Submitted:
20 May 2024
Posted:
21 May 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Patients and Methods
Demographic, Clinical and Laboratory Data
HRCT Assessment and Visual Reader-Based Disease Quantification
Patient-Reported Measures
Pulmonary Function Tests
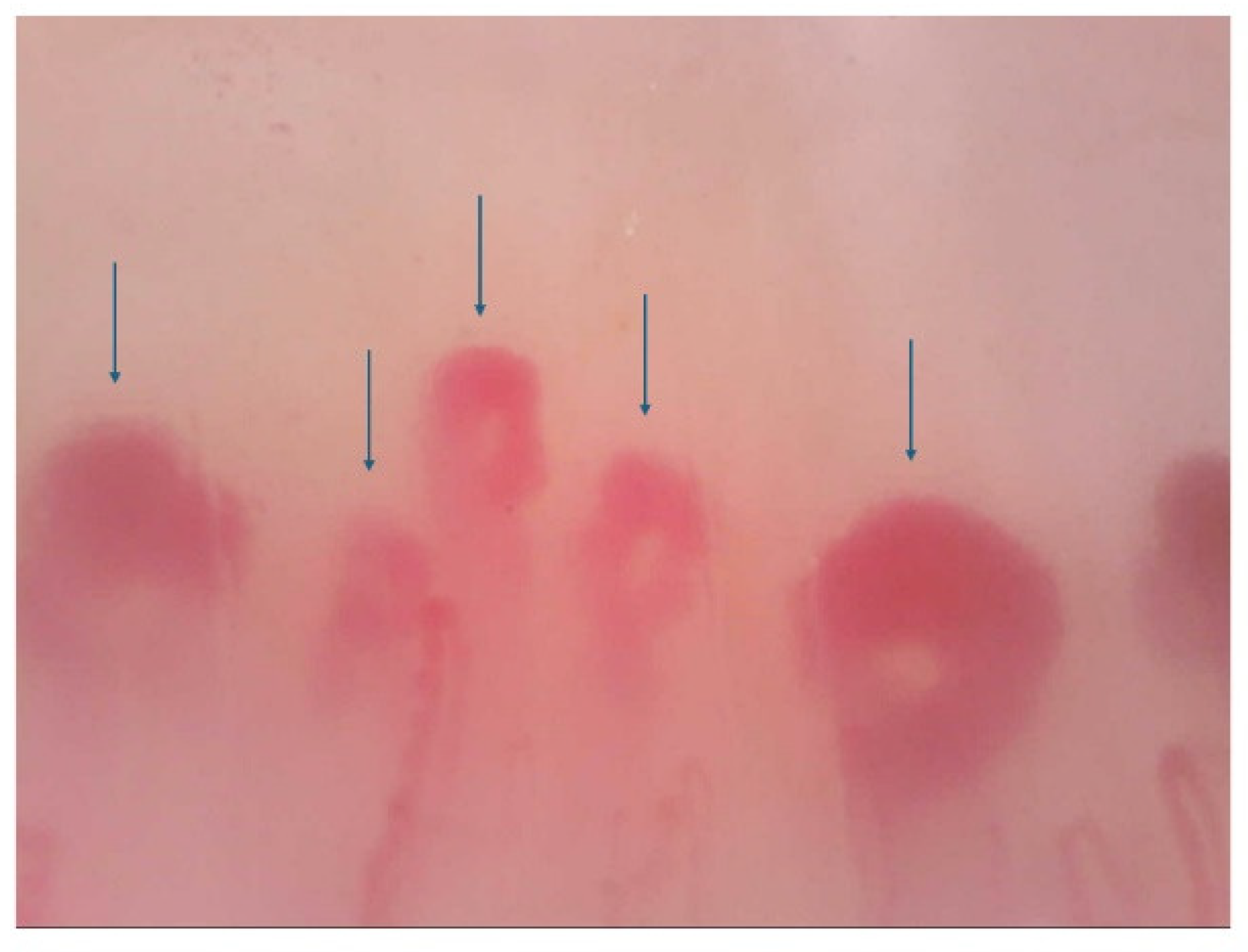
Nailfold Capillaroscopy
Statistical Analysis
3. Results
3.1. Variables Associated with SSc-ILD
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
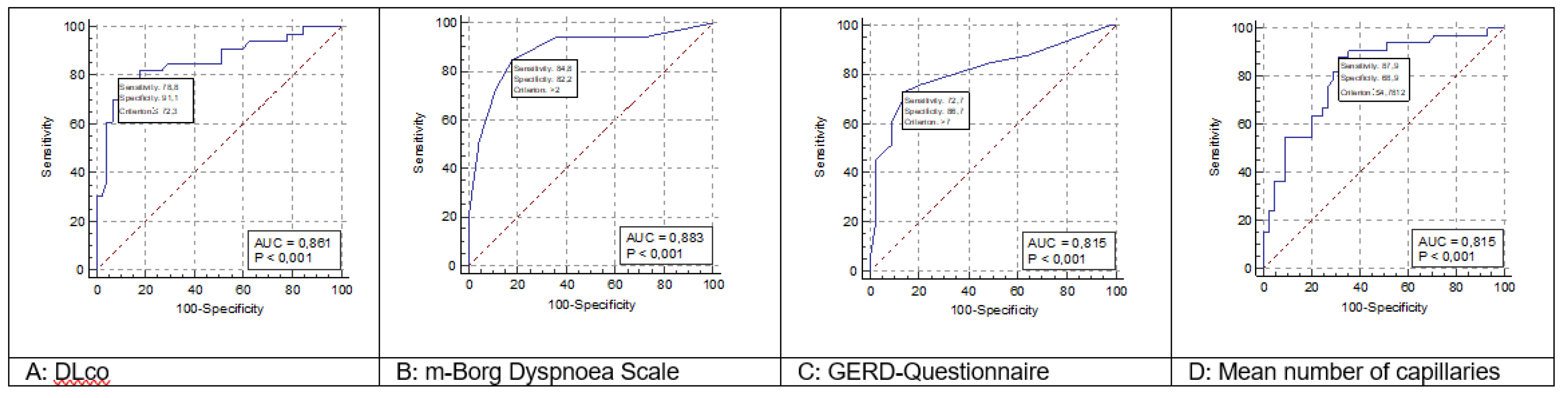
| ROC curve | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Variable | DLco | ||||||||
| Classification variable | CUT-OFF ILD | ||||||||
| Sample size | 78 | ||||||||
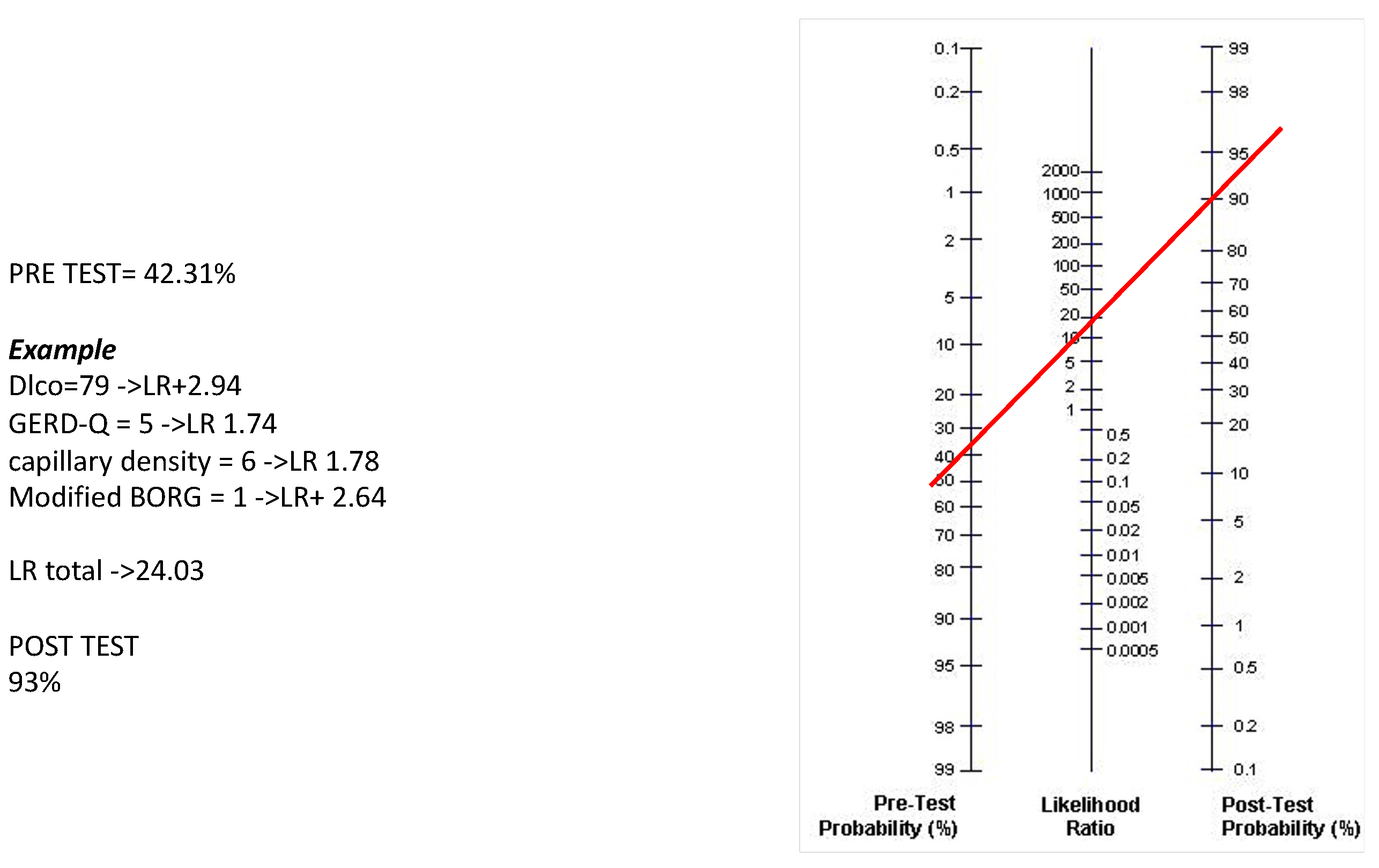
| Positive group a | 33 (42.31%) | ||||||||
| Negative group b | 45 (57.69%) | ||||||||
| Area under the ROC curve (AUC) | |||||||||
| Area under the ROC curve (AUC) | 0.861 | ||||||||
| Standard Error a | 0.0457 | ||||||||
| 95% Confidence interval b | 0.771 to 0.950 | ||||||||
| z statistic | 7.887 | ||||||||
| Significance level P (Area=0.5) | <0.0001 | ||||||||
| Youden index | |||||||||
| Youden index J | 0.6990 | ||||||||
| Associated criterion | ≤72.3 | ||||||||
| Sensitivity | 78.79 | ||||||||
| Specificity | 91.11 | ||||||||
| Criterion values and coordinates of the ROC curve | |||||||||
| Criterion | Sensitivity | 95% CI | Specificity | 95% CI | +LR | 95% CI | -LR | 95% CI | |
| ≤55.2 | 30.30 | 15.6 - 48.7 | 97.78 | 88.2 - 99.9 | 13.64 | 1.8 - 101.4 | 0.71 | 0.6 - 0.9 | |
| ≤56 | 36.36 | 20.4 - 54.9 | 95.56 | 84.9 - 99.5 | 8.18 | 2.0 - 34.1 | 0.67 | 0.5 - 0.9 | |
| ≤60 | 60.61 | 42.1 - 77.1 | 95.56 | 84.9 - 99.5 | 13.64 | 3.4 - 54.3 | 0.41 | 0.3 - 0.6 | |
| ≤61 | 60.61 | 42.1 - 77.1 | 93.33 | 81.7 - 98.6 | 9.09 | 2.9 - 28.1 | 0.42 | 0.3 - 0.6 | |
| ≤66 | 69.70 | 51.3 - 84.4 | 93.33 | 81.7 - 98.6 | 10.45 | 3.4 - 31.9 | 0.32 | 0.2 - 0.5 | |
| ≤67 | 69.70 | 51.3 - 84.4 | 91.11 | 78.8 - 97.5 | 7.84 | 3.0 - 20.5 | 0.33 | 0.2 - 0.6 | |
| ≤72.3 | 78.79 | 61.1 - 91.0 | 91.11 | 78.8 - 97.5 | 8.86 | 3.4 - 23.0 | 0.23 | 0.1 - 0.5 | |
