1. Introduction
Cholangiocarcinoma (CCA) is a highly aggressive malignancy that originates from epithelial cells lining the bile ducts [
1]. It accounts for approximately 3% of all gastrointestinal cancers and is classified based on its anatomical location within the biliary tree [
2,
3]. Intrahepatic CCAs, located above second-order bile ducts, remain the second most prevalent cause of primary liver cancer [
3]. Conversely, extrahepatic CCAs, found below this level, can be further divided based on their relation to the cystic duct into perihilar and distal lesions. Despite their common origin from biliary epithelial cells, these distinct subtypes exhibit great variability in clinical presentation and management [
3]. Intrahepatic lesions often present as a mass and may remain asymptomatic until reaching an advanced stage. In contrast, extrahepatic lesions frequently manifest with obstructive symptoms, such as jaundice or right upper quadrant pain [
4]. Due to the highly variable and nonspecific nature of its symptoms, CCA is often diagnosed at a more advanced stage. Less than one-third of cases present with solitary lesions less than 3 cm at diagnosis, approximately half exhibit regional lymph node invasion, and a quarter with distant metastases [
5].
Carcinogenesis of biliary epithelium is a multi-step process driven by chronic inflammation and cellular injury in combination with bile flow obstruction. This prolonged bile stasis exposes biliary cells to the carcinogenic effects of bile components [
4]. Although the mechanism of carcinogenesis remains similar amongst the different types of CCA, risk factors vary considerably, with primarily infectious etiology in the east and noninfectious in the west [
4]. The high incidence of exposure to liver flukes, namely Clonorchis sinensis, in the Eastern hemisphere, accounts for the majority of CCA in that region. Conversely, risk factors such as cirrhosis, Hepatitis B and C, and primary sclerosing cholangitis represent potential sources of malignancy in the Western hemisphere. Given a rising incidence of CCA in Western countries and its high mortality rate, the need to understand its pathogenesis and early diagnostic approaches becomes increasingly critical.
A Sister Mary Joseph Nodule (SMJN) is a rare extra intestinal manifestation indicative of advanced stage intra-abdominal malignancy [
2]. Named after Sister Mary Joseph, who first identified the link between periumbilical nodules and intra-abdominal cancers, the presence of this nodule should prompt immediate investigation with abdominal imaging and biopsy of the lesion [
6]. Its superficial position facilitates biopsy, helping pinpoint the origin of the malignancy [
2]. Although the incidence of umbilical metastasis, namely SMJN, remains low at 1%-3% of all intra-abdominal or pelvic malignancies, commonly gastric, colon or ovarian, its association with CCA is unusual, exemplifying its potential diagnostic significance [
7]. Currently, there have only been ten recorded cases of CCA presenting with a SMJN, making this case report the eleventh [
2].
Regarding the metastatic potential of intra-abdominal and pelvic malignancies, the mechanism of umbilical seeding from its primary tumors remains poorly understood, resulting in several hypotheses to account for the phenomena. One theory suggests that seeding may occur through contiguous spread via peritoneal infiltration, the most common route, as well as hematogenous or lymphatic spread [
8]. Another proposed mechanism involves spreading through embryonic structures. The connection of the umbilicus with embryological remnants and its ample vascular and lymphatic components facilitates migration of tumor cells. Additionally, its lack of a muscular layer provides fewer barriers to direct spread of peritoneal masses [
8]. The presence of a SMJN across various intra-abdominal or pelvic malignancies further exemplifies the complexity of determining the mechanism behind umbilical metastasis.
Clinical presentation of a SMJN can vary greatly. Depending on the primary tumor source, it can present as a fissured or ulcerated nodule that can secrete serous, mucinous, purulent, or bloody discharge. The lesion has been observed to be variously colored, including white, bluish-violet, or brownish red, with possible pruritus [
7]. Its wide array of presentations can lead to frequent initial misdiagnosis with differential diagnosis including omphalitis, umbilical hernia, and superficial malignant tumors [
7]. In this case, the SMJN was misdiagnosed as an umbilical hernia and presented as a polypoid, cauliflower-like, skin-colored mass.
