1. Introduction
The aortic heart valve (HV) is a complex structure in a challenging dynamic anatomical and mechanical environment. The blood flow exerts diverse stresses on the valve tissue during each cardiac cycle, which can trigger biological responses such as gene expression, protein activation, and cell phenotype. This plethora of forces may also impact valve remodeling or pathological changes. Understanding the complex mechanobiology of the aortic HV involving stress-strain distribution within the leaflet thickness, remodeling cascades during the cardiac cycle and complex biomechanics pathways of stimulus transmission from the organ to cellular microcosm remains a challenging endeavor (1, 2). Understanding the geometric and biomechanical adaptation of different bioprostheses after implantation is of great clinical interest and needs to be addressed. Severe aortic valve stenosis is still the most common heart valve disease (HD) in the world (3-5). For decades, con-ventional surgical AVR has been the gold standard of care (6-8). Conventional AVR in patients without serious comorbidities is widely considered to be a safe procedure with a low risk of mortality (9, 10). However, as patients' age and comorbidities continue to rise, conventional AVR procedures increasingly associated with complications, particularly when combined with other procedures such as CABG (11-14). The correlation between prolonged aortic cross-clamp and CPB times and increased mortality has been shown (15, 16). Consequently, rapid deployment sutureless (RDS) AVR is gaining ground due to its established simplified implantation technique, proven safety and reduced bypass and cross-clamp time. due to its established simplified implantation technique, proven safety, and reduced bypass and cross-clamp time (17-20). Compared to conventional valves, the Intuity delivers comparable initial clinical outcomes, with significantly better hemodynamics and clinical benefits on long-term morbidity and mortality(16, 21, 22).
The Intuity sutureless aortic valve (Edwards Lifesciences Inc., Irvine, CA, USA) is one of the two commercially available and mostly used RDS bioprostheses and is implanted using the Edwards Intuity rapid-deployment application system.
AVR with the Intuity valve is similar to conventional surgical AVR, which requires open-heart surgery with cardiopulmonary bypass to remove the calcified valve and decalcify the annulus. Unlike conventional AVR, the anchoring of the implanted Intuity valve in the annulus is not dependent on circumferential annular sutures. The Intuity design is based on the Magna Ease valve (Edwards Lifesciences), but with the addition of a balloon-expandable stainless steel stent frame covered by a polyester fabric that is attached to the inflow. Balloon inflation causes the stent frame to expand and seal against the adjacent subvalvular left ventricular outflow tract and ventriculoarterial junction (23). The tapered, fabric-covered expanded stent anchors and seals a properly placed valve in such an ideal position that the suture ring is located directly over the attachment of the native aortic leaflets to the aortic annulus over almost 90% of its circumference (23). The pericommissural region is the only area that extends beyond the level of the suture ring and accounts for the remaining 10% of the circumference. Three additional guide sutures placed at the nadir of each sinus help to orient the suture ring and valve prosthesis (23). The prosthesis is carefully guided into the correct position, after which the metal skirt is dilated in the left ventricular outflow tract (LVOT) (24-26). RD SuAVR is an attractive alternative in combined procedures, and in fragile aortas especially in elderly patients with multiple comorbidities. Multiple studies have validated and confirmed the safety and hemodynamic efficacy of the Intuity valve (27). Numerous technical aspects have to be considered such as a careful leaflet excision and decalcification with preservation of the aortic annulus being of paramount importance. Avoiding oversizing or undersizing is crucial, particularly when dealing with bicuspid or unicuspid valves, where extra caution is warranted. Precise placement prior to inflating the balloon is essential, especially in instances involving preexisting Right Bundle Branch Block (RBBB). In addition, when conducting mitral valve surgery, it is crucial to exercise care due to the fact that the sub-annular aortic region is frequently the focus of prosthetic mitral implants and suture material. This can impact the sub-annular landing region for the Intuity valve, resulting in a disrupted anatomy that could complicate the implantation process (23).
