Submitted:
15 December 2025
Posted:
17 December 2025
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
3. Results
3.1. Study Characteristics
3.2. Procedures and Facial Regions Prioritized
3.3. Outcome Domains
3.4. Primary Outcomes
3.5. Outcome Tracking and Measurement
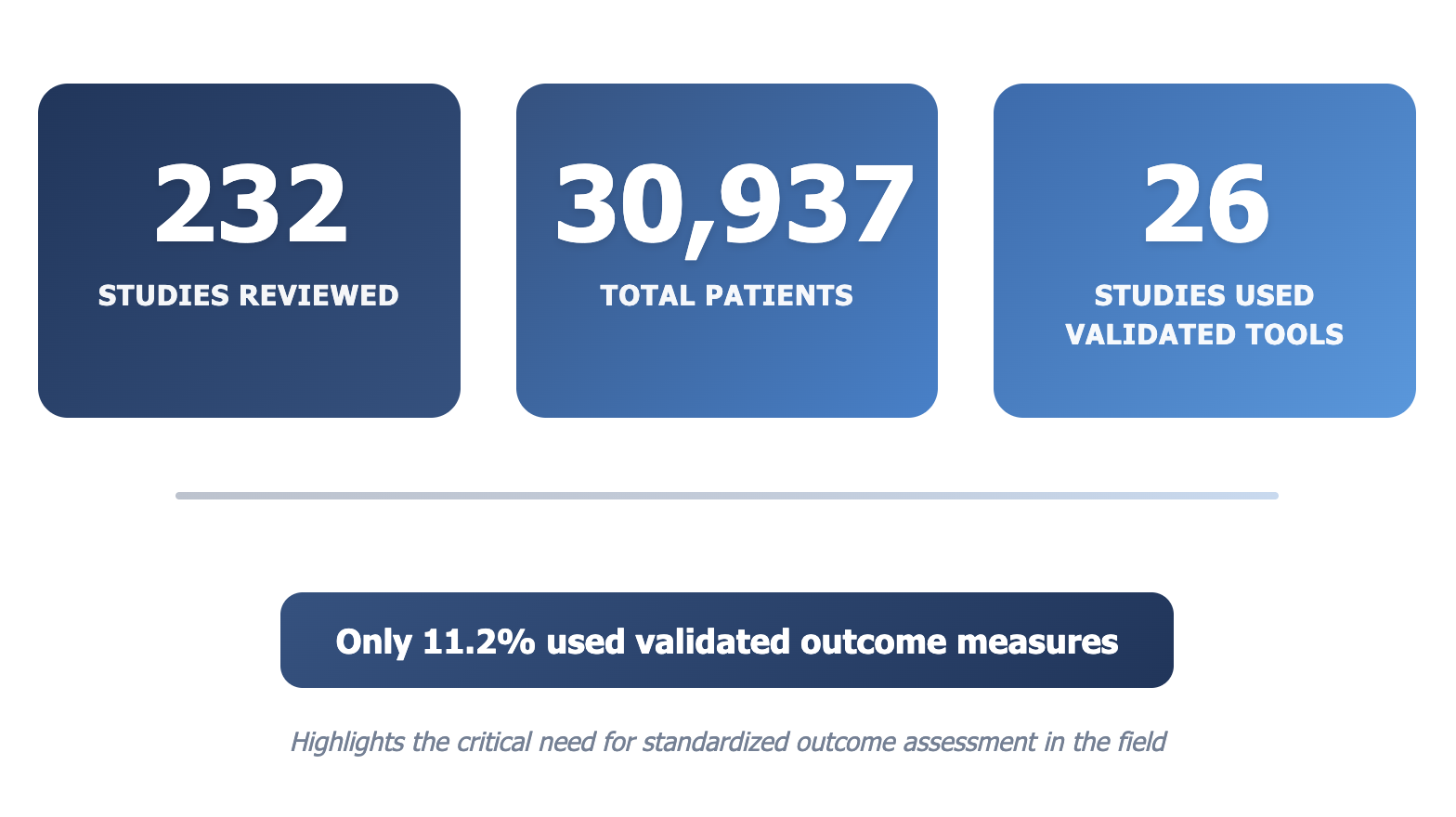
3.6. Validated Measurement Tools
3.7. Quality Assessment
3.8. Risk of Bias Assessment

| Outcome Domain | Papers Reported (%) |
|---|---|
| Psychosocial | 43.19 |
| Measurements | 37.09 |
| Aesthetics | 60.56 |
| Reoperation/Readmission | 21.60 |
| Complication | 62.44 |
| HRQOL | 22.54 |
| Other | 25.35 |
| Outcomes Reported | Papers Reported (%) |
|---|---|
| Quality of Life / Reintegration into Society | 35.21 |
| Observer-rated Appearance | 17.37 |
| Artificial Intelligence Rating | 0.94 |
| Quantitative Anatomical Measurement | 25.82 |
| Other | 45.07 |
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Registration
Abbreviations
| FGAS | Facial Gender Affirming Surgery |
| COS | Core Outcome Set |
| PROMIS | Patient-Reported Outcomes Measurement Information System. |
| FACE-Q | Facial Appearance and Cosmetic Enhancement Questionnaire |
Appendix A
| Database: PubMed Search Date: March 15, 2025 Search Strategy: ( transgender*[Title/Abstract] OR transsexual*[Title/Abstract] OR “gender dysphor*”[Title/Abstract] OR “gender incongruen*”[Title/Abstract] OR “gender non-binary”[Title/Abstract] OR “gender affirm*”[Title/Abstract] OR “gender transition*”[Title/Abstract] OR “gender reassign*”[Title/Abstract] OR “male-to-female”[Title/Abstract] OR “female-to-male”[Title/Abstract] ) AND ( “facial gender affirming surgery”[Title/Abstract] OR “facial gender confirmation surgery”[Title/Abstract] OR “facial feminization surgery”[Title/Abstract] OR “facial feminization surgeries”[Title/Abstract] OR “facial masculinization surgery”[Title/Abstract] OR “gender affirming facial surgery”[Title/Abstract] OR “gender confirming facial surgery”[Title/Abstract] OR (“FFS”[Title/Abstract] AND (transgender*[Title/Abstract] OR “gender affirm*”[Title/Abstract] OR “gender dysphoria”[Title/Abstract])) OR (“FMS”[Title/Abstract] AND (transgender*[Title/Abstract] OR “gender affirm*”[Title/Abstract] OR “gender dysphoria”[Title/Abstract])) OR ( (“feminization”[Title/Abstract] OR “masculinization”[Title/Abstract] OR “feminizing”[Title/Abstract] OR “masculinizing”[Title/Abstract]) AND (“facial surgery”[Title/Abstract] OR “face”[Title/Abstract] OR “jaw”[Title/Abstract] OR “chin”[Title/Abstract] OR “cheek”[Title/Abstract] OR “mandible”[Title/Abstract] OR “rhinoplasty”[Title/Abstract] OR “forehead”[Title/Abstract] OR “brow”[Title/Abstract] OR “tracheal shave”[Title/Abstract] OR “chondrolaryngoplasty”[Title/Abstract] OR “genioplasty”[Title/Abstract]) ) OR ( (“facial bone”[Title/Abstract] OR “forehead”[Title/Abstract] OR “brow”[Title/Abstract] OR “jaw”[Title/Abstract] OR “chin”[Title/Abstract] OR “cheek”[Title/Abstract] OR “rhinoplasty”[Title/Abstract] OR “mandible”[Title/Abstract] OR “mandibular”[Title/Abstract] OR “orbital”[Title/Abstract] OR “tracheal shave”[Title/Abstract] OR “chondrolaryngoplasty”[Title/Abstract]) AND (“surgery”[Title/Abstract] OR “surgical”[Title/Abstract] OR “contouring”[Title/Abstract] OR “reconstruction”[Title/Abstract] OR “reduction”[Title/Abstract] OR “augmentation”[Title/Abstract]) AND (“transgender”[Title/Abstract] OR “transsexual”[Title/Abstract] OR “gender affirming”[Title/Abstract] OR “gender dysphoria”[Title/Abstract]) ) ) NOT (“cosmetic surgery”[Title/Abstract] NOT (“transgender”[Title/Abstract] OR “gender affirming”[Title/Abstract])) NOT (“aesthetic surgery”[Title/Abstract] NOT (“transgender”[Title/Abstract] OR “gender affirming”[Title/Abstract])) NOT (“facial rejuvenation”[Title/Abstract] NOT (“transgender”[Title/Abstract] OR “gender affirming”[Title/Abstract])) NOT (“facial trauma”[Title/Abstract] NOT (“transgender”[Title/Abstract] OR “gender affirming”[Title/Abstract])) NOT (“facial reconstruction cancer”[Title/Abstract] NOT (“transgender”[Title/Abstract] OR “gender affirming”[Title/Abstract])) NOT (“facial deformity”[Title/Abstract] NOT (“transgender”[Title/Abstract] OR “gender affirming”[Title/Abstract])) NOT (“congenital facial”[Title/Abstract] NOT (“transgender”[Title/Abstract] OR “gender affirming”[Title/Abstract])) NOT (“cisgender”[Title/Abstract] NOT (“transgender”[Title/Abstract] OR “gender affirming”[Title/Abstract])) |
| Citation | N | Study Type | Facial Regions |
|---|---|---|---|
| Lee, H. H., & Singh, M. (2022). Jaw reduction surgery. Otolaryngol Clin North Am, 55(4), 859-870. | 3000 | Retrospective | Lower face |
| Tolley, P., Susarla, S., & Ettinger, R. E. (2024). Gender-affirming facial surgery: lower third of the face. Oral and Maxillofacial Surgery Clinics, 36(2), 207-219. | 0 | Retrospective | Whole face |
| Berli, J. U., & Loyo, M. (2019). Gender-confirming rhinoplasty. Facial Plastic Surgery Clinics, 27(2), 251-260. | 0 | Review | Middle face |
| Gupta, N., & Clark, C. (2023). Forehead Contouring. Facial Plastic Surgery Clinics of North America, 31(3), 363-370. | 0 | Review | Upper face |
| Gupta, N., & Clark, C. (2023). Forehead Contouring. Facial Plastic Surgery Clinics of North America, 31(3), 363-370. | 0 | Review | Upper/middle face |
| Báez-Márquez, J. (2022). Feminization Rhinoplasty. Otolaryngologic Clinics of North America, 55(4), 809-823. | 0 | Review | Middle face |
| Vandenberg, K. N., Plocienniczak, M. J., & Spiegel, J. H. (2023). Chondrolaryngoplasty. Facial Plastic Surgery Clinics of North America, 31(3), 355-361. | 0 | Review | Neck |
| Salgado, C. J., Nugent, A. G., Satterwaite, T., Carruthers, K. H., & Joumblat, N. R. (2018). Gender reassignment: feminization and masculinization of the neck. Clinics in plastic surgery, 45(4), 635-645. | 0 | Retrospective | Upper/middle face |
| Spiegel, J. H. (2019). Facial feminization for the transgender patient. Journal of Craniofacial Surgery, 30(5), 1399-1402. | 0 | Review | Face/neck |
