1. Introduction
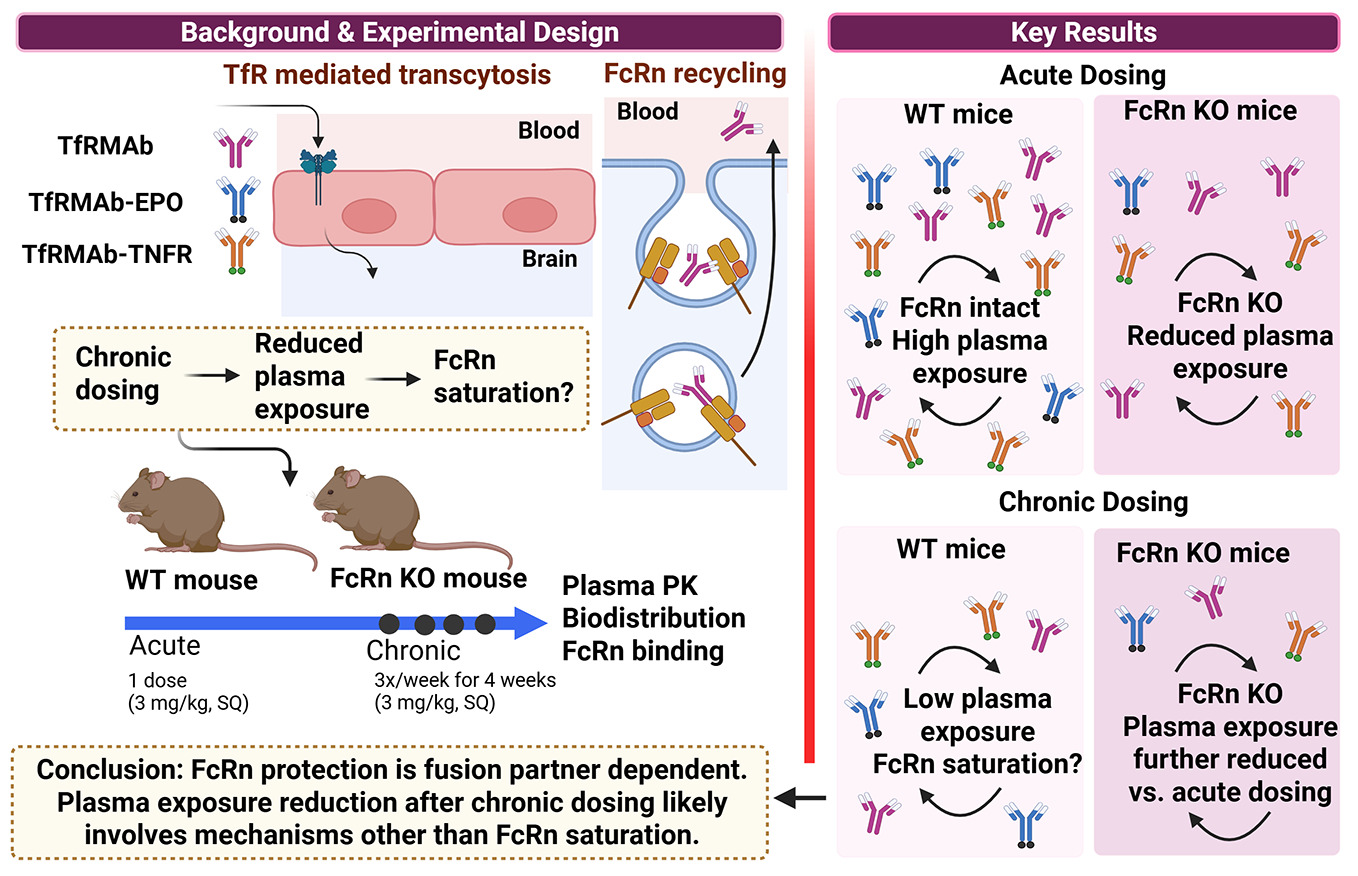
The blood-brain barrier (BBB) presents a major challenge for the delivery of biologics into the brain, necessitating drug-delivery strategies [
1]. One of the most widely studied and validated strategies to deliver biologics to the brain utilizes receptor-mediated transcytosis (RMT) receptors that are overexpressed at the BBB, such as the transferrin receptor-1 (TfR) [
1,
2]. Different variants of TfR-targeting antibodies (TfRMAbs) have been developed to facilitate the delivery of large molecular weight therapeutic molecules across the BBB [
3,
4,
5,
6,
7,
8,
9,
10,
11]. These antibodies differ in their valency and bind to the receptor with different affinities, sparing the transferrin binding site of the receptor to keep iron regulation intact [
1,
2,
5].