| ≤74 | 78.79 | 61.1 - 91.0 | 82.22 | 67.9 - 92.0 | 4.43 | 2.3 - 8.5 | 0.26 | 0.1 - 0.5 | |
| ≤74.3 | 81.82 | 64.5 - 93.0 | 82.22 | 67.9 - 92.0 | 4.60 | 2.4 - 8.8 | 0.22 | 0.1 - 0.5 | |
| ≤78.5 | 81.82 | 64.5 - 93.0 | 73.33 | 58.1 - 85.4 | 3.07 | 1.8 - 5.1 | 0.25 | 0.1 - 0.5 | |
| ≤79 | 84.85 | 68.1 - 94.9 | 71.11 | 55.7 - 83.6 | 2.94 | 1.8 - 4.7 | 0.21 | 0.09 - 0.5 | |
| ≤82.2 | 84.85 | 68.1 - 94.9 | 48.89 | 33.7 - 64.2 | 1.66 | 1.2 - 2.3 | 0.31 | 0.1 - 0.7 | |
| ≤84.5 | 90.91 | 75.7 - 98.1 | 48.89 | 33.7 - 64.2 | 1.78 | 1.3 - 2.4 | 0.19 | 0.06 - 0.6 | |
| ≤85.4 | 90.91 | 75.7 - 98.1 | 40.00 | 25.7 - 55.7 | 1.52 | 1.2 - 2.0 | 0.23 | 0.07 - 0.7 | |
| ≤88 | 93.94 | 79.8 - 99.3 | 37.78 | 23.8 - 53.5 | 1.51 | 1.2 - 1.9 | 0.16 | 0.04 - 0.6 | |
| ≤90.2 | 93.94 | 79.8 - 99.3 | 22.22 | 11.2 - 37.1 | 1.21 | 1.0 - 1.4 | 0.27 | 0.06 - 1.2 | |
| ≤91 | 96.97 | 84.2 - 99.9 | 22.22 | 11.2 - 37.1 | 1.25 | 1.1 - 1.5 | 0.14 | 0.02 - 1.0 | |
| ≤92.2 | 96.97 | 84.2 - 99.9 | 15.56 | 6.5 - 29.5 | 1.15 | 1.0 - 1.3 | 0.19 | 0.03 - 1.5 | |
| ≤93 | 100.00 | 89.4 - 100.0 | 15.56 | 6.5 - 29.5 | 1.18 | 1.0 - 1.3 | 0.00 | 0.04 - 1.6 | |
| ROC curve | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Variable | Modified Borg Dyspnea Scale | ||||||||
| Classification variable | CUT-OFF ILD | ||||||||
| Sample size | 78 | ||||||||
| Positive group a | 33 (42.31%) | ||||||||
| Negative group b | 45 (57.69%) | ||||||||
| Area under the ROC curve (AUC) | |||||||||
| Area under the ROC curve (AUC) | 0.883 | ||||||||
| Standard Error a | 0.0421 | ||||||||
| 95% Confidence interval b | 0.801 to 0.966 | ||||||||
| z statistic | 9.098 | ||||||||
| Significance level P (Area=0.5) | <0.0001 | ||||||||
| Youden index | |||||||||
| Youden index J | 0.6707 | ||||||||
| Associated criterion | >2 | ||||||||
| Sensitivity | 84.85 | ||||||||
| Specificity | 82.22 | ||||||||
| Criterion values and coordinates of the ROC curve | |||||||||
| Criterion | Sensitivity | 95% CI | Specificity | 95% CI | +LR | 95% CI | -LR | 95% CI | |
| >0.5 | 93.94 | 79.8 - 99.3 | 28.89 | 16.4 - 44.3 | 1.32 | 1.1 - 1.6 | 0.21 | 0.05 - 0.9 | |
