Submitted:
12 December 2023
Posted:
13 December 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. The Metabolic Shift in Cancer
2.1. Why Do Tumors Adopt Glycolysis over OXPHOS?
2.1.1. Reason 1: Mitochondrial Dysfunction
| Gene | Encoding DNA | Protein | Cycle | Reported dysregulation in cancer | Publications |
|---|---|---|---|---|---|
| Aco2 | Nuclear | Aconitase 2 | TCA (Krebs cycle) |
|
[76,92] |
| IDH1 | Nuclear | Isocitrate Dehydrogenase 1 | TCA | Point mutations | [74,76,93,94,95,96,97] |
| SDH | Nuclear | Succinate Dehydrogenase | TCA and ETC cycle |
|
[72,76,98,99,100,101,102,103,104,105,106] |
| FH | Nuclear | Fumarate Hydratase | TCA |
|
[73,76,107,108,109,110,111] |
| Gene | Class | Genetic alteration | Pathway affected | Effects on OXPHOS (ETC cycle) | The effect of cancer progression | References |
|---|---|---|---|---|---|---|
|
MYC (MYC proto-Oncogene Protein) |
Oncogene | Point mutation, amplification | TGF-β Signaling Pathway | Stimulates mitochondrial biogenesis and function through regulating Transcription Factor A Mitochondrial gene | Self-sufficiency in growth status | [76,112,113,114] |
|
AKT (Alpha Serine/Threonine Kinase) |
Oncogene | Point mutation, amplification, overexpression | AKT pathway |
|
Evade apoptosis | [113,115,116] |
| P53 | Tumor Suppressor gene | Point mutation, Deletion | P53 pathway, Cell Cycle Control: G2/M DNA Damage Checkpoint |
|
Evade apoptosis, insensitivity to anti-growth signals | [113,117,118] |
|
PI3K (Phophatidylinositol-4,5-Bisphosphate 3-Kinase) |
Tumor Suppressor | Point mutation | AKT pathway |
|
Evade apoptosis | [113,119] |
|
PTEN (Phosphatase and Tensin Homolog) |
Tumor Suppressor | Point mutation, deletion | PI3K pathway |
|
Evade apoptosis | [113,120] |
|
MDM2 (Mouse Double Minute 2, Human Homolog Of; P53-Binding Protein) |
Oncogenes | Amplification | Cell Cycle Control: G1/S Checkpoint |
|
Evade apoptosis | [113,121] |
|
BRAF (B-Raf Proto-Oncogene, Serine/Threonine Kinase) |
Oncogenes | Point mutation, amplification, increased expression | MAPK pathway (RAS) | BRAF upregulation inhibits oxidative phosphorylation gene transcription, mitochondrial b, biogenesis, and the expression of PGC1a by targeting the melanocyte lineage factor (MITF). | Self-sufficiency in growth status | [113,122] |
|
KRAS (Kirsten rat sarcoma viral oncogene homolog, GTPase) |
Oncogene | Point mutation | MAPK pathway | KRAS activation of MAPK and PI3K pathways stabilizes and activates hypoxia-inducible factors-1 alpha and -2 alpha (HIF-1α and HIF-2) which facilitates ischemic adaptation. KRAS stimulates aerobic glycolysis by overexpressing Hexokinase, lactate dehydrogenase, and glucose transporters. KRAS induces glutaminolysis by upregualting Glutamate Oxaloacetate Transaminase 1,2. (GOT), leading to aspartate and NADPH generation, and the activation of the NRF2 antioxidant system. Upregulation of RAS leads to increased autophagy and micropinocytosis contributing to the disruption of cellular energy balance and nutrient scavenging. |
Self-sufficiency in growth status | [113,123,124,125,126] |
|
NF-κB (Nuclear Factor Kappa B) |
Oncogene | Amplification, rearrangement, chromosomal translocation in several members of the NF-κB protein family or constitutional activation of NF-κB | NF-κB pathway | NF-κB upregulation and activity cause a decline in mitochondrial respiratory capacity and reduces the expression of key mitochondrial proteins including SDHA, ANT-1, UCP3, and MFN2 and causes increased fission and mitophagy of mitochondrial organelle. It upregulates PGC1α and correlates with high ROS. | Tumor growth | [113,127,128] |
| EGFR (ErbB1 Epidermal Growth Factor Receptor) | Oncogene | Amplification, upregulation | PI3K and MAPK pathway | EGFR modulates mitochondrial function through modification of Cox-II | Self-sufficiency in growth status | [113,129] |
|
IGFR (Insulin-like Growth factor receptor) |
Oncogene | Amplification | AKT, PI3K, and MAPK pathways | Increased IGFR expression alters ATP synthesis and increases mitochondrial function. And decrease mitochondrial ROS production associated with the induction of antioxidant response. | antiapoptotic, cell-survival, and transforming activities |
[113,130] |
|
ErbB2 (HER2, Receptor tyrosine-protein kinase erbB-2 ) |
Oncogene | Amplification | MAPK, PI3K, AKT, and mTOR | ErbB2 overexpression causes downregulation of pro-apoptotic Bcl-2 family protein (Bcl-xS) and increases levels of anti-apoptotic Bcl-xL. This leads to mitochondrial dysfunction and a loss of mitochondrial membrane potential, a 35% decline in ATP levels, and a loss of redox capacity (mitochondrial reductase activity). | Anti-apoptotic and pro-proliferative effects | [113,131] |
|
HIF-1 α (Hypoxia Inducible Factor 1 Subunit Alpha) |
Oncogene | It is stabilized and activated in hypoxic tumor conditions and by inactivating mutations of SDH, FH, IDH as well as due to oncogenic mutation activating other signaling pathways (MAPK, AKT, and mTOR) | HIF-1α induces the expression of pyruvate dehydrogenase kinase 1 (PDK1). PDK1 phosphorylates and inactivates mitochondrial pyruvate dehydrogenase. Enhances the dependence of cells on glycolysis for ATP production instead of OXPHOS. | Metabolism, cell survival, erythropoiesis, angiogenesis | [132,133,134] |
2.1.2. Reason 2: Glycolysis Supports the Proliferative Needs of Cancer Cells
2.1.3. Reason 3: Activation of HIF-1α by ROS
2.1.4. Reason 4: Dysregulation of the Glycolytic Machinery
| Gene ID | Gene Name | Mutation/deregulation | Function in glycolysis | Publication |
|---|---|---|---|---|
| HK | Hexokinase | Upregulated by p53 in cancer and promotes tumor growth and survival | Phosphorylates glucose when it enters the cells | [76,170,171,172] |
| PFK1 | 6-PhosphoFruktoKinsae-1 | Amplification and/or upregulation, posttranslational modification reported in multiple cancer types. | PFK1 catalyzes the phosphorylation of fructose-6-phosphate (F6P) to fructose-1, 6-bisphosphate (Fru-1,6-P2) using Mg-ATP as a phosphoryl donor. | [76,173,174,175] |
| PK | Pyruvate Kinase | Posttranslational modification or enhanced expression that benefits cancer | PK is involved in the final step of glycolysis, and it mediates the transfer of a phosphate group from phosphoenolpyruvate (PEP) to ADP resulting in pyruvate and ATP. | [76,176,177,178,179] |
| PDK-1 | Pyruvate Dehydrogenase Kinase -1 | Upregulation | PDK is a kinase enzyme that inactivates Pyruvate Dehydrogenase by phosphorylation dephosphorylation at different specific serine residues. PDK decreases the oxidation of pyruvate in mitochondria and increases the conversion of pyruvate to lactate in the cytosol. |
[76,180,181,182] |
2.1.5. Reason 5: AMPK Inhibition in Cancer Leads to a Glycolytic Shift
3. The Metabolic Shift in T2D
3.1. The Metabolic Shift During the Pathogenesis of Insulin Resistance and T2D
3.2. The Metabolic Shift in Established Insulin Resistance and T2D
3.3. Mitochondrial Dysfunction is a Result of Insulin Resistance
3.4. The Role of ROS in Insulin Resistance and T2D
3.6. AMPK Inhibition Implicated in Insulin Resistance and T2D
4. Metabolic Therapeutic Approaches in Cancer and T2D
4.1. Pharmacological-Based Approaches Targeting Mitochondrial Metabolism in Cancer
4.1.1. BACH1 Depletion Activates OXPHOS and Sensitizes Tumor Cells to Metformin
4.1.2. Dichloroacetate and EGFR-Inhibitors Reverse the Warburg Effect in Cancer
4.1.3. Metformin Activates AMPK to Induce Apoptosis in Cancer
4.1.4. Targeting PI3K/AKT pathway in cancer
4.2. Pharmacological-Based Approaches Targeting Mitochondrial Metabolism in T2D
4.2.1. Apoptosis-Inducing Factor Ablation in Diabetic Mice Inhibited OXPHOS
4.2.2. Metformin as a Metabolic Inhibitor in T2D
4.2.3. Targeting PI3K/AKT pathway in T2D
5. Nutritional Therapeutic Approaches in Cancer and T2D
5.1. Nutritional- and Dietary-Based Approaches Targeting Mitochondrial Metabolism in Cancer
5.1.1. Alpha-lipoic Acid as a Metabolic Modulator in Cancer
5.1.2. Flavonoids as a Metabolic Modulator in Cancer
5.2. Nutritional- and Dietary-Based Approaches Targeting Mitochondrial Metabolism in T2D
5.2.1. ALA as a Metabolic Modulator in T2D
5.2.2. Flavonoids as a Metabolic Modulator in T2D
5.2.3. Effects of glutamine supplementation on T2D
6. Conclusion
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- DeBeradinis R, Thompson C. Cellular Metabolism And Disease: What Do Metabolic Outliers Teach Us? NIH Public Access. 2012;148:1132–44.
- O’Connor C, Adams JU. Essentials of cell biology. 2001.
- Xian Zhang P, Qi Xing Y, Dong Niu Y. Fundamentals Of The Warburg Effect In Cancer. Journal of Nutritional Oncology. 2019;4:108–14.
- O. Warburg. On The Origin Of Cancer Cells. Science. 1956;123:309–14. [CrossRef]
- Warburg O. The Metabolism Of Carcinoma Cells. The Journal of Cancer Research. 1925;9:148–63. [CrossRef]
- Warburg O, Minami S. Experiments On Surviving Carcinoma Tissue. Journal Of Moelcular Medicine. 1923;2:776–7.
- Koukourakis MI, Giatromanolaki A, Bougioukas G, Sivridis E. Lung Cancer: A Comparative Study Of Metabolism Related Protein Expression In Cancer Cells And Tumor Associated Stroma. Cancer Biology & Therapy. 2007;6:1472–5.
- Isidoro A, Casado E, Redondo A, Acebo P, Espinosa E, Alonso AM, Cejas P, Hardisson D, Fresno Vara JA, Belda-Iniesta C, González-Barón M, Cuezva JM. Breast Carcinomas Fulfill The Warburg Hypothesis And Provide Metabolic Markers Of Cancer Prognosis. Carcinogenesis. 2005;26:2095–104. [CrossRef]
- Leung CO ning, Wong CC lui, Fan DN yin, Kai AK lun, Tung EK kwan, Xu IM jing, Ng IO lin, Lo RC lam. PIM1 Regulates Glycolysis And Promotes Tumor Progression In Hepatocellular Carcinoma. Oncotarget. 2015;6:10880–92.
- Fan P, Wang B, Meng Z, Zhao J, Jin X. PES1 Is Transcriptionally Regulated By BRD4 And Promotes Cell Proliferation And Glycolysis In Hepatocellular Carcinoma. International Journal of Biochemistry and Cell Biology. 2018;104:1–8. [CrossRef]
- Marie SKN, Shinjo SMO. Metabolism And Brain Cancer. Clinics. 2011;66:33–43. [CrossRef]
- Martiny PB, Alcoba DD, Neto BS, Carvalho PC, Brum IS. A Proteomic Glimpse Into The Oncogenesis Of Prostate Cancer. Journal of Applied Biomedicine. 2018;16:328–36. [CrossRef]
- Kobayashi Y, Banno K, Kunitomi H, Takahashi T, Takeda T, Nakamura K, Tsuji K, Tominaga E, Aoki D. Warburg Effect In Gynecologic Cancers. Journal of Obstetrics and Gynaecology Research. 2019;45:542–8.
- Zhou W, Capello M, Fredolini C, Racanicchi L, Piemonti L, Liotta LA, Novelli F, Petricoin EF. Proteomic Analysis Reveals Warburg Effect And Anomalous Metabolism Of Glutamine In Pancreatic Cancer Cells. Journal of Proteome Research. 2012;11:554–63. [CrossRef]
- Altenberg B, Greulich KO. Genes Of Glycolysis Are Ubiquitously Overexpressed In 24 Cancer Classes. Genomics. 2004;84:1014–20. [CrossRef]
- Kim TM, Paeng JC, Chun IK, Keam B, Jeon YK, Lee SH, Kim DW, Lee DS, Kim CW, Chung JK, Kim IH, Heo DS. Total Lesion Glycolysis In Positron Emission Tomography Is A Better Predictor Of Outcome Than The International Prognostic Index For Patients With Diffuse Large B Cell Lymphoma. Cancer. 2013;119:1195–202. [CrossRef]
- Guo B, Tan X, Ke Q, Cen H. Prognostic Value Of Baseline Metabolic Tumor Volume And Total Lesion Glycolysis In Patients With Lymphoma: A Meta-Analysis. PLoS ONE. 2019;14:1–17. [CrossRef]
- Suganuma K, Miwa H, Imai N, Shikami M, Gotou M, Goto M, Mizuno S, Takahashi M, Yamamoto H, Hiramatsu A, Wakabayashi M, Watarai M, Hanamura I, Imamura A, Mihara H, Nitta M. Energy Metabolism Of Leukemia Cells: Glycolysis Versus Oxidative Phosphorylation. Leukemia and Lymphoma. 2010;51:2112–9.
- Chen L, Hu N, Wang C, Zhao H. HOTAIRM1 Knockdown Enhances Cytarabine-Induced Cytotoxicity By Suppression Of Glycolysis Through The Wnt/β-Catenin/PFKP Pathway In Acute Myeloid Leukemia Cells. Archives of Biochemistry and Biophysics. 2020;680:108244. [CrossRef]
- Whitaker-Menezes D, Martinez-Outschoorn UE, Flomenberg N, Birbe RC, Witkiewicz AK, Howell A, Pavlides S, Tsirigos A, Ertel A, Pestell RG, Broda P, Minetti C, Lisanti MP, Sotgia F. Hyperactivation Of Oxidative Mitochondrial Metabolism In Epithelial Cancer Cells In Situ: Visualizing The Therapeutic Effects Of Metformin In Tumor Tissue. Cell Cycle. 2011;10:4047–64.
- Viale A, Corti D, Draetta GF. Tumors And Mitochondrial Respiration: A Neglected Connection. Cancer Research. 2015;75:3685–6. [CrossRef]
- Simonnet H. Low Mitochondrial Respiratory Chain Content Correlates With Tumor Aggressiveness In Renal Cell Carcinoma. Carcinogenesis. 2002;23:759–68. [CrossRef]
- Faure-Vigny H, Heddi A, Giraud S, Chautard D, Stepien G. Expression Of Oxidative Phosphorylation Genes In Renal Tumors And Tumoral Cell Lines. Molecular Carcinogenesis. 1996;16:165–72. [CrossRef]
- Hayashi JI, Takemitsu M, Nonaka I. Recovery Of The Missing Tumorigenicity In Mitochondrial DNA-Less HeLa Cells By Introduction Of Mitochondrial DNA From Normal Human Cells. Somatic Cell and Molecular Genetics. 1992;18:123–9. [CrossRef]
- Cavalli LR, Varella-Garcia M, Liang BC. Diminished Tumorigenic Phenotype After Depletion Of Mitochondrial DNA. Cell Growth and Differentiation. 1997;8:1189–98.
- Tan AS et al. Mitochondrial Genome Acquisition Restores Respiratory Function And Tumorigenic Potential Of Cancer Cells Without Mitochondrial DNA. Cell Metabolism. 2015;21:81–94.
- Lebleu VS, O’Connell JT, Gonzalez Herrera KN, Wikman H, Pantel K, Haigis MC, De Carvalho FM, Damascena A, Domingos Chinen LT, Rocha RM, Asara JM, Kalluri R. PGC-1α Mediates Mitochondrial Biogenesis And Oxidative Phosphorylation In Cancer Cells To Promote Metastasis. Nature Cell Biology. 2014;16:992–1003. [CrossRef]
- Yang L, Venneti S, Nagrath D. Glutaminolysis: A Hallmark Of Cancer Metabolism. Annual Review of Biomedical Engineering. 2017;19:163–94. [CrossRef]
- Moreadith RW, Lehninger AL. The Pathways Of Glutamate And Glutamine Oxidation By Tumor Cell Mitochondria. Role Of Mitochondrial NAD(P)+-Dependent Malic Enzyme. Journal of Biological Chemistry. 1984;259:6215–21. [CrossRef]
- Schiliro C, Firestein BL. Mechanisms Of Metabolic Reprogramming In Cancer Cells Supporting Enhanced Growth And Proliferation. Cells 2021, Vol 10, Page 1056. 2021;10:1056. [CrossRef]
- Fan J, Kamphorst JJ, Mathew R, Chung MK, White E, Shlomi T, Rabinowitz JD. Glutamine-Driven Oxidative Phosphorylation Is A Major ATP Source In Transformed Mammalian Cells In Both Normoxia And Hypoxia. Molecular Systems Biology. 2013;9:712. [CrossRef]
- Tardito S et al. Glutamine Synthetase Activity Fuels Nucleotide Biosynthesis And Supports Growth Of Glutamine-Restricted Glioblastoma. Nature Cell Biology. 2015;17:1556–68. [CrossRef]
- WILLIAMS JIMC, KIZAKI H, WEBER G, MORRIS HP. Increased CTP Synthetase Activity In Cancer Cells. Nature. 1978;271:71–3. [CrossRef]
- DeFronzo RA, Tripathy D. Skeletal Muscle Insulin Resistance Is The Primary Defect In Type 2 Diabetes. Diabetes Care. 2009;32:S157–63. [CrossRef]
- Weir GC, Leahy JL, Bonner-Weiner S. B-Cell Dysfunction Induced By Chronic Hyperglycemia. Diabetes Care. 1992;15:442–55.
