Submitted:
20 October 2023
Posted:
20 October 2023
You are already at the latest version
Abstract
Keywords:
I. Introduction
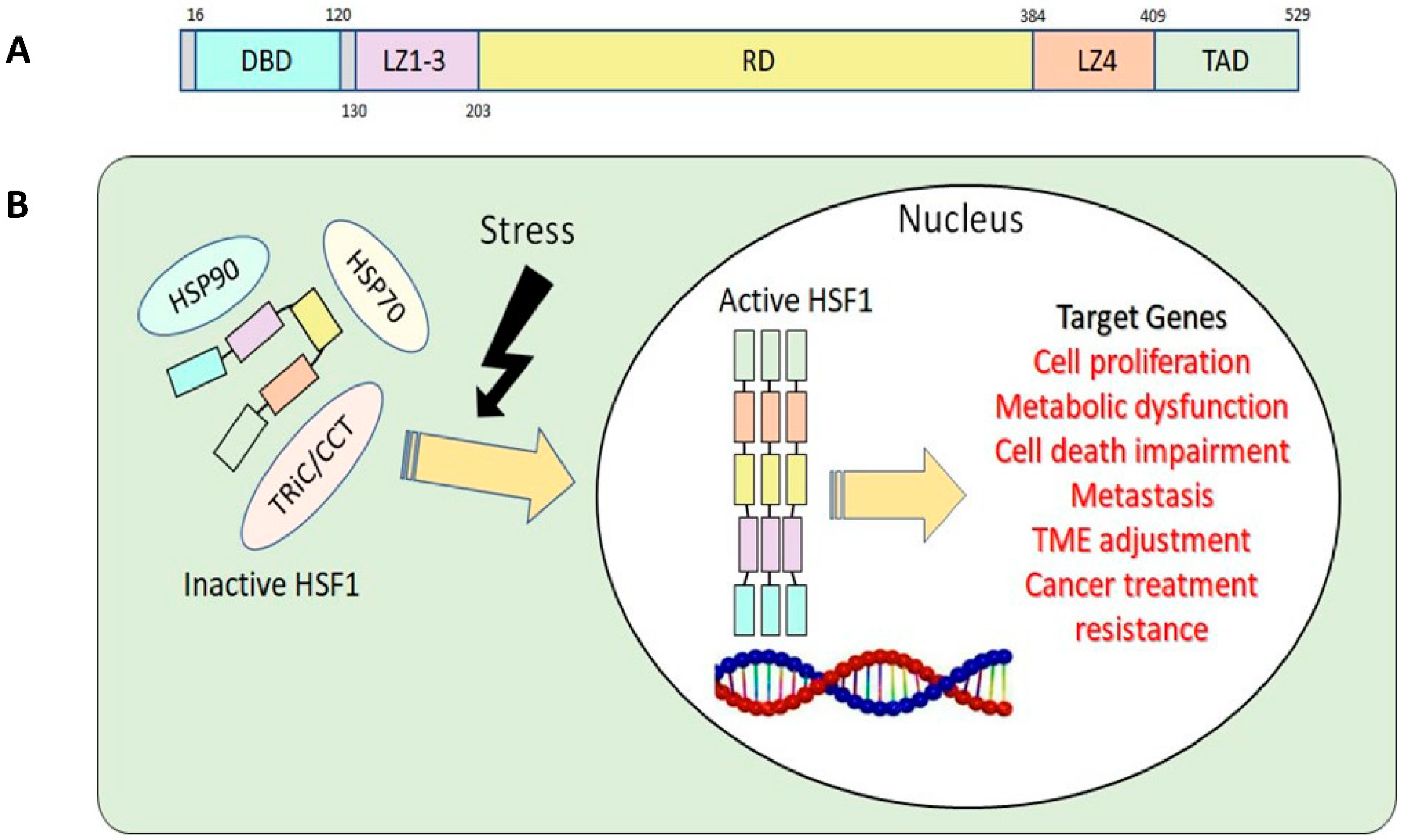
II. HSF1 biology
1. HSF1 structure and function
2. HSF1 regulatory mechanisms in normal and cancer cells
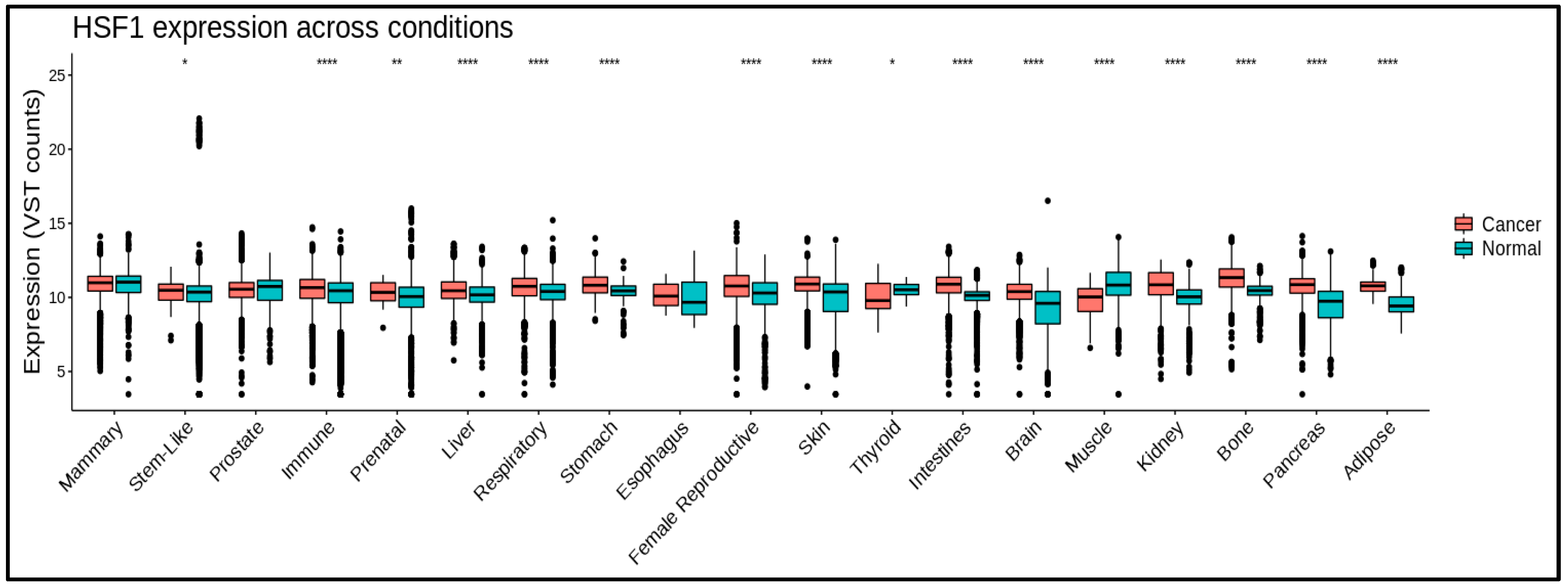
III. HSF1 involvement in various cancer types
1. Breast Cancer
2. Lung Cancer
3. Ovarian Cancer
4. Endometrial Cancer
5. Prostate Cancer
| Cancer Type | Effect on tumorigenesis | Reference |
| Liver cancer Breast Cancer Prostate Cancer Lung Cancer ESCC Colorectal Cancer Endometrial Cancer Ovarian Cancer |
Promotes cell proliferation, growth, migration, invasion, and survival, as well as kinase function, lipid metabolism, and glycolysis Promotes cell motility, metastasis, and survival as well as receptor and kinase maturation, stemness, drug resistance, DNA repair, and EMT Promotes development of polyploidy, high Gleason score, and cancer re-occurrence. Decreases patient survival. Promotes angiogenesis and Metastasis Promotes cell survival and expression of HSPs. Promotes expression of anti-apoptotic proteins, cell growth, and glutaminolysis Tumor progression Proliferation Tumor progression, cell spreading, ECM remodeling, and cancer invasion |
[63,64,65,66,67] [35,36,37,38,68,69] [31,59] [41,70,71] [10] [71,72] [32] [46,47] [49,73,74] |
IV. HSF1 in theurapetical resistance
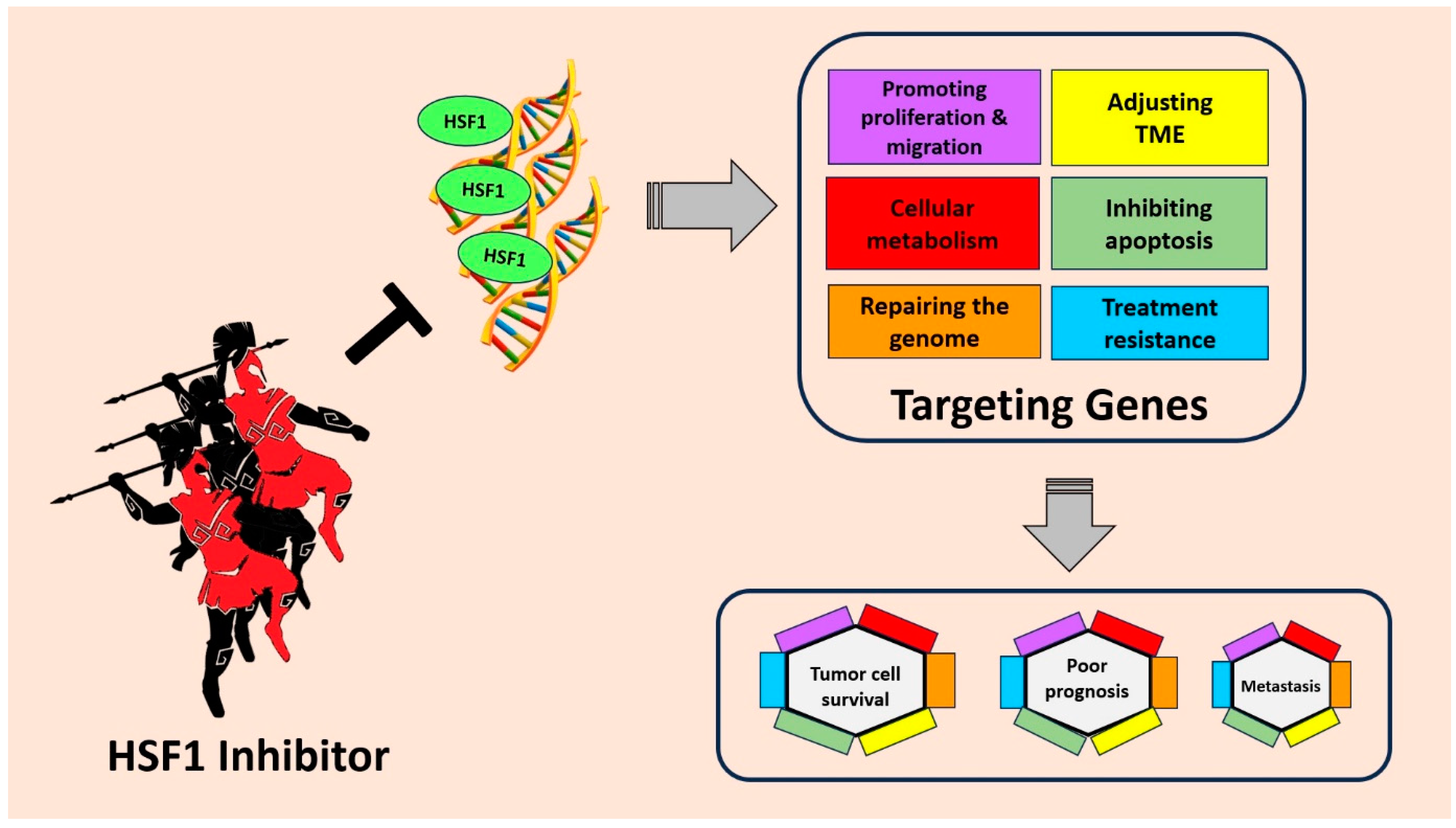
VI. Targeting HSF1 for cancer treatment
| Agents | Source | Cancer type | Reff. |
| Cantharidin | Blister beetles (Meloidae spp.) | colon cancer, lung cancer, prostate cancer, breast cancer | [114] |
| CCT251236 | Bisamide | ovarian cancer | [112] |
| Dorsomorphin | colon cancer; prostate cancer | [115] | |