| >1 | 93.94 | 79.8 - 99.3 | 64.44 | 48.8 - 78.1 | 2.64 | 1.8 - 4.0 | 0.094 | 0.02 - 0.4 | |
| >2 | 84.85 | 68.1 - 94.9 | 82.22 | 67.9 - 92.0 | 4.77 | 2.5 - 9.1 | 0.18 | 0.08 - 0.4 | |
| >3 | 72.73 | 54.5 - 86.7 | 88.89 | 75.9 - 96.3 | 6.55 | 2.8 - 15.4 | 0.31 | 0.2 - 0.5 | |
| >4 | 51.52 | 33.5 - 69.2 | 95.56 | 84.9 - 99.5 | 11.59 | 2.9 - 46.8 | 0.51 | 0.4 - 0.7 | |
| >5 | 21.21 | 9.0 - 38.9 | 100.00 | 92.1 - 100.0 | 12.29 | 3.1 - 48.9 | 0.52 | 0.7 - 0.9 | |
Appendix B
| ROC curve | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Variable | GERD-Q | ||||||||
| Classification variable | CUT-OFF ILD | ||||||||
| Sample size | 78 | ||||||||
| Positive group a | 33 (42.31%) | ||||||||
| Negative group b | 45 (57.69%) | ||||||||
| Area under the ROC curve (AUC) | |||||||||
| Area under the ROC curve (AUC) | 0.815 | ||||||||
| Standard Error a | 0.0528 | ||||||||
| 95% Confidence interval b | 0.712 to 0.919 | ||||||||
| z statistic | 5.964 | ||||||||
| Significance level P (Area=0.5) | <0.0001 | ||||||||
| Youden index | |||||||||
| Youden index J | 0.5939 | ||||||||
| Associated criterion | >7 | ||||||||
| Sensitivity | 72.73 | ||||||||
| Specificity | 86.67 | ||||||||
| Criterion values and coordinates of the ROC curve | |||||||||
| Criterion | Sensitivity | 95% CI | Specificity | 95% CI | +LR | 95% CI | -LR | 95% CI | |
| >4 | 87.88 | 71.8 - 96.6 | 35.56 | 21.9 - 51.2 | 1.36 | 1.1 - 1.8 | 0.34 | 0.1 - 0.9 | |
| >5 | 84.85 | 68.1 - 94.9 | 51.11 | 35.8 - 66.3 | 1.74 | 1.2 - 2.4 | 0.30 | 0.1 - 0.7 | |
| >6 | 75.76 | 57.7 - 88.9 | 80.00 | 65.4 - 90.4 | 3.79 | 2.0 - 7.0 | 0.30 | 0.2 - 0.6 | |
| >7 | 72.73 | 54.5 - 86.7 | 86.67 | 73.2 - 94.9 | 5.45 | 2.5 - 11.8 | 0.31 | 0.2 - 0.6 | |
| >8 | 69.70 | 51.3 - 84.4 | 86.67 | 73.2 - 94.9 | 5.23 | 2.4 - 11.4 | 0.35 | 0.2 - 0.6 | |
| >9 | 60.61 | 42.1 - 77.1 | 91.11 | 78.8 - 97.5 | 6.82 | 2.6 - 18.1 | 0.43 | 0.3 - 0.7 | |
| >10 | 51.52 | 33.5 - 69.2 | 91.11 | 78.8 - 97.5 | 5.80 | 2.1 - 15.6 | 0.53 | 0.4 - 0.8 | |
| >11 | 45.45 | 28.1 - 63.6 | 97.78 | 88.2 - 99.9 | 20.45 | 2.8 - 147.2 | 0.56 | 0.4 - 0.8 | |
