Submitted:
09 October 2023
Posted:
11 October 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
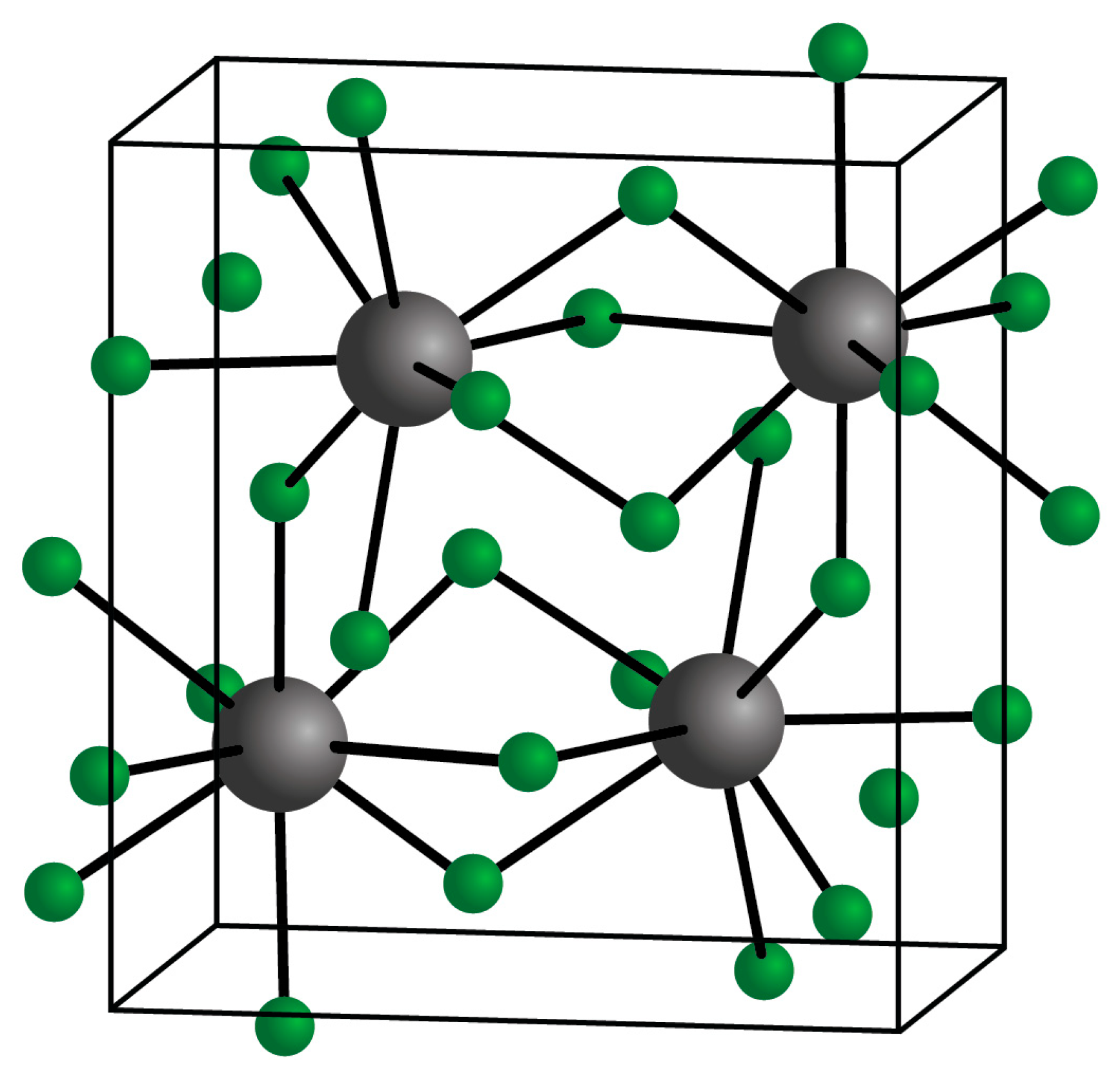
2. Ytterbium Compounds
3. Ytterbium Fluoride in Dental Materials
4. The Chemical Behavior of Ytterbium Fluoride when Used in Dental Materials
Funding
Acknowledgments
Conflicts of Interest
References
- Cotton, S. Lanthanide and Actinide Chemistry; John Wiley & Sons: Chichester, UK, 2006. [Google Scholar]
- Klemm, W.; Bommer, H. Contribution to the knowledge of the rare earths. Z. Anorg. Allg.Chem., 1937, 231, 138–171. [Google Scholar] [CrossRef]
- Daane, A.H.; Dennison, D.H.; Spedding, F.H. The preparation of samarium and ytterbium metals. J. Amer. Chem. Soc., 1953, 75, 2272–2273. [Google Scholar] [CrossRef]
- Greenwood, N.N.; Earnshaw, A. Chemistry of the Elements; Butterworth-Heinemnann: Oxford, UK, 1984; pp. 1437–1440. [Google Scholar]
- Lide, D.R. (Ed.) Handbook of Chemistry and Physics, 90th ed.; CRC Press: Boca Raton, Florida, USA, 1998. [Google Scholar]
- Shannon, R.D. Revised effective ionic radius and systematic studies of interatomic distances in halides and chalcogenides. Acta Crystallogr 1976, Sect. A32, 751–767. [Google Scholar] [CrossRef]
- Jia, Y.Q. Crystal radii and effective ionic radii of the Rare Earth ions. J. Solid State Chem., 1991, 95, 184–187. [Google Scholar] [CrossRef]
- Wells, A.F. Structural Inorganic Chemistry, 5th ed.Oxford Science Publishers: Oxford, UK, 1984. [Google Scholar]
- Schmidt, L.; Dimitrov, A.; Kemnitz, E. A new approach to prepare nanoscopic rare earth metal fluoride: the fluorolytic sol-gel synthesis of ytterbium fluoride. Chem. Commun., 2014, 50, 6613–6616. [Google Scholar] [CrossRef]
- Hiranao, S.; Suzuki, K.T. Exposure, metabolism, and toxicity of rare earths and related compounds. Environ. Health Perspect 1996, 104 (Suppl. 1), 85–95. [Google Scholar]
- Shahba, M.; El-Khyat, Z.; El-Wassef, M.M.; Sliem, M.A.; Farid, O.; El-Tayen, T.A. Study of mammalin acute toicity of sodium yttrium fluoride, erbium and yttrium doped upconversion materials. Egyptian J. Chem., 2022, 65, 699–705. [Google Scholar]
- Aldrich Chemical Company, Gillingham, Dorset, UK. Safety Data Sheet for ytterbium (III) fluoride. https://www.sigmaaldrich.com/GB/en/sds/ALDRICH/432121. Accessed 16th Sptember 2023.
- Strem Chemicals Inc., Newburyport, MA, USA, Safety Data Sheet for ytterbium (III) fluoride, 2021.
- Chang, L.W.; Magis, L.; Suzuki, T. (eds), Toxicology of Metals; CRC Press: Boca Raton, Florida, USA, 1996. [Google Scholar]
- Pearson, R.G. Hard and Soft Acids and Bases. J. Am. Chem. Soc. 1963, 85, 3533–3539. [Google Scholar] [CrossRef]
- Haley, T.J. ; Pharmacology and toxicology of the rare earth elements. J. Pharm. Sci., 1965, 54, 663–670. [Google Scholar] [CrossRef] [PubMed]