The prognosis of CCA remains poor with mean life expectancy ranging anywhere from 2 to 11 months without treatment. Current aggressive therapeutic approaches may extend survival rates up to 21 months [
8]. Interventions include surgical resection, photodynamic therapy, systemic chemotherapy, and palliative biliary decompression stenting [
4]. Despite these current advances, CCA has a dismal prognosis and often remains incurable because of its refractory nature and resistance to most currently used surgical or medical interventions [
4]. Additionally, metastatic disease manifesting as SMJN is an ominous sign of advanced disease that is not amenable to cure and often suggests that patients should focus on supportive care [
2].
We present a case report of a 65-year-old male with an umbilical hernia and cholestatic symptomatology pattern. The patient was initially set to undergo an elective open umbilical hernia repair. Abnormal presentation of the umbilical hernia suggested that the exophytic mass may be SMJN. Imaging and pathology reports of the mass were consistent with the diagnosis of advanced stage cholangiocarcinoma.
2. Case Presentation
An active 65-year-old male patient with no comorbidities presented with an umbilical lesion that was diagnosed as an umbilical hernia in the outpatient setting. He had noticed it over the past two months and requested an elective repair.
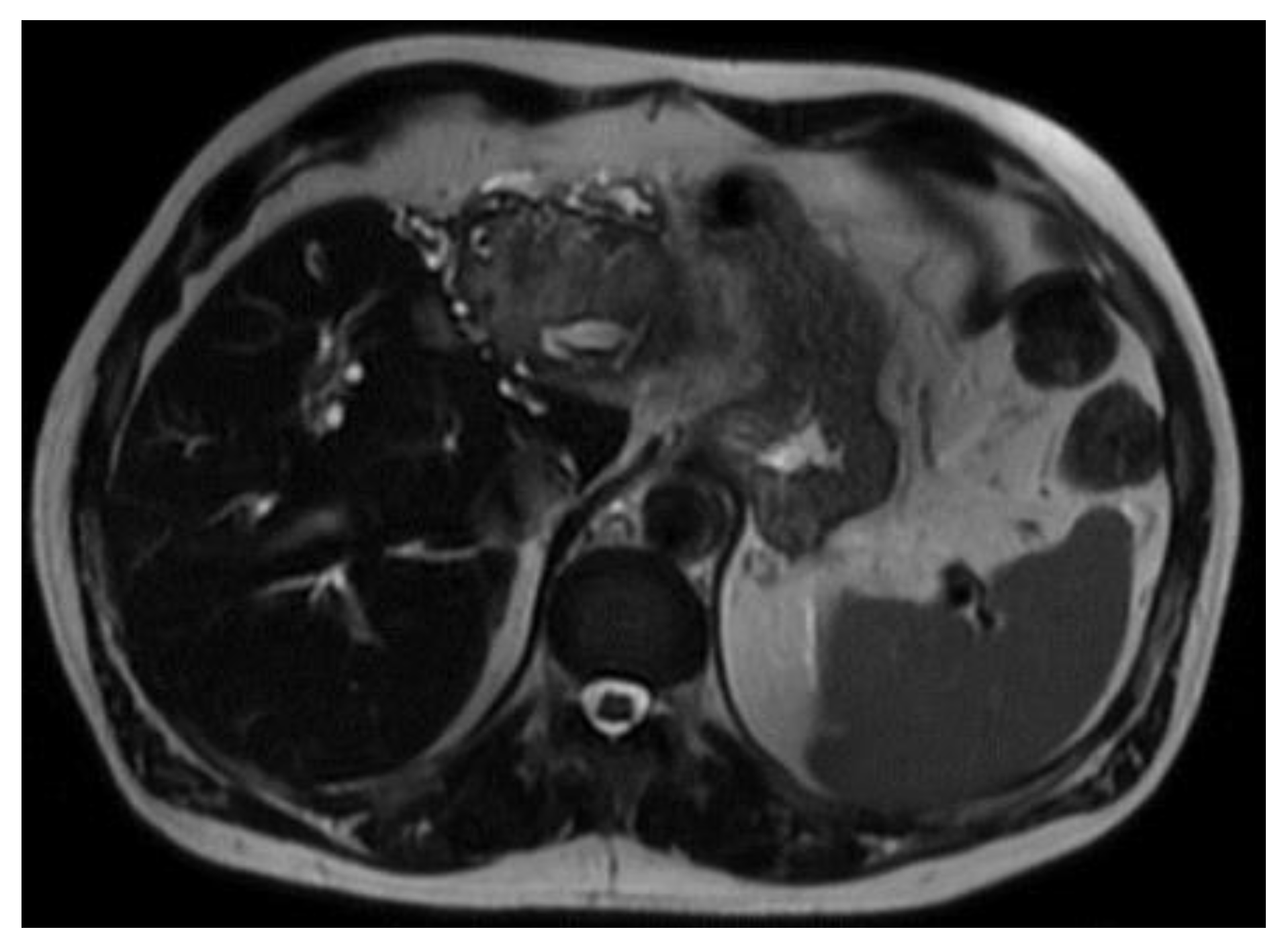
In preparation for the procedure, it was noted that the patient had endorsed lethargy over the past few weeks. Additionally, preprocedural routine labs were notable for a direct bilirubin of 2.93 mg/dL. Due to the polypoid and irregular nature of the lesion, his concomitant lethargy, and direct bilirubinemia, a CT scan of the patient’s abdomen and pelvis was performed, which revealed a distal intrahepatic cholangiocarcinoma with involvement of left hepatic lobe (
Figure 1) and umbilical induration corresponding to the skin lesion (
