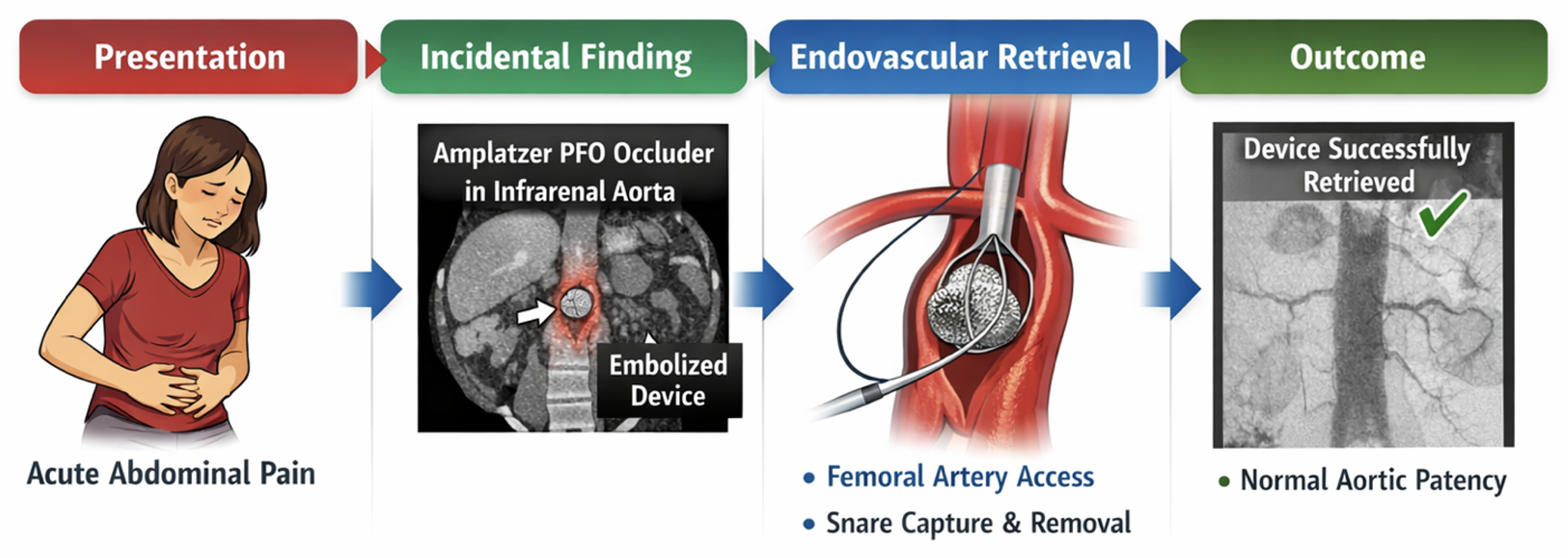
1. Introduction and Clinical Significance
Percutaneous closure of patent foramen ovale (PFO) has become a widely accepted therapeutic strategy in selected patients, particularly for secondary prevention of cryptogenic stroke and, in some cases, for the management of migraine with aura. The introduction of transcatheter occlusion devices, such as the Amplatzer occluder, has significantly reduced procedural invasiveness and is associated with high success rates and a low incidence of complications.
Despite the overall safety of this technique, device-related complications may occur. Among these, device migration or embolization represents a rare but potentially serious event, with reported incidences below 1%. Migration can occur early or in a delayed fashion and may involve various vascular territories, including the cardiac chambers, pulmonary arteries, or the systemic arterial circulation. When migration occurs, prompt identification is crucial, as the presence of a foreign body within the arterial system may lead to vascular obstruction, ischemic complications, or embolic events.
Imaging plays a central role in the diagnosis of device migration, often allowing incidental detection during investigations performed for unrelated clinical indications. Advances in endovascular techniques have made percutaneous retrieval the preferred treatment in most cases, avoiding open surgical intervention.