- Pallares, R.M.; Hebery, D.D.A.; Loguinov, A.; Proctor, M.; Villalobos, J.A.; Bjornsrad, K.A.; Rosen, C.J.; Vulpe, C.D.; Anergel, R.J. Identifying toxicity mechanisms associated with early lanthanide exposure through multi-dimensional genome-wide screening. ACS Omega, 2022, 7, 34412–34419. [Google Scholar] [CrossRef] [PubMed]
- Sun, G.; Li, Z.; Liu, T.; Chen, J.; Wu,; Feng, X. Rare earth elements in street dust and associated health risk in a municipal industrial base of central China. Environ. Geochem. Health, 2017, 39, 1469–1486. [Google Scholar] [CrossRef] [PubMed]
- Whaites, E. Essentials of dental radiography and radiology, 3rd ed.Churchill Livingstone: London, UK, 2002. [Google Scholar]
- Collares, F.M.; Ogliari, F.A.; Lima, G.S.; Fontanella, V.R.C.; Piva, E.; Samuel, S.M.W. Ytterbium trifluoride as a radiopaque agent for dental cements. Int. Endod. J., 2010, 43, 792–797. [Google Scholar] [CrossRef] [PubMed]
- Swartz, R.S; Robbins, J.W. ; Post placement and restoration of endodontically treated teeth: a literature review. J. Endod., 2004, 30, 289–301. [Google Scholar] [CrossRef] [PubMed]
- Soares, C.J.; Santana, F.R.; Fonesca, R.B.; Martens, L.R.; Neto, F.H. In vitro analysis of the radiopacity of indirect composites and ceramic inlay systems and its influence on the detection of cement overhangs. Clin. Oral Investig., 2007, 11, 331–336. [Google Scholar] [CrossRef] [PubMed]
- Moszner, N; Salz, U. ; Recent developments of new components for dental adhesives and composites. Macromol. Mater. Eng., 2007, 292, 245–271. [Google Scholar] [CrossRef]
- Bowen, R.L.; Cleek, G.W. A new series of X-ray-opaque reinforcing fillers for composite materials. J. Dent. Res., 1972, 51, 177–182. [Google Scholar] [CrossRef] [PubMed]
- Matsumura, H.; Sneyoshi, M; Atsuta, M. Radiopacity and physical properties of titanium-polymethacrylate composite. J. Dent. Res., 1992, 71, 2–6. [Google Scholar] [CrossRef] [PubMed]
- Prentice, L.H.; Tyas, M.J.; Burrow, M.F. The effect of ytterbium fluoride and barium sulphate nanoparticles on the reactivity and strength of a glass-ionomr cement. Dent. Mater., 2006, 22, 746–751. [Google Scholar] [CrossRef]
- Bowen, R.L.; Cleek, G.W. X-ray opaque reinforcing fillers for composite materials. J. Dent. Res., 1969, 48, 79–82. [Google Scholar] [CrossRef]
- Ginebra, M.P.; Albuixech, L.; Fernandez-Barragan, E.; Aparicio, C.; Gil, F.J.; San Roman, J.; Vazquez, B.; Planell, J.A. Mechanical performance of acrylic bone cements containing different radioacifying agents. Biomaterials, 2002, 23, 1873–1882. [Google Scholar] [CrossRef]
- Young, A.; von der Fehr, F.R.; Sonju, T.; Nordbo, H. Fluoride release and uptake in vitro from a composite resin and two orthodontic adhesives. Acta Odontol. Scand., 1996, 54, 223–228. [Google Scholar] [CrossRef]
- Naoum, S.; Ellakwa, A.; Martin, F.; Swan, M. Fluoride release, recharge and mechanical property stability of various fluoride-containing resin composites. Oper. Dent., 2011, 36, 422–432. [Google Scholar] [CrossRef] [PubMed]