| IHSF1115 | Thiazole acrylamide | multiple myeloma; breast cancer | [116,117] |
| KNK437 | Benzylidene lactam | colon cancer; squamous cell carcinoma; breast Cancer | [117,118,119] |
| KRIBB11 | Pyridinediamine | multiple myeloma; lung cancer | [41,117,120,121,122] |
| NZ28 | Emetine | myeloma; prostate cancer; lung cancer; breast cancer |
[97,123] |
| NXP800 (CCT361814) |
Bisamide | multiple myeloma; solid tumor (under clinical trial) |
[109,110,111] |
| NZ28 | Emetine | myeloma; prostate cancer; lung cancer; breast cancer |
[97,123] |
| PW3405 | Anthraquinone | HeLa cancer cell | [113,117] |
| Quercetin |
plant pigment (flavonoid) | liver and breast cancer | [124] |
| Rohinitib (rocaglamide / rocaglates) |
Flavaglines; | leukemia | [79,125] |
| SISU-102 (DTHIB) |
prostate cancer; leukemia | [31,108] | |
| SNS-032 | Sulfur compounds | leukemia | [126,127,128] |
| Triptolide | Tripterygium wilfordii | chronic lymphocytic leukemia; pancreatic cancer; liver cancer multiple myeloma |
[129] [130][131] |
| 2,4-Bis (4-hydroxy benzyl) phenol |
Gastrodia elata | lung cancer | [132] |
| 4,6-disubstituted pyrimidines | Aromatic heterocyclic organic compound | osteosarcoma | [128] |
VII. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Ethical Approval
Consent for publication
Availability of data and materials
References
- Akerfelt M, Morimoto RI, and Sistonen L, Heat shock factors: integrators of cell stress, development and lifespan. Nat Rev Mol Cell Biol, 2010. 11(8): p. 545-55. [CrossRef]
- Morimoto RI, The heat shock response: systems biology of proteotoxic stress in aging and disease. Cold Spring Harb Symp Quant Biol, 2011. 76: p. 91-9. [CrossRef]
- Richter K, Haslbeck M, and Buchner J, The heat shock response: life on the verge of death. Mol Cell, 2010. 40(2): p. 253-66.
