1. Introduction
Patellofemoral pain syndrome (PFPS) represents a frequent knee joint disorder seen in clinical settings. Collins et al. suggest expanding research into patellofemoral pain syndrome as a means of reducing the impact of knee injuries [
1]. PFPS is a prevalent knee pain affecting both adults and young individuals, including those who lead an active and healthy lifestyl [
2]. Pain caused by PFPS is often worsened by prolonged sitting or climbing stairs. This has a significant impact on a person’s daily activities [
3]. The presence of pain has been shown in a meta-analysis upon squatting was the most sensitive physical examination assessment for PFPS [
4]. The cause of PFPS is unknown but most likely is the outcome of a number of different factors, including training techniques. According to research, four significant factors contribute to the condition: imbalances in the lower extremity or patella, muscle imbalances in the lower extremity, overuse, and traumatic events. [
5]. Of these four factors, overuse is the cause in the vast majority of cases [
6].
A systematic review found that lower quadriceps strength is associated with a significantly higher proportion of patellar instability-related knee pain. [
7]. There is compelling evidence that muscle imbalances have a pivotal role in the development of PFPS. [
3]. Many previous studies have focused on the dysfunction of the vastus medialis oblique (VMO) and vastus lateralis (VL) muscles in PFPS patients, as these muscles attach directly to the patella [
8,
9]. Such studies have shown that an asymmetry in the activation of the VMO and VL muscles is associated with lateral patellar tracking in patients with PFPS [
8,
9].
Knee valgus is another mechanism associated with PFPS. With knee valgus, a knee will collapse medially due to pronounced supination, internal rotation, external rotation, or both [
10]. The outward force on the patella increases and leads to hallux valgus. Female athletes are at a greater risk of presenting with dynamic valgus, potentially elucidating the higher rate of PFPS incidence in women [
11]. Several studies indicate that valgus deformity of the knee is not due to the knee joint, but rather to the weak hip abductors causing internal femur rotation. [
12].
PFPS is typically treated conservatively with the aim of reducing pain, improving monitoring of the patella, and reestablishing previous levels of function. Several studies indicate that exercise is a beneficial treatment for individuals with PFPS [
3,
13]. Exercise is an effective treatment; indeed, it is the most extensively researched treatment and it can specifically address the valgus malalignment that many individuals have [
4,
13,
14]. The forward lunge is a prevalent weight-bearing exercise that athletes and individuals with healthy knees use to train the hip and quadriceps muscles [
15,
16]. Physical therapists employ the forward lunge and other load-bearing exercises to restore knee function in patients afflicted with knee injuries and conditions, such as patellofemoral rehabilitation in individuals with PFPS [
17].
Several studies have suggested that enhancing hip posture and performing quadriceps exercises can be beneficial for individuals suffering from patellofemoral pain syndrome [
18,
19]. Strengthening the hip adductors improved the therapeutic benefit of PFPS by increasing strength in the hip adductors. It is therefore recommended that hip adductor strengthening exercises be included in the management of PFPS. This, in turn, lengthens the VMO and alters its length-tension characteristics. As a result, the VMO performs better with increased positive contractile force. It is also important to note that technical terms will be explained when used for the first time [
20]. However, previous research conducted in the squatting position has demonstrated that the activation of hip flexors leads to a reduction in the strength of the VL, resulting in a greater degree of PFPS [
21,
22].
Numerous studies have investigated the efficiency of hip adduction forward lunge (HADF) and hip abduction forward lunge (HABF) for the treatment of PFPS [
23,
24,
25,
26,
27]. Strengthening the VMO and VL through HADF and HABF, respectively, produces a therapeutic effect for PFPS. Hip adduction and abduction place pressure on the lateral and medial aspects of the knee, resulting in knee valgus and varus [
27]; however, few studies have investigated this in combination with VMO and VL strengthening exercises. In this study, three forward lunge positions targeting hip placement were investigated to determine their effectiveness in reducing the risk of knee injury by measuring muscle activity along with changes in the center of pressure (CoP) of the foot. We hypothesized that there would be minimal changes in CoP and minimal muscle activity in the hip neutral forward lunge (HNEF) position among the three positions examined.
2. Materials and Methods
2.1. Participants
The sample size was estimated through an a priori power analysis carried out with the G* Power program (G power program Version 3.1, Heinrich-Heine-University Düsseldorf, Germany) assuming a univariate approach for within effects. In a preliminary study, a power of 0.81, an effect size (ES) of 0.82, and a significance level of 0.05 suggested a sample size of 18. To allow for a possible dropout rate of 10-20%, the projected sample size has been set at 20. The recruitment period of this study was conducted at the university between September and October 2022. Participants were excluded by the criteria as follows: (1) current or previous knee injury or patellofemoral pathology; (2) If the participant has experienced pain in the knee during recreational activities or during everyday activities, such as stepping forward, within the last three months. and (3) if their BMI was over 30. The human subjects authorization form, approved by the university, was read and signed by all participants to taking part in the study and were informed of their right to withdraw. All participants also signed a consent form before the investigation proceeded. The Institutional Review Board at Daegu University granted approval for the study (approval number: 1040621–202207-HR-068).
