1. Introduction
Over the past two decades, fully digital workflows have progressively transformed implant prosthodontics, offering new opportunities in terms of accuracy, predictability, and simplification of clinical procedures [
1]. While the literature has consolidated the effectiveness of these protocols in partially edentulous cases, the treatment of completely edentulous patients still represents one of the most complex challenges for clinicians. The main issue lies in the need to achieve an accurate and passive fit of full-arch prosthetic frameworks, as even minimal inaccuracies may lead to mechanical complications, such as screw loosening or material fracture, as well as biological complications, including peri-implant disease and marginal bone loss [
2,
3].
Several studies have demonstrated that inaccuracies in implant impressions originate from both clinical and laboratory procedures, emphasizing the critical role of impression-taking and workflow control [
4]. In recent years, numerous materials and innovative techniques have been proposed to increase the accuracy of digital protocols. However, most available evidence focuses on comparisons between different impression techniques in completely edentulous patients, whereas data on hybrid approaches combining conventional methods with advanced digital tools remain limited [
5].
Intraoral scan bodies (ISBs), used in combination with intraoral scanners (IOS), enable the digital transfer of implant position and orientation for prosthetic design. The accuracy of this procedure is influenced by multiple factors, including scanning technology, scanning strategy, and inter-implant distance [
6]. In fully edentulous arches, the absence of distinct anatomical landmarks further complicates image stitching and superimposition, thereby reducing scanning reliability [
5,
7]. Despite ongoing technological advances, desktop scanners and photogrammetry are still considered reference methods for impression-taking in full-arch implant cases, although clinical verification using a metallic framework try-in remains recommended [
8]. To streamline chairside workflows, significant improvements in ISB design and scanning techniques have recently been introduced; however, procedural standardization and clinician experience remain key determinants of clinically acceptable outcomes [
9].
An additional step forward may be represented by the integration of artificial intelligence (AI) into digital workflows. AI-based tools have shown potential in optimizing implant planning, improving digital impressions, and reducing operator-dependent variability [
10]. Nevertheless, clinical success still depends on implant design and clinician expertise, including comprehensive knowledge of digital workflows and software applications. Recent in vitro investigations have demonstrated promising accuracy and precision of AI-based systems for automated, real-time alignment in full-arch implant-supported restorations; however, robust in vivo clinical evidence is still lacking to confirm their effectiveness and reproducibility in daily practice [
10,
11].
In this context, clinical studies evaluating the reliability of innovative AI-based digital workflows are required to determine whether these systems may represent a valid alternative or adjunct to established protocols. Therefore, the primary aim of this clinical study was to evaluate and validate a digital impression workflow based on a novel AI-integrated tool (Smart-X) for full-arch (all-on-X) implant-supported rehabilitations in completely edentulous patients. Specifically, the study investigated whether this protocol could improve digital impression accuracy and optimize the intraoral scanning experience compared with conventional methods.
2. Materials and Methods
2.1. Study Design and Ethical Considerations
This study was designed as a multicenter prospective observational case series (Phase IV), conducted using exclusively CE-marked materials and devices applied within their intended use and standard clinical practice, without additional risks for the participants. All procedures were performed in accordance with the principles of the Declaration of Helsinki (2013 revision) and Good Medical Practice guidelines. Clinical data were anonymized to ensure patient confidentiality and were handled in compliance with the General Data Protection Regulation (GDPR, EU Regulation 2016/679).
Treatments were performed at two private dental clinics located in Rome, Italy, and Cairo, Egypt. Data analysis was conducted at the Department of Medicine, Surgery, and Pharmacy, University of Sassari, Italy. The research protocol was evaluated by the British University in Egypt and was deemed exempt from approval by a Research Ethics Committee, as it did not involve human subjects research requiring ethical oversight or continuing review (Research Approval Number: 25-064). The manuscript was prepared in accordance with the STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) guidelines.
2.2. Study Population
Completely edentulous patients aged 18 years or older requiring implant-supported full-arch rehabilitation in either the maxilla or mandible were considered eligible for inclusion. All patients were rehabilitated using an all-on-X protocol supported by four to eight implants with an internal conical connection, converted using multi-unit abutments (TSIII, Osstem Implant, Seoul, South Korea). Only patients with clinically osseointegrated implants demonstrating a minimum Implant Stability Quotient (ISQ) value of ≥67, measured using a Penguin resonance frequency analysis device (Osstem Implant), were included.