- Robertson R, Zhou H, Zhang T, Harmon JS. Chronic Oxidative Stress As A Mechanism For Glucose Toxicity Of The Beta Cell In Type 2 Diabetes. Cell Biochemistry and Biophysics. 2007;48:139–46. [CrossRef]
- Sakai K, Matsumoto K, Nishikawa T, Suefuji M, Nakamaru K, Hirashima Y, Kawashima J, Shirotani T, Ichinose K, Brownlee M, Araki E. Mitochondrial Reactive Oxygen Species Reduce Insulin Secretion By Pancreatic β-Cells. Biochemical and Biophysical Research Communications. 2003;300:216–22. [CrossRef]
- Lortz S, Tiedge M. Glucose Toxicity In B-Cells: Type 2 Diabetes, Good Radicals Gone Bad, And The Glutathione Connection. Free Radical Biology and Medicine. 2003;34:581–7.
- Larsen S, Scheede-Bergdahl C, Whitesell T, Boushel R, Bergdahl A. Increased Intrinsic Mitochondrial Respiratory Capacity In Skeletal Muscle From Rats With Streptozotocin-Induced Hyperglycemia. Physiological Reports. 2015;3:1–10. [CrossRef]
- Boirie Y. Insulin Regulation Of Mitochondrial Proteins And Oxidative Phosphorylation In Human Muscle. Trends in Endocrinology and Metabolism. 2003;14:393–4. [CrossRef]
- Zhang Y, Ye J. Mitochondrial Inhibitor As A New Class Of Insulin Sensitizer. Acta Pharmaceutica Sinica B. 2012;2:341–9. [CrossRef]
- Stump CS, Short KR, Bigelow ML, Schimke JM, Nair KS. Effect Of Insulin On Human Skeletal Muscle Mitochondrial ATP Production, Protein Synthesis, And MRNA Transcripts. Proceedings of the National Academy of Sciences of the United States of America. 2003;100:7996–8001.
- Špaček T, Šantorová J, Zacharovová K, Berková Z, Hlavatá L, Saudek F, Ježek P. Glucose-Stimulated Insulin Secretion Of Insulinoma INS-1E Cells Is Associated With Elevation Of Both Respiration And Mitochondrial Membrane Potential. International Journal of Biochemistry and Cell Biology. 2008;40:1522–35. [CrossRef]
- Ahmad W, Ijaz B, Shabbiri K, Ahmed F, Rehman S. Oxidative Toxicity In Diabetes And Alzheimer’s Disease: Mechanisms Behind ROS/ RNS Generation. Journal of Biomedical Science. 2017;24:1–10. [CrossRef]
- Bhansali S, Bhansali A, Walia R, Saikia UN, Dhawan V. Alterations In Mitochondrial Oxidative Stress And Mitophagy In Subjects With Prediabetes And Type 2 Diabetes Mellitus. Frontiers in Endocrinology. 2017;8. [CrossRef]
- Bitar MS, Al-Saleh E, Al-Mulla F. Oxidative Stress - Mediated Alterations In Glucose Dynamics In A Genetic Animal Model Of Type II Diabetes. Life Sciences. 2005;77:2552–73. [CrossRef]
- Petersen KF, Dufour S, Befroy D, Garcia R, Shulman GI. Impaired Mitochondrial Activity In The Insulin-Resistant Offspring Of Patients With Type 2 Diabetes. New England Journal of Medicine. 2004;350:664–71. [CrossRef]
- Kelley DE, He J, Menshikova E V., Ritov VB. Dysfunction Of Mitochondria In Human Skeletal Muscle In Type 2 Diabetes. Diabetes. 2002;51:2944–50. [CrossRef]
- Frederiksen CM, Højlund K, Hansen L, Oakeley EJ, Hemmings B, Abdallah BM, Brusgaard K, Beck-Nielsen H, Gaster M. Transcriptional Profiling Of Myotubes From Patients With Type 2 Diabetes: No Evidence For A Primary Defect In Oxidative Phosphorylation Genes. Diabetologia. 2008;51:2068–77. [CrossRef]
- Boushel R, Gnaiger E, Schjerling P, Skovbro M, Kraunsøe R, Dela F. Patients With Type 2 Diabetes Have Normal Mitochondrial Function In Skeletal Muscle. Diabetologia. 2007;50:790–6. [CrossRef]
- Fisher-Wellman KH, Weber TM, Cathey BL, Brophy PM, Gilliam LAA, Kane CL, Maples JM, Gavin TP, Houmard JA, Neufer PD. Mitochondrial Respiratory Capacity And Content Are Normal In Young Insulin-Resistant Obese Humans. Diabetes. 2014;63:132–41. [CrossRef]
- Misu H, Takamura T, Matsuzawa N, Shimizu A, Ota T, Sakurai M, Ando H, Arai K, Yamashita T, Honda M, Yamashita T, Kaneko S. Genes Involved In Oxidative Phosphorylation Are Coordinately Upregulated With Fasting Hyperglycaemia In Livers Of Patients With Type 2 Diabetes. Diabetologia. 2006;50:268–77. [CrossRef]
- Buchner DA, Yazbek SN, Solinas P, Burrage LC, Morgan MG, Hoppel CL, Nadeau JH. Increased Mitochondrial Oxidative Phosphorylation In The Liver Is Associated With Obesity And Insulin Resistance. Obesity. 2011;19:917–24. [CrossRef]
- Ciapaite J, Bakker SJL, Van Eikenhorst G, Wagner MJ, Teerlink T, Schalkwijk CG, Fodor M, Ouwens DM, Diamant M, Heine RJ, Westerhoff H V., Krab K. Functioning Of Oxidative Phosphorylation In Liver Mitochondria Of High-Fat Diet Fed Rats. Biochimica et Biophysica Acta - Molecular Basis of Disease. 2007;1772:307–16. [CrossRef]
- Petersen KF, Befroy D, Dufour S, Dziura J, Ariyan C, Rothman DL, DiPietro L, Cline GW, Shulman GI. Mitochondrial Dysfunction In The Elderly: Possible Role In Insulin Resistance. Science. 2003;300:1140–2. [CrossRef]
- Chen H, Fang Y, Liang L, Wang C. Insulin Resistance Leads to Mitochondrial Dysfunction in Hepatocyte. Eur. Soc. Paediatr. Endocrinol., vol. 92, 2019.
- Sasaki M, Fujimoto S, Sato Y, Nishi Y, Mukai E, Yamano G, Sato H, Tahara Y, Ogura K, Nagashima K, Inagaki N. Reduction Of Reactive Oxygen Species Ameliorates Metabolism-Secretion Coupling In Islets Of Diabetic GK Rats By Suppressing Lactate Overproduction. Diabetes. 2013;62:1996–2003. [CrossRef]
- Cantley J, Biden TJ. Sweet And Sour β-Cells: ROS And Hif1α Induce Warburg-Like Lactate Production During Type 2 Diabetes. Diabetes. 2013;62:1823–5. [CrossRef]
- Choi CS, Kim YB, Lee FN, Zabolotny JM, Kahn BB, Youn JH. Lactate Induces Insulin Resistance In Skeletal Muscle By Suppressing Glycolysis And Impairing Insulin Signaling. American Journal of Physiology - Endocrinology and Metabolism. 2002;283:233–40. [CrossRef]
- Akram M. Citric Acid Cycle And Role Of Its Intermediates In Metabolism. Cell Biochemistry and Biophysics. 2014;68:475–8. [CrossRef]
- Akram M. Mini-Review On Glycolysis And Cancer. Journal of Cancer Education. 2013;28:454–7. [CrossRef]
- Nolfi-Donegan D, Braganza A, Shiva S. Mitochondrial Electron Transport Chain: Oxidative Phosphorylation, Oxidant Production, And Methods Of Measurement. Redox Biology. 2020:101674. [CrossRef]
- Simonnet H, Demont J, Pfeiffer K, Guenaneche L, Bouvier R, Brandt U, Schägger H, Godinot C. Mitochondrial Complex I Is Deficient In Renal Oncocytomas. Carcinogenesis. 2003;24:1461–6. [CrossRef]
- Baracca A, Chiaradonna F, Sgarbi G, Solaini G, Alberghina L, Lenaz G. Mitochondrial Complex I Decrease Is Responsible For Bioenergetic Dysfunction In K-Ras Transformed Cells. Biochimica et Biophysica Acta - Bioenergetics. 2010;1797:314–23. [CrossRef]
- Bonora E, Porcelli AM, Gasparre G, Biondi A, Ghelli A, Carelli V, Baracca A, Tallini G, Martinuzzi A, Lenaz G, Rugolo M, Romeo G. Defective Oxidative Phosphorylation In Thyroid Oncocytic Carcinoma Is Associated With Pathogenic Mitochondrial DNA Mutations Affecting Complexes I And III. Cancer Research. 2006;66:6087–96. [CrossRef]
- Bellance N, Benard G, Furt F, Begueret H, Smolková K, Passerieux E, Delage JP, Baste JM, Moreau P, Rossignol R. Bioenergetics Of Lung Tumors: Alteration Of Mitochondrial Biogenesis And Respiratory Capacity. International Journal of Biochemistry and Cell Biology. 2009;41:2566–77. [CrossRef]
- Liberti M V, Locasale JW. The Warburg Effect: How Does It Benefit Cancer Cells? Trends in Biochemical Sciences. 2016;41:287.
- Lee M, Yoon J. Metabolic Interplay Between Glycolysis And Mitochondrial Oxidation: The Reverse Warburg Effect And Its Therapeutic Implication. World Journal of Biological Chemistry. 2015;6:148–62. [CrossRef]
- Kim SY. Cancer Energy Metabolism: Shutting Power Off Cancer Factory. Biomolecules and Therapeutics. 2018;26:39–44. [CrossRef]
- Fu Y, Liu S, Yin S, Niu W, Xiong W. The Reverse Warburg Effect Is Likely To Be An Achilles ’ Heel Of Cancer That Can Be Exploited For Cancer Therapy 2017;8:57813–25. [CrossRef]
- Luis C, Duarte F, Faria I, Jarak I, Oliveira PF, Alves MG, Soares R, Fernandes R. Warburg Effect Inversion: Adiposity Shifts Central Primary Metabolism In MCF-7 Breast Cancer Cells. Life Sciences. 2019;223:38–46. [CrossRef]
- Slane BG, Aykin-Burns N, Smith BJ, Kalen AL, Goswami PC, Domann FE, Spitz DR. Mutation Of Succinate Dehydrogenase Subunit C Results In Increased O 2.-, Oxidative Stress, And Genomic Instability. Cancer Research. 2006;66:7615–20.
- Alam NA, Olpin S, Rowan A, Kelsell D, Leigh IM, Tomlinson IPM, Weaver T. Missense Mutations In Fumarate Hydratase In Multiple Cutaneous And Uterine Leiomyomatosis And Renal Cell Cancer. Journal of Molecular Diagnostics. 2005;7:437–43. [CrossRef]
- Gross S, Cairns RA, Minden MD, Driggers EM, Bittinger MA, Jang HG, Sasaki M, Jin S, Schenkein DP, Su SM, Dang L, Fantin VR, Mak TW. Cancer-Associated Metabolite 2-Hydroxyglutarate Accumulates In Acute Myelogenous Leukemia With Isocitrate Dehydrogenase 1 And 2 Mutations. Journal of Experimental Medicine. 2010;207:339–44. [CrossRef]
- Grassian AR et al. IDH1 Mutations Alter Citric Acid Cycle Metabolism And Increase Dependence On Oxidative Mitochondrial Metabolism. Cancer Research. 2014;74:3317–31.
- Chen JQ, Russo J. Dysregulation Of Glucose Transport, Glycolysis, TCA Cycle And Glutaminolysis By Oncogenes And Tumor Suppressors In Cancer Cells. Biochimica et Biophysica Acta - Reviews on Cancer. 2012;1826:370–84.
- Bourgeron T, Rustin P, Chretien D, Birch-machin M, Bourgeois M, Viegas-pequignot E, Munnich A, Rotig A. Mutation Of A Nuclear Succinate Dehydrogenase Gene Results In Mitochondrial Respiratory Chain Deficiency. Nature Genetics. 1995;11:144–9. [CrossRef]
- Böttcher M, Renner K, Berger R, Mentz K, Thomas S, Cardenas-Conejo ZE, Dettmer K, Oefner PJ, Mackensen A, Kreutz M, Mougiakakos D. D-2-Hydroxyglutarate Interferes With HIF-1α Stability Skewing T-Cell Metabolism Towards Oxidative Phosphorylation And Impairing Th17 Polarization. OncoImmunology. 2018;7:1–12. [CrossRef]
- Ferro F, Servais S, Besson P, Roger S, Dumas JF, Brisson L. Autophagy And Mitophagy In Cancer Metabolic Remodelling. Seminars in Cell and Developmental Biology. 2020;98:129–38. [CrossRef]
- Gonzalez CD, Alvarez S, Ropolo A, Rosenzvit C, Gonzalez Bagnes MF, Vaccaro MI. Autophagy, Warburg, And Warburg Reverse Effects In Human Cancer. BioMed Research International. 2014;2014. [CrossRef]
- Bhattacharya B, Mohd Omar MF, Soong R. The Warburg Effect And Drug Resistance. British Journal of Pharmacology. 2016;173:970–9. [CrossRef]
- Das CK, Mandal M, Kögel D. Pro-Survival Autophagy And Cancer Cell Resistance To Therapy. Cancer and Metastasis Reviews. 2018;37:749–66. [CrossRef]
- Poulogiannis G, McIntyre RE, Dimitriadi M, Apps JR, Wilson CH, Ichimura K, Luo F, Cantley LC, Wyllie AH, Adams DJ, Arends MJ. PARK2 Deletions Occur Frequently In Sporadic Colorectal Cancer And Accelerate Adenoma Development In Apc Mutant Mice. Proceedings of the National Academy of Sciences of the United States of America. 2010;107:15145–50.
- Veeriah S et al. Somatic Mutations Of The Parkinson’s Disease-Associated Gene PARK2 In Glioblastoma And Other Human Malignancies. Nature Genetics. 2010;42:77–82. [CrossRef]
- Hu HH et al. PARKIN Inactivation Links Parkinson’s Disease To Melanoma. Journal of the National Cancer Institute. 2016;108:1–8.
- Lee SB, She J, Deng B, Kim JJ, de Andrade M, Na J, Sun Z, Wampfler JA, Cunningham JM, Wu Y, Limper AH, Aubry MC, Wendt C, Biterman P, Yang P, Lou Z. Multiple-Level Validation Identifies PARK2 In The Development Of Lung Cancer And Chronic Obstructive Pulmonary Disease. Oncotarget. 2016;7:44211–23. [CrossRef]
- Letessier A, Garrido-Urbani S, Ginestier C, Fournier G, Esterni B, Monville F, Adélaïde J, Geneix J, Xerri L, Dubreuil P, Viens P, Charafe-Jauffret E, Jacquemier J, Birnbaum D, Lopez M, Chaffanet M. Correlated Break At PARK2/FRA6E And Loss Of AF-6/Afadin Protein Expression Are Associated With Poor Outcome In Breast Cancer. Oncogene. 2007;26:298–307.
- Sreedhar A, Petruska P, Miriyala S, Panchatcharam M, Zhao Y. UCP2 Overexpression Enhanced Glycolysis Via Activation Of PFKFB2 During Skin Cell Transformation. Oncotarget. 2017;8:95504–15. [CrossRef]
- Xu XD, Shao SX, Jiang HP, Cao YW, Wang YH, Yang XC, Wang YL, Wang XS, Niu HT. Warburg Effect Or Reverse Warburg Effect? A Review Of Cancer Metabolism. Oncology Research and Treatment. 2015;38:117–22. [CrossRef]
- Brandi J, Cecconi D, Cordani M, Torrens-Mas M, Pacchiana R, Dalla Pozza E, Butera G, Manfredi M, Marengo E, Oliver J, Roca P, Dando I, Donadelli M. The Antioxidant Uncoupling Protein 2 Stimulates HnRNPA2/B1, GLUT1 And PKM2 Expression And Sensitizes Pancreas Cancer Cells To Glycolysis Inhibition. Free Radical Biology and Medicine. 2016;101:305–16. [CrossRef]
- Pons DG, Nadal-Serrano M, Torrens-Mas M, Valle A, Oliver J, Roca P. UCP2 Inhibition Sensitizes Breast Cancer Cells To Therapeutic Agents By Increasing Oxidative Stress. Free Radical Biology and Medicine. 2015;86:67–77. [CrossRef]
- Mycielska ME, Broke-Smith TP, Palmer CP, Beckerman R, Nastos T, Erguler K, Djamgoz MBA. Citrate Enhances In Vitro Metastatic Behaviours Of PC-3M Human Prostate Cancer Cells: Status Of Endogenous Citrate And Dependence On Aconitase And Fatty Acid Synthase. International Journal of Biochemistry and Cell Biology. 2006;38:1766–77. [CrossRef]
- Arceci RJ. An Integrated Genomic Analysis Of Human Glioblastoma Multiforme. Yearbook of Oncology. 2009;2009:185–6. [CrossRef]
- Yan H, Parsons DW, Jin G, McLendon R, Rasheed BA, Yuan W, Kos I, Batinic-Haberle I, Jones S, Riggins GJ, Friedman H, Friedman A, Reardon D, Herndon J, Kinzler KW, Velculescu VE, Vogelstein B, Bigner DD. IDH1 And IDH2 Mutations In Gliomas. New England Journal of Medicine. 2009;360:765–73.
- Ward PS, Patel J, Wise DR, Abdel-Wahab O, Bennett BD, Coller HA, Cross JR, Fantin VR, Hedvat C V., Perl AE, Rabinowitz JD, Carroll M, Su SM, Sharp KA, Levine RL, Thompson CB. The Common Feature Of Leukemia-Associated IDH1 And IDH2 Mutations Is A Neomorphic Enzyme Activity Converting α-Ketoglutarate To 2-Hydroxyglutarate. Cancer Cell. 2010;17:225–34. [CrossRef]
- Kranendijk M et al. IDH2 Mutations In Patients With D-2-Hydroxyglutaric Aciduria. Science. 2010;330:7. [CrossRef]
- Dang L et al. Cancer-Associated IDH1 Mutations Produce 2-Hydroxyglutarate. Nature. 2009;462:739–44.
- Bardella C, Pollard PJ, Tomlinson I. SDH Mutations In Cancer. Biochimica et Biophysica Acta - Bioenergetics. 2011;1807:1432–43.
- Oyedotun KS, Lemire BD. The Quaternary Structure Of The Saccharomyces Cerevisiae Succinate Dehydrogenase: Homology Modeling, Cofactor Docking, And Molecular Dynamics Simulation Studies. Journal of Biological Chemistry. 2004;279:9424–31.