The Intuity valve offers several advantages over conventional alternatives, but associated with a greater frequency of new conductive system abnormalities (25). This applies to recently inserted pacemakers and the occurrence of new left bundle branch block (LBBB). When a right bundle branch block (RBBB) preexists, the emergence of an additional LBBB will require the insertion of a pacemaker. Therefore, the Intuity valve should be avoided in such cases. Several publications have shown that the hemodynamic characteristics of the Intuity valve exceed those of conventional aortic valve prostheses (18, 22). Our objective was to conduct a thorough analysis of the morphological and functional adaptation of the Intuity Prosthesis through a comprehensive evaluation that included in vitro testing and in vivo 3D analysis following AVR.
2. Materials and Methods
2.1. Data Source
Retrospectively, patient data, clinical information prior, during, and after surgery were gathered and examined through our institution's database. Our research was granted approval by the local ethics committee (Ethics Commission RWTH Aachen) with an Institutional Review Board (IRB) authorization: EK 151/09 version 1.2.3, dated March 2016. As a result of the retrospective nature of the research, informed consent was not required. Patient data included medical history, postoperative echocardiographic examinations, cardiac CT scans, intraoperative data, as well as the 30-day postoperative outcomes.
2.2. Study Cohort
This is a single-center, retrospective observational study. Data of patients who received a SuAVR in our Department of cardiothoracic surgery at RWTH Aachen University Hospital between January 2018 and December 2020were retrieved from the institutional database and then screened. The CT scans of patients who received sutureless surgical aortic valve replacement (SuAVR), clinical, operative, echocardiographic, and radiographic data of patients who underwent isolated or combined SAVR with the Intuity bio-prosthesis were included. Inclusion parameters were elective cases of isolated or combined SuAVR with the Intuity bio-prosthesis. exclusion criteria included cases that were of emergent or urgent nature, presence of bicuspid aortic valve, anatomical contraindications to suAVR such as dilated aortic root, endocarditis, hypertrophic cardiomyopathy with LV outflow tract obstruction, redo cases, poor quality of the outflow tract, poor echocardiographic images or incomplete data. All patients received a standardized evaluation and management, prior, during and after surgery by the same team of highly experienced experts.
2.3. Operative Technique
All patients underwent a standardized surgical procedure performed by the consistent team of cardiac surgeons. CPB was established by central aorto-caval cannulation. The best site for cross-clamp and aortotomy for the given surgical access was chosen based on the anatomy and the pathological changes of the ventriculoarterial junction, aortic root, and ascending aorta. Antegrade cardioplegia Bretschneider was administered. The aortotomy was carefully performed to ensure precise placement of the Intuity valve directly above the aortic annulus. These included variations such as a lazy-S, lazy-U, hockey-stick, strict longitudinal, and transverse types of aortotomy. In this cohort, no cases appeared with the diameter of the sinotubular junction (STJ) smaller or equal to the aortic annulus, so that no opening of the aortic root for implantation was required. No high transverse incisions were required. Focal exophytic calcifications projecting into the lumen of the aortic root were delicately excised, and any damage to the aortic wall was meticulously repaired with sutures, resulting in a seamless aortic wall surface. This ensured the smooth insertion of the prosthesis into the ideal position without dislodging any remaining calcific particles.
2.4. The Intuity Edwards Bio-Prosthesis
The Intuity aortic valve is built upon the Perimount valve technology, with the addition of a stainless steel frame at the inflow section that is covered by a textured sealing cloth. The leaflets consist of bovine pericardium. After positioning the prosthesis in the correct position, the stent is expanded with a balloon in the LVOT, which helps to seal the prosthesis and secures the prosthesis in the correct position. The prosthesis is available in the sizes 19, 21, 23, 25 and 27 mm (25, 26).
2.5. Computed Tomography Analysis
A meticulous technical assessment was conducted for each instance to evaluate the positioning, orientation, and integration of the valve with the adjacent anatomy utilizing advanced cardiovascular 3D reconstruction software (OSIRIX DICOM Viewer © 2024 (Pixmeo SARL, Switzerland)). Two postoperative computed tomography scans were utilized for visualization and analysis. This evaluation was conducted to assess whether the Intuity valve is prone to deformation in its natural placement. In order to gain a deeper comprehension of the mechanical characteristics of the Intuity valve, the radial forces of the valve were assessed in an in vitro setting as well. This also enables a more intricate comparison to the evaluation of its biomechanics.