Figure 2). A magnetic resonance cholangiopancreatography (MRCP) was performed for further characterization of the cholangiocarcinoma, which revealed an intrahepatic cholangiocarcinoma (
Figure 3).
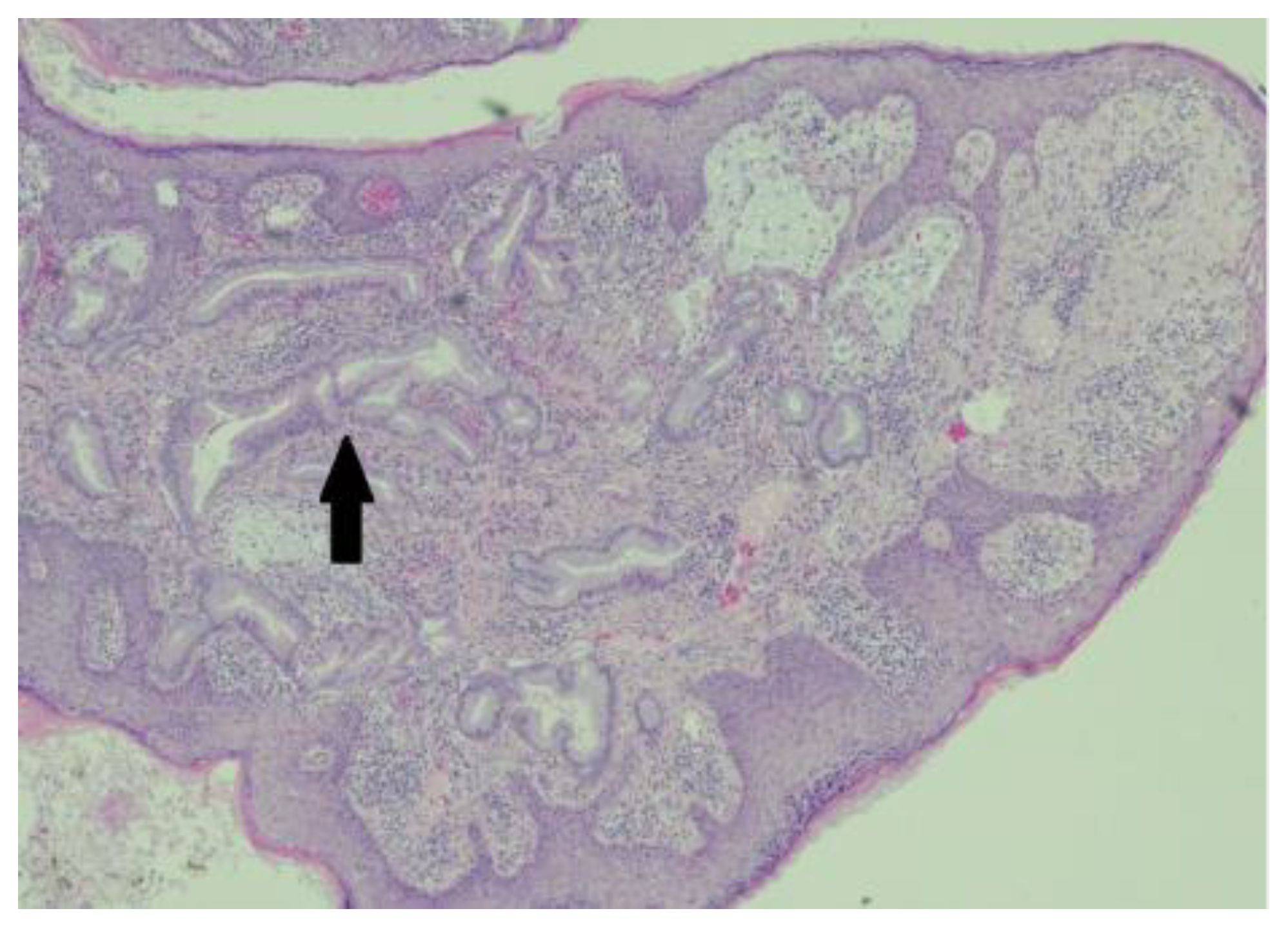
An excisional biopsy of the umbilical mass was performed and the specimen was fixed in formalin. Pathology of the umbilical mass was compatible with metastatic carcinoma. The specimen showed malignant glands infiltrating through the papillary and reticular dermis with nuclear palisading in the metastatic glands, luminal macrophages, associated inflammatory response, desmoplasia, pseudoepitheliomatous hyperplasia of the overlying squamous epithelium, and occasional inflammatory cells infiltrating the epidermis, as seen in
Figure 4.
Following the procedure and diagnosis of metastatic cholangiocarcinoma, the patient was referred for palliative chemotherapy and biliary stenting at another facility. Further follow-up was unavailable to document the patient’s long-term response.
3. Discussion
In this case report, we describe a 65-year-old previously healthy male with approximately one month of fatigue and cholestatic symptoms who presented for an elective umbilical hernia repair. The patient’s abnormal labs, history of fatigue, and atypical umbilical mass increased clinical suspicion for potential malignancy. Further diagnostic imaging and pathology confirmed distal intrahepatic cholangiocarcinoma involving the left liver lobe with metastasis to the umbilicus, which was initially misdiagnosed as an umbilical hernia.
SMJN is a rare extra intestinal manifestation of underlying intra-abdominal and pelvic malignancies that present as umbilical masses [
2]. Their detection often indicates an ominous sign of advanced metastasis and is associated with significantly reduced patient survival. A major barrier to early detection lies with both patients and clinicians. The typically benign appearance of the lesion and its infrequent occurrence reduce the likelihood of patients reporting it or clinicians correctly identifying it [
