Submitted:
21 April 2024
Posted:
07 May 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Results
2.1. Assessment of the Incidence of Transient GHD with Respect to Pediatric Criteria from 2000 (GH Peak below 10 µg/l, IGF-1 Deficiency Not Required) [3] in Relation to the Moment of rhGH Therapy Withdrawal and Patients’ Sex
2.2. Verification of GHD Diagnosis in Childhood and the Incidence of Transient GHD with Respect to Currently Proposed Pediatric Criteria [15]
- ✓
- “Unlikely” GHD – the patients with IGF 1 SDS over 0.0, who could have GHD excluded without stimulation tests;
- ✓
- “Doubtful” GHD – the patients with IGF-1 SDS below 0.0 and GH peak in stimulation tests between 7.0 µg/l and 10.0 µg/l, who did not fulfill the criteria of GHD after applying lower cut-off of GH peak in stimulation tests;
- ✓
- “True” GHD – the patients with IGF-1 SDS below 0.0 and GH peak below 7.0 µg/l, the only subgroup that should be treated with rhGH according to current guidelines [15].
- ✓
- transient GHD (Group transGHD) – patients with IGF-1 SDS at retesting over 0.0 or GH peak at retesting over 7.0 µg/l,
- ✓
- “childhood-only” GHD (Group childGHD) – patients with IGF-1 SDS below 0.0 and GH peak 5.0-7.0 µg/l
- ✓
- persistent GHD (Group persistGHD) – patients with IGF-1 SDS below 0.0 and GH peak in retesting below 5.0 µg/l.
2.3. Characteristics of the Patients with Persistent Severe GHD According to Current Criteria (GH Peak in Retesting below 3.0 µg/l) [18].
2.4. Effect of Application of Diagnostic Strategy Proposed by Wit et al. [16] on the Diagnosis of GHD in Childhood and during Retesting
2.5. Characteristics of Poor Responders to rhGH Therapy
3. Discussion
4. Materials and Methods
4.1. Auxological Indices
4.2. Hormonal Tests
4.3. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Grimberg, A.; DiVall, S.A.; Polychronakos, C.; Allen, D.B.; Cohen, L.E.; Quintos, J.B.; Rossi, W.C.; Feudtner, C.; Murad, M.H. Guidelines for Growth Hormone and Insulin-Like Growth Factor-I Treatment in Children and Adolescents: Growth Hormone Deficiency, Idiopathic Short Stature, and Primary Insulin-Like Growth Factor-I Deficiency. Horm. Res. Paediatr. 2016, 86, 361–397. [Google Scholar] [CrossRef] [PubMed]
- Ahmid, M.; Perry, C.G.; Ahmed, S.F.; Shaikh, M.G. Growth hormone deficiency during young adulthood and the benefits of growth hormone replacement. Endocr. Connect. 2016, 5, R1–R11. [Google Scholar] [CrossRef] [PubMed]
- Growth Hormone Research Society Consensus guidelines for the diagnosis and treatment of growth hormone (GH) deficiency in childhood and adolescence: summary statement of the GH Research Society. GH Research Society. J. Clin. Endocrinol. Metab. 2000, 85, 3990–3993. [CrossRef]
- Clayton, P.E.; Cuneo, R.C.; Juul, A.; Monson, J.P.; Shalet, S.M.; Tauber, M. Consensus statement on the management of the GH-treated adolescent in the transition to adult care. Eur. J. Endocrinol. 2005, 152, 165–170. [Google Scholar] [CrossRef]
- Ho, K.K.Y. Consensus guidelines for the diagnosis and treatment of adults with GH deficiency II: A statement of the GH Research Society in association with the European Society for Pediatric Endocrinology, Lawson Wilkins Society, European Society of Endocrinology, Japan Endocrine Society, and Endocrine Society of Australia. Eur. J. Endocrinol. 2007, 157, 695–700. [Google Scholar] [CrossRef]