- Jiang S, Tu K, Fu Q, Schmitt DC, Zhou L, Lu N, and Zhao Y, Multifaceted roles of HSF1 in cancer. Tumour Biol, 2015. 36(7): p. 4923-31. [CrossRef]
- Dai C and Sampson SB, HSF1: Guardian of Proteostasis in Cancer. Trends Cell Biol, 2016. 26(1): p. 17-28.
- Li J, Labbadia J, and Morimoto RI, Rethinking HSF1 in Stress, Development, and Organismal Health. Trends Cell Biol, 2017. 27(12): p. 895-905. [CrossRef]
- Chen F, Fan Y, Cao P, Liu B, Hou J, Zhang B, and Tan K, Pan-Cancer Analysis of the Prognostic and Immunological Role of HSF1: A Potential Target for Survival and Immunotherapy. Oxid Med Cell Longev, 2021. 2021: p. 5551036. [CrossRef]
- Wang G, Cao P, Fan Y, and Tan K, Emerging roles of HSF1 in cancer: Cellular and molecular episodes. Biochim Biophys Acta Rev Cancer, 2020. 1874(1): p. 188390. [CrossRef]
- Mendillo ML, Santagata S, Koeva M, Bell GW, Hu R, Tamimi RM, Fraenkel E, Ince TA, Whitesell L, and Lindquist S, HSF1 Drives a Transcriptional Program Distinct from Heat Shock to Support Highly Malignant Human Cancers. Cell, 2012. 150(3): p. 549-62. [CrossRef]
- Wan T, Shao J, Hu B, Liu G, Luo P, and Zhou Y, Prognostic role of HSF1 overexpression in solid tumors: a pooled analysis of 3,159 patients. Onco Targets Ther, 2018. 11: p. 383-93. [CrossRef]
- Dong B, Jaeger AM, and Thiele DJ, Inhibiting Heat Shock Factor 1 in Cancer: A Unique Therapeutic Opportunity. Trends Pharmacol Sci, 2019. 40(12): p. 986-1005. [CrossRef]
- Gomez-Pastor R, Burchfiel ET, and Thiele DJ, Regulation of heat shock transcription factors and their roles in physiology and disease. Nat Rev Mol Cell Biol, 2018. 19(1): p. 4-19. [CrossRef]
- Dayalan Naidu S and Dinkova-Kostova AT, Regulation of the mammalian heat shock factor 1. Febs j, 2017. 284(11): p. 1606-27.
- Neudegger T, Verghese J, Hayer-Hartl M, Hartl FU, and Bracher A, Structure of human heat-shock transcription factor 1 in complex with DNA. Nat Struct Mol Biol, 2016. 23(2): p. 140-6. [CrossRef]
- Anckar J and Sistonen L, Regulation of HSF1 function in the heat stress response: implications in aging and disease. Annu Rev Biochem, 2011. 80: p. 1089-115. [CrossRef]
- Kmiecik SW and Mayer MP, Molecular mechanisms of heat shock factor 1 regulation. Trends Biochem Sci, 2022. 47(3): p. 218-34. [CrossRef]
- Ravarani CN, Erkina TY, De Baets G, Dudman DC, Erkine AM, and Babu MM, High-throughput discovery of functional disordered regions: investigation of transactivation domains. Mol Syst Biol, 2018. 14(5): p. e8190. [CrossRef]
- Pincus D, Regulation of Hsf1 and the Heat Shock Response. Adv Exp Med Biol, 2020. 1243: p. 41-50.
- Li G, Kryczek I, Nam J, Li X, Li S, Li J, Wei S, Grove S, Vatan L, Zhou J, et al., LIMIT is an immunogenic lncRNA in cancer immunity and immunotherapy. Nat Cell Biol, 2021. 23(5): p. 526-37. [CrossRef]
- Masser AE, Ciccarelli M, and Andreasson C, Hsf1 on a leash - controlling the heat shock response by chaperone titration. Exp Cell Res, 2020. 396(1): p. 112246. [CrossRef]
- Guettouche T, Boellmann F, Lane WS, and Voellmy R, Analysis of phosphorylation of human heat shock factor 1 in cells experiencing a stress. BMC Biochem, 2005. 6: p. 4. [CrossRef]
- Holmes B, Benavides-Serrato A, Freeman RS, Landon KA, Bashir T, Nishimura RN, and Gera J, mTORC2/AKT/HSF1/HuR constitute a feed-forward loop regulating Rictor expression and tumor growth in glioblastoma. Oncogene, 2018. 37(6): p. 732-43.