10]. Additionally, the lesion may be misdiagnosed as a benign epithelial cyst, umbilical hernia, granuloma, umbolith, or endometrial deposit [
10]. Possible primary umbilical malignancies also include malignant melanoma, basal cell carcinoma, and mesenchymal tumors [
11]. Because most differential diagnoses for umbilical masses are benign, a false sense of reassurance can occur. Rising rates of intra-abdominal and pelvic malignancies, and their potential extra intestinal manifestations, should prompt a high index of suspicion for malignancy.
Another major barrier to diagnosing a SMJN is the wide variability in its clinical appearance. Clinically, the lesions are often firm, irregular shaped masses fixed to the skin [
10]. They may range from indurated, painful plaques that are ulcerated or fissured, to erythematous, painless, pruritic nodules with a vascular appearance [
10,
11]. The nodule may occasionally secrete pus, blood or serous fluid while others may be void of any discharge [12]. In this case study, the patient had a mildly erythematous, polypoid mass with a cauliflower-like appearance. This further emphasizes how broad variation among lesions complicates the recognition of SMJNs.
Most SMJNs are adenocarcinomas originating from intra-abdominal or pelvic malignancies. Gastric carcinomas are the most common sources, accounting for up to 25% of cases, followed by ovarian, colorectal, and pancreatic malignancies [
11]. SMJN arising from cholangiocarcinoma remains extremely rare, with only ten prior cases being reported, and thus making this case the eleventh [
2]. CCA metastasis often occurs via lymphatic or hematogenous routes, and the abundant vascular and lymphatic supply of the umbilicus may facilitate the spread from the primary tumor [
2,
9]. This highlights the importance of early recognition of these rare umbilical metastases, which can aid in earlier diagnosis and management of advanced abdominal malignancies.