3D analysis of the CT images after Intuity Implantation were conducted using the software OSIRIX DICOM Viewer © 2024 (Pixmeo SARL, Switzerland).
Figures S3-S6, and Videos S1-S3.
Ovality measurements were performed at the annulus level and the distal end of the skirt. Stent ovality
O was used as a metric for stent deformation. The percentage ovality
O can be calculated mathematically using the length of the major axis
and the length of the orthogonal minor axis
of an ellipse according to the following formula:
2.6. In Vitro Radial Force Assessment
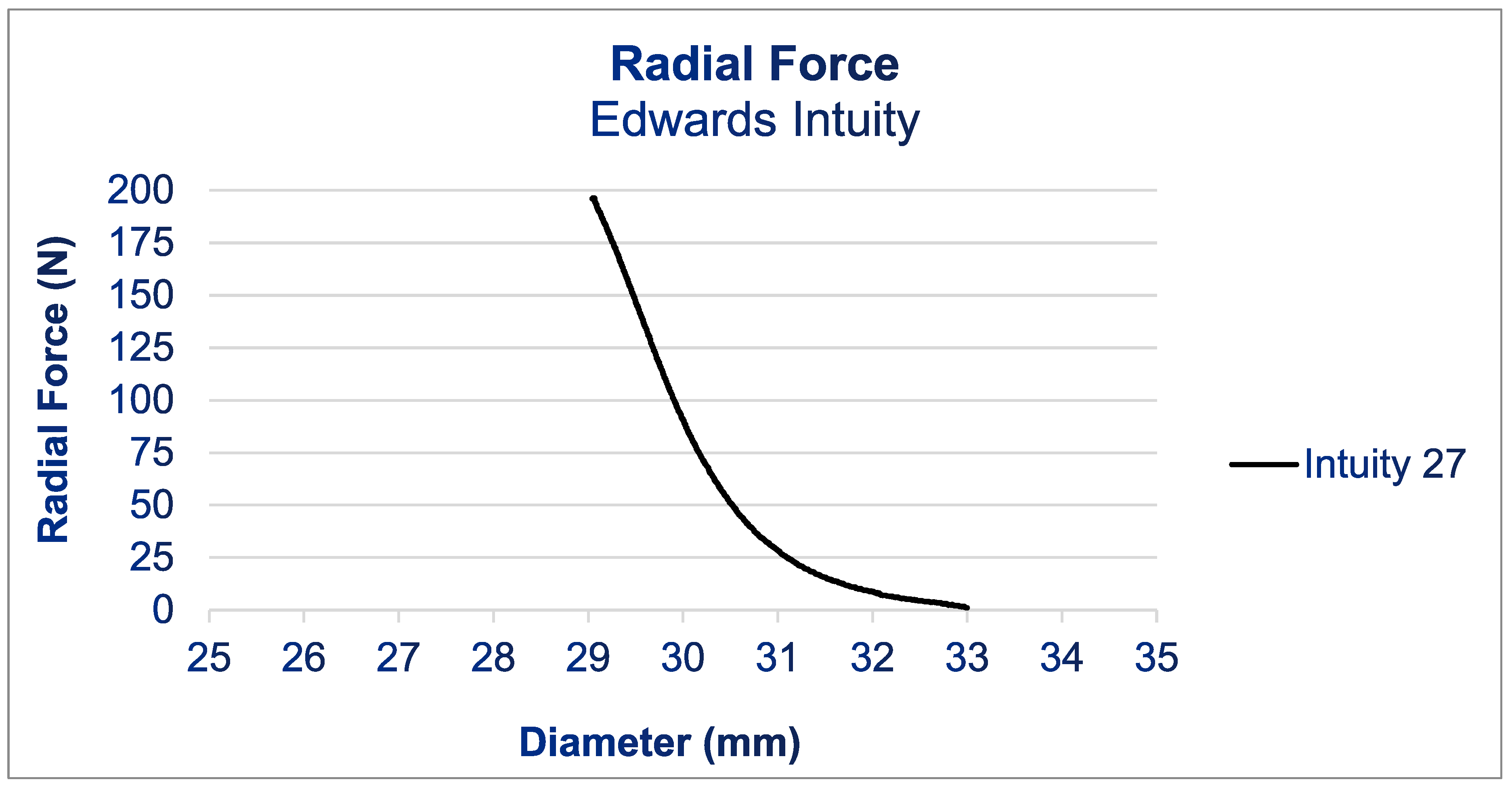
Radial force (RF) is a parameter utilized to gauge the resistance of a stent structure to external radial deformation, as this most accurately replicates the in situ conditions (18). Measuring of the RF is a common practice in the design of heart valves, and analyzing this data can provide valuable insights into the performance and behavior of a valve prosthesis in vivo (28). RF measurements were conducted using the commercial RF tester RX650 from Machine Solutions in Flagstaff, Arizona, USA, which is also utilized in regulatory assessments in accordance with ISO 5840-3, see
Figure 1. A crimping mechanism consisting of 12 triangular crimping jaws opens and closes around the stent to crimp it down and let it expand, respectively. Intuity prosthesis with a diameter 27mm were introduced into the tester. The tester was programmed to crimp down and compress gradually from 35 mm to 25 mm while consistently measuring the exerted RF. The manufacturer has specified the measurement accuracy of the tester as 0.06%.