- Srivastava P, Takii R, Okada M, Fujimoto M, and Nakai A, MED12 interacts with the heat-shock transcription factor HSF1 and recruits CDK8 to promote the heat-shock response in mammalian cells. FEBS Lett, 2021. 595(14): p. 1933-48. [CrossRef]
- Chou SD, Prince T, Gong J, and Calderwood SK, mTOR is essential for the proteotoxic stress response, HSF1 activation and heat shock protein synthesis. PLoS One, 2012. 7(6): p. e39679. [CrossRef]
- Huang CY, Lee FL, Peng SF, Lin KH, Chen RJ, Ho TJ, Tsai FJ, Padma VV, Kuo WW, and Huang CY, HSF1 phosphorylation by ERK/GSK3 suppresses RNF126 to sustain IGF-IIR expression for hypertension-induced cardiomyocyte hypertrophy. J Cell Physiol, 2018. 233(2): p. 979-89. [CrossRef]
- Raychaudhuri S, Loew C, Korner R, Pinkert S, Theis M, Hayer-Hartl M, Buchholz F, and Hartl FU, Interplay of acetyltransferase EP300 and the proteasome system in regulating heat shock transcription factor 1. Cell, 2014. 156(5): p. 975-85. [CrossRef]
- Westerheide SD, Anckar J, Stevens SM, Jr., Sistonen L, and Morimoto RI, Stress-inducible regulation of heat shock factor 1 by the deacetylase SIRT1. Science, 2009. 323(5917): p. 1063-6.
- Kmiecik SW, Le Breton L, and Mayer MP, Feedback regulation of heat shock factor 1 (Hsf1) activity by Hsp70-mediated trimer unzipping and dissociation from DNA. EMBO J, 2020. 39(14): p. e104096. [CrossRef]
- Zhao YH, Zhou M, Liu H, Ding Y, Khong HT, Yu D, Fodstad O, and Tan M, Upregulation of lactate dehydrogenase A by ErbB2 through heat shock factor 1 promotes breast cancer cell glycolysis and growth. Oncogene, 2009. 28(42): p. 3689-701. [CrossRef]
- Desai S, Liu Z, Yao J, Patel N, Chen J, Wu Y, Ahn EE, Fodstad O, and Tan M, Heat shock factor 1 (HSF1) controls chemoresistance and autophagy through transcriptional regulation of autophagy-related protein 7 (ATG7). J Biol Chem, 2013. 288(13): p. 9165-76. [CrossRef]
- Dong B, Jaeger AM, Hughes PF, Loiselle DR, Hauck JS, Fu Y, Haystead TA, Huang J, and Thiele DJ, Targeting therapy-resistant prostate cancer via a direct inhibitor of the human heat shock transcription factor 1. Sci Transl Med, 2020. 12(574). [CrossRef]
- Engerud H, Tangen IL, Berg A, Kusonmano K, Halle MK, Oyan AM, Kalland KH, Stefansson I, Trovik J, Salvesen HB, et al., High level of HSF1 associates with aggressive endometrial carcinoma and suggests potential for HSP90 inhibitors. Br J Cancer, 2014. 111(1): p. 78-84. [CrossRef]
- Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, and Bray F, Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin, 2021. 71(3): p. 209-49. [CrossRef]
- Society AC, Cancer Facts & Figures 2021. 2021, Atlanta: American Cancer Society.
- He L, Lv S, Ma X, Jiang S, Zhou F, Zhang Y, Yu R, and Zhao Y, ErbB2 promotes breast cancer metastatic potential via HSF1/LDHA axis-mediated glycolysis. Med Oncol, 2022. 39(4): p. 45. [CrossRef]
- Vydra N, Janus P, Kus P, Stokowy T, Mrowiec K, Toma-Jonik A, Krzywon A, Cortez AJ, Wojtas B, Gielniewski B, et al., Heat shock factor 1 (HSF1) cooperates with estrogen receptor α (ERα) in the regulation of estrogen action in breast cancer cells. Elife, 2021. 10. [CrossRef]
- Vydra N, Janus P, Toma-Jonik A, Stokowy T, Mrowiec K, Korfanty J, Długajczyk A, Wojtaś B, Gielniewski B, and Widłak W, 17β-Estradiol Activates HSF1 via MAPK Signaling in ERα-Positive Breast Cancer Cells. Cancers (Basel), 2019. 11(10). [CrossRef]
- Liu K and Ma R, MicroRNA-615-5p regulates the proliferation and apoptosis of breast cancer cells by targeting HSF1. Exp Ther Med, 2021. 21(3): p. 192.
- Yang W, Feng B, Meng Y, Wang J, Geng B, Cui Q, Zhang H, Yang Y, and Yang J, FAM3C-YY1 axis is essential for TGFbeta-promoted proliferation and migration of human breast cancer MDA-MB-231 cells via the activation of HSF1. J Cell Mol Med, 2019. 23(5): p. 3464-75.
- Sanchez-Ortega M, Carrera AC, and Garrido A, Role of NRF2 in Lung Cancer. Cells, 2021. 10(8). [CrossRef]
- Lee S, Jung J, Lee YJ, Kim SK, Kim JA, Kim BK, Park KC, Kwon BM, and Han DC, Targeting HSF1 as a Therapeutic Strategy for Multiple Mechanisms of EGFR Inhibitor Resistance in EGFR Mutant Non-Small-Cell Lung Cancer. Cancers (Basel), 2021. 13(12). [CrossRef]
- Marc L. Mendillo SS, Martina Koeva, George W. Bell, Rong Hu, Rulla M. Tamimi, Ernest Fraenkel, Tan A. Ince, Luke Whitesell, and Susan and Lindquist S, HSF1 drives a transcriptional program distinct from heat shock to support highly malignant human cancers. Cell, 2012. 29(37): p. 5204-13. [CrossRef]
- Dai C, Whitesell L, Rogers AB, and Lindquist S, Heat shock factor 1 is a powerful multifaceted modifier of carcinogenesis. Cell, 2007. 130(6): p. 1005-18.