2. Case Presentation
An 18-year-old woman presented to the emergency department with acute-onset abdominal pain. Her medical history was notable for percutaneous closure of a PFO using an Amplatzer occluder performed approximately one month earlier at another institution. No other relevant comorbidities were reported.
On admission, the patient was hemodynamically stable, alert, and oriented. Physical examination revealed a soft, mildly tender abdomen without signs of peritonitis. Laboratory tests showed mild anemia (hemoglobin 11.5 g/dL) and elevated D-dimer levels, while coagulation parameters and cardiac biomarkers were within normal limits.
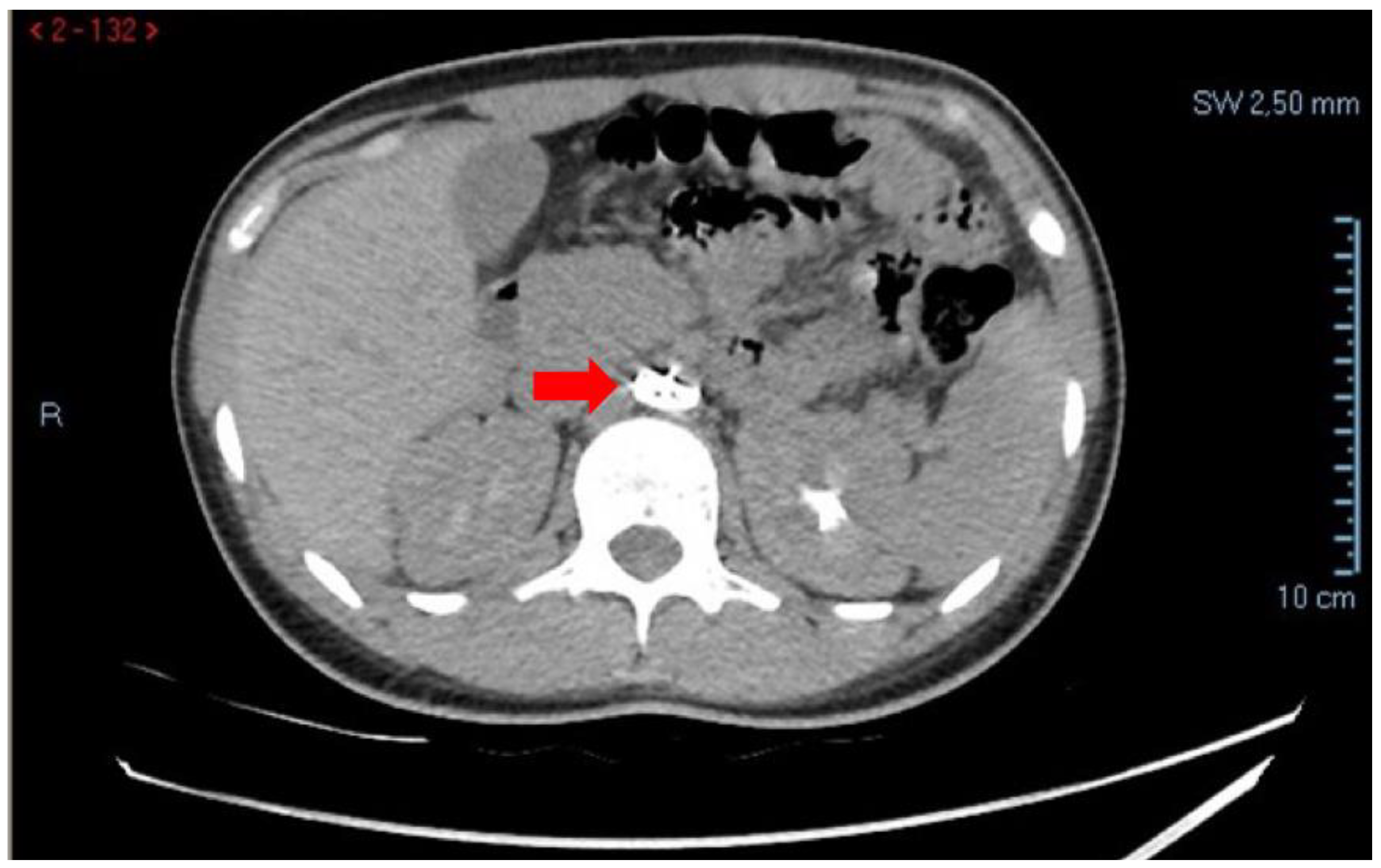
Given the persistence of abdominal pain, contrast-enhanced CT of the abdomen and thoracic aorta was performed. Imaging demonstrated hemoperitoneum secondary to a hemorrhagic ovarian cyst, with blood collection in the Douglas pouch and peritoneal recesses. Incidentally, CT also revealed migration of the Amplatzer device into the infra-renal abdominal aorta, with preserved patency of the renal arteries and no evidence of vascular obstruction or ischemia (
Figure 1).