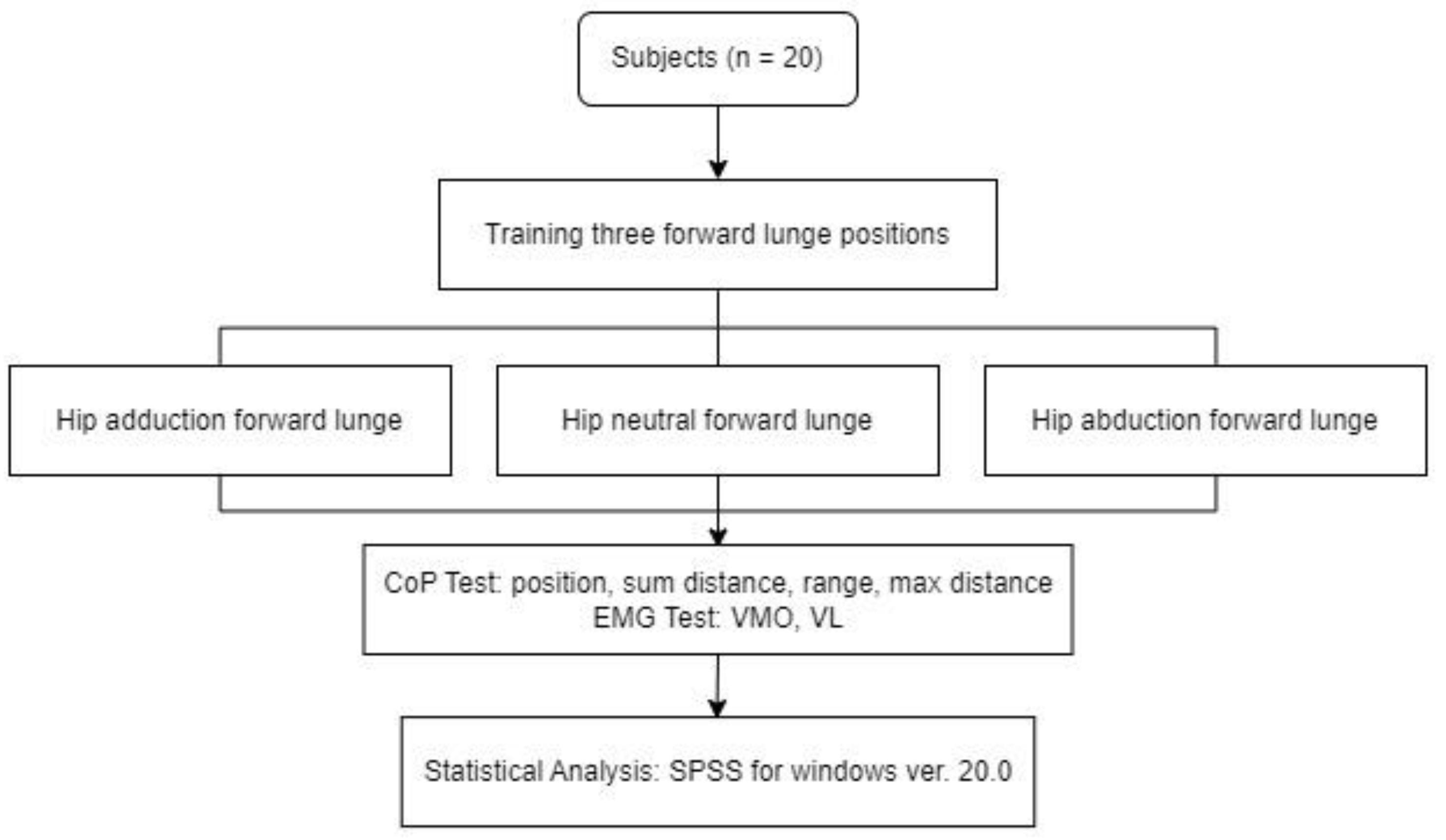
2.2. Study Procedure
2.2.1. Study Design
Twenty participants were recruited for this study. Before the study commenced, participants completed a standardized 5 min warm-up that entailed lunge forwards with a multi-plane movement of the hip. Then they were provided with instructions to familiarize themselves to record and practice the measurements of CoP (position, sum distance, range, and max distance) and VMO and VL muscle activity so that they could execute the movements correctly. Then, while performing the HNEF, HADF, and HABF, both VMO and VL muscle activity and the CoP were recorded. Three repetitions of the three positions were performed in randomized order. There was a 1 min rest between repetitions. A 5 min recovery period was included before assuming a new position, to prevent muscle fatigue (
Figure 1).