- Hoj JP, Mayro B, and Pendergast AM, The ABL2 kinase regulates an HSF1-dependent transcriptional program required for lung adenocarcinoma brain metastasis. Proc Natl Acad Sci U S A, 2020. 117(52): p. 33486-95. [CrossRef]
- Kim J, Park EY, Kim O, Schilder JM, Coffey DM, Cho CH, and Bast RC, Jr., Cell Origins of High-Grade Serous Ovarian Cancer. Cancers (Basel), 2018. 10(11). [CrossRef]
- Wilson AL, Moffitt LR, Duffield N, Rainczuk A, Jobling TW, Plebanski M, and Stephens AN, Autoantibodies against HSF1 and CCDC155 as Biomarkers of Early-Stage, High-Grade Serous Ovarian Cancer. Cancer Epidemiol Biomarkers Prev, 2018. 27(2): p. 183-92. [CrossRef]
- Moody R, Wilson K, Kampan NC, McNally OM, Jobling TW, Jaworowski A, Stephens AN, and Plebanski M, Mapping Epitopes Recognised by Autoantibodies Shows Potential for the Diagnosis of High-Grade Serous Ovarian Cancer and Monitoring Response to Therapy for This Malignancy. Cancers (Basel), 2021. 13(16). [CrossRef]
- van Zyl B, Tang D, and Bowden NA, Biomarkers of platinum resistance in ovarian cancer: what can we use to improve treatment. Endocr Relat Cancer, 2018. 25(5): p. R303-R18.
- Ferrari N, Ranftl R, Chicherova I, Slaven ND, Moeendarbary E, Farrugia AJ, Lam M, Semiannikova M, Westergaard MCW, Tchou J, et al., Dickkopf-3 links HSF1 and YAP/TAZ signalling to control aggressive behaviours in cancer-associated fibroblasts. Nat Commun, 2019. 10(1): p. 130. [CrossRef]
- Gynecologists ACoOa, Polycystic Ovary Syndrome. ACOG Practice Bulletin, 2018. 131(6): p. 157-71.
- Hu G, Zhang J, Zhou X, Liu J, Wang Q, and Zhang B, Roles of estrogen receptor α and β in the regulation of proliferation in endometrial carcinoma. Pathol Res Pract, 2020. 216(10): p. 153149. [CrossRef]
- Rodriguez AC, Blanchard Z, Maurer KA, and Gertz J, Estrogen Signaling in Endometrial Cancer: a Key Oncogenic Pathway with Several Open Questions. Horm Cancer, 2019. 10(2-3): p. 51-63. [CrossRef]
- Yu K, Huang ZY, Xu XL, Li J, Fu XW, and Deng SL, Estrogen Receptor Function: Impact on the Human Endometrium. Front Endocrinol (Lausanne), 2022. 13: p. 827724. [CrossRef]
- Guha P, Sen K, Chowdhury P, and Mukherjee D, Estrogen receptors as potential therapeutic target in endometrial cancer. J Recept Signal Transduct Res, 2023. 43(1): p. 19-26. [CrossRef]
- Ranhotra HS, The estrogen-related receptors in metabolism and cancer: newer insights. J Recept Signal Transduct Res, 2018. 38(2): p. 95-100. [CrossRef]
- Silveira MA, Tav C, Berube-Simard FA, Cuppens T, Leclercq M, Fournier E, Cote MC, Droit A, and Bilodeau S, Modulating HSF1 levels impacts expression of the estrogen receptor alpha and antiestrogen response. Life Sci Alliance, 2021. 4(5). [CrossRef]
- Schatten H, Brief Overview of Prostate Cancer Statistics, Grading, Diagnosis and Treatment Strategies. Adv Exp Med Biol, 2018. 1095: p. 1-14. [CrossRef]
- Watson PA, Arora VK, and Sawyers CL, Emerging mechanisms of resistance to androgen receptor inhibitors in prostate cancer. Nat Rev Cancer, 2015. 15(12): p. 701-11. [CrossRef]
- Björk JK, Ahonen I, Mirtti T, Erickson A, Rannikko A, Bützow A, Nordling S, Lundin J, Lundin M, Sistonen L, et al., Increased HSF1 expression predicts shorter disease-specific survival of prostate cancer patients following radical prostatectomy. Oncotarget, 2018. 9(58): p. 31200-13. [CrossRef]
- Xia Y, Wang M, Beraldi E, Cong M, Zoubeidi A, Gleave M, and Peng L, A Novel Triazole Nucleoside Suppresses Prostate Cancer Cell Growth by Inhibiting Heat Shock Factor 1 and Androgen Receptor. Anti-Cancer Agents in Medicinal Chemistry, 2015. 15(10): p. 1333-40. [CrossRef]
- Wyatt AW and Gleave ME, Targeting the adaptive molecular landscape of castration-resistant prostate cancer. EMBO Mol Med, 2015. 7(7): p. 878-94.
- Moses MA, Kim YS, Rivera-Marquez GM, Oshima N, Watson MJ, Beebe KE, Wells C, Lee S, Zuehlke AD, Shao H, et al., Targeting the Hsp40/Hsp70 Chaperone Axis as a Novel Strategy to Treat Castration-Resistant Prostate Cancer. Cancer Res, 2018. 78(14): p. 4022-35.
- Fang F, Chang R, and Yang L, Heat shock factor 1 promotes invasion and metastasis of hepatocellular carcinoma in vitro and in vivo. Cancer, 2012. 118(7): p. 1782-94. [CrossRef]
- Shen Z, Yin L, Zhou H, Ji X, Jiang C, Zhu X, and He X, Combined inhibition of AURKA and HSF1 suppresses proliferation and promotes apoptosis in hepatocellular carcinoma by activating endoplasmic reticulum stress. Cell Oncol (Dordr), 2021. 44(5): p. 1035-49. [CrossRef]
- Li M, Hu J, Jin R, Cheng H, Chen H, Li L, and Guo K, Effects of LRP1B Regulated by HSF1 on Lipid Metabolism in Hepatocellular Carcinoma. J Hepatocell Carcinoma, 2020. 7: p. 361-76. [CrossRef]
- Liu HT, Huang DA, Li MM, Liu HD, and Guo K, HSF1: a mediator in metabolic alteration of hepatocellular carcinoma cells in cross-talking with tumor-associated macrophages. Am J Transl Res, 2019. 11(8): p. 5054-64.
- Zhang N, Wu Y, Lyu X, Li B, Yan X, Xiong H, Li X, Huang G, Zeng Y, Zhang Y, et al., HSF1 upregulates ATG4B expression and enhances epirubicin-induced protective autophagy in hepatocellular carcinoma cells. Cancer Lett, 2017. 409: p. 81-90. [CrossRef]
- Santagata S, Hu R, Lin NU, Mendillo ML, Collins LC, Hankinson SE, Schnitt SJ, Whitesell L, Tamimi RM, Lindquist S, et al., High levels of nuclear heat-shock factor 1 (HSF1) are associated with poor prognosis in breast cancer. Proc Natl Acad Sci U S A, 2011. 108(45): p. 18378-83. [CrossRef]
- Yang T, Ren C, Lu C, Qiao P, Han X, Wang L, Wang D, Lv S, Sun Y, and Yu Z, Phosphorylation of HSF1 by PIM2 Induces PD-L1 Expression and Promotes Tumor Growth in Breast Cancer. Cancer Res, 2019. 79(20): p. 5233-44.