- Yuen, K.C.J.; Biller, B.M.K.; Radovick, S.; Carmichael, J.D.; Jasim, S.; Pantalone, K.M.; Hoffman, A.R. American Association of Clinical Endocrinologists and American College of Endocrinology Guidelines for Management of Growth Hormone Deficiency in Adults and Patients Transitioning From Pediatric To Adult Care. Endocr. Pract. 2019, 25, 1191–1232. [Google Scholar] [CrossRef]
- Penta, L.; Cofini, M.; Lucchetti, L.; Zenzeri, L.; Leonardi, A.; Lanciotti, L.; Galeazzi, D.; Verrotti, A.; Esposito, S. Growth hormone (GH) therapy during the transition period: Should we think about early retesting in patients with idiopathic and isolated GH deficiency? Int. J. Environ. Res. Public Health. 2019, 16. [Google Scholar] [CrossRef] [PubMed]
- Cavarzere, P.; Gaudino, R.; Sandri, M.; Ramaroli, D.A.; Pietrobelli, A.; Zaffanello, M.; Guzzo, A.; Salvagno, G.L.; Piacentini, G.; Antoniazzi, F. Growth hormone retesting during puberty: a cohort study. Eur. J. Endocrinol. 2020, 182, 559–567. [Google Scholar] [CrossRef] [PubMed]
- Loche, S.; Bizzarri, C.; Maghnie, M.; Faedda, A.; Tzialla, C.; Autelli, M.; Casini, M.R.; Cappa, M. Results of early reevaluation of growth hormone secretion in short children with apparent growth hormone deficiency. J. Pediatr. 2002, 140, 445–449. [Google Scholar] [CrossRef]
- Bright, G.M.; Morris, P.A.; Rosenfeld, R.G. When Is a Positive Test for Pediatric Growth Hormone Deficiency a True-Positive Test? Horm. Res. Paediatr. 2022, 94, 399–405. [Google Scholar] [CrossRef]
- Allen, D.B. Diagnosis of Growth Hormone Deficiency Remains a Judgment Call-and That Is Good. Horm. Res. Paediatr. 2022, 94, 406–409. [Google Scholar] [CrossRef] [PubMed]
- Wit, J.-M.; Ranke, M.B.; Kelnar, C.J.H. The ESPE classification of paediatric endocrine diagnoses. Horm. Res. 2007, 68, 1–120. [Google Scholar]
- Gasco, V.; Corneli, G.; Beccuti, G.; Prodam, F.; Rovere, S.; Bellone, J.; Grottoli, S.; Aimaretti, G.; Ghigo, E. Retesting the childhood-onset GH-deficient patient. Eur. J. Endocrinol. 2008, 159, 45–52. [Google Scholar] [CrossRef] [PubMed]
- Meazza, C.; Gertosio, C.; Pagani, S.; Pilotta, A.; Tinelli, C.; Buzi, F.; Farello, G.; Genoni, G.; Bona, G.; Bozzola, M. Is retesting in growth hormone deficient children really useful? Minerva Endocrinol. 2017, 42, 325–330. [Google Scholar] [CrossRef]
- Collett-Solberg, P.F.; Ambler, G.; Backeljauw, P.F.; Bidlingmaier, M.; Biller, B.M.K.; Boguszewski, M.C.S.; Cheung, P.T.; Choong, C.S.Y.; Cohen, L.E.; Cohen, P.; et al. Diagnosis, Genetics, and Therapy of Short Stature in Children: A Growth Hormone Research Society International Perspective. Horm. Res. Paediatr. 2019, 92, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Wit, J.M.; Bidlingmaier, M.; de Bruin, C.; Oostdijk, W. A Proposal for the Interpretation of Serum IGF-I Concentration as Part of Laboratory Screening in Children with Growth Failure. J. Clin. Res. Pediatr. Endocrinol. 2020, 12, 130–139. [Google Scholar] [CrossRef] [PubMed]
- Palczewska I, Niedźwiecka Z. Indices of somatic development of children and adolescents in Warsaw. Develop. Pediatr. Med. 2001, Suppl 1 to 5, 17–118. [in Polish].