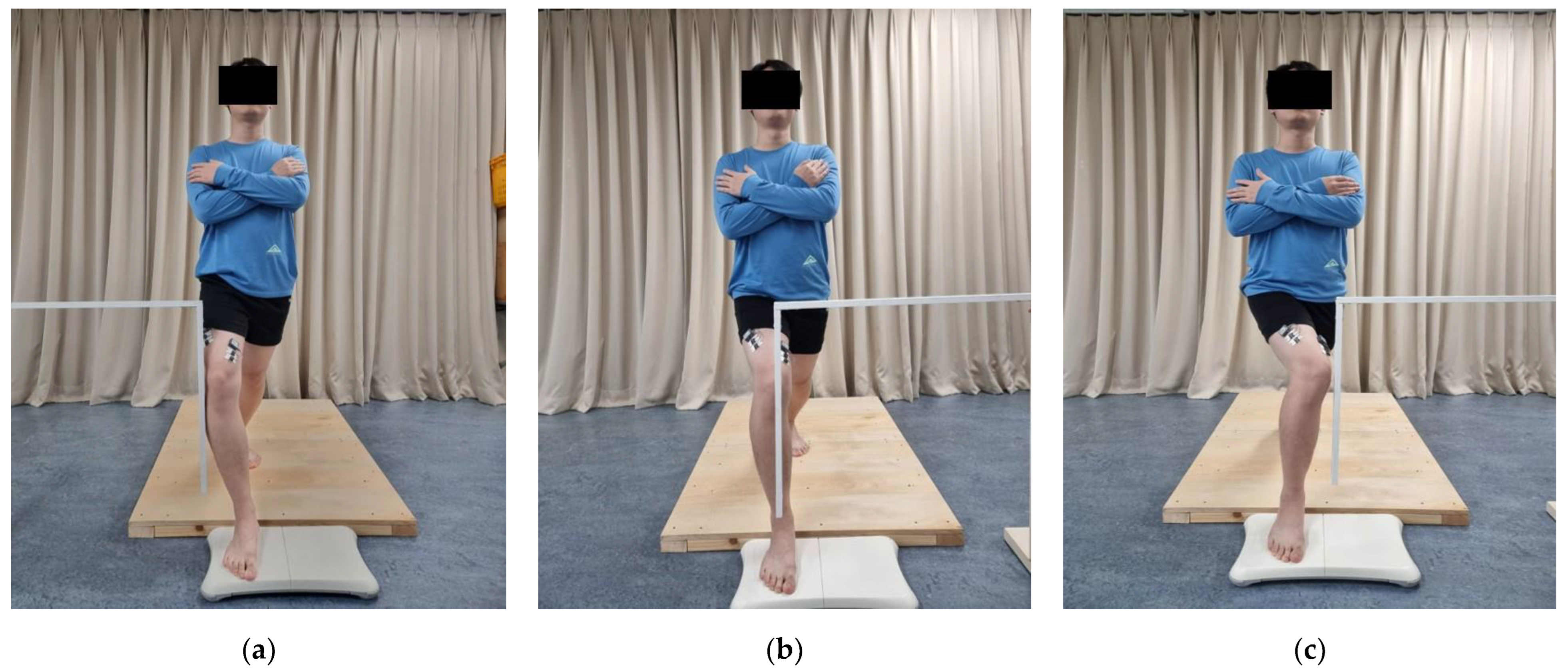
2.2.2. Three Forward Lunge Positions
When standing on both legs, the participant was instructed to take a step forward with the dominant lower limb while flexing the knee joint to a 60° angle. The lower leg maintained a perpendicular position to the ground while producing peak hip adduction or abduction or neutral displacement, with no pelvic shift. Enabling the participants to carry out various hip adduction, abduction and neutral motions prior to the assessment and inserting a guide plate into position helped ascertain the distance of the peak hip adduction, peak abduction and neutral. The guide plate was touched by the subject during measurement to achieve peak hip adduction, peak abduction and neutral distance. The opposite leg was extended, with the heel fixed to the ground. Then the patient held his or her hands together over the chest and stood up straight, facing straight ahead.
2.3. Measurements
2.3.1. Measurement of the CoP
A Balancia measuring device (version 2.0; Mintosys, Seoul, Korea) was used to assess the CoP of the three movements. The participant performed the forward lunge while placing his or her front leg on a “Wii Balance Board” and the back leg on a hard board of the same height. In measuring the CoP, we collected four types of data: position of the average CoP point on the frontal plane within 5 s (position); sum of the CoP positions at each time point on the frontal plane within 5 s at 0.01 s intervals (sum distance); the distance between the maximum and minimum of the CoP moving on the frontal plane within 5 s (range); and the maximum value of the CoP moving to the distance from the starting position on the frontal plane within 5 s (max distance). The position represents the size of the CoP moving on the frontal plane. The sum distance represents the direction and trend of the CoP moving on the frontal plane. The range represents the distance of the CoP from the medial to the lateral within the frontal plane. The max distance represents the distance at which the starting point is the standard and the distance away from the CoP reaches a maximum. Positive numbers represent lateral direction in the frontal plane, and negative numbers represent medial direction in the frontal plane.
2.3.2. Measurement of the Muscle Activity
To quantify the muscle activity of the individual’s VMO and VL, data were gathered using wireless surface electromyography (EMG) (TeleMyo DTS; Noraxon Inc, Scottsdale, AZ, USA). For each movement, electromyography signals were collected for five seconds. The initial and final second of data have been removed, leaving only a three-second analysis. Electromyography was recorded for three trials and the results were averaged. A one-minute break was permitted between each recording. The acquired data were expressed as a percentage of the root mean square of the maximum voluntary isometric contraction (% MVIC). A maximal voluntary isometric contraction (MVIC) test was performed before the patient assumed each of the three positions to ensure consistent measurement of the EMG signals from the postures. The knees were positioned against the edge of the platform, with the knees flexed at 90°. Participants were instructed to sit on an elevated platform without allowing their feet to make contact with the floor. Then they were instructed to elevate their affected legs flexed to a knee angle of 60°, and subsequently extend them to their fullest extent. To prevent any movement and to facilitate a maximal isometric contraction of the knee extension, the examiner placed his hand on the ankle of the test leg. To avoid fatiguing the muscles, the evaluation was performed three times, resting for 2 min between each trial [
28]. An electrode pad was situated 10 cm away from the patella using the connection line between the anterior superior pelvic spine and the outer edge of the patella for VL measurement. In addition, an electrode was positioned at a 50° angle along a straight line. with respect to the parallel line running between external patellar margin and anterior superior pelvic spines., 4 cm from the patella [
29]. After completing the MVIC test, participants were given a 5 min break before undergoing training in the three specific movements. CoP and muscle activity measurements were performed simultaneously. Each position was repeated three times. There was a rest period of 1 min after each movement. The participant took a 5 min break after each position trial to minimize muscle fatigue.
Figure 2.
Measurement of the CoP and the muscle activity of VMO and VL: (a) hip abduction forward lunge; (b) hip neutral forward lunge; (c) hip adduction forward lunge.
Figure 2.
Measurement of the CoP and the muscle activity of VMO and VL: (a) hip abduction forward lunge; (b) hip neutral forward lunge; (c) hip adduction forward lunge.