| >14 | 18.18 | 7.0 - 35.5 | 97.78 | 88.2 - 99.9 | 8.18 | 1.0 - 64.8 | 0.84 | 0.7 - 1.0 | |
| ROC curve | |||||||||
| Variable | Mean capillary density (number of capillary/mm2) | ||||||||
| Classification variable | CUT-OFF ILD | ||||||||
| Sample size | 78 | ||||||||
| Positive group a | 33 (42.31%) | ||||||||
| Negative group b | 45 (57.69%) | ||||||||
| Area under the ROC curve (AUC) | |||||||||
| Area under the ROC curve (AUC) | 0.815 | ||||||||
| Standard Error a | 0.0492 | ||||||||
| 95% Confidence interval b | 0.718 to 0.911 | ||||||||
| z statistic | 6.396 | ||||||||
| Significance level P (Area=0.5) | <0.0001 | ||||||||
| Youden index | |||||||||
| Youden index J | 0.5677 | ||||||||
| Associated criterion | ≤4.78125 | ||||||||
| Sensitivity | 87.88 | ||||||||
| Specificity | 68.89 | ||||||||
| Criterion values and coordinates of the ROC curve | |||||||||
| Criterion | Sensitivity | 95% CI | Specificity | 95% CI | +LR | 95% CI | -LR | 95% CI | |
| ≤2.53125 | 15.15 | 5.1 - 31.9 | 97.78 | 88.2 - 99.9 | 6.82 | 0.8 - 55.7 | 0.87 | 0.7 - 1.0 | |
| ≤2.875 | 24.24 | 11.1 - 42.3 | 97.78 | 88.2 - 99.9 | 10.91 | 1.4 - 83.0 | 0.77 | 0.6 - 0.9 | |
| ≤3 | 36.36 | 20.4 - 54.9 | 95.56 | 84.9 - 99.5 | 8.18 | 2.0 - 34.1 | 0.67 | 0.5 - 0.9 | |
| ≤3.375 | 54.55 | 36.4 - 71.9 | 91.11 | 78.8 - 97.5 | 6.14 | 2.3 - 16.4 | 0.50 | 0.3 - 0.7 | |
| ≤3.84375 | 54.55 | 36.4 - 71.9 | 80.00 | 65.4 - 90.4 | 2.73 | 1.4 - 5.3 | 0.57 | 0.4 - 0.8 | |
| ≤4.09375 | 63.64 | 45.1 - 79.6 | 80.00 | 65.4 - 90.4 | 3.18 | 1.7 - 6.0 | 0.45 | 0.3 - 0.7 | |
| ≤4.34375 | 66.67 | 48.2 - 82.0 | 73.33 | 58.1 - 85.4 | 2.50 | 1.5 - 4.3 | 0.45 | 0.3 - 0.8 | |
| ≤4.53125 | 78.79 | 61.1 - 91.0 | 71.11 | 55.7 - 83.6 | 2.73 | 1.7 - 4.5 | 0.30 | 0.2 - 0.6 | |
| ≤4.59375 | 81.82 | 64.5 - 93.0 | 68.89 | 53.4 - 81.8 | 2.63 | 1.7 - 4.2 | 0.26 | 0.1 - 0.6 | |
| ≤4.78125 | 87.88 | 71.8 - 96.6 | 68.89 | 53.4 - 81.8 | 2.82 | 1.8 - 4.4 | 0.18 | 0.07 - 0.5 | |
| ≤4.875 | 87.88 | 71.8 - 96.6 | 64.44 | 48.8 - 78.1 | 2.47 | 1.6 - 3.7 | 0.19 | 0.07 - 0.5 | |
