Introduction
Cirrhosis, as a nowadays disease, is characterized by fibrosis and nodule formation of the liver. In the secondary plan, it is known as a chronic injury, which leads to alteration of the normal lobular organization of the liver. A complex of factors, such as life style, or environmentals, can injure the liver, and beside also including viral infections, toxins, hereditary. With each injury, the liver suffer alterations as fibrosis. Finally but after a long-standing injury, liver functionalteration, develop in time cirrhosis as a complex diseases.
Ethiology of the chronic liver diseases usually progress unfortunately in cirrhosis, following pathological mechanisms. In the research, the most common causes of cirrhosis are hepatitis C virus (HCV), alcoholic liver disease, and nonalcoholic steatohepatitis (NASH). Hepatitis B virus (HBV) and HCV are the most common causes [
1]. Other ethiological points of cirrhosis include autoimmune hepatitis, primary biliary cholangitis, primary sclerosing cholangitis, hemochromatosis, Budd-Chiari syndrome, Wilson disease, alpha-1 antitrypsin deficiency, drug-induced liver cirrhosis, and chronic right-sided heart failure [
1].
The cause of morbidity and mortality in cirrhosis is the development of portal hypertension and hyperdynamic circulation. Portal hypertension develops secondary to fibrosis and vasoregulatory alterations [
2].
Liver fibrosis it is known by excessive synthesis and deposition of connective tissue proteins. Interstitial collagens in the extracellular matrix of the liver has been discovered in this liver pathology. Hepatocytes alterations, results of an abnormal wound healing in response to chronic liver injury, previously mentioned in this written pages. The long term stimuli involved in the initiation of fibrosis leads to oxidative stress. Next point that concure to disease include mediators of molecular events involved in the pathogenesis of hepatic fibrosis. These processes lead to cellular injury and initiate inflammatory responses. As a response, cytokines and growth factors play a role as trigger activation and transformation of resting hepatic stellate cells into myofibroblast like cells. At the end of process, start an excessive synthesis of connective tissue proteins, including collagens. Uncontrolled and hepatocyte fibrosis results in distortion of lobular architecture of the liver. Pathologists show the nodular formations in the liver as a diagnosis of cirrhosis. The liver strucure injury and regeneration process could also results in genomic aberrations and mutations. Finally, develop hepatocellular carcinoma. This review try to cover various aspects of the molecular mechanisms involved in the pathogenesis of hepatic fibrosis. A great point of our this scientific orientation, is hepatic fibrosis diagnosis, with special emphasize on N-Nitrosodimethylamine (NDMA; Dimethylnitorsmaine, DMN) as the inducing agent [
3].
Prevention and treatment of liver cirrhosis are best done by an interdisciplinary medical team. This scientifically team, include a pathologist, a gastroenterologist, liver surgeon. Beside, a medical team include nurse practitioner, primary care provider and an internist. Liver cirrhosis is associated with systemic complications that can cause death of pacients. A liver transplant is not an option from different causes.
Weight loss of at least 7% is good for reneval pathological alterations of the liver structure.
Therapy methods and drugs, are more important, including antiviral medications in viral hepatitis, steroids, and immunosuppressant agents in autoimmune hepatitis, ursodeoxycholic acid and obeticholic acid in primary biliary cholangitis, copper chelation in Wilson disease, and iron chelation and phlebotomy in hemochromatosis [
4].
Material and methods
In order to analize morphological structural particularities, samples liver collected during necropsy, from healthy patients and from patients diagnosed with cirrhosis.