| Tang, C. G., Debbaneh, P. M., & Kleinberger, A. J. (2022). Chondrolaryngoplasty. Otolaryngologic Clinics of North America, 55(4), 871-884. | 0 | Review | Neck |
| Salibian, A. A., & Bluebond-Langner, R. (2019). Lip lift. Facial Plastic Surgery Clinics, 27(2), 261-266. | 0 | Review | Lower face |
| Sturm, A., & Chaiet, S. R. (2019). Chondrolaryngoplasty-thyroid cartilage reduction. Facial plastic surgery clinics of North America, 27(2), 267-272. | 0 | Review | Neck |
| Vandenberg, K. N., Plocienniczak, M. J., & Spiegel, J. H. (2023). Chondrolaryngoplasty. Facial Plastic Surgery Clinics of North America, 31(3), 355-361. | 0 | Prospective | Upper face |
| Lundgren, K. C., & Koudstaal, M. J. (2019). Midfacial bony remodeling. Facial Plast Surg Clin North Am, 27(2), 221-226. | 0 | Prospective | Middle face |
| England, H., & Totonchi, A. (2023). Commentary on: Facial Gender Affirming Surgery: Frontal Bossing Surgical Techniques Outcomes and Safety. Aesthetic Plastic Surgery, 47(4), 1362-1363. | 0 | Commentary | Upper face |
| Flaherty, A. J., Sharma, A., Crosby, D. L., & Nuara, M. J. (2020). Should gender-affirming surgery Be prioritized during the COVID-19 pandemic?. Otolaryngology–Head and Neck Surgery, 163(6), 1140-1143. | 0 | Commentary | Face/neck |
| Ching, A. H., & Persing, J. A. (2022). Objectification of transgender female patients in surgical goals of facial feminization surgery. Plastic and Reconstructive Surgery, 149(2), 358e-360e. | 0 | Commentary | Middle/lower face |
| Selvaggi, G., Vieira Saint Clair Mafra, N., & Tarnow, P. (2025). Commentary on: Facial Gender-Affirming Surgery: Frontal Bossing Surgical Techniques, Outcomes and Safety. Aesthetic Plastic Surgery, 49(11), 3339-3340. | 0 | Commentary | Upper face |
| Gibstein, A. R., Jabori, S. K., & Danker, S. (2022). Facial feminization surgery: part 1 of the plastic surgeon’s perspective of gender-affirming surgery. Plastic and Aesthetic Nursing, 42(3), 137-142. | 0 | Review | Whole face |
| Spiegel, J. H. (2020). Gender affirming and aesthetic cranioplasty: what’s new?. Current opinion in otolaryngology & head and neck surgery, 28(4), 201-205. | 0 | Review | Upper face |
| Massenburg, B. B., Ettinger, R. E., & Morrison, S. D. (2023). Gender-affirming surgery of the mandible: lower jaw feminization and masculinization. Facial Plastic Surgery Clinics, 31(3), 381-392. | 0 | Review | Lower face |
| Weinstein, B., Alba, B., Dorafshar, A., & Schechter, L. (2023). Gender Facial Affirmation Surgery: Cheek Augmentation. Facial Plastic Surgery Clinics of North America, 31(3), 393-397. | 0 | Review | Middle face |
| Jumaily, J. S. (2022). Cheek Augmentation in Gender-Affirming Facial Surgery. Otolaryngologic Clinics of North America, 55(4), 825-834. | 0 | Review | Middle face |
| Donaldson, L., Okifo, F., & Garcia-Rodriguez, L. (2023). Preparing for Facial Feminization Surgery. Facial plastic surgery clinics of North America, 31(3), 349-354. | 0 | Review | Face/neck |
