Submitted:
12 March 2024
Posted:
13 March 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Fabrication of Electrospun Nanofibers
2.3. Morphological Characterization
2.4. Thermogravimetric Analysis
2.5. Fourier-transform Infrared Spectroscopy (FTIR) Analysis
2.6. Mechanical Characterization
2.7. In vitro Degradation Assays
2.8. Antibacterial Assay
Determination of Growth Inhibition Zones of the H. lupulus Extract
Determination of Growth Inhibition Zones of the Matrices
2.9. Cell Culture and Cell Viability Assay
2.10. Statistical Analysis
3. Results
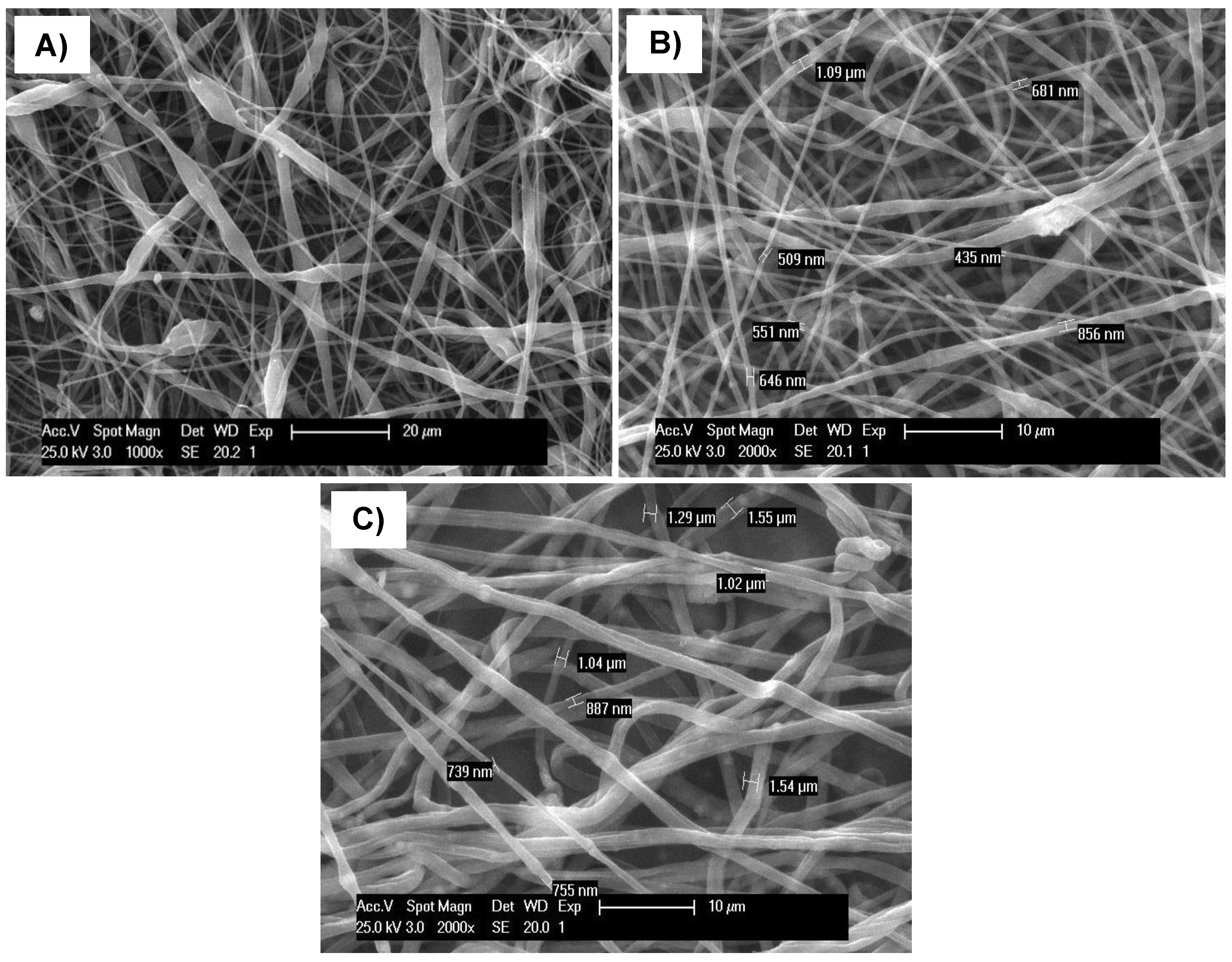
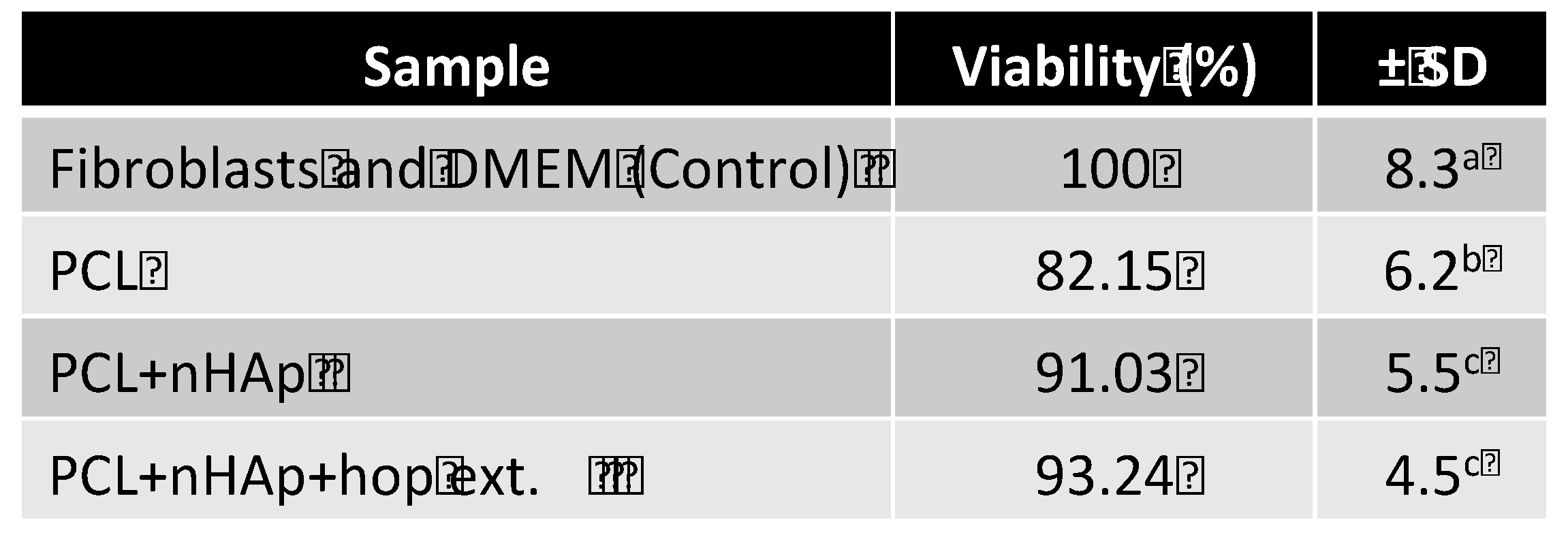
3.1. Morphological Characterization
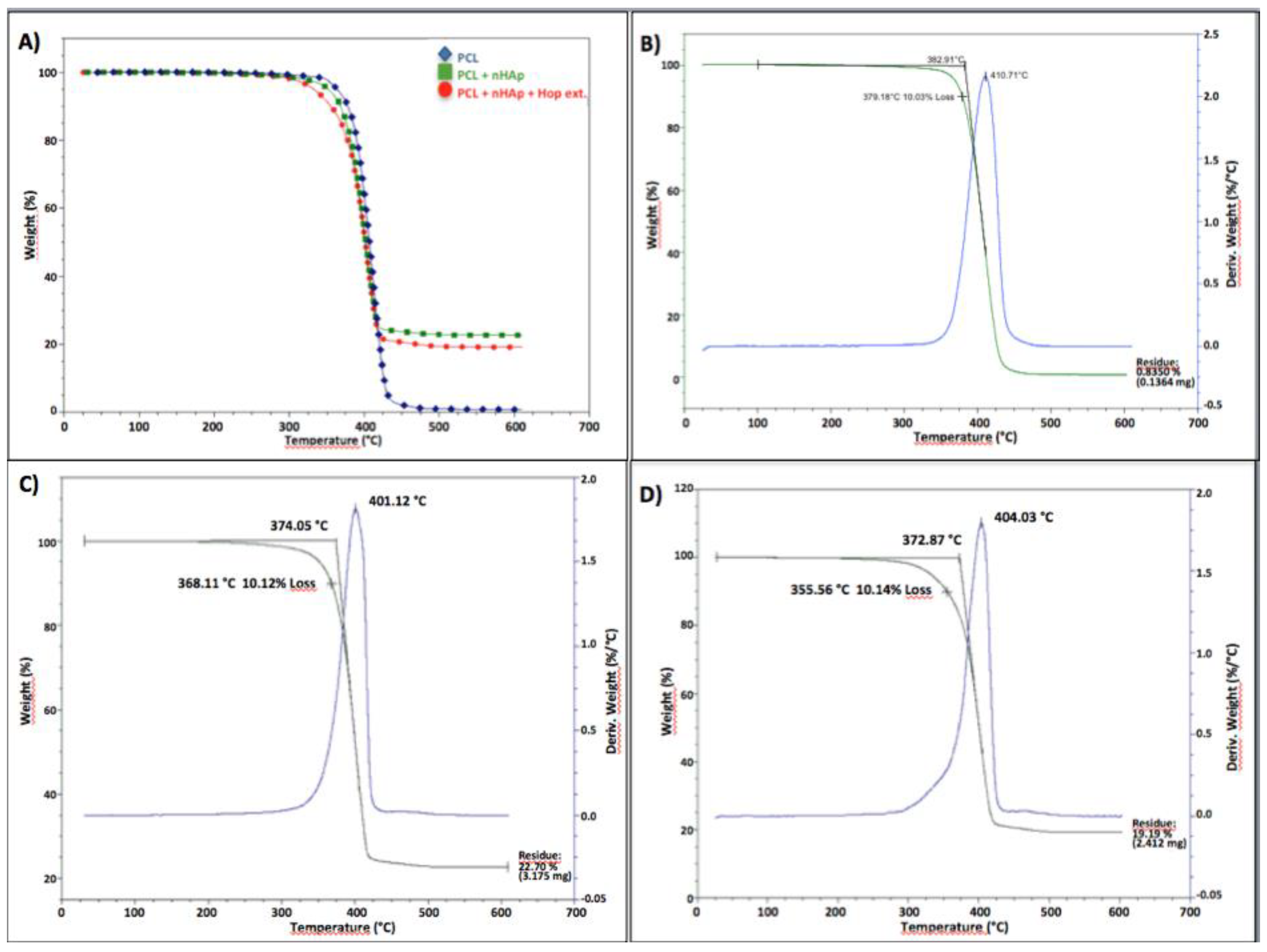