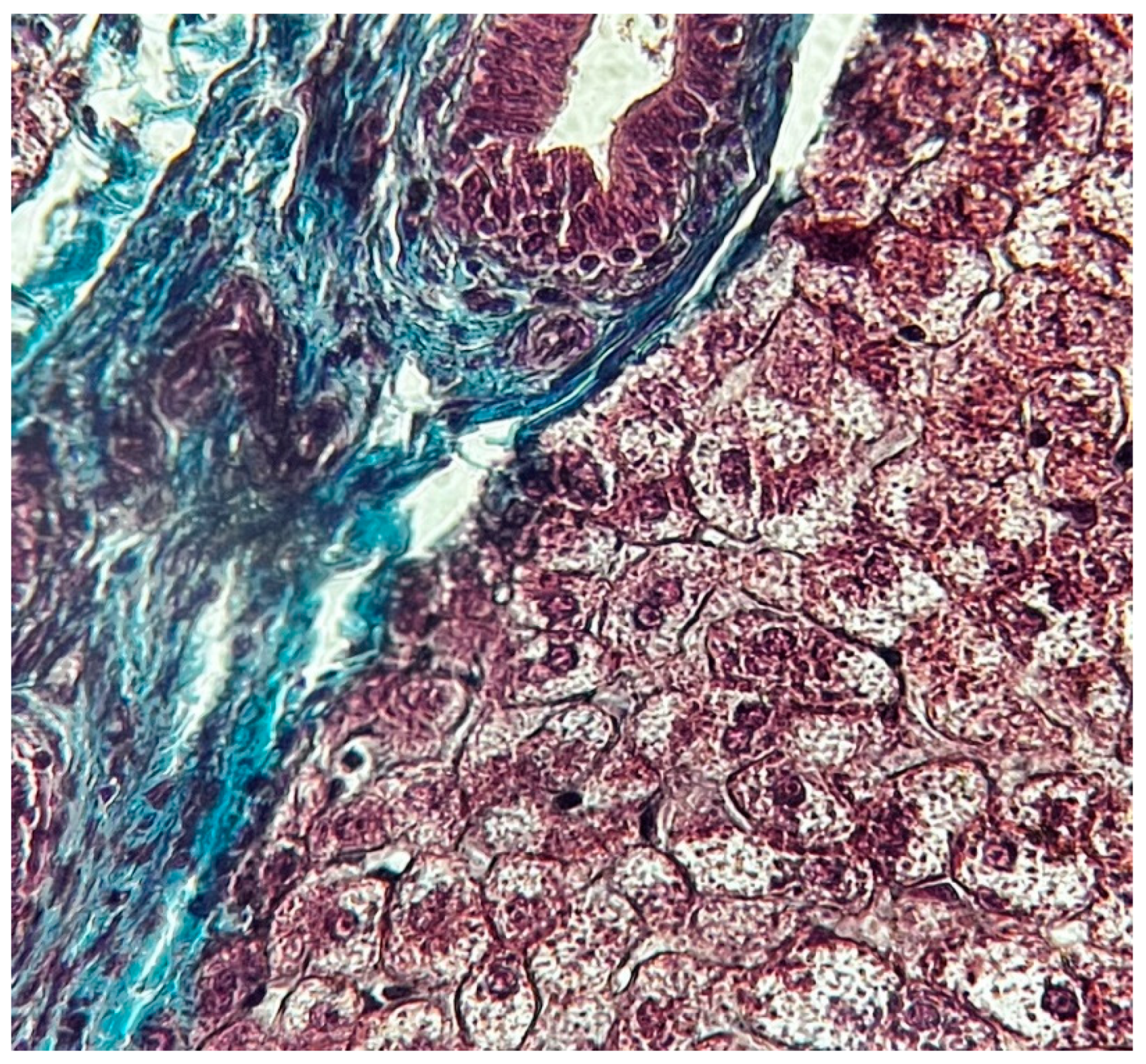
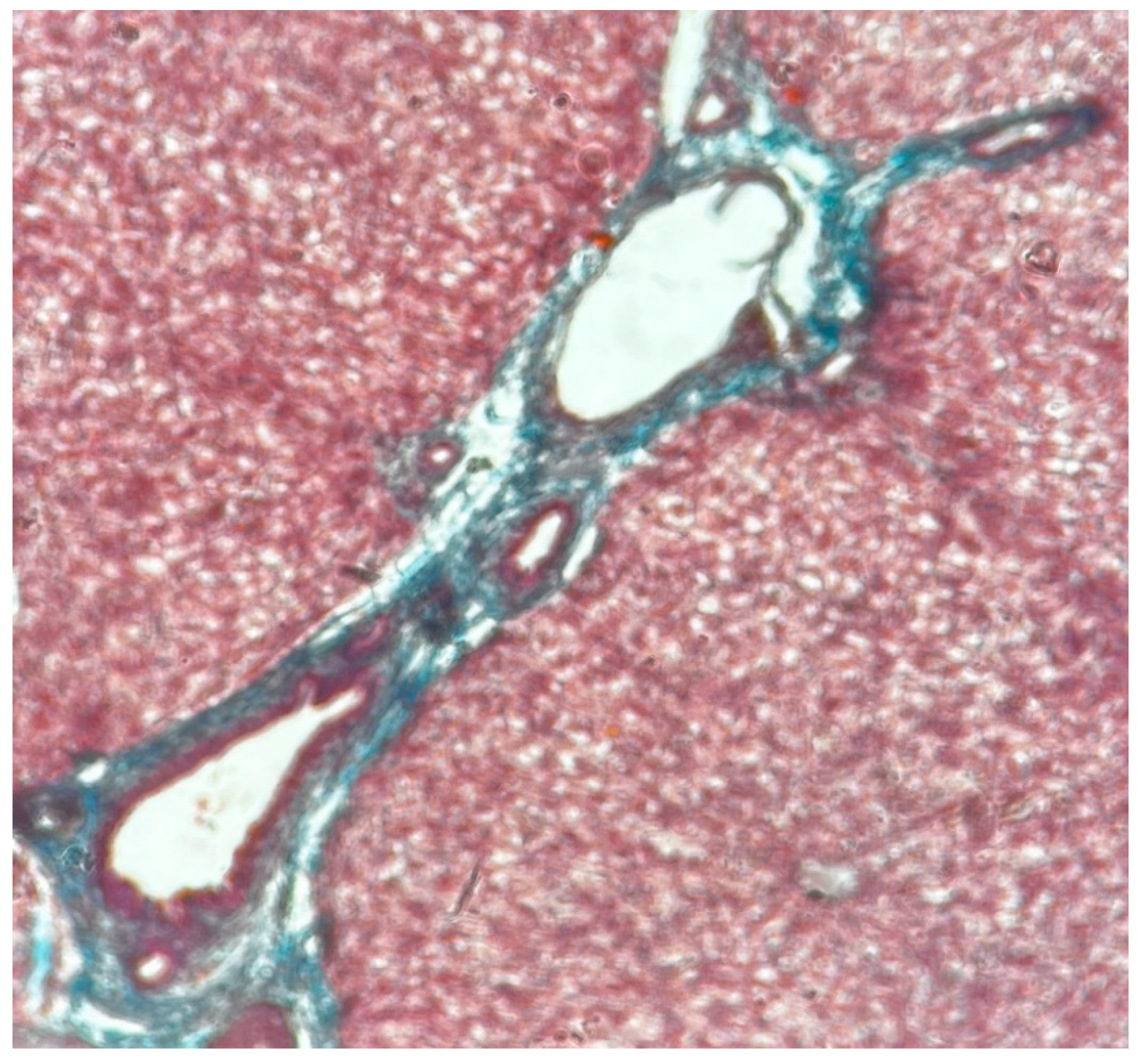
Following this purpose, were made permanent preparations that were stained with hematoxylin and eosin for observation at optical microscope. The process of the permanent microscopic preparations was based on prior knowledge of the steps from the classical method, using a standard H&E staining technique. Also normally liver samples, were observed by optical microscope using Goldner Szekely trichrome stains. Optical microscope examination were used lens with magnification x10 and x40.
Results
The functional unit of the liver is the lobule with hexagonal form. Kienann space is specific for liver strucutre, including a portal triad (portal vein, hepatic artery, bile duct) sits at each corner of the hexagon. Mitochondri as points observing with lens x40. Portal vein with enlarge lumen (
Figure 1).