2.4. Statistical Analysis
Statistics were analyzed using SPSS version 20.0 for Windows (SPSS, IBM Corp., Armonk, NY, USA). All data underwent a normal distribution test using the Kolmogorov-Smirnov method. To assess the difference in muscle activity and CoP, a one-way analysis of variance was conducted. The least-squares difference was determined as a post-test to explain the differences among the three positions after the test. Statistical significance was set at P < 0.05. The ES (Cohen d) was considered weak (ES = 0.1), intermediate (ES = 0.25), or strong (ES = 0.4).
3. Results
The general characteristics of subjects are shown in
Table 1. The average age was 23.7 years old (21–31 years), average height was 169.4 cm (158–185 cm), average weight was 64.35 kg (50–100 kg), and average body mass index (BMI) was 22.3 (19.53–29.22 kg/m
2).
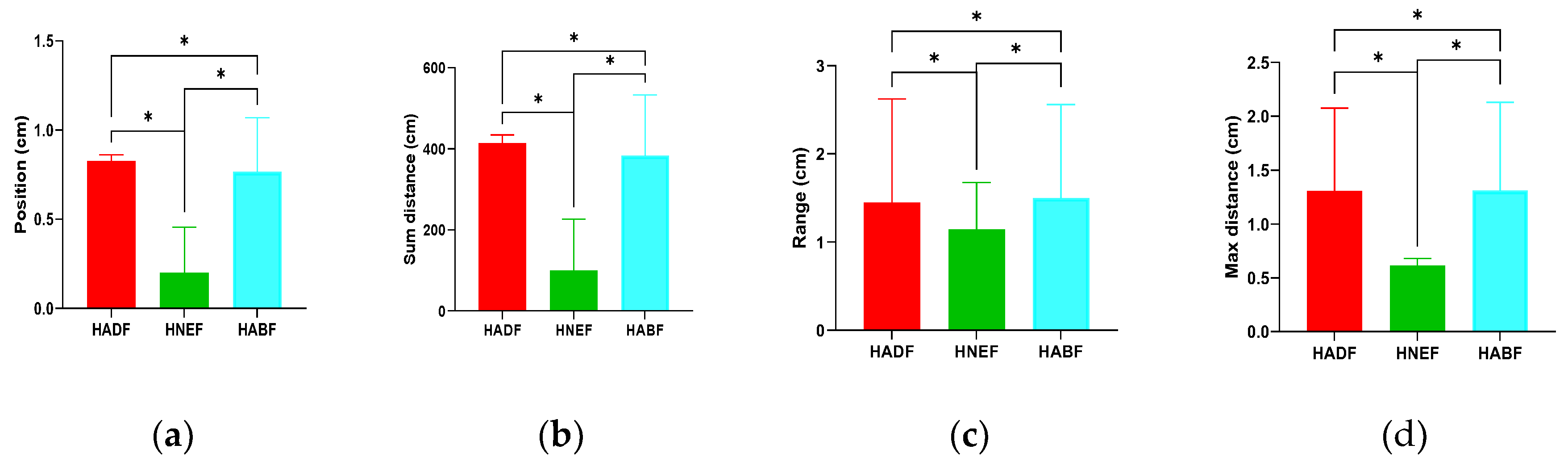
The position (ES = 3.03), sum distance (ES = 3.05), range (ES = 6.31), and max distance (ES = 5.39) significantly (p < 0.05 unless stated otherwise) differed among the three positions. The outcomes of the CoP in the HADF were all negative values; in contrast, the outcomes of the CoP in the HABF and HNEF were positive values. Judging from the size of the numbers, the HABF produced significantly higher CoP outcomes than the HADF and HNEF in position, sum distance, range, and max distance. The HNEF showed significantly higher CoP outcomes than the HADF (
Table 2) (
Figure 3).
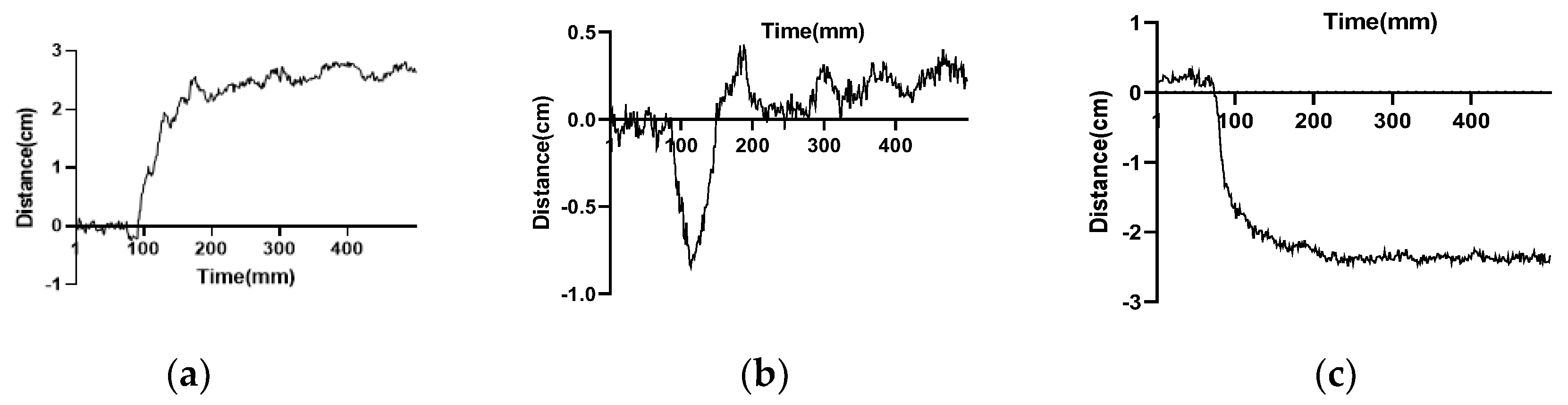
The movement trajectories of the CoP for the three postures within 5 s at intervals of 1 ms showed that the most outcomes of the CoP in the HADF were negative numbers; on the contrary, most of the CoP outcomes in the HABF were positive numbers. The movement trajectories of the CoP in the HNEF first showed negative numbers and then positive numbers (
Figure 4).