- Lewiński, A.; Smyczyńska, J.; Stawerska, R.; Hilczer, M.; Stasiak, M.; Bednarczuk, T.; Bolanowski, M.; Junik, R.; Ruchała, M.; Syrenicz, A.; et al. National Program of Severe Growth Hormone Deficiency Treatment in Adults and Adolescents after Completion of Growth Promoting Therapy. Pol. J. Endocrinol. 2018, 69, 468–524. [Google Scholar] [CrossRef]
- Tauber, M.; Moulin, P.; Pienkowski, C.; Jouret, B.; Rochiccioli, P. Growth hormone (GH) retesting and auxological data in 131 GH-deficient patients after completion of treatment. J. Clin. Endocrinol. Metab. 1997, 82, 352–356. [Google Scholar] [CrossRef]
- Maghnie, M.; Strigazzi, C.; Tinelli, C.; Autelli, M.; Cisternino, M.; Loche, S.; Severi, F. Growth hormone (GH) deficiency (GHD) of childhood onset: reassessment of GH status and evaluation of the predictive criteria for permanent GHD in young adults. J. Clin. Endocrinol. Metab. 1999, 84, 1324–1328. [Google Scholar] [CrossRef]
- Aimaretti, G.; Baffoni, C.; Bellone, S.; Di Vito, L.; Corneli, G.; Arvat, E.; Benso, L.; Camanni, F.; Ghigo, E. Retesting young adults with childhood-onset growth hormone (GH) deficiency with GH-releasing-hormone-plus-arginine test. J. Clin. Endocrinol. Metab. 2000, 85, 3693–3699. [Google Scholar] [CrossRef]
- Cacciari, E.; Tassoni, P.; Parisi, G.; Pirazzoli, P.; Zucchini, S.; Mandini, M.; Cicognani, A.; Balsamo, A. Pitfalls in diagnosing impaired growth hormone (GH) secretion: retesting after replacement therapy of 63 patients defined as GH deficient. J. Clin. Endocrinol. Metab. 1992, 74, 1284–1289. [Google Scholar] [CrossRef]
- Zucchini, S.; Pirazzoli, P.; Baronio, F.; Gennari, M.; Bal, M.O.; Balsamo, A.; Gualandi, S.; Cicognani, A. Effect on adult height of pubertal growth hormone retesting and withdrawal of therapy in patients with previously diagnosed growth hormone deficiency. J. Clin. Endocrinol. Metab. 2006, 91, 4271–4276. [Google Scholar] [CrossRef]
- Bizzarri, C.; Pedicelli, S.; Boscherini, B.; Bedogni, G.; Cappa, M.; Cianfarani, S. Early retesting by GHRH + arginine test shows normal GH response in most children with idiopathic GH deficiency. J. Endocrinol. Invest. 2015, 38, 429–436. [Google Scholar] [CrossRef]
- Lanzetta, M.A.; Dalla Bona, E.; Tamaro, G.; Vidonis, V.; Vittori, G.; Faleschini, E.; Barbi, E.; Tornese, G. Clinical and laboratory characteristics but not response to treatment can distinguish children with definite growth hormone deficiency from short stature unresponsive to stimulation tests. Front. Endocrinol. (Lausanne). 2024, 15, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Smyczyńska, J.; Stawerska, R.; Lewiński, A.; Hilczer, M. Incidence and predictors of persistent growth hormone deficiency (GHD) in patients with isolated, childhood-onset GHD. Pol. J. Endocrinol. 2014, 65, 334–341. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, T.; Soneda, S.; Sato, N.; Kishi, K.; Noda, M.; Ogasawara, A.; Nose, O.; Nakano, Y.; Kinoshita, E.; Mochizuki, T.; et al. The Boy:Girl ratio of children diagnosed with growth hormone deficiency-induced short stature is associated with the boy:Girl ratio of children visiting short stature clinics. Horm. Res. Paediatr. 2021, 94, 211–218. [Google Scholar] [CrossRef]
- Henry, R.K.; Mamilly, L.; Chaudhari, M.; Klamer, B.G.; Nikahd, M.; Pyle-Eilola, A.L. Beyond the bias! Sex distribution in paediatric growth hormone deficiency reexamined. Clin. Endocrinol. (Oxf). 2024, 100, 441–446. [Google Scholar] [CrossRef] [PubMed]
- Migliaretti, G.; Ditaranto, S.; Guiot, C.; Vannelli, S.; Matarazzo, P.; Cappello, N.; Stura, I.; Cavallo, F. Long-term response to recombinant human growth hormone treatment: a new predictive mathematical method. J. Endocrinol. Invest. 2018, 41, 839–848. [Google Scholar] [CrossRef]
- Smyczyńska, U.; Smyczyńska, J.; Hilczer, M.; Stawerska, R.; Tadeusiewicz, R.; Lewiński, A. Pre-treatment growth and IGF-I deficiency as main predictors of response to growth hormone therapy in neural models. Endocr. Connect. 2018, 7, 239–249. [Google Scholar] [CrossRef]