Based on function and perfusion, hepatocytes are divided into three zones.
Zone I is considered to be the periportal region of hepatocytes and are the best perfused and first to regenerate due to their proximity to oxygenated blood and nutrients. Implication in oxidative metabolisms.
Zone II is defined as the pericentral region of the hepatocytes.
Zone III has the lowest perfusion due to its distance from the portal triad. Implication role in detoxification.
Also Kiernann space, hepatocytes, connective septa, in normal liver(
Figure 2).
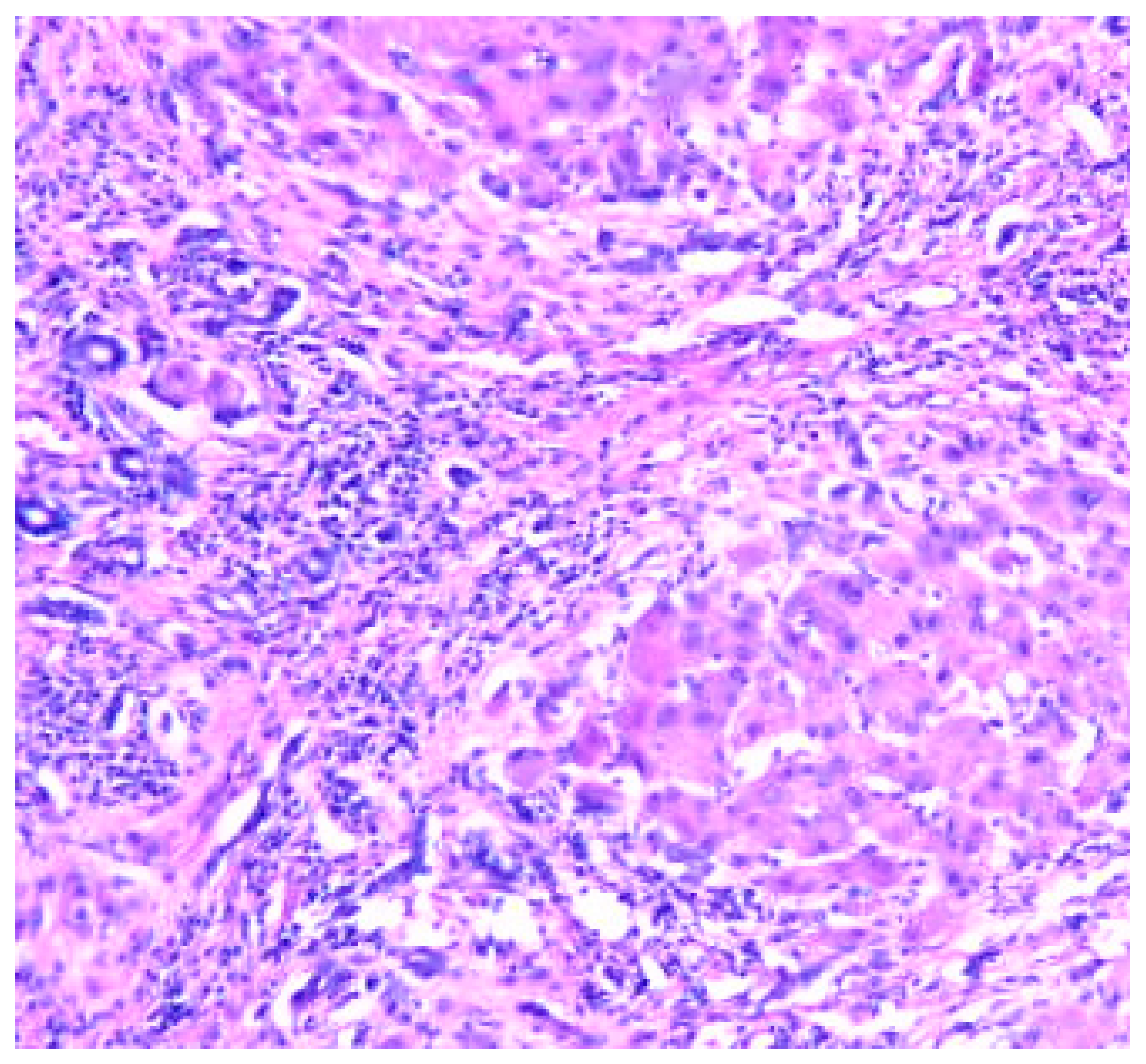
Cirrhosis is a result of continuous liver injury, inflammation, fibrosis, and necrosis. Commonly cause cirrhosis are chronic hepatitis B and C and also life style including alcoholism. The fibrosis present in cirrhosis occurs from the secretion of TGF-beta from the Ito cells in the space of Disse (
Figure 3).