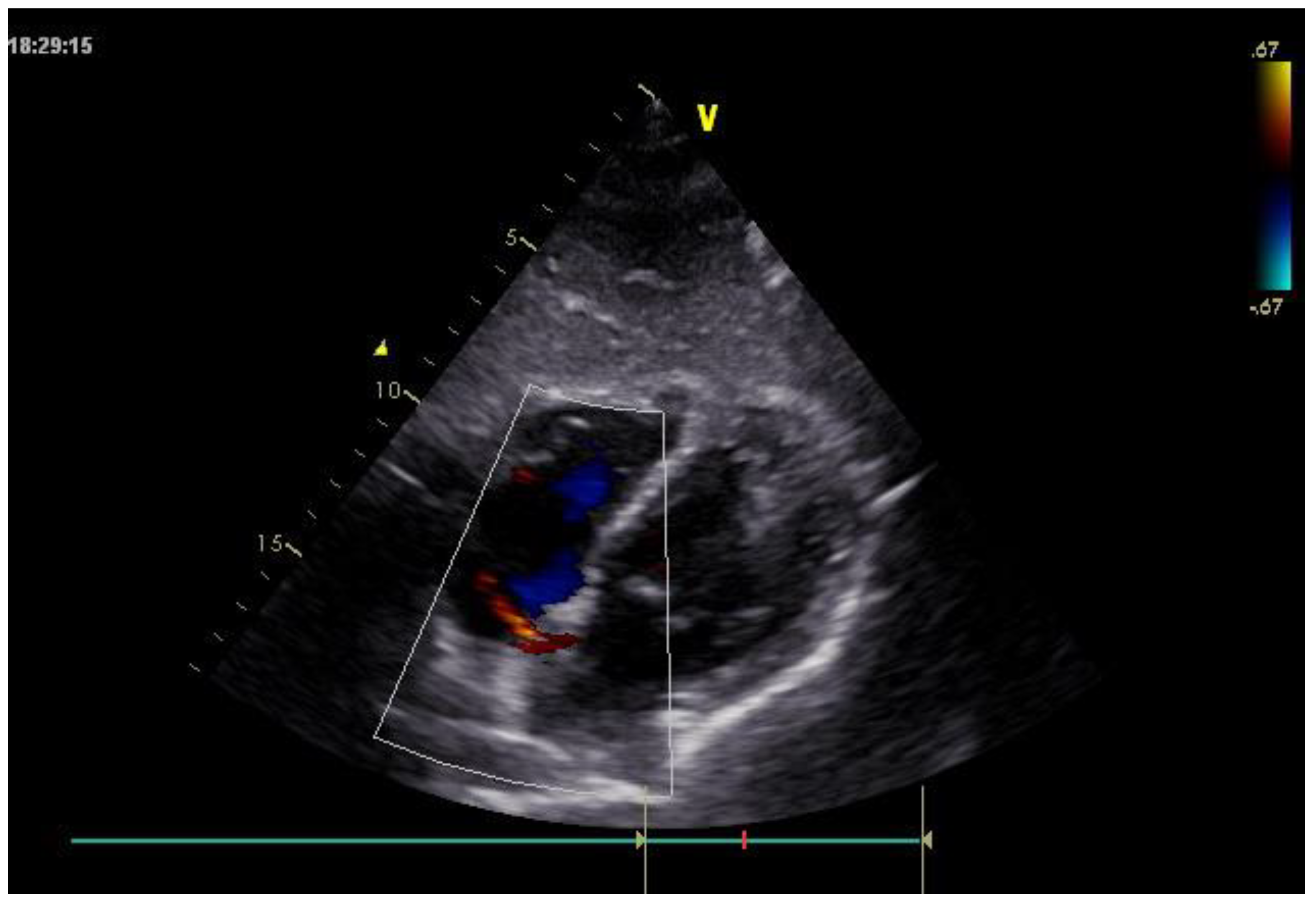
Furthermore, transthoracic echocardiography performed on admission confirmed the absence of the Amplatzer device at the interatrial septum and demonstrated a residual left-to-right shunt across the atrial septum (
Figure 2).
As no indication for urgent gynecological surgical intervention was identified and the patient remained clinically stable, endovascular retrieval of the migrated device was planned.
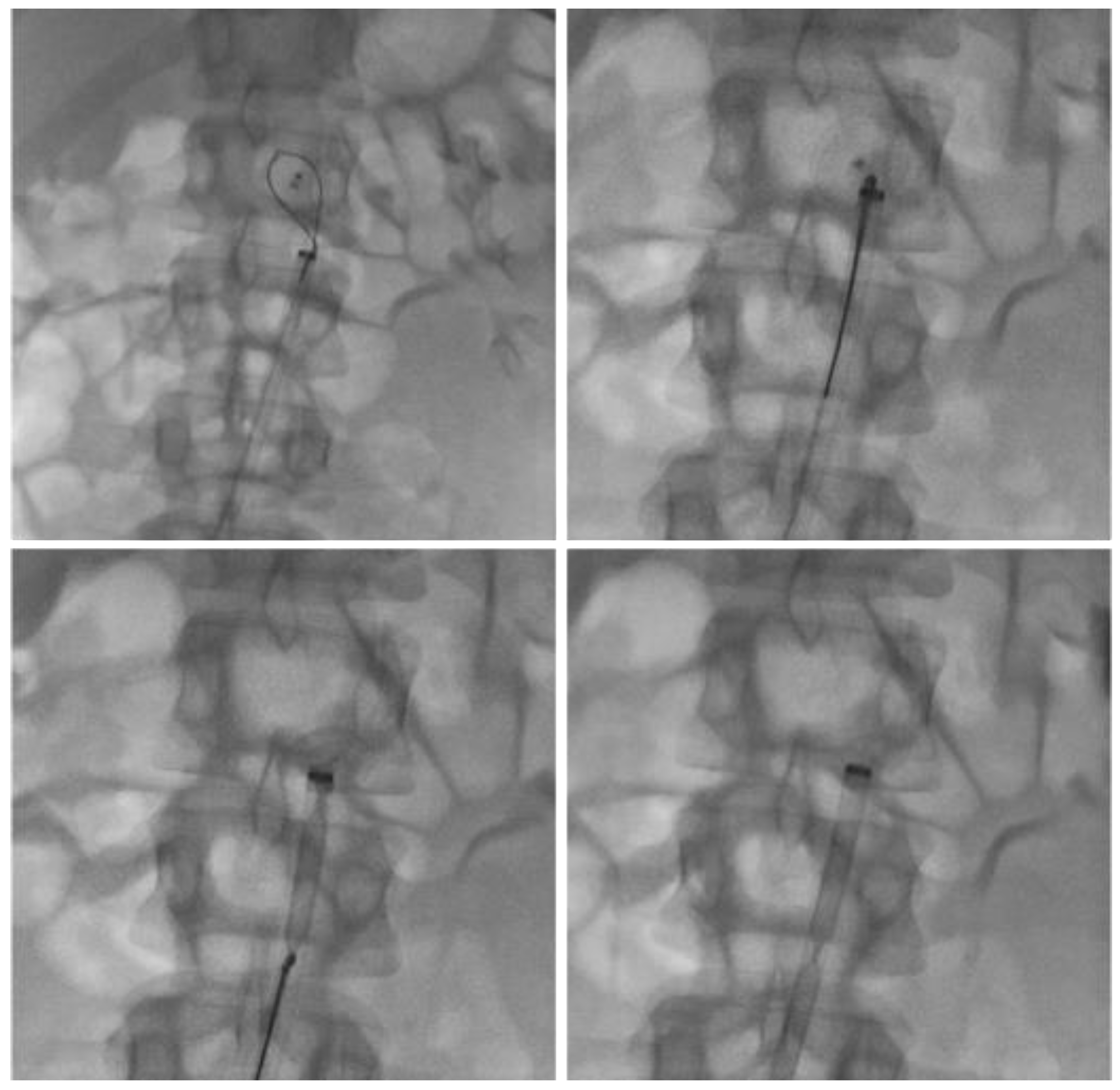
The procedure was performed under local anesthesia via right common femoral artery access. Diagnostic aortography confirmed the presence of the device lodged within the infra-renal abdominal aorta, without impairment of aorto-iliac flow. Using a snare retrieval system, the device was successfully captured and removed through a large-bore introducer sheath. Final angiographic control demonstrated normal patency of the abdominal aorta, renal arteries, and iliac vessels, with no procedural complications (
Figure 3).
The post-procedural course was uneventful. Serial clinical and laboratory evaluations showed stable hemoglobin levels and progressive resolution of abdominal symptoms. Subsequent cardiological assessment did