The prognosis of Cholangiocarcinoma remains poor, as it is often incurable and largely refractory to both surgical and medical interventions [
4]. Although the overall pathogenesis is consistent, differences between intrahepatic and extrahepatic classifications, along with associated infectious and noninfectious etiologies, result in a broad spectrum of clinical behaviors and management pathways. Additionally, the rarity of CCA has limited the depth of available studies and clinical guidance. The rising incidence and mortality associated with CCA underscores the need for increased awareness and further research regarding its diagnosis and treatment.
This case of a Sister Mary Joseph Nodule found in the setting of cholangiocarcinoma illustrates the complex interactions between neoplasms and different organ systems. Early recognition of these manifestations can increase clinical awareness and aid in early detection with the goal of improving patient outcomes.
4. Conclusion
Sister Mary Joseph Nodules are rare extra intestinal manifestations indicative of intra-abdominal and pelvic malignancies including cholangiocarcinoma. This finding suggests advanced disease processes and oftentimes a poor prognosis. This case, to the best of our knowledge, represents the 11th reported case of SMJN in the setting of CCA. Furthermore, this emphasizes the importance of early recognition and further research into the complex disease process for improvement in long-term management and palliative care.
Author Contributions
Conceptualization, formal analysis, resources, data curation, and writing – original draft preparation, Toni Esposito; methodology, validation, and writing – review and editing, Dr. Niharika Singh; supervision and project administration, Dr. Riddhish Sheth. Dr.George Keckeisen. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
SMJN Sister Mary Joseph Nodule
CCA Cholangiocarcinoma
References
- Chang, J.; et al. An integrated microfluidic system for automatic detection of cholangiocarcinoma cells from bile. Lab Chip 2024, 24, 375–382. [Google Scholar] [CrossRef] [PubMed]
- Ismail, B.; et al. Sister Mary Joseph’s nodule: A rare metastasis of hilar cholangiocarcinoma: A new case report and review of the literature. Helion 2025, 11, e42449. [Google Scholar] [CrossRef] [PubMed]
- Qurashi, M.; Vithayathil, M.; Khan, S. Epidemiology of cholangiocarcinoma. European Journal of Surgical Oncology 2025, 51, 107064. [Google Scholar] [CrossRef] [PubMed]
- Braconi, C.; Patel, T. Cholangiocarcinoma: New Insights into Disease Pathogenesis and Biology. Infectious Disease Clinics of North America 2010, 24, 871–884. [Google Scholar] [CrossRef] [PubMed]
- Vithayathil, M.; Khan, S. Current Epidemiology of cholangiocarcinoma in Western countries. Journal of Hepatology 2022, 77, 1690–1698. [Google Scholar] [CrossRef] [PubMed]
- O’ Conner-Byrne, N.; et al. Sister Mary Joseph nodule in mantle cell lymphoma. Lancet Oncology 2020, 21, e337. [Google Scholar] [CrossRef] [PubMed]
- Qi, A.; et al. Sister Mary Joseph’s Nodule from Fallopian tube cancer. Asian Journal of Surgery 2025, 48, 2686–2687. [Google Scholar]
- Palaniappan, M.; et al. Umbilical metastasis: a case series of four Sister Joseph nodules from four different visceral malignancies. Current Oncology 2010, 17, 78–81. [Google Scholar] [CrossRef] [PubMed]
- Wronski, M.; et al. Sister Mary Joseph Nodule: A Tip of an Iceberg. Journal of Ultrasound in Medicine 2014, 33, 531–534. [Google Scholar] [CrossRef] [PubMed]
- Rubik, R.; et al. Umbilical nodule – A not always innocuous abdominal finding. Journal of Cancer Research and Therapeutics 2023, 19, 946–949. [Google Scholar] [CrossRef] [PubMed]
- Sina, B.; Deng, A. Umbilical metastasis from prostate carcinoma (Sister Mary Joseph’s nodule): a case report and review of literature. Journal of Cutaneous Pathology 2006, 34, 581–583. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).