TfRMAbs fused to different therapeutics are under development for many chronic neurological disorders, including Parkinson’s disease [
12], Alzheimer’s disease [
10,
13,
14,
15], and this strategy has been granted regulatory approval in Japan for brain delivery of a therapeutic enzyme for Hunter's syndrome after a successful phase 3 clinical trial [
11,
16]. Effective treatment of such chronic diseases requires long-term treatment necessitating continuous dosing. Previous work demonstrated that chronic administration of a 3 mg/kg subcutaneous (SQ) dose of a high-affinity bivalent rat/mouse chimeric transferrin receptor monoclonal antibody (TfRMAb) for 4 weeks reduced systemic bioavailability compared to a single dose in mice [
17]. A similar reduction in systemic bioavailability of TfRMAb was observed following chronic SQ dosing of an isotype control mouse IgG1 [
17]. Similarly, chronic intravenous (IV) dosing of a humanized high-affinity bivalent TfRMAb alone for 4 weeks at doses ranging between 3-30 mg/kg was associated with a reduction in plasma concentrations in Rhesus monkeys [
18]. Moreover, chronic IV dosing of a humanized TfRMAb-iduronate-2-sulfatase fusion protein for up to 26 weeks resulted in a reduction in plasma concentrations at doses ranging between 1-30 mg/kg in cynomolgus monkeys [
19]. On the contrary, chronic dosing of high-affinity bivalent TfRMAb fused to glial-derived neurotrophic factor (GDNF) or a TNF-α inhibitor at lower doses (1-1.75 mg/kg) did not alter plasma pharmacokinetics of the TfRMAb-fusion protein in mice [
15,
20]. The exact mechanisms underlying the reduction in the plasma exposure of the TfRMAbs and TfRMAb-fusion proteins are not clearly defined, but suggested mechanisms include the formation of anti-drug antibody (ADA), an increase in peripheral TfR expression, fusion partner-specific clearance mechanisms, and saturation of the neonatal crystallizable fragment receptor (FcRn) [
17,
19,
21,
22]; the latter is the focus of this study.
FcRn plays a crucial role in maintaining the long circulating half-life of IgGs. This process of FcRn-mediated recycling involves binding of the IgG Fc domain to the FcRn at an acidic pH, lysosomal escape of the IgG, and IgG release into the circulation at physiological pH [
23]. Accordingly, strategies to enhance FcRn binding of therapeutic antibodies through Fc domain engineering have significantly improved antibody recycling and extended half-life, thereby possibly increasing their therapeutic efficacy [
24]. Conversely, engineering antibody-binding fragment (Fab) antibody-fusion proteins without the Fc domain is a widely used strategy to reduce Fc-mediated effector function side effects but results in decreased systemic exposure and shorter duration of action [
24,
25]. This reduction in systemic exposure is also observed with long-term antibody dosing, which can potentially saturate FcRn-mediated recycling and increase antibody catabolism [
24].
Although the role of FcRn in regulating the systemic half-life of IgG and Fc-fusion proteins is well established, studies examining the FcRn-mediated rescue of TfRMAbs have been limited. A recent study investigated the role of FcRn in mediating the systemic and brain exposure of a TfRMAb Fab fragment fused to an anti-amyloid antibody [
26]. As expected, a significant increase in systemic clearance was observed in the presence of a mutation in the FcRn binding domain of the anti-amyloid antibody after a single IV injection [
26]. However, the contribution of FcRn in regulating plasma and brain concentrations of full-length TfRMAb and associated fusion proteins after extravascular chronic dosing, which is the preferred route of administration to treat chronic diseases, is unclear. Therefore, the aim of the current study was two-fold: to elucidate the role of FcRn in regulating acute and chronic plasma pharmacokinetics and biodistribution of a high-affinity bivalent full-length mouse/rat chimeric TfRMAb [
27], and to determine if FcRn-mediated rescue is a function of the therapeutic fusion partner attached to the TfRMAb. For this, we used TfRMAb and two model TfRMAb-fusion proteins: TfRMAb fused to a neurotrophin (erythropoietin) (TfRMAb-EPO) and TfRMAb fused to the extracellular domain of the type II TNF-α receptor (TfRMAb-TNFR), and examined how FcRn regulates systemic exposure and biodistribution following acute and chronic dosing in wild-type (WT) and FcRn knockout (KO) mice. The results of the study demonstrate a significant, albeit variable, role of FcRn in sustaining systemic and tissue exposure of TfRMAb fusion proteins. In addition, the findings provide insights into how the FcRn regulates the systemic and tissue persistence of TfRMAb therapeutics following single and repeated dosing. These observations may also be useful when considering the engineering of TfRMAb Fab fusion proteins, which are currently under development [
28].
2. Materials and Methods
2.1. Transferrin Receptor Monoclonal Antibody Fusion Proteins
The TfRMAb-TNFR and TfRMAb-EPO fusion proteins were produced via transient expression in Chinese hamster ovary (CHO-K1) cells [
29,
30]. Following expression, the fusion proteins were purified using protein A affinity chromatography and size-exclusion chromatography to ensure high purity. The purified TfRMAb-TNFR and TfRMAb-EPO fusion proteins were formulated at concentrations of 1.1 mg/mL and 1.49 mg/mL, respectively. TfRMAb-TNFR was prepared in a buffer containing 0.01 M sodium acetate, 0.148 M NaCl, and 0.01% polysorbate 80 at pH 5.5, while TfRMAb-EPO was formulated in a buffer containing 0.05 M sodium acetate, 0.148 M NaCl, and 0.01% polysorbate 80 at pH 5.5. The solutions were sterile-filtered and stored at −80 °C until needed. To produce TfRMAb, ExpiCHO cells were cultured in serum-free expression medium. The expressed protein was formulated at a concentration of 1.05 mg/mL in 10 mM sodium acetate, 150 mM NaCl, and 0.01% polysorbate 80 at pH 6.0 [
17]. The TfRMAb protein was sterile-filtered and stored at −80 °C for future use.