not reveal urgent findings, and antiplatelet therapy was temporarily withheld. The patient was discharged in good general condition with recommendations for outpatient cardiological and gynecological follow-up.
3. Discussion
Percutaneous closure of PFO using occluder devices is a well-established procedure with high technical success rates and a low incidence of complications. Nevertheless, device-related adverse events may occur, including thrombus formation, residual shunting, arrhythmias, and, more rarely, device migration or embolization [
1]. Although reported in less than 1% of cases, device migration represents a potentially serious complication that requires prompt recognition and appropriate management [
2].
Migration may occur early, usually related to undersizing of the device, inadequate septal rims, or suboptimal positioning, but delayed migration has also been described [
3]. Late or very late embolization is particularly insidious, as patients may remain asymptomatic and the complication may be incidentally discovered during imaging performed for unrelated clinical indications [
4]. Reported embolization sites include cardiac chambers, pulmonary arteries, and, less frequently, the systemic arterial circulation, such as the abdominal aorta [
5].
In the present case, the migrated Amplatzer device was incidentally identified during CT performed for evaluation of acute abdominal pain caused by hemoperitoneum secondary to a hemorrhagic ovarian cyst. Similar incidental diagnoses have been described in the literature, underscoring the pivotal role of cross-sectional imaging in detecting unexpected device-related complications [
6]. The preserved patency of the renal and iliac arteries allowed careful procedural planning and avoided emergent surgical intervention.
Management of migrated occluder devices depends on their anatomical location, the patient’s clinical status, and institutional expertise. Endovascular retrieval has become the preferred first-line approach in most cases, offering a minimally invasive and highly effective alternative to open surgical removal. Snare-assisted techniques using large-bore introducer sheaths have been successfully employed even in large-caliber vessels such as the abdominal aorta. Surgical retrieval is generally reserved for cases in which percutaneous techniques fail or when migration results in hemodynamic instability or organ ischemia [
7].