| ≤5.125 | 90.91 | 75.7 - 98.1 | 64.44 | 48.8 - 78.1 | 2.56 | 1.7 - 3.8 | 0.14 | 0.05 - 0.4 | |
| ≤6.0625 | 90.91 | 75.7 - 98.1 | 48.89 | 33.7 - 64.2 | 1.78 | 1.3 - 2.4 | 0.19 | 0.06 - 0.6 | |
| ≤6.09375 | 93.94 | 79.8 - 99.3 | 48.89 | 33.7 - 64.2 | 1.84 | 1.4 - 2.5 | 0.12 | 0.03 - 0.5 | |
| ≤7.875 | 93.94 | 79.8 - 99.3 | 31.11 | 18.2 - 46.6 | 1.36 | 1.1 - 1.7 | 0.19 | 0.05 - 0.8 | |
| ≤8.09375 | 96.97 | 84.2 - 99.9 | 28.89 | 16.4 - 44.3 | 1.36 | 1.1 - 1.7 | 0.10 | 0.01 - 0.8 | |
| ≤8.59375 | 96.97 | 84.2 - 99.9 | 6.67 | 1.4 - 18.3 | 1.04 | 0.9 - 1.1 | 0.45 | 0.05 - 4.2 | |
| ≤8.65625 | 100.00 | 89.4 - 100.0 | 6.67 | 1.4 - 18.3 | 1.07 | 1.0 - 1.2 | 0.00 | 0.06 – 4.5 | |
References
- Allanore, Y.; Simms, M.; Distler, O.; Trojanowska, M.; Pope, J.; Denton, C.P.; Varga, J. Systemic sclerosis. Nat Rev Dis Primers 2015, 1, 15002. [Google Scholar] [CrossRef]
- Truchetet, M.E.; Brembilla, M.C.; Chizzolini, C. Current concepts on the pathogenesis of systemic sclerosis. Clin Rev Allergy Immunol 2023, 64, 262–283. [Google Scholar] [CrossRef]
- Khanna, S.A.; Nance, J.W.; Suliman, S.A. Detection and monitoring of interstitial lung disease in patients with systemic sclerosis. Curr Rheumatol Rep 2022, 24, 166–173. [Google Scholar] [CrossRef]
- Salaffi, F.; Carotti, M.; Tardella, M.; Di Carlo, M.; Fraticelli, P.; Fischetti, C.; Giovagnoni, A.; Gabrieli, A. Computed tomography assessment of evolution of interstitial lung disease in systemic sclerosis: comparison of two scoring systems. Eur J Intern Med 2020, 76, 71–75. [Google Scholar] [CrossRef]
- Denton, C.P.; Wells, A.U.; Coghlan, J.G. Major lung complications of systemic sclerosis. Nat Rev Rheumatol 2018, 14, 511–527. [Google Scholar] [CrossRef] [PubMed]
- Hoffmann-Vold, A.M.; Maher, T.M.; Philpot, E.E.; Ashrafzadeh, A.; Barake, R.; Barsotti, S.; Bruni, C.; Carducci, P.; Carreira, P.E.; Castellvi, I.; et al. The identification and management of interstitial lung disease in systemic sclerosis: evidence- based European consensus statements. Lancet Rheumatol 2020, 2: e71–e83. 10.1016/S2665-9913(19)30144-4.
