organs and systems in animals in terms of the development of malignant neoplasms based on the “histological-pathological” analysis of the eyeballs after bilateral and unilateral enucleating.
2. Materials and Methods
The study of MFIs of organs and systems in animals in terms of malignant neoplasm development was performed based on “histological-pathological” analysis of the eyeballs after bilateral and unilateral enucleating in the 19 cats living in Moscow and admitted to a veterinary clinics for diagnostic and therapeutic manipulations. Data on the animal species, breed, presence and manifestation of concomitant oncological diseases were collected.
During enucleating of the eyeball and accessory organs, premedication was performed: meloxicam 0.2 mg/kg, maropitant 1 mg/kg, cefazolin 30 mg/kg. Then induction was performed using tiletamine and zolazepam 3 mg/kg, propofol 3-5 mg/kg and ET intubation. Anesthesia was maintained with isoflurane 0.5-1 vol.%. Histological studies of enucleated eyes were performed in the control and experimental groups, which were represented in approximately equal proportions by animals with and without a history of oncological diseases, males 52.6% (control - 37.5% and experiment - 62.5%) and females 47.4% (control - 66.7% and experiment - 33.30%). The study sample included the following cat breeds: crossbreeds - 15 (78.95%) cases, Bengal - 3 (15.79%) cases and Sphynx - 1 (5.26%). Morphological studies were carried out on animals of the age category mainly 7-12 years - 79.0% (control - 31.6% and experiment - 47.4%) and over 13 years old - 21.0% (control - 5.2% and experiment - 15.8%). After enucleating, the eyeballs were immediately placed in labeled sealed containers containing 10% neutral buffered formalin. Subsequently, after fixation, pathological material was excised, during which a macroscopic examination of the eyeballs was performed. In this case, for each animal, one or two sections of each eyeball (right and left) were obtained, for a total of 2-4 sections. After histological processing, the tissues were embedded in paraffin, microtomy was performed to obtain sections 5 μm thick. Preparation and staining of histological preparations with hematoxylin and eosin were carried out according to the standard technique. After preparation, histological preparations of the eyeballs, kidneys and oral cavity were subjected to “histological-pathological” examination. Examination of the preparations was carried out on an Olympus CX23 microscope (objective x10; eyepieces x4, x10, x40). An assessment was made of changes in the following structures of the eyeball: cornea, choroid, retina, optic nerve region, and lens.
3. Results
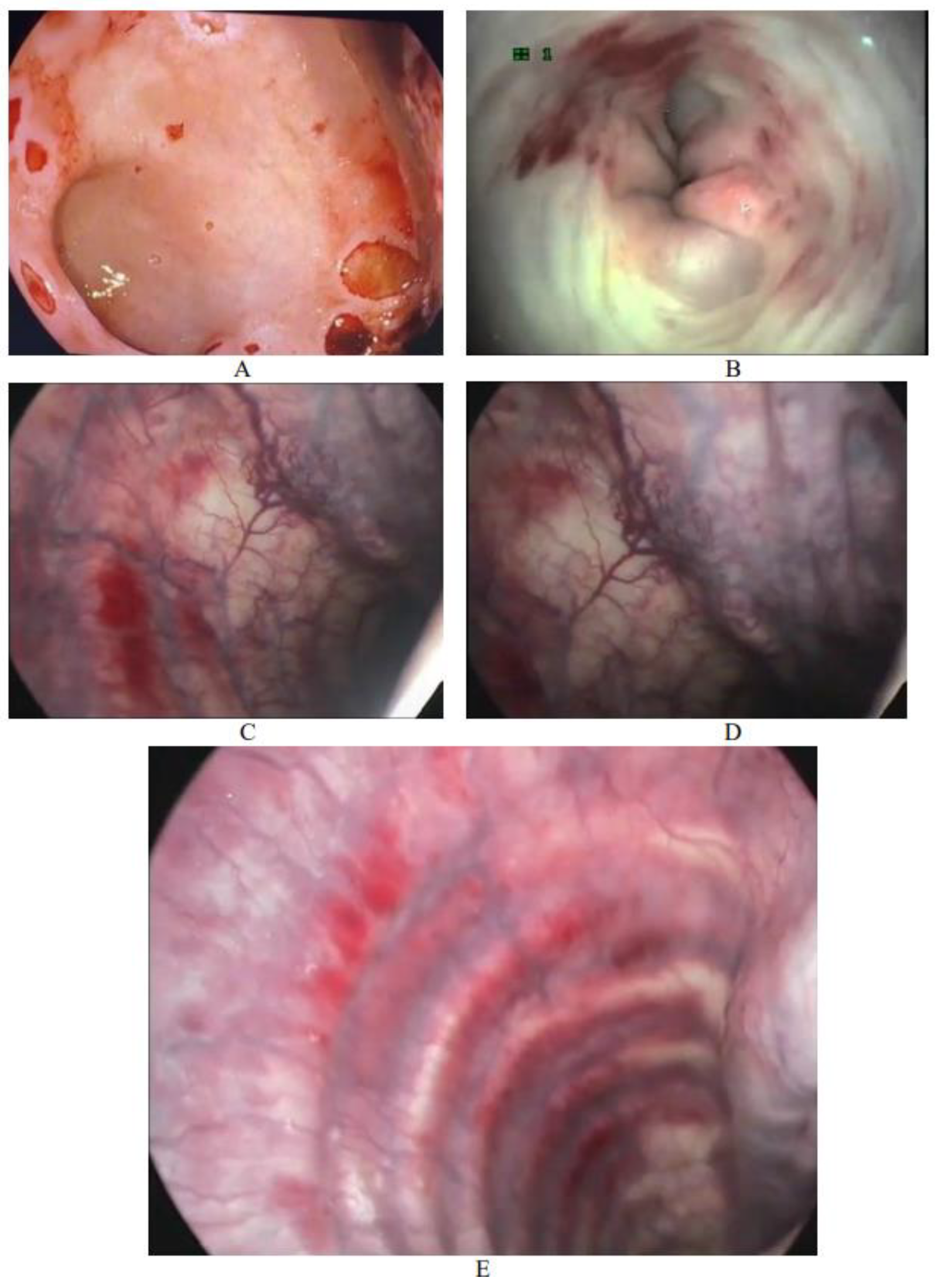
It was found that gastrointestinal “paraneoplastic” syndromes were the most common in the studied sample of animals. The manifestation of this syndrome was noted in 90.59% of cats. These symptoms worsened in 98.16% of cases with the use of chemotherapy and / or radiation therapy. This was confirmed by the results of endoscopic studies (
Figure 1).
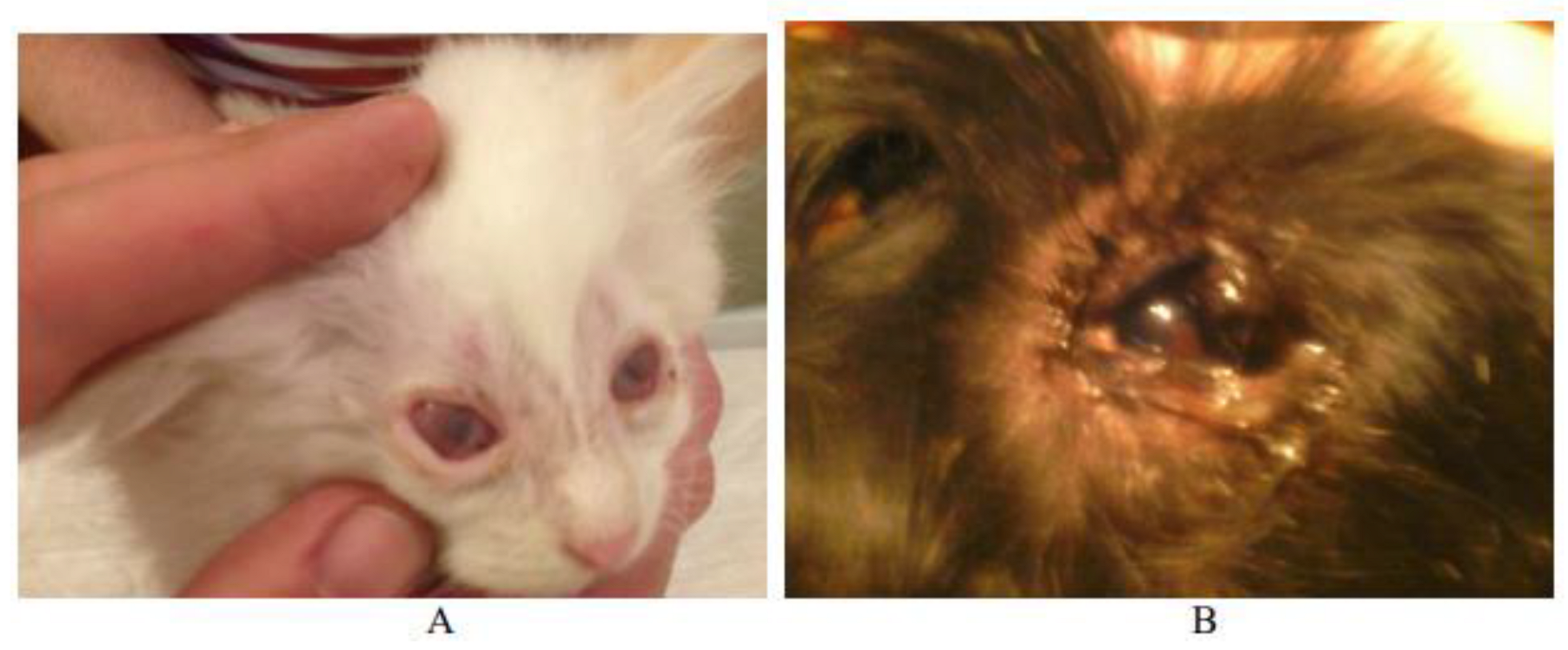
In the digestive system, the mucous and submucous layers of all organs are affected with the formation of acute inflammation with hemorrhages. It was found that ophthalmological paraneoplastic syndromes were the most common in the studied sample of animals (
Figure 1 and
Figure 2).