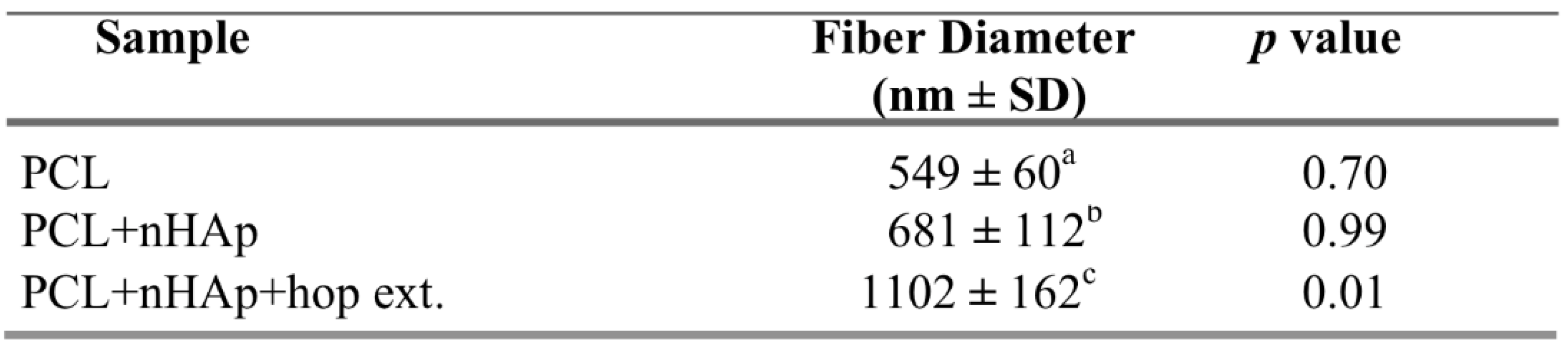
3.2. Thermogravimetric Analysis (TGA)
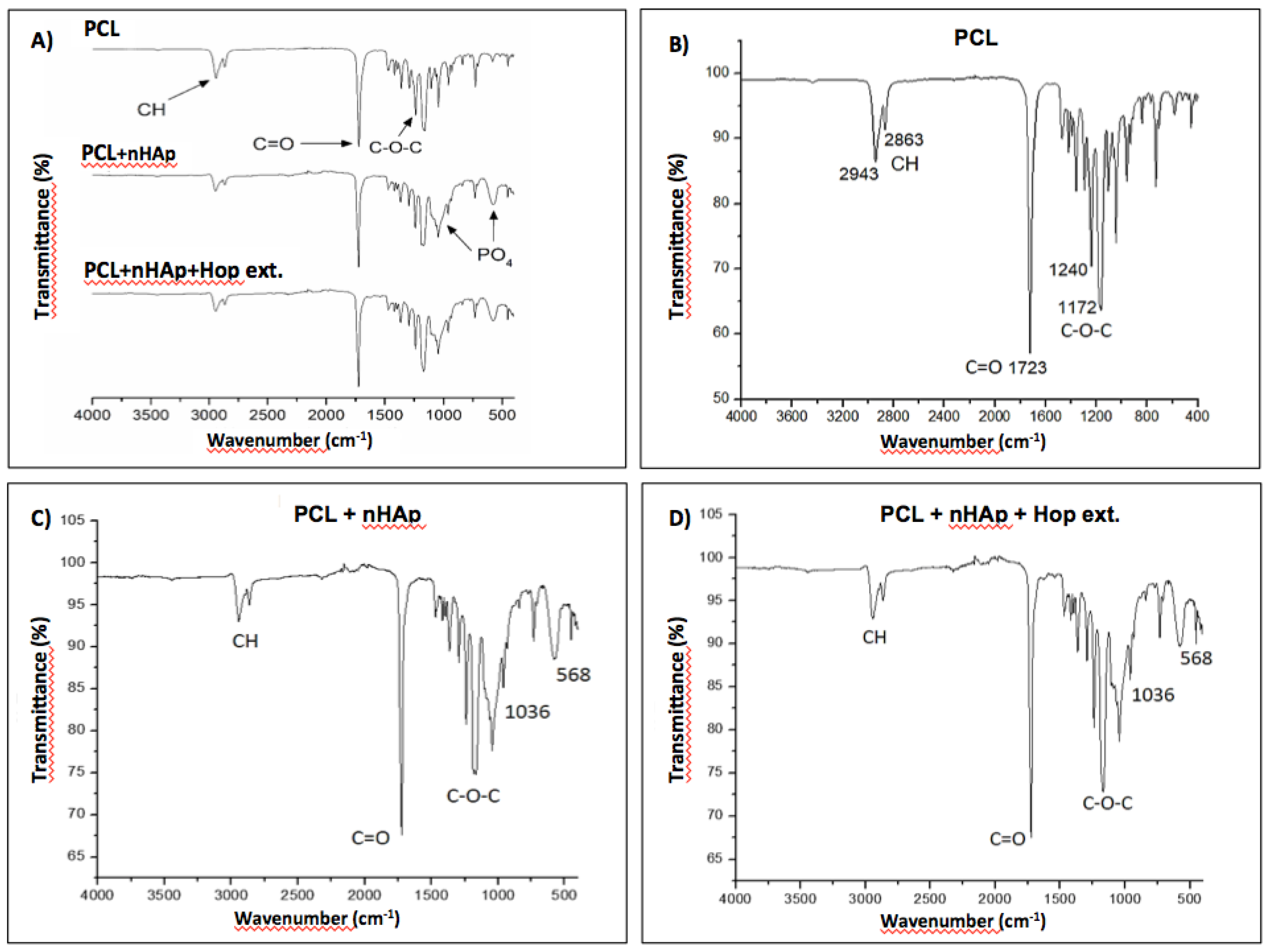
3.3. FTIR Analysis
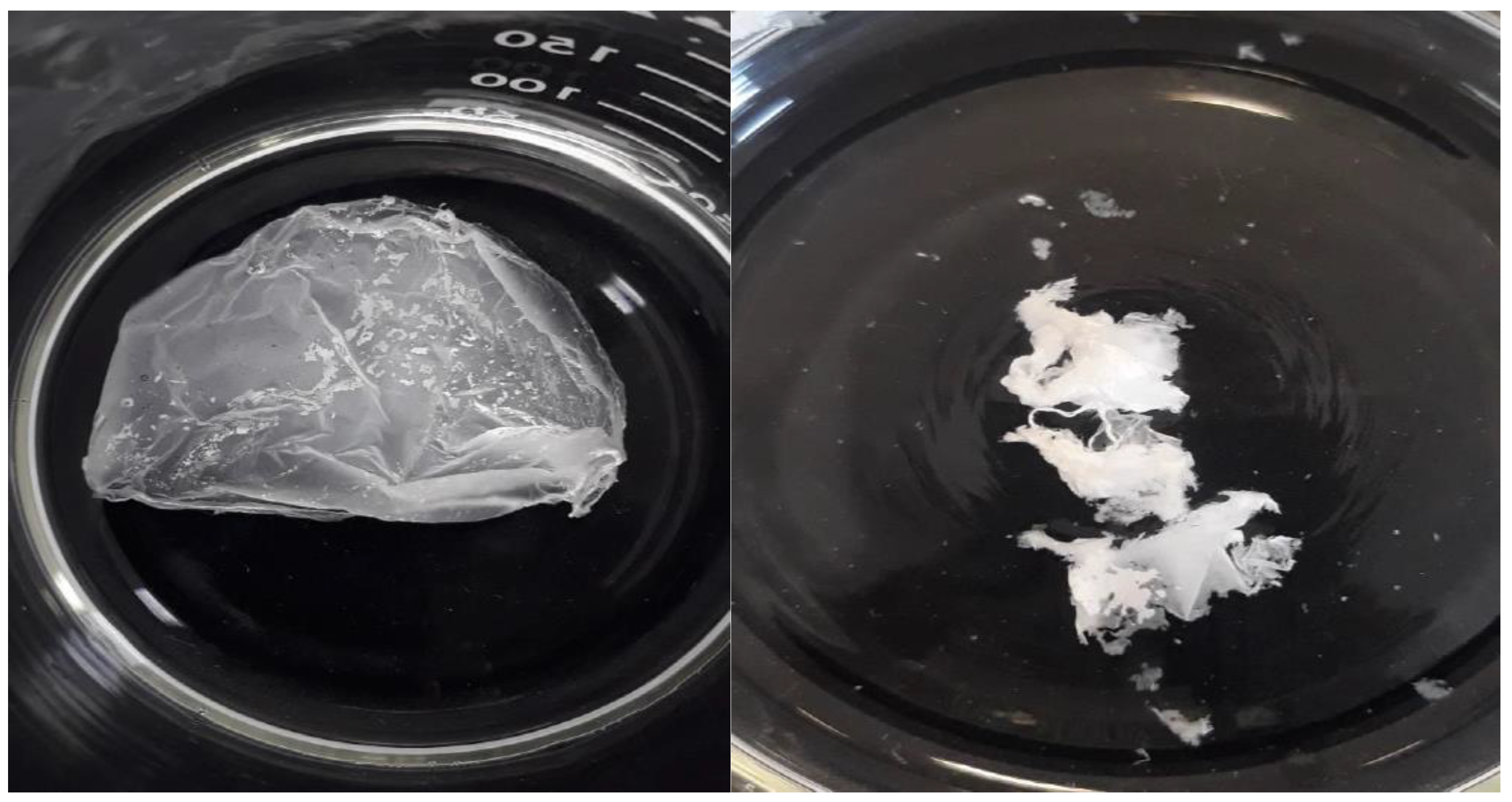
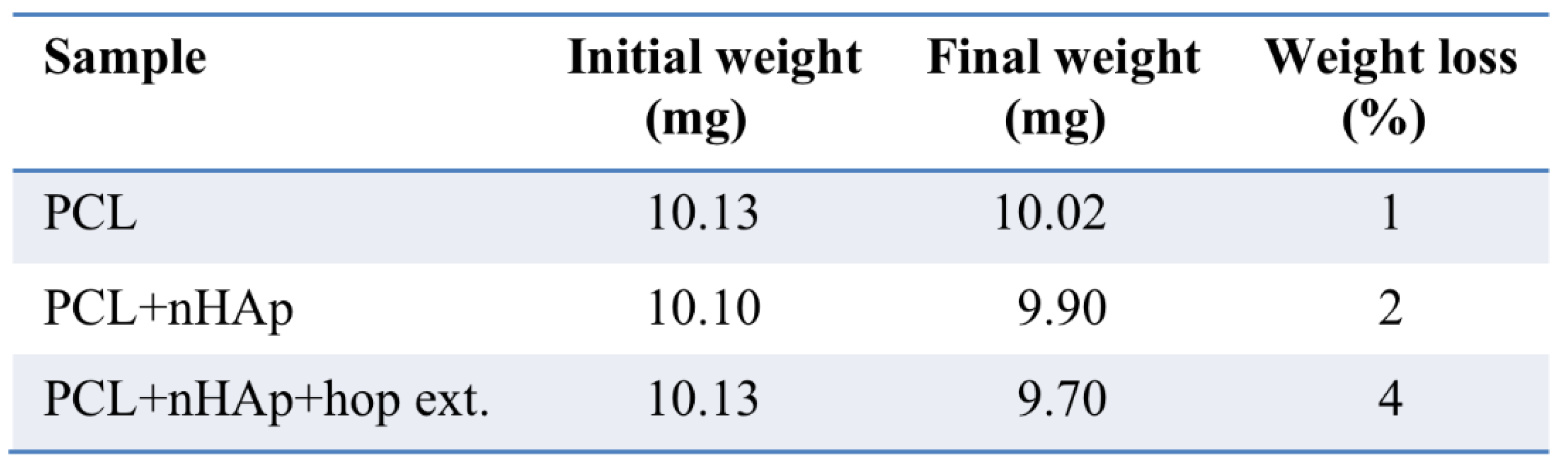
3.4. In Vitro Degradation Analysis
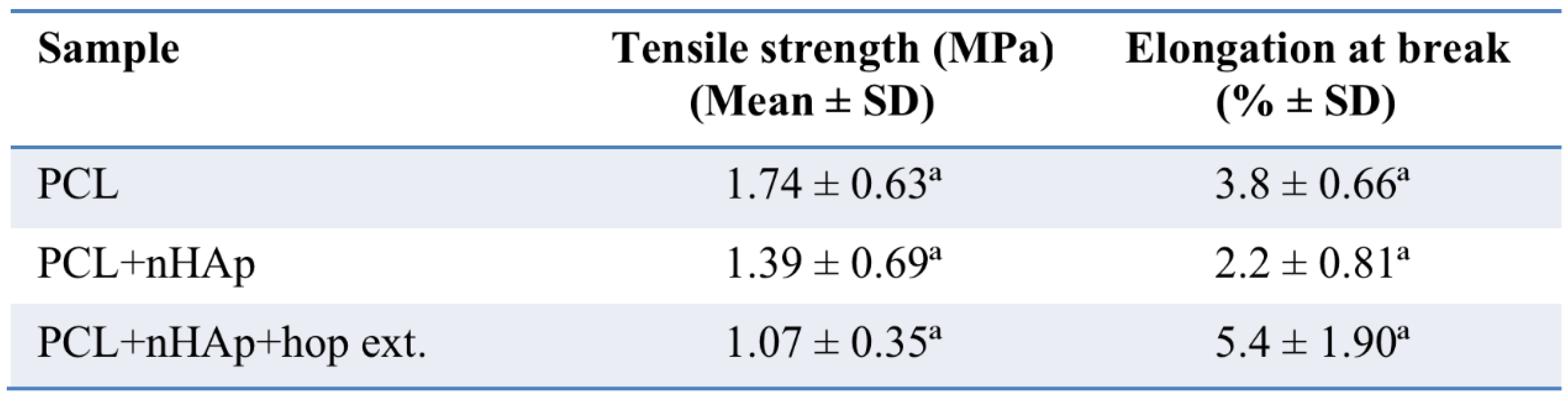
3.5. Mechanical Characterization.
