Submitted:
23 January 2024
Posted:
24 January 2024
You are already at the latest version
Abstract
Keywords:
Introduction
Materials and Methods
Statistical analysis
Results
30. -day outcomes of simultaneous and staged CABG and CEA.
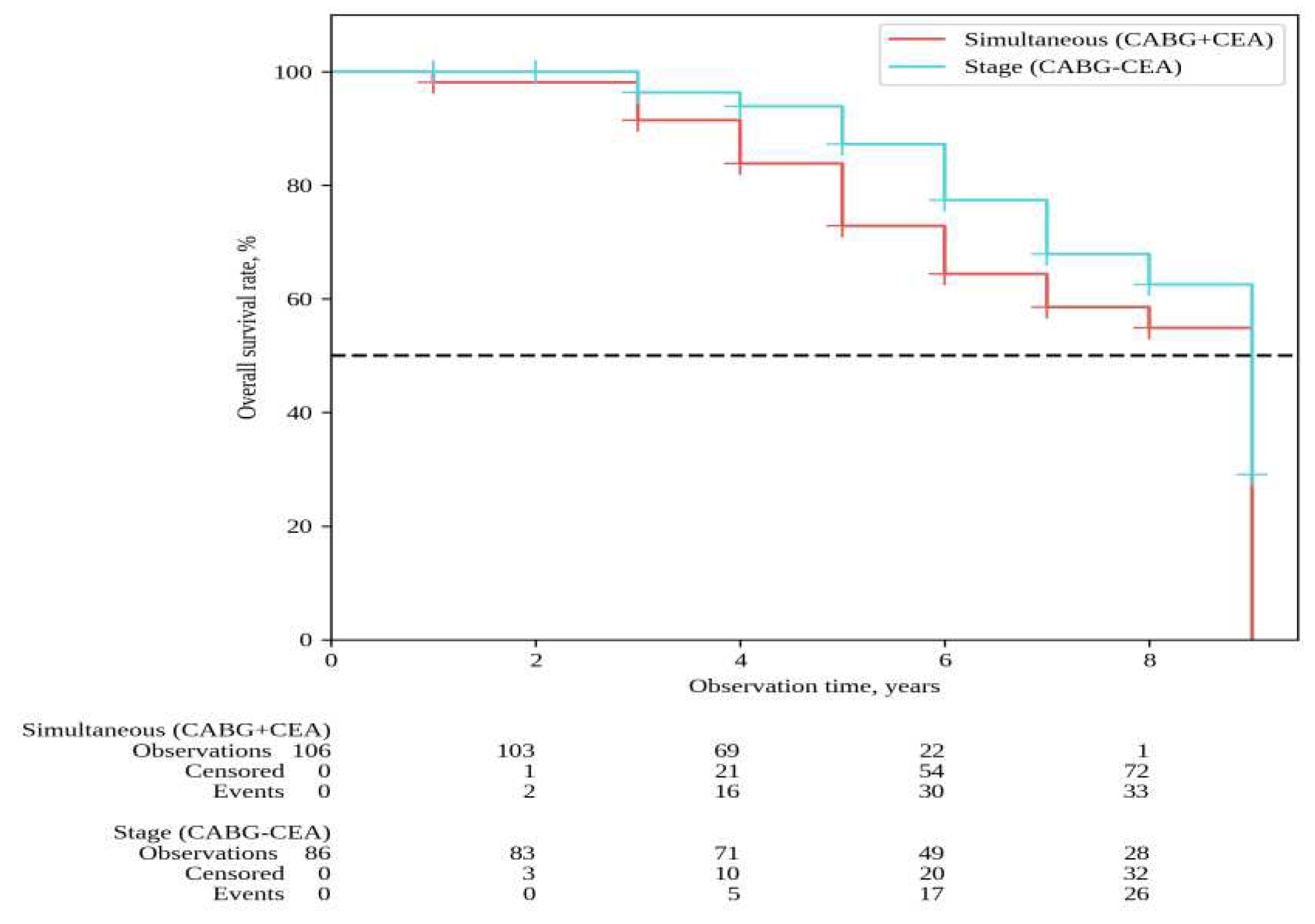
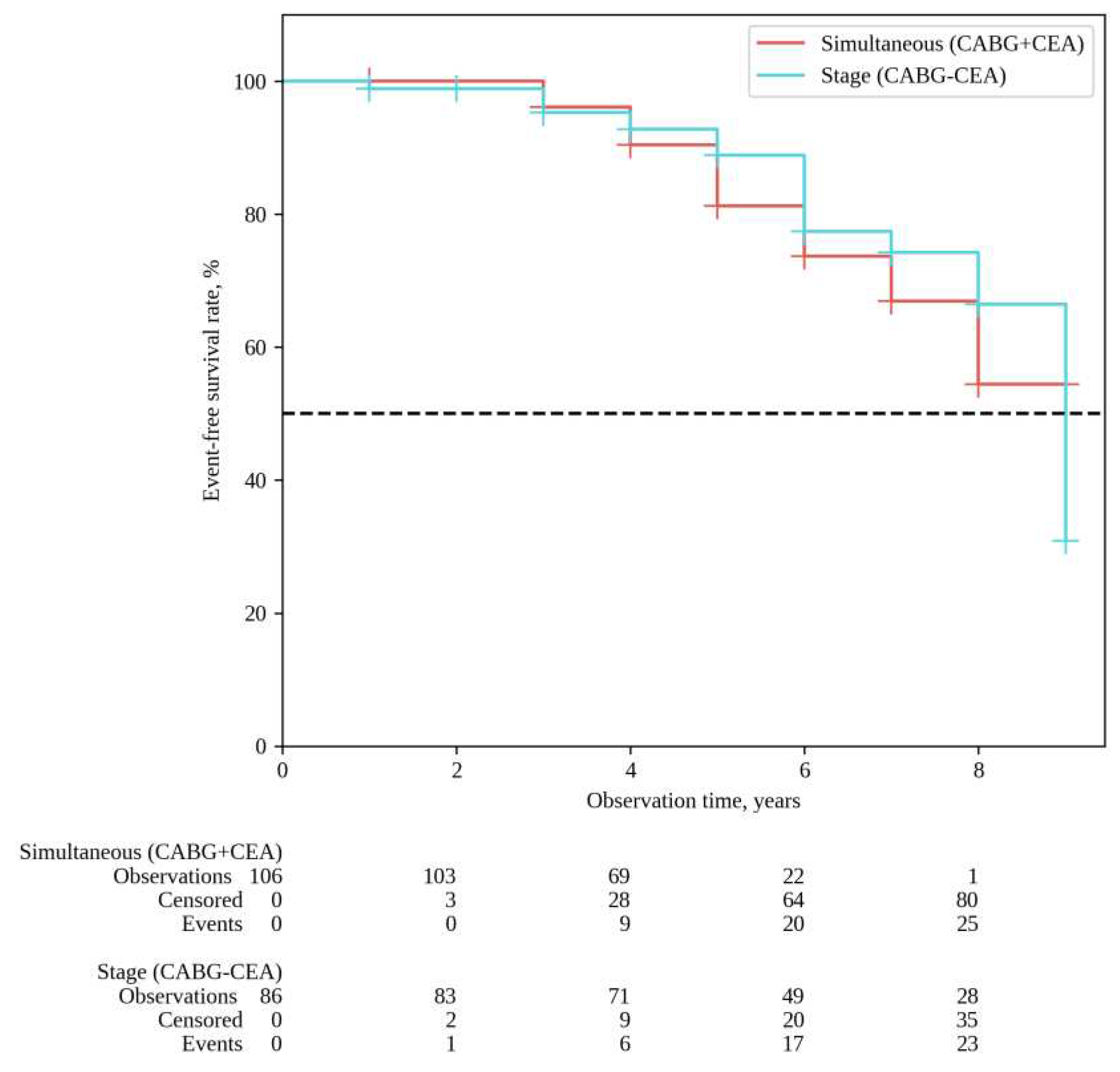
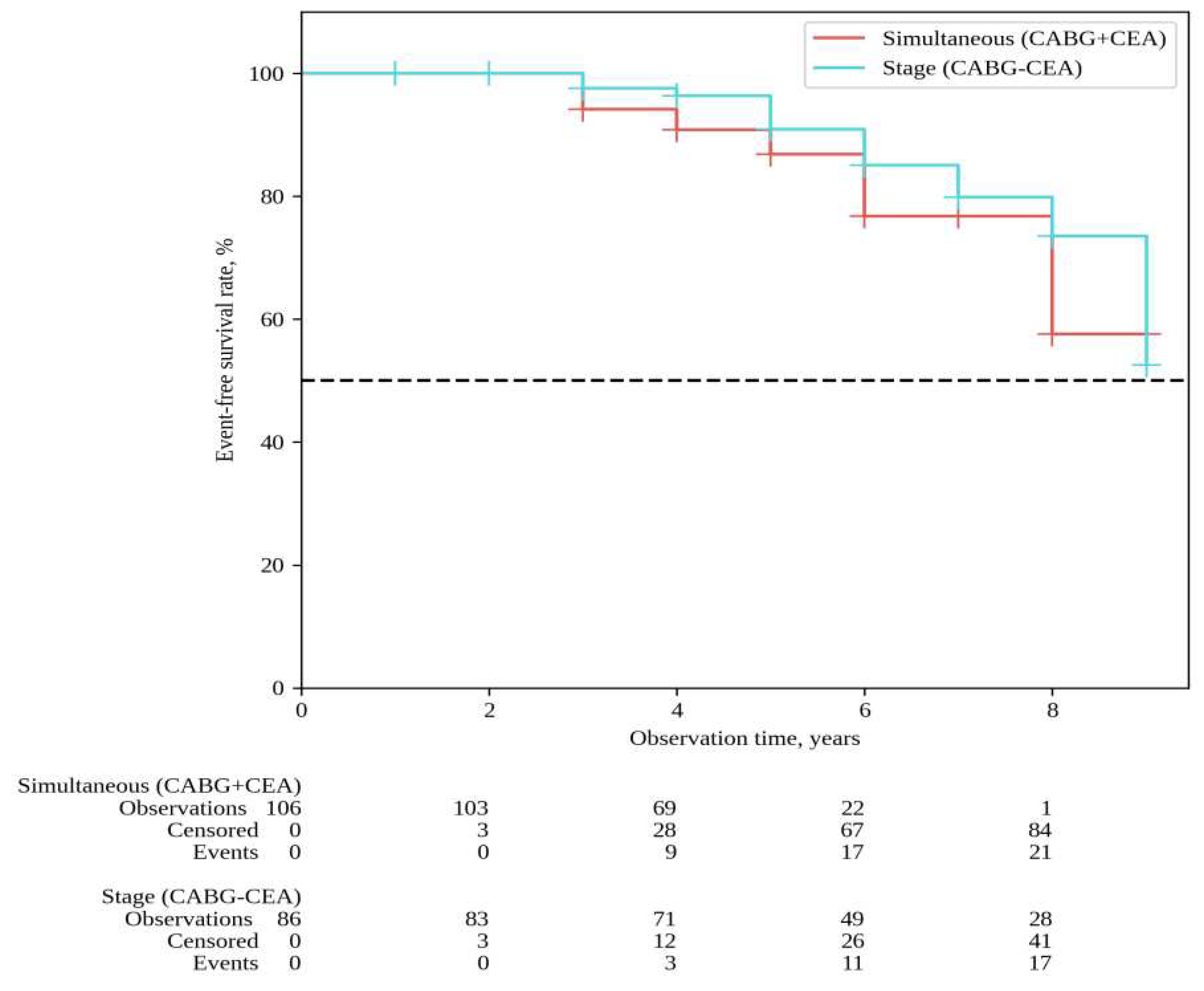
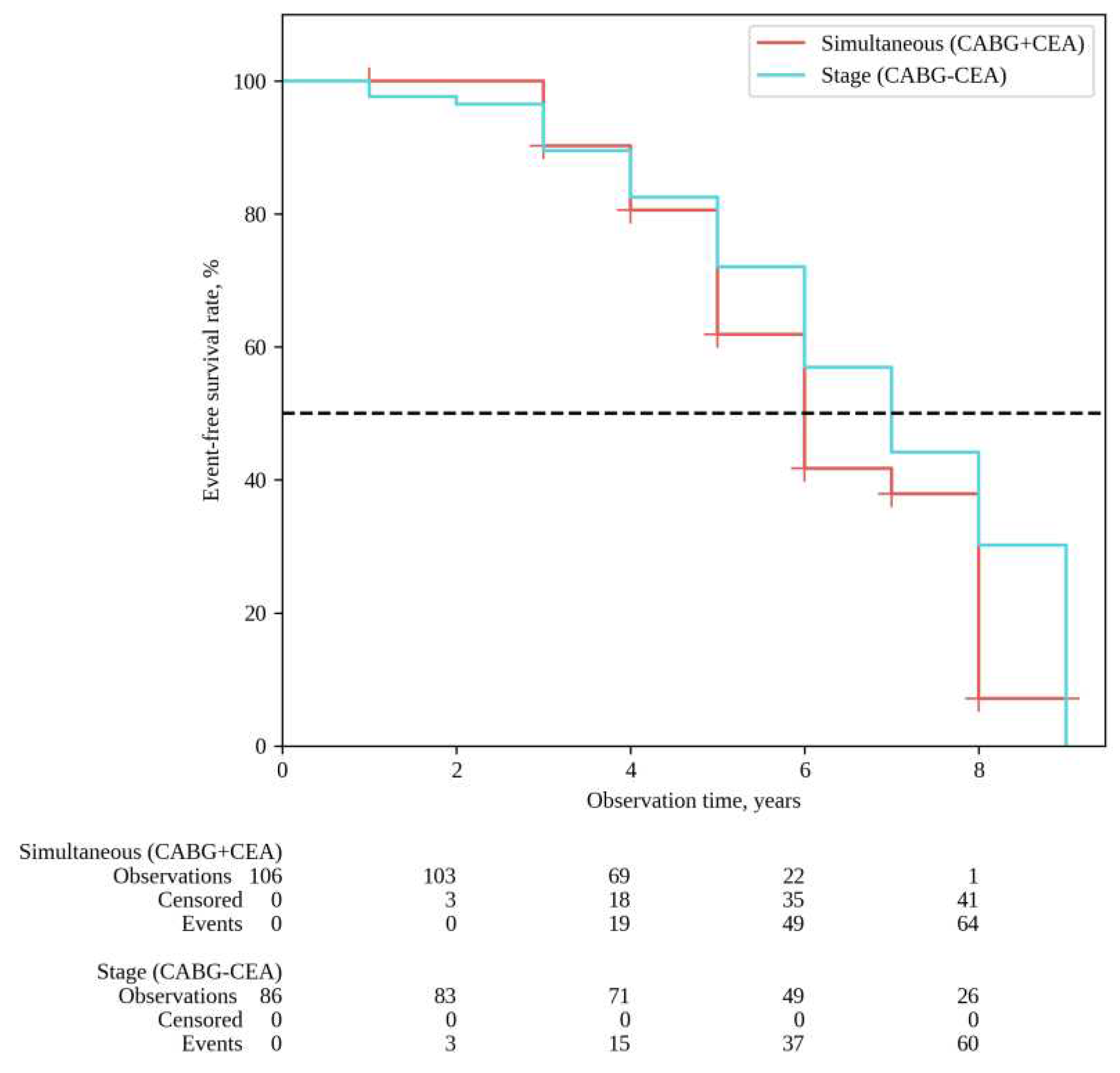
Long-term results
Discussion
Conclusions
References
- Aboyans V, Ricco JB, Bartelink MEL, et al. 2017 ESC Guidelines on the Diagnosis and Treatment of Peripheral Arterial Diseases, in collaboration with the European Society for Vascular Surgery (ESVS): Document covering atherosclerotic disease of extracranial carotid and vertebral, mesenteric, renal, upper and lower extremity arteriesEndorsed by: the European Stroke Organization (ESO)The Task Force for the Diagnosis and Treatment of Peripheral Arterial Diseases of the European Society of Cardiology (ESC) and of the European Society for Vascular Surgery (ESVS). Eur Heart J. 2018;39(9):763-816. [CrossRef]
- Naylor AR, Mehta Z, Rothwell PM, Bell PR. Carotid artery disease and stroke during coronary artery bypass: a critical review of the literature. Eur J Vasc Endovasc Surg. 2002;23(4):283-294. [CrossRef]
- Haywood NS, Ratcliffe SJ, Zheng X, et al. Operative and long-term outcomes of combined and staged carotid endarterectomy and coronary bypass. J Vasc Surg. 2023;77(5):1424-1433.e1. [CrossRef]
- Gopaldas RR, Chu D, Dao TK, et al. Staged versus synchronous carotid endarterectomy and coronary artery bypass grafting: analysis of 10-year nationwide outcomes. Ann Thorac Surg. 2011;91(5):1323-1329. [CrossRef]
- Tzoumas A, Giannopoulos S, Texakalidis P, Charisis N, Machinis T, Koullias GJ. Synchronous versus Staged Carotid Endarterectomy and Coronary Artery Bypass Graft for Patients with Concomitant Severe Coronary and Carotid Artery Stenosis: A Systematic Review and Meta-analysis. Ann Vasc Surg. 2020;63:427-438.e1. [CrossRef]
- Chan JSK, Shafi AMA, Grafton-Clarke C, Singh S, Harky A. Concomitant severe carotid and coronary artery diseases: a separate management or concomitant approach. J Card Surg. 2019;34(9):803-813. [CrossRef]