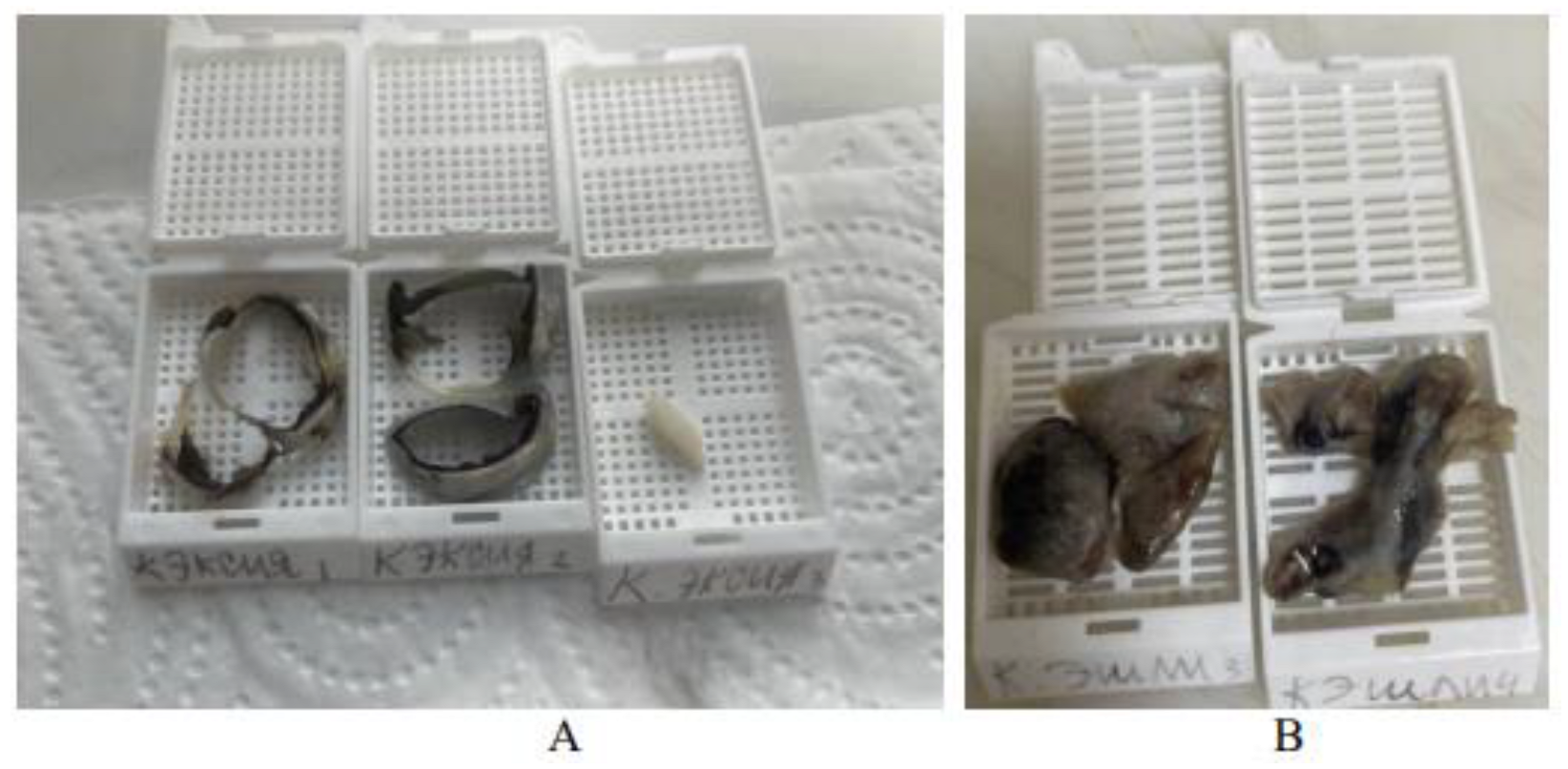
Since the sample included a large proportion of neoplasms of unknown morphology, additional histopathological studies of autopsy material from organs were carried out: lung tissue, kidney and jaw (
Figure 3).
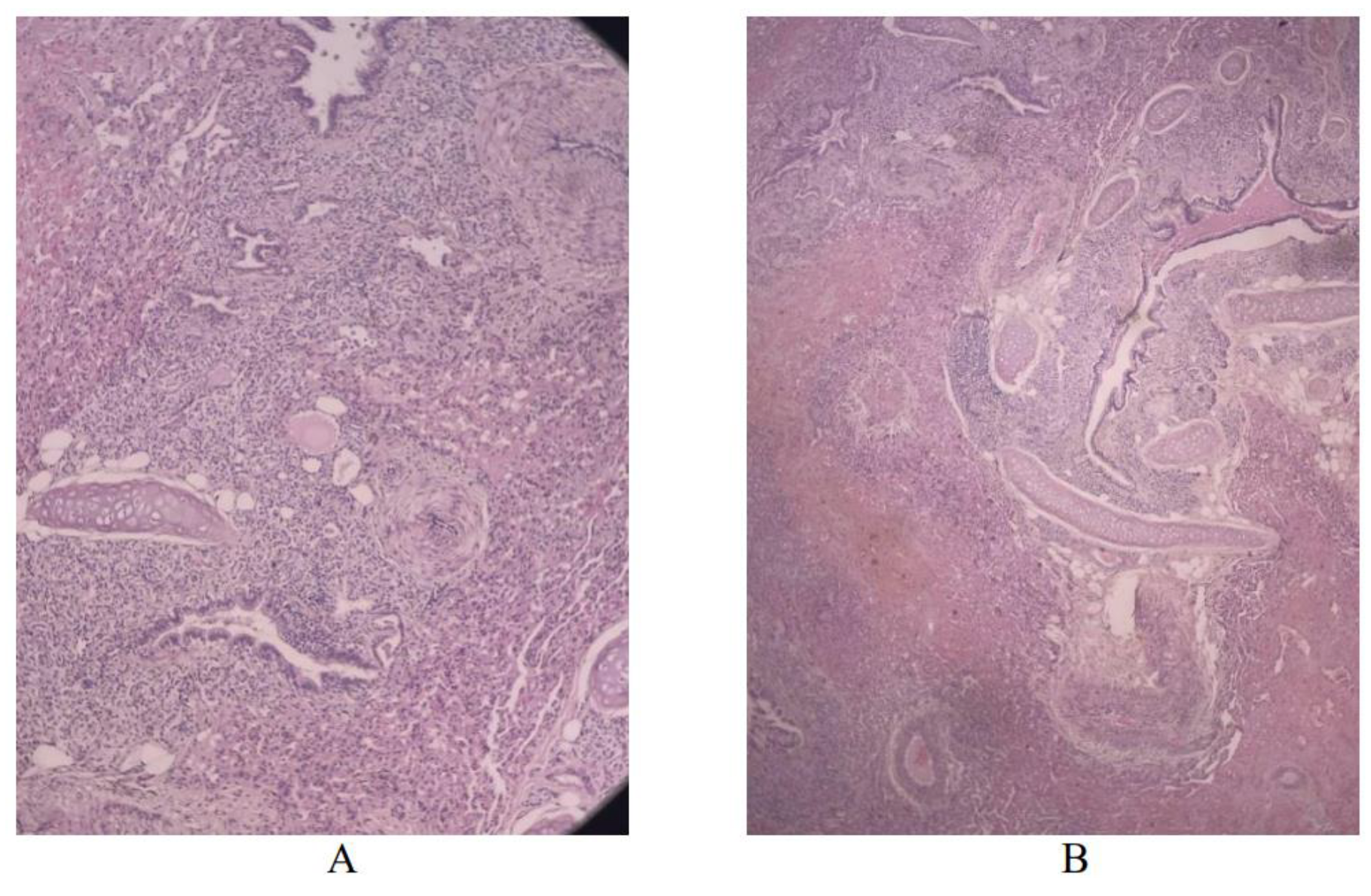
Histological studies were used to supplement and expand the diagnoses in animals. When examining the lung tissue of an 11-year-old female Bengal cat diagnosed with lymphoma, the following diagnosis was made: diffuse venous-capillary congestion, mild chronic-active interstitial pneumonia with parenchymal fibrosis (
Figure 4).