2.2. Acute Dosing of TfRMAb Fusion Proteins
All experimental procedures were conducted in accordance with the protocol (2010-1170) approved by the Chapman University Institutional Animal Care and Use Committee. The study utilized 8-week-old male wild-type (WT, C57BL/6 JAX Stock Number: 000664) and male FcRn KO mice (B6.129X1-Fcgrt<tm1Dcr>/DcrJ JAX Stock Number: 003982) purchased from The Jackson Laboratory (Bar Harbor, ME, US) which were housed under standard conditions with unrestricted access to food and water and maintained on a 12-hour light/dark cycle. Mice were randomized into treatment groups based on body weight to ensure comparable group averages at the start of the study. The treatment groups received SQ injections of TfRMAb (3 mg/kg, n = 5), TfRMAb-TNFR (3 mg/kg, n = 5), or TfRMAb-EPO (3 mg/kg, n = 5). Following injections, mice were closely monitored for 2 hours to assess their general appearance and posture to rule out severe immune response [
17].
For blood collection, mice were briefly anesthetized using 2% isoflurane (Vetone Fluriso, 502017) delivered using the Somnoflo anaesthesia system (Kent Scientific, KENT-SS-0) and blood samples were collected in sodium citrate (Thermo Fisher Scientific, 02-683-172) as 9 parts blood 1 part sodium citrate, from the retro-orbital sinus at 3-, 6-, and 24-hours post-injection. Plasma was collected by centrifuging blood samples at 10,000 g for 5 minutes at 4°C, aliquoted, and stored at -80°C to prevent multiple freeze-thaw cycles. Plasma was analyzed by immunoassays to quantify plasma fusion protein concentrations. At the terminal 24-hour timepoint, mice were euthanized, cardiac perfusion with ice-cold phosphate-buffered saline (PBS) was performed, and organs, including the brain, liver, kidney, and spleen, were harvested. Tissues were snap-frozen in liquid nitrogen to analyze fusion protein concentrations. Additional blood samples were collected in lithium-heparin tubes (SARSTEDT Inc, 41.1393.105), and plasma was separated by centrifugation. Terminal whole blood and plasma samples were also used to measure hematocrit using HemataStat II Hematocrit Analyzer (Separation Technology, 0502HS03015) and for a comprehensive diagnostic panel using VetScan rotor (Abaxis, 10023220) and the VetScan VS2 chemical analyzer (Abaxis, 1200-1000).
2.3. Chronic Dosing of TfRMAb Fusion Proteins
All animal studies were conducted under protocol 2010-1170, approved by the Chapman University Institutional Animal Care and Use Committee. The study utilized 8-week-old male WT and FcRn KO mice (Jackson Laboratory, Bar Harbor, ME, US). Mice were housed under standard conditions with ad libitum access to food and water and maintained on a 12-hour light/dark cycle. Mice were randomized into treatment groups based on body weight to ensure similar group averages before the study start. The mice were injected SQ with TfRMAb, TfRMAb-TNFR, or TfRMAb-EPO fusion proteins at a dosage of 3 mg/kg, three times a week for four weeks. Each treatment group consisted of five mice. Mice were monitored carefully after injection, and a complete health assessment was performed weekly after injection for general appearance [
17]. After the final injection, blood samples were collected at 3-, 6-, and 24-hours post-injection, plasma was isolated and stored as described below. Briefly, blood samples were collected via the retro-orbital sinus under 2% isoflurane anesthesia (Vetone Fluriso, 502017) delivered using the Somnoflo anesthesia system (Kent Scientific, KENT-SS-0) into sodium citrate-containing tubes (Thermo Fisher Scientific, 02-683-172). Plasma was separated by centrifuging the blood samples at 10,000 g for 5 minutes at 4°C. Plasma aliquots were frozen and stored in well-labeled Eppendorf vials at -80°C until immunoassays to determine fusion protein concentrations. At the terminal time-point, mice were euthanized, cardiac perfusion with ice-cold PBS was performed, and the brain, liver, kidney, and spleen were harvested. Tissues were gently blotted on filter paper and snap-frozen in liquid nitrogen. Additional blood samples were collected in lithium-heparin tubes (SARSTEDT Inc, 41.1393.105), and plasma was separated by centrifugation. The supernatant was then analyzed using the VetScan VS2 chemical analyzer (Abaxis, 1200-1000), with a VetScan rotor (Abaxis, 10023220). Hematology analysis was performed on whole blood samples collected in Microvette potassium-EDTA tubes (SARSTEDT Inc, 20.1278.100) at 4°C, either on the same day of collection or within 24 hours, using the VetScan HM5 Hematology analyzer (Zoetis, 10023319).