- Naylor R, Rantner B, Ancetti S, et al. Editor's Choice - European Society for Vascular Surgery (ESVS) 2023 Clinical Practice Guidelines on the Management of Atherosclerotic Carotid and Vertebral Artery Disease. Eur J Vasc Endovasc Surg. 2023;65(1):7-111. [CrossRef]
- Lang RM, Badano LP, Mor-Avi V, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2015;28(1):1-39.e14. [CrossRef]
- Nedkoff L, Briffa T, Zemedikun D, Herrington S, Wright FL. Global Trends in Atherosclerotic Cardiovascular Disease. Clin Ther. 2023;45(11):1087-1091. [CrossRef]
- Zivkovic I, Vukovic P, Milacic P, et al. Midterm Results After Simultaneous Carotid Artery Stenting and Cardiac Surgery. Ann Thorac Surg. 2020;110(5):1557-1563. [CrossRef]
- Doenst T, Sigusch H. Surgical collateralization: The hidden mechanism for improving prognosis in chronic coronary syndromes. J Thorac Cardiovasc Surg. 2022;163(2):703-708.e2. [CrossRef]
- Newman MF, Mathew JP, Grocott HP, et al. Central nervous system injury associated with cardiac surgery. Lancet. 2006;368(9536):694-703. [CrossRef]
- Hood R, Budd A, Sorond FA, Hogue CW. Peri-operative neurological complications. Anaesthesia. 2018;73 Suppl 1:67-75. [CrossRef]
- Roger VL, Go AS, Lloyd-Jones DM, et al. Heart disease and stroke statistics--2011 update: a report from the American Heart Association [published correction appears in Circulation. 2011 Feb 15;123(6):e240] [published correction appears in Circulation. 2011 Oct 18;124(16):e426]. Circulation. 2011;123(4):e18-e209. [CrossRef]
- Neumann FJ, Sousa-Uva M, Ahlsson A, et al. 2018 ESC/EACTS Guidelines on myocardial revascularization [published correction appears in Eur Heart J. 2019 Oct 1;40(37):3096]. Eur Heart J. 2019;40(2):87-165. [CrossRef]
- Wang LJ, Ergul EA, Mohebali J, et al. The effect of combining coronary bypass with carotid endarterectomy in patients with unrevascularized severe coronary disease. J Vasc Surg. 2019;70(3):815-823. [CrossRef]
- Illuminati G, Ricco JB, Caliò F, et al. Short-term results of a randomized trial examining timing of carotid endarterectomy in patients with severe asymptomatic unilateral carotid stenosis undergoing coronary artery bypass grafting. J Vasc Surg. 2011;54(4):993-999. [CrossRef]
- Fareed KR, Rothwell PM, Mehta Z, Naylor AR. Synchronous carotid endarterectomy and off-pump coronary bypass: an updated, systematic review of early outcomes. Eur J Vasc Endovasc Surg. 2009;37(4):375-378. [CrossRef]