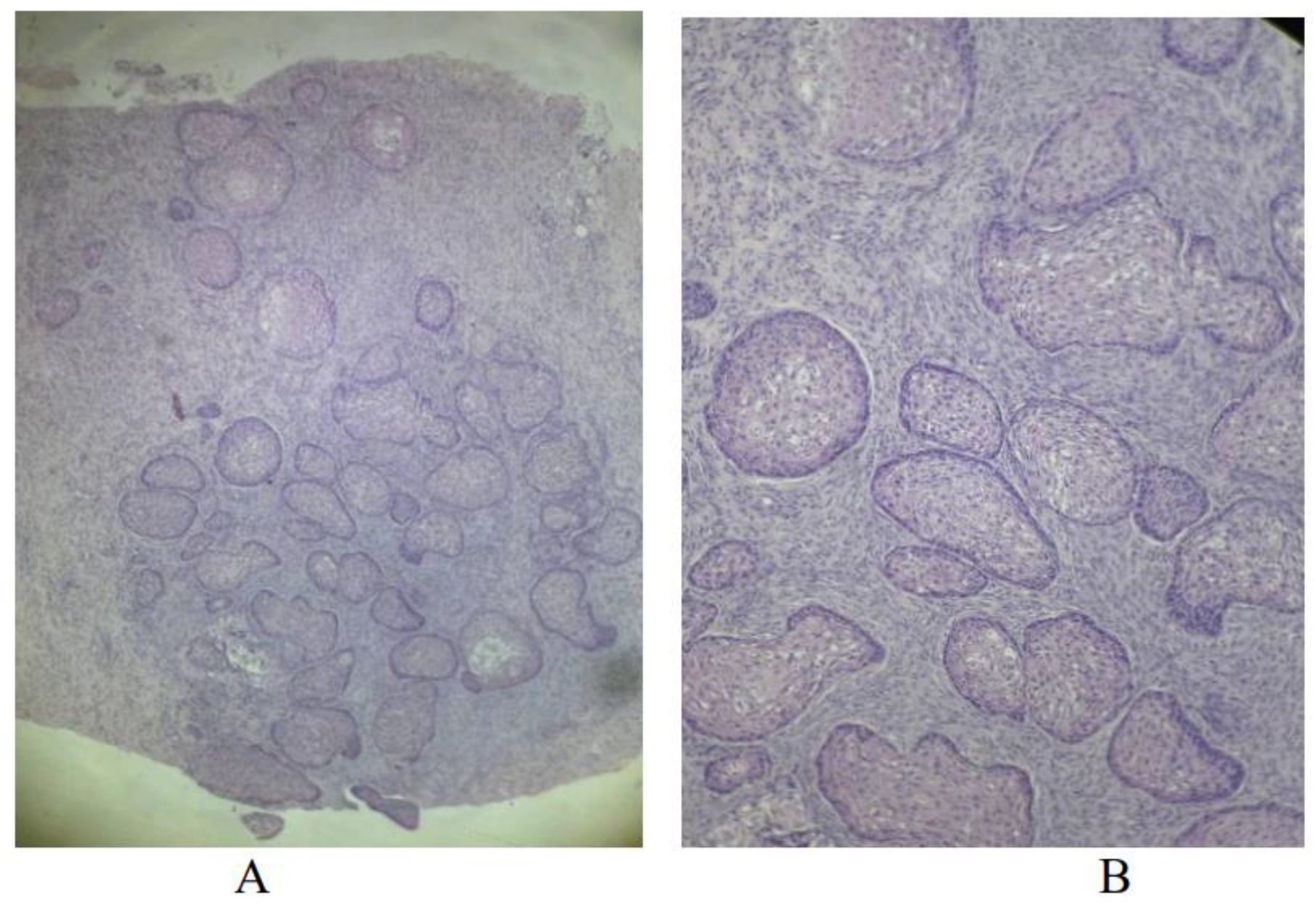
Autopsy material from a male mixed-breed cat was used to examine a neoplasm of the oral cavity. “Histological-pathological” examination revealed squamous cell carcinoma (
Figure 5).
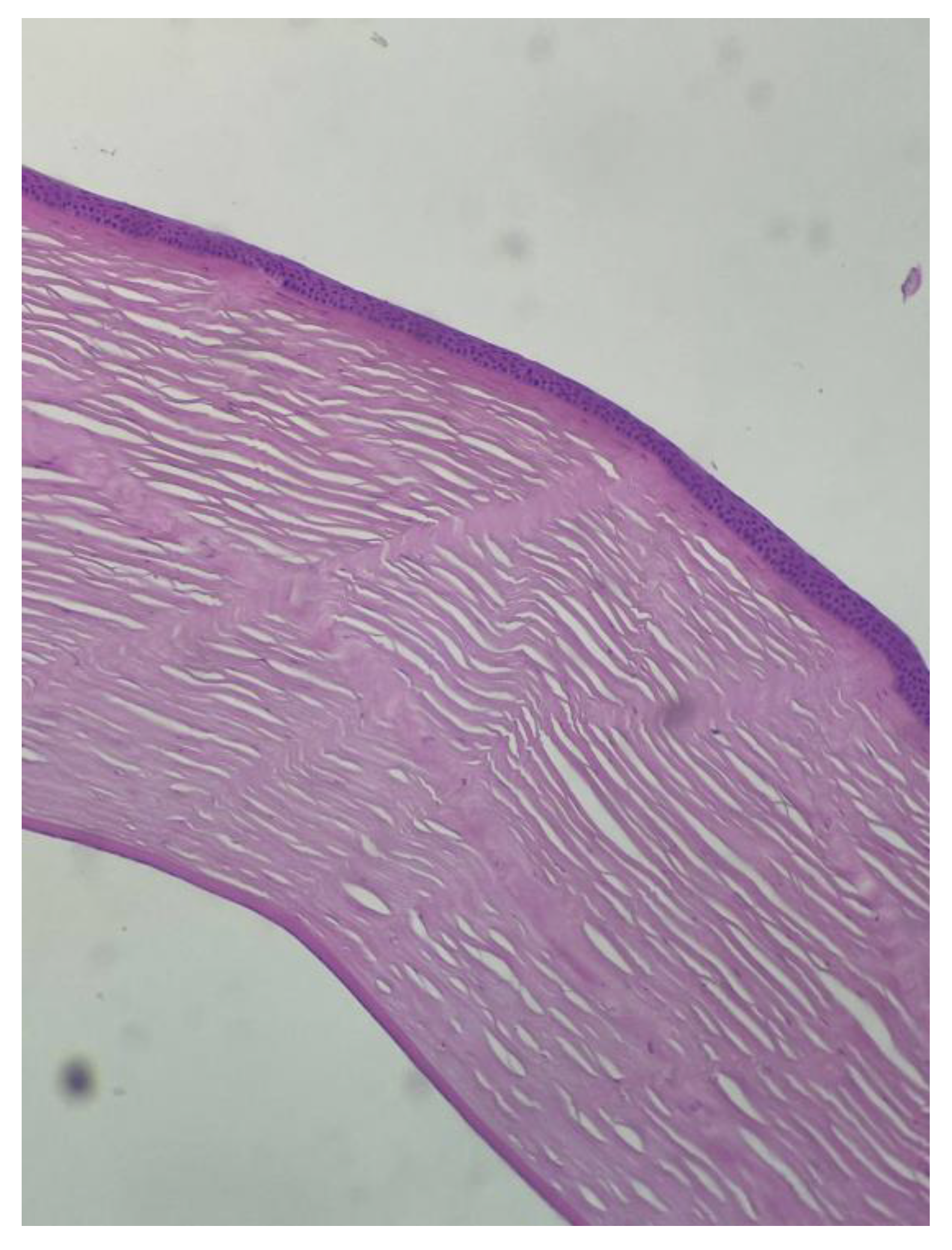
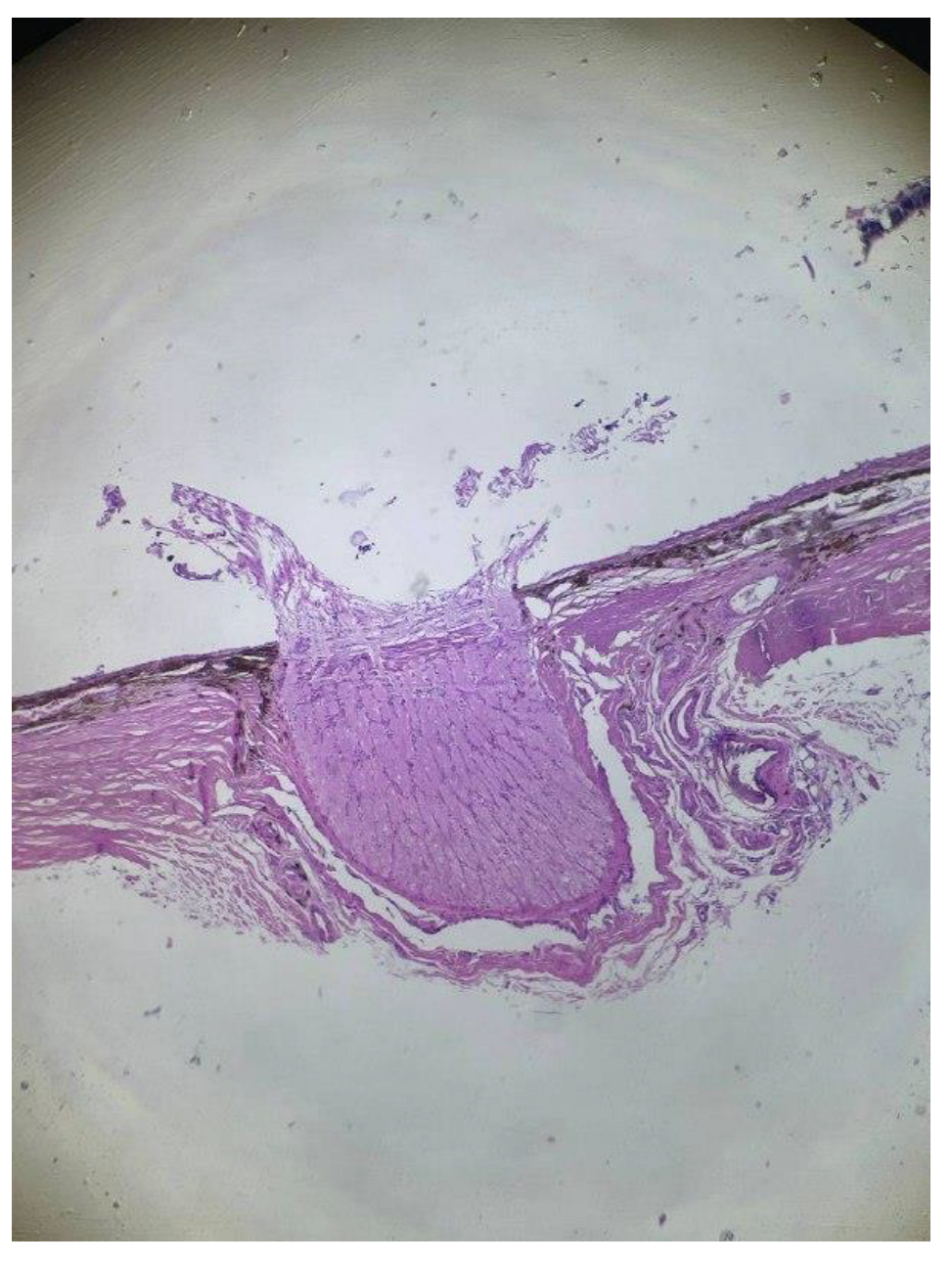
In about 94.7% of cats, histologically significant deviations in the structure of the cornea were not found (
Figure 6).