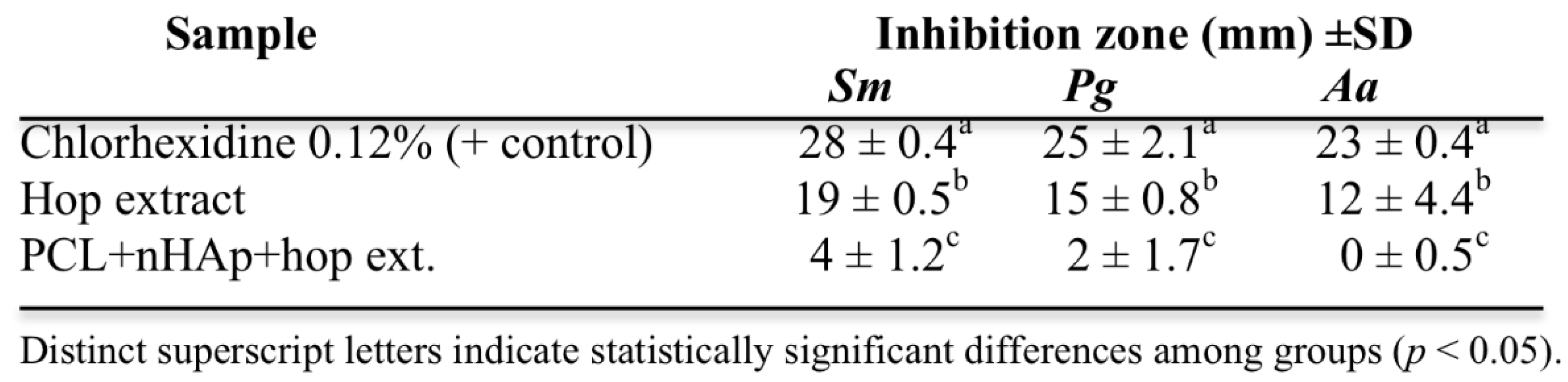
3.6. Antibacterial Assay
Determination of Growth Inhibition Zones
Determination of Growth Inhibition Zones of the Matrices
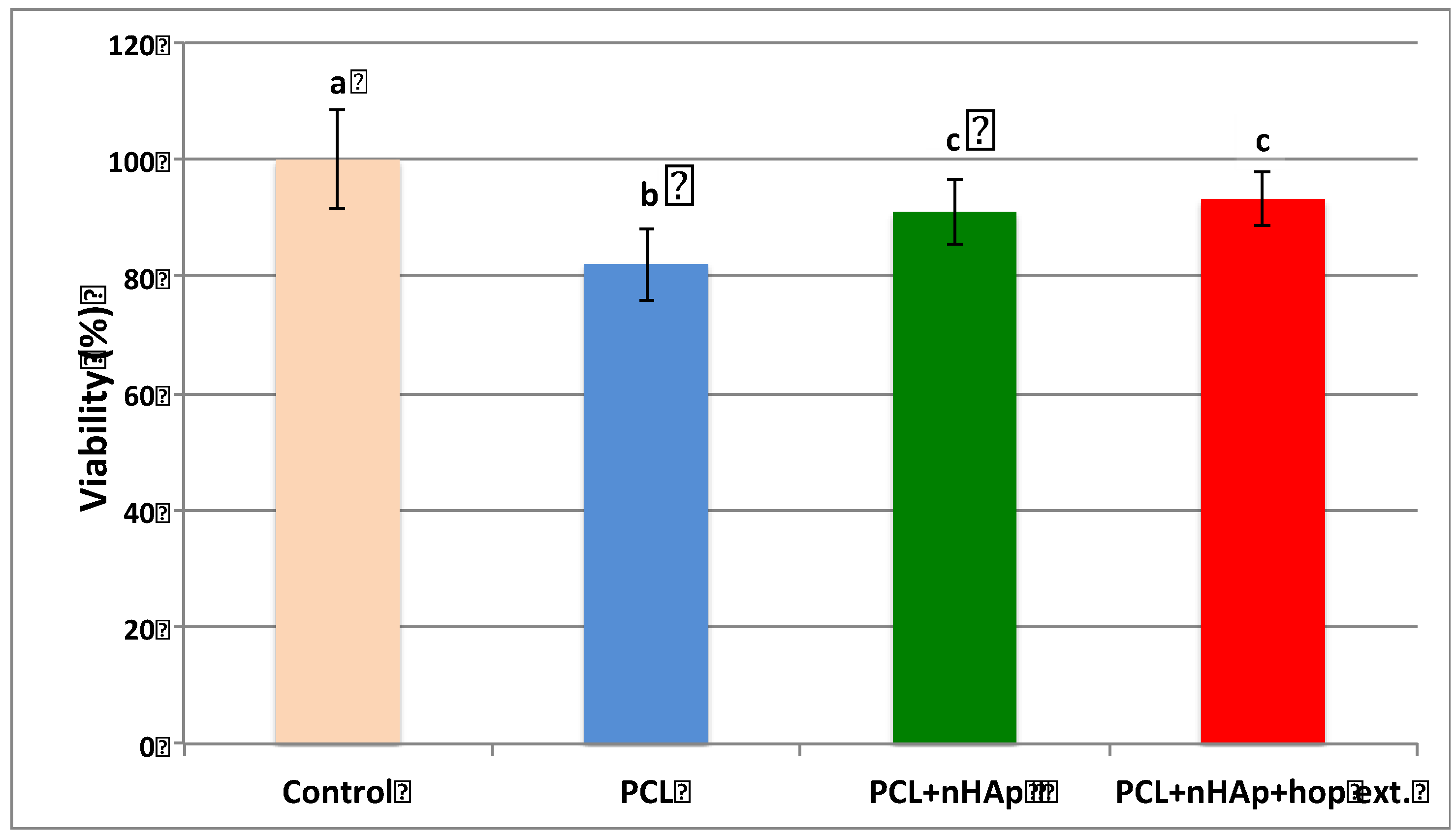
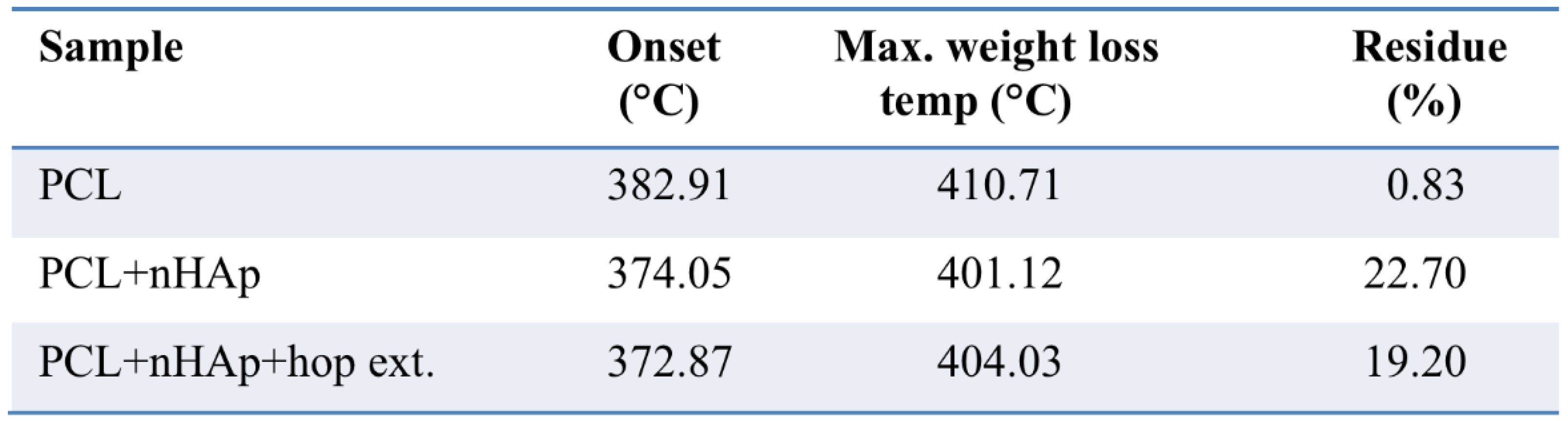
3.7. Cytotoxicity Assay
4. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| FT-IR | Fourier transform infrared spectroscopy |
| Hop | Humulus lupulus L. |
| nHAp | Nano-hydroxyapatite |
| PBS | Phosphate-buffered saline |
| PCL | Poly(ε-caprolactone) |
| SEM | Scanning Electron Microscope |
| TGA | Thermogravimetric Analysis (TGA) |
References
- Khademhosseini, A.; Langer, R. Nanobiotechnology - drug delivery and tissue engineering. Chem. Eng. Prog. 2006, 102, 38−42.