| Rodman, R. (2022). Developments in facial feminization surgery. Current Opinion in Otolaryngology & Head and Neck Surgery, 30(4), 249-253. | 0 | Review | Whole face |
| Jacobs, J., & Flaherty, A. J. (2023). Re:“Sex Differences in Adult Facial Three-Dimensional Morphology: Application to Gender-Affirming Facial Surgery” by Bannister et al. Facial Plastic Surgery & Aesthetic Medicine, 25(6), 455-455. | 0 | Commentary | Whole face |
| Jordan Deschamps-Braly, M. D. (2019). Feminization of the Chin Genioplasty Using Osteotomies. Facial Gender Affirmation Surgery, An Issue of Facial Plastic Surgery Clinics of North America, 27(2), 243. | 0 | Review | Lower face |
| Van Boerum, M. S., Salibian, A. A., Bluebond-Langner, R., & Agarwal, C. (2019). Chest and facial surgery for the transgender patient. Translational Andrology and Urology, 8(3), 219. | 0 | Review | Face/neck |
| Sykes, J. M., Dilger, A. E., & Sinclair, A. (2019). Surgical Facial Esthetics for Gender Affirmation. Dermatologic Clinics, 38(2), 261-268. | 0 | Review | Face/neck |
| Sykes, J. M., Dilger, A. E., & Sinclair, A. (2019). Surgical Facial Esthetics for Gender Affirmation. Dermatologic Clinics, 38(2), 261-268. | 0 | Commentary | Upper face |
| Therattil, P. J., Hazim, N. Y., Cohen, W. A., & Keith, J. D. (2019). Esthetic reduction of the thyroid cartilage: a systematic review of chondrolaryngoplasty. JPRAS open, 22, 27-32. | 69 | Review | Neck |
| Tollinche, L. E., Rosa, W. E., & van Rooyen, C. D. (2021). Perioperative considerations for person-centered gender affirming surgery. Advances in anesthesia, 39, 77. | 0 | Review | Face/neck |
| Morrison, S. D., & Satterwhite, T. (2019). Lower jaw recontouring in facial gender-affirming surgery. Facial Plastic Surgery Clinics, 27(2), 233-242. | 0 | Review | Middle/lower face |
| Juszczak, H. M., Fridirici, Z., Knott, P. D., Park, A. M., & Seth, R. (2019). An update in facial gender confirming surgery. Current Opinion in Otolaryngology & Head and Neck Surgery, 27(4), 243-252. | 0 | Review | Face/neck |
| Chao, J. W., & Malyavko, A. (2020). The utility of diced cartilage fascia graft augmentation of the nasal dorsum in transgender feminizing rhinoplasty. Plastic and Reconstructive Surgery, 146(5), 697e-698e. | 7 | Review | Middle face |
| Barnett, S. L., Choe, J., Aiello, C., & Bradley, J. P. (2023). Facial feminization surgery: anatomical differences, preoperative planning, techniques, and ethical considerations. Medicina, 59(12), 2070. | 0 | Review | Whole face |
| Glorion, A., Perrillat, A., Foletti, J. M., & Cristofari, S. (2022). Surgical techniques used in chin feminization: Literature review and knowledge update. Journal of Stomatology, Oral and Maxillofacial Surgery, 123(6), e883-e887. | 0 | Review | Lower face |
| Rodman, R. (2022). Commentary on “Sex Differences in Adult Facial 3D Morphology: Application of Gender-Affirming Facial Surgery” by Bannister et al. Facial Plastic Surgery & Aesthetic Medicine, 24(S2), S-31. | 0 | Commentary | Whole face |