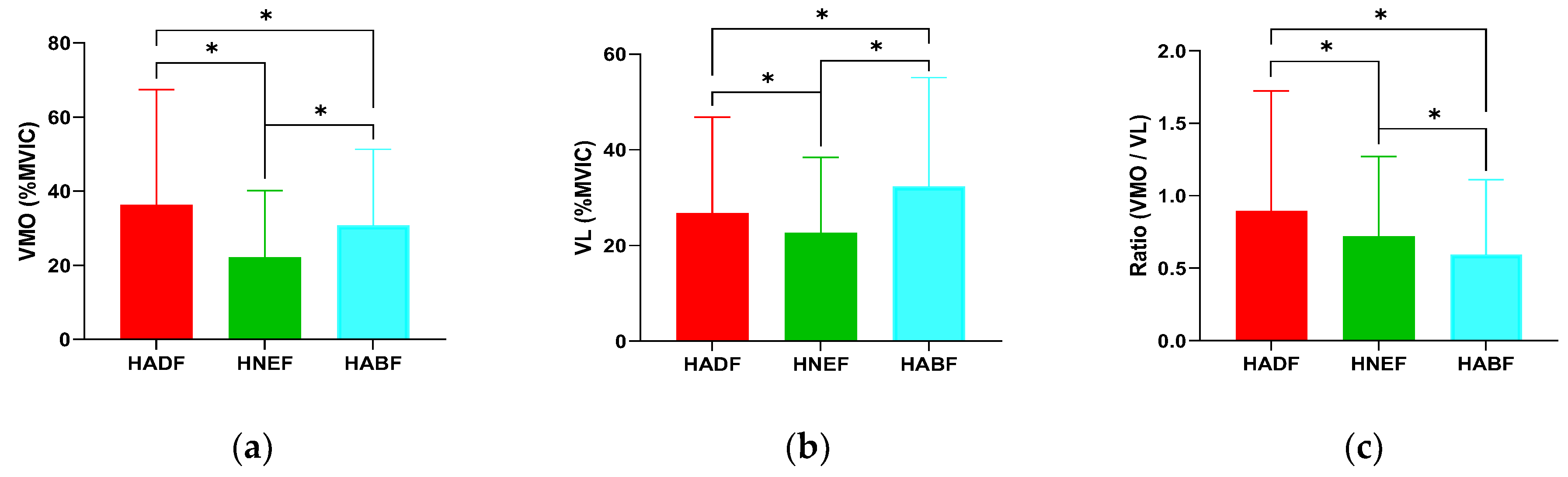
VMO (ES = 1.71) and VL (ES = 0.53) muscle activity and the ratio of VMO/VL (ES = 1.27) significantly differed among the three positions. In the VMO, the HADF produced significantly higher muscle activity (58.30 ± 14.42% MVIC) than the HABF and HNEF. The HABF (45.28 ± 16.23% MVIC) showed significantly higher muscle activity than the HNEF (34.88 ± 9.49% MVIC). In the VL, the HABF produced significantly higher muscle activity (48.44 ± 16.19% MVIC) than the HADF and HNEF. The HADF (40.98 ± 12.64% MVIC) showed significantly higher muscle activity than the HNEF (33.79 ± 11.57% MVIC). In the ratio of VMO/VL, the HADF produced significantly higher muscle activity (1.48 ± 0.31) than the HABF and HNEF. In addition, the HNEF (1.11 ± 0.33) showed significantly higher muscle activity than the HABF (0.96 ± 0.23) (
Table 3) (
Figure 5).
4. Discussion
We investigated the effect of the HADF, HABF, and HNEF on changes in CoP and quadriceps muscle activity. Out results are in line with previous studies, in that quadriceps activity and the change in CoP significantly increased for the HADF and HABF compared to the HNEF.
Based on the position and sum distance results, the CoP of the HABF moved laterally in the frontal plane, that of the HADF moved medially in the frontal plane, and that in the frontal plane for the HNEF moved minimally to zero. The alternative explanation could be a biomechanical one; specifically, when the hip joint was adducted, the lower limb moved medially, and the resulting position was reflected medially. Similarly, when the hip joint was abducted, the lower limb moved laterally, and the resulting position was reflected laterally [
30]. Because the forward lunge is a closed kinetic chain movement, the foot is immobilized when the hip is internally adducted. This causes the knee to move medially, creating a variable amount of pressure at the lateral aspect of the patellofemoral joint. At the same time, such a movement increases the risk of developing knee valgus [
31,
32]. Similar to this is the danger of knee inversion that occurs when the hip is abducted. Compared to the HABF and the HADF, evidence implies that the HNEF is more beneficial for the patellofemoral joint. According to the results of assessments of the CoP, the HNEF showed a slight lateral movement in the coronal plane, which may be explained by the fact that the CoP was in the middle of the legs during the onset of the movement. After the forward lunge, the CoP shifted forward toward the flexed leg. Because all of our subjects were right-leg dominant, the CoP of the HNEF would have shown a slight lateral movement in the coronal plane. Compared to the other two exercises, the HNEF added little significant knee valgus pressure and thus was less likely to produce valgus and varus pressures. The results of the range and max distance assessments showed that the CoP range of displacement and the maximum distance of movement in the HADF and HABF were significantly larger than those of the HNEF on the medial and lateral sides of the frontal plane. The HADF and HABF may produce a noticeable medial and lateral expansion of the knee joint, so that compared to the HNEF there is a greater distance [
30].