- Carvalho, M.S.; Cabral, J.; da Silva, C.; Vashishth, D. Bone Matrix Non-Collagenous Proteins in Tissue Engineering: Creating New Bone by Mimicking the Extracellular Matrix. Polymers 2021, 13, 1095. [CrossRef]
- Bernard, M.; Jubeli, E.; Pungente, M. D.; Yagoubi, N. Biocompatibility of polymer-based biomaterials and medical devices – regulations, in vitro screening and risk-management. Biomater. Sci. 2018, 6, 2025−2053.
- Kolarijani, N.R.; Cheraghali, D.; Khastar, H.; Ehterami, A.; Alizade, M.; Vaez, A.; Amini, S.M.; Salehi, M. Nanofibrous polycaprolactone/gelatin scaffold containing gold nanoparticles: Physicochemical and biological characterization for wound healing. Wound Repair Regen. 2023, 31, 804–815. [CrossRef]
- Lykins, W.R.; Bernards, D.A.; Schlesinger, E.B.; Wisniewski, K.; Desai, T.A. Tuning polycaprolactone degradation for long acting implantables. Polymer 2022, 262, 125473–125480. [CrossRef]
- Rahimkhoei, V.; Padervand, M.; Hedayat, M.; Seidi, F.; Dawi, E.; Akbari, A. Biomedical applications of electrospun polycaprolactone-based carbohydrate polymers: A review. Int. J. Biol. Macromol. 2023, 253, 126642. [CrossRef]
- Halim, N.A.A.; Hussein, M.Z.; Kandar, M.K. Nanomaterials-Upconverted Hydroxyapatite for Bone Tissue Engineering and a Platform for Drug Delivery. Int. J. Nanomed. 2021, 16, 6477–6496. [CrossRef]
- Munir, M.U.; Salman, S.; Javed, I.; Bukhari, S.N.A.; Ahmad, N.; Shad, N.A.; Aziz, F. Nano-hydroxyapatite as a delivery system: overview and advancements. Artif. Cells, Nanomedicine Biotechnol. 2021, 49, 717–727. [CrossRef]
- Du, M.; Chen, J.; Liu, K.; Xing, H.; Song, C. Recent advances in biomedical engineering of nano-hydroxyapatite including dentistry, cancer treatment and bone repair. Compos. Part B: Eng. 2021, 215. [CrossRef]
- Haider, K.; Kharaghani, D.; Sun, L.; Ullah, S.; Sarwar, M.N.; Ullah, A.; Khatri, M.; Yoshiko, Y.; Gopiraman, M.; Kim, I.S. Synthesized bioactive lignin nanoparticles/polycaprolactone nanofibers: A novel nanobiocomposite for bone tissue engineering. Mater. Sci. Eng. C 2023, 144, 213203. [CrossRef]
- Hussain, Z.; Mehmood, S.; Liu, X.; Liu, Y.; Wang, G.; Pei, R. Decoding bone-inspired and cell-instructive cues of scaffolds for bone tissue engineering. Eng. Regen. 2023, 5, 21–44. [CrossRef]
- Zhao, Y.; Fan, T.; Chen, J.; Su, J.; Zhi, X.; Pan, P.; Zou, L.; Zhang, Q. Magnetic bioinspired micro/nanostructured composite scaffold for bone regeneration. Colloids Surfaces B: Biointerfaces 2019, 174, 70–79. [CrossRef]
- Hoveidaei, A.H.; Sadat-Shojai, M.; Mosalamiaghili, S.; Salarikia, S.R.; Roghani-Shahraki, H.; Ghaderpanah, R.; Ersi, M.H.; Conway, J.D. Nano-hydroxyapatite structures for bone regenerative medicine: Cell-material interaction. Bone 2023, 179, 116956. [CrossRef]
- Awad, H. A.; O’Keefe, R. J.; Mao, J. J. Bone tissue engineering. In: Principles of Tissue Engineering, Elsevier: Oxford, UK, 2020; pp. 1511−1519.
- Slots, J. Periodontitis: facts, fallacies and the future. Periodontology 2000 2017, 75, 7–23. [CrossRef]
- Hamada, S.; Slade, H. D. Biology, immunology, and cariogenicity of Streptococcus mutans. Microbiol. Rev. 1980, 44, 331−384.
- He, M.; Wang, Q.; Xie, L.; Wu, H.; Zhao, W.; Tian, W. Hierarchically multi-functionalized graded membrane with enhanced bone regeneration and self-defensive antibacterial characteristics for guided bone regeneration. Chem. Eng. J. 2020, 398. [CrossRef]
- Li, J.; Lai, Y.; Li, M.; Chen, X.; Zhou, M.; Wang, W.; Li, J.; Cui, W.; Zhang, G.; Wang, K.; et al. Repair of infected bone defect with Clindamycin-Tetrahedral DNA nanostructure Complex-loaded 3D bioprinted hybrid scaffold. Chem. Eng. J. 2022, 435, 134855. [CrossRef]
- Song, M.; Liu, Y.; Li, T.; Liu, X.; Hao, Z.; Ding, S.; Panichayupakaranant, P.; Zhu, K.; Shen, J. Plant Natural Flavonoids Against Multidrug Resistant Pathogens. Adv. Sci. 2021, 8, 2100749. [CrossRef]
- Abiko, Y.; Paudel, D.; Uehara, O. Hops components and oral health. J. Funct. Foods 2022, 92, 105035. [CrossRef]
- González-Salitre, L.; González-Olivares, L.G.; Basilio-Cortes, U.A. Humulus lupulus L. a potential precursor to human health: High hops craft beer. Food Chem. 2023, 405, 134959. [CrossRef]
- Betancur, M.; López, J.; Salazar, F. Antimicrobial activity of compounds from hop (Humulus lupulus L.) following supercritical fluid extraction: An overview. Chil. J. Agric. Res. 2023, 83, 499–509. [CrossRef]
- Khaliullina, A.; Kolesnikova, A.; Khairullina, L.; Morgatskaya, O.; Shakirova, D.; Patov, S.; Nekrasova, P.; Bogachev, M.; Kurkin, V.; Trizna, E.; Kayumov, A. The antimicrobial potential of the hop (Humulus lupulus L.) extract against Staphylococcus aureus and oral Streptococci. Pharmaceuticals. 2024, 17, 162. [CrossRef]
- Bolton, J. L.; Dunlap, T. L.; Hajirahkimkhan, A.; Mbachu, O.; Chen, S.-N.; Chadwick, L.; Nikolic, D.; van Breemen, R. B.; Pauli, G. F.; Dietz, B. M. The multiple biological targets of hops and bioactive compounds. Chem. Res. Toxicol. 2019, 32, 222−233. [CrossRef]
- Hiraki, D.; Uehara, O.; Harada, F.; Takai, R.; Takahasi, S.; Taraya, S.; Abiko, Y. Effect of xanthohumol on Porphyromonas gingivalis. Jpn. J. Conserv. Dent. 2019, 62, 271–278.