Patients were excluded if they presented with uncontrolled systemic diseases (ASA ≥ III); untreated or uncontrolled periodontal disease; active oral infections or peri-implant pathology; history of head and neck radiotherapy; use of medications affecting bone metabolism (e.g., bisphosphonates); severe parafunctional habits (e.g., bruxism); poor oral hygiene; or inability to comply with follow-up visits.
2.3. Prosthetic Protocol
The prosthetic workflow consisted of the following steps.
Digital impressions were acquired using SmartFlag scan bodies (Apollo, Pabianice, Poland) specifically designed for Osstem multi-unit abutments. To ensure accurate three-dimensional capture of implant positions, each SmartFlag scan body was rigidly connected to the multi-unit abutments prior to intraoral scanning. The distinctive geometry of the SmartFlag, characterized by well-defined planar and angular reference surfaces, facilitated consistent detection by the intraoral scanner software. During scanning, operators performed a systematic capture of the edentulous arch, ensuring complete visualization of each scan body from multiple orientations.
During data acquisition, the dedicated SmartX workflow algorithm automatically aligned scan body data with the corresponding digital libraries, allowing real-time validation of scan completeness and reducing operator-dependent variability. Once sufficient scan data were captured, the acquired images were automatically matched with the corresponding digital libraries, enabling a predictable transfer of implant spatial data into the prosthetic design environment and contributing to improved clinical accuracy of the digital impressions [
12].