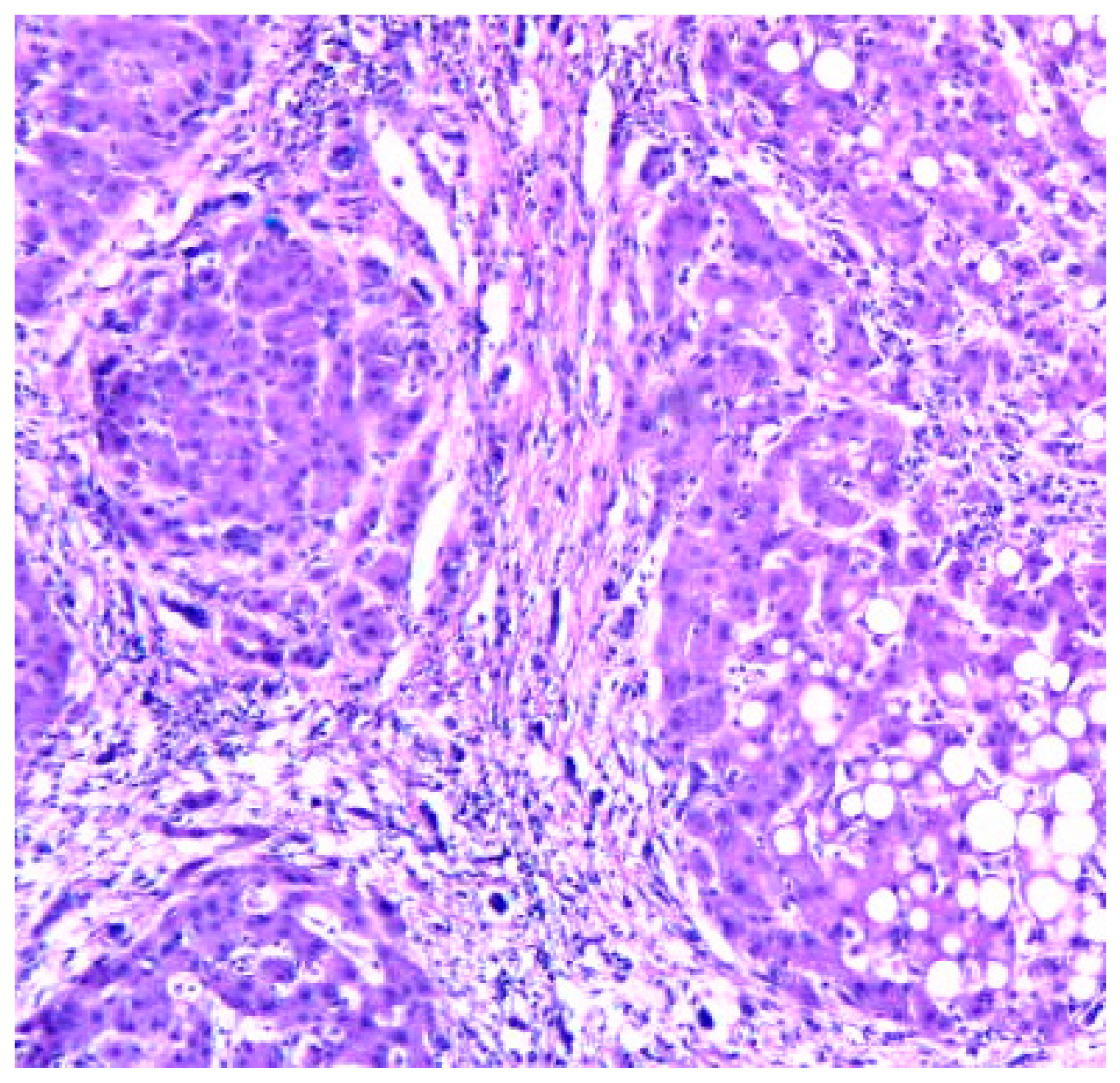
Cirrhosis usually represents with end-stage liver disease. Hepatitis C is the most damaging. Cirrhosis develops after a period of inflammation. The ill liver has parenchyma with fibrotic tissue and regenerative nodules (
Figure 4).