2.4. Plasma TfRMAb and TfRMAb Fusion Protein Concentrations by ELISA
Plasma concentrations of TfRMAb, TfRMAb-TNFR, and TfRMAb-EPO were determined using sandwich ELISA [
17,
30]. Nunc Maxisorp plates (Fisher Scientific, 501123685) were coated overnight at 4°C with recombinant human EPOR/Fc fusion protein (200 ng/well) to measure TfRMAb-EPO (R&D systems, 963-ER) or recombinant murine TfR (200 ng/well) to measure TfRMAb and TfRMAb-TNFR (R&D systems, 9706-TR) in 0.1M and 0.05M NaHCO3, pH 8.3, (Sigma-Aldrich, S5761), respectively. Following overnight incubation, the coating solution was aspirated, and the wells were washed three times with Tris-buffered saline containing 0.05% Tween-20 (Bio-rad Laboratories, 1200274186) (TBST). Plates were blocked with TBS containing 1% bovine serum albumin (BSA) (Roche Diagnostics GmbH, 10735078001) (TBSB) for 30 minutes at room temperature (RT) to prevent non-specific binding. After blocking, 100 μL of the appropriate standards and diluted plasma samples (1:10 in TBSB) for TfRMAb, TfRMAb-TNFR, and TfRMAb-EPO were added to the wells and incubated for up to 2 hours at RT. Plates were washed three times with TBST to remove unbound proteins. For TfRMAb-TNFR measurements, an additional step included incubation with rabbit anti-TNFRII (Sino Biologicals, 20230119980430) for 30 minutes at RT after removing unbound proteins. Goat anti-mouse alkaline phosphatase conjugate 100 ng/well (Bethyl Laboratories Inc, A90-119A) that binds to TfRMAb domain was added and incubated for 45 minutes at RT to measure TfRMAb and TfRMAb-EPO. Goat anti-rabbit IgG alkaline phosphatase conjugate 100 ng/well (Invitrogen, 656122) that binds to the anti-TNFRII was added and incubated for 45 minutes at RT to measure TfRMAb-TNFR. Plates were then washed three more times with TBST and incubated with p-nitrophenyl phosphate substrate (Sigma-Aldrich, P5994). The substrate was incubated in the dark for 5-15 minutes to allow for color development, with careful observation to prevent overdevelopment. The reaction was stopped by adding 100 μL of 1.2 M NaOH per well, and absorbance was measured at 405 nm using a plate reader. Blank-corrected absorbance values were used to calculate plasma concentrations of TfRMAb, TfRMAb-TNFR, and TfRMAb-EPO.
2.5. Tissue Processing
Frozen organs (spleen, kidney, liver, and brain) were pulverized into a fine powder using an ice-cold pulverizer in a cold room. Approximately 40 mg of spleen, 80 mg of kidney and liver, and 50 mg of brain tissue were weighed and homogenized in Tissue Protein Extraction Reagent (TPER) buffer (ThermoScientific, 78510) containing EDTA-free protease inhibitors (Sigma, 3032642568) and Halt™ Phosphatase Inhibitor Single-Use Cocktail (ThermoScientific, P178420). Homogenization of spleen, kidney, and liver was performed using 5 µL of buffer per mg of tissue, while brain homogenization was performed using 2 µL of buffer per mg of tissue. Homogenates were incubated for 1 hour, followed by centrifugation at 14,000 g for 20 minutes at 4°C. Supernatants were aliquoted into labeled Eppendorf vials for further analysis.
2.6. MSD Electrochemiluminescence Assay
To determine the concentration of TfRMAb and TfRMAb-fusion proteins in tissue homogenates of the liver, spleen, kidney, and brain, a Mesoscale Discovery (MSD) electrochemiluminescence assay was performed using the MSD GOLD™ 96-well Small Spot Streptavidin SECTOR 96-well plate (Meso Scale Diagnostics, L45SA). The plate was blocked with 150 µL per well of TBS and 3% BSA (Roche Diagnostics GmbH, 10735078001) and incubated at RT for 1 hour at 900 rpm shaking. After blocking, wells were aspirated, and 30 µL of biotinylated EPOR (BPS Bioscience, 100612) for TfRMAb-EPO, biotinylated TNFα (Sino Biological, 50349-MNAE-B) for TfRMAb-TNFR, and biotinylated mouse transferrin R (ACROBiosystems, TFR-M8249) for TfRMAb, at 0.25 µg/mL in TBST and 1% BSA (Roche Diagnostics GmbH, 10735078001) (TBSB) was added to each well. The plate was incubated for 1 hour at RT with shaking (900 rpm), followed by three washes with 150 µL/well of TBST. Tissue homogenates and standards (25 µL) were added per well, and the plate was incubated for 1 hour at RT with shaking (900 rpm). After incubation, wells were washed three times with TBST. For detection, 25 µL of 1 µg/mL goat anti-mouse sulfo-tag (Meso Scale Diagnostics, R32AC-5) in 1% BSA in TBS at 25 ng/well was added and incubated for 1 hour at RT with shaking (900 rpm). After washing three times with TBST, 150 µL of Gold Read Buffer B (Meso Scale Diagnostics, B-R60AM-3) was added. The plate was read using an MSD MESO QuickPlex SQ 120 96-well plate reader (Meso Scale Diagnostics, AI0AA-0), and data were collected and analyzed.