- Sharma V, Deo SV, Park SJ, Joyce LD. Meta-analysis of staged versus combined carotid endarterectomy and coronary artery bypass grafting. Ann Thorac Surg. 2014;97(1):102-109. [CrossRef]
- Peng C, Yang YF, Zhao Y, Yang XY. Staged Versus Synchronous Carotid Endarterectomy and Coronary Artery Bypass Grafting: A Meta-Analysis and Systematic Review. Ann Vasc Surg. 2022;86:428-439. [CrossRef]
- Naylor AR, Cuffe RL, Rothwell PM, Bell PR. A systematic review of outcomes following staged and synchronous carotid endarterectomy and coronary artery bypass. Eur J Vasc Endovasc Surg. 2003;25(5):380-389. [CrossRef]
- Blecha M, DeJong M, Carlson K. Risk factors for mortality within 5 years of carotid endarterectomy for asymptomatic stenosis. J Vasc Surg. 2022;75(6):1945-1957. [CrossRef]
- Halliday A, Bulbulia R, Bonati LH, et al. Second asymptomatic carotid surgery trial (ACST-2): a randomised comparison of carotid artery stenting versus carotid endarterectomy. Lancet. 2021;398(10305):1065-1073. [CrossRef]
- Brassington K, Selemidis S, Bozinovski S, Vlahos R. Chronic obstructive pulmonary disease and atherosclerosis: common mechanisms and novel therapeutics. Clin Sci (Lond). 2022;136(6):405-423. [CrossRef]
- Kristensen SD, Knuuti J, Saraste A, et al. 2014 ESC/ESA Guidelines on non-cardiac surgery: cardiovascular assessment and management: The Joint Task Force on non-cardiac surgery: cardiovascular assessment and management of the European Society of Cardiology (ESC) and the European Society of Anaesthesiology (ESA). Eur J Anaesthesiol. 2014;31(10):517-573. [CrossRef]
- Bonaca MP, Bhatt DL, Storey RF, et al. Ticagrelor for Prevention of Ischemic Events After Myocardial Infarction in Patients With Peripheral Artery Disease. J Am Coll Cardiol. 2016;67(23):2719-2728. [CrossRef]
- Elbaz-Greener G, Rozen G, Carasso S, et al. The Relationship Between Body Mass Index and In-Hospital Mortality in Patients Following Coronary Artery Bypass Grafting Surgery. Front Cardiovasc Med. 2021;8:754934. Published 2021 Oct 8. [CrossRef]
- Oz K, Aydın Ü, Kyaruzi M, et al. Staged or Combined Approach for Carotid Endarterectomy in Patients Undergoing Coronary Artery Bypass Grafting: A 5-Year-Long Experience. Heart Surg Forum. 2016;19(6):E276-E281. Published 2016 Dec 7. [CrossRef]