Liver fibrosis impairs hepatic function and causes structural change with different types of dameges.(5)
Clinically, liver cirrhosis is the severe period of chronic liver diseases. Early prevention and treatment of the causes of development and progression and pathogenic mechanism may slow down or reverse liver cirrhosis and its severe complications.
Decompensated liver cirrhosis and its complications, take attention to the clinicians. Various clinically signs as ascites, esophagogastric variceal bleeding, hepatic encephalopathy, acute kidney injury, and hepatocellular carcinoma, could be observing at the medical examination. Clearly that patients' quality of life is affected in liver cirrhosis.
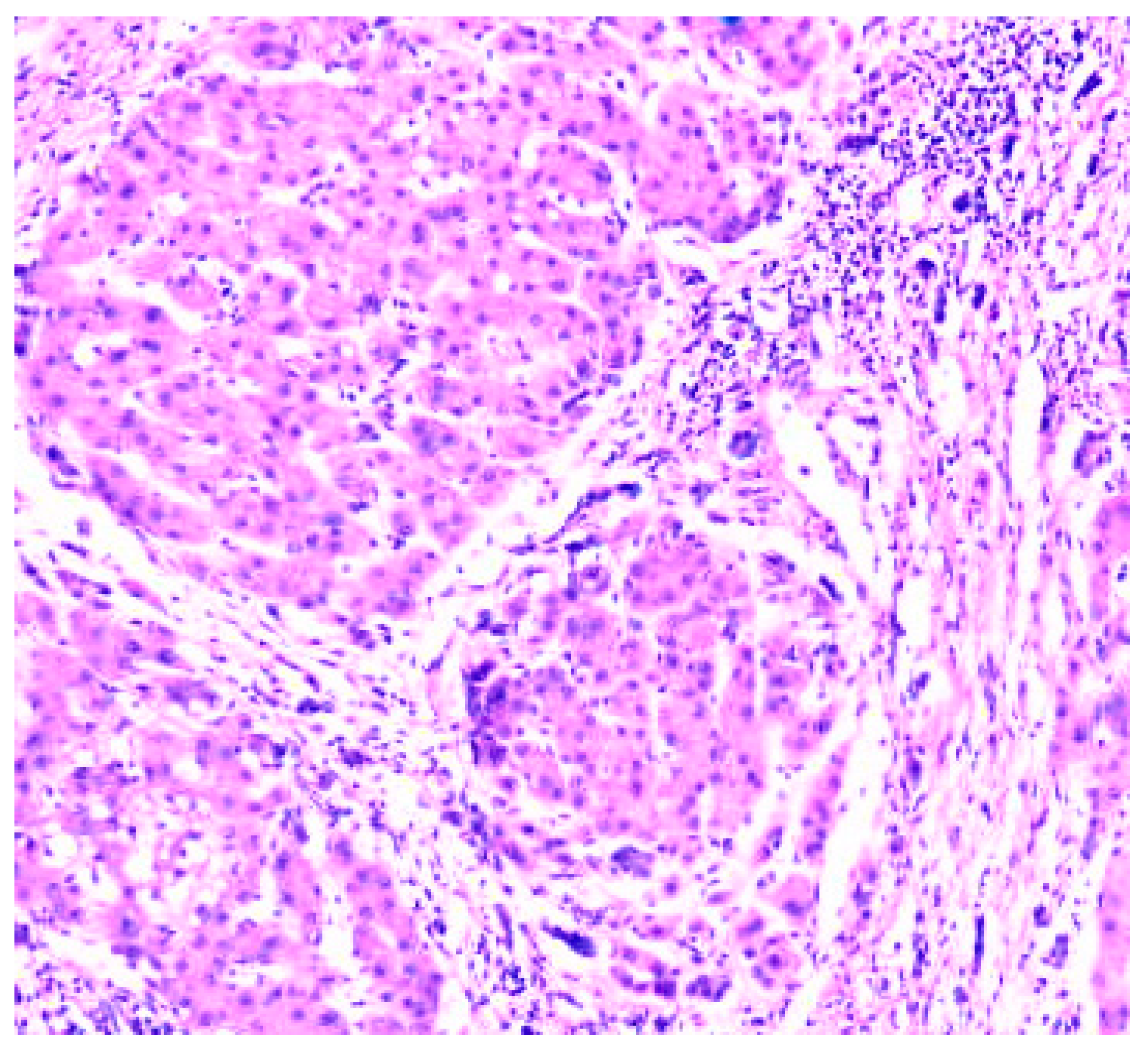
Figure 5.
Cirrhosis liver x10 H&E stain.
Figure 5.
Cirrhosis liver x10 H&E stain.
Liver fibrosis score, standard ultrasonography, and transient elastography are important for practicum. Also useful in identifying ill patients with no to minimal fibrosis or advanced fibrosis., medical tests.(6) In this medical direction, chronic liver disease management includes directed counseling, laboratory testing, and ultrasound monitoring.
The management of liver cirrhosis is centred on the clinical part. The proper treatment of the causes and complications and liver transplantation could be prioritaire.
Figure 6.
Cirrhosis liver x10 H&E stain.
Figure 6.
Cirrhosis liver x10 H&E stain.