All scans were performed using the Medit i900 intraoral scanner (Medit, Seoul, South Korea) following the dedicated SmartX workflow (Medit, South Korea), which includes a predefined scanning sequence optimized for all-on-X rehabilitations and incorporates AI-based real-time scan body recognition and alignment (
Figure 1) [
12].
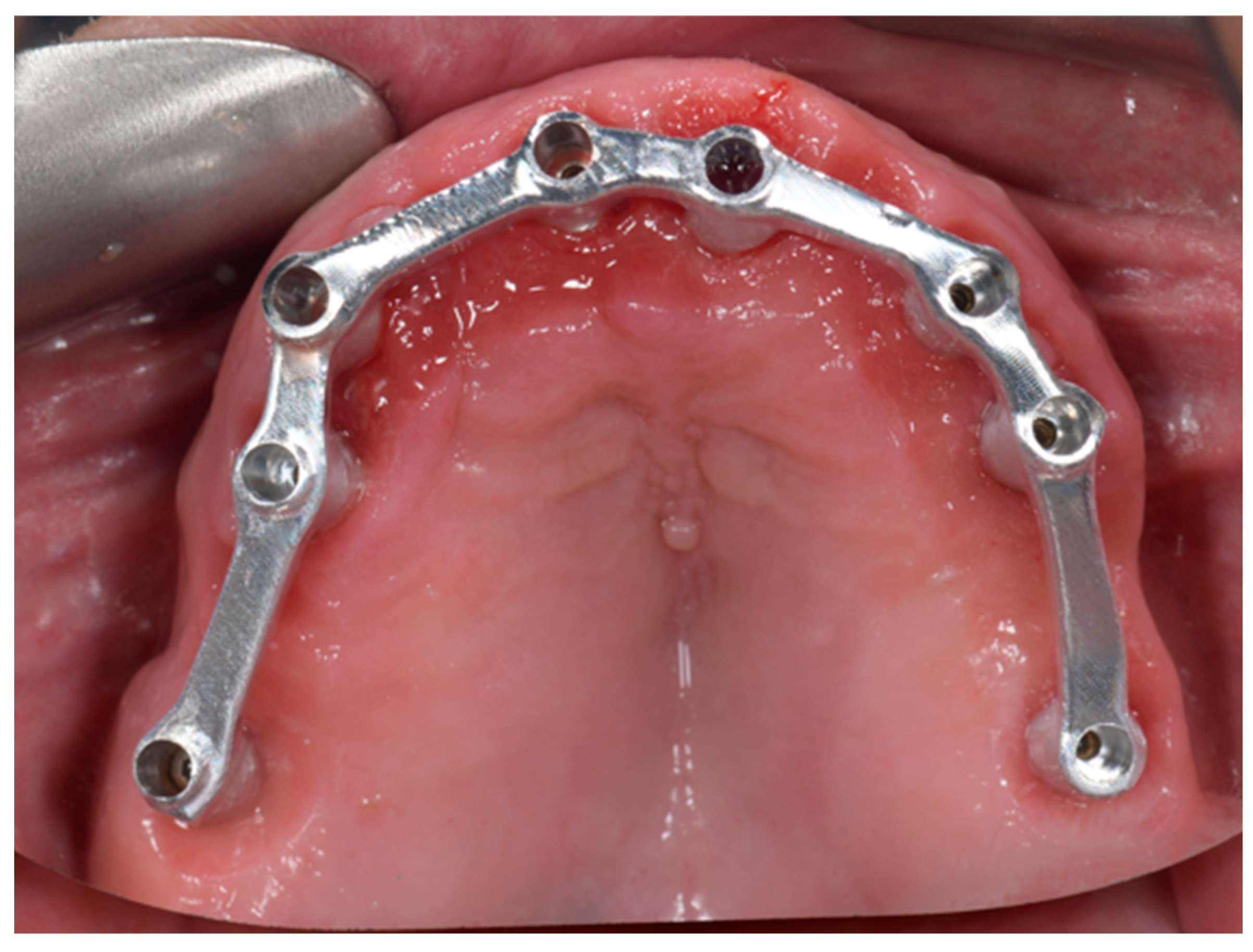
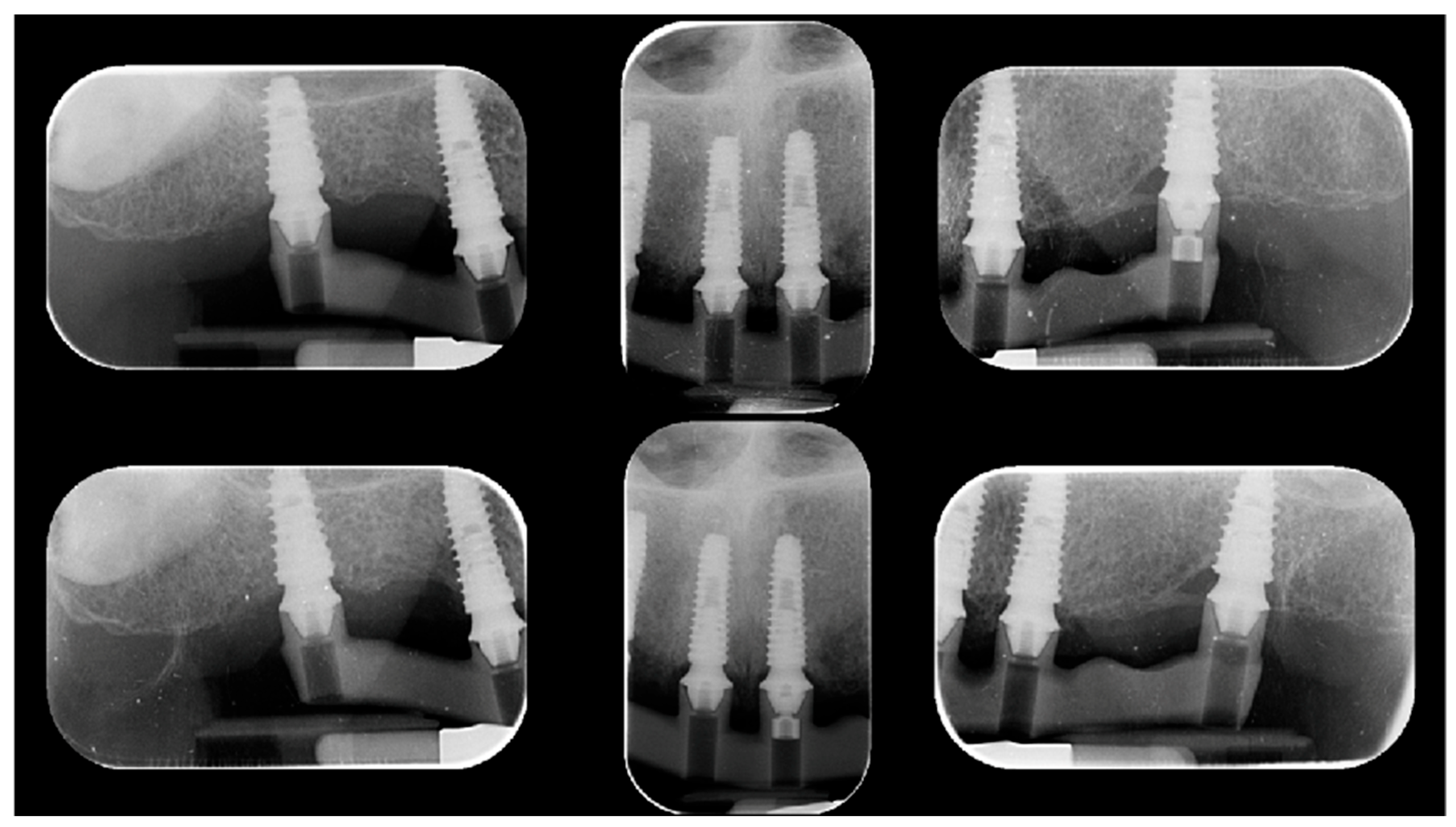
Following definitive impression acquisition, a milled metal verification bar was fabricated and clinically/radiographically evaluated (
Figure 2).
Passive fit of the metal verification bar was assessed using the one-screw test (Sheffield test) combined with tactile verification using a dental explorer. The Sheffield test consisted of tightening a single prosthetic screw to 5 Ncm at one terminal implant or at the most anterior implant, while leaving all other screws unfastened (
Figure 3). Standardized periapical radiographs were obtained using a Rinn holder.
Passive fit was assumed when the framework seated completely without visible gaps, rocking, or distortion at the remaining implant interfaces. Conversely, lifting or marginal discrepancies detected clinically or radiographically were interpreted as evidence of misfit [
13,
14].
Subsequently, the definitive monolithic zirconia prosthesis bonded to a CAD/CAM titanium bar was delivered following additional visual and tactile verification of passive fit (
Figure 4) according to the the screw resistance test. All prosthetic screws were initially tightened to 5 Ncm and then progressively tightened from 5 to 20 Ncm using a calibrated universal torque wrench (TorqControl, Anthogyr).
Patients were recalled every three months up to a 6-month follow-up period to evaluate the presence of biological or technical complications (
Figure 5).
2.4. Primary and Secondary Outcomes
The primary outcome was the clinical accuracy of digital impressions, evaluated through the following assessments:
Visual and tactile inspection, recorded as a dichotomous outcome (acceptable passive fit: yes/no).
One-screw (Sheffield) test, recorded as a dichotomous outcome (acceptable passive fit: yes/no).
The screw resistance test was recorded as a dichotomous outcome (acceptable passive fit: yes/no) using the manual driver (TorqControl, Anthogyr). All prosthetic screws were initially tightened to 5 Ncm and subsequently progressively tightened up to 20 Ncm, in accordance with the manufacturer’s recommendations (Osstem Implant). During progressive tightening, the angular displacement required to reach the final torque value was visually and clinically assessed. The angular displacement (arc length) between the torque values of 5 Ncm (point A) and 20 Ncm (point B) was evaluated and compared as an indirect indicator of framework seating and resistance [
15]. Based on this assessment, passive fit was classified as acceptable or non-acceptable.
Secondary outcomes included implant and prosthesis survival rates, as well as the incidence of biological complications (e.g., peri-implant mucositis, peri-implantitis) and technical complications (e.g., screw loosening, framework fracture).
2.5. Statistical Analysis
Statistical analysis was performed on patient demographic variables (age and sex) and on study outcomes. Categorical variables were expressed as frequencies and percentages. The accuracy of the digital impression protocol, assessed by visual and tactile inspection, one-screw test, and screw resistance test, was analyzed as a dichotomous variable (passive fit: yes/no). Descriptive statistics were used to summarize all outcomes. Statistical analyses were performed using dedicated statistical software, with the level of significance set at α = 0.05.