- Carel, J.C.; Ecosse, E.; Nicolino, M.; Tauber, M.; Leger, J.; Cabrol, S.; Bastie-Sigeac, I.; Chaussain, J.L.; Coste, J. Adult height after long term treatment with recombinant growth hormone for idiopathic isolated growth hormone deficiency: observational follow up study of the French population based registry. BMJ 2002, 325, 70. [Google Scholar] [CrossRef] [PubMed]
- de Ridder, M.A.J.; Stijnen, T.; Hokken-Koelega, A.C.S. Prediction of adult height in growth-hormone-treated children with growth hormone deficiency. J. Clin. Endocrinol. Metab. 2007, 92, 925–931. [Google Scholar] [CrossRef] [PubMed]
- Ranke, M.B.; Lindberg, A.; Martin, D.D.; Bakker, B.; Wilton, P.; Albertsson-Wikland, K.; Cowell, C.T.; Price, D.A.; Reiter, E.O.; Kabi Intl Growth Study Pfizer, I. The mathematical model for total pubertal growth in idiopathic growth hormone (GH) deficiency suggests a moderate role of GH dose. J. Clin. Endocrinol. Metab. 2003, 88, 4748–4753. [Google Scholar] [CrossRef] [PubMed]
- Lonero A, Giotta M, Guerrini G, Calcaterra V, Galazzi E, Iughetti L, Cassio A, Wasniewska GM, Mameli C, Tornese G, Salerno M, Cherubini V, Caruso Nicoletti M, Street ME, Grandone A, Giacomozzi C, Faienza MF, Guzzetti C, Bellone S, Parpagnoli M, Musolino G, Maggio MC, Bozzola M, Trerotoli P, Delvecchio M; Study Group on Physiopathology of growth processes of ISPED. Isolated childhood growth hormone deficiency: a 30-year experience on final height and a new prediction model. J. Endocrinol. Invest 2022, 45, 1709–1717. [CrossRef] [PubMed]
- Brettell, E.; Högler, W.; Woolley, R.; Cummins, C.; Mathers, J.; Oppong, R.; Roy, L.; Khan, A.; Hunt, C.; Dattani, M. The Growth Hormone Deficiency (GHD) Reversal Trial: effect on final height of discontinuation versus continuation of growth hormone treatment in pubertal children with isolated GHD—a non-inferiority Randomised Controlled Trial (RCT). Trials 2023, 24, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Hilczer, M.; Smyczyńska, J.; Lewiński, A. Limitations of clinical utility of growth hormone stimulating tests in diagnosing children with short stature. Endocr. Regul. 2006, 40, 69–75. [Google Scholar] [PubMed]
- Kamoun, C.; Hawkes, C.P.; Grimberg, A. Provocative growth hormone testing in children: how did we get here and where do we go now? J. Pediatr. Endocrinol. Metab. 2021, 34, 679–696. [Google Scholar] [CrossRef] [PubMed]
- Partenope, C.; Galazzi, E.; Albanese, A.; Bellone, S.; Rabbone, I.; Persani, L. Sex steroid priming in short stature children unresponsive to GH stimulation tests: Why, who, when and how. Front. Endocrinol. (Lausanne). 2022, 13, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Binder, G.; Reinehr, T.; Ibáñez, L.; Thiele, S.; Linglart, A.; Woelfle, J.; Saenger, P.; Bettendorf, M.; Zachurzok, A.; Gohlke, B.; et al. GHD Diagnostics in Europe and the US: An Audit of National Guidelines and Practice. Horm. Res. Paediatr. 2020, 92, 150–156. [Google Scholar] [CrossRef]
- Rapaport, R.; Wit, J.M.; Savage, M.O. Growth failure: ‘Idiopathic’ only after a detailed diagnostic evaluation. Endocr. Connect. 2021, 10, R125–R138. [Google Scholar] [CrossRef]
- Greulich, W.W.; Pyle, S.I. Radiographic Atlas of Skeletal Development of the Hand and Wrist, 2nd ed.; Stanford University Press: Stanford, 1993; pp. 1–272. [Google Scholar]
- Felício, J.S.; Janaú, L.C.; Moraes, M.A.; Zahalan, N.A.; de Souza Resende, F.; de Lemos, M.N.; de Souza Neto, N.J.K.; Farias de Franco, I.I.; Leitão, L.T.C.; Silva, L. de S. d. A.; et al. Diagnosis of Idiopathic GHD in Children Based on Response to rhGH Treatment: The Importance of GH Provocative Tests and IGF-1. Front. Endocrinol. (Lausanne). 2019, 10, 1–9. [CrossRef] [PubMed]
- Guzzetti, C.; Ibba, A.; Pilia, S.; Beltrami, N.; Di Iorgi, N.; Rollo, A.; Fratangeli, N.; Radetti, G.; Zucchini, S.; Maghnie, M.; et al. Cut-off limits of the peak GH response to stimulation tests for the diagnosis of GH deficiency in children and adolescents: Study in patients with organic GHD. Eur. J. Endocrinol. 2016, 175, 41–47. [Google Scholar] [CrossRef] [PubMed]
- Siemens Healthcare Diagnostics Inc. Introducing the Restandardized Insulin-Like Growth Factor-I (IGF-I) Assay. Cust. Bull. 2016, 5.