- Ferracane, J.L. Resin composite – state of the art. Dent. Mater., 2011, 27, 29–38. [Google Scholar] [CrossRef] [PubMed]
- Aoyagi, Y.; Takahashi, H.; Iwasaki, N.; Honda, E. Kurabayashi, T.; Radiopacity of experimental composite resins containing radiopaque materials. Dent. Mater. J., 2005, 24, 315–320. [Google Scholar] [CrossRef] [PubMed]
- Michl, R.J.; Rheinberger, V.M.; Ott, G. Radiopaque dental materials, US Patent 4,629, 746 1986. [Google Scholar]
- Ivoclar Vivadent, Safety Data Sheet for Tetric EvoFlow, dated 06. 03. 2019.
- Ivoclar Vivadent, Safety Data Sheet for Tetric EvoCeram, dated 31. 01. 2020.
- Harhash, A.Y.; El Sayad, I.I.; Zaghloul, A.G.S. A comparative in vitro study on fluoride release and water sorption of different flowable esthetic restorative materials. Eur. J. Dent., 2017, 11, 174–179. [Google Scholar] [CrossRef]
- Porenczuk, A.; Jankiewicz, B.; Naurecka, M.; Bartosewicz, B.; Sierakowski, B.; Gozdowski, D.; Kostecki, J.; Nasiłowska, B.; Mielczarek, A. A comparison of the remineralizing potential of dental restorative materials by analyzing their fluoride release profiles. Adv. Clin. Exp. Med. 2019, 28, 815–823. [Google Scholar] [CrossRef]
- Mathias, M.R.; Rathi, N.; Bendgude, V.D.; Tirupathi, S.; Chauhan, R.S.; Border, A.; Lath, T.; Shas, S.S. Comparative fluoride ion release pre and postrecharge situations among three different pediatric dental restorative materials: An in vitro study. Int. J. Clin. Pediatr. Dent. 2022, 15, 729–735. [Google Scholar]
- Attar, N.; Turgul, M.D. Fluoride release and uptake capacities of fluoride-releasing restorative materials. Oper. Dent., 2003, 28, 395–402. [Google Scholar]
- Dasgupta, S.; Saraswarthi, M.V.; Somayaji, K.; Pentapati, K.C.; Shetty, P. Comparative evaluation of fluoride release and recharge potential of novel and traditional fluoride-releasing restorative materials: An in vitro study. J. Conserv. Dent., 2018, 21, 622–626. [Google Scholar] [PubMed]
- Burgess, J.O.; Walker, R.; Davidson, J.M. Posterior resin-based composites: review of the literature. Pediatr. Dent., 2002, 24, 465–479. [Google Scholar] [PubMed]
- Xu, X.; Burgess, J.O. Compressive strength, fluoride release and recharge of fluoride-releasing materials. Biomaterials, 2003, 24, 2451–2461. [Google Scholar] [CrossRef] [PubMed]
- Mangota, V.; Sharma, S. A new alkasite restorative material – Cention N. Asian Pac. J. Health Sci., 2021, 8, 18–19. [Google Scholar] [CrossRef]
- Abdallah, R.M.; Aref, N.S. Development of newly formulated nanoalumina-alkasite-based restorative material. Int. J. Dent., 2021, 2021, article 9944909. [Google Scholar] [CrossRef]
- International Organization for Standardization. ISO, 6876: Dentistry - Root canal sealing materials. Geneva, Switzerland: International Organization for Standardization, 2012.