3. Results
3.1. Study Population and Baseline Characteristics
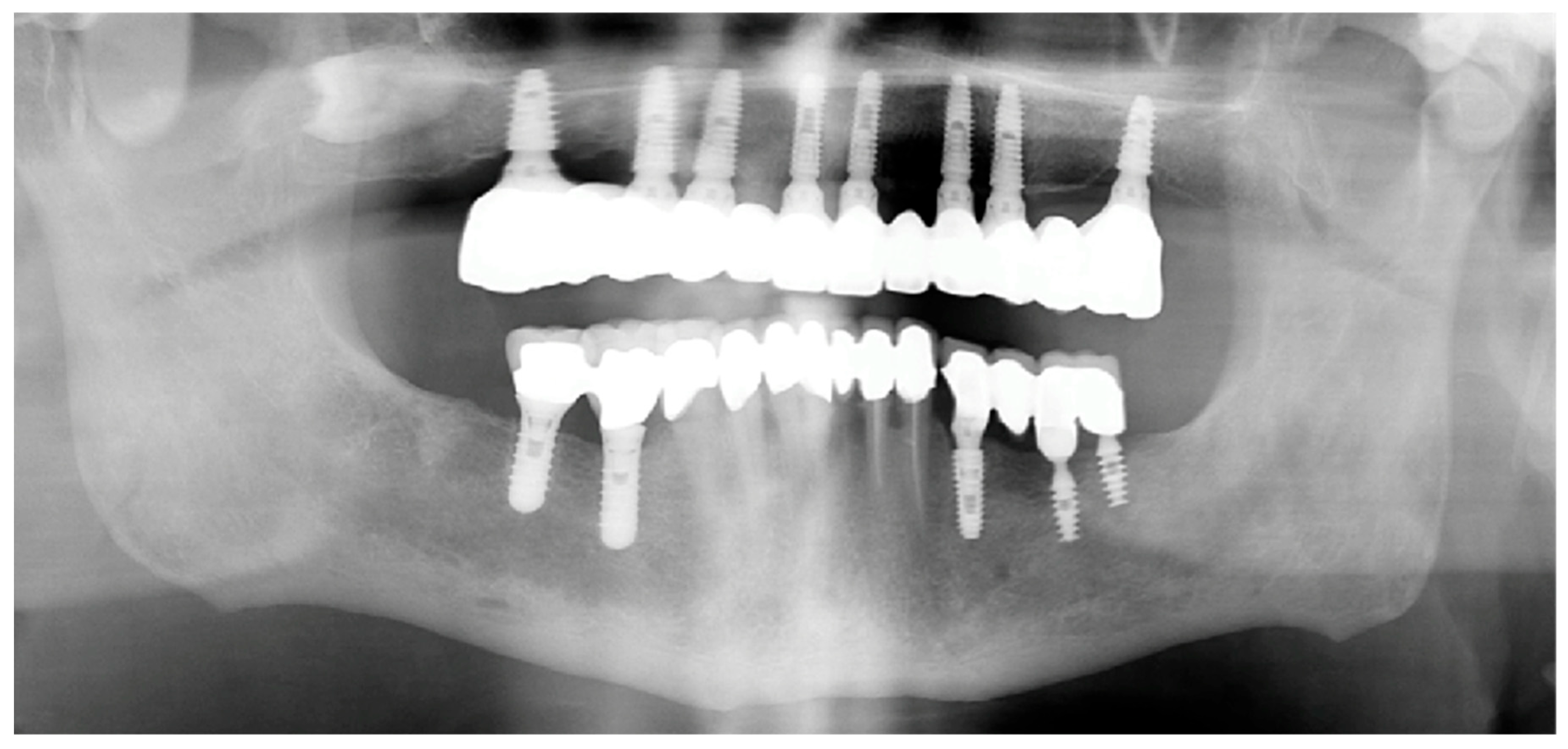
A total of 10 consecutive completely edentulous patients were enrolled, treated, and followed for a minimum period of 6 months. No patients were excluded after enrollment, and no dropouts occurred during the follow-up period. The study population consisted of 7 males and 3 females, with a mean age of 62 years. A total of 54 implants (TSIII Osstem Implant) were placed, with each patient receiving between 4 and 8 implants (mean: 5.4 implants per patient). All the implants were rehabilitated with multi abutments (Osstem Implant). Seven patients were rehabilitated in the maxilla and three in the mandible. Implant placement was performed using guided surgery (OneGuide, Osstem Implant) in five patients and free-hand surgery in the remaining five patients. Immediate loading was applied in four cases. Two patients were light smokers (<10 cigarettes/day). Data are summarized in
Table 1.