- Chanson, P.; Arnoux, A.; Mavromati, M.; Brailly-Tabard, S.; Massart, C.; Young, J.; Piketty, M.L.; Souberbielle, J.C. Reference values for IGF-I serum concentrations: Comparison of six immunoassays. J. Clin. Endocrinol. Metab. 2016, 101, 3450–3458. [Google Scholar] [CrossRef] [PubMed]
- Aneke-Nash, C.S.; Dominguez-Islas, C.; Bůžková, P.; Qi, Q.; Xue, X.; Pollak, M.; Strickler, H.D.; Kaplan, R.C. Agreement between circulating IGF-I, IGFBP-1 and IGFBP-3 levels measured by current assays versus unavailable assays previously used in epidemiological studies. Growth Horm. IGF Res. 2016, 26, 11–16. [Google Scholar] [CrossRef]
- Blum, W.F.; Schweizer, R. Insulin-like growth factors and their binding proteins. In Diagnostics of Endocrine Function in Children and Adolescents; Ranke, M.B., Ed.; Karger, Basel, 2003; pp. 166–169.
- Elmlinger, M.W.; Kühnel, W.; Weber, M.M.; Ranke, M.B. Reference ranges for two automated chemiluminescent assays for serum insulin-like growth factor I (IGF-I) and IGF-binding protein 3 (IGFBP-3). Clin. Chem. Lab. Med. 2004, 42, 654–664. [Google Scholar] [CrossRef]
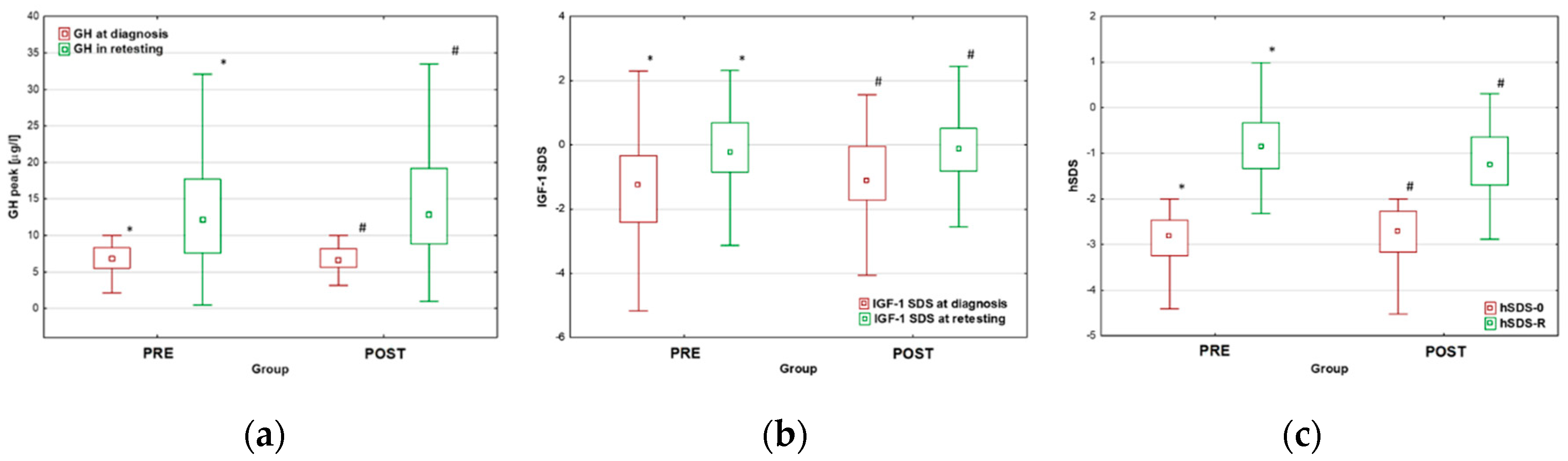
| All | Group PRE | Group POST | p | |
|---|---|---|---|---|
| N (boys/girls)* | 260 (173/87) | 121 (92/29) | 139 (81/58) | |
| Age at therapy onset [years] Age at retesting [years] Therapy duration [years] |
13.2 (11.9-14.4) 17.6 (16.5;18.3) 4.2 (3.4;5.2) |
13.7 (12.4;14.7) 17.6 (16.8;18.3) 3.9 (2.9;4.7) |
12.7 (11.5;14.0) 17.6 (16.4;18.3) 4.5 (3.8;5.6) |
0.001 0.985 <0.001 |
| GH peak at diagnosis [µg/l] GH peak in retesting [µg/l] Δ GH peak [µg/l] |
6.80 (5.58-8.23) 12.40 (7.98;18.45) 7.54 (1.25;11.29) |
6.86 (5.51;8.30) 12.20 (7.57;17.70) 7.22 (0.90;10.70) |
7.22 (0.90;10.70) 12.80 (8.84;19.20) 7.82 (1.81;11.95) |
0.960 0.262 0.328 |
| IGF-1 SDS at diagnosis IGF-1 SDS at retesting Δ IGF-1 SDS |
-1.23 (-1.94;-0.18) -0.18 (-0.81;0.58) 0.99 (0.04;2.11) |