2.7. FcRn Binding of Mouse IgG, TfRMAb, and TfRMAb Fusion Proteins
To characterize FcRn binding affinity, an MSD electrochemiluminescence assay was performed using an MSD GOLD™ 96-well Small Spot Streptavidin SECTOR plate (Meso Scale Diagnostics, L45SA). The plate was blocked with 150 µL/well of 3% BSA (Roche Diagnostics GmbH, 10735078001) in PBS (pH 6.0) and incubated at RT for 1 hour with shaking at 900 rpm. After blocking, 30 µL/well of biotinylated FcRn (Kactus Bio, FRN-MM401B) diluted to 0.2 µg/well in PBS containing 1% BSA (Roche Diagnostics GmbH, 10735078001) (PBSB, pH 6.0) was added, with select wells left uncoated as negative controls. The plate was incubated for 1 hour at RT with shaking, followed by three washes with 150 µL/well PBS containing 0.05% Tween-20 (Bio-rad Laboratories, 1200274186) (PBST, pH 6.0).
Mouse IgG, TfRMAb, TfRMAb-EPO, and TfRMAb-TNFR were prepared in PBSB pH 6.0 by serial dilution of stock solutions (TfRMAb: 1.05 mg/mL; TfRMAb-EPO: 1.49 mg/mL; TfRMAb-TNFR: 1.1 mg/mL; Mouse IgG: 9.78 mg/mL). For TfRMAb, Mouse IgG, and TfRMAb-EPO, standards spanned 200,000-78.13 ng/mL (5,000-1.95 ng/well in 25 µL). For TfRMAb-TNFR, standards ranged from 800,000-78.13 ng/mL (20,000-1.95 ng/well). Standards (25 µL/well) were added in duplicates and incubated for 1 hour at RT with shaking. After three PBST washes, sulfo-tagged detection Fab antibody was added, which was previously prepared by conjugating the Fab fragment (Jackson Immunoresearch,115-006-072) with Sulfo-TAG NHS-Ester (Meso Scale Diagnostics, R91AN-1) using a 20:1 molar challenge ratio. Briefly, 7.3 µL of reconstituted Sulfo-TAG reagent (3 nmol/µL in distilled water) was added to 100 µL of Fab antibody (1.3 mg/mL) and incubated at RT for 2 hours (protected from light). The conjugated Fab was diluted to 25 ng/well in PBS containing 1% BSA Roche Diagnostics GmbH, 10735078001) (pH 6.0), added to wells (25 µL/well), and incubated for 1 hour at RT with shaking. Following three PBST washes, 150 µL/well of Gold Read Buffer B (Meso Scale Diagnostics, B-R60AM-3) was added, and the plate was immediately analyzed using an MSD MESO QuickPlex SQ 120 96-well plate reader (Meso Scale Diagnostics, AI0AA-0). The data was collected and analyzed.
2.8. Statistical Analysis
The data are presented as mean ± SEM, and statistical analyses were conducted using GraphPad Prism (v10.04.1, La Jolla, CA, US). Outliers were identified and removed using Grubb’s outlier test. Using G*Power for sample size estimation, it was determined that 3-5 mice per group would be sufficient to detect an effect size of 35-50%, with a standard deviation of 15%, 80% power, and a significance level of 5%, as supported by previous studies [
22,
30]. An unpaired two-sample t-test and one-way ANOVA followed by Holm-Sidak’s post-hoc test were used for comparing two or more independent groups, respectively. A repeated-measures two-way ANOVA was used to evaluate the plasma drug concentrations over time in WT and FcRn KO mice, followed by Holm-Sidak’s post hoc analysis. Statistical significance was established at a two-tailed p ≤ 0.05.
4. Discussion
Previous studies have shown reduced plasma exposure and accelerated clearance following chronic dosing of TfRMAb in mice and non-human primates [
17,
18,
19,
21,
22]. One possible mechanism of reduced plasma exposure is FcRn saturation [
24]. FcRn is essential for maintaining IgG homeostasis, as it binds to the Fc domain of IgG proteins in acidic conditions (pH 6). This interaction occurs at a location distinct from the traditional Fc effector receptor binding site (FcγR) [
31]. The key residues at the CH2-CH3 domain interface of the Fc region facilitate binding, which ensures the recycling and extended half-life of IgG molecules, thus enhancing their stability and systemic availability [
24,
32]. This study focuses on understanding the contribution of FcRn in maintaining plasma pharmacokinetics and tissue biodistribution of identical doses of TfRMAb and TfRMAb-fusion proteins in C57BL6 WT mice and FcRn KO mice following acute and chronic administration.