| Harris, J., Premaratne, I. D., & Spector, J. A. (2021). Facial masculinization from procedures to payment: a review. LGBT health, 8(7), 444-453. | 0 | Review | Whole face |
| Callen, A. L., Badiee, R. K., Phelps, A., Potigailo, V., Wang, E., Lee, S., ... & Narvid, J. (2021). Facial feminization surgery: key CT findings for preoperative planning and postoperative evaluation. American Journal of Roentgenology, 217(3), 709-717. | 0 | Review | Whole face |
| Aires, M. M., Vasconcelos, D. D., & Moraes, B. T. D. (2021). Chondrolaryngoplasty in transgender women: Prospective analysis of voice and aesthetic satisfaction. International Journal of Transgender Health, 22(4), 394-402. | 15 | Prospective | Neck |
| Labarthe, P., Beaudoin, P. L., Wong, E., Garrel, R., de Boutray, M., & Damecourt, A. (2023). Combined genioplasty, chondrolaryngoplasty, and glottoplasty: A novel scarless procedure in facial feminization surgery. Journal of Stomatology, Oral and Maxillofacial Surgery, 124(6), 101575. | 15 | Case Study | Lower face |
| Hohman, M. H., & Teixeira, J. (2021). Transgender surgery of the head and neck. | 0 | Review | Whole face |
| Escandón, J. M., Morrison, C. S., Langstein, H. N., Ciudad, P., Del Corral, G., & Manrique, O. J. (2022). Applications of three-dimensional surgical planning in facial feminization surgery: a systematic review. Journal of Plastic, Reconstructive & Aesthetic Surgery, 75(7), e1-e14. | 1473 | Review | Whole face |
| Pansritum, K. (2021). Forehead and hairline surgery for gender affirmation. Plastic and Reconstructive Surgery–Global Open, 9(3), e3486. | 23 | Retrospective | Upper face |
| Nassar, A., Naba, J., & Demian, J. (2024). Lip feminization: A review. JPRAS open, 41, 311-319. | 0 | Review | Lower face |
| Tang, C. G. (2020). Evaluating patient benefit from laryngochondroplasty. The Laryngoscope, 130, S1-S14. | 73 | Retrospective | Neck |
| Mommaerts, M. Y., Voisin, C., Otero, J. J., & Loomans, N. A. J. (2019). Mandibular feminization osteotomy—preliminary results. International Journal of Oral and Maxillofacial Surgery, 48(5), 597-600. | 5 | Retrospective | Lower face |
| Tolley, P., Susarla, S., & Ettinger, R. E. (2024). Gender-affirming facial surgery: lower third of the face. Oral and Maxillofacial Surgery Clinics, 36(2), 207-219. | 0 | Review | Face/neck |
| Thomas, J. P. (2022). Feminization Laryngoplasty-A Comprehensive Approach to Reducing the Size of the Larynx and Pharynx. Otolaryngologic Clinics of North America, 55(4), 739-748. | 0 | Review | Neck |
| Ramly, E. P., Katave, C., & Ranganathan, K. (2024). Facial feminization: Upper third of the face. Oral and Maxillofacial Surgery Clinics, 36(2), 183-194. | 0 | Review | Upper face |
| Ascha, M., Hassan, B., & Liang, F. (2024). Facial feminization: middle third of the face. Oral and Maxillofacial Surgery Clinics, 36(2), 195-205. | 0 | Review | Middle face |