2.7. Transthoracic and Trans-Esophageal Echocardiography Assessments
Echocardiographic assessment included at least one preoperative TTE the day before surgery, an intraoperative TEE prior to CPB establishment and after CPB weaning, as well as a postoperative TTE control during the early postoperative period and the day of admission. All TTE evaluations were conducted in adherence with the guidelines set forth by both the European Society of Cardiovascular Imaging and the American Society of Echocardiography (29-31). Echocardiographic assessments were conducted with the aid of the Vivid E9 device (GE Vingmed Ultrasound AS, Horten, Norway).
2.8. Statistical Analysis
The statistical analysis was conducted utilizing the software Minitab (version 19). The assessment involved utilizing both Graphical Summary and individual variables table tools. The Graphical Summary tool was utilized to provide a summary of numerical data, incorporating various statistics such as sample size, mean, standard deviation, confidence interval, minimum and maximum values. Meanwhile, the Individual Variable Table tool was employed to summarize categorical data with counts and percentages. It is important to note that certain variables contained missing values (N*) due to missing information within the dataset; these missing values were not included by Minitab during statistical calculation processes.
3. Results
3.1. Clinical Findings
Between March 2018 and June 2020, a total of 19 patients (57% females) with a mean age of 76.2 years received an AVR using the Intuity bio-prosthesis (
Table 1). Thirteen patients (n=13, 68.4%) underwent simultaneous surgery in addition to the aortic valve replacement (AVR). The postoperative mortality rate was 10.5 %, none death was cardiac related. The postoperative rate of permanent pacemaker implantation was 5.5%.
Echocardiographic findings are presented in
Table 3.
3.2. Computed Tomography Analysis
Stent ovality at the annulus level was 0 and 10.4%, respectively. Stent ovality at the distant edge of the skirt was 2 and 19.9%, respectively.
3.3. Radial Force RF Measurements
Figure 1 shows the results of the RF measurements. For the Intuity prosthesis, the radial force increased gradually starting at a diameter of 33 mm during compression. Below a diameter of 31 mm, the RF increased quickly until it reached 200 N at 29 mm. The test had to be halted upon reaching 200 N, as this exceeded the load cell's maximum capacity in the radial force tester and risked damaging the equipment.
4. Discussion
RD prostheses are often considered a safe alternative to traditional aortic valve replacement, albeit at a considerably higher cost compared to the standard option. The main noticeable benefit over conventional procedures is the decrease in both bypass and aortic clamp time in the majority of cases. SuAVR demonstrated lower pressure gradients compared to traditional AVR in individuals receiving prosthetic valves of equivalent dimensions (32).