Acute dosing studies showed significantly lower plasma concentrations and/or plasma AUC values in FcRn KO mice for TfRMAb and TfRMAb-fusion proteins when compared to WT mice. Interestingly, TfRMAb-TNFR-treated FcRn KO mice demonstrated the most substantial reduction in AUC (~90%). Similarly, TfRMAb and TfRMAb-EPO cleared from the plasma of FcRn KO mice more quickly than from WT mice within 24 hours, although the impact on overall plasma AUC was less compared to that for TfRMAb-TNFR. These observations align with previous reports that FcRn plays a critical role in regulating IgG half-life by protecting it from lysosomal degradation through pH-dependent binding and recycling or transcytosis [
25,
32]. For instance, engineered IgG subclasses or Fc-fusion proteins with enhanced FcRn binding at acidic pH (pH 6.0) have prolonged half-life and improved therapeutic efficacy [
33]. Furthermore, we observe that the associated fusion partner differentially affects the contribution of FcRn recycling in regulating IgG persistence, which may be linked to their interaction with FcRn. Accordingly, previous findings demonstrate that Fc-fusion proteins bind to FcRn less effectively than IgG, possibly due to steric hindrance or structural changes that may interfere with FcRn interaction [
7].
IgG recycling by FcRn can be saturable [
24], and studies have shown that chronic dosing can saturate FcRn and increase IgG catabolism [
34,
35]. In our hands, the plasma pharmacokinetics of the TfRMAb fusion proteins following chronic dosing demonstrated varying degrees of dependence on FcRn-mediated recycling. Compared with acute dosing, plasma exposure of TfRMAb and TfRMAb-EPO declined in the FcRn KO following chronic dosing. Therefore, despite the absence of FcRn, chronic dosing reduced plasma exposure of TfRMAb and TfRMAb-EPO even in FcRn KO mice, indicating that mechanisms beyond FcRn saturation regulate their plasma concentrations following chronic dosing. In contrast, in TfRMAb-TNFR-treated mice, only WT mice showed a decline in plasma concentrations following chronic dosing in comparison with acute dosing, while plasma concentrations in FcRn KO mice were relatively unchanged between acute and chronic dosing. Further, no significant changes were observed in the plasma concentrations of TfRMAb-TNFR between WT and FcRn KO mice at 3, 6, and 24 hours during chronic dosing, suggesting that FcRn saturation may be implicated. Comparing these profiles, we can likely deduce that even though there may be changes in FcRn recycling due to continuous antibody exposure via chronic dosing, there may be other mechanisms that contribute to the retention or clearance of these fusion proteins following chronic dosing. Studies show that factors beyond FcRn recycling may significantly affect the clearance and pharmacokinetics of TfRMAb therapeutics following chronic dosing [
17,
21,
22].
FcRn is essential for managing the distribution and availability of IgGs and Fc-fusion proteins in the body [
24], and its tissue expression levels differ among different organs [
36]. FcRn enables the bidirectional transport of IgG across mucosal surfaces and epithelial membranes, efficiently recycling antibodies and ensuring their systemic availability [
36]. Studies show that FcRn transcytosis may play a role in the transport of antibodies between tissues and the peripheral circulation, highlighted by the differences in tissue bioavailability of antibodies observed in FcRn KO and WT models [
36]. In the current study, acutely dosed WT mice consistently exhibited greater tissue biodistribution across all TfRMAb constructs and organs measured, including kidney, liver, spleen, and brain, in comparison to acutely dosed FcRn KO mice and the chronically dosed mice. This observation likely indicates that tissue biodistribution is driven by the plasma exposure of the TfRMAb constructs. However, a closer look at the tissue-to-plasma ratio showed that FcRn also regulates tissue biodistribution of the TfRMAb constructs. For example, despite the higher plasma concentrations of TfRMAb in WT compared to FcRn KO mice following acute dosing, TfRMAb showed higher tissue-to-plasma ratios in the kidney, spleen, and brain (with the same trend in the liver) in FcRn KO acute-dosed mice (Supplemental
Figure S2). An increase in the tissue-to-plasma ratio of TfRMAb in the FcRn KO mice suggests that FcRn plays an important role in tissue efflux in these organs. This finding is consistent with existing literature indicating that FcRn-mediated transcytosis aids in the transport of antibodies between the bloodstream and tissues [
36,
37], and that elevated IgG1 levels are found in FcRn KO mice at later time points, implying a function for FcRn in the IgG efflux from tissues [
36]. This is also consistent with previous work showing that the BBB FcRn regulates the efflux of IgG from the brain parenchyma [
37]. Notably, this increase in tissue-to-plasma ratio was not seen in the presence of a fusion partner (Supplemental
Figure S2), implying that the fusion partner could possibly influence FcRn binding dynamics and, in turn, affect tissue biodistribution.
Hematologic and metabolic panel indices provide a comprehensive evaluation of systemic health, facilitating the assessment of TfRMAb fusion proteins by tracking key biomarkers related to organ function, metabolic stability, and potential systemic effects, ensuring both efficacy and safety in development and application. Both treated and untreated FcRn KO mice exhibited lower albumin levels compared to fusion protein-treated and untreated WT mice (Supplemental
Figure S3), consistent with impaired FcRn-mediated albumin recycling, as FcRn is essential for this process [
38]. Reduced calcium and total protein levels in both treated and untreated FcRn KO mice, compared to the WT mice, are likely a consequence of hypoalbuminemia [
39]. The higher globulin levels observed in FcRn KO mice compared to their WT counterparts (treated or untreated) may reflect a compensatory feedback mechanism for reduced albumin [
40]. These shifts in metabolic indices occur in both treated and untreated FcRn KO mice, indicating that they arise from FcRn deficiency itself rather than from TfRMAb fusion protein treatment.