- Assassi, S.; Tumuluri, S.; Levin, R.W. Interstitial lung disease in patients with systemic sclerosis: what can we learn from the SENCIS trial? Clin Exp Rheumatol 2023, 41, 1713–1719. [Google Scholar] [CrossRef] [PubMed]
- Hoffmann-Vold, A.M.; Allanore, Y.; Alves, M.; Brunborg, C.; Airò, P.; Ananieva, L.P.; Czirjak, L.; Guiducci, S.; Hachulla, E.; Li, M.; et al. Progressive interstitial lung disease in patients with systemic sclerosis-associated interstitial lung disease in the EUSTAR database. Ann Rheum Dis 2021; 80, 219–227. [CrossRef]
- Distler, O.; Assassi, S. , Cottin, V. ; Cutolo, M.; Danoff, S.K.; Denton, C.P.; Distler, J.H.V.; Hoffmann-Vold, A.M.; Johnson, S.R.; et al. Predictors of progression in systemic sclerosis patients with interstitial lung disease. Eur Resp J 2020, 55, 1902026. [Google Scholar] [CrossRef] [PubMed]
- Saketkoo, L.A.; Scholand, M.B.; Lammi, M.R.; Russell, A.M. Patient-reported outcome measures in systemic sclerosis-related interstitial lung disease for clinical practice and clinical trials. J Scleroderma Relat Disord 2020, 5 (2 Suppl): 48-60. [CrossRef]
- Lafyatis, R.; Valenzi, E. Assessment of disease outcome measures in systemic sclerosis. Nature Reviews Rheumatology 2022, 18, 527–541. [Google Scholar] [CrossRef]
- Salaffi, F.; Di Carlo, M.; Carotti, M.; Fraticelli, P.; Gabrielli, A.; Giovagnoni, A. Relationship between interstitial lung diseases and oesophageal dilatation on chest high resolution computed tomography in patients with systemic sclerosis: a cross-sectional study. Radiol Med 2018, 123, 655–663. [Google Scholar] [CrossRef]
- Smith, V.; Vanhaecke, A.; Guerra, M.G.; Melsens, K.; Vandecasteele, E.; Paolino, S.; Cutolo, M. May capillaroscopy be a candidate tool in future algorithms for SSc-ILD: are we looking for the holy gray? A systematic review. Autoimmunity Rev 2020, 19, 102619. [Google Scholar] [CrossRef]
- Umashankar, E.; Abdel-Shaheed, C.; Plit, M.; Girgis, L. Assessing the role of nailfold capillaroscopy in interstitial lung disease classification: a systematic review and meta-analysis. Rheumatology 2022, 30, 61–2221. [Google Scholar] [CrossRef] [PubMed]
- Van den Hoogen, F.; Khanna, D.; Fransen, J.; Johnson, S.R.; Baron, M.; Tyndall, A.; Matucci-Cerinic, M.; Naden, R.P.; Medsger, T.A. jr; Carreira, P.E.; et al. 2013 classification criteria for systemic sclerosis: an American College of Rheumatology/European League Against Rheumatism collaborative initiative. Arthritis Rheum 2013, 65, 2737–2747. [Google Scholar] [CrossRef] [PubMed]
- Weatherald, J.; Montani, D.; Jevnikar, M.; Jais, X.; Savale, L.; Humbert, M. Screening for pulmonary arterial hypertension in systemic sclerosis. Eur Respir Rev 2019, 28, 190023. [Google Scholar] [CrossRef] [PubMed]
- De Angelis, R.; Ferri, C.; Giuggioli, D.; Bajocchi, G.; Dagna, L.; Bellando-Randone, S.; Zanframundo, G.; Foti, R.; Cacciapaglia, F.; Cuomo, G.; et al. Systemic sclerosis sine scleroderma: clinical and serological features and relationship with other cutaneous subsets in a large series of patients from the national registry ‘SPRING’ of the Italian Society for Rheumatology. RMD Open 2023, 9:e002890. [CrossRef]
- Black, C.M. Measurement of skin involvement in scleroderma. J Rheumatol 1995, 22, 1217–1219. [Google Scholar] [PubMed]
- Salaffi, F.; Carotti, M.; Bosello, S.; Ciapetti, A.; Gutierrez, M.; Bichisecchi, E.; Giuseppetti, G.; Ferraccioli, G. Computer-aided quantification of interstitial lung disease from high resolution computed tomography images in systemic sclerosis: correlation with visual reader base score and physiologic tests. Biomed Res Int 2015, 2015, 834262. [Google Scholar] [CrossRef] [PubMed]
- Salaffi, F.; Carotti, M.; Di Donato, E.; Di Carlo, M.; Ceccarelli, M.; Giuseppetti, G. Computer-Aided tomographic analysis of interstitial lung disease (ILD) in patients with systemic sclerosis (SSc). Correlation with pulmonary physiologic tests and patient-centred measures of perceived dyspnoea and functional disability. PLoS One 2016,11: e0149240. [CrossRef]
- Warrick, J.H.; Bhalla, M.; Schabel, S.I.; Silver, R.M. High resolution computed tomography in early scleroderma lung disease. J Rheumatol 1991; 18, 1520–1528.
- Borg, E.; Borg, G.; Larsson, K.; Letzter, M.; Sundblad, B.M. An index for breathlessness and leg fatigue. Scand J Med Sci Sports 2010; 20, 644-650. [CrossRef]
- Clements, P.; Wong, W.K.; Hurwitz, E.L.; Furst, D.E.; Mayes, M.; White, B.; Wigley, F.; Weisman, M.; Barr, W.; Moreland, L.; et al. Correlates of the disability index of the Health Assessment Questionnaire: a measure of functional impairment in systemic sclerosis. Arthritis Rheum 1999; 42, 2372–2380. [CrossRef]
- Jonasson, C.; Wernersson, B.; Hoff, D.; Hatlebakk, J. Validation of the GerdQ questionnaire for the diagnosis of gastro-oesophageal reflux disease. Aliment Pharmacol Ther 2013; 37, 564-572. [CrossRef]