- Baysal BE. On The Association Of Succinate Dehydrogenase Mutations With Hereditary Paraganglioma. Trends in Endocrinology and Metabolism. 2003;14:453–9. [CrossRef]
- Neumann HPH, Pawlu C, Peczkowska M, Bausch B, McWhinney SR, Muresan M, Buchta M, Franke G, Klisch J, Bley TA, Hoegerle S, Boedeker CC, Opocher G, Schipper J, Januszewicz A, Eng C. Distict Clinical Features Of Paraganglioma Syndromes Associated With SDHB And SDHD Gene Mutations. The Journal of the American Medical Association. 2004;292:943–52.
- Pollard PJ, Wortham NC, Tomlinson IPM. The TCA Cycle And Tumorigenesis: The Examples Of Fumarate Hydratase And Succinate Dehydrogenase. Annals of Medicine. 2003;35:634–5. [CrossRef]
- Habano W, Sugai T, Nakamura SI, Uesugi N, Higuchi T, Terashima M, Horiuchi S. Reduced Expression And Loss Of Heterozygosity Of The SDHD Gene In Colorectal And Gastric Cancer. Oncology Reports. 2003;10:1375–80. [CrossRef]
- Gimenez-Roqueplo AP, Favier J, Rustin P, Mourad JJ, Plouin PF, Corvol P, Rötig A, Jeunemaitre X. The R22X Mutation Of The SDHD Gene In Hereditary Paraganglioma Abolishes The Enzymatic Activity Of Complex II In The Mitochondrial Respiratory Chain And Activates The Hypoxia Pathway. American Journal of Human Genetics. 2001;69:1186–97. [CrossRef]
- Gimenez-Roqueplo AP, Favier J, Rustin P, Rieubland C, Crespin M, Nau V, Van Kien PK, Corvol P, Plouin PF, Jeunemaitre X. Mutations In The SDHB Gene Are Associated With Extra-Adrenal And/Or Malignant Phaeochromocytomas. Cancer Research. 2003;63:5615–21.
- Selak MA, Armour SM, MacKenzie ED, Boulahbel H, Watson DG, Mansfield KD, Pan Y, Simon MC, Thompson CB, Gottlieb E. Succinate Links TCA Cycle Dysfunction To Oncogenesis By Inhibiting HIF-α Prolyl Hydroxylase. Cancer Cell. 2005;7:77–85. [CrossRef]
- Jaramillo MC, Zhang DD. The Emerging Role Of The Nrf2-Keap1 Signaling Pathway In Cancer. Genes and Development. 2013;27:2179–91. [CrossRef]
- Tomlinson IPM et al. Germline Mutations In FH Predispose To Dominantly Inherited Uterine Fibroids, Skin Leiomyomata And Papillary Renal Cell Cancer The Multiple Leiomyoma Consortium. Nature Genetics. 2002;30:406–10.
- Martinez-Mir A, Glaser B, Chuang GS, Horev L, Waldman A, Engler DE, Gordon D, Spelman LJ, Hatzibougias I, Green J, Christiano AM, Zlotogorski A. Germline Fumarate Hydratase Mutations In Families With Multiple Cutaneous And Uterine Leiomyomata. Journal of Investigative Dermatology. 2003;121:741–4. [CrossRef]
- Bardella C et al. Aberrant Succination Of Proteins In Fumarate Hydratase-Deficient Mice And HLRCC Patients Is A Robust Biomarker Of Mutation Status. Journal of Pathology. 2011;225:4–11. [CrossRef]
- Ooi A, Furge KA. Fumarate Hydratase Inactivation In Renal Tumors: HIF1α, NRF2 And “Cryptic Targets” Of Transcription Factors. Chinese Journal of Cancer. 2012;31:413–20.
- Goetzman ES, Prochownik E V. The Role For Myc In Coordinating Glycolysis, Oxidative Phosphorylation, Glutaminolysis, And Fatty Acid Metabolism In Normal And Neoplastic Tissues. Frontiers in Endocrinology. 2018;9. [CrossRef]
- Levine AJ, Puzio-Kuter AM. The Control Of The Metabolic Switch In Cancers By Oncogenes And Tumor Suppressor Genes. Science. 2010;330:1340–4. [CrossRef]
- Li F, Wang Y, Zeller KI, Potter JJ, Wonsey DR, O’Donnell KA, Kim J -w., Yustein JT, Lee LA, Dang C V. Myc Stimulates Nuclearly Encoded Mitochondrial Genes And Mitochondrial Biogenesis. Molecular and Cellular Biology. 2005;25:6225–34.
- Song HP, Zhang L, Dang YM, Yan H, Chu ZG, Huang YS. The Phosphatidylinositol 3-Kinase-Akt Pathway Protects Cardiomyocytes From Ischaemic And Hypoxic Apoptosis Via Mitochondrial Function. Clinical and Experimental Pharmacology and Physiology. 2010;37:598–604. [CrossRef]
- Goo CK, Lim HY, Ho QS, Too HP, Clement MV, Wong KP. PTEN/Akt Signaling Controls Mitochondrial Respiratory Capacity Through 4E-BP1. PLoS ONE. 2012;7:1–12. [CrossRef]
- Lebedeva MA, Eaton JS, Shadel GS. Loss Of P53 Causes Mitochondrial DNA Depletion And Altered Mitochondrial Reactive Oxygen Species Homeostasis. Biochimica et Biophysica Acta - Bioenergetics. 2009;1787:328–34. [CrossRef]
- Matoba S, Kang JG, Patino WD, Wragg A, Boehm M, Gavrilova O, Hurley PJ, Bunz F, Hwang PM. P53 Regulates Mitochondrial Respiration. Science. 2006;312:1650–3. [CrossRef]
- Goan YG, Wu WT, Liu CI, Neoh CA, Wu YJ. Involvement Of Mitochondrial Dysfunction, Endoplasmic Reticulum Stress, And The PI3K/AKT/MTOR Pathway In Nobiletin-Induced Apoptosis Of Human Bladder Cancer Cells. Molecules. 2019;24. [CrossRef]
- Luo J, Manning BD, Cantley LC. Targeting The PI3K-Akt Pathway In Human Cancer: Rationale And Promise. Cancer Cell. 2003;4:257–62. [CrossRef]
- Rubio-Patiño C, Trotta AP, Chipuk JE. MDM2 And Mitochondrial Function: One Complex Intersection. Biochemical Pharmacology. 2019;162:14–20. [CrossRef]
- Haq R, Shoag J, Andreu-Perez P, Yokoyama S, Edelman H, Rowe GC, Frederick DT, Hurley AD, Nellore A, Kung AL, Wargo JA, Song JS, Fisher DE, Arany Z, Widlund HR. Oncogenic BRAF Regulates Oxidative Metabolism Via PGC1α And MITF. Cancer Cell. 2013;23:302–15. [CrossRef]
- Chun SY, Johnson C, Washburn JG, Cruz-Correa MR, Dang DT, Dang LH. Oncogenic KRAS Modulates Mitochondrial Metabolism In Human Colon Cancer Cells By Inducing HIF-1α And HIF-2α Target Genes. Molecular Cancer. 2010;9:1–11. [CrossRef]
- Pylayeva-Gupta Y, Grabocka E, Bar-Sagi D. RAS Oncogenes: Weaving A Tumorigenic Web. Nature Reviews Cancer. 2011;11:761–74. [CrossRef]
- Mukhopadhyay S, Vander Heiden MG, McCormick F. The Metabolic Landscape Of RAS-Driven Cancers From Biology To Therapy. Nature Cancer. 2021;2:271–83. [CrossRef]
- Moss DY, McCann C, Kerr EM. Rerouting The Drug Response: Overcoming Metabolic Adaptation In KRAS-Mutant Cancers. Science Signaling. 2022;15:eabj3490. [CrossRef]
- Holmström KM, Kostov R V., Dinkova-Kostova AT. The Multifaceted Role Of Nrf2 In Mitochondrial Function. Current Opinion in Toxicology. 2016;2:80–91. [CrossRef]
- Nisr RB, Shah DS, Ganley IG, Hundal HS. Proinflammatory NFkB Signalling Promotes Mitochondrial Dysfunction In Skeletal Muscle In Response To Cellular Fuel Overloading. Cellular and Molecular Life Sciences. 2019;76:4887–904. [CrossRef]
- Demory ML, Boerner JL, Davidson R, Faust W, Miyake T, Lee I, Hüttemann M, Douglas R, Haddad G, Parsons SJ. Epidermal Growth Factor Receptor Translocation To The Mitochondria. Journal of Biological Chemistry. 2009;284:36592–604. [CrossRef]
- Logan S, Pharaoh GA, Marlin MC, Masser DR, Matsuzaki S, Wronowski B, Yeganeh A, Parks EE, Premkumar P, Farley JA, Owen DB, Humphries KM, Kinter M, Freeman WM, Szweda LI, Van Remmen H, Sonntag WE. Insulin-Like Growth Factor Receptor Signaling Regulates Working Memory, Mitochondrial Metabolism, And Amyloid-β Uptake In Astrocytes. Molecular Metabolism. 2018;9:141–55. [CrossRef]
- Grazette LP, Boecker W, Matsui T, Semigran M, Force TL, Hajjar RJ, Rosenzweig A. Inhibition Of ErbB2 Causes Mitochondrial Dysfunction In Cardiomyocytes: Implications For Herceptin-Induced Cardiomyopathy. Journal of the American College of Cardiology. 2004;44:2231–8. [CrossRef]
- Bui T, Thompson CB. Cancer’s Sweet Tooth. Cancer Cell. 2006;9:419–20.
- Kim JW, Tchernyshyov I, Semenza GL, Dang C V. HIF-1-Mediated Expression Of Pyruvate Dehydrogenase Kinase: A Metabolic Switch Required For Cellular Adaptation To Hypoxia. Cell Metabolism. 2006;3:177–85. [CrossRef]
- Papandreou I, Cairns RA, Fontana L, Lim AL, Denko NC. HIF-1 Mediates Adaptation To Hypoxia By Actively Downregulating Mitochondrial Oxygen Consumption. Cell Metabolism. 2006;3:187–97. [CrossRef]
- Wasylenko TM, Ahn WS, Stephanopoulos G. The Oxidative Pentose Phosphate Pathway Is The Primary Source Of NADPH For Lipid Overproduction From Glucose In Yarrowia Lipolytica. Metabolic Engineering. 2015;30:27–39. [CrossRef]
- De Preter G, Neveu MA, Danhier P, Brisson L, Payen VL, Porporato PE, Jordan BF, Sonveaux P, Gallez B. Inhibition Of The Pentose Phosphate Pathway By Dichloroacetate Unravels A Missing Link Between Aerobic Glycolysis And Cancer Cell Proliferation. Oncotarget. 2016;7:2910–20. [CrossRef]
- DeBerardinis RJ, Mancuso A, Daikhin E, Nissim I, Yudkoff M, Wehrli S, Thompson CB. Beyond Aerobic Glycolysis: Transformed Cells Can Engage In Glutamine Metabolism That Exceeds The Requirement For Protein And Nucleotide Synthesis. Proceedings of the National Academy of Sciences of the United States of America. 2007;104:19345–50. [CrossRef]
- Locasale JW et al. Phosphoglycerate Dehydrogenase Diverts Glycolytic Flux And Contributes To Oncogenesis. Nature Genetics. 2011;43:869–74. [CrossRef]
- Luengo A, Li Z, Gui DY, Sullivan LB, Zagorulya M, Spranger S, Matheson NJ, Heiden MG Vander. Increased Demand For NAD+ Relative To ATP Drives Aerobic Glycolysis. BioRxiv. 2020:1–58. [CrossRef]
- White KA, Grillo-Hill BK, Barber DL. Cancer Cell Behaviors Mediated By Dysregulated PH Dynamics At A Glance. Journal of Cell Science. 2017;130:663–9. [CrossRef]
- Luengo A, Li Z, Gui DY, Sullivan LB, Zagorulya M, Do BT, Ferreira R, Naamati A, Ali A, Lewis CA, Thomas CJ, Spranger S, Matheson NJ, Vander Heiden MG. Increased Demand For NAD+ Relative To ATP Drives Aerobic Glycolysis. Molecular Cell. 2020:1–17. [CrossRef]
- Heiden MGV the warburg effect: T metabolic requirements of cell proliferation, Cantley LC, Thompson CB. Understanding The Warburg Effect: The Metabolic Requirements Of Cell Proliferation. Science. 2009;324:1029–33. [CrossRef]
- Kondoh H, Lleonart ME, Nakashima Y, Yokode M, Tanaka M, Bernard D, Gil J, Beach D. A High Glycolytic Flux Supports The Proliferative Potential Of Murine Embryonic Stem Cells. Antioxidants & Redox Signaling. 2006;0:061221112325011.
- Ciavardelli D, Rossi C, Barcaroli D, Volpe S, Consalvo A, Zucchelli M, De Cola A, Scavo E, Carollo R, D’Agostino D, Forlì F, D’Aguanno S, Todaro M, Stassi G, Di Ilio C, De Laurenzi V, Urbani A. Breast Cancer Stem Cells Rely On Fermentative Glycolysis And Are Sensitive To 2-Deoxyglucose Treatment. Cell Death and Disease. 2014;5:1–12. [CrossRef]
- Ravera S, Podestà M, Sabatini F, Fresia C, Columbaro M, Bruno S, Fulcheri E, Ramenghi LA, Frassoni F. Mesenchymal Stem Cells From Preterm To Term Newborns Undergo A Significant Switch From Anaerobic Glycolysis To The Oxidative Phosphorylation. Cellular and Molecular Life Sciences. 2018;75:889–903. [CrossRef]
- Da Veiga Moreira J, Hamraz M, Abolhassani M, Bigan E, Pérès S, Paulevé L, Nogueira ML, Steyaert JM, Schwartz L. The Redox Status Of Cancer Cells Supports Mechanisms Behind The Warburg Effect. Metabolites. 2016;6:1–12. [CrossRef]
- Pouysségur J, Franchi A, L’Allemain G, Paris S. Cytoplasmic PH, A Key Determinant Of Growth Factor-Induced DNA Synthesis In Quiescent Fibroblasts. FEBS Letters. 1985;190:115–9.
- Aerts RJ, Durston AJ, Moolenaar WH. Cytoplasmic PH And The Regulation Of The Dictyostelium Cell Cycle. Cell. 1985;43:653–7. [CrossRef]
- Birkeland ES, Koch LM, Dechant R. Another Consequence Of The Warburg Effect? Metabolic Regulation Of Na+/H+ Exchangers May Link Aerobic Glycolysis To Cell Growth. Frontiers in Oncology. 2020;10:1–9.
- Calderón Montaño J, Burgos Morón E, Pérez Guerrero M, Salvador Bofill F, Robles Frías A, López Lázaro M. Role Of The Intracellular PH In The Metabolic Switch Between Oxidative Phosphorylation And AerobicGlycolysis - Relevance To Cancer 2011:1–10.
- Icard P, Shulman S, Farhat D, Steyaert JM, Alifano M, Lincet H. How The Warburg Effect Supports Aggressiveness And Drug Resistance Of Cancer Cells? Drug Resistance Updates. 2018;38:1–11.
- Alreshidi MM, Dunstan RH, Gottfries J, Macdonald MM, Crompton MJ, Ang CS, Williamson NA, Roberts TK. Changes In The Cytoplasmic Composition Of Amino Acids And Proteins Observed In Staphylococcus Aureus During Growth Under Variable Growth Conditions Representative Of The Human Wound Site. PLoS ONE. 2016;11:1–19.
- Reshkin SJ, Bellizzi A, Caldeira S, Albarani V, Malanchi I, Poignee M, Alunni-Fabbroni M, Casavola V, Tommasino M. Na + /H + Exchanger-dependent Intracellular Alkalinization Is An Early Event In Malignant Transformation And Plays An Essential Role In The Development Of Subsequent Transformation-associated Phenotypes. The FASEB Journal. 2000;14:2185–97.
- Riddle SR, Ahmad A, Ahmad S, Deeb SS, Malkki M, Schneider BK, Allen CB, White CW. Hypoxia Induces Hexokinase II Gene Expression Inhuman Lung Cell Line A549. American Journal of Physiology - Lung Cellular and Molecular Physiology. 2000;278:L407–16.
- Bergeron M, Yu AY, Solway KE, Semenza GL, Sharp FR. Induction Of Hypoxia-Inducible Factor-1 (HIF-1) And Its Target Genes Following Focal Ischaemia In Rat Brain. European Journal of Neuroscience. 1999;11:4159–70.
- Cota-Ruiz K, Leyva-Carrillo L, Peregrino-Uriarte AB, Valenzuela-Soto EM, Gollas-Galván T, Gómez-Jiménez S, Hernández J, Yepiz-Plascencia G. Role Of HIF-1 On Phosphofructokinase And Fructose 1, 6-Bisphosphatase Expression During Hypoxia In The White Shrimp Litopenaeus Vannamei. Comparative Biochemistry and Physiology -Part A : Molecular and Integrative Physiology. 2016;198:1–7.
- Pelletier J, Bellot G, Gounon P, Lacas-Gervais S, Pouysségur J, Mazure NM. Glycogen Synthesis Is Induced In Hypoxia By The Hypoxia-Inducible Factor And Promotes Cancer Cell Survival. Frontiers in Oncology. 2012;2:1–9. [CrossRef]
- Semenza GL, Jiang BH, Leung SW, Passantino R, Concordat JP, Maire P, Giallongo A. Hypoxia Response Elements In The Aldolase A, Enolase 1, And Lactate Dehydrogenase A Gene Promoters Contain Essential Binding Sites For Hypoxia-Inducible Factor 1. Journal of Biological Chemistry. 1996;271:32529–37. [CrossRef]
- Wigfield SM, Winter SC, Giatromanolaki A, Taylor J, Koukourakis ML, Harris AL. PDK-1 Regulates Lactate Production In Hypoxia And Is Associated With Poor Prognosis In Head And Neck Squamous Cancer. British Journal of Cancer. 2008;98:1975–84. [CrossRef]
- Rosafio K, Pellerin L. Oxygen Tension Controls The Expression Of The Monocarboxylate Transporter MCT4 In Cultured Mouse Cortical Astrocytes Via A Hypoxia-Inducible Factor-1α-Mediated Transcriptional Regulation. Glia. 2014;62:477–90. [CrossRef]
- McClelland GB, Brooks GA. Changes In MCT 1, MCT 4, And LDH Expression Are Tissue Specific In Rats After Long-Term Hypobaric Hypoxia. Journal of Applied Physiology. 2002;92:1573–84. [CrossRef]
- Ullah MS, Davies AJ, Halestrap AP. The Plasma Membrane Lactate Transporter MCT4, But Not MCT1, Is Up-Regulated By Hypoxia Through A HIF-1α-Dependent Mechanism. Journal of Biological Chemistry. 2006;281:9030–7.