Hematologic indices of WT and FcRn KO mice after chronic treatment of fusion proteins were compared to untreated, WT, or FcRn KO mice (Supplemental
Figure S4). Chronic TfRMAb treatment was associated with splenomegaly (Supplemental
Figure S1) and hematologic changes, including lower RBC, hematocrit, and hemoglobin compared with control values (Supplemental
Figure S4) in WT and FcRn KO mice, indicating that these changes are driven by TfRMAb and not FcRn. This finding is consistent with previous studies, which have shown a reduction in reticulocytes associated with TfRMAb treatment [
30,
41]. As for TfRMAb-EPO-treated WT and FcRn KO mice, there were no changes to the RBC, hematocrit, and hemoglobin compared to their respective control, while in TfRMAb-TNFR-treated WT and FcRn KO mice, we see lower hemoglobin in comparison to their respective control mice. Splenomegaly was not observed with TfRMAb-EPO and TfRMAb-TNFR treatment. These varying effects observed with TfRMAb, TfRMAb-EPO, and TfRMAb-TNFR treatment again emphasize the role of the fusion partner in regulating the side effects of TfRMAb constructs [
17].
The different pharmacokinetic profiles of TfRMAb-TNFR, TfRMAb, and TfRMAb-EPO in FcRn KO mice likely result from differences in FcRn binding, which regulates IgG recycling and half-life. The binding affinity of TfRMAb-TNFR for FcRn was 14- to 16-fold lower than that of TfRMAb and TfRMAb-EPO (
Table 1); this could imply superior FcRn-mediated recycling of the latter two constructs and a greater impact of FcRn in regulating their pharmacokinetics. However, our work shows that TfRMAb-TNFR pharmacokinetics were the most impacted by the absence of FcRn. Studies have demonstrated that strong FcRn binding may impair exocytosis into the blood circulation and fail to improve IgG half-life, affecting IgG pharmacokinetics and persistence [
42,
43,
44]. Therefore, it is conceivable that the stronger FcRn affinity of TfRMAb and TfRMAb-EPO hinders IgG exocytosis into the blood circulation, offsetting the benefits of FcRn recycling. This may explain the reduced reliance of TfRMAb and TfRMAb-EPO on FcRn for plasma retention. In contrast, the weaker FcRn binding of TfRMAb-TNFR may enhance exocytosis into the bloodstream and increase FcRn-mediated protection, an effect absent in FcRn KO mice, thereby explaining its greater dependence on FcRn recycling.
Figure 1.
Plasma pharmacokinetics of TfRMAb-EPO following acute and chronic dosing. WT and FcRn KO mice received acute or chronic four-week dosing of TfRMAb-EPO (3 mg/kg SQ). (A) Plasma concentrations (ng/mL) at 3 h, 6 h, and 24 h post-acute dosing and (B) after one final dose after chronic dosing. (C) Merged plasma concentration vs. time curves for acute and chronic dosing regimens. (D) Plasma AUC from 0-24h (ng·h/mL) following acute and chronic dosing. Data are shown as mean ± SEM of n = 4–10 mice per group. *p < 0.05, **p < 0.01, ***p < 0.001, ****p < 0.0001.
Figure 1.
Plasma pharmacokinetics of TfRMAb-EPO following acute and chronic dosing. WT and FcRn KO mice received acute or chronic four-week dosing of TfRMAb-EPO (3 mg/kg SQ). (A) Plasma concentrations (ng/mL) at 3 h, 6 h, and 24 h post-acute dosing and (B) after one final dose after chronic dosing. (C) Merged plasma concentration vs. time curves for acute and chronic dosing regimens. (D) Plasma AUC from 0-24h (ng·h/mL) following acute and chronic dosing. Data are shown as mean ± SEM of n = 4–10 mice per group. *p < 0.05, **p < 0.01, ***p < 0.001, ****p < 0.0001.
Figure 2.
Tissue biodistribution of TfRMAb-EPO following acute and chronic dosing. Biodistribution of TfRMAb-EPO following a single 3 mg/kg SQ dose (acute) or four weeks of chronic dosing. Tissue concentrations (pg/mg of tissue) were measured in (A) kidney, (B) liver, (C) spleen, and (D) brain. Data are shown as mean ± SEM of n = 4-10 mice per group. **p < 0.01, ***p < 0.001.
Figure 2.
Tissue biodistribution of TfRMAb-EPO following acute and chronic dosing. Biodistribution of TfRMAb-EPO following a single 3 mg/kg SQ dose (acute) or four weeks of chronic dosing. Tissue concentrations (pg/mg of tissue) were measured in (A) kidney, (B) liver, (C) spleen, and (D) brain. Data are shown as mean ± SEM of n = 4-10 mice per group. **p < 0.01, ***p < 0.001.