-1.26 (-2.42;-0.33) -0.23 (-0.84;0.69) 1.30 (0.17;2,65) |
-1.12 (-1.72;-0.05) -0.13 (-0.82;0.51) 1.04 (0.17;1,91) |
0.135 0.879 0.209 |
| hSDS-0 TH SDS corr hSDS-0 hSDS-R corr hSDS-R Δ hSDS |
-2.76 (-3.20;-2.43) -1.08 (-1.58;-0.50) -1.70 (-2.31;-1.12) -1.02 (-1.54;-0.52) -0.01 (-0.59;0.57) 1.74 (1.29;2.28) |
-2.81 (-3.26;-2.47) -0.92 (-1.41;-0.46) -1.89 (-2.42;-1.43) -0.86 (-1.33;-0.33) 0.09 (-0.52;0.62) 2.01 (1.56;2.56) |
-2.71 (-3.17;-2.27) -1.21 (-1.70;-0.58) -1.58 (-2.19;-0.99) -1.26 (-1.70;-0.64) -0.01 (-0.60;0.57) 1.58 (1.01;2.06) |
0.166 0.029 0.010 <0.001 0.024 <0.001 |
| GH peak [µg/l] | All (n=260) | Group PRE (n=121) | Group POST (n=139) |
|---|---|---|---|
|
<3.0 3.0-6.0 6.0-10.0 |
10 (3.85%) 24 (9.23%) 58 (22.31%) |
9 (7.44%) 12 (9.91%) 97 (19.83%) |
1 (0.72%) 12 (8.63%) 34 (24.46%) |
| >10.0 | 168 (64.61%) | 76 (62.81%) | 92 (66.19%) |
| GH peak [µg/l] | Boys (n=173) | Girls (n=87) |
|---|---|---|
|
<3.0 3.0-6.0 6.0-10.0 |
7 (4.05%) 13 (7.51%) 29 (16.76%) |
3 (3.45%) 11 (12.65%) 29 (33.33%) |
| >10.0 | 124 (71.68%*) | 92 (66.19%*) |
| Boys | Girls | p | |
| N (%)* | 173 (66.5%) | 87 (33.5%) | |
| Age at therapy onset [years] Age at retesting [years] Therapy duration [years] |
13.8 (12.6;14.8) 18.0 (17.5;18.7) 4.3 (3.4;5.3) |
11.9 (10.7;12.8) 16.1 (15.4;16.9) 4.1 (3.3;5.1) |
<0.001 <0.001 0.442 |
| GH peak at diagnosis [µg/l] GH peak in retesting [µg/l] Δ GH peak [µg/l] |
6.53 (5.28;8.20) 14.20 (8.91;19.30) 7.85 (2.60;12.20) |
7.20 (5.97;8.28) 10.20 (7.19;14.70) 2.96 (0.28;7.50) |
0.117 <0.001 <0.001 |
| IGF-1 SDS at diagnosis IGF-1 SDS at retesting Δ IGF-1 SDS |
-1.26 (-2.06;-0.24) -0.05 (-0.84;0.61) 1.23 (0.11;2.32) |
-1.05 (-1.80;-0.16) -0.34 (-0.79;0.42) 0.98 (-0.24;1.93) |
0.314 0.261 0.267 |
| hSDS-0 TH SDS corr hSDS-0 hSDS-R corr hSDS-R Δ hSDS |
-2.84 (-3.30;-2.49) -1.00 (-1.58;-0.50) -1.79 (-2.31;-1.18) -1.07 (-1.45;-0.46) 0.03 (-0.59;0.62) 1.81 (1.40;2.31) |