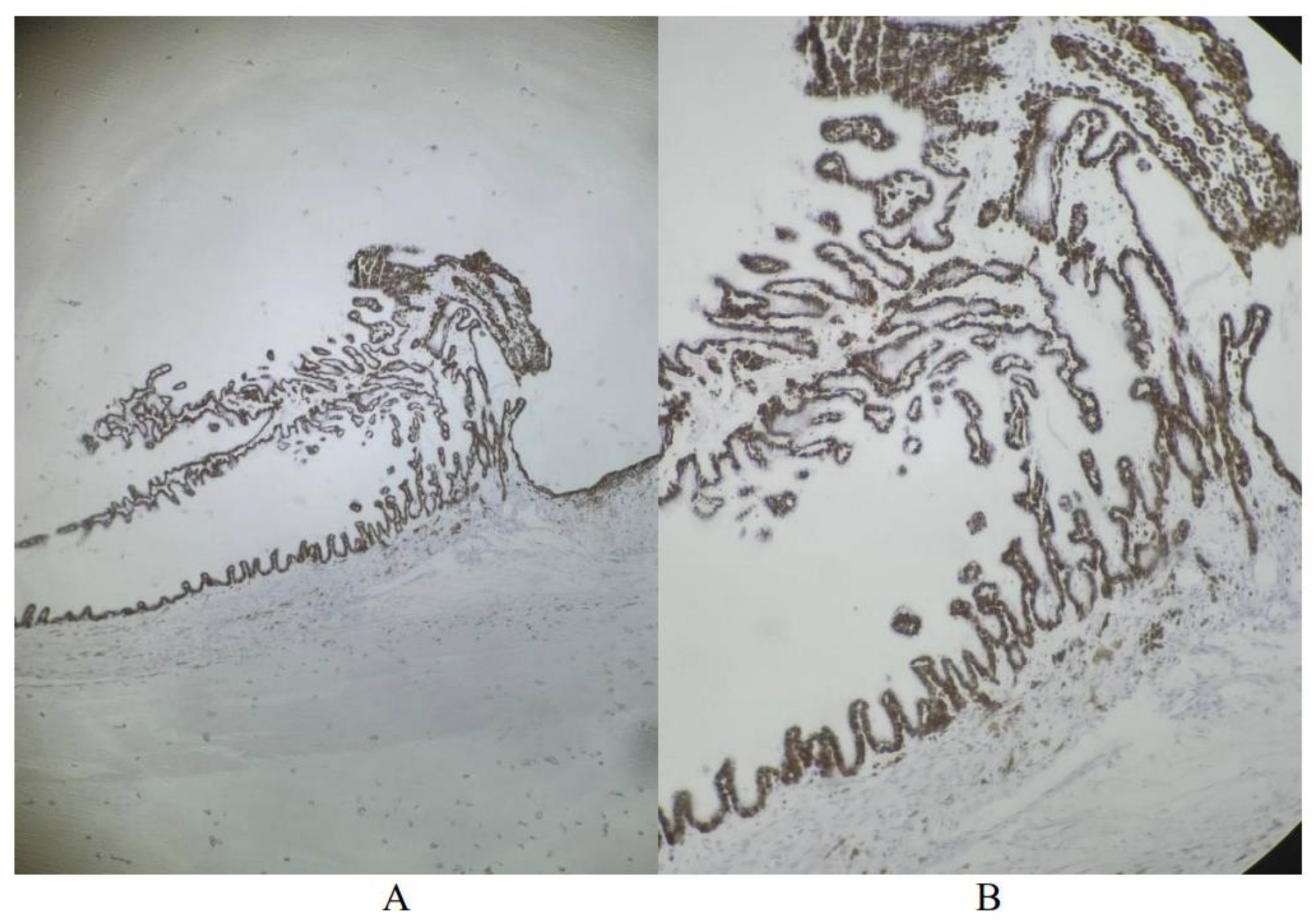
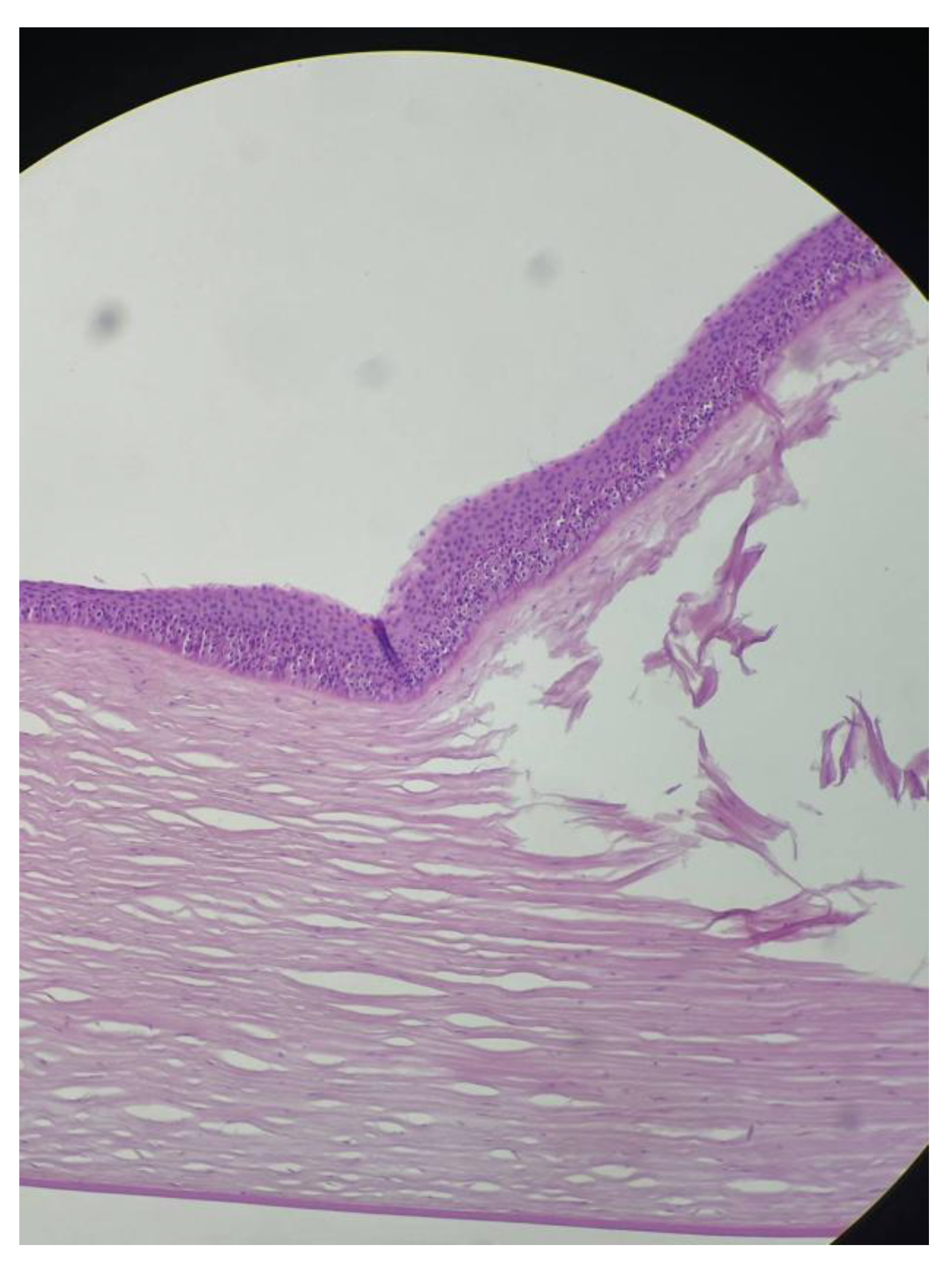
All cats had no histological findings in the choroid (
Figure 7).
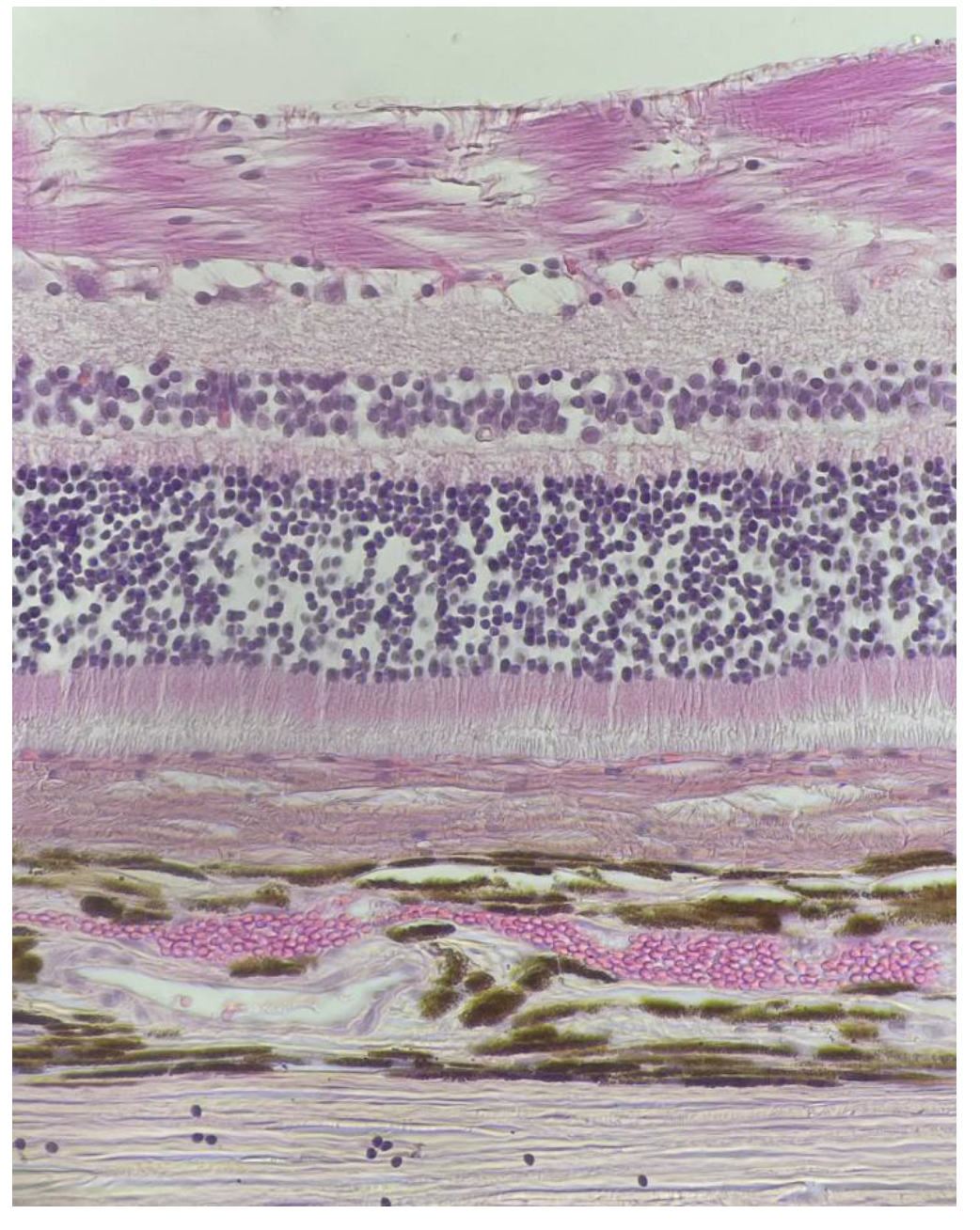
In 100.0% of cases, histological examination of the retina of cats revealed that the vessels were not dilated, without significant histological changes (
Figure 8).