- Jones, R.; Junghard, O.; Dent, J.; Vakil, N.; Halling, K.; Wernersson, B.; Lind, T. Development of the GerdQ, a tool for the diagnosis and management of gastro-oesophageal reflux disease in primary care. Aliment Pharmacol Ther 2009, 30, 1030–1038. [Google Scholar] [CrossRef] [PubMed]
- Gutierrez, M.; Bertolazzi, C.; Tardella, M.; Becciolini, A.; Di Carlo, M.; Dottori, M.; Grassi, W.; De Angelis, R. Inter-reader reliability in assessment of nailfold capillary abnormalities by beginners: pilot study of an intensive videocapillaroscopy training programme. J Rheumatol 2012, 39, 1248–1255. [Google Scholar] [CrossRef]
- Smith, V.; Herrick, A.L.; Ingegnoli, F.; Damjanov, N.; De Angelis, R.; Denton, C.P. , Distler, O, Espejo K, Foeldvari I, Frech T, et al. EULAR study group on microcirculation in rheumatic diseases and the scleroderma clinical trials consortium group on capillaroscopy. Standardization of nailfold capillaroscopy for the assessment of patients with Raynaud’s phenomenon and systemic sclerosis. Autoimmun Rev 2020, 19, 102458. [Google Scholar] [CrossRef]
- De Angelis, R.; Riccieri, V.; Cipolletta, E.; Del Papa, N.; Ingegnoli, F.; Bosello, S.; Spinella, A.; Pellegrino, G.; de Pinto, M.; Papa, S.; et al. Significant nailfold capillary loss and late capillaroscopic pattern are associated with pulmonary arterial hypertension in systemic sclerosis. Rheumatology 2023 Online ahead of print. [CrossRef]
- Steele, R.; Hudson, M.; Lo, E.; Baron, M. Canadian Scleroderma Research Group. Clinical decision rule to predict the presence of interstitial lung disease in systemic sclerosis. Arthritis Care Res 2012, 64, 519–524. [Google Scholar] [CrossRef]
- Hoffmann-Vold, A.M.; Fretheim, H.; Halse, A.K. ; Seip M, Bitter, H. ; Wallenius, M.; Garen, T.; Salberg, A.; Brunborg, C.; Midtvedt, O.; et al. Tracking impact of interstitial lung disease in systemic sclerosis in a complete nationwide cohort. Am J Respir Crit Care Med 2019, 200, 1258–1266. [Google Scholar] [CrossRef]
- Caron, M.; Hoa, S.; Hudson, M.; Schwartzman, K.; Steel, R. Pulmonary function test as outcomes for systemic sclerosis in interstitial lung diseases. Eur Respir Rev 2018, 27, 170102. [Google Scholar] [CrossRef] [PubMed]
- Showalter, K.; Hoffmann, A.; Rouleau, G.; Aaby, D.; Lee, J.; Richardson, C.; Dematte, J.; Agrawal, R.; Chang, R.W.; Hinccliff, M. Performance of forced vital capacity and lung diffusion cut points for associated radiographic interstitial lung disease in systemic sclerosis. J Rheumatol 2018; 45, 1572-1576. [CrossRef]
- Suliman, Y.A.; Dobrota, R.; Huscher, D.; Nguyen-Kim, T.D.L.; Maurer, B.; Jordan, S.; Speich, R.; frauenfelder, T.; Distler, O. Pulmonary function tests: high rate of false-negative results in the early detection and screening of scleroderma-related interstitial lung disease. Arthritis Rheumatol 2015, 67, 3256–3261. [Google Scholar] [CrossRef] [PubMed]
- Antoniou, K.M.; Margaritopoulos, G.A.; Goh, N.S.; Karagiannis, K.; Desai, S.R.; Nicholson, A.G.; Siafakas, N.M.; Coghlan, J.G.; Denton, C.P.; Hansell, D.M.; Wells, A.U. Combined pulmonary fibrosis and emphysema in scleroderma-related lung disease has a major confounding effect on lung physiology and screening for pulmonary hypertension. Arthritis Rheum 2016, 68, 1004–1012. [Google Scholar] [CrossRef] [PubMed]
- Murphy, S.L.; Chen, Y.T.; Lee, Y.C.; Carns, N.; Aren, K.; Korman, B. ; Hinchcliff, M,; Varga, J. Differences in symptom experience among patients with systemic sclerosis: a cluster analytic approach to identifying subgroups. Rheumatology 2023, 62:SI64-SI73. [CrossRef]
- Tashkin, D.P.; Volkmann, E.R. ; Tseng, C-H. ; Kim, H.J.; Goldin, J.; Clements, P.; Furst, D.; Kanna, D.; Kleerup, E.; Roth, M.D.; Elashoff, R. Relationship between quantitative radiographic assessments of interstitial lung disease and physiological and clinical features of systemic sclerosis. Ann Rheum Dis 2016, 75, 374–381. [Google Scholar]
- Khanna, D.; Clements, P.J.; Furst, D.E.; Chon, Y.; Elashoff, R.; Roth, M.D.; Stertz, M.G.; Chung, J.; Fitzgerald, J.D.; Seibold, J.R.; et al. Correlation of the degree of dyspnea with health-related quality of life, functional abilities, and diffusing capacity for carbon monoxide in patients with systemic sclerosis and active alveolitis: results from the scleroderma lung study. Arthritis Rheum 2005, 52, 592–600. [Google Scholar] [CrossRef] [PubMed]
- Savarino, E.; Bazzica, M.; Zentilin, P.; Pohl, D.; Parodi, A.; Cittadini, G. , Negrini, S.; Indiveri, F.; Tutuian, R.; Savarino, V.; Ghio M. Gastroesophageal reflux and pulmonary fibrosis in scleroderma: a study using pH-impedance monitoring. Am J Respir Crit Care Med 2009;179, 408–413. [CrossRef]