Reports of 12,000 patients and comparing the Intuity RDAVR to TAVR procedures, or conventional AVR with other sutured and sutureless bioprostheses, have shown that the Intuity Su-AVR exhibits a 30-day mortality of only 3.8%, with no reported incidence of paravalvular leak or myocardial infarction. Furthermore, an Intuity-related PPM rate of 11.11 % and a stroke frequency of 2.2% are reported (33). Compared to other sutured bioprostheses, the mortality rate with the Intuity valve ranged from 0% to 3.9%, while for conventional it ranged from 0% to 6.9%. The short-term mortality rate for Intuity ranged from 0.9% to 12.4%. This is comparable to our outcomes. The long-term cardiovascular mortality rate for the Intuity valve varied from 0.9% to 1.55%.
The human aortic annulus is not absolutely circle-shaped(34). It is also described that the ellipticity of the aortic annulus can influence the results of some prosthesis implantation while not affecting other alternatives(35). Sutured, stented valves enforce the human annular plane into its desired circular shape, providing proper long-term performance of the cusps. However, there are only few studies regarding the prosthesis-annular plane adaptation in case of sutureless valves. In our previous study we analyzed the biomechanics of the Perceval prosthesis. In this single-center study our objectives were to provide insights into the technical attributes of the widely used Intuity prosthesis. The RF results obtained from our in vitro testing indicate that the Intuity valve exhibits a high degree of rigidity, suggesting a reduced susceptibility to deformation. This is also confirmed by the low degrees of ovality found at the annulus level in the analyzed CT images. The RF of the Intuity valve at 29 mm, which is 2 mm above the upper end of its intended implantation range, (200 N). Within its implantation range, the Intuity valve is potentially even more rigid, but the RF tester maxed out at 200 N and did not allow for additional measurements. 200 N of radial force, however, corresponds to putting a load of 20 kg on the stent frame, which should be sufficient for its intended purpose. The Intuity bioprosthesis seems sufficiently rigid to sustain a round contour in vivo. This could explain the satisfying results, good hemodynamic performance, and low rate of patient-prosthesis mismatch even in patients with a small aortic root (36).
An explanation of our findings may be attributed to the expandable stainless double-crimped frame steel cloth-covered skirt's role in facilitating a larger orifice area for the prosthesis, that is flexible enough to be implanted and favour gentle surgical approaches. The skirt section showed higher degrees of ovality than the stent section housing the valve. This allows the skirt to adapt well to the native anatomy decreasing the risk of paravalvular leakage. At the same time the skirt is rigid enough to maintain its structure and provide good haemodynamic response to the remodelling of the left ventricular outflow tract due to the infra-annular frame and freedom from Teflon supported sutures, thus reducing turbulent flows in the left ventricular outflow tract.
Limitations of the Study
To the best of our knowledge, this is one of the few studies investigating the biomechanical adaptation of the Intuity valve; however, one potential limitation of our study is the small cohort size. Additionally, the data focuses on short-term measures, gathered mainly directly and up to 30 days after surgery, and does not include long-term follow-up to assess patient outcomes and valve-related data such as structural valve deterioration. It should be noted that individual characteristics and parameters, such as aortic root distensibility and aortic root stiffness, may impact the geometrical orifice area (GOA) and aortic valve kinematics, thereby affecting the mechanical load on the aortic valve cusps. Further investigation is required to determine whether these alterations have a significant impact on the onset of structural valve deterioration and the valve’s longevity (1, 37) as well as to further determine the potential clinical implications of these findings in long-term survival and prognosis.
5. Conclusion
The Intuity bioprosthesis demonstrates remarkable structural rigidity, and thus, the potential capacity to dynamically adjust to the hemodynamic patterns in the aortic root. Its high RFs may explain the resistance to deformation, ensuring harmonious, natural-like cusp mobility. This may reduce the risk of turbulence-induced fibrosis and increased transvalvular pressure gradients, and may clinically translate into less hemolysis. However, the generated radial forces may invite high-grade postoperative conduction system disorders. Additional research with larger sample sizes and longer follow-up periods is needed to confirm our findings and their impact in longterm.
Supplementary Materials
The following supporting information can be downloaded at the website of this paper posted on Preprints.org.
Conflicts of Interest
none declared.