- Yun HH, Baek JY, Seo G, Kim YS, Ko JH, and Lee JH, Effect of BIS depletion on HSF1-dependent transcriptional activation in A549 non-small cell lung cancer cells. Korean J Physiol Pharmacol, 2018. 22(4): p. 457-65. [CrossRef]
- Song P, Feng L, Li J, Dai D, Zhu L, Wang C, Li J, Li L, Zhou Q, Shi R, et al., β-catenin represses miR455-3p to stimulate m6A modification of HSF1 mRNA and promote its translation in colorectal cancer. Mol Cancer, 2020. 19(1): p. 129. [CrossRef]
- Cen H, Zheng S, Fang YM, Tang XP, and Dong Q, Induction of HSF1 expression is associated with sporadic colorectal cancer. World J Gastroenterol, 2004. 10(21): p. 3122-6. [CrossRef]
- Scherz-Shouval R, Santagata S, Mendillo ML, Sholl LM, Ben-Aharon I, Beck AH, Dias-Santagata D, Koeva M, Stemmer SM, Whitesell L, et al., The reprogramming of tumor stroma by HSF1 is a potent enabler of malignancy. Cell, 2014. 158(3): p. 564-78. [CrossRef]
- Heng BC, Zhang X, Aubel D, Bai Y, Li X, Wei Y, Fussenegger M, and Deng X, An overview of signaling pathways regulating YAP/TAZ activity. Cell Mol Life Sci, 2021. 78(2): p. 497-512. [CrossRef]
- Kijima T, Prince TL, Tigue ML, Yim KH, Schwartz H, Beebe K, Lee S, Budzynski MA, Williams H, Trepel JB, et al., HSP90 inhibitors disrupt a transient HSP90-HSF1 interaction and identify a noncanonical model of HSP90-mediated HSF1 regulation. Sci Rep, 2018. 8(1): p. 6976. [CrossRef]
- Workman P, Reflections and Outlook on Targeting HSP90, HSP70 and HSF1 in Cancer: A Personal Perspective. Adv Exp Med Biol, 2020. 1243: p. 163-79.
- Cyran AM and Zhitkovich A, Heat Shock Proteins and HSF1 in Cancer. Front Oncol, 2022. 12: p. 860320. [CrossRef]
- Yeh C, Gumilar KE, Xing-Guo Li, Brahmana A. Tjokroprawiro, Chien-Hsing Lu, Jianrong Lu, Ming Zhou, Robert W. Sobol, and Tan M, Targeting HSF1 for cancer treatment: mechanisms and inhibitor development. Theranostic, 2023. [CrossRef]
- Santagata S, Mendillo ML, Tang YC, Subramanian A, Perley CC, Roche SP, Wong B, Narayan R, Kwon H, Koeva M, et al., Tight coordination of protein translation and HSF1 activation supports the anabolic malignant state. Science, 2013. 341(6143): p. 1238303. [CrossRef]
- Chang Z, Lu M, Park SM, Park HK, Kang HS, Pak Y, and Park JS, Functional HSF1 requires aromatic-participant interactions in protecting mouse embryonic fibroblasts against apoptosis via G2 cell cycle arrest. Mol Cells, 2012. 33(5): p. 465-70. [CrossRef]
- Luft JC, Benjamin IJ, Mestril R, and Dix DJ, Heat shock factor 1-mediated thermotolerance prevents cell death and results in G2/M cell cycle arrest. Cell Stress Chaperones, 2001. 6(4): p. 326-36.
- Bruce JL, Chen C, Xie Y, Zhong R, Wang YQ, Stevenson MA, and Calderwood SK, Activation of heat shock transcription factor 1 to a DNA binding form during the G(1)phase of the cell cycle. Cell Stress Chaperones, 1999. 4(1): p. 36-45. [CrossRef]
- Fujimoto M, Takii R, Takaki E, Katiyar A, Nakato R, Shirahige K, and Nakai A, The HSF1-PARP13-PARP1 complex facilitates DNA repair and promotes mammary tumorigenesis. Nat Commun, 2017. 8(1): p. 1638. [CrossRef]
- Shi X, Deng Z, Wang S, Zhao S, Xiao L, Zou J, Li T, Tan S, Tan S, and Xiao X, Increased HSF1 Promotes Infiltration and Metastasis in Cervical Cancer via Enhancing MTDH-VEGF-C Expression. Onco Targets Ther, 2021. 14: p. 1305-15. [CrossRef]
- Tian X, Zhou N, Yuan J, Lu L, Zhang Q, Wei M, Zou Y, and Yuan L, Heat shock transcription factor 1 regulates exercise-induced myocardial angiogenesis after pressure overload via HIF-1α/VEGF pathway. J Cell Mol Med, 2020. 24(3): p. 2178-88. [CrossRef]
- Gabai VL, Meng L, Kim G, Mills TA, Benjamin IJ, and Sherman MY, Heat shock transcription factor Hsf1 is involved in tumor progression via regulation of hypoxia-inducible factor 1 and RNA-binding protein HuR. Mol Cell Biol, 2012. 32(5): p. 929-40. [CrossRef]
- McConnell JR, Buckton LK, and McAlpine SR, Regulating the master regulator: Controlling heat shock factor 1 as a chemotherapy approach. Bioorg Med Chem Lett, 2015. 25(17): p. 3409-14.
- Mun GI, Choi E, Lee Y, and Lee YS, Decreased expression of FBXW7 by ERK1/2 activation in drug-resistant cancer cells confers transcriptional activation of MDR1 by suppression of ubiquitin degradation of HSF1. Cell Death Dis, 2020. 11(5): p. 395.
- Bukowski K, Kciuk M, and Kontek R, Mechanisms of Multidrug Resistance in Cancer Chemotherapy. Int J Mol Sci, 2020. 21(9). [CrossRef]
- Natalia Vydra AT, Magdalena Glowala-Kosinska, Agnieszka Gogler-Piglowska and Wieslawa Widlak, Overexpression of heat shock transcription factor 1 enhances the resistance of melanoma cells to doxorubicin and paclitaxe. BMC Cancer, 2013. 13.