- Baumann MU, Zamudio S, Illsley NP. Hypoxic Upregulation Of Glucose Transporters In BeWo Choriocarcinoma Cells Is Mediated By Hypoxia-Inducible Factor-1. American Journal of Physiology - Cell Physiology. 2007;293:477–85. [CrossRef]
- Hervouet E, Cízková A, Demont J, Vojtísková A, Pecina P, Franssen-van Hal NLW, Keijer J, Simonnet H, Ivének R, Kmoch S, Godinot C, Houstek J. HIF And Reactive Oxygen Species Regulate Oxidative Phosphorylation In Cancer. Carcinogenesis. 2008;29:1528–37. [CrossRef]
- Hervouet E, Demont J, Pecina P, Vojtísková A, Houstek J, Simonnet H, Godinot C. A New Role For The Von Hippel-Lindau Tumor Suppressor Protein: Stimulation Of Mitochondrial Oxidative Phosphorylation Complex Biogenesis. Carcinogenesis. 2005;26:531–9. [CrossRef]
- Fukuda R, Zhang H, Kim J whan, Shimoda L, Dang C V., Semenza GLL. HIF-1 Regulates Cytochrome Oxidase Subunits To Optimize Efficiency Of Respiration In Hypoxic Cells. Cell. 2007;129:111–22. [CrossRef]
- Kang JH, Lee SH, Lee JS, Nam B, Seong TW, Son J, Jang H, Hong KM, Lee C, Kim SY. Aldehyde Dehydrogenase Inhibition Combined With Phenformin Treatment Reversed NSCLC Through ATP Depletion. Oncotarget. 2016;7:49397–410. [CrossRef]
- Kang JH, Lee SH, Hong D, Lee JS, Ahn HS, Ahn JH, Seong TW, Lee CH, Jang H, Hong KM, Lee C, Lee JH, Kim SY. Aldehyde Dehydrogenase Is Used By Cancer Cells For Energy Metabolism. Experimental & Molecular Medicine. 2016;48:e272. [CrossRef]
- Hong SM, Hwang SW, Wang T, Park CW, Ryu YM, Jung JH, Shin JH, Kim SY, Lee JL, Kim CW, Yoon G, Kim KH, Myung SJ, Choi KY. Increased Nicotinamide Adenine Dinucleotide Pool Promotes Colon Cancer Progression By Suppressing Reactive Oxygen Species Level. Cancer Science. 2019;110:629–38. [CrossRef]
- Rempel A, Mathupala SP, Griffin CA, Hawkins AL, Pedersen PL. Glucose Catabolism In Cancer Cells: Amplification Of The Gene Encoding Type II Hexokinase. Cancer Research. 1996;56:2468–71.
- Chen Z, Zhang H, Lu W, Huang P. Role Of Mitochondria-Associated Hexokinase II In Cancer Cell Death Induced By 3-Bromopyruvate. Biochimica et Biophysica Acta - Bioenergetics. 2009;1787:553–60. [CrossRef]
- Anderson M, Marayati R, Moffitt R, Yeh JJ. Hexokinase 2 Promotes Tumor Growth And Metastasis By Regulating Lactate Production In Pancreatic Cancer. Oncotarget. 2017;8:56081–94. [CrossRef]
- Yi W, Clark PM, Mason DE, Keenan MC, Hill C, William A, Iii G, Peters EC, Driggers EM, Hsieh-wilson LC. PFK1 Glycosylation Is A Key Regulator Of Cancer Cell Growth And Central Metabolic Pathways Wen. Science. 2013;337:975–80.
- Zancan P, Sola-Penna M, Furtado CM, Da Silva D. Differential Expression Of Phosphofructokinase-1 Isoforms Correlates With The Glycolytic Efficiency Of Breast Cancer Cells. Molecular Genetics and Metabolism. 2010;100:372–8. [CrossRef]
- Sun CM, Xiong DB, Yan Y, Geng J, Liu M, Yao XD. Genetic Alteration In Phosphofructokinase Family Promotes Growth Of Muscle-Invasive Bladder Cancer. International Journal of Biological Markers. 2016;31:e286–93. [CrossRef]
- Mazurek S, Boschek CB, Hugo F, Eigenbrodt E. Pyruvate Kinase Type M2 And Its Role In Tumor Growth And Spreading. Seminars in Cancer Biology. 2005;15:300–8. [CrossRef]
- Prakasam G, Iqbal MA, Bamezai RNK, Mazurek S. Posttranslational Modifications Of Pyruvate Kinase M2: Tweaks That Benefit Cancer. Frontiers in Oncology. 2018;8:1–12. [CrossRef]
- Zahra K, Dey T, Ashish, Mishra SP, Pandey U. Pyruvate Kinase M2 And Cancer: The Role Of PKM2 In Promoting Tumorigenesis. Frontiers in Oncology. 2020;10:1–9. [CrossRef]
- Shiroki T, Yokoyama M, Tanuma N, Maejima R, Tamai K, Yamaguchi K, Oikawa T, Noguchi T, Miura K, Fujiya T, Shima H, Sato I, Murata-Kamiya N, Hatakeyama M, Iijima K, Shimosegawa T, Satoh K. Enhanced Expression Of The M2 Isoform Of Pyruvate Kinase Is Involved In Gastric Cancer Development By Regulating Cancer-Specific Metabolism. Cancer Science. 2017;108:931–40. [CrossRef]
- Kolobova E, Tuganova A, Boulatnikov I, Popov KM. Regulation Of Pyruvate Dehydrogenase Activity Through Phosphorylation At Multiple Sites. Biochemistry. 2001;77:69–77.
- Dai ZJ, Pan S, Chen C, Cao L, Li X, Chen X, Su X, Lin S. Down-Regulation Of Succinate Dehydrogenase Subunit B And Up-Regulation Of Pyruvate Dehydrogenase Kinase 1 Predicts Poor Prognosis In Recurrent Nasopharyngeal Carcinoma. Tumor Biology. 2016;37:5145–52. [CrossRef]
- Wang JJ, Siu MK, Jiang YX, Leung TH, Chan DW, Cheng RR, Cheung AN, Ngan HY, Chan KK. Aberrant Upregulation Of PDK1 In Ovarian Cancer Cells Impairs CD8+ T Cell Function And Survival Through Elevation Of PD-L1. OncoImmunology. 2019;8. [CrossRef]
- Herzig S, Shaw RJ. AMPK: Guardian Of Metabolism And Mitochondrial Homeostasis. Nature Reviews Molecular Cell Biology. 2018;19:121–35. [CrossRef]
- Hong SP, Leiper FC, Woods A, Carling D, Carlson M. Activation Of Yeast Snf1 And Mammalian AMP-Activated Protein Kinase By Upstream Kinases. Proceedings of the National Academy of Sciences of the United States of America. 2003;100:8839–43. [CrossRef]
- Shaw RJ, Kosmatka M, Bardeesy N, Hurley RL, Witters LA, DePinho RA, Cantley LC. The Tumor Suppressor LKB1 Kinase Directly Activates AMP-Activated Kinase And Regulates Apoptosis In Response To Energy Stress. Proceedings of the National Academy of Sciences of the United States of America. 2004;101:3329–35. [CrossRef]
- Xiao B, Sanders MJ, Underwood E, Heath R, Mayer F V., Carmena D, Jing C, Walker PA, Eccleston JF, Haire LF, Saiu P, Howell SA, Aasland R, Martin SR, Carling D, Gamblin SJ. Structure Of Mammalian AMPK And Its Regulation By ADP. Nature. 2011;472:230–3. [CrossRef]
- Liu Q, Gauthier M, Sun L, Ruderman N, Lodish H. Activation Of AMP-activated Protein Kinase Signaling Pathway By Adiponectin And Insulin In Mouse Adipocytes: Requirement Of Acyl-CoA Synthetases FATP1 And Acsl1 And Association With An Elevation In AMP/ATP Ratio. The FASEB Journal. 2010;24:4229–39. [CrossRef]
- Hardie DG. Molecular Pathways: Is AMPK A Friend Or A Foe In Cancer? Clinical Cancer Research. 2015;21:3836–40.
- Li N, Huang D, Lu N, Luo L. Role Of The LKB1/AMPK Pathway In Tumor Invasion And Metastasis Of Cancer Cells (Review). Oncology Reports. 2015;34:2821–6.
- Yung MMH, Chan DW, Liu VWS, Yao KM, Ngan HYS. Activation Of AMPK Inhibits Cervical Cancer Cell Growth Through AKT/FOXO3a/FOXM1 Signaling Cascade. BMC Cancer. 2013;13. [CrossRef]
- Zhou J, Huang W, Tao R, Ibaragi S, Lan F, Ido Y, Wu X, Alekseyev YO, Lenburg ME, Hu GF, Luo Z. Inactivation Of AMPK Alters Gene Expression And Promotes Growth Of Prostate Cancer Cells. Oncogene. 2009;28:1993–2002. [CrossRef]
- Mack HID, Zheng B, Asara JM, Thomas SM. AMPK-Dependent Phosphorylation Of ULK1 Regulates ATG9 Localization. Autophagy. 2012;8:1197–214. [CrossRef]
- Petherick KJ, Conway OJL, Mpamhanga C, Osborne SA, Kamal A, Saxty B, Ganley IG. Pharmacological Inhibition Of ULK1 Kinase Blocks Mammalian Target Of Rapamycin (MTOR)-Dependent Autophagy. Journal of Biological Chemistry. 2015;290:11376–83.
- Nardo A Di, Wertz MH, Kwiatkowski E, Tsai PT, Leech JD, Greene-Colozzi E, Goto J, Dilsiz P, Talos DM, Clish CB, Kwiatkowski DJ, Sahin M. Neuronal Tsc1/2 Complex Controls Autophagy Through AMPK-Dependent Regulation Of ULK1. Human Molecular Genetics. 2014;23:1–10.
- Faubert B, Boily G, Izreig S, Griss T, Samborska B, Dong Z, Dupuy F, Chambers C, Fuerth BJ, Viollet B, Mamer OA, Avizonis D, Deberardinis RJ, Siegel PM, Jones RG. AMPK Is A Negative Regulator Of The Warburg Effect And Suppresses Tumor Growth In Vivo. Cell Metabolism. 2013;17:113–24. [CrossRef]
- Inoki K, Zhu T, Guan K-LG. TSC2 Mediates Cellular Energy Response To Control Cell Growth And Survival. Cell Press. 2003;115:577–90. [CrossRef]
- Inoki K, Li Y, Zhu T, Wu J, Guan KL. TSC2 Is Phosphorylated And Inhibited By Akt And Suppresses MTOR Signalling. Nature Cell Biology. 2002;4:648–57. [CrossRef]
- Inoki K, Li Y, Xu T, Guan KL. Rheb GTpase Is A Direct Target Of TSC2 GAP Activity And Regulates MTOR Signaling. Genes and Development. 2003;17:1829–34. [CrossRef]
- Sun Q et al. Mammalian Target Of Rapamycin Up-Regulation Of Pyruvate Kinase Isoenzyme Type M2 Is Critical For Aerobic Glycolysis And Tumor Growth. Proceedings of the National Academy of Sciences of the United States of America. 2011;108:4129–34.
- Ling NXY, Kaczmarek A, Hoque A, Davie E, Ngoei KRW, Morrison KR, Smiles WJ, Forte GM, Wang T, Lie S, Dite TA, Langendorf CG, Scott JW, Oakhill JS, Petersen J. MTORC1 Directly Inhibits AMPK To Promote Cell Proliferation Under Nutrient Stress. Nature Metabolism. 2020;2:41–9. [CrossRef]
- Guo X, Li H, Xu H, Woo S, Dong H, Lu F, Lange AJ, Wu C. Glycolysis In The Control Of Blood Glucose Homeostasis. Acta Pharmaceutica Sinica B. 2012;2:358–67. [CrossRef]
- Praiss M, Cerasi E. Immediate And Time-Dependent Effects Of Gluoce An Insulin Release: Differential Calcium Requirements. Acta Endocrinologica. 1988;117:409–16.
- Nesher R, Praiss M, Cerasi E. Immediate And Time-Dependent Effects Of Glucose On Insulin Release: Differential Calcium Requirements. Acta Endocrinologica. 1988;117:409–16. [CrossRef]
- Pottout V, Robertson RP. Secondary B-Cell Failure In Type 2 Diabetes-A Convergence Of Glucotoxicity And Lipotoxicity. Endocrinology. 2002;143:339–42.
- Rossetti L, Shulman GI, Zawalich W, DeFronzo RA. Effect Of Chronic Hyperglycemia On In Vivo Insulin Secretion In Partially Pancreatectomized Rats. Journal of Clinical Investigation. 1987;80:1037–44. [CrossRef]
- Gerber PA, Rutter GA. The Role Of Oxidative Stress And Hypoxia In Pancreatic Beta-Cell Dysfunction In Diabetes Mellitus. Antioxidants and Redox Signaling. 2017;26:501–18.
- Noguchi R, Kubota H, Yugi K, Toyoshima Y, Komori Y, Soga T, Kuroda S. The Selective Control Of Glycolysis, Gluconeogenesis And Glycogenesis By Temporal Insulin Patterns. Molecular Systems Biology. 2013;9:1–12. [CrossRef]
- Bitar MS, Al-Mulla F. ROS Constitute A Convergence Nexus In The Development Of IGF1 Resistance And Impaired Wound Healing In A Rat Model Of Type 2 Diabetes. DMM Disease Models and Mechanisms. 2012;5:375–88. [CrossRef]
- Al-Lahham R, Deford JH, Papaconstantinou J. Mitochondrial-Generated ROS Down Regulates Insulin Signaling Via Activation Of The P38MAPK Stress Response Pathway. Molecular and Cellular Endocrinology. 2016;419:1–11. [CrossRef]
- Ogihara T, Asano T, Katagiri H, Sakoda H, Anai M, Shojima N, Ono H, Fujishiro M, Kushiyama A, Fujita Y, M. F, Kikuchi N, Noguchi I, Aburatani H, Gotoh Y, Komuro T. Oxidative Stress Induces Insulin Resistance By Activating The Nuclear Factor-Kappa B Pathway And Disrupting Normal Subcellular Distribution Of Phosphatidylinositol 3-Kinase. Diabetologia. 2004;47:794–805.
- Newsholme P, Haber EP, Hirabara SM, Rebelato ELO, Procopio J, Morgan D, Oliveira-Emilio HC, Carpinelli AR, Curi R. Diabetes Associated Cell Stress And Dysfunction: Role Of Mitochondrial And Non-Mitochondrial ROS Production And Activity. Journal of Physiology. 2007;583:9–24. [CrossRef]
- Hoeks J, Van Herpen NA, Mensink M, Moonen-Kornips E, Van Beurden D, Hesselink MKC, Schrauwen P. Prolonged Fasting Identifies Skeletal Muscle Mitochondrial Dysfunction As Consequence Rather Than Cause Of Human Insulin Resistance. Diabetes. 2010;59:2117–25. [CrossRef]
- Bonnard C, Durand A, Peyrol S, Chanseaume E, Chauvin MA, Morio B, Vidal H, Rieusset J. Mitochondrial Dysfunction Results From Oxidative Stress In The Skeletal Muscle Of Diet-Induced Insulin-Resistant Mice. Journal of Clinical Investigation. 2008;118:789–800. [CrossRef]
- Mootha VK et al. PGC-1α-Responsive Genes Involved In Oxidative Phosphorylation Are Coordinately Downregulated In Human Diabetes. Nature Genetics. 2003;34:267–73. [CrossRef]
- Asmann YW, Stump CS, Short KR, Coenen-Schimke JM, Guo ZK, Bigelow ML, Nair KS. Skeletal Muscle Mitochondrial Functions, Mitochondrial DNA Copy Numbers, And Gene Transcript Profiles In Type 2 Diabetic And Nondiabetic Subjects At Equal Levels Of Low Or High Insulin And Euglycemia. Diabetes. 2006;55:3309–19. [CrossRef]
- Sparks LM, Xie H, Koza RA, Mynatt R, Hulver MW, Bray GA, Smith SR. A High-Fat Diet Coordinately Downregulates Genes Required For Mitochondrial Oxidative Phosphorylation In Skeletal Muscle. Diabetes. 2005;54:1926–33. [CrossRef]
- Mogensen M, Sahlin K, Fernström M, Glintborg D, Vind BF, Beck-Nielsen H, Højlund K. Mitochondrial Respiration Is Decreased In Skeletal Muscle Of Patients With Type 2 Diabetes. Diabetes. 2007;56:1592–9. [CrossRef]
- Poussin C, Ibberson M, Hall D, Ding J, Soto J, Abel ED, Thorens B. Oxidative Phosphorylation Flexibility In The Liver Of Mice Resistant To High-Fat Diet-Induced Hepatic Steatosis. Diabetes. 2011;60:2216–24. [CrossRef]
- Pospisilik JA, Knauf C, Joza N, Benit P, Orthofer M, Cani PD, Ebersberger I, Nakashima T, Sarao R, Neely G, Esterbauer H, Kozlov A, Kahn CR, Kroemer G, Rustin P, Burcelin R, Penninger JM. Targeted Deletion Of AIF Decreases Mitochondrial Oxidative Phosphorylation And Protects From Obesity And Diabetes. Cell. 2007. [CrossRef]
- Roden M. Muscle Triglycerides And Mitochondrial Function: Possible Mechanisms For The Development Of Type 2 Diabetes. International Journal of Obesity. 2005;29:S111–5. [CrossRef]
- Fazakerley DJ, Minard AY, Krycer JR, Thomas KC, Stöckli J, Harney DJ, Burchfield JG, Maghzal GJ, Caldwell ST, Hartley RC, Stocker R, Murphy MP, James DE. Mitochondrial Oxidative Stress Causes Insulin Resistance Without Disrupting Oxidative Phosphorylation. Journal of Biological Chemistry. 2018;293:7315–28.
- Lewis MT, Kasper JD, Bazil JN, Frisbee JC, Wiseman RW. Quantification Of Mitochondrial Oxidative Phosphorylation In Metabolic Disease: Application To Type 2 Diabetes. International Journal of Molecular Sciences. 2019;20. [CrossRef]
- El-Najjar N, Chatila M, Moukadem H, Vuorela H, Ocker M, Gandesiri M, Schneider-Stock R, Gali-Muhtasib H. Reactive Oxygen Species Mediate Thymoquinone-Induced Apoptosis And Activate ERK And JNK Signaling. Apoptosis. 2010;15:183–95. [CrossRef]
- Schreck R, Rieber P, Baeuerle PA. Reactive Oxygen Intermediates As Apparently Widely Used Messengers In The Activation Of The NF-ΚB Transcription Factor And HIV-1. EMBO Journal. 1991;10:2247–58.