The optic nerve of cats was examined in 63.2%, inflammatory infiltrate was not present (
Figure 9).
In the structure of the cornea, a single specimen of deformation of the corneal wall (artifact) and slight thickening due to hyperplasia of the anterior corneal epithelium were revealed (
Figure 10).
In the first case, a female Bengal cat, 11 years old, with a history of lymphoma, had a neoplasm of the iris, melanocytoma (
Figure 11).
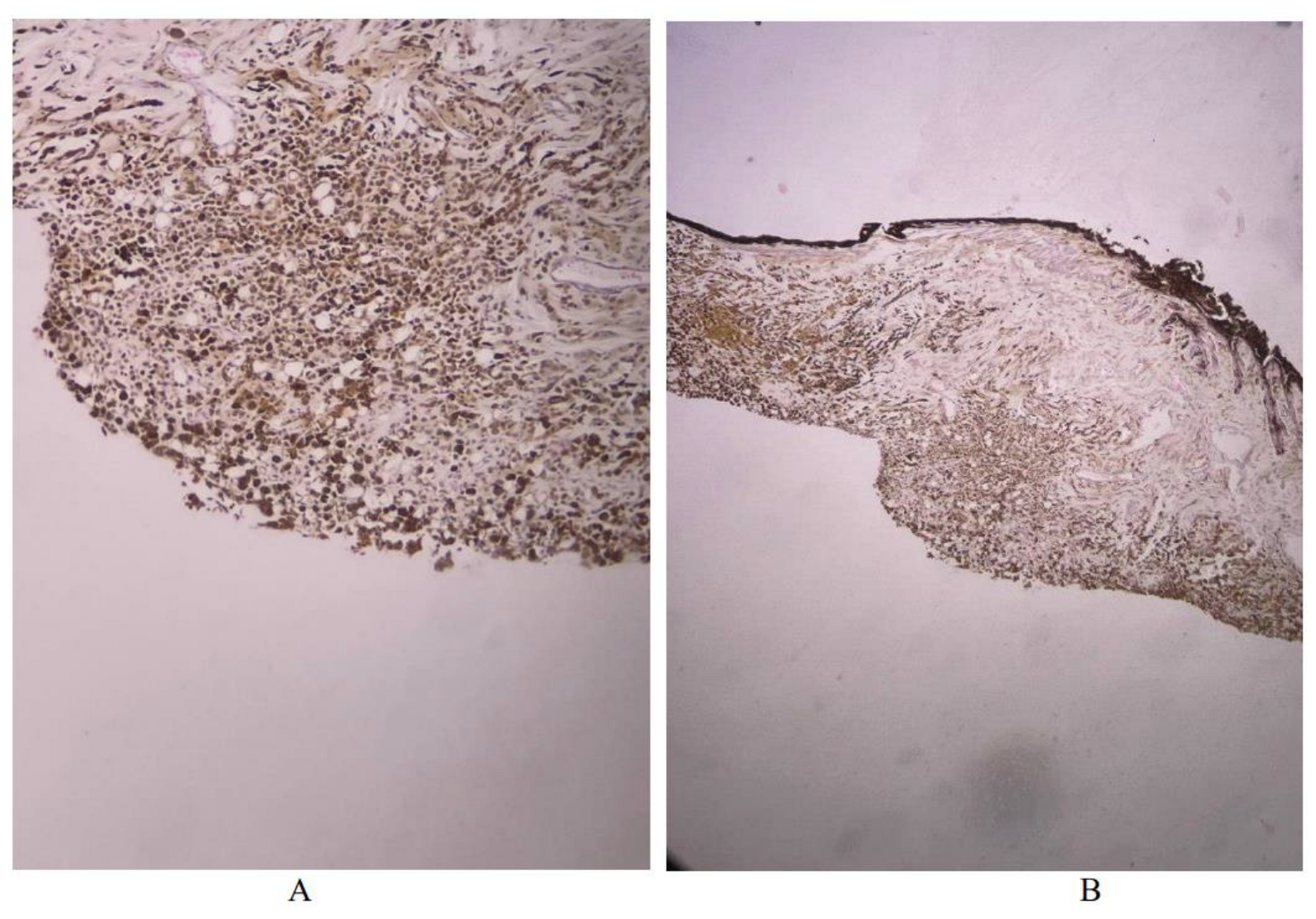
In the second case, a female Bengal cat, 11 years old, with a history of neoplasm of the eyeball, was diagnosed with melanoma (
Figure 12).
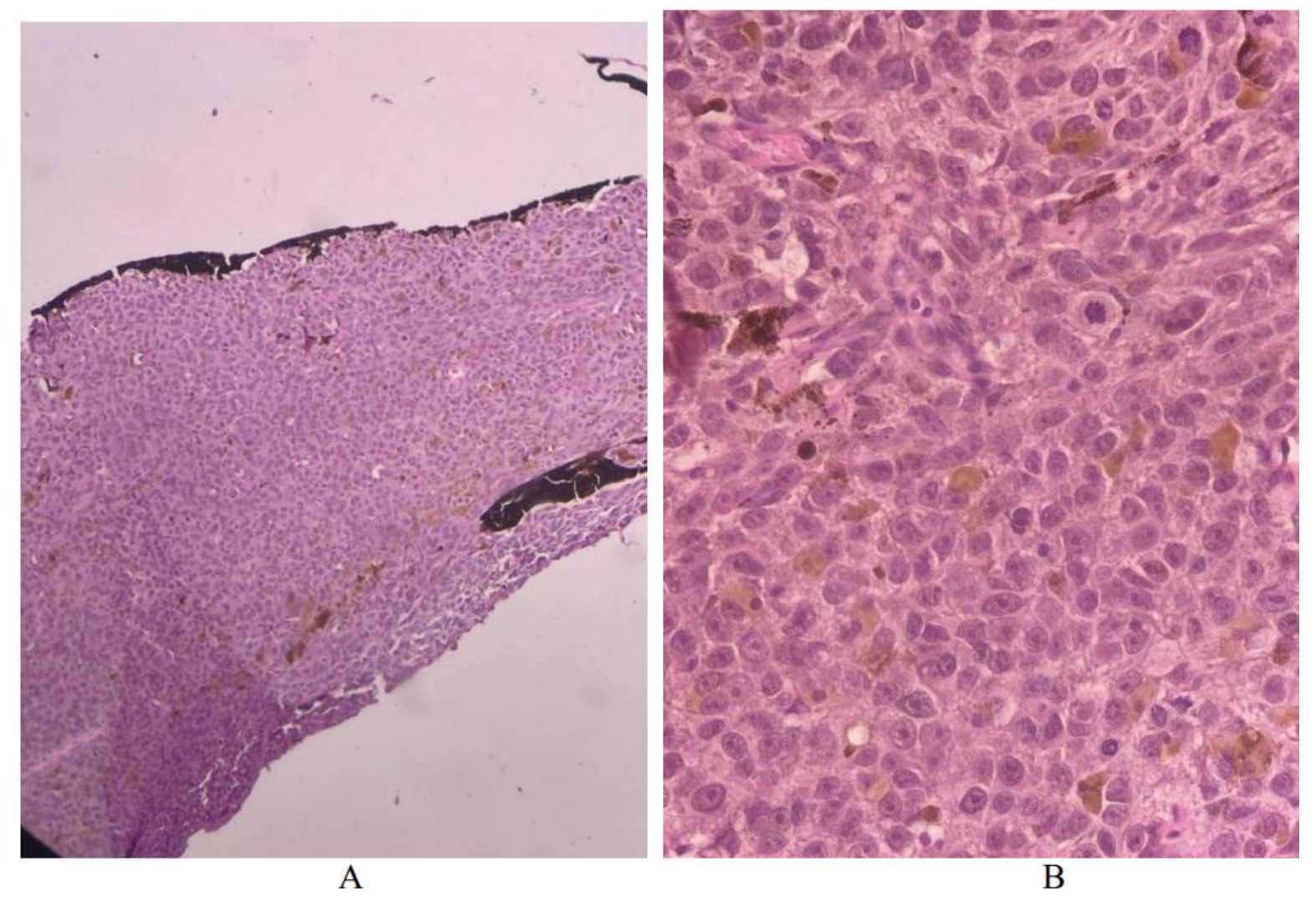
In the third case, a mixed-breed cat, 9 years 2 months old, history of neoplasm of the eye, diffuse neoplasm of the iris, melanoma was established (
Figure 13).
In the fourth case, a mixed-breed cat with a history of an intestinal neoplasm has a diffuse formation of the iris. The sections show a neoplasm of lymphoid tissue, large cell lymphoma (
Figure 14).