Abbreviations
AF atrial fibrillation
AV atrioventricular
AVR aortic valve replacement
COPD chronic obstructive pulmonary disease
CPB cardiopulmonary bypass
EOA effective orifice area
GOA geometrical orifice area
HVD heart valve disease
HLP hyperlipoproteinaemia
IDDM insulin-dependent diabetes mellitus
ICU intensive care unit
KD kidney disease
LBBB left Bundle Branch Block
MPG mean pressure gradient
PAD peripheral artery disease
PM Pacemaker
PVL para-valvular leak
RBBB Right Bundle Branch Block
RDAVR Rapid Deployment Aortic Valve Replacement
RDS rapid deployment sutureless
RD-SAVR Rapid deployment sutureless aortic valve replacement
RF radial force
SuAVR sutureless aortic valve replacement
SD standard deviation
TTE transthoracic echocardiography
PPG peak preassure gradient
PVL paravalvular leakage
TEE trans-esophageal echocardiography
3D three dimension
References
- Butcher JT, Simmons CA, Warnock JN. Mechanobiology of the aortic heart valve. J Heart Valve Dis 2008, 17, 62–73. [Google Scholar]
- Rossini G, Caimi A, Redaelli A, Votta E. Subject-specific multiscale modeling of aortic valve biomechanics. Biomech Model Mechanobiol 2021, 20, 1031–1046. [Google Scholar] [CrossRef] [PubMed]
- Benjamin EJ, Blaha MJ, Chiuve SE, Cushman M, Das SR, Deo R, et al. Heart Disease and Stroke Statistics-2017 Update: A Report From the American Heart Association. Circulation 2017, 135, e146–e603. [Google Scholar]
- Iung B, Baron G, Butchart EG, Delahaye F, Gohlke-Bärwolf C, Levang OW, et al. A prospective survey of patients with valvular heart disease in Europe: The Euro Heart Survey on Valvular Heart Disease. Eur Heart J 2003, 24, 1231–1243. [Google Scholar] [CrossRef] [PubMed]
- Funkat A, Beckmann A, Lewandowski J, Frie M, Ernst M, Schiller W, et al. Cardiac surgery in Germany during 2013: a report on behalf of the German Society for Thoracic and Cardiovascular Surgery. Thorac Cardiovasc Surg 2014, 62, 380–392. [Google Scholar] [CrossRef] [PubMed]
- Schwarz F, Baumann P, Manthey J, Hoffmann M, Schuler G, Mehmel HC, et al. The effect of aortic valve replacement on survival. Circulation 1982, 66, 1105–1110. [Google Scholar] [CrossRef]
- Murphy ES, Lawson RM, Starr A, Rahimtoola SH. Severe aortic stenosis in patients 60 years of age or older: left ventricular function and 10-year survival after valve replacement. Circulation 1981, 64 Pt 2, Ii184–8. [Google Scholar]
- Lund, O. Preoperative risk evaluation and stratification of long-term survival after valve replacement for aortic stenosis. Reasons for earlier operative intervention. Circulation 1990, 82, 124–139. [Google Scholar]
- Shahian DM, O'Brien SM, Filardo G, Ferraris VA, Haan CK, Rich JB, et al. The Society of Thoracic Surgeons 2008 cardiac surgery risk models: part 3--valve plus coronary artery bypass grafting surgery. Ann Thorac Surg, S: Suppl).
- O'Brien SM, Shahian DM, Filardo G, Ferraris VA, Haan CK, Rich JB, et al. The Society of Thoracic Surgeons 2008 cardiac surgery risk models: part 2--isolated valve surgery. Ann Thorac Surg 2009, 88, S23–42. [Google Scholar] [CrossRef]
- Bouma BJ, van der Meulen JH, van den Brink RB, Smidts A, Cheriex EC, Hamer HP, et al. Validity of conjoint analysis to study clinical decision making in elderly patients with aortic stenosis. J Clin Epidemiol 2004, 57, 815–823. [Google Scholar] [CrossRef]
- Iung B, Cachier A, Baron G, Messika-Zeitoun D, Delahaye F, Tornos P, et al. Decision-making in elderly patients with severe aortic stenosis: why are so many denied surgery? Eur Heart J 2005, 26, 2714–2720.