- Gloire G, Legrand-Poels S, Piette J. NF-ΚB Activation By Reactive Oxygen Species: Fifteen Years Later. Biochemical Pharmacology. 2006;72:1493–505.
- Dabrowski A, Boguslowicz C, Dabrowska M, Tribillo I, Gabryelewicz A. Reactive Oxygen Species Activate Mitogen-Activated Protein Kinases In Pancreatic Acinar Cells. Pancreas. 2000;21:376–84. [CrossRef]
- Ringvold HC, Khalil RA. Chapter Six - Protein Kinase C as Regulator of Vascular Smooth Muscle Function and Potential Target in Vascular Disorders. Vascul. Pharmacol., vol. 78, Academic Press; 2017, p. 203–301.
- Bitar MS, Al-Mulla F. Upregulation Of CREM/ICER Suppresses Wound Endothelial CRE-HIF-1α-VEGF-Dependent Signaling And Impairs Angiogenesis In Type 2 Diabetes. DMM Disease Models and Mechanisms. 2015;8:65–80.
- Bitar MS, Wahid S, Mustafa S, Al-Saleh E, Dhaunsi GS, Al-Mulla F. Nitric Oxide Dynamics And Endothelial Dysfunction In Type II Model Of Genetic Diabetes. European Journal of Pharmacology. 2005;511:53–64. [CrossRef]
- Bitar MS, Al-Mulla F. A Defect In Nrf2 Signaling Constitutes A Mechanism For Cellular Stress Hypersensitivity In A Genetic Rat Model Of Type 2 Diabetes. American Journal of Physiology - Endocrinology and Metabolism. 2011;301. [CrossRef]
- Akhter N, Madhoun A, Arefanian H, Wilson A, Kochumon S, Thomas R, Shenouda S, Al-Mulla F, Ahmad R, Sindhu S. Oxidative Stress Induces Expression Of The Toll-Like Receptors (TLRs) 2 And 4 In The Human Peripheral Blood Mononuclear Cells: Implications For Metabolic Inflammation. Cellular Physiology and Biochemistry. 2019;53:1–18. [CrossRef]
- Ben Djoudi Ouadda A, Levy E, Ziv E, Lalonde G, Sané AT, Delvin E, Elchebly M. Increased Hepatic Lipogenesis In Insulin Resistance And Type 2 Diabetes Is Associated With AMPK Signalling Pathway Up-Regulation In Psammomys Obesus. Bioscience Reports. 2009;29:283–92.
- Ji J, Petropavlovskaia M, Khatchadourian A, Patapas J, Makhlin J, Rosenberg L, Maysinger D. Type 2 Diabetes Is Associated With Suppression Of Autophagy And Lipid Accumulation In β-Cells. Journal of Cellular and Molecular Medicine. 2019;23:2890–900. [CrossRef]
- Luo Z, Zhang Y, Li F, He J, Ding H, Yan L, Cheng H. Resistin Induces Insulin Resistance By Both AMPK-Dependent And AMPK-Independent Mechanisms In HepG2 Cells. Endocrine. 2009;36:60–9. [CrossRef]
- Fujii N, Ho RC, Manabe Y, Jessen N, Toyoda T, Holland WL, Summers SA, Hirshman MF, Goodyear LJ. Ablation Of AMP-Activated Protein Kinase α 2 Activity Exacerbates Insulin Resistance Induced By High-Fat Feeding Of Mice. Diabetes. 2008;57:2958–66. [CrossRef]
- Kraegen EW, Saha AK, Preston E, Wilks D, Hoy AJ, Cooney GJ, Ruderman NB. Increased Malonyl-CoA And Diacylglycerol Content And Reduced AMPK Activity Accompany Insulin Resistance Induced By Glucose Infusion In Muscle And Liver Of Rats. American Journal of Physiology - Endocrinology and Metabolism. 2006;290:471–9.
- Lee JM, Seo WY, Song KH, Chanda D, Kim YD, Kim DK, Lee MW, Ryu D, Kim YH, Noh JR, Lee CH, Chiang JYL, Koo SH, Choi HS. AMPK-Dependent Repression Of Hepatic Gluconeogenesis Via Disruption Of CREB·CRTC2 Complex By Orphan Nuclear Receptor Small Heterodimer Partner. Journal of Biological Chemistry. 2010;285:32182–91. [CrossRef]
- Lu J. The Warburg Metabolism Fuels Tumor Metastasis. Cancer and Metastasis Reviews. 2019;38:157–64. [CrossRef]
- Hsu CC, Tseng LM, Lee HC. Role Of Mitochondrial Dysfunction In Cancer Progression. Experimental Biology and Medicine. 2016;241:1281–95. [CrossRef]
- Chaudhary AK, Bhat TA, Kumar S, Kumar A, Kumar R, Underwood W, Koochekpour S, Shourideh M, Yadav N, Dhar S, Chandra D. Mitochondrial Dysfunction-Mediated Apoptosis Resistance Associates With Defective Heat Shock Protein Response In African-American Men With Prostate Cancer. British Journal of Cancer. 2016;114:1090–100. [CrossRef]
- Esner M, Graifer D, Lleonart ME, Lyakhovich A. Targeting Cancer Cells Through Antibiotics-Induced Mitochondrial Dysfunction Requires Autophagy Inhibition. Cancer Letters. 2017;384:60–9. [CrossRef]
- Sun J, Hoshino H, Takaku K, Nakajima O, Muto A, Suzuki H, Tashiro S, Takahashi S, Shibahara S, Alam J, Taketo MM, Yamamoto M, Igarashi K. Hemoprotein Bach1 Regulates Enhancer Availability Of Heme Oxygenase-1 Gene. EMBO Journal. 2002;21:5216–24. [CrossRef]
- Dohi Y, Ikura T, Hoshikawa Y, Katoh Y, Ota K, Nakanome A, Muto A, Omura S, Ohta T, Ito A, Yoshida M, Noda T, Igarashi K. Bach1 Inhibits Oxidative Stress-Induced Cellular Senescence By Impeding P53 Function On Chromatin. Nature Structural and Molecular Biology. 2008;15:1246–54. [CrossRef]
- Lee J et al. Effective Breast Cancer Combination Therapy Targeting BACH1 And Mitochondrial Metabolism. Nature. 2019;568:254–8.
- Pomatto LCD, Davies KJA. The Role Of Declining Adaptive Homeostasis In Ageing. Journal of Physiology. 2017;595:7275–309. [CrossRef]
- Wiel C, Le Gal K, Ibrahim MX, Jahangir CA, Kashif M, Yao H, Ziegler D V., Xu X, Ghosh T, Mondal T, Kanduri C, Lindahl P, Sayin VI, Bergo MO. BACH1 Stabilization By Antioxidants Stimulates Lung Cancer Metastasis. Cell. 2019;178:330-345.e22. [CrossRef]
- Mansoori B, Dehghan R, Duijf P, Mohammadi A. MiR - 142 - 3p As Tumor Suppressor MiRNA In The Regulation Of Tumorigenicity, Invasion And Migration Of Human Breast Cancer By Targeting Bach - 1 Expression 2018.
- Id SS, Mansoori B, Mohammadi A, Shajari N, Duijf PHG, Najafi S. MiR-330 Regulates Colorectal Cancer Oncogenesis By Targeting BACH1. Tabriz University of Medical Sciences. 2020;10:444–51. [CrossRef]
- Zhou L, Zhang H, Davies KJA, Forman HJ. Aging-Related Decline In The Induction Of Nrf2-Regulated Antioxidant Genes In Human Bronchial Epithelial Cells. Redox Biology. 2018;14:35–40. [CrossRef]
- Sun RC, Fadia M, Dahlstrom JE, Parish CR, Board PG, Blackburn AC. Reversal Of The Glycolytic Phenotype By Dichloroacetate Inhibits Metastatic Breast Cancer Cell Growth In Vitro And In Vivo. Breast Cancer Research and Treatment. 2010;120:253–60. [CrossRef]
- De Rosa V, Iommelli F, Monti M, Fonti R, Votta G, Stoppelli MP, Del Vecchio S. Reversal Of Warburg Effect And Reactivation Of Oxidative Phosphorylation By Differential Inhibition Of EGFR Signaling Pathways In Non-Small Cell Lung Cancer. Clinical Cancer Research. 2015;21:5110–20. [CrossRef]
- Zhuang Y, Keith WK. Cell Cycle Arrest In Metformin Treated Breast Cancer Cells Involves Activation Of AMPK, Downregulation Of Cyclin D1, And Requires P27Kip1 Or P21Cip1. Journal of Molecular Signaling. 2008;3:1–11.
- Liang J, Shao SH, Xu ZX, Hennessy B, Ding Z, Larrea M, Kondo S, Dumont DJ, Gutterman JU, Walker CL, Slingerland JM, Mills GB. The Energy Sensing LKB1-AMPK Pathway Regulates P27 Phosphorylation Mediating The Decision To Enter Autophagy Or Apoptosis. Nature Cell Biology. 2007;9:218–24. [CrossRef]
- Yang J, Nie J, Ma X, Wei Y, Peng Y, Wei X. Targeting PI3K In Cancer: Mechanisms And Advances In Clinical Trials. Molecular Cancer. 2019;18:1–28. [CrossRef]
- Khan KH, Wong M, Rihawi K, Bodla S, Morganstein D, Banerji U, Molife LR. Hyperglycemia And Phosphatidylinositol 3-Kinase/Protein Kinase B/Mammalian Target Of Rapamycin (PI3K/AKT/MTOR) Inhibitors In Phase I Trials: Incidence, Predictive Factors, And Management. The Oncologist. 2016;21:855–60. [CrossRef]
- Cui Y, Zhou J, Rong F. Combination Of Metformin And RG7388 Enhances Inhibition Of Growth And Induction Of Apoptosis Of Ovarian Cancer Cells Through The PI3K/AKT/MTOR Pathway. Biochemical and Biophysical Research Communications. 2020;533:665–71. [CrossRef]
- Candido S, Abrams SL, Steelman L, Lertpiriyapong K, Martelli AM, Cocco L, Ratti S, Follo MY, Murata RM, Rosalen PL, Lombardi P, Montalto G, Cervello M, Gizak A, Rakus D, Suh P-G, Libra M, McCubrey JA. Metformin Influences Drug Sensitivity In Pancreatic Cancer Cells. Advances in Biological Regulation. 2018;68:13–30. [CrossRef]
- Cantley LC. The Phosphoinositide 3-Kinase Pathway. Science. 2002;296:1655–7.
- Lennartz MR. Phospholipases And Phagocytosis: The Role Of Phospholipid-Derived Second Messengers In Phagocytosis. The International Journal of Biochemistry & Cell Biology. 1999;31:415–30. [CrossRef]
- Fang Y, Park IH, Wu AL, Du G, Huang P, Frohman MA, Walker SJ, Brown HA, Chen J. PLD1 Regulates MTOR Signaling And Mediates Cdc42 Activation Of S6K1. Current Biology. 2003;13:2037–44. [CrossRef]
- O’neil TK, Duffy LR, Frey JW, Hornberger TA. The Role Of Phosphoinositide 3-Kinase And Phosphatidic Acid In The Regulation Of Mammalian Target Of Rapamycin Following Eccentric Contractions. Journal of Physiology. 2009;587:3691–701. [CrossRef]
- Hong-Brown LQ, Brown CR, Navaratnarajah M, Lang CH. Activation Of AMPK/TSC2/PLD By Alcohol Regulates MTORC1 And MTORC2 Assembly In C2C12 Myocytes. Alcoholism: Clinical and Experimental Research. 2013;37:1849–61.
- Standaert ML, Avignon A, Yamada K, Bandyopadhyay G, Farese R V. The Phosphatidylinositol 3-Kinase Inhibitor, Wortmannin, Inhibits Insulin-Induced Activation Of Phosphatidylcholine Hydrolysis And Associated Protein Kinase C Translocation In Rat Adipocytes. Biochemical Journal. 1996;313:1039–46. [CrossRef]
- Lee JS, Kim JH, Jang IH, Kim HS, Han JM, Kazlauskas A, Yagisawa H, Suh P-G, Ryu SH. Phosphatidylinositol (3,4,5)-Trisphosphate Specifically Interacts With The Phox Homology Domain Of Phospholipase D1 And Stimulates Its Activity. Journal of Cell Science. 2005;118:4405–13. [CrossRef]
- Toschi A, Lee E, Xu L, Garcia A, Gadir N, Foster DA. Regulation Of MTORC1 And MTORC2 Complex Assembly By Phosphatidic Acid: Competition With Rapamycin. Molecular and Cellular Biology. 2009;29:1411–20. [CrossRef]
- Franke TF, Kaplan DR, Cantley LC, Toker A. Direct Regulation Of The Akt Proto-Oncogene Product By Phosphatidylinositol-3,4-Bisphosphate. Science. 1997;275:665–8.
- Frame S, Cohen P, Biondi RM. A Common Phosphate Binding Site Explains The Unique Substrate Specificity Of GSK3 And Its Inactivation By Phosphorylation. Molecular Cell. 2001;7:1321–7. [CrossRef]
- Salazar M, Rojo AI, Velasco D, de Sagarra RM, Cuadrado A. Glycogen Synthase Kinase-3β Inhibits The Xenobiotic And Antioxidant Cell Response By Direct Phosphorylation And Nuclear Exclusion Of The Transcription Factor Nrf2*. Journal of Biological Chemistry. 2006;281:14841–51. [CrossRef]
- Kensler TW, Wakabayashi N, Biswal S. Cell Survival Responses To Environmental Stresses Via The Keap1-Nrf2-ARE Pathway. Annual Review of Pharmacology and Toxicology. 2007;47:89–116. [CrossRef]
- Wang X-J, Sun Z, Villeneuve NF, Zhang S, Zhao F, Li Y, Chen W, Yi X, Zheng W, Wondrak GT, Wong PK, Zhang DD. Nrf2 Enhances Resistance Of Cancer Cells To Chemotherapeutic Drugs, The Dark Side Of Nrf2. Carcinogenesis. 2008;29:1235–43. [CrossRef]
- Mitsuishi Y, Taguchi K, Kawatani Y, Shibata T, Nukiwa T, Aburatani H, Yamamoto M, Motohashi H. Nrf2 Redirects Glucose And Glutamine Into Anabolic Pathways In Metabolic Reprogramming. Cancer Cell. 2012;22:66–79. [CrossRef]
- DeNicola GM, Karreth FA, Humpton TJ, Gopinathan A, Wei C, Frese K, Mangal D, Yu KH, Yeo CJ, Calhoun ES, Scrimieri F, Winter JM, Hruban RH, Iacobuzio-Donahue C, Kern SE, Blair IA, Tuveson DA. Oncogene-Induced Nrf2 Transcription Promotes ROS Detoxification And Tumorigenesis. Nature. 2011;475:106–9. [CrossRef]
- Wang H et al. NRF2 Activation By Antioxidant Antidiabetic Agents Accelerates Tumor Metastasis. Science Translational Medicine. 2016;8:334ra51-334ra51.
- Padmanabhan B, Tong KI, Ohta T, Nakamura Y, Scharlock M, Ohtsuji M, Kang M-I, Kobayashi A, Yokoyama S, Yamamoto M. Structural Basis For Defects Of Keap1 Activity Provoked By Its Point Mutations In Lung Cancer. Molecular Cell. 2006;21:689–700. [CrossRef]
- Mukhopadhyay S, Goswami D, Adiseshaiah PP, Burgan W, Yi M, Guerin TM, Kozlov S V, Nissley D V, McCormick F. Undermining Glutaminolysis Bolsters Chemotherapy While NRF2 Promotes Chemoresistance In KRAS-Driven Pancreatic Cancers. Cancer Research. 2020;80:1630–43.
- Hayes JD, Dinkova-Kostova AT. The Nrf2 Regulatory Network Provides An Interface Between Redox And Intermediary Metabolism. Trends in Biochemical Sciences. 2014;39:199–218. [CrossRef]
- Taguchi K, Motohashi H, Yamamoto M. Molecular Mechanisms Of The Keap1–Nrf2 Pathway In Stress Response And Cancer Evolution. Genes to Cells. 2011;16:123–40. [CrossRef]
- Joza N, Oudit GY, Brown D, Bénit P, Kassiri Z, Vahsen N, Benoit L, Patel MM, Nowikovsky K, Vassault A, Backx PH, Wada T, Kroemer G, Rustin P, Penninger JM. Muscle-Specific Loss Of Apoptosis-Inducing Factor Leads To Mitochondrial Dysfunction, Skeletal Muscle Atrophy, And Dilated Cardiomyopathy. Molecular and Cellular Biology. 2005;25:10261–72. [CrossRef]
- Susin SA, Lorenzo HK, Zamzami N, Marzo I, Snow BE, Brothers GM, Mangion J, Jacotot E, Costantini P, Loef¯er M, Larochette N, Goodlett DR, Aebersold R, Siderovski DP, M.Penninger J, Kroemer G. Molecular Characterization Of Mitochondrial Apoptosis-Inducing Factor. Letters to Nature. 1999;353:441–6.
- Vahsen N et al. AIF Deficiency Compromises Oxidative Phosphorylation. EMBO Journal. 2004;23:4679–89. [CrossRef]
- Cheung ECC, Joza N, Steenaart NAE, McClellan KA, Neuspiel M, McNamara S, MacLaurin JG, Rippstein P, Park DS, Shore GC, McBride HM, Penninger JM, Slack RS. Dissociating The Dual Roles Of Apoptosis-Inducing Factor In Maintaining Mitochondrial Structure And Apoptosis. EMBO Journal. 2006;25:4061–73. [CrossRef]
- Berg J, Tymoczko J, Stryer L. Gluconeogenesis and Glycolysis Are Reciprocally Regulated. In: Freeman WH, editor. Biochemistry. fifth, New York: 2002, p. 1–4.
- Pizarro-Delgado J, Deeney JT, Corkey BE, Tamarit-Rodriguez J. Direct Stimulation Of Islet Insulin Secretion By Glycolytic And Mitochondrial Metabolites In KCL-Depolarized Islets. PLoS ONE. 2016;11:1–18.
- OWEN MR, DORAN E, HALESTRAP AP. Evidence That Metformin Exerts Its Anti-Diabetic Effects Through Inhibition Of Complex 1 Of The Mitochondrial Respiratory Chain. Biochemical Journal. 2000;348:607–14.