- Kawashima H, Serruys PW, Ono M, et al. Impact of Optimal Medical Therapy on 10-Year Mortality After Coronary Revascularization. J Am Coll Cardiol. 2021;78(1):27-38. [CrossRef]
| Variables | 1 Group | 2 Group | P-value | ||
|---|---|---|---|---|---|
| CABG + CEA (n=106) |
CABG/CEA (n=86) |
||||
| Anthropometric data | |||||
| Gender, n (%) | M–90 (84.9) F–16 (15.1) |
M–66 (76.7) F–20 (23.3) |
0.150 | ||
| Age, years, Ме [IQR] | 64 [60-69] | 66 [61-69] | 0.115 | ||
| BMI, kg/m2, Ме [M ± SD] | 28.20 ± 3.68 | 29.35 ± 4.09 | 0.041* | ||
| Clinical and anamnestic data, risk factors, comorbidity | |||||
| III-IV angina (CCS), n (%) | 91 (85.8) 15 (14.2) |
78 (90.7) 8 (9.3) |
0.304 | ||
| Previous MI, n (%) | 44 (41.5) | 36 (41.9) | 0.961 | ||
| Previous Stroke, n (%) | 21 (19.8) | 17 (19.8) | 0.994 | ||
| Hypertension, n (%) | 106 (100) | 84 (97.7) | 0.199 | ||
| Smoking, n (%) | 46 (43.4) | 20 (23.3) | 0.003* | ||
| CKD, n (%) | 24 (24.4) | 16 (18.6) | 0.493 | ||
| Diabetes, n (%) | 22 (20.8) | 28 (32.6) | 0.064 | ||
| COPD, n (%) | 10 (9.5) | 2 (2.3) | 0.069 | ||
| Diagnostic data | |||||
| LV EF, %, Ме [IQR] | 55 [52–55] | 55 [51–56] | 0.090 | ||
| One-vessel disease, n (%) | 5 (4.7) | 2 (2.3) | 0.463 | ||
| Two-vessel disease, n (%) | 24 (22.6) | 15 (17.4) | 0.373 | ||
| Three-vessel disease, n (%) | 77 (72.6) | 68 (79.1) | 0.303 | ||
| LCA trunk disease >50%, n (%) | 40 (38.1) | 25 (29.4) | 0.207 | ||
| Target CA stenosis, %, Ме [IQR] | 77 [70–90] | 77 [70–87] | 0.387 | ||
| Linear blood flow rate in target CA, cm/s, Ме [IQR] | 247 [187–279] | 246 [208–291] | 0.848 | ||
| Bilateral CA stenosis >70%, n (%) | 10 (9.4) | 8 (9.3) | 1.0 | ||
| Stenosis of the renal arteries>70%, n (%) | 2 (1.9) | 0 | 0.503 | ||
| Lower extremity artery stenosis >70%, n (%) | 9 (8.5) | 6 (6.9) | 0.791 | ||
| Interventions data | |||||
| CABG off-pump, n (%) | 32 (30.2) | 26 (30.2) | 0.995 |
||
| CABG CPB, n (%) | 74 (69.8) | 60 (69.8) | |||
| LITA to the LAD, n (%) | 83 (78.3) | 76 (88.4) | 0.066 | ||
| CPB time, min, [M ± SD] | 70.3±12.4 | 72.4±11.9 | 0.788 | ||
| Eversion CEA, n (%) | 65 (61.3) | 49 (57.0) | 0.542 | ||
| CEA with a synthetic patch angioplasty, n (%) | 41 (38.7) | 37 (43.0) | |||