- Dewey TM, Brown D, Ryan WH, Herbert MA, Prince SL, Mack MJ. Reliability of risk algorithms in predicting early and late operative outcomes in high-risk patients undergoing aortic valve replacement. J Thorac Cardiovasc Surg 2008, 135, 180–187. [Google Scholar] [CrossRef] [PubMed]
- Di Eusanio M, Fortuna D, De Palma R, Dell'Amore A, Lamarra M, Contini GA, et al. Aortic valve replacement: results and predictors of mortality from a contemporary series of 2256 patients. J Thorac Cardiovasc Surg 2011, 141, 940–947. [Google Scholar] [CrossRef] [PubMed]
- Doenst T, Borger MA, Weisel RD, Yau TM, Maganti M, Rao V. Relation between aortic cross-clamp time and mortality--not as straightforward as expected. Eur J Cardiothorac Surg 2008, 33, 660–665. [Google Scholar] [CrossRef]
- Al-Sarraf N, Thalib L, Hughes A, Houlihan M, Tolan M, Young V, et al. Cross-clamp time is an independent predictor of mortality and morbidity in low- and high-risk cardiac patients. Int J Surg 2011, 9, 104–109. [Google Scholar] [CrossRef]
- Schlömicher M, Haldenwang PL, Moustafine V, Bechtel M, Strauch JT. Minimal access rapid deployment aortic valve replacement: initial single-center experience and 12-month outcomes. J Thorac Cardiovasc Surg 2015, 149, 434–440. [Google Scholar] [CrossRef]
- Ferrari E, Roduit C, Salamin P, Caporali E, Demertzis S, Tozzi P, et al. Rapid-deployment aortic valve replacement versus standard bioprosthesis implantation. J Card Surg 2017, 32, 322–327. [Google Scholar] [CrossRef]
- Liakopoulos OJ, Gerfer S, Weider S, Rahmanian P, Zeriouh M, Eghbalzadeh K, et al. Direct Comparison of the Edwards Intuity Elite and Sorin Perceval S Rapid Deployment Aortic Valves. Ann Thorac Surg 2018, 105, 108–114. [Google Scholar] [CrossRef]
- Sohn SH, Jang MJ, Hwang HY, Kim KH. Rapid deployment or sutureless versus conventional bioprosthetic aortic valve replacement: A meta-analysis. J Thorac Cardiovasc Surg 2018, 155, 2402–2412. [Google Scholar] [CrossRef]
- Folliguet TA, Laborde F, Zannis K, Ghorayeb G, Haverich A, Shrestha M. Sutureless perceval aortic valve replacement: results of two European centers. Ann Thorac Surg 2012, 93, 1483–1488. [Google Scholar] [CrossRef]
- D'Onofrio A, Cibin G, Lorenzoni G, Tessari C, Bifulco O, Lombardi V, et al. Propensity-Weighted Comparison of Conventional Stented and Rapid-Deployment Aortic Bioprostheses. Curr Probl Cardiol 2023, 48, 101426. [Google Scholar] [CrossRef] [PubMed]
- Laufer, G. The 10 Commandments of Rapid Deployment Intuity Valve Implantation. Innovations (Phila) 2023, 18, 316–319. [Google Scholar] [CrossRef] [PubMed]
- Sadri V, Bloodworth CHt, Madukauwa-David ID, Midha PA, Raghav V, Yoganathan AP. A mechanistic investigation of the EDWARDS INTUITY Elite valve's hemodynamic performance. Gen Thorac Cardiovasc Surg 2020, 68, 9–17. [Google Scholar] [CrossRef] [PubMed]
- Barnhart GR, Accola KD, Grossi EA, Woo YJ, Mumtaz MA, Sabik JF, et al. TRANSFORM (Multicenter Experience With Rapid Deployment Edwards INTUITY Valve System for Aortic Valve Replacement) US clinical trial: Performance of a rapid deployment aortic valve. J Thorac Cardiovasc Surg 2017, 153, 241–251. [Google Scholar] [CrossRef] [PubMed]
- Accola KD, Chitwood WR, Jr. , Mumtaz MA, Barnhart GR. Step-by-Step Aortic Valve Replacement With a New Rapid Deployment Valve. Ann Thorac Surg 2018, 105, 966–971. [Google Scholar] [CrossRef]
- Young C, Laufer G, Kocher A, Solinas M, Alamanni F, Polvani G, et al. One-year outcomes after rapid-deployment aortic valve replacement. J Thorac Cardiovasc Surg 2018, 155, 575–585. [Google Scholar] [CrossRef]