- Wheaton WW, Weinberg SE, Hamanaka RB, Soberanes S, Sullivan LB, Anso E, Glasauer A, Dufour E, Mutlu GM, Scott Budigner GR, Chandel NS. Metformin Inhibits Mitochondrial Complex I Of Cancer Cells To Reduce Tumorigenesis. ELife. 2014;2014:1–18.
- Anedda A, Rial E, Gonza MM. Metformin Induces Oxidative Stress In White Adipocytes And Raises Uncoupling Protein 2 Levels. Journal of Endocrinology. 2008;199:33–40. [CrossRef]
- Huang X, Liu G, Guo J, Su ZQ. The PI3K/AKT Pathway In Obesity And Type 2 Diabetes. International Journal of Biological Sciences. 2018;14:1483–96. [CrossRef]
- Kousteni S. FoxO1, The Transcriptional Chief Of Staff Of Energy Metabolism. Bone. 2012;50:437–43.
- O-Sullivan I, Zhang W, Wasserman DH, Liew CW, Liu J, Paik J, Depinho RA, Stolz DB, Kahn CR, Schwartz MW, Unterman TG. FoxO1 Integrates Direct And Indirect Effects Of Insulin On Hepatic Glucose Production And Glucose Utilization. Nature Communications. 2015;6. [CrossRef]
- Hay N. Interplay Between FOXO, TOR, And Akt. Biochimica et Biophysica Acta - Molecular Cell Research. 2011;1813:1965–70.
- Cross DAE, Alessi DR, Cohen P, Andjelkovich M, Hemmings BA. Inhibition Of Glycogen Synthase Kinase-3 By Insulin Mediated By Protein Kinase B. Nature. 1995;378:785–9. [CrossRef]
- Krycer JR, Sharpe LJ, Luu W, Brown AJ. The Akt-SREBP Nexus: Cell Signaling Meets Lipid Metabolism. Trends in Endocrinology and Metabolism. 2010;21:268–76.
- Ortega-Molina A, Lopez-Guadamillas E, Mattison JA, Mitchell SJ, Muñoz-Martin M, Iglesias G, Gutierrez VM, Vaughan KL, Szarowicz MD, González-García I, López M, Cebrián D, Martinez S, Pastor J, De Cabo R, Serrano M. Pharmacological Inhibition Of PI3K Reduces Adiposity And Metabolic Syndrome In Obese Mice And Rhesus Monkeys. Cell Metabolism. 2015;21:558–70. [CrossRef]
- Wang C et al. FAM3A Activates PI3K P110$α$/Akt Signaling To Ameliorate Hepatic Gluconeogenesis And Lipogenesis. Hepatology. 2014;59:1779–90.
- Golbidi S, Badran M, Laher I. Diabetes And Alpha Lipoic Acid. Frontiers in Pharmacology. 2011;2 NOV:1–15. [CrossRef]
- Schwartz L, Seyfried T, Alfarouk KO, Da Veiga Moreira J, Fais S. Out Of Warburg Effect: An Effective Cancer Treatment Targeting The Tumor Specific Metabolism And Dysregulated PH. Seminars in Cancer Biology. 2017;43:134–8. [CrossRef]
- Babu PVA, Liu D, Gilbert ER. Recent Advances In Understanding The Anti-Diabetic Actions Of Dietary Flavonoids. Journal of Nutritional Biochemistry. 2013;24:1777–89. [CrossRef]
- Sak K. Cytotoxicity Of Dietary Flavonoids On Diffeernt Human Cancer Types. Pharmacognosy Review. 2014;8:1–36.
- Feuerecker B, Pirsig S, Seidl C, Aichler M, Feuchtinger A, Bruchelt G, Senekowitsch-Schmidtke R. Lipoic Acid Inhibits Cell Proliferation Of Tumor Cells In Vitro And In Vivo. Cancer Biology and Therapy. 2012;13:1425–35. [CrossRef]
- Na MH, Seo EY, Kim WK. Effects Of α-Lipoic Acid On Cell Proliferation And Apoptosis In MDA-MB-231 Human Breast Cells. Nutrition Research and Practice. 2009;3:265. [CrossRef]
- Jeon MJ, Kim WG, Lim S, Choi HJ, Sim S, Kim TY, Shong YK, Kim WB. Alpha Lipoic Acid Inhibits Proliferation And Epithelial Mesenchymal Transition Of Thyroid Cancer Cells. Molecular and Cellular Endocrinology. 2016;419:113–23. [CrossRef]
- Konrad T, Vicini P, Kusterer K, Höflich A, Assadkhani A, Böhles HJ, Sewell A, Tritschler HJ, Cobelli C, Usadel KH. A-Lipoic Acid Treatment Decreases Serum Lactate And Pyruvate Concentrations And Improves Glucose Effectiveness In Lean And Obese Patients With Type 2 Diabetes. Diabetes Care. 1999;22:280–7.
- Korotchkina LG, Sidhu S, Patel MS. R-Lipoic Acid Inhibits Mammalian Pyruvate Dehydrogenase Kinase. Free Radical Research. 2004;38:1083–92. [CrossRef]
- Gandhi VM, Wagh SS, Natraj C V., Menon KKG. Lipoic Acid And Diabetes II: Mode Of Action Of Lipoic Acid. Journal of Biosciences. 1985;9:117–27. [CrossRef]
- Wenzel U, Nickel A, Daniel H. α-Lipoic Acid Induces Apoptosis In Human Colon Cancer Cells By Increasing Mitochondrial Respiration With A Concomitant O2-.-Generation. Apoptosis. 2005;10:359–68.
- Mantovani G, Macciò A, Madeddu C, Mura L, Gramignano G, Lusso MR, Murgia V, Camboni P, Ferreli L, Mocci M, Massa E. The Impact Of Different Antioxidant Agents Alone Or In Combination On Reactive Oxygen Species, Antioxidant Enyzmes And Cytokines In A Series Of Advanced Cancer Patients At Different Sites: Correlation With Disease Progression. Free Radical Research. 2003;37:213–23.
- Mantovani G, Macciò A, Madeddu C, Mura L, Massa E, Gramignano G, Lusso MR, Murgia V, Camboni P, Ferreli L. Reactive Oxygen Species, Antioxidant Mechanisms And Serum Cytokine Levels In Cancer Patients: Impact Of An Antioxidant Treatment. Journal of Cellular and Molecular Medicine. 2002;6:570–82. [CrossRef]
- Dörsam B, Fahrer J. The Disulfide Compound α-Lipoic Acid And Its Derivatives: A Novel Class Of Anticancer Agents Targeting Mitochondria. Cancer Letters. 2016;371:12–9. [CrossRef]
- Dörsam B, Göder A, Seiwert N, Kaina B, Fahrer J. Lipoic Acid Induces P53-Independent Cell Death In Colorectal Cancer Cells And Potentiates The Cytotoxicity Of 5-Fluorouracil. Archives of Toxicology. 2015;89:1829–46. [CrossRef]
- Kafara P, Icard P, Guillamin M, Schwartz L, Lincet H. Lipoic Acid Decreases Mcl-1, Bcl-XL And Up Regulates Bim On Ovarian Carcinoma Cells Leading To Cell Death. Journal of Ovarian Research. 2015;8:1–13.
- Piotrowski P, Wierzbicka K, Śmiałek M. Neuronal Death In The Rat Hippocampus In Experimental Diabetes And Cerebral Ischaemia Treated With Antioxidants. Folia Neuropathologica. 2001;39:147–54.
- Pierce RH, Campbell JS, Stephenson AB, Franklin CC, Chaisson M, Poot M, Kavanagh TJ, Rabinovitch PS, Fausto N. Disruption Of Redox Homeostasis In Tumor Necrosis Factor-Induced Apoptosis In A Murine Hepatocyte Cell Line. American Journal of Pathology. 2000;157:221–36. [CrossRef]
- Lin HY, Han HW, Sun WX, Yang YS, Tang CY, Lu GH, Qi JL, Wang XM, Yang YH. Design And Characterization Of α-Lipoic Acyl Shikonin Ester Twin Drugs As Tubulin And PDK1 Dual Inhibitors. European Journal of Medicinal Chemistry. 2018;144:137–50. [CrossRef]
- Shen QW, Zhu MJ, Tong J, Ren J, Du M. Ca2+/Calmodulin-Dependent Protein Kinase Kinase Is Involved In AMP-Activated Protein Kinase Activation By α-Lipoic Acid In C2C12 Myotubes. American Journal of Physiology - Cell Physiology. 2007;293:1395–403.
- Dozio E, Ruscica M, Passafaro L, Dogliotti G, Steffani L, Pagani A, Demartini G, Esposti D, Fraschini F, Magni P. The Natural Antioxidant Alpha-Lipoic Acid Induces P27Kip1-Dependent Cell Cycle Arrest And Apoptosis In MCF-7 Human Breast Cancer Cells. European Journal of Pharmacology. 2010;641:29–34. [CrossRef]
- Yadav VR, Prasad S, Sung B, Kannappan R, Aggarwal BB. Targeting Inflammatory Pathways By Triterpenoids For Prevention And Treatment Of Cancer. Toxins. 2010;2:2428–66. [CrossRef]
- Wei J, Huang Q, Bai F, Lin J, Nie J, Lu S, Lu C, Huang R, Lu Z, Lin X. Didymin Induces Apoptosis Through Mitochondrial Dysfunction And Up-Regulation Of RKIP In Human Hepatoma Cells. Chemico-Biological Interactions. 2017;261:118–26. [CrossRef]
- Zhao Y, Zhou Y, Wang M. Brosimone I, An Isoprenoid-Substituted Flavonoid, Induces Cell Cycle G1 Phase Arrest And Apoptosis Through ROS-Dependent Endoplasmic Reticulum Stress In HCT116 Human Colon Cancer Cells. Food and Function. 2019;10:2729–38.
- Al-Mulla F. Novel Flavonoid Didymin Inhibits Neuroblastomas - Letter. Cancer Prevention Research. 2012;5:883. [CrossRef]
- Kyriakis E, Stravodimos GA, Kantsadi AL, Chatzileontiadou DSM, Skamnaki VT, Leonidas DD. Natural Flavonoids As Antidiabetic Agents. The Binding Of Gallic And Ellagic Acids To Glycogen Phosphorylase B. FEBS Letters. 2015;589:1787–94. [CrossRef]
- Samec M et al. Flavonoids Against The Warburg Phenotype—Concepts Of Predictive, Preventive And Personalised Medicine To Cut The Gordian Knot Of Cancer Cell Metabolism. EPMA Journal. 2020;11:377–98. [CrossRef]
- Shan S, Shi J, Yang P, Jia B, Wu H, Zhang X, Li Z. Apigenin Restrains Colon Cancer Cell Proliferation Via Targeted Blocking Of Pyruvate Kinase M2-Dependent Glycolysis. Journal of Agricultural and Food Chemistry. 2017;65:8136–44. [CrossRef]
- Wei R, Mao L, Xu P, Zheng X, Hackman RM, MacKenzie GG, Wang Y. Suppressing Glucose Metabolism With Epigallocatechin-3-Gallate (EGCG) Reduces Breast Cancer Cell Growth In Preclinical Models. Food and Function. 2018;9:5682–96. [CrossRef]
- Feng J, Wu L, Ji J, Chen K, Yu Q, Zhang J, Chen J, Mao Y, Wang F, Dai W, Xu L, Wu J, Guo C. PKM2 Is The Target Of Proanthocyanidin B2 During The Inhibition Of Hepatocellular Carcinoma. Journal of Experimental and Clinical Cancer Research. 2019;38:1–15. [CrossRef]
- Chen J, Xie J, Jiang Z, Wang B, Wang Y, Hu X. Shikonin And Its Analogs Inhibit Cancer Cell Glycolysis By Targeting Tumor Pyruvate Kinase-M2. Oncogene. 2011;30:4297–306. [CrossRef]
- Zhao X, Zhu Y, Hu J, Jiang L, Li L, Jia S, Zen K. Shikonin Inhibits Tumor Growth In Mice By Suppressing Pyruvate Kinase M2-Mediated Aerobic Glycolysis. Scientific Reports. 2018;8:1–8. [CrossRef]
- Jia L, Huang S, Yin X, Zan Y, Guo Y, Han L. Quercetin Suppresses The Mobility Of Breast Cancer By Suppressing Glycolysis Through Akt-MTOR Pathway Mediated Autophagy Induction. Life Sciences. 2018;208:123–30.
- Liu W, Li W, Liu H, Yu X. Xanthohumol Inhibits Colorectal Cancer Cells Via Downregulation Of Hexokinases Ii-Mediated Glycolysis. International Journal of Biological Sciences. 2019;15:2497–508. [CrossRef]
- Deng X, Liu R, Li J, Li Z, Liu J, Xiong R, Lei X, Zheng X, Xie Z, Tang G. Design, Synthesis, And Preliminary Biological Evaluation Of 3′,4′,5′-Trimethoxy Flavonoid Salicylate Derivatives As Potential Anti-Tumor Agents. New Journal of Chemistry. 2019;43:1874–84.
- Guo Y, Wei L, Zhou Y, Lu N, Tang X, Li Z, Wang X. Flavonoid GL-V9 Induces Apoptosis And Inhibits Glycolysis Of Breast Cancer Via Disrupting GSK-3β-Modulated Mitochondrial Binding Of HKII. Free Radical Biology and Medicine. 2020;146:119–29. [CrossRef]
- Zhou Y, Lu N, Qiao C, Ni T, Li Z, Yu B, Guo Q, Wei L. FV-429 Induces Apoptosis And Inhibits Glycolysis By Inhibiting Akt-Mediated Phosphorylation Of Hexokinase II In MDA-MB-231 Cells. Molecular Carcinogenesis. 2016;55:1317–28. [CrossRef]
- Tao L, Liu Y, Ding Y, Liu X, Zhang X, Hu R, Wei L, Wang X, Yao Y, Lu J, Wang Q. Gen-27, a newly synthesized flavonoid, inhibits glycolysis and induces cell apoptosis via suppression of hexokinase II in human breast cancer cells. vol. 125. 2017. [CrossRef]
- Li W, Hao J, Zhang L, Cheng Z, Deng X, Shu G. Astragalin Reduces Hexokinase 2 Through Increasing MiR-125b To Inhibit The Proliferation Of Hepatocellular Carcinoma Cells In Vitro And In Vivo. Journal of Agricultural and Food Chemistry. 2017;65:5961–72. [CrossRef]
- Mazlaghaninia M, Atri MS, Seyedalipour B. Scopoletin And Morin Inhibit Lactate Dehydrogenase Enzyme Activity Is Critical For Cancer Metabolism. Hormozgan Medical Journal. 2019;In Press:1–6. [CrossRef]
- Liu Y, Venna CK, Morgan JB, Mohammed KA, Jekabsons MB, Nagle DG, Zhou YD. Methylalpinumisoflavone Inhibits Hypoxia-Inducible Factor-1 (HIF-1) Activation By Simultaneously Targeting Multiple Pathways. Journal of Biological Chemistry. 2009;284:5859–68. [CrossRef]
- Wei L, Zhou Y, Qiao C, Ni T, Li Z, You Q, Guo Q, Lu N. Oroxylin A Inhibits Glycolysis-Dependent Proliferation Of Human Breast Cancer Via Promoting SIRT3-Mediated SOD2 Transcription And HIF1α Destabilization. Cell Death and Disease. 2015;6:1–12. [CrossRef]
- Chen F, Zhuang M, Zhong C, Peng J, Wang X, Li J, Chen Z, Huang Y. Baicalein Reverses Hypoxia-Induced 5-FU Resistance In Gastric Cancer AGS Cells Through Suppression Of Glycolysis And The PTEN/Akt/HIF-1α Signaling Pathway. Oncology Reports. 2015;33:457–63. [CrossRef]
- Wang H, Zhao L, Zhu LT, Wang Y, Pan D, Yao J, You QD, Guo QL. Wogonin Reverses Hypoxia Resistance Of Human Colon Cancer HCT116 Cells Via Downregulation Of HIF-1α And Glycolysis, By Inhibiting PI3K/Akt Signaling Pathway. Molecular Carcinogenesis. 2014;53:1–12.
- Zhao Y, Zhang L, Wu Y, Dai Q, Zhou Y, Li Z, Yang L, Guo Q, Lu N. Selective Anti-Tumor Activity Of Wogonin Targeting The Warburg Effect Through Stablizing P53. Pharmacological Research. 2018;135:49–59. [CrossRef]
- Li J, Zou Y, Pei M, Zhang Y, Jiang Y. Berberine Inhibits The Warburg Effect Through TET3/MiR-145/HK2 Pathways In Ovarian Cancer Cells. Journal of Cancer. 2021;12:207–16.
- Li Z, Li H, Lu Y, Yang P, Li Z. Berberine Inhibited The Proliferation Of Cancer Cells By Suppressing The Activity Of Tumor Pyruvate Kinase M2. Natural Product Communications. 2017;12:1415–8. [CrossRef]
- Li W, Ma X, Li N, Liu H, Dong Q, Zhang J, Yang C, Liu Y, Liang Q, Zhang S, Xu C, Song W, Tan S, Rong P, Wang W. Resveratrol Inhibits Hexokinases II Mediated Glycolysis In Non-Small Cell Lung Cancer Via Targeting Akt Signaling Pathway. Experimental Cell Research. 2016;349:320–7. [CrossRef]
- Saunier E, Antonio S, Regazzetti A, Auzeil N, Laprévote O, Shay JW, Coumoul X, Barouki R, Benelli C, Huc L, Bortoli S. Resveratrol Reverses The Warburg Effect By Targeting The Pyruvate Dehydrogenase Complex In Colon Cancer Cells. Scientific Reports. 2017;7:1–16. [CrossRef]
- Omidian K, Rafiei H, Bandy B. Increased Mitochondrial Content And Function By Resveratrol And Select Flavonoids Protects Against Benzo[A]Pyrene-Induced Bioenergetic Dysfunction And ROS Generation In A Cell Model Of Neoplastic Transformation. Free Radical Biology and Medicine. 2020;152:767–75. [CrossRef]
- Samec M, Liskova A, Koklesova L, Mersakova S, Strnadel J, Kajo K, Pec M, Zhai K, Smejkal K, Mirzaei S, Hushmandi K, Ashrafizadeh M, Saso L, Brockmueller A, Shakibaei M, Büsselberg D, Kubatka P. Flavonoids Targeting HIF-1: Implications On Cancer Metabolism. Cancers. 2021;13:130. [CrossRef]
- Bisol Â, de Campos PS, Lamers ML. Flavonoids As Anticancer Therapies: A Systematic Review Of Clinical Trials. Phytotherapy Research. 2020;34:568–82. [CrossRef]
- Thilakarathna SH, Vasantha Rupasinghe HP. Flavonoid Bioavailability And Attempts For Bioavailability Enhancement. Nutrients. 2013;5:3367–87. [CrossRef]
- dos Santos Lima B, Shanmugam S, de Souza Siqueira Quintans J, Quintans-Júnior LJ, de Souza Araújo AA. Inclusion Complex With Cyclodextrins Enhances The Bioavailability Of Flavonoid Compounds: A Systematic Review. Phytochemistry Reviews. 2019;18:1337–59. [CrossRef]
- Foretz M, Ancellin N, Andreelli F, Saintillan Y, Grondin P, Kahn A, Thorens B, Vaulont S, Viollet B. Short-Term Overexpression Of A Constitutively Active Form Of AMP-Activated Protein Kinase In The Liver Leads To Mild Hypoglycemia And Fatty Liver. Diabetes. 2005;54:1331–9. [CrossRef]
- Woo JL, Song KH, Eun HK, Jong CW, Hyoun SK, Park HS, Kim MS, Kim SW, Lee KU, Park JY. α-Lipoic Acid Increases Insulin Sensitivity By Activating AMPK In Skeletal Muscle. Biochemical and Biophysical Research Communications. 2005;332:885–91. [CrossRef]
- Gosselin LE, Chrapowitzky L, Rideout TC. Metabolic Effects Of α-Lipoic Acid Supplementation In Pre-Diabetics: A Randomized, Placebo-Controlled Pilot Study. Food and Function. 2019;10:5732–8.