- Harish, V.; Haque, E.; Śmiech, M.; Taniguchi, H.; Jamieson, S.; Tewari, D.; Bishayee, A. Xanthohumol for Human Malignancies: Chemistry, Pharmacokinetics and Molecular Targets. Int. J. Mol. Sci. 2021, 22, 4478. [CrossRef]
- Jeong, H.M.; Han, E.H.; Jin, Y.H.; Choi, Y.H.; Lee, K.Y.; Jeong, H.G. Xanthohumol from the hop plant stimulates osteoblast differentiation by RUNX2 activation. Biochem. Biophys. Res. Commun. 2011, 409, 82–89. [CrossRef]
- Hameed, M.M.A.; Khan, S.A.P.M.; Thamer, B.M.; Rajkumar, N.; El-Hamshary, H.; El-Newehy, M. Electrospun nanofibers for drug delivery applications: Methods and mechanism. Polym. Adv. Technol. 2023, 34, 6–23. [CrossRef]
- Liu, H.; Bai, Y.; Huang, C.; Wang, Y.; Ji, Y.; Du, Y.; Xu, L.; Yu, D.-G.; Bligh, S.W.A. Recent Progress of Electrospun Herbal Medicine Nanofibers. Biomolecules 2023, 13, 184. [CrossRef]
- Liu, J.; Zou, Q.; Wang, C.; Lin, M.; Li, Y.; Zhang, R.; Li, Y. Electrospinning and 3D printed hybrid bi-layer scaffold for guided bone regeneration. Mater. Des. 2021, 210, 110047. [CrossRef]
- ISO. Biological evaluation of medical devices - Part 13: Identification and quantification of degradation products from polymeric medical devices; ISO 10993-13; ISO: Geneva, Switzerland 2010.
- Bauer, A. W. Antibiotic susceptibility testing by a standardized single disc method. Am. J. Clin. Pathol. 1966, 45, 149−158.
- ISO. Biological Evaluation of Medical Devices. Part 5: Tests for Cytotoxicity: In Vitro Methods; ISO 10993-5; ISO: Geneva, Switzerland 1993.
- Zhu, P.; Yin, H.; Wei, J.; Wu, J.; Ping, D.; Zhang, X. A bilayer biocompatible polycaprolactone/zinc oxide/Capparis spinosa L. ethyl acetate extract/polylactic acid nanofibrous composite scaffold for novel wound dressing applications. Int. J. Biol. Macromol. 2023, 242, 125093. [CrossRef]
- Irani, M.; Abadi, P.G.; Ahmadian-Attari, M.M.; Rezaee, A.; Kordbacheh, H.; Goleij, P. In vitro and in vivo studies of Dragon's blood plant (D. cinnabari)-loaded electrospun chitosan/PCL nanofibers: Cytotoxicity, antibacterial, and wound healing activities. Int. J. Biol. Macromol. 2024, 257, 128634. [CrossRef]
- Szewczyk, P.K.; Stachewicz, U. The impact of relative humidity on electrospun polymer fibers: From structural changes to fiber morphology. Adv. Colloid Interface Sci. 2020, 286, 102315. [CrossRef]
- Ahmadi Bonakdar; M., Rodrigue, D. Electrospinning: processes, structures, and materials. Macromolecules. 2024, 4, 58−103. [CrossRef]
- Chong, L. H.; Hassan, M. I.; Sultana, N. Electrospun polycaprolactone (PCL) and PCL/nano-hydroxyapatite (PCL/nHA)-based nanofibers for bone tissue engineering application. In: IEEE 10th Asian Control Conference (ASCC), Malaysia, 2015, 1−4.
- Hassan, M.I.; Sultana, N. Characterization, drug loading and antibacterial activity of nanohydroxyapatite/polycaprolactone (nHA/PCL) electrospun membrane. 3 Biotech 2017, 7, 1–9. [CrossRef]
- Fortună, M.E.; Ungureanu, E.; Rotaru, R.; Bargan, A.; Ungureanu, O.C.; Brezuleanu, C.O.; Harabagiu, V. Synthesis and Properties of Modified Biodegradable Polymers Based on Caprolactone. Polymers 2023, 15, 4731. [CrossRef]
- Emadi, H.; Karevan, M.; Rad, M.M.; Sadeghzade, S.; Pahlevanzadeh, F.; Khodaei, M.; Khayatzadeh, S.; Lotfian, S. Bioactive and Biodegradable Polycaprolactone-Based Nanocomposite for Bone Repair Applications. Polymers 2023, 15, 3617. [CrossRef]
- Yu, P.; Huang, S.; Yang, Z.; Liu, T.; Qilin, Z.; Feng, J.; Zeng, B. Biomechanical properties of a customizable TPU/PCL blended esophageal stent fabricated by 3D printing. Mater. Today Commun. 2023, 34, 105196. [CrossRef]
- Su, T.-T.; Jiang, H.; Gong, H. Thermal Stabilities and the Thermal Degradation Kinetics of Poly(ε-Caprolactone). Polym. Technol. Eng. 2008, 47, 398–403. [CrossRef]
- Motloung, M. P.; Mofokeng, T. G.; Ray, S. S. Viscoelastic, thermal, and mechanical properties of melt-processed poly(ε-caprolactone) (PCL)/hydroxyapatite (HAP) composites. Materials. 2021, 15, 104. [CrossRef]
- Dias, D.; Vale, A. C.; Cunha, E. P.; C Paiva, M.; Reis, R. L., Vaquette, C.; Alves, N. M. 3D-printed cryomilled poly(ε-caprolactone)/graphene composite scaffolds for bone tissue regeneration. J. Biomed. Mater. Res. -B: Appl. Biomater. 2021, 109, 961−972. [CrossRef]
- Loyo, C.; Cordoba, A.; Palza, H.; Canales, D.; Melo, F.; Vivanco, J.F.; Baier, R.V.; Millán, C.; Corrales, T.; Zapata, P.A. Effect of Gelatin Coating and GO Incorporation on the Properties and Degradability of Electrospun PCL Scaffolds for Bone Tissue Regeneration. Polymers 2023, 16, 129. [CrossRef]
- Alexeev, D.; Tschopp, M.; Helgason, B.; Ferguson, S. J. Electrospun biodegradable poly(ε-caprolactone) membranes for annulus fibrosus repair: Long-term material stability and mechanical competence. JOR Spine. 2021, 4, e1130. [CrossRef]
- Swetha, S.; Balagangadharan, K.; Lavanya, K.; Selvamurugan, N. Three-dimensional-poly(lactic acid) scaffolds coated with gelatin/magnesium-doped nano-hydroxyapatite for bone tissue engineering. Biotechnol. J. 2021, 16, 2100282. [CrossRef]