- Egron S, Fujita B, Gullón L, Pott D, Schmitz-Rode T, Ensminger S, et al. Radial Force: An Underestimated Parameter in Oversizing Transcatheter Aortic Valve Replacement Prostheses: In Vitro Analysis with Five Commercialized Valves. ASAIO Journal 2018, 64, 536–543. [Google Scholar] [CrossRef]
- Baumgartner HC, Hung JC-C, Bermejo J, Chambers JB, Edvardsen T, Goldstein S, et al. Recommendations on the echocardiographic assessment of aortic valve stenosis: a focused update from the European Association of Cardiovascular Imaging and the American Society of Echocardiography. Eur Heart J Cardiovasc Imaging 2017, 18, 254–275. [Google Scholar] [CrossRef]
- Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging 2015, 16, 233–270. [Google Scholar] [CrossRef]
- Zoghbi WA, Chambers JB, Dumesnil JG, Foster E, Gottdiener JS, Grayburn PA, et al. Recommendations for evaluation of prosthetic valves with echocardiography and doppler ultrasound: a report From the American Society of Echocardiography's Guidelines and Standards Committee and the Task Force on Prosthetic Valves, developed in conjunction with the American College of Cardiology Cardiovascular Imaging Committee, Cardiac Imaging Committee of the American Heart Association, the European Association of Echocardiography, a registered branch of the European Society of Cardiology, the Japanese Society of Echocardiography and the Canadian Society of Echocardiography, endorsed by the American College of Cardiology Foundation, American Heart Association, European Association of Echocardiography, a registered branch of the European Society of Cardiology, the Japanese Society of Echocardiography, and Canadian Society of Echocardiography. J Am Soc Echocardiogr 2009, 22, 975–1014. [Google Scholar]
- Taghiyev ZT, Bechtel M, Schlömicher M, Useini D, Taghi HN, Moustafine V, et al. Early-Term Results of Rapid-Deployment Aortic Valve Replacement versus Standard Bioprosthesis Implantation Combined with Coronary Artery Bypass Grafting. Thorac Cardiovasc Surg 2023, 71, 519–527. [Google Scholar] [CrossRef] [PubMed]
- Dokollari A, Torregrossa G, Sicouri S, Veshti A, Margaryan R, Cameli M, et al. Pearls, pitfalls, and surgical indications of the Intuity TM heart valve: A rapid deployment bioprosthesis. A systematic review of the literature. J Card Surg 2022, 37, 5411–5417. [Google Scholar] [CrossRef] [PubMed]
- Ng AC, Delgado V, van der Kley F, Shanks M, van de Veire NR, Bertini M, et al. Comparison of aortic root dimensions and geometries before and after transcatheter aortic valve implantation by 2- and 3-dimensional transesophageal echocardiography and multislice computed tomography. Circ Cardiovasc Imaging 2010, 3, 94–102. [Google Scholar] [CrossRef] [PubMed]
- Tomii D, Okuno T, Lanz J, Stortecky S, Windecker S, Pilgrim T. Aortic annulus ellipticity and outcomes after transcatheter aortic valve implantation. Catheter Cardiovasc Interv 2023, 101, 199–208. [Google Scholar] [CrossRef] [PubMed]
- Arribas-Leal JM, Rivera-Caravaca JM, Aranda-Domene R, Moreno-Moreno JA, Espinosa-Garcia D, Jimenez-Aceituna A, et al. Mid-term outcomes of rapid deployment aortic prostheses in patients with small aortic annulus. Interactive CardioVascular and Thoracic Surgery 2021, 33, 695–701. [Google Scholar] [CrossRef]
- Jahren SE, Winkler BM, Heinisch PP, Wirz J, Carrel T, Obrist D. Aortic root stiffness affects the kinematics of bioprosthetic aortic valves. Interact Cardiovasc Thorac Surg 2017, 24, 173–180. [Google Scholar]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).