| CEA from the left CA, n (%) | 59 (55.7) | 44 (51.2) | 0.534 | ||
| CEA from the right CA, n (%) | 47 (44.3) | 42 (48.8) | |||
| * – differences in indicators are statistically significant (p<0.05) CABG - coronary artery bypass grafting, CEA - Carotid endarterectomy, BMI - body mass index, CCS - Canadian Cardiovascular Society, MI - myocardial infarction, AF - atrial fibrillation, CKD - chronic kidney disease, GFR - glomerular filtration rate, COPD - chronic obstructive pulmonary disease, LV EF - left ventricular ejection fraction, LCA - left coronary artery, CA - carotid artery, CPB - cardiopulmonary bypass, LITA - left internal thoracic artery, LAD - left anterior descending artery. | |||||
| Complications | 1 Group | 2 Group |
OR |
95% CI |
Р-value |
|---|---|---|---|---|---|
| CABG + CEA (n=106) | CABG/CEA (n=86) | ||||
| Structure complications | |||||
| Death, n (%) | 3 (2.8) | 2 (2.3) | 1.233 | 0.133-5.006 | 1.0 |
| Non-fatal MI, n (%) | 0 | 2 (2.3) | 6.302 | 0.299- 133.032 | 0.199 |
| Non-fatal stroke, n (%) | 3 (2.8) | 1 (1.2) | 2.476 | 0.041-3.954 | 0.629 |
| MACE, n (%) | 6 (5.7) | 5 (5.8) | 1.029 | 0.303-3.493 | 1.0 |
| Brain swelling, n (%) | 2 (1.9) | 0 | 4.139 | 0.011-5.100 | 0.503 |
| GI bleed, n (%) | 1 (0.9) | 0 | 2.406 | 0.016-10.106 | 1.0 |
| Respiratory failure, n (%) | 2 (1.9) | 1 (1.2) | 1.635 | 0.055-6.863 | 1.0 |
| Heart rhythm disorders, n (%) | 8 (7.5) | 4 (4.7) | 1.673 | 0.174-2.056 | 0.553 |
| Acute heart failure, n (%) | 2 (1.9) | 2 (2.3) | 1.238 | 0.171-8.976 | 1.0 |
| Multiple organ failure, n (%) | 2 (1.9) | 2 (2.3) | 1.238 | 0.171-8.976 | 1.0 |
| Duration of mechanical ventilation, h, Ме [IQR] | 15.5 [10,0-18.1] | 11.5 [8,0-16.2] | 0.004* | ||
| Rethoracotomy for bleeding, n (%) | 7 (6.6) | 6 (7.0) | 1.061 | 0.343-3.282 | 1.0 |
| Infectious complications, n (%) | 7 (6.6) | 2 (2.3) | 2.970 | 0.068-1.665 | 0.191 |
| Risk of complications | |||||
| Number of patients with 1 or more any postoperative complication, n (%) | 28 (26.4) | 12 (14.0) | 2.214 | 1.048-4.674 | 0.035* |
| * – differences in indicators are statistically significant (p<0.05) CABG - coronary artery bypass grafting, CEA - carotid endarterectomy, MI - myocardial infarction, MACE – major adverse cardiac events, GI - gastrointestinal tract | |||||