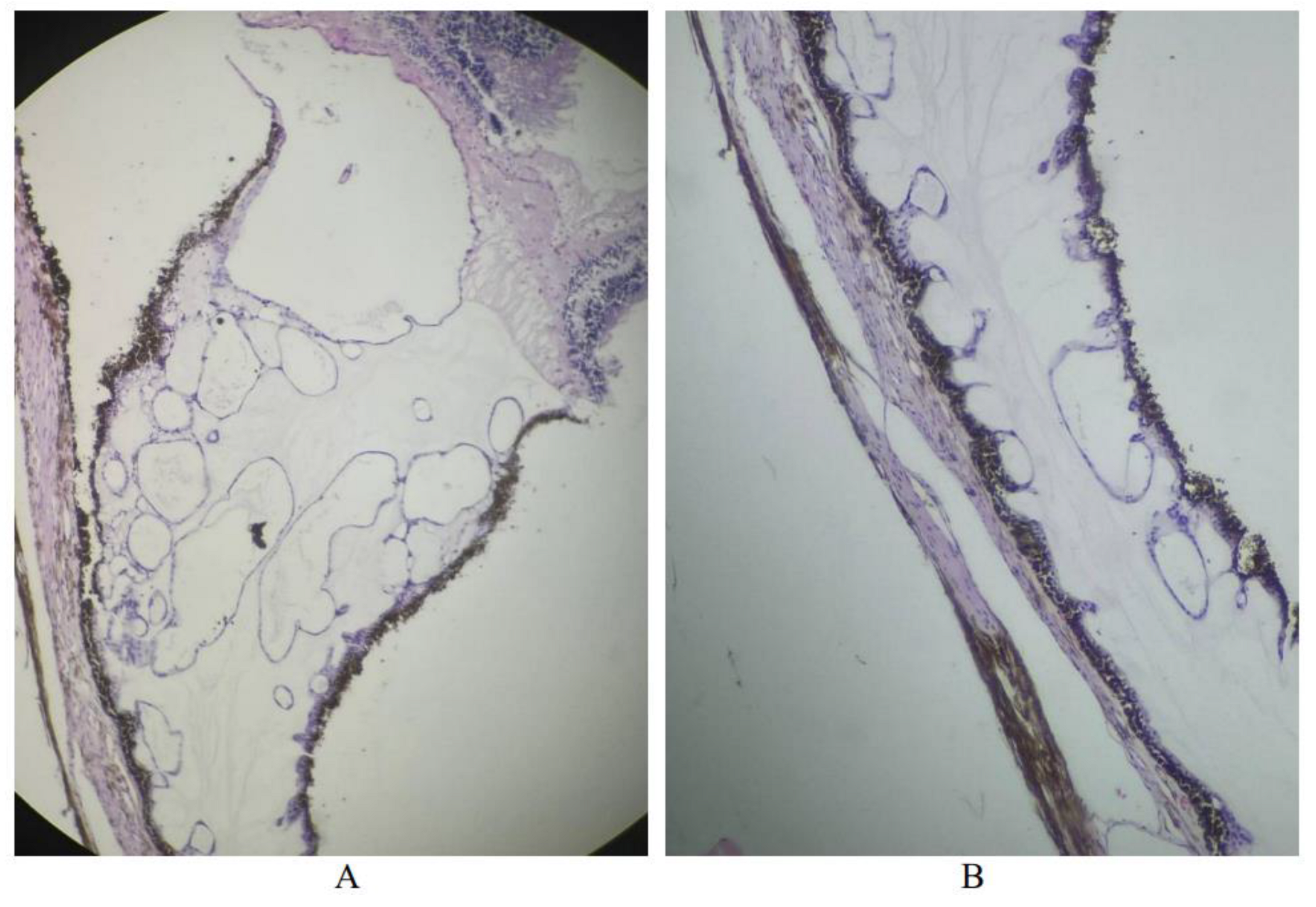
In the first case, during a histological examination of the eyeball of a mixed-breed male cat, with a history of chest neoplasm, iris cysts were noted (
Figure 15).
In the second case, during a histological examination of the eyeball of a mixed-breed female cat, 7 years old, with a history of a neoplasm of the mammary gland, cysts of the iris were also noted, however, they were less pronounced than in the previous patient (
Figure 16).
Conclusions
Histological changes were detected in 36.8% of the cats in the study sample. Histologically significant findings were detected only in the iris of the cats in the experimental group and the cornea in the control group. The iris was the most sensitive structure of the eyeball in the study. In 21.1% of cases, “histological-pathological” studies made or clarified an oncological diagnosis: melanoma, lymphoma.
Funding
The work was carried out within the framework of the topic: “Etiopathogenesis and development of methods for diagnosing, preventing and treating immune-mediated paraneoplastic ophthalmopathies in animals” (project code FSMF-2022-0003 of the Ministry of Higher Education and Science of the Russian Federation) of the Research Laboratory of Ophthalmology, Oncology and Biochemistry of Animals, Federal State Budgetary Educational Institution of Higher Education “Russian Biotechnological University (ROSBIOTECH)”. (Moscow, Russia)
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, internationally recognized guidelines (concerning experiments with animals), and approved by the Institutional Review Board of the Institute of Veterinary Medicine, Veterinary Sanitary Expertise and Agrosafety of the Federal State Budgetary Educational Institution of Higher Education “Russian Biotechnological University (ROSBIOTECH)” (protocol code 11_2022, Moscow, 125080, Russia and date of approval: 7 November 2022).
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
References
- Teuvazhukova D.A., Arutyunyan L.L., Tlupova T.G. Clinical and functional eye condition changes in the dry form of age macular degeneration depending on the AREDS stage. Russian Ophthalmological Journal. 2024;17(1):62-67. [CrossRef]
- Aprelev A.E., Abdulgazizova Z.F., Zakirova I.I., Aprelev A.A. Prevalence of neoplasms of the eye, its adnexa and orbit according to the ophthalmology department No. 2 of the Orenburg Regional Clinical Hospital No. 1". Orenburgskiy meditsinskiy vestnik. 2019; 7, 3(27): 5-9. Available online: https://cyberleninka.ru/article/n/rasprostranennost-novoobrazovaniy-glaza-ego-pridatochnogo-apparata-i-orbity-po-dannym-oftalmologicheskogo-otdeleniya-2-gbuz.
- Yarovoy A.A., Golubeva O.V. Interstitial brachytherapy for orbital tumors (literature review). Meditsinskaya radiologiya i radiatsionnaya bezopasnost'. 2011; 56(6): 68-76. Available online: https://elibrary.ru/item.asp?id=22625712.
- Dobson D.M., Mellanbi R., Bejkon N. Oncology of dogs and cats. Moscow: Akvarium-Print; 2017. 448 p.
- Khyul'ya G.S. Ophthalmological manifestations of systemic oncological diseases. Tochka zreniya. Vostok - Zapad. 2019; 4: 23-26. [CrossRef]
- Boginskaya O.A., Pershin B.S., Smirnova A.B. Clinic, diagnosis and treatment of paraneoplastic syndromes in ophthalmology. Rossiyskaya pediatricheskaya oftal'mologiya. 2015; 10(4): 26-31. Available online: https://cyberleninka.ru/article/n/klinika-diagnostika-i-lechenie-paraneoplasticheskih-sindromov-v-oftalmologii.
- Trofimcov D.V., Vilkovyskij I.F., Kornjushenkov E.A. Small Animal Oncology. Moskva: Izdatel'skij dom «Nauchnaja biblioteka»; 2017. 574 p.
- Solomahina L.A. Oftal'mologicheskie projavlenija virusnoj lejkemii koshek. Veterinarija, zootehnija i biotehnologija. 2016;12: 35-42. Available online: https://cyberleninka.ru/article/n/oftalmologicheskie-proyavleniya-virusnoy-leykemii-koshek.
- Shul'ga, E.S. Intraocular lymphoma and its manifestations in small domestic animals. Izvestiya Orenburgskogo gosudarstvennogo agrarnogo universiteta. 2019; 1(75): 131-132. Available online: https://cyberleninka.ru/article/n/vnutriglaznaya-limfoma-i-eyo-proyavleniya-u-melkih-domashnih-zhivotnyh.
- Kovalcuka L., Sarpio L., Nikolajenko M. Comparison of five conjunctival cytology sampling methods in normal cat eyes. Vet. World. 2023 Apr; 16(4): 779-785. [CrossRef]
- Kartashov S., Rakitjanskaya A., Petrova M., Sultanova M., Oboeva M. Cytological diagnosis of infectious conjunctivitis in cats. E3S Web of Conferences. 2019; 135: 01073. [CrossRef]
- Alroy J., Bachrach A.Jr., Thalhammer J.G., Panjwani N., Richard R., DeGasperi R., Warren C.D., Albert D.M., Raghavan S.S. Clinical, neurophysiological, biochemical and morphological features of eyes in Persian cats with mannosidosis. Virchows Arch B Cell Pathol Incl Mol Pathol. 1991; 60(3): 173-80. [CrossRef]
- Lütjen-Drecoll E., Narfström K. Morphological changes in the anterior segment of the Abyssinian cat eye with hereditary rod-cone degeneration. Curr Eye Res. 2005; 30(10): 855-62. [CrossRef]
- Lucyshyn D.R., Vernau W., Maggs D.J., Murphy C.J., Leonard B.C. Correlations between clinical signs and corneal cytology in feline eosinophilic keratoconjunctivitis. Vet Ophthalmol. 2021; 00: 1–7. [CrossRef]
- Lim Christine, Brazzell Jennifer. (2020). Ocular Cytology of the Cat // Veterinary Cytology. [CrossRef]
- Saakyan S.V., Svirina I.V., Tsygankov A.Yu., Zharov A.A., Izmailova N.S. Clinical and morphological features and the assessment of survival in patients with iris melanoma. Russian Ophthalmological Journal. 2024;17(1):47-54. [CrossRef]
Figure 1.
Gastrointestinal paraneoplastic syndrome : A - ulcers, from B to E - hemorrhages on the mucous membrane.
Figure 1.
Gastrointestinal paraneoplastic syndrome : A - ulcers, from B to E - hemorrhages on the mucous membrane.
Figure 2.
Ophthalmological syndrome in oncopathies: A - blepharitis, catarrhal conjunctivitis, vascular keratitis, B - purulent conjunctivitis, decreased tear production.