- Richardson, C.; Agrawal, R.; Lee, J.; Almagor, O. ; Nelson, R,; Varga, J. ; Cuttica, M.J.; Dematte, J.D.; Chang, R.W.; Hinchcliff, M.E. Esophageal dilatation and interstitial lung disease in systemic sclerosis: a cross-sectional study. Semin Arthritis Rheum 2016, 46, 109–114. [Google Scholar] [CrossRef]
- Christmann, R.; Wells, A.; Capelozzi, V.; Silver, R. Gastroesophageal reflux incites interstitial lung disease in systemic sclerosis: clinical, radiologic, histopathologic, and treatment evidence. Semin Arthritis Rheum 2010, 40, 241–249. [Google Scholar] [CrossRef] [PubMed]
- De Lorenzis, E.; Wasson, C.W.; Del Galdo, F. Alveolar epithelial-to-mesenchymal transition in scleroderma interstitial lung disease: Technical challenges, available evidence, and therapeutic perspectives. J Scleroderma Related Dis 2024, 9, 7–15. [Google Scholar] [CrossRef]
- Volkmann, E.R.; Tashkin, D.P.; Leng, M.; Kim, G.H.J.; Goldin, J.; Roth, M.D. Association of symptoms of gastroesophageal reflux, oesophageal dilatation, and progression of systemic sclerosis-related interstitial lung disease. Arthritis Care Res 2023, 75, 1690–1697. [Google Scholar] [CrossRef]
- Liakouli, V.; Ciancio, A.; Del Galdo, F.; Giacomelli, R.; Ciccia, F. Systemic sclerosis interstitial lung disease: unmet needs and potential solutions. Nat Rev Rheumatol 2024, 20, 21–32. [Google Scholar] [CrossRef]
- Caetano, J.; Paula, F.S.; Amaral, M.; Oliveira, S.; Alves, J. Nailfold videocapillaroscopy changes are associated with the presence and severity of systemic sclerosis-related interstitial lung disease. J Clin Rheumatol 2019, 25: e12-e15. [CrossRef]
- Guillen-Del-Castillo, A.; Simeon-Aznar, C.P.; Callejas-Moraga, E.L.; Tolosa-Vilella, C.; Alonso-Vila, S. ; Fonollosa-Pla, V,; Selva-O’Callaghan, A. Quantitative videocapillaroscopy correlates with functional respiratory parameters: a clue for vasculopathy as a pathogenic mechanism for lung injury in systemic sclerosis. Arthritis Res Ther 2018, 20, 281. [Google Scholar] [CrossRef] [PubMed]
- Sulli, A.; Paolino, S.; Pizzorni, C.; Ferrari, G.; Pacini, G.; Pesce, G.; Carmisciano, L.; Smith, V.; Cutolo, M. Progression of nailfold capillaroscopic patterns and correlation with organ involvement in systemic sclerosis: a 12-year study. Rheumatology 2020, 59, 1051–1058. [Google Scholar] [CrossRef] [PubMed]
- Salaffi, F.; Carotti, M.; Di Carlo, M.; Ceccarelli, L.; Galli, M.; Sarzi-Puttini, P.; Giovagnoni, A. Predicting severe/critical outcomes in patients with SARS-CoV2 pneumonia: development of the prediCtion seveRe/crItical ouTcome in COVID-19 (CRITIC) model. Front Med 2021, 8, 695195. [Google Scholar] [CrossRef] [PubMed]
- Emrani, Z.; Karbalaie, A.; Fatemi, A.; Etahadtavakol, M.; Erlandsson, B.E. Capillary density: an important parameter in nailfold capillaroscopy. Microvascular Res 2017, 109, 7–18. [Google Scholar] [CrossRef]
- Rahaghi, F.F.; Hsu, V.M.; Kaner, R.J.; Mayes, M.D.; Rosas, I.O.; Saggar, R.; Steen, V.D.; Strek, M.E.; Bernstein, E.J.; Bhatt, N.; et al. Expert consensus on the management of systemic sclerosis-associated interstitial lung disease. Respir Res 2023, 24, 6. [Google Scholar] [CrossRef]
| Variables | Mean | SD | Median | 25 - 75 P | |
|---|---|---|---|---|---|
| Age (years) | 63.60 | 10.34 | 65.00 | 56.00 to 71.00 | |
| Disease duration (years) | 10.53 | 7.38 | 8.00 | 5.00 to 16.00 | |
| Modified Rodnan Skin Score | 10.70 | 7.97 | 9.00 | 4.00 to 16.00 | |
| HRCT extent of disease score | 5.64 | 3.69 | 3.00 | 3.00 to 9.00 | |
| HRCT severity of disease score | 5.97 | 4.03 | 4.50 | 3.00 to 8.00 | |
| HRCT total score | 11.62 | 7.79 | 6.00 | 5.00 to 18.00 | |
| DLco (% predicted) | 73.41 | 16.76 | 78.15 | 59.00 to 88.00 | |
| FVC (% predicted) | 87.72 | 18.51 | 88.95 | 76.00 to 103.00 | |
| HAQ-DI score | 0.96 | 0.45 | 0.92 | 0.62 to 1.12 | |
| m-Borg score | 2.73 | 2.22 | 2.00 | 1.00 to 5.00 | |
| Gerd-Q | 8.19 | 4.03 | 6.00 | 5.00 to 11.00 | |
| Capillary density | 5.44 | 2.22 | 5.15 | 3.43 to 7.65 | |
| Independent variables | Coefficient | Std. Error | t | P | rpartial | rsemipartial |
|---|---|---|---|---|---|---|
| (Constant) | 13.0435 | |||||
| Age | 0.0981 | 0.0851 | 1.153 | 0.253 | 0.1416 | 0.07871 |
| Sex | 0.1117 | 1.8317 | 0.061 | 0.951 | 0.0075 | 0.00416 |
| Disease duration | -0.1681 | 0.1285 | -1.309 | 0.195 | -0.1602 | 0.08935 |
| Anti-topoisomerase I | -0.0878 | 1.6181 | -0.054 | -0.956 | 0.0067 | 0.00370 |
| modified Rodnan Skin Score | -0.02611 | 0.0990 | -0.264 | 0.792 | -0.0326 | 0.01800 |
| DLco (% predicted) | -0.1101 | 0.0541 | -2.035 | 0.045 | -0.2448 | 0.13895 |
| FVC (% predicted) | -0.0341 | 0.0386 | -0.885 | 0.379 | -0.1091 | 0.06041 |
| HAQ-DI score | 2.6693 | 1.5923 | 1.676 | 0.098 | 0.2036 | 0.11442 |
| m-Borg | 1.3327 | 0.5202 | 2.562 | 0.012 | 0.3029 | 0.17491 |
| GERD-Q | 0.6810 | 0.2819 | 2.416 | 0.018 | 0.2870 | 0.16497 |
| Capillary density | -0.8847 | 0.4132 | -2.141 | 0.036 | -0.2567 | 0.14622 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