|
Risk factors |
Univariate analysis | Multivariate analysis | ||
|---|---|---|---|---|
| OR (95% CI) | Р-value | OR (95% CI) | Р-value | |
| Age per 1 y | 1.16 (0.05-1.28) | 0.004* | 1.15 (1.03-1.27) | 0.01* |
| Female | 1.68 (0.42-6.68) | 0.460 | - | - |
| BMI per 1 kg\m2 | 0.81 (0.66–0.97) | 0.023* | 0.81 (0.66-1.01) | 0.057 |
| Smoking | 1.64 (0.48-5.58) | 0.429 | - | - |
| Previous Stroke | 2.47 (0.68-8.92) | 0.167 | - | - |
| Previous MI | 2.59 (0.73-9.16) | 0.140 | ||
| Bilateral CA stenosis | 0.96 (0.12-8.00) | 0.973 | - | - |
| LV EF | 0.94 (0.71-1.64) | 0.647 | - | - |
| Three-vessel disease | 3.41 (0.42-27.35) | 0.249 | - | - |
| LCA trunk disease >50% | 0.42 (0.09-1.99) | 0.272 | - | - |
| Lower extremity artery stenosis | 1.19 (0.14-10.00) | 0.871 | - | - |
| Diabetes | 1.07 (0.27-4.20) | 0.924 | - | - |
| CKD | 0.36 (0.04-2.93) | 0.342 | - | - |
| COPD | 3.80 (0.72-19.98) | 0.115 | - | - |
| CABG CPB | 1.16 (0.30-4.55) | 0.827 | - | - |
| Stage | 1.03 (0.31-3.49) | 0.964 | - | - |
| * – differences in indicators are statistically significant (p<0.05) MACE – major adverse cardiac events, BMI - body mass index, MI – myocardial infarction, CA - carotid artery, LV EF - left ventricular ejection fraction, LCA - left coronary artery , CKD - chronic kidney disease, COPD - chronic obstructive pulmonary disease, CABG - coronary artery bypass grafting, CPB - cardiopulmonary bypass. | ||||
|
Risk factors |
Univariate analysis | Multivariate analysis | ||
|---|---|---|---|---|
| HR (95% CI) | Р-value | HR (95% CI) | Р-value | |
| Age per 1 y | 1.01 (0.97-1.04) | 0.850 | - | - |
| BMI per increase 1 kg\m² | 0.92 (0.86–0.99) | 0.035* | 0.93 (0.85-0.99) | 0.036* |
| Smoking | 1.87 (1.10 – 3.18) | 0.021* | - | - |
| Female | 1.47 (0.82 – 2.64) | 0.198 | - | - |
| Previous Stroke | 1.34 (0.72-2.49) | 0.348 | - | - |
| Previous MI | 1.01 (0.56-1.68) | 0.988 | - | - |
| Bilateral CA stenosis | 1.01 (0.43-2.35) | 0.979 | - | - |
| LV EF | 1.03 (0.91-1.17) | 0.621 | - | - |
| Three-vessel disease | 0.53 (0.31-0.98) | 0.063 | - | - |
| LCA trunk disease >50% | 1.34 (0.79-2.28) | 0.282 | - | - |
| Lower extremity artery stenosis | 0.85 (0.31-2.35) | 0.758 | - | - |
| Diabetes | 0.84 (0.48-1.50) | 0.566 | - | - |