- Kamenova P. Improvement Of Insulin Sensitivity In Patients With Type 2 Diabetes Mellitus After Oral Administration Of Alpha-Lipoic Acid. Hormones. 2006;5:251–8. [CrossRef]
- Ziegler D, Hanefeld M, Ruhnau KJ, Mei\ner HP, Lobisch M, Schütte K, Gries FA. Treatment Of Symptomatic Diabetic Peripheral Neuropathy With The Anti-Oxidant α-Lipoic Acid - A 3-Week Multicentre Randomized Controlled Trial (ALADIN Study). Diabetologia. 1995;38:1425–33.
- Lagouge M, Argmann C, Gerhart-Hines Z, Meziane H, Lerin C, Daussin F, Messadeq N, Milne J, Lambert P, Elliott P, Geny B, Laakso M, Puigserver P, Auwerx J. Resveratrol Improves Mitochondrial Function And Protects Against Metabolic Disease By Activating SIRT1 And PGC-1α. Cell. 2006;127:1109–22. [CrossRef]
- Meng Q, Qi X, Fu Y, Chen Q, Cheng P, Yu X, Sun X, Wu J, Li W, Zhang Q, Li Y, Wang A, Bian H. Flavonoids Extracted From Mulberry (Morus Alba L.) Leaf Improve Skeletal Muscle Mitochondrial Function By Activating AMPK In Type 2 Diabetes. Journal of Ethnopharmacology. 2020;248:112326. [CrossRef]
- Han G, Takahashi H, Murao N, Gheni G, Yokoi N, Hamamoto Y, Asahara S-I, Seino Y, Kido Y, Seino S. Glutamate Is An Essential Mediator In Glutamine-Amplified Insulin Secretion. J Diabetes Investig. 2021;12:920–30. [CrossRef]
- Satapati S, Sunny NE, Kucejova B, Fu X, He TT, Méndez-Lucas A, Shelton JM, Perales JC, Browning JD, Burgess SC. Elevated TCA Cycle Function In The Pathology Of Diet-Induced Hepatic Insulin Resistance And Fatty Liver. Journal of Lipid Research. 2012;53:1080–92. [CrossRef]
- Maurer J, Hoene M, Weigert C. Signals From The Circle: Tricarboxylic Acid Cycle Intermediates As Myometabokines. Metabolites. 2021;11. [CrossRef]
- Gilbert M. Role Of Skeletal Muscle Lipids In The Pathogenesis Of Insulin Resistance Of Obesity And Type 2 Diabetes. Journal of Diabetes Investigation. 2021;12:1934–41. [CrossRef]
- Nagao H, Nishizawa H, Bamba T, Nakayama Y, Isozumi N, Nagamori S, Kanai Y, Tanaka Y, Kita S, Fukuda S, Funahashi T, Maeda N, Fukusaki E, Shimomura I. Increased Dynamics Of Tricarboxylic Acid Cycle And Glutamate Synthesis In Obese Adipose Tissue: IN VIVO METABOLIC TURNOVER ANALYSIS. The Journal of Biological Chemistry. 2017;292:4469–83.
- Newsholme P, Rowlands J, Rose’meyer R, Cruzat V. Metabolic Adaptions/Reprogramming In Islet Beta-Cells In Response To Physiological Stimulators-What Are The Consequences. Antioxidants (Basel, Switzerland). 2022;11. [CrossRef]
- Zhang GF, Jensen M V., Gray SM, El K, Wang Y, Lu D, Becker TC, Campbell JE, Newgard CB. Reductive TCA Cycle Metabolism Fuels Glutamine- And Glucose-Stimulated Insulin Secretion. Cell Metabolism. 2021;33:804-817.e5. [CrossRef]
- Heart E, Cline GW, Collis LP, Pongratz RL, Gray JP, Smith PJS. Role For Malic Enzyme, Pyruvate Carboxylation, And Mitochondrial Malate Import In Glucose-Stimulated Insulin Secretion. American Journal of Physiology Endocrinology and Metabolism. 2009;296. [CrossRef]
- Wang L, Yi D, Hou Y, Ding B, Li K, Li B, Zhu H, Liu Y, Wu G. The Journal Of Nutrition Nutrient Physiology, Metabolism, And Nutrient-Nutrient Interactions Dietary Supplementation With A-Ketoglutarate Activates MTOR Signaling And Enhances Energy Status In Skeletal Muscle Of Lipopolysaccharide-Challenged Piglets 1,2 n.d.
- Yao K, Yin Y, Li X, Xi P, Wang J, Lei J, Hou Y, Wu G. Alpha-Ketoglutarate Inhibits Glutamine Degradation And Enhances Protein Synthesis In Intestinal Porcine Epithelial Cells. Amino Acids. 2012;42:2491–500. [CrossRef]
- Fazakerley DJ, Krycer JR, Kearney AL, Hocking SL, James DE. Muscle And Adipose Tissue Insulin Resistance: Malady Without Mechanism? Journal of Lipid Research. 2019;60:1720–32.
- Tretter L, Adam-Vizi V. Alpha-Ketoglutarate Dehydrogenase: A Target And Generator Of Oxidative Stress. Philosophical Transactions of the Royal Society of London Series B, Biological Sciences. 2005;360:2335–45. [CrossRef]
- Selak MA, Armour SM, MacKenzie ED, Boulahbel H, Watson DG, Mansfield KD, Pan Y, Simon MC, Thompson CB, Gottlieb E. Succinate Links TCA Cycle Dysfunction To Oncogenesis By Inhibiting HIF-α Prolyl Hydroxylase. Cancer Cell. 2005;7:77–85. [CrossRef]
- Gabryelska A, Karuga FF, Szmyd B, Białasiewicz P. HIF-1α As A Mediator Of Insulin Resistance, T2DM, And Its Complications: Potential Links With Obstructive Sleep Apnea. Frontiers in Physiology. 2020;11. [CrossRef]
- Badole SL, Chaudhari SM, Bagul PP, Mahamuni SP, Khose RD. Effect Of Concomitant Administration Of L-Glutamine And Cycloart-23-Ene-3b, 25-Diol (B2) With Sitagliptin In GLP-1 (7-36) Amide Secretion, Biochemical And Oxidative Stress In Streptozotocin-Nicotinamide Induced Diabetic Sprague Dawley Rats. PLoS ONE. 2013;8:72817.
- Badole SL, Jangam GB, Chaudhari SM, Ghule AE, Zanwar AA. L-Glutamine Supplementation Prevents The Development Of Experimental Diabetic Cardiomyopathy In Streptozotocin-Nicotinamide Induced Diabetic Rats. PLOS ONE. 2014;9:e92697. [CrossRef]
- Tsai PH, Liu JJ, Yeh CL, Chiu WC, Yeh SL. Effects Of Glutamine Supplementation On Oxidative Stress-Related Gene Expression And Antioxidant Properties In Rats With Streptozotocin-Induced Type 2 Diabetes. The British Journal of Nutrition. 2012;107:1112–8. [CrossRef]
- Tsai PH, Liu JJ, Chiu WC, Pai MH, Yeh SL. Effects Of Dietary Glutamine On Adhesion Molecule Expression And Oxidative Stress In Mice With Streptozotocin-Induced Type 1 Diabetes. Clinical Nutrition. 2011;30:124–9. [CrossRef]
- Tsai PH, Yeh CL, Liu JJ, Chiu WC, Yeh SL. Effects Of Dietary Glutamine On Inflammatory Mediator Gene Expressions In Rats With Streptozotocin-Induced Diabetes. Nutrition. 2012;28:288–93. [CrossRef]
- Jafari-Vayghan H, Varshosaz P, Hajizadeh-Sharafabad F, Razmi HR, Amirpour M, Tavakoli-Rouzbehani OM, Alizadeh M, Maleki V. A Comprehensive Insight Into The Effect Of Glutamine Supplementation On Metabolic Variables In Diabetes Mellitus: A Systematic Review. Nutrition & Metabolism. 2020;17:80. [CrossRef]
- Noto H, Goto A, Tsujimoto T, Noda M. Cancer Risk In Diabetic Patients Treated With Metformin: A Systematic Review And Meta-Analysis. PLoS ONE. 2012;7:1–9. [CrossRef]
- Saraei P, Asadi I, Kakar MA, Moradi-Kor N. The Beneficial Effects Of Metformin On Cancer Prevention And Therapy: A Comprehensive Review Of Recent Advances. Cancer Management and Research. 2019;11:3295–313. [CrossRef]
- Mallik R, Chowdhury TA. Metformin In Cancer. Diabetes Research and Clinical Practice. 2018;143:409–19.
- Chen TM, Lin CC, Huang PT, Wen CF. Metformin Associated With Lower Mortality In Diabetic Patients With Early Stage Hepatocellular Carcinoma After Radiofrequency Ablation. Journal of Gastroenterology and Hepatology (Australia). 2011;26:858–65. [CrossRef]
- Doherty JR et al. Blocking Lactate Export By Inhibiting The Myc Target MCT1 Disables Glycolysis And Glutathione Synthesis. Cancer Research. 2014;74:908–20.
- Buzzai M, Jones RG, Amaravadi RK, Lum JJ, DeBerardinis RJ, Zhao F, Viollet B, Thompson CB. Systemic Treatment With The Antidiabetic Drug Metformin Selectively Impairs P53-Deficient Tumor Cell Growth. Cancer Research. 2007;67:6745–52.
- DeCensi A, Puntoni M, Goodwin P, Cazzaniga M, Gennari A, Bonanni B, Gandini S. Metformin And Cancer Risk In Diabetic Patients: A Systematic Review And Meta-Analysis. Cancer Prevention Research. 2010;3:1451–61. [CrossRef]
- Kim YS, Choi EA, woo Lee J, Kim Y, You HS, Han YE, Kim HS, Bae YJ, Kang HT, Kim J. Metformin Use Reduced The Overall Risk Of Cancer In Diabetic Patients: A Study Based On The Korean NHIS-HEALS Cohort. Nutrition, Metabolism and Cardiovascular Diseases. 2020;30:1714–22. [CrossRef]
- Kim J, Hyun HJ, Choi EA, Kim Y, Bae YJ, Kang HT. Metformin Use Reduced The Risk Of Stomach Cancer In Diabetic Patients In Korea: An Analysis Of Korean NHIS-HEALS Database. Gastric Cancer. 2020;23:1075–83. [CrossRef]
- Shuai Y, Li C, Zhou X. The Effect Of Metformin On Gastric Cancer In Patients With Type 2 Diabetes: A Systematic Review And Meta-Analysis. Clinical and Translational Oncology. 2020;22:1580–90. [CrossRef]
- Hu J, Fan HD, Gong JP, Mao QS. The Relationship Between The Use Of Metformin And The Risk Of Pancreatic Cancer In Patients With Diabetes: A Systematic Review And Meta-Analysis. BMC Gastroenterology. 2023;23:1–21. [CrossRef]
- Zhang K, Bai P, Dai H, Deng Z. Metformin And Risk Of Cancer Among Patients With Type 2 Diabetes Mellitus: A Systematic Review And Meta-Analysis. Primary Care Diabetes. 2021;15:52–8. [CrossRef]
- Mekuria AN, Ayele Y, Tola A, Mishore KM. Monotherapy With Metformin Versus Sulfonylureas And Risk Of Cancer In Type 2 Diabetic Patients: A Systematic Review And Meta-Analysis. Journal of Diabetes Research. 2019;2019. [CrossRef]
- Cunha V, Cotrim HP, Rocha R, Carvalho K, Lins-Kusterer L. Metformin In The Prevention Of Hepatocellular Carcinoma In Diabetic Patients: A Systematic Review. Annals of Hepatology. 2020;19:232–7. [CrossRef]
- Farmer RE, Ford D, Mathur R, Chaturvedi N, Kaplan R, Smeeth L, Bhaskaran K. Metformin Use And Risk Of Cancer In Patients With Type 2 Diabetes: A Cohort Study Of Primary Care Records Using Inverse Probability Weighting Of Marginal Structural Models. International Journal of Epidemiology. 2019;48:527–37. [CrossRef]
- Govindarajan R, Ratnasinghe L, Simmons DL, Siegel ER, Midathada M V, Kim L, Kim PJ, Owens RJ, Lang NP. Thiazolidinediones And The Risk Of Lung, Prostate, And Colon Cancer In Patients With Diabetes. Journal of Clinical Oncology. 2007;25:1476–81. [CrossRef]
- Du R, Lin L, Cheng D, Xu Y, Xu M, Chen Y, Wang W, Bi Y, Li D, Lu J. Thiazolidinedione Therapy And Breast Cancer Risk In Diabetic Women: A Systematic Review And Meta-Analysis. Diabetes/Metabolism Research and Reviews. 2018;34:9–11. [CrossRef]
- Chang CH, Lin JW, Wu LC, Lai MS, Chuang LM, Arnold Chan K. Association Of Thiazolidinediones With Liver Cancer And Colorectal Cancer In Type 2 Diabetes Mellitus. Hepatology. 2012;55:1462–72. [CrossRef]
- Lin HC, Hsu YT, Kachingwe BH, Hsu CY, Uang YS, Wang LH. Dose Effect Of Thiazolidinedione On Cancer Risk In Type 2 Diabetes Mellitus Patients: A Six-Year Population-Based Cohort Study. Journal of Clinical Pharmacy and Therapeutics. 2014;39:354–60. [CrossRef]
- Liao KF, Lin CL, Lai SW. Association Between Colorectal Cancer And Thiazolidinediones Administration In A Case-Control Study. BioMedicine (France). 2019;9:31–6. [CrossRef]
- Ramos-Nino ME, MacLean CD, Littenberg B. Association Between Cancer Prevalence And Use Of Thiazolidinediones: Results From The Vermont Diabetes Information System. BMC Medicine. 2007;5:1–7. [CrossRef]
- Bsch INC, Bowker SL, Majumdar SR, Johnson JA. Use Of Thiazolidinediones And The Risk Of Bladder Cancer Among People With Type 2 Diabetes: A Meta-Analysis. Canadian Medical Association Journal. 2012;184:675–83.
- Dankner R, Roth J. More Recent, Better Designed Studies Have Weakened Links Between Antidiabetes Medications And Cancer Risk. Diabetic Medicine. 2019;37:194–202. [CrossRef]
- Kim J, Yang G, Kim Y, Kim J, Ha J. AMPK Activators: Mechanisms Of Action And Physiological Activities. Experimental and Molecular Medicine. 2016;48:1–12. [CrossRef]
- Miller RA, Chu Q, Xie J, Foretz M, Viollet B, Birnbaum MJ. Biguanides Suppress Hepatic Glucagon Signaling By Decreasing Production Of Cyclic AMP. Physiology & Behavior. 2019;176:139–48. [CrossRef]
- Foretz M, Hébrard S, Leclerc J, Zarrinpashneh E, Soty M, Mithieux G, Sakamoto K, Andreelli F, Viollet B. Metformin Inhibits Hepatic Gluconeogenesis In Mice Independently Of The LKB1/AMPK Pathway Via A Decrease In Hepatic Energy State. The Journal of Clinical Investigation. 2010;120:2355–69.