- American Dental Association. Specification no. 57 for endodontic filling materials. J. Am. Dent. Assoc. 1984, 108, 108. [Google Scholar]
- Tagger, M.; Katz, A. Radiopacity of endodontic sealers: development of a new method for direct measurement. J. Endod., 2003, 29, 751–755. [Google Scholar] [CrossRef] [PubMed]
- Rud, J.; Rud, V.; Munksgaard, E.C. Retrograde root filling with dentin-bonded modified resin composite. J. Endod., 1996, 22, 477–480. [Google Scholar] [CrossRef]
- Niederman, R.; Theodosopoulou, J.N. A systematic review of in vivo retrograde obturation materials. Int. Endod. J., 2003, 36, 577–585. [Google Scholar] [CrossRef]
- Collares, F.M.; Klein, M.; Santos, P.D.; Portella, F.F.; Ogliari, F.; Leitune, V.C.B.; Samuel, S.M.W. Inlfuence of radiopaque fillers on physicochemical properties of a model epoxy resin-based root canal sealer. J. Appl. Oral Sci., 2013, 21, 533–539. [Google Scholar] [CrossRef]
- De Souza, M.O.; Leitune, V.C.B.; Bohn, P.V.; Samuel, S.M.W.; Collares, F.M. Phyisical-mechanical properties of bis-EMA based root canal sealer with different fillers addition. J. Conserv. Dent., 2015, 18, 227–231. [Google Scholar] [PubMed]
- Sidhu, S.K.; Nicholson, J.W. A review of glass-ionomer cements for clinical dentistry. J. Funct. Biomater., 2016, 7, 16. [Google Scholar] [CrossRef] [PubMed]
- Antonijevic, D.; Jeschke, A.; Colovic, B. , Milovanovic, P.; Jevremovic, D.; vom Scheidt, A.; Hahn, M.; Amling, M.; Jokanovic, V.; Busse, B.; Djuric, M. Addition of a fluoride-containing radiopacifier improves micromechanical and biological charcateristics of modified calcium silicate cements. J. Endod., 2015, 41, 2050–2057. [Google Scholar] [CrossRef] [PubMed]
- Torabinejad, M.; Parirokh, M. Mineral trioxide aggregate: a comprehensive review – Part II: leakage and biocompatibility investigations. J. Endod., 2010, 36, 190–202. [Google Scholar] [CrossRef] [PubMed]
- Roberts, H.W.; Toth, J.M.; Berzins, D.W.; Charlton, D.W. Mineral trixide aggregate material use in endodontic treatment: a review of the literature. Dent. Mater., 2008, 24, 149–164. [Google Scholar] [CrossRef] [PubMed]
- Tawil, P.Z.; Duggan, D.J.; Galicia, J.C. MTA: A clinical review. Compend. Contin. Educ. Dent., 2015, 36, 247–264. [Google Scholar] [PubMed]
- Holland, R.; de Souza, V.; Nery, M.J.; Filho, J.A.O.; Bernabe, P.F.; Dezan Jr, E. Reaction of rat connective tissue to implanted dentin tube filled with mineral trioxide aggregate, Portland cement or calcium hydroxide. J. Endod., 1999, 25, 161–166. [Google Scholar] [CrossRef]
- Li, Q.; Coleman, N.J. The hydration chemistry of ProRoot MTA. Dent. Mater. J., 2015, 34, 458–465. [Google Scholar] [CrossRef]
- Taylor, H.F.W. Cement Chemistry; Academic Press: London, 1990. [Google Scholar]
- Li, Q.; Coleman, N.J. Early hydration of white Portland cement in the presence of bismuth oxide. Adv. Appl. Ceram., 2013, 112, 207–212. [Google Scholar] [CrossRef]
- Camilleri, J.; Pitt Ford, T.R. Review of constituents and properties of mineral trioxide aggregate. Int. Endod. J., 2006, 39, 747–754. [Google Scholar] [CrossRef]
- Camilleri, J. Hydration mechanisms of mineral trioxide aggregate. Int. Endod. J., 2007, 40, 462–470. [Google Scholar] [CrossRef]