Figure 2.
Ophthalmological syndrome in oncopathies: A - blepharitis, catarrhal conjunctivitis, vascular keratitis, B - purulent conjunctivitis, decreased tear production.
Figure 3.
Macrophotographs of circular sections of the eyeball and organs: A - the eyeball and jaw of a cat, mixed breed, female, 14 years old, diagnosed with jaw neoplasm; B - circular sections of the eyeball and lung of a cat, Bengal, female, 11 years old, diagnosed with lymphoma.
Figure 3.
Macrophotographs of circular sections of the eyeball and organs: A - the eyeball and jaw of a cat, mixed breed, female, 14 years old, diagnosed with jaw neoplasm; B - circular sections of the eyeball and lung of a cat, Bengal, female, 11 years old, diagnosed with lymphoma.
Figure 4.
Micrograph of lung tissue of a female Bengal cat, 11 years old, diagnosed with lymphoma (staining, 10x10).
Figure 4.
Micrograph of lung tissue of a female Bengal cat, 11 years old, diagnosed with lymphoma (staining, 10x10).
Figure 5.
Micrographs of squamous cell carcinoma in a male cat, crossbreed (staining, 10x10).
Figure 5.
Micrographs of squamous cell carcinoma in a male cat, crossbreed (staining, 10x10).
Figure 6.
Cornea of a cat, control group (staining, 10x40).
Figure 6.
Cornea of a cat, control group (staining, 10x40).
Figure 7.
Choroid of a male, crossbreed cat, 15 years 4 months, history of bladder sarcoma. Ciliary body (staining): A - 10x2; B - 10x20.
Figure 7.
Choroid of a male, crossbreed cat, 15 years 4 months, history of bladder sarcoma. Ciliary body (staining): A - 10x2; B - 10x20.
Figure 8.
Retina of a crossbreed, cat, history of neoplasm in the chest cavity (staining, 10x40).
Figure 8.
Retina of a crossbreed, cat, history of neoplasm in the chest cavity (staining, 10x40).
Figure 9.
The exit of the optic nerve of a cat (from control group) without histological changes (staining, 10x20).
Figure 9.
The exit of the optic nerve of a cat (from control group) without histological changes (staining, 10x20).
Figure 10.
Hyperplastic corneal epithelium of a control group cat (staining, 10x20).
Figure 10.
Hyperplastic corneal epithelium of a control group cat (staining, 10x20).
Figure 11.
Micrographs of the iris of a female Bengal cat, 11 years old, with a history of lymphoma. Melanocytoma (staining): A - 10x10, B - 10x20.
Figure 11.
Micrographs of the iris of a female Bengal cat, 11 years old, with a history of lymphoma. Melanocytoma (staining): A - 10x10, B - 10x20.
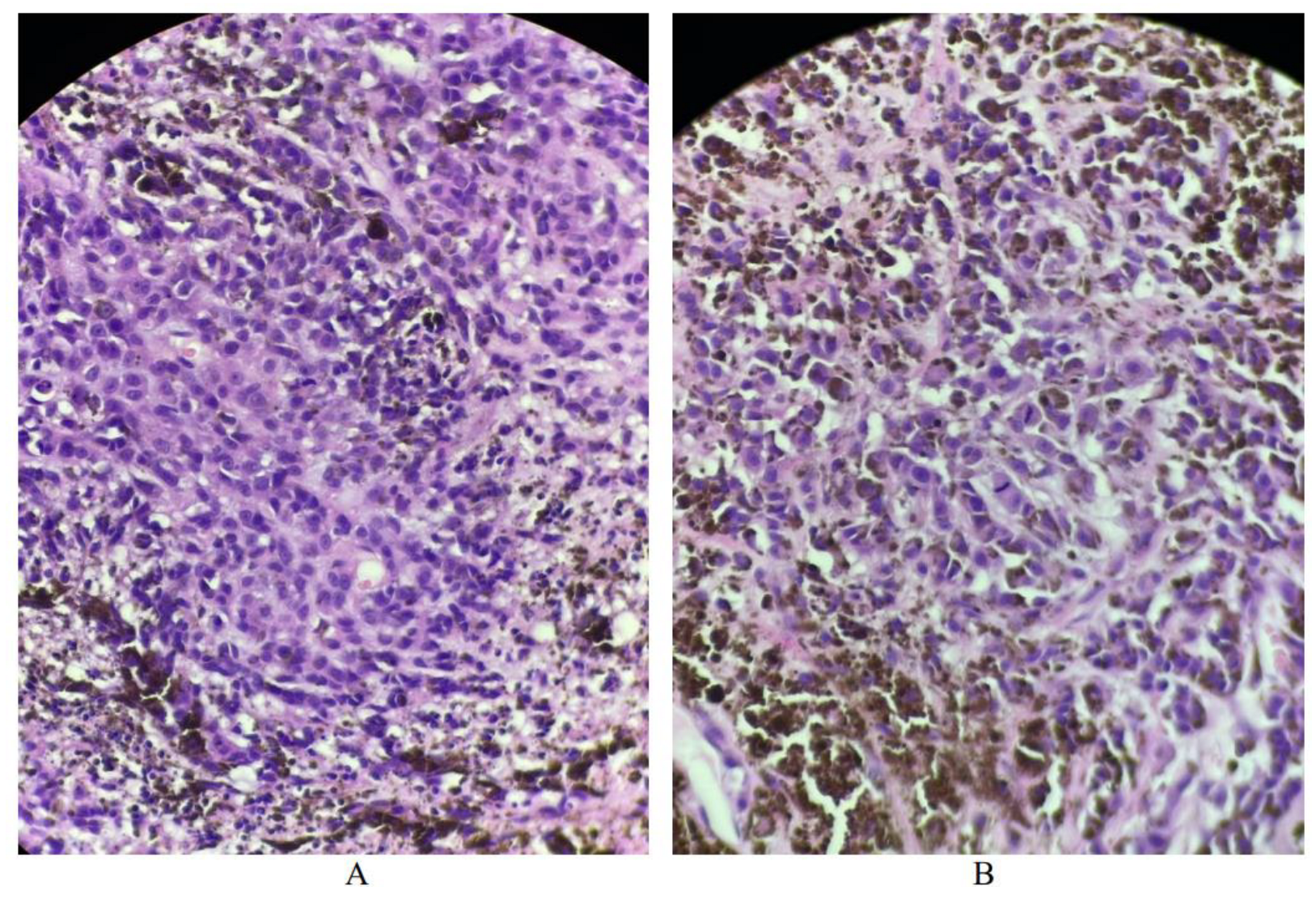
Figure 12.
Micrographs of iris melanoma in a female Bengal cat, 11 years old, history of neoplasm of the eyeball (staining): A - neoplasm (10x20), B - mitotic activity and cells with pigment (melanin) (10x40).
Figure 12.
Micrographs of iris melanoma in a female Bengal cat, 11 years old, history of neoplasm of the eyeball (staining): A - neoplasm (10x20), B - mitotic activity and cells with pigment (melanin) (10x40).
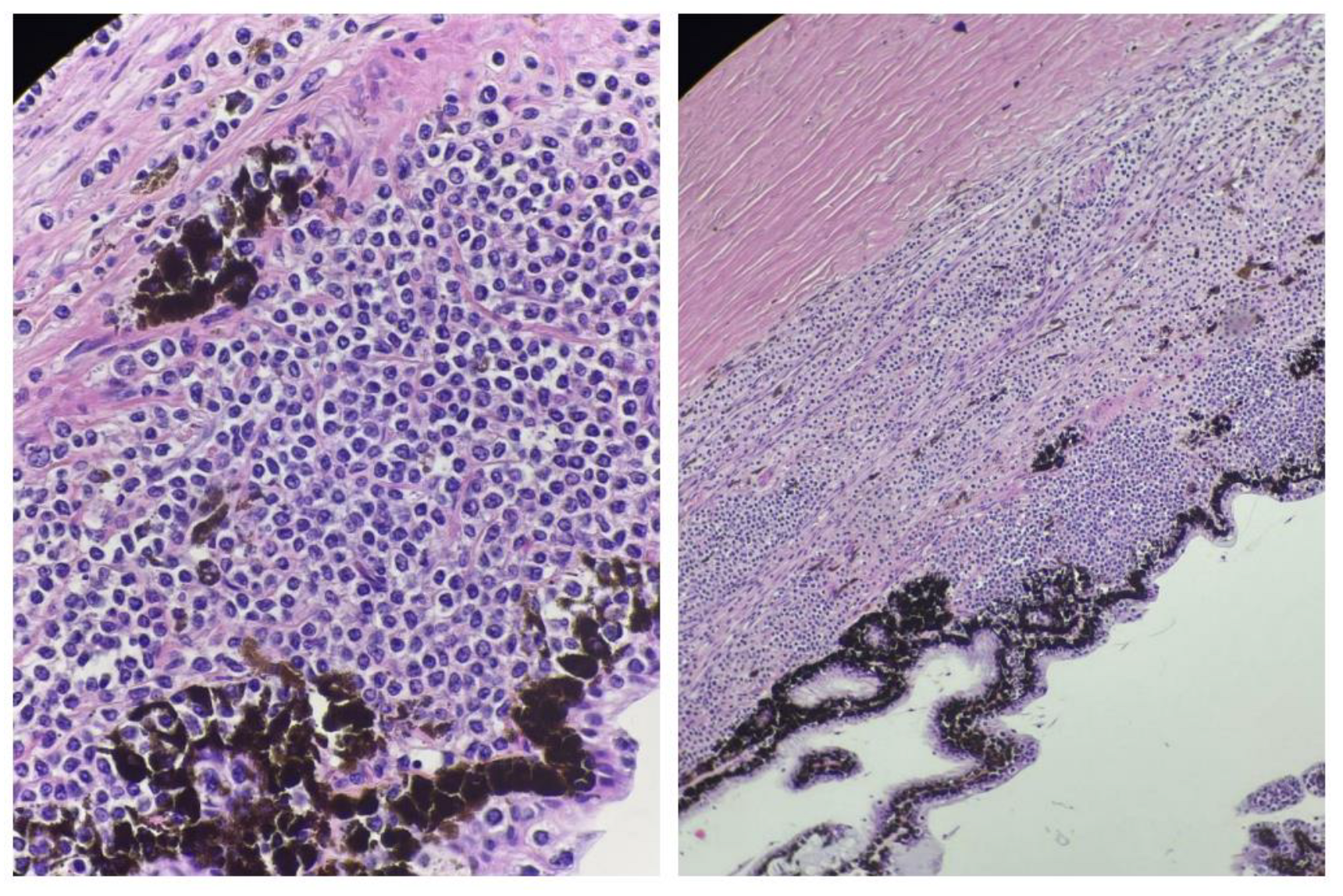
Figure 13.