-2.65 (-3.12;-2.24) -1.08 (-1.67;-0.50) -1.62 (-2.32;-0.97) -0.98 (-1.66;-0.58) 0.00 (-0.58;0.47) 1.61 (1.15;2.09) |
0.519 0.910 0.330 0.519 0.640 0.020 |
|
Childhood Retesting |
“Unlikely” GHD (n=55) |
“Doubtful” GHD (n=96) |
“True” GHD (n=109) |
||||
| Boys (n=37) |
Girls (n=18) |
Boys (n=62) |
Girls (n=34) |
Boys (n=74) |
Girls (n=35) |
||
| transGHD (n=139) | 34 | 15 | 58 | 28 | 64 | 30 | |
|
childGHD (n=15) persistGHD (n=16) |
1 2 |
2 1 |
3 1 |
4 2 |
5 5 |
0 5 |
|
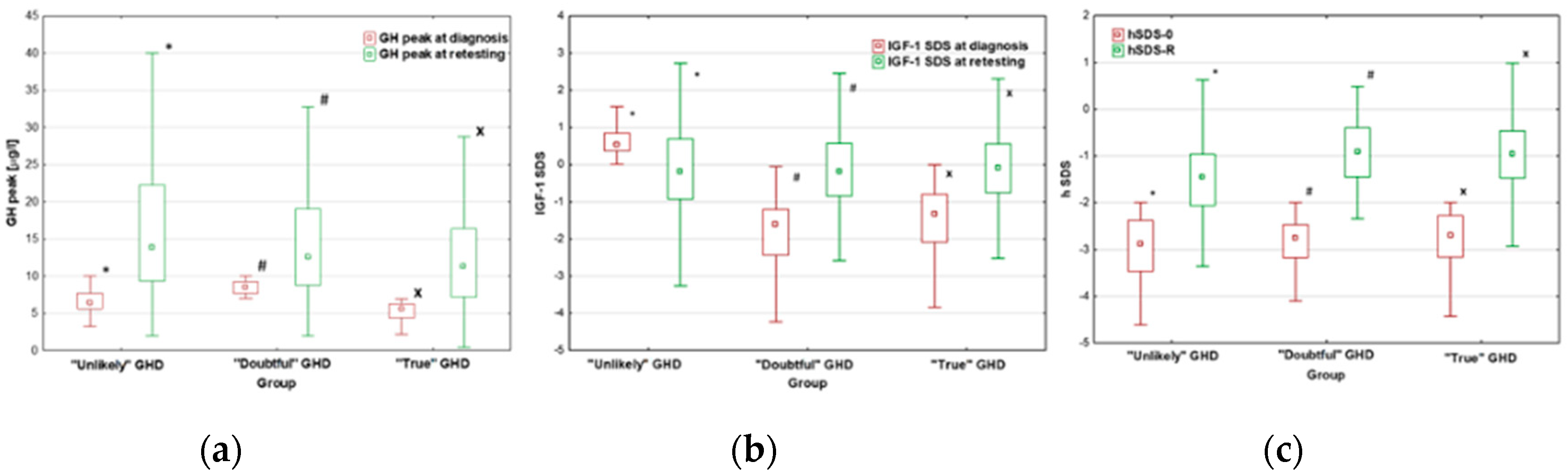
| “Unlikely” GHD | “Doubtful” GHD | “True” GHD | p | |
|---|---|---|---|---|
| N (boys/girls)* | 55 (37/18) | 96 (62/32) | 109 (74/35) | |
| Age at therapy onset [years] Age at retesting [years] Therapy duration [years] |
12.8 (11.3-14.7) 17.3 (16.3;18.5) 4.1 (2.9;5.7) |
13.2 (11.9;14.2) 17.5 (16.3;18.2) 4.1 (3.3;5.1) |
13.3 (12.0;14.5) 17.7 (17.1;18.4) 4.2 (3.6;5.1) |
0.001 0.985 <0.001 |
| GH peak at diagnosis [µg/l] GH peak in retesting [µg/l] Δ GH peak [µg/l] |
6.41 (5.60;7.70) 12.90 (9.30;22.30) 7.70 (3.50;16.00) |
8.52 (7.68;9.25) 12.60 (8.78;19.05) 4.20 (0.69;10.38) |
5.60 (4.40;6.28) 11.30 (7.17;16.40) 6.22 (1.11;11.19) |
<0.001 0.017 0.018 |
| IGF-1 SDS at diagnosis IGF-1 SDS at retesting Δ IGF-1 SDS |
0.54 (0.37;0.85) -0.41 (-0.93;0.69) -1.12 (-1.56;0.05) |
-1.60 (-2.43;-1.20) -0.19 (-0.85;0.57) 1.60 (0.61;2.78) |
-1.33 (-2.09;-0.80) -0.09 (-0.75;0.56) 1.50 (0.60;2.22) |
<0.001 0.991 <0.001 |
| hSDS-0 TH SDS corr hSDS-0 hSDS-R corr hSDS-R Δ hSDS |
-2.88 (-3.47;-2.38) -1.39 (-1.68;-0.75) -1.57 (-2.28;-0.99) -1.45 (-2.06;-0.96) -0.15 (-0,73;0.12) 1.41 (0.91;2.08) |
-2.76 (-3.18;-2.47) -0.92 (-1.51;-0.49) -1.86 (-2.39;-1.17) -0.91 (-1.45;-0.40) 0.12 (-0.62;0.78) 1.94 (1.48;2.30) |
-2.70 (-3.17;-2.28) -1.06 (-1.58;-0.50) -1.66 (-2.28;-1.03) -0.96 (-1.47;-0.46) 0.08 (-0.52;0.61) 1.69 (1.34;2.31) |