| CKD | 1.34 (0.73 – 2.44) | 0.341 | - | - |
| COPD | 1.56 (0.62-3.91) | 0.341 | - | - |
| CABG CPB | 1.47 (0.83-2.62) | 0.186 | - | - |
| Stage | 0.62 (0.37 – 1.04) | 0.069 | - | - |
| * – differences in indicators are statistically significant (p<0.05) MACE – major adverse cardiac events, BMI - body mass index, MI – myocardial infarction, CA - carotid artery, LV EF - left ventricular ejection fraction, LCA - left coronary artery, CKD - chronic kidney disease, COPD - chronic obstructive pulmonary disease, CABG - coronary artery bypass grafting, CPB - cardiopulmonary bypass. | ||||
|
Risk factors |
Univariate analysis | Multivariate analysis | ||
|---|---|---|---|---|
| HR (95% CI) | Р-value | HR (95% CI) | Р-value | |
| Age per 1 y | 1.01 (0.98-1.03) | 0.814 | - | - |
| Female | 1.14 (0.76 – 1.70) | 0.523 | - | - |
| BMI per 1 kg/m² | 0.95 (0.91–0.99) | 0.042* | 0.96 (0.92-1.01) | 0.080 |
| Smoking | 1.44 (1.01 – 2.04) | 0.043* | 1.36 (0.95-1.94) | 0.09 |
| Previous Stroke | 1.12 (0.74-1.70) | 0.583 | - | - |
| Previous MI | 0.92 (0.66-1.29) | 0.629 | ||
| Bilateral CA stenosis | 0.96 (0.55-1.67) | 0.896 | - | - |
| LV EF | 0.94 (0.87-1.02) | 0.135 | - | - |
| Three-vessel disease | 0.76 (0.52-1.12) | 0.164 | - | - |
| LCA trunk disease >50% | 1.19 (0.84-1.68) | 0.331 | - | - |
| Lower extremity artery stenosis | 1.08 (0.60-1.95) | 0.803 | - | - |
| Diabetes | 0.82 (0.57-1.19) | 0.820 | - | - |
| CKD | 1.35 (0.92 – 1.97) | 0.124 | - | - |
| COPD | 1.40 (0.76-2.59) | 0.283 | - | - |
| CABG CPB | 1.64 (1.12-2.28) | 0.082 | - | - |
| Stage | 0.715 (0.50 –1.01) | 0.060 | - | - |
| * – differences in indicators are statistically significant (p<0.05) MACE – major adverse cardiac events, BMI - body mass index, MI – myocardial infarction, CA - carotid artery, LV EF - left ventricular ejection fraction, LCA - left coronary artery, CKD - chronic kidney disease, COPD - chronic obstructive pulmonary disease, CABG - coronary artery bypass grafting, CPB - cardiopulmonary bypass. | ||||
|
Risk factors |
Univariate analysis | Multivariate analysis | ||
|---|---|---|---|---|
| HR (95% CI) | Р-value | HR (95% CI) | Р-value | |
| Age per 1 y | 0.99 (0.95-1.04) | 0.899 | - | - |
| Female | 0,81 (0,34 – 1,94) | 0.638 | - | - |
| BMI per 1 kg/m² | 1.03 (0.95-1.11) | 0.510 | - | - |