At the same time, the range values were larger than max distances. This suggests that the movement trajectory of the CoP does not change continuously in one direction. There was a process of reverse movement for all three positions that was larger in the HNEF than in both the HADF and HABF. The smaller reverse movement in the latter two may have been due to wobbling of the ankle joint from the adaptation process in response to the increased stress at the beginning of the forward lunge [
33]. The larger reverse movement in the HNEF may have been caused by unconscious hip adduction occurring at the beginning of the movement.
For the EMG of VMO, there were significant differences among the three positions. The muscle activity of both HADF and HABF were more effective than HNEF, and HADF was the most effective position. This behavior is in accordance with theories reported in the literature. According to Miao et al. [
34], hip adduction dilates the VMO muscle, changing its tension–length characteristics such that a greater contraction force is produced. The three adductor muscles (the longus, magnus, and brevis) make up the adductor complex [
35]. From the adductor magnus tendon, the distal part of the vastus medialis (VM) muscle is derived [
36]. The VM muscle has two components, VML and VMO, which differ in their orientation angle of muscle fibers [
36]. According to Kumar et al. [
24], strong hip adapters provide a stable origin for the VMO. Thus, when adducting the hip, the VMO participates in the motion. Greater muscle activity of the VMO was observed in the HADF condition. Mechanically, the HADF could lead to increased femoral adduction and medial rotation, which would increase the lateral patellofemoral joint vector, leading to patellar facet overload [
37].
At the same time, there were significant differences in VL among the three positions. Muscle activity was highest while performed each lunge, with that of the HADF being higher than that of the HNEF. This confirms that hip abduction exercises can improve hip abductor muscle activity [
24,
31], as reported in the literature. According to Chen et al. [
27], the lateral patellar vector increases during hip abduction due to increased VL muscle activation. For the agonist muscle to be able to provide resistance and produce movement, there must be muscular co-contraction to stabilize the motion. In a systematic study, Santos et al. [
38] discovered that strengthening the hip abductor muscles successfully lowers discomfort and enhances function. By performing exercises focused on the forward lunge with hip abduction, motor control can be reestablished, resulting in less-controlled knee movements and the onset of knee valgus in functional tasks [
23]. Due to the potential for patellar lateralization, Escamilla et al. [
39] propose that exercise training regimens for PFPS should avoid movements heavily activating the VL.
It is important to acknowledge the limitations of our study. The hip joint’s range of motion was not considered and we did not assess the activity of the frontal plane muscles of the hip. Furthermore, our study participants were young and healthy and our results may not apply to other groups. More studies are needed to determine the effects of HNEF on the CoP and quadriceps muscle activity in normal subjects and PFPS patients.
5. Conclusions
The forward lunge is an exercise used to strengthen the quadriceps muscle. In this study, HADF was the best for activating the quadriceps; however, this exercise increased the valgus pressure of the knee joint, thereby increasing the risk for knee valgus. The HNEF may be beneficial in terms of reducing the risk of injury while exercising. In addition, HNEF should be carried out with active control to prevent unconscious medial movement of the knee joint.
Author Contributions
Conceptualization, X.-H.Z.; methodology, T.-H.K.; software, X.-H.Z., X.Y. and Q.-S.T.; validation, X.-H.Z., X.Y., Q.-S.T. and T.-H.K.; formal analysis, X.-H.Z., X.Y. and Q.-S.T.; investigation, X.-H.Z., X.Y. and Q.-S.T.; resources, X.-H.Z. and T.-H.K.; data curation, X.-H.Z. and T.-H.K.; writing—original draft preparation, X.-H.Z., X.Y. and Q.-S.T.; writing—review and editing, X.-H.Z. and T.-H.K.; visualization, X.-H.Z., X.Y. and Q.-S.T.; supervision, X.-H.Z.; project administration, T.-H.K.; funding acquisition, X.-H.Z. and T.-H.K. All authors have read and agreed to the published version of the manuscript.
Funding
This research was supported by Daegu University Future Scholars Program, 2023
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board of Daegu University (IRB No. 1040621-202207-HR-068) for studies involving humans.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
All data related to this study are included in the article.