0.272 0.109 0.468 <0.001 0.020 0.010 |
|
Childhood Retesting |
“Pre-test unlikely” GHD (n=168) |
“Excluded” GHD (n=45) |
“Confirmed” GHD (n=47) |
||||
| Boys (n=110) |
Girls (n=58) |
Boys (n=62) |
Girls (n=32) |
Boys (n=74) |
Girls (n=35) |
||
| T-GHD (n=247) | 107 | 57 | 32 | 10 | 25 | 16 | |
|
NT-GHD (n=3) P-GHD (n=10) |
1 0 |
1 2 |
1 0 |
0 2 |
0 5 |
0 1 |
|
| “Pre-test Unlikely” GHD | “Excluded” GHD | “Confirmed” GHD | p | |
| N (boys/girls)* | 168 (110/58) | 45 (33/12) | 47 (30/17) | |
| Age at therapy onset [years] Age at retesting [years] Therapy duration [years] |
12.8 (11.6;14.2) 17.4 (16.4;18.4) 4.3 (3.4;5.4) |
13.7 (12.7;14.4) 17.8 (17.0;18.2) 4.1 (3.4;4.6) |
13.7 (12.1;14.8) 17.7 (17.0;18.3) 4.0 (3.4;5.1) |
0.471 0.233 0.425 |
| GH peak at diagnosis [µg/l] GH peak in retesting [µg/l] Δ GH peak [µg/l] |
6.75 (5.63;8.09) 13.90 (9.06;20.15) 7.38 (2.33;13.18) |
8.69 (7.60;9.38) 12.40 (8.37;17.80) 3.72 (-0.68;8.57) |
4.84 (3.73;5.97) 8.40 (4.06;13.00) 4.03 (0.62;8.10) |
<0.001 0.017 0.018 |
| IGF-1 SDS for CA at diagnosis IGF-1 SDS for BA at diagnosis IGF-1 SDS for CA at retesting Δ IGF-1 SDS for CA |
-0.59 (-1.24;0.35) 0.14 (-0.48;0.78) 0.04 (-0.58;0.69) 0.52 (-0.69;1.55) |
-2.45 (-3.03;-1.91) -1.73 (-2.42;1.27) -0.46 (-1.04;0.33) 2.15 (1.34;3.29) |
-2.48 (-3.30;-1.64) -1.52 (-2.35;1.23) -0.46 (-0.95;0.56) 2.06 (0.87;3.07) |
<0.001 <0.001 0.069 <0.001 |
| hSDS-0 TH SDS corr hSDS-0 hSDS-R corr hSDS-R Δ hSDS |
-2.71 (-3.17;-2.38) -1.08 (-1.67;-0.50) -1.65 (-2.31;-1.13) -1.18 (-1.66;-1.04) -0.04 (-0,63;0.36) 1.58 (1.13;2.14) |
-2.81 (-3.32;-2.53) -1.08 (-1.57;-0.58) -1.76 (-2.27;-1.14) -0.79 (-1.34;-0.21) 0.37 (-0.22;0.88) 2.12 (1.73;2.51)) |
-2.84 (-3.24;-2.28) -1.07 (-1.58;-0.33) -1.78 (-2.35;-0.97) -0.76 (-1.42;-0.29) 0.12 (-0.59;0.70) 2.02 (1.46;2.66) |
0.425 0.685 0.964 0.011 0.009 <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