| Smoking | 1.71 (0.88-3.35) | 0.114 | - | - |
| Previos Stroke | 1,08 (0,47-2,46) | 0.851 | - | - |
| Previous MI | 0.99 (0.32-1.26) | 0.194 | - | - |
| Bilateral CA stenosis | 1.06 (0.38-0.99) | 0.913 | - | - |
| LV EF | 0.84 (0.73-0.98) | 0.022* | 0.87(0.74-1.01) | 0.061 |
| Three-vessel disease | 0.80 (0.38-1.70) | 0.568 | - | - |
| LCA trunk disease >50% | 0.74 (0.35-1.58) | 0.442 | - | - |
| Lower extremity artery stenosis | 2.24 (0.94-5.37) | 0.069 | 2.45 (1.20-7.23) | 0.018* |
| Diabetes | 0.94 (0.46-1.89) | 0.856 | - | - |
| CKD | 0.94 (0.42-2.15) | 0.892 | - | - |
| COPD | 3.19 (1.33-7.66) | 0.009* | 2.89 (1.17-7.13) | 0.021* |
| CABG CPB | 1.93 (0.48-1.81) | 0.839 | - | - |
| Stage | 0.64 (0.34 – 1.21) | 0.169 | - | - |
| * – differences in indicators are statistically significant (p<0.05) MI – myocardial infarction, BMI - body mass index, CA - carotid artery, LV EF - left ventricular ejection fraction, LCA - left coronary artery, CKD - chronic kidney disease, COPD - chronic obstructive pulmonary disease, CABG - coronary artery bypass grafting, CPB - cardiopulmonary bypass. | ||||
|
Risk factors |
Univariate analysis | |
|---|---|---|
| HR (95% CI) | Р-value | |
| Age per 1 y | 1.01 (0.96-1.04) | 0.879 |
| Female | 0.88 (0.41 – 1.88) | 0.745 |
| BMI per 1 kg/m² | 0.96 (0.89–1.04) | 0.365 |
| Smoking | 0.82 (0.42 – 1.63) | 0.577 |
| Previous Stroke | 0.92 (0.43-1.97) | 0.829 |
| Previous MI | 1.08 (0.61-1.92) | 0.780 |
| Bilateral CA stenosis | 0.83 (0.30-2.30) | 0.715 |
| LV EF | 0.90 (0.79-1.03) | 0.121 |
| Three-vessel disease | 1.30 (0.61-2.78) | 0.500 |
| LCA trunk disease >50% | 1.42 (0.79-2.56) | 0.236 |
| Lower extremity artery stenosis | 0.80 (0.95-2.58) | 0.710 |
| Diabetes | 0.87 (0.46-1.64) | 0.665 |
| CKD | 1.56 (0.83 – 2.96) | 0.169 |
| COPD | 0.05 (0.01-10.74) | 0.268 |
| CABG CPB | 2.02 (0.86-4.06) | 0.115 |
| Stage | 0.772 (0.443-1.347) | 0.364 |
| BMI - body mass index, MI – myocardial infarction, CA - carotid artery, LV EF - left ventricular ejection fraction, LCA - left coronary artery, CKD - chronic kidney disease, COPD - chronic obstructive pulmonary disease, CABG - coronary artery bypass grafting, CPB - cardiopulmonary bypass. | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