- Mohamed, N.I.; Safy, R.K.; Elezz, A.F.A. Microtensile bond strength, marginla leakage, and antibacterial effect of bulk fill resin composite with alkaline fillers versus incremental nanohybrid composite resin. Eur. J. Dent., 2021, 15, 425–432. [Google Scholar]
- Lou, S.; Westbrook, J.A.; Schaus, S.E. Decarboxylative aldol reactions of allyl β-keto esters via heterobimetallic catalysts. Prep. Org. Chem., 2000, 41, 447–449. [Google Scholar]
- Zhang, L.J.; Lu, H-L. ; Wu, Z-W.; Huang, Y-S. Ytterbium triflate: A versatile catalyst in organic chemistry. Curr. Org. Chem., 2013, 17, 2906–2920. [Google Scholar] [CrossRef]
- Davis, M.F.; Levason, W.; Reid, G.; Webster, M. Synthesis and charactersation of tin (IV) fluoride complexes phosphine and arsine oxide ligands. Polyhedron, 2006, 25, 930–936. [Google Scholar] [CrossRef]
| Property | Value | Reference |
|---|---|---|
| Atomic number | 70 | 4 |
| Relative atomic mass | 173.04 | 4 |
| Stable isotopes (relative abundance) | 168 (0.13%), 170 (3.02% 171 (14.2%, 172 (21.8%), 173 (16.1%), 174 (31.9%, 176 (12.9%). |
4 |
| Oxidation states | +3, +2 | 4 |
| Atomic radius | 176 pm | 5 |
| Electronic configuration | [Xe]4f146s2 | 4 |
| Ionic radius (8 coordination) | 98.5 pm1 | 6, 7 |
| Ionic radius (6 coordination) | 86.8 pm1 | 6, 7 |
| Property | Value | |
|---|---|---|
| Appearance | White crystalline solid | |
| Relative molecular mass | 230.04 | |
| Melting point | 1157 °C | |
| Boiling point | 2380 °C | |
| Atomic radius | 176 pm | |
| Solubility in water | Insoluble | |
| Density | 8.17 g cm-1 |
| Material | Fluoride release/ppm | Reference |
|---|---|---|
| Tetric N-flow | 0.60 (0.07) | 36 |
| Tetric N-Ceram | 0.41 (0.08) | 40 |
| Property | CaWO4 | YbF3 | BaSO4 |
|---|---|---|---|
| Setting time/min | 501 | 388 | 385 |
| pH | 6.84 | 6.25 | 6.45 |
| Radiopacity/mm Al | 1.96 | 2.07 | 1.62 |
| Water sorption/μg/mm³ | 183.2 | 67.8 | 51.3 |
| Solubility/μg/mm³ | 200.1 | 10.7 | 13.2 |
| Cement | Working time/s | Setting time/s |
|---|---|---|
| GPA only (no additive) | 155.4 | 442.6 |
| GPA + 5% YbF3 | 64.6 | 213.0 |
| GPA + 5% BaSO4 | 132.4 | 376.0 |
| GPA + 15% YbF3 | 73.0 | 163.0 |
| GPA + 15% BaSO4 | 169.8 | 351.0 |
| Material | Composition |
|---|---|
| Cement 1 | Calcium silicate 30%, calcium carbonate 40%, YbF3 30% |
| Cement 2 Cement 3 |
Calcium silicate 17.5%, nano-HA 35%, gypsum 17.5%,YbF3 30% 70% Portland cement, 30% YbF3 |
| Property | Cement 1 | Cement 2 | Cement 3 |
|---|---|---|---|
| Setting time/min | 6 | 24 | 20 |
| pH | 9.38 | 9.23 | 9.43 |
| Radiopacity/mm Al | 5.45 | 4.90 | 5.75 |
| F- release/μg/L | 8.79 | 44.87 | 74.47 |
| Yb release/μg/cm2 | 0.073 | 0.16 | 1.35 |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
The radiopacity of specimens is typically measured on a specimen of size… The radiopacity value is determined using an aluminium step-wedge standard whose thickness ranges from 0.5 to 9.0 mm. The radiographic images are analysed using appropriate software that is able to measure the pixel density of the grey image. This gives values equivalent to thickness of aluminium as the measure of the radiopacity of the sample.
|
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