Micrographs of a neoplasm in a mixed-breed cat (9 years 2 months) with a history of an eye neoplasm (staining): A - neoplasm (10x20), B - mitotic activity and cells with pigment (melanin) (10x40).
Figure 13.
Micrographs of a neoplasm in a mixed-breed cat (9 years 2 months) with a history of an eye neoplasm (staining): A - neoplasm (10x20), B - mitotic activity and cells with pigment (melanin) (10x40).
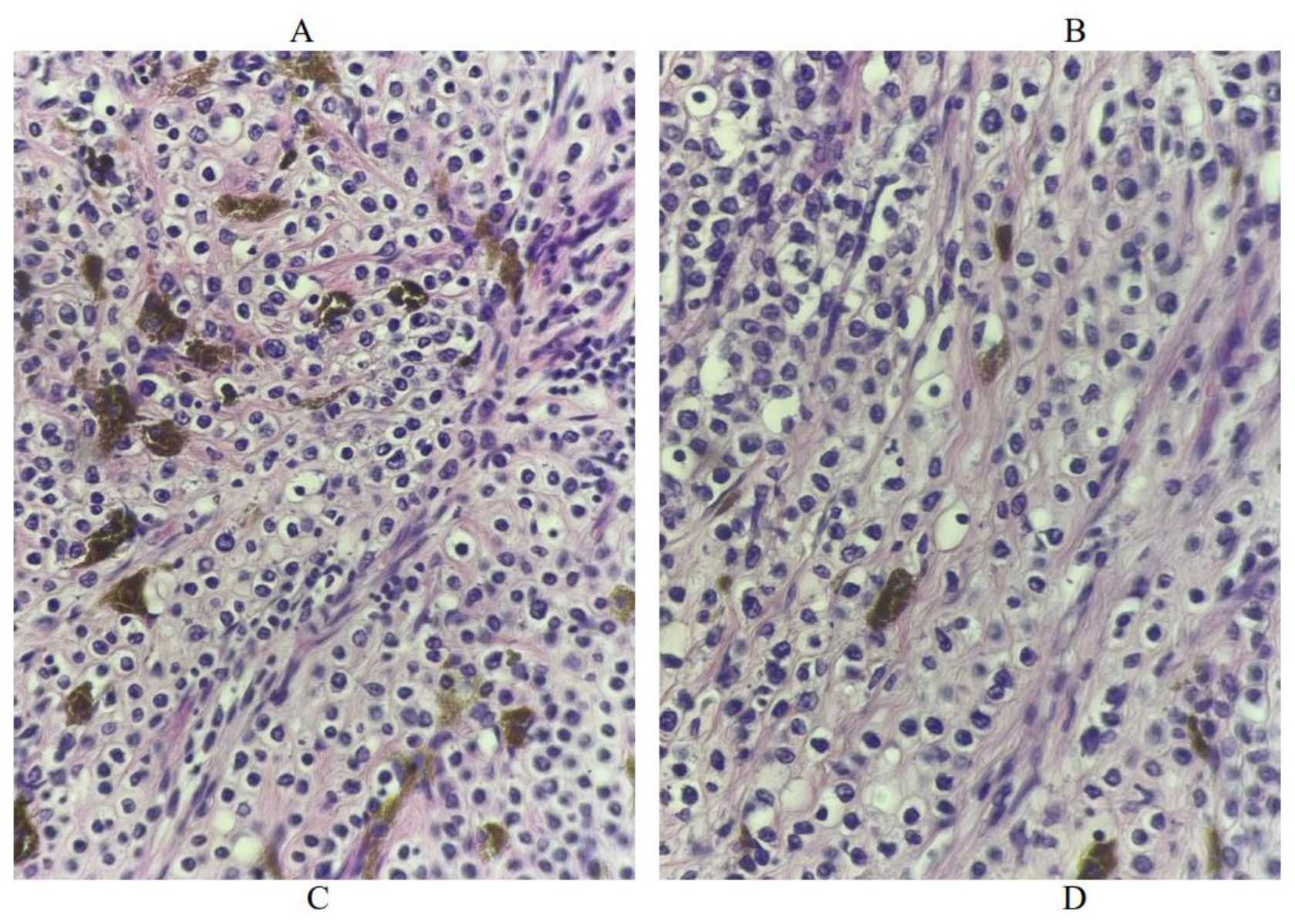
Figure 14.
Microphotographs of a neoplasm in a mixed-breed cat, with a history of intestinal neoplasm (staining): neoplasm A – 10x10, B – 10x20, C, D – mitotic activity and cells with pigment (melanin) (10x40).
Figure 14.
Microphotographs of a neoplasm in a mixed-breed cat, with a history of intestinal neoplasm (staining): neoplasm A – 10x10, B – 10x20, C, D – mitotic activity and cells with pigment (melanin) (10x40).
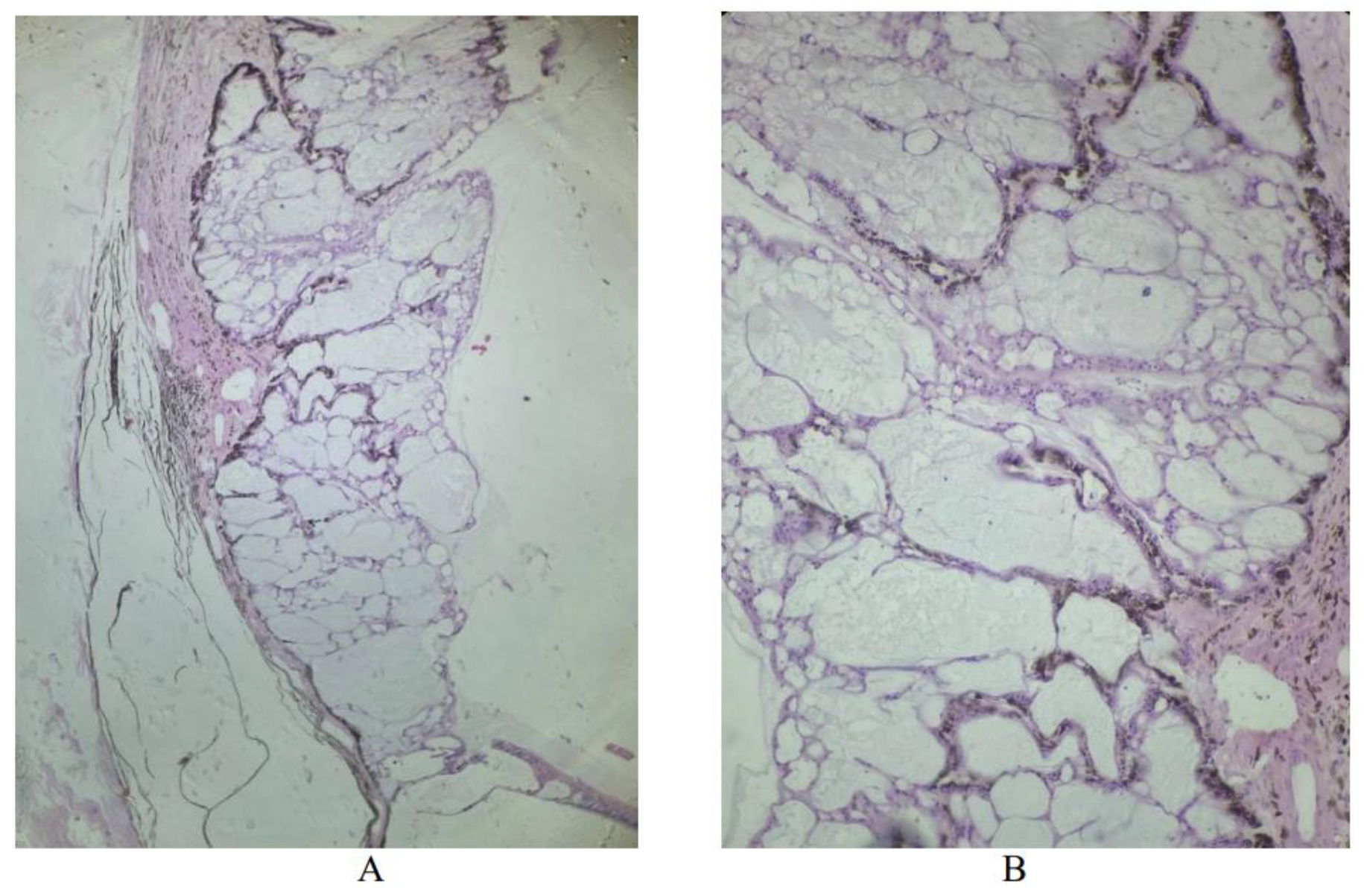
Figure 15.
Cystic cavities of the iris of a mixed-breed cat with a history of a neoplasm of the chest cavity, filled with eosinophil substance (staining) : A - 10x20, B - 10x10.
Figure 15.
Cystic cavities of the iris of a mixed-breed cat with a history of a neoplasm of the chest cavity, filled with eosinophil substance (staining) : A - 10x20, B - 10x10.
Figure 16.
Cystic cavities of the iris of a female mixed-breed cat, 7 years old, with a history of breast neoplasm, filled with eosinophil substance (staining) : A - 10x20, B - 10x10.
Figure 16.
Cystic cavities of the iris of a female mixed-breed cat, 7 years old, with a history of breast neoplasm, filled with eosinophil substance (staining) : A - 10x20, B - 10x10.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).