Acknowledgments
We thank our colleagues and the reviewers who provided constructive criticism on drafts of this essay.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Collins, N.J.; Barton, C.J.; van Middelkoop, M.; Callaghan, M.J.; Rathleff, M.S.; Vicenzino, B.T.; Davis, I.S.; Powers, C.M.; Macri, E.M.; Hart, H.F.; et al. 2018 Consensus statement on exercise therapy and physical interventions (orthoses, taping and manual therapy) to treat patellofemoral pain: recommendations from the 5th International Patellofemoral Pain Research Retreat, Gold Coast, Australia, 2017. Br J Sports Med, 2018, 52, 1170–1178. [Google Scholar] [CrossRef] [PubMed]
- Smith, B.E.; Selfe, J.; Thacker, D.; Hendrick, P.; Bateman, M.; Moffatt, F.; Rathleff, M.S.; Smith, T.O.; Logan, P. Incidence and prevalence of patellofemoral pain: A systematic review and meta-analysis. PLoS One, 2018, 13, e0190892. [Google Scholar] [CrossRef] [PubMed]
- Crossley, K.M.; van Middelkoop, M.; Callaghan, M.J.; Collins, N.J.; Rathleff, M.S.; Barton, C.J. 2016 Patellofemoral pain consensus statement from the 4th International Patellofemoral Pain Research Retreat, Manchester. Part 2: recommended physical interventions (exercise, taping, bracing, foot orthoses and combined interventions). Br J Sports Med, 2016, 50, 844–852. [Google Scholar] [CrossRef] [PubMed]
- Nunes, G.S.; Stapait, E.L.; Kirsten, M.H.; de Noronha, M.; Santos, G.M. Clinical test for diagnosis of patellofemoral pain syndrome: Systematic review with meta-analysis. Phys Ther Sport, 2013, 14, 54–59. [Google Scholar] [CrossRef] [PubMed]
- Gulati, A.; McElrath, C.; Wadhwa, V.; Shah, J.P.; Chhabra, A. Current clinical, radiological and treatment perspectives of patellofemoral pain syndrome. Br J Radiol, 2018, 91, 20170456. [Google Scholar] [CrossRef]
- Hall, R.; Barber, Foss, K.; Hewett, T.E.; Myer, G.D. Sport specialization's association with an increased risk of developing anterior knee pain in adolescent female athletes. J Sport Rehabil, 2015, 24, 31–35. [Google Scholar] [CrossRef]
- Lankhorst, N.E.; Bierma-Zeinstra, S.M.; van Middelkoop, M. Risk factors for patellofemoral pain syndrome: a systematic review. J Orthop Sports Phys Ther, 2012, 42, 81–94. [Google Scholar] [CrossRef]
- Cavazzuti, L.; Merlo, A.; Orlandi, F.; Campanini, I. ; Delayed onset of electromyographic activity of vastus medialis obliquus relative to vastus lateralis in subjects with patellofemoral pain syndrome. Gait & posture, 2010, 32, 290–295. [Google Scholar]
- Chen, H.-Y.; Chien, C.-C.; Wu, S.-K.; Liau, J.-J.; Jan, M.-H. Electromechanical delay of the vastus medialis obliquus and vastus lateralis in individuals with patellofemoral pain syndrome. Journal of Orthopaedic & sports physical therapy, 2012, 42, 791–796. [Google Scholar]
- Schmitz, R.J.; Shultz, S.J.; Nguyen, A.D. Dynamic valgus alignment and functional strength in males and females during maturation. Journal of athletic training, 2009, 44, 26–32. [Google Scholar] [CrossRef]
- Myer, G.D.; Ford, K.R.; Barber Foss, K.D.; Goodman, A.; Ceasar, A.; Rauh, M.J.; Divine, J.G.; Hewett, T.E. The incidence and potential pathomechanics of patellofemoral pain in female athletes. Clin Biomech (Bristol, Avon), 2010, 25, 700–707. [Google Scholar] [CrossRef] [PubMed]
- Petersen, W.; Rembitzki, I.; Liebau, C. Patellofemoral pain in athletes. Open access journal of sports medicine 2017, 143–154. [Google Scholar] [CrossRef] [PubMed]
- Barton, C.J.; Lack, S.; Hemmings, S.; Tufail, S.; Morrissey, D. The 'Best Practice Guide to Conservative Management of Patellofemoral Pain': incorporating level 1 evidence with expert clinical reasoning. Br J Sports Med. 2015, 49, 923–934. [Google Scholar] [CrossRef] [PubMed]
- Bump, J.M. Patellofemoral Syndrome. In StatPearls; Lewis, L, Ed.; StatPearls Publishing LLC: Treasure Island, FL, USA, 2022. [Google Scholar]
- Boling, M.C.; Bolgla, L.A.; Mattacola, C.G.; Uhl, T.L.; Hosey, R.G. Outcomes of a weight-bearing rehabilitation program for patients diagnosed with patellofemoral pain syndrome. Arch Phys Med Rehabil, 2006, 87, 1428–1435. [Google Scholar] [CrossRef] [PubMed]
- Matthews, M.; Rathleff, M.S.; Claus, A.; McPoil, T.; Nee, R.; Crossley, K.; Vicenzino, B. Can we predict the outcome for people with patellofemoral pain? A systematic review on prognostic factors and treatment effect modifiers. Br J Sports Med, 2017, 51, 1650–1660. [Google Scholar] [CrossRef]
- Zago, J.; Amatuzzi, F.; Rondinel, T.; Matheus, J.P. ; Osteopathic Manipulative Treatment Versus Exercise Program in Runners With Patellofemoral Pain Syndrome: A Randomized Controlled Trial. J Sport Rehabil, 2020, 30, 609–618. [Google Scholar] [CrossRef]
- Meira EP, Brumitt J. Influence of the hip on patients with patellofemoral pain syndrome: a systematic review. Sports Health, 2011, 3, 455–465. [Google Scholar] [CrossRef]
- Powers CM: Patellar kinematics, part I: the influence of vastus muscle activity in subjects with and without patellofemoral pain. Physical therapy, 2000, 80, 956–964. [CrossRef]
- Adel J, Koura G, Hamada HA, El Borady AA, El-Habashy H, Balbaa AE, Saab IM: Squatting versus squatting with hip adduction in management of patellofemoral osteoarthritis: A randomized controlled trial. J Back Musculoskelet Rehabil, 2019, 32, 463–470. [CrossRef]
- Kalytczak MM, Lucareli PRG, Dos Reis AC, Bley AS, Biasotto-Gonzalez DA, Correa JCF, Politti F: Female PFP patients present alterations in eccentric muscle activity but not the temporal order of activation of the vastus lateralis muscle during the single leg triple hop test. Gait Posture, 2018, 62, 445–450.