- Coughlan KA, Valentine RJ, Ruderman NB, Saha AK. AMPK Activation: A Therapeutic Target For Type 2 Diabetes? Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy. 2014:7–241. [CrossRef]
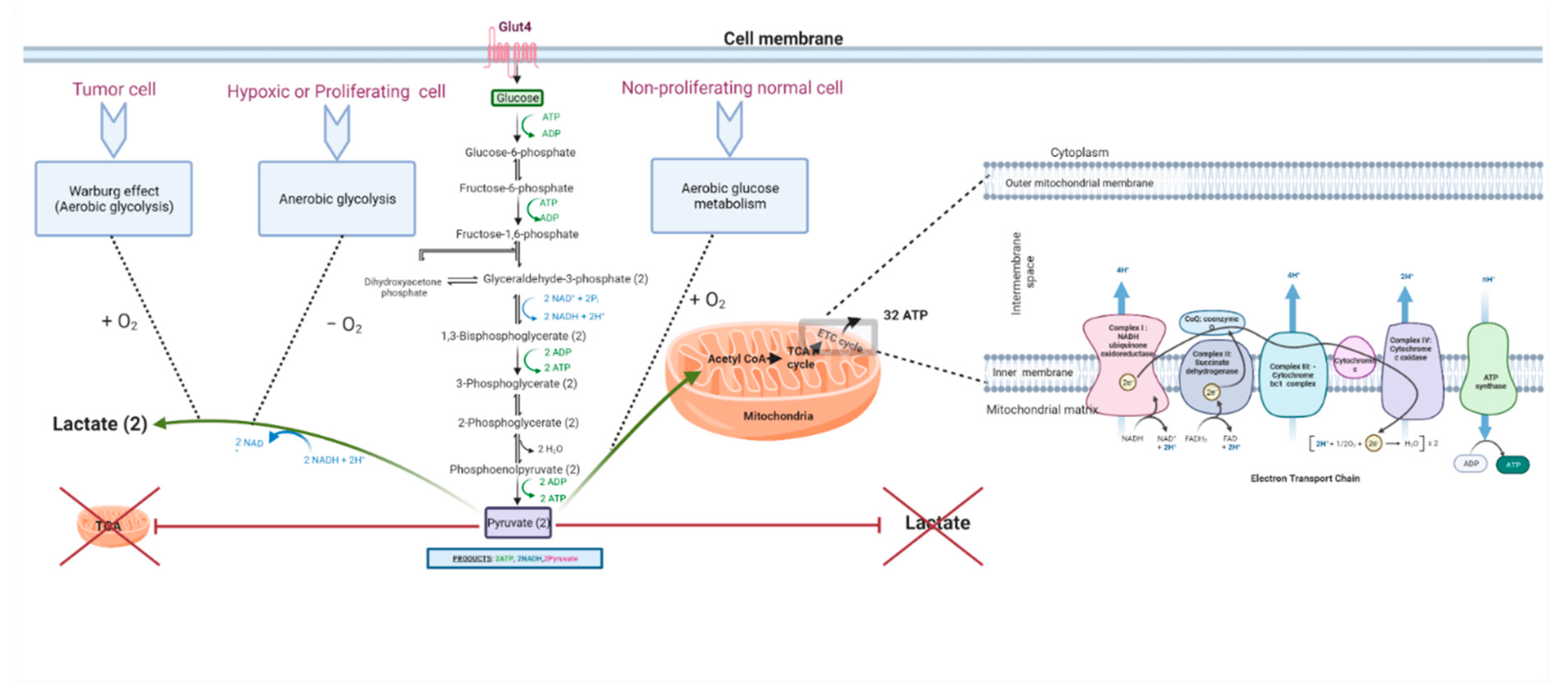

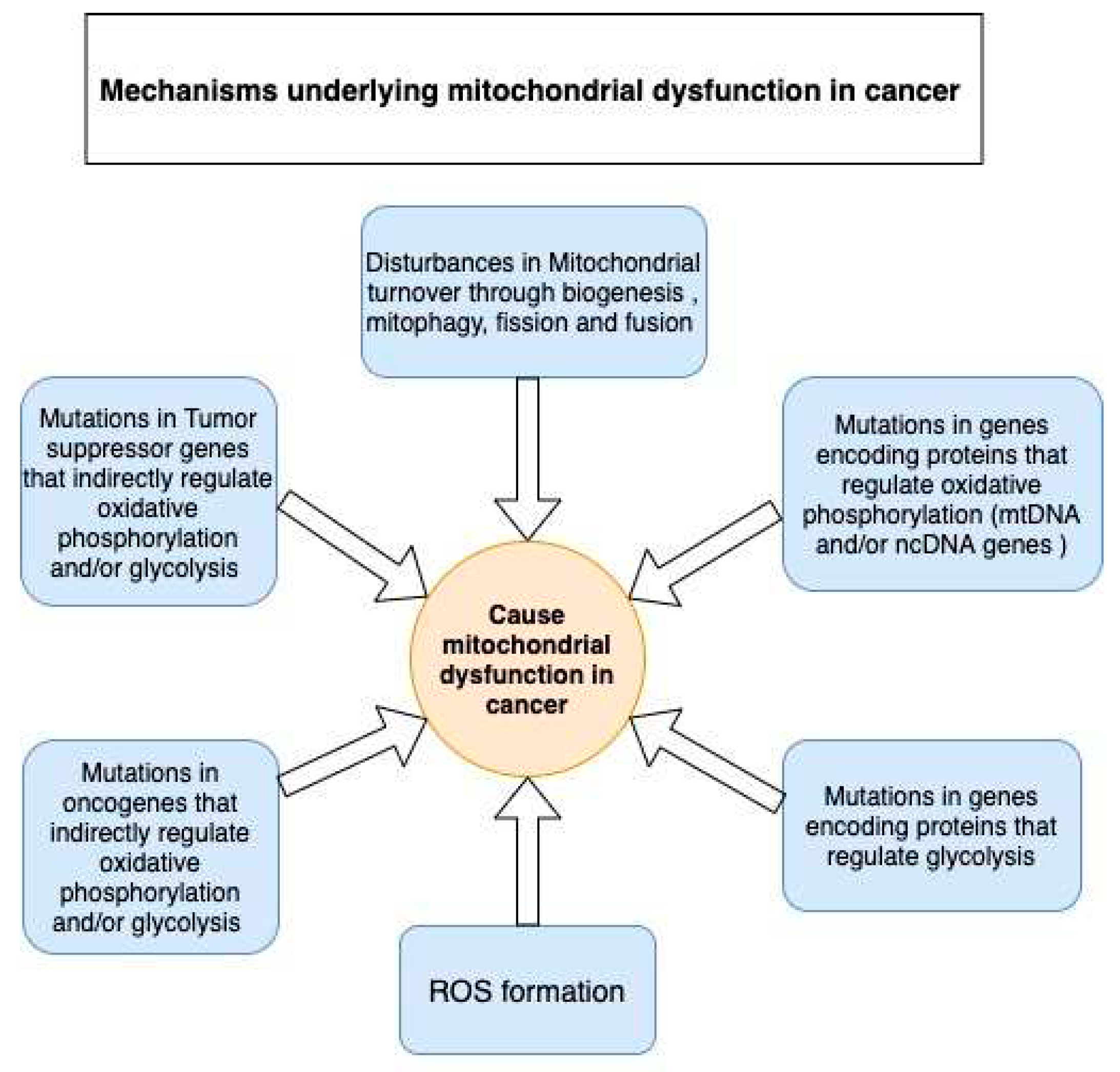
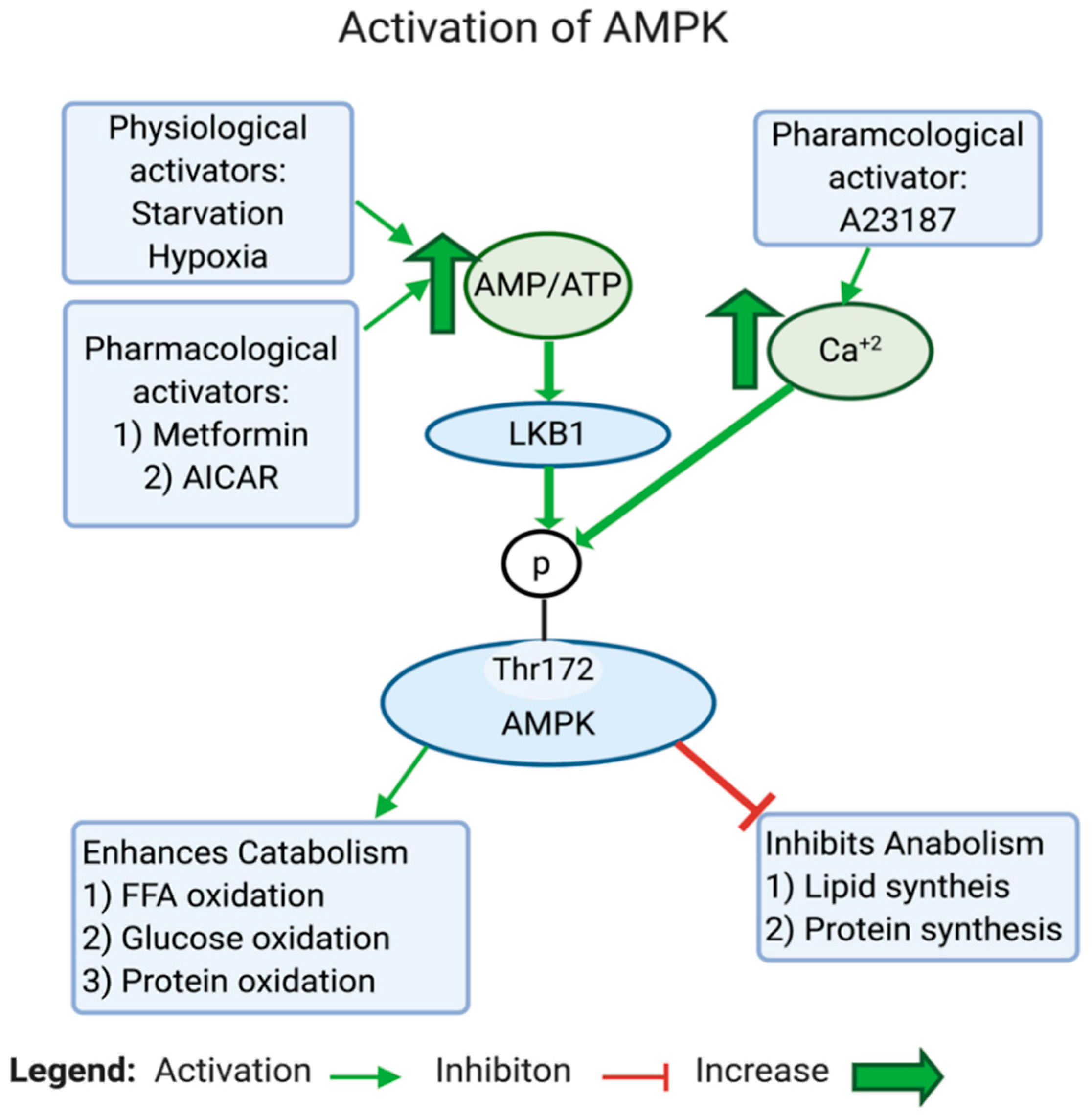
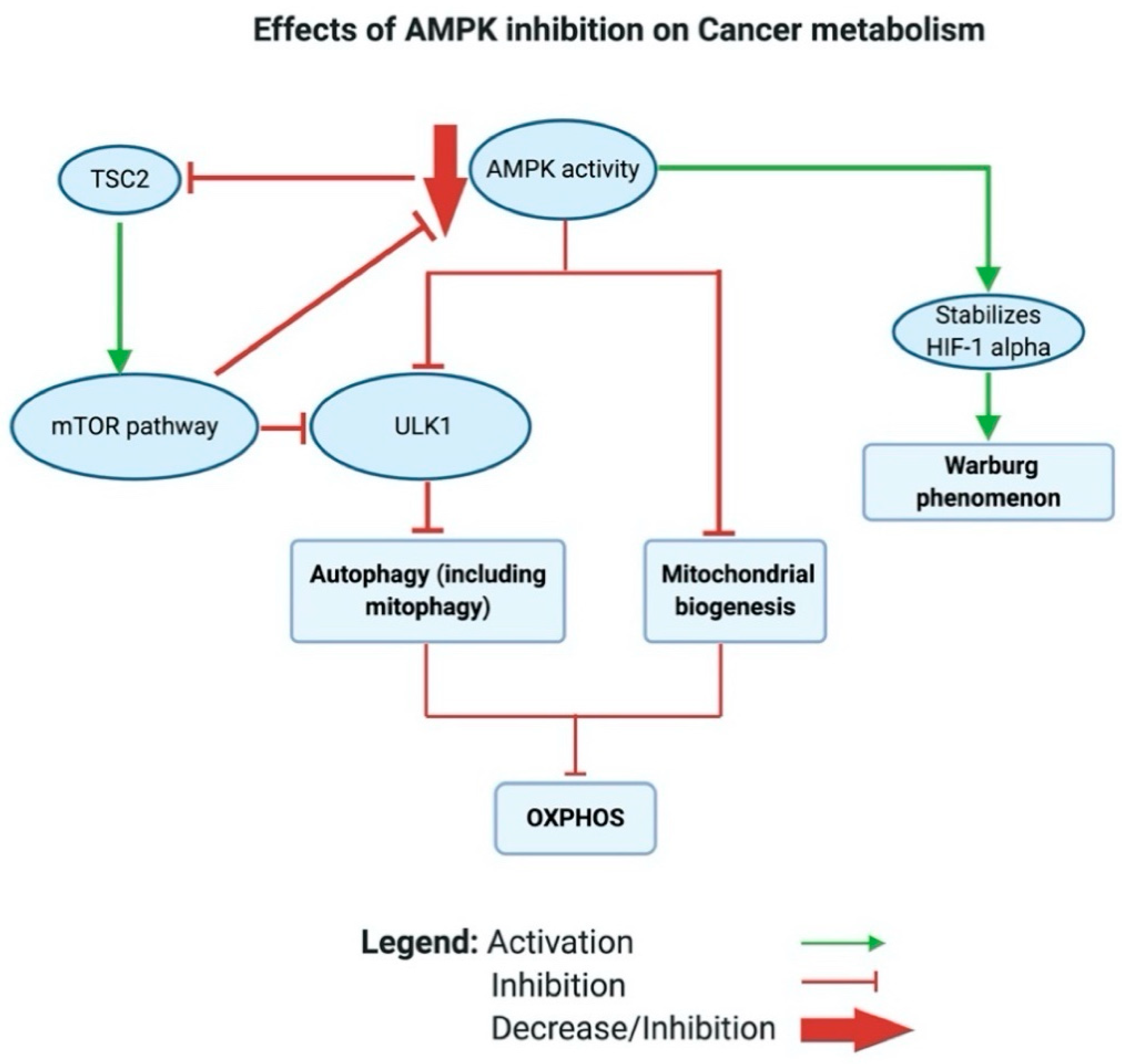
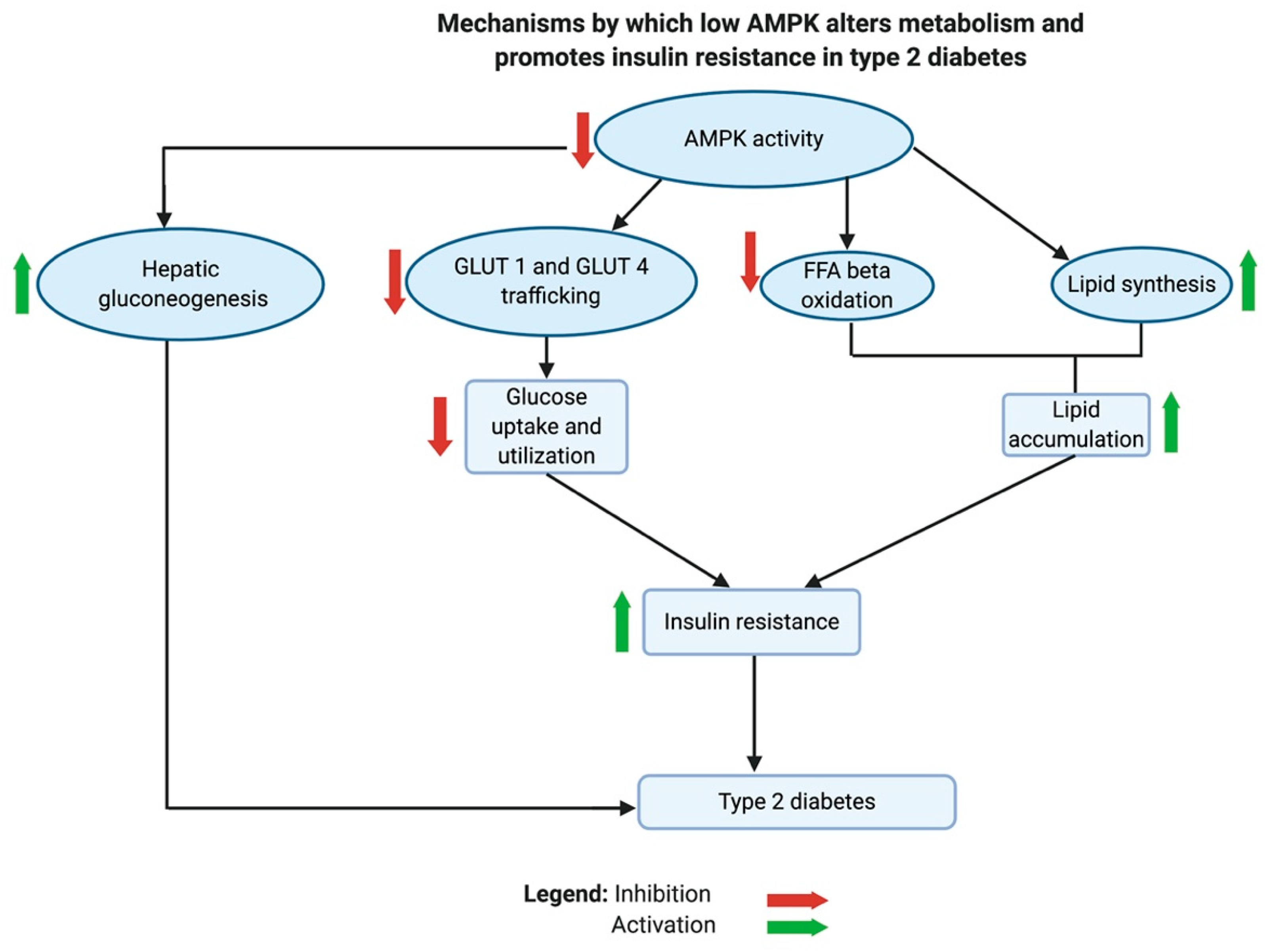
| Flavonoid’s name | Flavonoid subfamily | Mechanism of targeting Warburg glycolysis | Warburg glycolytic target | References |
|---|---|---|---|---|
| Apegenin | Flavones |
|
PKM2 | [322] |
| epigallocatechin-3-gallate (EGCG) | Flavan-3-ols |
|
PKM2 | [323] |
|
HK2 HIF-1a |
[323] [323] |
||
| Proanthocyanidin B2 (PB2) | Anthocyanidins |
|
PKM2 | [324] |
| Shikonin (SHI) | Naphthoquinone flavonoid |
|
PKM2 | [325,326] |
| Quercetin (QUE) | Flavonol |
|
PKM2 | [327] |
|
HK2 | [327] | ||
|
LDH | [327] | ||
| Xanthohumol (XA) | Prenylated Flavonoid |
|
HK2 | [328] |
| 10v | Synthetic flavonoid |
|
HK2 | [329] |
| GL-V9 | Synthetic flavonoid |
|
HK2 | [330] |
| FV-429 | Synthetic flavonoid |
|
HK2 | [331] |
| Gen-27 | Synthetic flavonoid |
|
HK2 | [332] |
| Astragalin (ASG) | O-glycoside flavonoid |
|
HK2 | [333] |
| Morin (MO) | Flavonol |
|
LDH | [334] |
| Methylalpinumisoflavon (MF) | Isoflavone |
|
HIF-1α | [335] |
| Oroxylin A (OX-A) | Flavone |
|
HIF-1α | [336] |
| Baicalein (BA) | Flavone |
|
HIF-1α | [337] |
| Wogonin | O-methylated flavone |
|
HIF-1α | [338] [339] |
| Berberine (BBR) | Isoquinoline flavonoid |
|
HK2 | [340] [341] |
| Resveratrol |
|
HK2 PDH complex |
[342] [343] [344] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