3.2. Primary Outcome: Accuracy of Digital Impressions
The clinical accuracy of the digital impression protocol was assessed using visual and tactile inspection, the one-screw (Sheffield) test, and the screw resistance test.
- -
Visual and tactile inspection demonstrated an acceptable passive fit in all 10 cases (100%).
- -
Similarly, the one-screw (Sheffield) test showed complete passive seating of the verification framework in all patients, with no detectable gaps, rocking, or distortion, corresponding to a 100% positive outcome.
- -
The screw resistance test also yielded positive results in all 10 cases. During progressive tightening from 5 to 20 Ncm, an increased angular displacement of approximately 60° (corresponding to one-sixth of a full rotation) was consistently observed across all cases, indicating uniform framework seating without resistance discrepancies. Overall, all accuracy assessments resulted in dichotomous “yes” outcomes in all patients.
3.3. Secondary Outcomes: Implant and Prosthesis Survival
At the 6-month follow-up, no implant failures were recorded, resulting in an implant survival rate of 100%. Similarly, no prosthesis failures occurred, yielding a prosthesis survival rate of 100%. No biological complications, including peri-implant mucositis or peri-implantitis, were observed during the follow-up period. Likewise, no technical complications, such as screw loosening or framework fracture, were recorded in any of the treated cases. Data are summarized in
Table 2.
4. Discussion
The present prospective clinical study evaluated the accuracy of a novel AI-integrated digital impression workflow for full-arch implant-supported rehabilitations in completely edentulous patients. The main finding of this investigation was that the SmartX workflow, used in combination with extended SmartFlag scan bodies, achieved a clinically acceptable passive fit in all cases, as confirmed by visual and tactile inspection, the one-screw (Sheffield) test, and the screw resistance test. Direct comparison of the present results with existing literature is not possible, as to the best of the authors’ knowledge this study represents the first prospective clinical investigation evaluating the SmartX AI-assisted digital workflow for full-arch implant-supported rehabilitations.
The SmartFlag scan bodies used in this study feature high-contrast geometry and stable reference surfaces, which facilitate automated recognition and registration within the digital workflow. This design reduces the risk of partial data loss or scan body misalignment, a well-known limitation of intraoral scanning in full-arch cases where anatomical landmarks are scarce or absent [
5,
6,
7]. The reliable identification of implant position and orientation is particularly critical in completely edentulous arches, where cumulative stitching errors may compromise the accuracy of the digital impression [
6,
7].
The consistent achievement of passive fit observed in this study supports the hypothesis that extended scan bodies, when combined with AI-assisted real-time alignment, may improve the robustness of digital full-arch workflows. These findings align with previous systematic reviews reporting that scan body geometry, scanning strategy, and inter-implant distance significantly influence impression accuracy, especially in edentulous scenarios [
6,
9].
Passive fit remains a cornerstone concept in implant prosthodontics, as misfit between the prosthetic framework and osseointegrated implants may induce internal stresses within the prosthesis, the implant components, and the surrounding bone [
2,
14]. Although a universally accepted definition of passive fit is lacking, Jemt proposed that an “acceptable” passive fit corresponds to a misfit below approximately 150 µm, a threshold considered biologically tolerable and unlikely to induce long-term complications [
14]. Nevertheless, truly ideal passive fit is rarely achievable in clinical practice, and some degree of biologic tolerance to misfit appears to exist [
15].
Several authors have emphasized that even clinically undetectable misfits may generate stresses that contribute to technical complications such as screw loosening or framework fracture, as well as biological complications affecting peri-implant tissues [
2,
3]. Therefore, the consistent achievement of positive outcomes across all passive fit assessment methods in the present study is clinically relevant, particularly in the context of full-arch rehabilitations, which are more susceptible to cumulative inaccuracies.