- Kourtis N, Moubarak RS, Aranda-Orgilles B, Lui K, Aydin IT, Trimarchi T, Darvishian F, Salvaggio C, Zhong J, Bhatt K, et al., FBXW7 modulates cellular stress response and metastatic potential through HSF1 post-translational modification. Nat Cell Biol, 2015. 17(3): p. 322-32. [CrossRef]
- Zheng T, Long noncoding RNA NBAT1 inhibits autophagy via suppression of ATG7 in non-small cell lung cancer. Am J Cancer Res, 2018. 8(9): p. 1801-11.
- Gabai VL, Budagova KR, and Sherman MY, Increased expression of the major heat shock protein Hsp72 in human prostate carcinoma cells is dispensable for their viability but confers resistance to a variety of anticancer agents. Oncogene, 2005. 24(20): p. 3328-38. [CrossRef]
- Schilling D, Bayer C, Li W, Molls M, Vaupel P, and Multhoff G, Radiosensitization of normoxic and hypoxic h1339 lung tumor cells by heat shock protein 90 inhibition is independent of hypoxia inducible factor-1α. PLoS One, 2012. 7(2): p. e31110. [CrossRef]
- Zaidi S, McLaughlin M, Bhide SA, Eccles SA, Workman P, Nutting CM, Huddart RA, and Harrington KJ, The HSP90 inhibitor NVP-AUY922 radiosensitizes by abrogation of homologous recombination resulting in mitotic entry with unresolved DNA damage. PLoS One, 2012. 7(4): p. e35436. [CrossRef]
- Li Q and Martinez JD, Loss of HSF1 results in defective radiation-induced G(2) arrest and DNA repair. Radiat Res, 2011. 176(1): p. 17-24.
- Schilling D, Kuhnel A, Konrad S, Tetzlaff F, Bayer C, Yaglom J, and Multhoff G, Sensitizing tumor cells to radiation by targeting the heat shock response. Cancer Lett, 2015. 360(2): p. 294-301. [CrossRef]
- Jacobs AT and Marnett LJ, HSF1-mediated BAG3 expression attenuates apoptosis in 4-hydroxynonenal-treated colon cancer cells via stabilization of anti-apoptotic Bcl-2 proteins. J Biol Chem, 2009. 284(14): p. 9176-83. [CrossRef]
- Kim HY, Kim Y-S, Yun HH, Im C-N, Ko J-H, and Lee J-H, ERK-mediated phosphorylation of BIS regulates nuclear translocation of HSF1 under oxidative stress. Experimental & Molecular Medicine, 2016. 48(9): p. e260-e. [CrossRef]
- Janus P, Pakuła-Cis M, Kalinowska-Herok M, Kashchak N, Szołtysek K, Pigłowski W, Widlak W, Kimmel M, and Widlak P, NF-κB signaling pathway is inhibited by heat shock independently of active transcription factor HSF1 and increased levels of inducible heat shock proteins. Genes Cells, 2011. 16(12): p. 1168-75.
- Li W, Hu C, Zhong X, Wu J, and Li G, Melatonin Induces AGS Gastric Cancer Cell Apoptosis via Regulating PERK/eIF2α and HSF1/NF-κB Signaling Pathway. Ann Clin Lab Sci, 2022. 52(1): p. 40-7.
- Li J, Liu Y, Duan P, Yu R, Gu Z, Li L, Liu Z, and Su L, NF-κB regulates HSF1 and c-Jun activation in heat stress-induced intestinal epithelial cell apoptosis. Mol Med Rep, 2018. 17(2): p. 3388-96.
- Kühnel A, Schilling D, Combs SE, Haller B, Schwab M, and Multhoff G, Radiosensitization of HSF-1 Knockdown Lung Cancer Cells by Low Concentrations of Hsp90 Inhibitor NVP-AUY922. Cells, 2019. 8(10). [CrossRef]
- Carpenter RL and Gokmen-Polar Y, HSF1 as a Cancer Biomarker and Therapeutic Target. Curr Cancer Drug Targets, 2019. 19(7): p. 515-24. [CrossRef]
- Nytko KJ, Thumser-Henner P, Russo G, Weyland MS, and Rohrer Bley C, Role of HSP70 in response to (thermo)radiotherapy: analysis of gene expression in canine osteosarcoma cells by RNA-seq. Sci Rep, 2020. 10(1): p. 12779. [CrossRef]
- Multhoff G, Pockley AG, Schmid TE, and Schilling D, The role of heat shock protein 70 (Hsp70) in radiation-induced immunomodulation. Cancer Lett, 2015. 368(2): p. 179-84. [CrossRef]
- Velayutham M, Cardounel AJ, Liu Z, and Ilangovan G, Discovering a Reliable Heat-Shock Factor-1 Inhibitor to Treat Human Cancers: Potential Opportunity for Phytochemists. Front Oncol, 2018. 8: p. 97. [CrossRef]
- Dong Q, Xiu Y, Wang Y, Hodgson C, Borcherding N, Jordan C, Buchanan J, Taylor E, Wagner B, Leidinger M, et al., HSF1 is a driver of leukemia stem cell self-renewal in acute myeloid leukemia. Nat Commun, 2022. 13(1): p. 6107. [CrossRef]
- Workman P, Clarke PA, Te Poele R, Powers M, Box G, De Billy E, De Haven Brandon A, Hallsworth A, Hayes A, McCann H, et al., Discovery and validation of biomarkers to support clinical development of NXP800: A first-in-class orally active, small-molecule HSF1 pathway inhibitor. European Journal of Cancer, 2022. 174. [CrossRef]
- Karen Menezes GA, Fabio Mirabella, David C Johnson, Amy L Sherborne, Richard S Houlston, Matthew D Cheeseman, Elisa Pasqua, Paul Clarke, Paul Workman, Keith Jones, Martin F Kaiser, The Novel Protein HSF1 Stress Pathway Inhibitor Bisamide CCT361814 Demonstrates Pre-Clinical Anti-Tumor Activity in Myeloma. Blood, 2017. 130.
- Diane Marsolini SS. A Phase 1 Clinical Study of NXP800 in Subjects With Advanced Cancers. 2022; Available from: https://clinicaltrials.gov/ct2/show/NCT05226507?term=HSF1&draw=2&rank=3#contacts.