Finally, this case emphasizes the importance of post-procedural surveillance following PFO closure. Although standardized follow-up protocols are lacking, awareness of potential delayed complications is crucial. Early recognition of device migration allows timely intervention and reduces the risk of serious adverse events.
4. Conclusions
Migration of an Amplatzer occluder is a rare but potentially serious complication of percutaneous PFO closure. Delayed migration may remain clinically silent and be incidentally detected during imaging performed for unrelated conditions. Prompt recognition and appropriate management are essential to prevent vascular complications. Endovascular retrieval represents a safe and effective treatment option and should be considered the first-line approach in stable patients. This case highlights the importance of imaging assessment and a multidisciplinary approach in ensuring timely diagnosis and optimal management of device-related complications.
Author Contributions
Conceptualization, F.C.; methodology, F.C. and M.E.; software, E.R.; validation, F.C. and C.M.; formal analysis, F.C.; and R.N. investigation, F.C. and N.V.; resources, M.E.; data curation, F.C. and N.V.; writing—original draft preparation, F.C.; writing—review and editing, F.C.; visualization, M.E. and N.V.; supervision, F.C. and C.M.; project administration, F.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Ethical review and approval were waived for this study; the “Antonio Cardarelli” Ethics Committee on Scientific Ethics waived the need for IRB approval for the case report, wherein the patient had signed informed consent.
Informed Consent Statement
Written informed consent has been obtained from the patient to publish this paper.
Data Availability Statement
The original contributions presented in this work are included in the article. Further inquiries can be directed to the corresponding author.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Ferrero, E.; Ferri, M.; Viazzo, A.; Beqaraj, F.; Gibello, L.; Berardi, G.; Santovito, D.; Nessi, F. Migration of an AMPLATZER atrial septal occluder to the abdominal aorta. Am J Cardiol. 2013, 112(4), 612–613. [Google Scholar] [CrossRef] [PubMed]
- Davies, A.J.; Collins, N.; Organ, N. Retrieval of Embolized Amplatzer Patent Foramen Ovale Occlusion Device: Issues Related to Late Recognition. Case Rep Cardiol. 2017, 2017, 9894215. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Musuraca, G.; Agostoni, P.; Boldi, E.; Imperadore, F.; Terraneo, C.; Broso, G.P. Very late migration to and retrieval of an Amplatzer patent foramen ovale occlusion device from the abdominal aortic carrefour. J Cardiovasc Med (Hagerstown) 2018, 19(8), 459–461. [Google Scholar] [CrossRef] [PubMed]
- Kovacevic, M.; Atanaskovic, M.; Obradovic, K.; Todic, M.; Crnomarkovic, B.; Bjelobrk, M.; Bjelic, S.; Cankovic, M.; Milovancev, A.; Srdanovic, I. Embolization of Patent Foramen Ovale Closure Device-Rare Complication and Unique Management Approach. Medicina (Kaunas) 2024, 60(5), 717. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Filippone, G.; La Barbera, G.; Valentino, F.; Ocello, S.; Talarico, F. Transcatheter retrieval of Amplatzer Septal Occluder device embolized into the abdominal aorta. SAGE Open Med Case Rep. 2019, 7, 2050313X19842462. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Guimaraes, M.; Denton, C.E.; Uflacker, R.; Schonholz, C.; Selby, BJr; Hannegan, C. Percutaneous retrieval of an Amplatzer septal occluder device that had migrated to the aortic arch. Cardiovasc Intervent Radiol. 2012, 35(2), 430–433. [Google Scholar] [CrossRef] [PubMed]
- Berk, T.A.; Kroeze, S.; Suttorp, M.J.; Heijmen, R.H. Open surgical retrieval of a migrated patent foramen ovale closure device from the descending aorta following failed percutaneous retrieval from the aortic arch: a case report with a word of caution. Eur Heart J Case Rep. 2023, 7(3), ytad099. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2026 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).