The one-screw (Sheffield) test remains one of the most widely used qualitative clinical methods for evaluating the accuracy of implant position transfer and the passive fit of implant-supported frameworks prior to definitive prosthesis delivery [
13]. In the present study, the Sheffield test confirmed complete framework seating in all cases, supporting the reliability of the digital impression workflow. In addition, the screw resistance test provided further indirect validation of framework accuracy. The consistent angular displacement of approximately 60° observed during progressive torque application from 5 to 20 Ncm suggests uniform seating behavior without localized resistance discrepancies. The pitch of the screws used (defined as the distance between adjacent threads measured parallel to the screw axis) was 0.3 mm. Consequently, a 60° rotation—corresponding to one-sixth of a full turn—results in a vertical displacement of approximately 50 microns (µm) of the prosthesis during tightening from 5 to 20 Ncm.
In the present study, a uniform vertical displacement was observed across all tested screws, indicating consistent framework seating. Achieving a passive fit is considered a fundamental prerequisite in implant-supported prosthetic rehabilitations, as it minimizes the induction of preload and residual stresses within the implant–prosthesis complex. Inadequate passive fit may generate tension at the implant–abutment and framework interfaces, leading to unfavorable stress concentration. Over time, these biomechanical imbalances may contribute to mechanical complications such as screw loosening, screw or framework fracture, and, in severe cases, implant failure [
14,
15].
This finding is consistent with recent investigations proposing the screw resistance test as a clinically useful method to detect misfit-related discrepancies in implant-supported prostheses [
15].
The innovative aspect of this study lies in its design as the first prospective clinical evaluation of extended scan bodies combined with the SmartX AI-based workflow for all-on-X full-arch digital implant rehabilitations. Previous investigations on AI-assisted digital impression workflows have been limited to in vitro studies or isolated clinical reports [
11,
12]. Therefore, the present work represents the first systematic clinical validation of this methodology.
The results of this clinical study corroborate previous in vitro findings demonstrating high accuracy and precision of AI-based alignment systems for full-arch digital impressions [
12]. Importantly, the translation of these results into a clinical setting supports the feasibility and reliability of this approach in routine practice.
This study presents several limitations. First, the relatively small sample size and the short follow-up period limit the generalizability of the results and preclude long-term evaluation of biological and technical outcomes. However, this investigation was primarily designed to assess the clinical accuracy of digital impressions, rather than long-term prosthetic performance. Second, the absence of a control group does not allow direct comparison with conventional impression techniques. Nonetheless, the prospective design and the consistency of outcomes across multiple accuracy assessments strengthen the validity of the findings.
5. Conclusions
Within the limitations of this prospective clinical study, the SmartX AI-integrated digital workflow combined with extended SmartFlag scan bodies demonstrated high clinical accuracy for full-arch implant-supported rehabilitations in completely edentulous patients. All evaluated cases achieved acceptable passive fit, as confirmed by multiple complementary clinical assessment methods.
These findings suggest that AI-assisted digital impression workflows may represent a reliable and clinically viable alternative to conventional protocols for full-arch implant prosthodontics. Further controlled clinical studies with larger sample sizes and longer follow-up periods are required to confirm these results and to evaluate long-term biological and technical outcomes.
Supplementary Materials
The following supporting information can be downloaded at the website of this paper posted on Preprints.org. The original contributions presented in the study are included in the article, further inquiries can be directed to the corresponding authors.
Author Contributions
Conceptualization, M.T. and M.Q.; methodology, M.T.; software, M.Q.; formal analysis, M.T.; investigation, M.T.; M.F.El A.; resources, D.G.; data curation, M.O. and A.A.; writing—original draft preparation, M.T. and C.C.; writing—review and editing, D.C. and C.C.; supervision, S.M.M. and F.M.C.. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
All procedures were performed in accordance with the principles of the Declaration of Helsinki (2013 revision) and Good Medical Practice guidelines. Clinical data were anonymized to ensure patient confidentiality and were handled in compliance with the General Data Protection Regulation (GDPR, EU Regulation 2016/679). Treatments were performed at two private dental clinics located in Rome, Italy, and Cairo, Egypt. Data analysis was conducted at the Department of Medicine, Surgery, and Pharmacy, University of Sassari, Italy. The research protocol was evaluated by the British University in Egypt and was deemed exempt from approval by a Research Ethics Committee, as it did not involve human subjects research requiring ethical oversight or continuing review (Research Approval Number: 25-064). The manuscript was prepared in accordance with the STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) guidelines.