- Cheeseman MD, Chessum NE, Rye CS, Pasqua AE, Tucker MJ, Wilding B, Evans LE, Lepri S, Richards M, Sharp SY, et al., Discovery of a Chemical Probe Bisamide (CCT251236): An Orally Bioavailable Efficacious Pirin Ligand from a Heat Shock Transcription Factor 1 (HSF1) Phenotypic Screen. J Med Chem, 2017. 60(1): p. 180-201. [CrossRef]
- Zhang D and Zhang B, Selective killing of cancer cells by small molecules targeting heat shock stress response. Biochem Biophys Res Commun, 2016. 478(4): p. 1509-14. [CrossRef]
- Kim JA, Kim Y, Kwon BM, and Han DC, The natural compound cantharidin induces cancer cell death through inhibition of heat shock protein 70 (HSP70) and Bcl-2-associated athanogene domain 3 (BAG3) expression by blocking heat shock factor 1 (HSF1) binding to promoters. J Biol Chem, 2013. 288(40): p. 28713-26. [CrossRef]
- Li N, Wang T, Li Z, Ye X, Deng B, Zhuo S, Yao P, Yang M, Mei H, Chen X, et al., Dorsomorphin induces cancer cell apoptosis and sensitizes cancer cells to HSP90 and proteasome inhibitors by reducing nuclear heat shock factor 1 levels. Cancer Biol Med, 2019. 16(2): p. 220-33.
- Vilaboa N, Bore A, Martin-Saavedra F, Bayford M, Winfield N, Firth-Clark S, Kirton SB, and Voellmy R, New inhibitor targeting human transcription factor HSF1: effects on the heat shock response and tumor cell survival. Nucleic Acids Res, 2017. 45(10): p. 5797-817. [CrossRef]
- Sharma C and Seo YH, Small Molecule Inhibitors of HSF1-Activated Pathways as Potential Next-Generation Anticancer Therapeutics. Molecules, 2018. 23(11).
- Whitesell L and Lindquist S, Inhibiting the transcription factor HSF1 as an anticancer strategy. Expert Opin Ther Targets, 2009. 13(4): p. 469-78. [CrossRef]
- Oommen D and Prise KM, KNK437, abrogates hypoxia-induced radioresistance by dual targeting of the AKT and HIF-1α survival pathways. Biochem Biophys Res Commun, 2012. 421(3): p. 538-43. [CrossRef]
- Yoon YJ, Kim JA, Shin KD, Shin DS, Han YM, Lee YJ, Lee JS, Kwon BM, and Han DC, KRIBB11 inhibits HSP70 synthesis through inhibition of heat shock factor 1 function by impairing the recruitment of positive transcription elongation factor b to the hsp70 promoter. J Biol Chem, 2011. 286(3): p. 1737-47. [CrossRef]
- Kang MJ, Yun HH, and Lee JH, KRIBB11 accelerates Mcl-1 degradation through an HSF1-independent, Mule-dependent pathway in A549 non-small cell lung cancer cells. Biochem Biophys Res Commun, 2017. 492(3): p. 304-9. [CrossRef]
- Fok JHL, Hedayat S, Zhang L, Aronson LI, Mirabella F, Pawlyn C, Bright MD, Wardell CP, Keats JJ, De Billy E, et al., HSF1 Is Essential for Myeloma Cell Survival and A Promising Therapeutic Target. Clin Cancer Res, 2018. 24(10): p. 2395-407. [CrossRef]
- Zaarur N, Gabai VL, Porco JA, Jr., Calderwood S, and Sherman MY, Targeting heat shock response to sensitize cancer cells to proteasome and Hsp90 inhibitors. Cancer Res, 2006. 66(3): p. 1783-91. [CrossRef]
- Yang W, Cui M, Lee J, Gong W, Wang S, Fu J, Wu G, and Yan K, Heat shock protein inhibitor, quercetin, as a novel adjuvant agent to improve radiofrequency ablation-induced tumor destruction and its molecular mechanism. Chin J Cancer Res, 2016. 28(1): p. 19-28. [CrossRef]
- Iwasaki S, Floor SN, and Ingolia NT, Rocaglates convert DEAD-box protein eIF4A into a sequence-selective translational repressor. Nature, 2016. 534(7608): p. 558-61. [CrossRef]
- Chen R, Wierda WG, Chubb S, Hawtin RE, Fox JA, Keating MJ, Gandhi V, and Plunkett W, Mechanism of action of SNS-032, a novel cyclin-dependent kinase inhibitor, in chronic lymphocytic leukemia. Blood, 2009. 113(19): p. 4637-45.
- Wu Y, Chen C, Sun X, Shi X, Jin B, Ding K, Yeung SC, and Pan J, Cyclin-dependent kinase 7/9 inhibitor SNS-032 abrogates FIP1-like-1 platelet-derived growth factor receptor alpha and bcr-abl oncogene addiction in malignant hematologic cells. Clin Cancer Res, 2012. 18(7): p. 1966-78.
- Rye CS, Chessum NE, Lamont S, Pike KG, Faulder P, Demeritt J, Kemmitt P, Tucker J, Zani L, Cheeseman MD, et al., Discovery of 4,6-disubstituted pyrimidines as potent inhibitors of the heat shock factor 1 (HSF1) stress pathway and CDK9. Medchemcomm, 2016. 7(8): p. 1580-6.
- Siddhartha Ganguly TH, Joseph McGuirk, Rekha Rao, Abdulraheem Yacoub Kambhampati, Huidong Shi, Prasad Dandawate, Subhash Padhye Saluja, Joseph McGuirk, Rekha Rao, Targeting HSF1 disrupts HSP90 chaperone function in chronic lymphocytic leukemia. Oncotarget, 2015. 6. [CrossRef]
- Sangwan V, Banerjee S, Jensen KM, Chen Z, Chugh R, Dudeja V, Vickers SM, and Saluja AK, Primary and liver metastasis-derived cell lines from KrasG12D; Trp53R172H; Pdx-1 Cre animals undergo apoptosis in response to triptolide. Pancreas, 2015. 44(4): p. 583-9. [CrossRef]
- Heimberger T, Andrulis M, Riedel S, Stuhmer T, Schraud H, Beilhack A, Bumm T, Bogen B, Einsele H, Bargou RC, et al., The heat shock transcription factor 1 as a potential new therapeutic target in multiple myeloma. Br J Haematol, 2013. 160(4): p. 465-76. [CrossRef]
- Yoon T, Kang GY, Han AR, Seo EK, and Lee YS, 2,4-Bis(4-hydroxybenzyl)phenol inhibits heat shock transcription factor 1 and sensitizes lung cancer cells to conventional anticancer modalities. J Nat Prod, 2014. 77(5): p. 1123-9. [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