Figure 3.
Plasma pharmacokinetics of TfRMAb following acute and chronic dosing. WT and FcRn KO mice received acute or chronic four-week dosing of TfRMAb (3 mg/kg SQ). (A) Plasma concentrations (ng/mL) at 3 h, 6 h, and 24 h post-acute dosing and (B) after one final dose after chronic dosing. (C) Merged plasma concentration vs. time curves for acute and chronic dosing regimens. (D) Plasma AUC from 0-24h (ng·h/mL) following acute and chronic dosing. Data are shown as mean ± SEM of n = 4-5 mice per group. *p < 0.05, **p < 0.01.
Figure 3.
Plasma pharmacokinetics of TfRMAb following acute and chronic dosing. WT and FcRn KO mice received acute or chronic four-week dosing of TfRMAb (3 mg/kg SQ). (A) Plasma concentrations (ng/mL) at 3 h, 6 h, and 24 h post-acute dosing and (B) after one final dose after chronic dosing. (C) Merged plasma concentration vs. time curves for acute and chronic dosing regimens. (D) Plasma AUC from 0-24h (ng·h/mL) following acute and chronic dosing. Data are shown as mean ± SEM of n = 4-5 mice per group. *p < 0.05, **p < 0.01.
Figure 4.
Tissue biodistribution of TfRMAb following acute and chronic dosing. Biodistribution of TfRMAb following a single 3 mg/kg SQ dose (acute) or four weeks of chronic dosing. Tissue concentrations (pg/mg of tissue) were measured in (A) kidney, (B) liver, (C) spleen, and (D) brain. Data are shown as mean ± SEM of n =4- 5 mice per group. *p < 0.05, **p < 0.01, ***p < 0.001, ****p < 0.0001.
Figure 4.
Tissue biodistribution of TfRMAb following acute and chronic dosing. Biodistribution of TfRMAb following a single 3 mg/kg SQ dose (acute) or four weeks of chronic dosing. Tissue concentrations (pg/mg of tissue) were measured in (A) kidney, (B) liver, (C) spleen, and (D) brain. Data are shown as mean ± SEM of n =4- 5 mice per group. *p < 0.05, **p < 0.01, ***p < 0.001, ****p < 0.0001.
Figure 5.
Plasma pharmacokinetics of TfRMAb-TNFR following acute and chronic dosing. WT and FcRn KO mice received acute or chronic four-week dosing of TfRMAb-TNFR (3 mg/kg SQ). (A) Plasma concentrations (ng/mL) at 3 h, 6 h, and 24 h post-acute dosing and (B) after one final dose after chronic dosing. (C) Merged plasma concentration vs. time curves for acute and chronic dosing regimens. (D) Plasma AUC from 0-24h (ng·h/mL) following acute and chronic dosing. Data are shown as mean ± SEM of n = 4-5 mice per group. *p < 0.05, **p < 0.01, ****p < 0.0001.
Figure 5.
Plasma pharmacokinetics of TfRMAb-TNFR following acute and chronic dosing. WT and FcRn KO mice received acute or chronic four-week dosing of TfRMAb-TNFR (3 mg/kg SQ). (A) Plasma concentrations (ng/mL) at 3 h, 6 h, and 24 h post-acute dosing and (B) after one final dose after chronic dosing. (C) Merged plasma concentration vs. time curves for acute and chronic dosing regimens. (D) Plasma AUC from 0-24h (ng·h/mL) following acute and chronic dosing. Data are shown as mean ± SEM of n = 4-5 mice per group. *p < 0.05, **p < 0.01, ****p < 0.0001.
Figure 6.
Tissue biodistribution of TfRMAb-TNFR following acute and chronic dosing. Biodistribution of TfRMAb-TNFR following a single 3 mg/kg SQ dose (acute) or four weeks of chronic dosing. Tissue concentrations (pg/mg of tissue) were measured in (A) kidney, (B) liver, (C) spleen, and (D) brain. Data are shown as mean ± SEM of n = 4-5 mice per group. *p < 0.05, **p < 0.01, ****p < 0.0001.
Figure 6.
Tissue biodistribution of TfRMAb-TNFR following acute and chronic dosing. Biodistribution of TfRMAb-TNFR following a single 3 mg/kg SQ dose (acute) or four weeks of chronic dosing. Tissue concentrations (pg/mg of tissue) were measured in (A) kidney, (B) liver, (C) spleen, and (D) brain. Data are shown as mean ± SEM of n = 4-5 mice per group. *p < 0.05, **p < 0.01, ****p < 0.0001.
Table 1.
FcRn binding of mouse IgG1, chimeric TfRMAb, and TfRMAb fusion proteins.
Table 1.
FcRn binding of mouse IgG1, chimeric TfRMAb, and TfRMAb fusion proteins.
| Fusion 114. |
KD nM |
| TfRMAb-TNFR |
114 ± 10.92 |
| Mouse IgG1 |
5.8 ± 0.16 |
| TfRMAb-EPO |
7.9 ± 0.07 |
| TfRMAb |
6.7 ± 1.2 |