Informed Consent Statement
Written informed consent has been obtained from the patients to publish this paper.
Data Availability Statement
Dataset available on request from the authors.
Acknowledgments
The authors would like to thank Rhein83, in the persons of Gianni Storni and Raffaele Lombardo, for making their research facilities available for the execution of the static and dynamic mechanical tests. The authors also wish to thank Osstem Implant for performing the finite element analysis (FEA) and for carrying out and sharing the results of the initial static loading tests. Finally, the authors acknowledge Osstem Implant Headquarters for kindly providing the materials used in this study.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Rutkūnas, V. (2024). Intraoral scanners in implant prosthodontics: A narrative review. Journal of Dentistry.
- Karl, M., & Taylor, T. D. (2004). Effect of implant-level discrepancies on the fit of implant frameworks. Journal of Prosthetic Dentistry, 91(4), 341–347. [CrossRef]
- Schwarz, F., Hegewald, A., & Becker, J. (2014). Impact of implant–abutment connection and positioning on marginal bone loss. Clinical Oral Implants Research, 25(9), 1038–1045. [CrossRef]
- Albanchez-González, M. I., Brinkmann, J. C. B., Peláez-Rico, J., López-Suárez, C., Rodríguez-Alonso, V., & Suárez-García, M. J. (2022). Accuracy of digital dental implant impression taking with intraoral scanners compared with conventional impression techniques: A systematic review of in vitro studies. International Journal of Environmental Research and Public Health, 19(4), 2026. [CrossRef]
- Srivastava, G., et al. (2023). Accuracy of intraoral scanners for recording completely edentulous arches: A systematic review. Dentistry Journal, 11(10), 241. [CrossRef]
- Gehrke, P., Rashidpour, M., Sader, R., & Weigl, P. (2024). Factors influencing the accuracy of intraoral scanning in implant dentistry: A systematic review. International Journal of Implant Dentistry, 10, 20. [CrossRef]
- Giménez, B., Özcan, M., Martínez-Rus, F., & Pradíes, G. (2015). Accuracy of digital impressions in implant dentistry: A systematic review. Clinical Oral Implants Research, 26(Suppl 11), 13–24. [CrossRef]
- Tohme, H., et al. (2021). Accuracy of implant-level intraoral scanning and photogrammetry: An in vitro study. Applied Sciences, 11(21), 9859. [CrossRef]
- Vieira, F. L., Carnietto, M., Cerqueira Filho, J. R. A., Bordini, E. A. F., Oliveira, H. F. F., Pegoraro, T. A., & Santiago Junior, J. F. (2025). Intraoral scanning versus conventional methods for obtaining full-arch implant-supported prostheses: A systematic review and meta-analysis. Applied Sciences, 15(2), 533. [CrossRef]
- Revilla-León, M., et al. (2021). Artificial intelligence applications in implant dentistry: A systematic review. Journal of Prosthetic Dentistry, 125(4), 569–577. [CrossRef]
- Róth, I., et al. (2025). Artificial intelligence-based alignment systems for full-arch digital impressions: Accuracy and clinical significance. Journal of Dentistry.
- Tallarico, M., Qaddomi, M., De Rosa, E., Cacciò, C., Meloni, S. M., Gendviliene, I., Att, W., Bourgi, R., Lumbau, A. M., & Cervino, G. (2025). Effectiveness of an AI-assisted digital workflow for complete-arch implant impressions: An in vitro comparative study. Dentistry Journal, 13(10), 462. [CrossRef]
- Sheffield. (1997). Sheffield test for assessment of passive fit in implant-supported prostheses. British Dental Journal.
- Jemt, T. (1991). Failures and complications in 391 consecutively inserted fixed prostheses supported by Brånemark implants. International Journal of Oral & Maxillofacial Implants, 6, 270–276.
- Rutkunas, V., Dirse, J., Kules, D., Mischitz, I., Larsson, C., & Janda, M. (2024). Misfit simulation on implant prostheses with different combinations of engaging and nonengaging titanium bases. Part 2: Screw resistance test. The Journal of prosthetic dentistry, 131(2), 262–271. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2026 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).