- Ismail MM, Gamaleldein MH, Hassa KA: Closed kinetic chain exercises with or without additional hip strengthening exercises in management of patellofemoral pain syndrome: a randomized controlled trial. Eur J Phys Rehabil Med, 2013, 49, 687–698.
- Emamvirdi, M.; Letafatkar, A.; Khaleghi, Tazji, M. The Effect of Valgus Control Instruction Exercises on Pain, Strength, and Functionality in Active Females With Patellofemoral Pain Syndrome. Sports Health, 2019, 11, 223–237. [Google Scholar] [CrossRef] [PubMed]
- Kumar, M.; Srivastava, S. Electromyographic analysis of VMO and VL across straight leg raise, short arc quad, medial tibial rotation and hip adduction in normal individuals. Work, 2020, 65, 153–159. [Google Scholar] [CrossRef] [PubMed]
- Hott, A.; Brox, J.I.; Pripp, A.H.; Juel, N.G.; Paulsen, G.; Liavaag, S. Effectiveness of Isolated Hip Exercise, Knee Exercise, or Free Physical Activity for Patellofemoral Pain: A Randomized Controlled Trial. Am J Sports Med, 2019, 47, 1312–1322. [Google Scholar] [CrossRef] [PubMed]
- Plastaras, C.; McCormick, Z.; Nguyen, C.; Rho, M.; Nack, S.H.; Roth, D.; Casey, E.; Carneiro, K.; Cucchiara, A.; Press, J.; et al. Is Hip Abduction Strength Asymmetry Present in Female Runners in the Early Stages of Patellofemoral Pain Syndrome? Am J Sports Med, 2016, 44, 105–112. [Google Scholar] [CrossRef]
- Chen, S.; Chang, W.D.; Wu, J.Y.; Fong, Y.C. Electromyographic analysis of hip and knee muscles during specific exercise movements in females with patellofemoral pain syndrome: An observational study. Medicine (Baltimore), 2018, 97, e11424. [Google Scholar] [CrossRef]
- Chang, W.D.; Huang, W.S.; Lai, P.T. Muscle Activation of Vastus Medialis Oblique and Vastus Lateralis in Sling-Based Exercises in Patients with Patellofemoral Pain Syndrome: A Cross-Over Study. Evid Based Complement Alternat Med, 2015, 2015, 740315. [Google Scholar] [CrossRef]
- Rainoldi, A.; Melchiorri, G.; Caruso, I. A method for positioning electrodes during surface EMG recordings in lower limb muscles. J Neurosci Methods, 2004, 134, 37–43. [Google Scholar] [CrossRef]
- Sawada, T.; Kito, N.; Yukimune, M.; Tokuda, K.; Tanimoto, K.; Anan, M.; Takahashi, M.; Shinkoda, K. Biomechanical effects of lateral and medial wedge insoles on unilateral weight bearing. J Phys Ther Sci, 2016, 28, 280–285. [Google Scholar] [CrossRef]
- Hall, M.; Diamond, L.E.; Lenton, G.K.; Pizzolato, C.; Saxby, D.J. Immediate effects of valgus knee bracing on tibiofemoral contact forces and knee muscle forces. Gait Posture, 2019, 68, 55–62. [Google Scholar] [CrossRef]
- Kagaya, Y.; Fujii, Y.; Nishizono, H. Association between hip abductor function, rear-foot dynamic alignment, and dynamic knee valgus during single-leg squats and drop landings. Journal of Sport and Health Science, 2015, 4, 182–187. [Google Scholar] [CrossRef]
- Thijs, Y.; Van.; Tiggelen, D.; Willems, T.; De, Clercq, D.; Witvrouw, E. Relationship between hip strength and frontal plane posture of the knee during a forward lunge. Br J Sports Med, 2007, 41, 723–727. [CrossRef] [PubMed]
- Miao, P.; Xu, Y.; Pan, C.; Liu, H.; Wang, C. Vastus medialis oblique and vastus lateralis activity during a double-leg semisquat with or without hip adduction in patients with patellofemoral pain syndrome. BMC Musculoskelet Disord, 2015, 16, 28. [Google Scholar] [CrossRef] [PubMed]
- Kiel, J. Adductor Strain. In StatPearls, Kaiser, K.; StatPearls Publishing LLC: Treasure Island, FL, USA, 2023. [Google Scholar]
- Rajput, H.B.; Rajani, S.J.; Vaniya, V.H. Variation in Morphometry of Vastus Medialis Muscle. J Clin Diagn Res, 2017, 11, Ac01-ac04. [Google Scholar] [CrossRef] [PubMed]
- Constantinou, A.; Mamais, I.; Papathanasiou, G.; Lamnisos, D.; Stasinopoulos, D. Comparing hip and knee focused exercises versus hip and knee focused exercises with the use of blood flow restriction training in adults with patellofemoral pain. European Journal of physical and rehabilitation Medicine, 2022, 58, 225. [Google Scholar] [CrossRef]
- Santos, T.R.; Oliveira, B.A.; Ocarino, J.M.; Holt, K.G.; Fonseca, S.T. Effectiveness of hip muscle strengthening in patellofemoral pain syndrome patients: a systematic review. Braz J Phys Ther, 2015, 19, 167–176. [Google Scholar] [CrossRef]
- Escamilla, R.F.; Zheng, N.; Macleod, T.D.; Edwards, W.B.; Imamura, R.; Hreljac, A.; Fleisig, G.S.; Wilk, K.E.; Moorman, C.T., 3rd; Andrews, J.R. Patellofemoral joint force and stress during the wall squat and one-leg squat. Med Sci Sports Exerc, 2009, 41, 879–888. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).