The Child-Pugh score and model for end-stage liver disease (MELD) score are both used to assess and determine prognosis in cirrhotic patients. The MELD score uses creatinine, bilirubin, and INR. While both are used to create a predictive model for cirrhotic patients, the MELD score is the scale of choice for the evaluation of liver transplant patients.
Discusions
Patient lifestyle changes, unfortunately cannot cure cirrhosis. Complications accompanying hepatic cirrhosis include, portal hypertension, edema in the abdomen and lower extremities, splenomegaly, infections, hepatic encephalopathy.
Behavioral modifications can prevent or at least delay disease progression and provide symptomatic relief.
Lifestyle changes, include factors, as eliminating ethanol consumption and dietary interventions as possible low-sodium diet, in order to reduce water retention. Regulate protein intake according to their doctor's directions and some medical recommandations, will be proper in the treatment of cirrhosis.
Diferential diagnosis of cirrhosis include research directions reffering to neonatal iron storage diseases, HELLP(hemolysis, elevated liver enzymes, low platelets) syndrome of pregnancy, idiopathic drug reaction. More than, other diseases are included in the diferential diagnosis of cirrhosis. This are Tyrosinemia, Galactosemia, Fructose intolerance
Conclusions
HCC is the known common primary cancer in the liver. HCC has nowadays an incidence in increasing [
5].
Cirrhosis secondary to HBV and HCV is one of the common risk factor for liver degeneration in cirrhosis.
Practically monitoring of cirrhotic patients is recommended, with at least six monthly screenings. For monitorisation of liver disease, abdominal ultrasonography is better [
6].