- Masek, A.; Chrzescijanska, E.; Kosmalska, A.; Zaborski, M. Characteristics of compounds in hops using cyclic voltammetry, UV–VIS, FTIR and GC–MS analysis. Food Chem. 2014, 156, 353–361. [CrossRef]
- Pawar, R.; Pathan, A.; Nagaraj, S.; Kapare, H.; Giram, P.; Wavhale, R. Polycaprolactone and its derivatives for drug delivery. Polym. Adv. Technol. 2023, 34, 3296–3316. [CrossRef]
- Yaseri, R.; Fadaie, M.; Mirzaei, E.; Samadian, H.; Ebrahiminezhad, A. Surface modification of polycaprolactone nanofibers through hydrolysis and aminolysis: a comparative study on structural characteristics, mechanical properties, and cellular performance. Sci. Rep. 2023, 13, 1–17. [CrossRef]
- Alharbi, N.; Daraei, A.; Lee, H.; Guthold, M. The effect of molecular weight and fiber diameter on the mechanical properties of single, electrospun PCL nanofibers. Mater. Today Commun. 2023, 35, 105773. [CrossRef]
- Fu, S. Y.; Feng, X. Q.; Lauke, B.; Mai, Y. W. Effects of particle size, particle/matrix interface adhesion and particle loading on mechanical properties of particulate–polymer composites. Composites Part B: Eng. 2008, 39, 933−961. [CrossRef]
- Croisier, F.; Duwez, A.-S.; Jérôme, C.; Léonard, A.F.; van der Werf, K.O.; Dijkstra, P.J.; Bennink, M.L. Mechanical testing of electrospun PCL fibers. Acta Biomater. 2012, 8, 218–224. [CrossRef]
- Alharbi, N.; Daraei, A.; Lee, H.; Guthold, M. The effect of molecular weight and fiber diameter on the mechanical properties of single, electrospun PCL nanofibers. Mater. Today Commun. 2023, 35, 105773. [CrossRef]
- Modiri-Delshad, T.; Ramazani, A.; Khoobi, M.; Javar, H.A.; Akbari, T.; Amin, M. Fabrication of chitosan/polycaprolactone/Myrtus communis L. extract nanofibrous mats with enhanced antibacterial activities. Polym. Polym. Compos. 2023, 31, 09673911231151506. [CrossRef]
- Moraczewski, K.; Stepczyńska, M.; Malinowski, R.; Karasiewicz, T.; Jagodziński, B.; Rytlewski, P. Modification of Polycaprolactone with Plant Extracts to Improve the Aging Resistance. Materials 2023, 16, 5154. [CrossRef]
- Rad, Z.P.; Mokhtari, J.; Abbasi, M. Preparation and characterization of Calendula officinalis-loaded PCL/gum arabic nanocomposite scaffolds for wound healing applications. Iran. Polym. J. 2019, 28, 51–63. [CrossRef]
- Bhattacharya, S.; Virani, S.; Zavro, M.; Haas, G.J. Inhibition of Streptococcus Mutans and Other Oral Streptococci by Hop (Humulus Lupulus L.) Constituents. Econ. Bot. 2003, 57, 118–125. [CrossRef]
- Haas, G.J.; Barsoumian, R. Antimicrobial Activity of Hop Resins. J. Food Prot. 1994, 57, 59–61. [CrossRef]
- Teuber, M. Low antibiotic potency of isohumulone. Appl. Microbiol. 1970, 19, 871.
- Klimek, K.; Tyśkiewicz, K.; Miazga-Karska, M.; Dębczak, A.; Rój, E.; Ginalska, G. Bioactive Compounds Obtained from Polish “Marynka” Hop Variety Using Efficient Two-Step Supercritical Fluid Extraction and Comparison of Their Antibacterial, Cytotoxic, and Anti-Proliferative Activities In Vitro. Molecules 2021, 26, 2366. [CrossRef]
- Gregory, E.R.; Bakhaider, R.F.; Gomez, G.F.; Huang, R.; Moser, E.A.S.; Gregory, R.L. Evaluating hop extract concentrations found in commercial beer to inhibit Streptococcus mutans biofilm formation. J. Appl. Microbiol. 2022, 133, 1333–1340. [CrossRef]
- Stompor, M.; Żarowska, B. Antimicrobial Activity of Xanthohumol and Its Selected Structural Analogues. Molecules 2016, 21, 608. [CrossRef]
- Inaba, H.; Tagashira, M.; Kanda, T.; Ohno, T.; Kawai, S.; Amano, A. Apple- and Hop-Polyphenols Protect Periodontal Ligament Cells Stimulated With Enamel Matrix Derivative From Porphyromonas gingivalis. J. Periodontol. 2005, 76, 2223–2229. [CrossRef]
- Shinada, K.; Tagashira, M.; Watanabe, H.; Sopapornamorn, P.; Kanayama, A.; Kanda, T.; Ikeda, M.; Kawaguchi, Y. Hop bract polyphenols reduced three-day dental plaque regrowth.. J. Dent. Res. 2007, 86, 848–851. [CrossRef]
- DeSimone, E.; Aigner, T.B.; Humenik, M.; Lang, G.; Scheibel, T. Aqueous electrospinning of recombinant spider silk proteins. Mater. Sci. Eng. C 2020, 106, 110145. [CrossRef]
- Dalton, P.D.; Klinkhammer, K.; Salber, J.; Klee, D.; Möller, M. Direct in Vitro Electrospinning with Polymer Melts. Biomacromolecules 2006, 13, 686–690. [CrossRef]
- Lim, M.M.; Sun, T.; Sultana, N. In VitroBiological Evaluation of Electrospun Polycaprolactone/Gelatine Nanofibrous Scaffold for Tissue Engineering. J. Nanomater. 2015, 16, 416. [CrossRef]
- Safaeijavan, R.; Soleimani, M.; Divsalar, A.; Eidi, A.; Ardeshirylajimi, A. Biological behavior study of gelatin coated PCL nanofiberous electrospun scaffolds using fibroblasts. J. Paramed. Sci. 2014, 5.
- Philips, N.; Samuel, P.; Lozano, T.; Gvaladze, A.; Guzman, B.; Siomyk, H.; Haas, G. Effects of Humulus lupulus extract or its Components on Viability, Lipid Peroxidation, and expression of Vascular Endothelial Growth Factor in Melanoma Cells and Fibroblasts. Madridge J. Clin. Res. 2017, 1, 15–19. [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