Liver biopsy is the gold standard technique highly promising non-invasive methodology under development, that are used in diagnosis.
Liver transplantation (LT) is also an effective therapeutic option for the management of cirrhosis end-stage.
Relatively recently research investigations try to elucidate the signal transduction pathways that link hepatocytes alterations including cellular disfunctionality.
Author Contributions
Conceptualization; methodology; software; validation; formal analysis; investigation; resources.; data curation; writing—original draft preparation; writing—review and editing; visualization.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The author have disclosed no conflict of interest. This study was independently conducted without financial grants from any group or institution. Author have read and agreed to the published version of the manuscript.
References
- Naveau, S.; Perlemuter, G.; Balian, A. [Epidemiology and natural history of cirrhosis]. Rev Prat. 2005, 55, 1527–1532. [Google Scholar] [PubMed]
- Kim, M.Y.; Baik, S.K.; Lee, S.S. Hemodynamic alterations in cirrhosis and portal hypertension. Korean J Hepatol. 2010, 16, 347–352. [Google Scholar] [CrossRef]
- George, J.; Tsutsumi, M. Molecular mechanisms in the pathogenesis of N-nitrosodimethylamine induced hepatic fibrosis. Cell Death Dis. 2019, 10, 18. [Google Scholar] [CrossRef] [PubMed]
- Promrat, K.; Kleiner, D.E.; Niemeier, H.M.; Jackvony, E.; Kearns, M.; Wands, J.R.; Fava, J.L.; Wing, R.R. Randomized controlled trial testing the effects of weight loss on nonalcoholic steatohepatitis. Hepatology. 2010, 51, 121–129. [Google Scholar] [CrossRef] [PubMed]
- Hayward, K.L.; Weersink, R.A. Improving Medication-Related Outcomes in Chronic Liver Disease. Hepatol Commun. 2020, 4, 1562–1577. [Google Scholar] [CrossRef]
- Mittal, S.; El-Serag, H.B. Epidemiology of hepatocellular carcinoma: Consider the population. J Clin Gastroenterol. 2013, 47 Suppl. S2-6. [Google Scholar] [CrossRef]
- Schuppan, D.; Afdhal, N.H. Liver cirrhosis. Lancet. 2008, 371, 838–851. [Google Scholar] [CrossRef] [PubMed]
- Scaglione, S.; Kliethermes, S.; Cao, G.; Shoham, D.; Durazo, R.; Luke, A.; Volk, M.L. The Epidemiology of Cirrhosis in the United States: A Population-based Study. J Clin Gastroenterol. 2015, 49, 690–696. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.Y.; Baik, S.K.; Lee, S.S. Hemodynamic alterations in cirrhosis and portal hypertension. Korean J Hepatol. 2010, 16, 347–352. [Google Scholar] [CrossRef] [PubMed]
- John, S.; Thuluvath, P.J. Hyponatremia in cirrhosis: Pathophysiology and management. World J Gastroenterol. 2015, 21, 3197–3205. [Google Scholar] [CrossRef]
- Lata, J. Hepatorenal syndrome. World J Gastroenterol. 2012, 18, 4978–4984. [Google Scholar] [CrossRef] [PubMed]
- Promrat, K.; Kleiner, D.E.; Niemeier, H.M.; Jackvony, E.; Kearns, M.; Wands, J.R.; Fava, J.L.; Wing, R.R. Randomized controlled trial testing the effects of weight loss on nonalcoholic steatohepatitis. Hepatology. 2010, 51, 121–129. [Google Scholar] [CrossRef] [PubMed]
- Vinaixa, C.; Rubín, A.; Aguilera, V.; Berenguer, M. Recurrence of hepatitis C after liver transplantation. Ann Gastroenterol. 2013, 26, 304–313. [Google Scholar] [PubMed]
- Tangkijvanich, P.; Yee Hal, F., Jr. Cirrhosis--can we reverse hepatic fibrosis? Eur J Surg Suppl.. 2002, 587, 100–112. [Google Scholar]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).