| Özer, M., Toulabi, S. P., Fisher, A. D., t’Sjoen, G., Buncamper, M. E., Monstrey, S., ... & Motmans, J. (2022). ESSM position statement “sexual wellbeing after gender affirming surgery”. | 0 | Review | Whole body |
| Ngaage, L. M., McGlone, K. L., Xue, S., Knighton, B. J., Benzel, C. A., Rada, E. M., ... & Rasko, Y. M. (2020). Gender surgery beyond chest and genitals: current insurance landscape. Aesthetic surgery journal, 40(4), NP202-NP210. | 0 | Review | Whole face |
| Akhavan, A. A., Pang, J. H., Morrison, S. D., & Satterwhite, T. (2024). Gender Affirming Facial Surgery–Anatomy and Procedures for Facial Masculinization. Oral and Maxillofacial Surgery Clinics, 36(2), 221-236. | 0 | Review | Whole face |
| Hazkour, N., Palacios, J., Lu, W., Goote, P., Rivera, R., & Bastidas, N. (2022). Multiprocedural facial feminization surgery: a review of complications in a cohort of 31 patients. Journal of Craniofacial Surgery, 33(8), 2502-2506. | 31 | Review | Whole face |
| Donaldson, L., Wulu, J., & Garcia-Rodriguez, L. (2023). Gender affirmation surgery of the face for the transfeminine patient. Facial Plastic Surgery, 39(05), 569-574. | 0 | Review | Whole face |
| Bonapace-Potvin, M., Pepin, M., Navals, P., Medor, M. C., Lorange, E., & Bensimon, E. (2023). Facial gender-affirming surgery: Frontal bossing surgical techniques, outcomes and safety. Aesthetic Plastic Surgery, 47(4), 1353-1361. | 100 | Retrospective | Upper face |
| Amendola, S., Stemmler, N., Cosgrove, M., & Ruggiero, F. (2024). Anesthetic Considerations for Gender-Affirming Airway and Facial Procedures. AANA journal, 92(4). | 0 | Review | Whole face |
| Caprini, R. M., Oberoi, M. K., Dejam, D., Chan, C. H., Potemra, H. I. M., Morgan, K. B., ... & Lee, J. C. (2023). Effect of gender-affirming facial feminization surgery on psychosocial outcomes. Annals of surgery, 277(5), e1184-e1190. | 169 | Comparative cohort study | Whole face |
| Stowell, J. T., Jha, P., Martinez-Jorge, J., Middlebrooks, E. H., Broderick, D. F., & Bhatt, A. A. (2022). Neuroradiology in transgender care: facial feminization, laryngeal surgery, and beyond. Radiographics, 42(1), 233-249. | 0 | Review | Face/neck |
| Ihnat, J. M., Aral, A., Mukherjee, T., & Alperovich, M. (2024, August). Computerized surgical planning in gender affirming facial surgery. In Seminars in Plastic Surgery (Vol. 38, No. 03, pp. 209-213). Thieme Medical Publishers, Inc.. | 0 | Review | Face/neck |
| Murphy, A. I., Asadourian, P. A., Marano, A. A., & Rohde, C. H. (2022). Patients and procedures of facial gender confirmation surgery: a NSQIP study. Journal of Craniofacial Surgery, 33(1), 298-302. | 203 | Retrospective | Face/neck |
| Salesky, M., Zebolsky, A. L., Benjamin, T., Wulu, J. A., Park, A., Knott, P. D., & Seth, R. (2022). Gender-affirming facial surgery: experiences and outcomes at an academic center. Facial Plastic Surgery & Aesthetic Medicine, 24(1), 54-59. | 77 | Retrospective | Whole face |
| Asokan, A., Sudheendran, M. K., Mohandas, M., George, P. S., & Nair, R. M. (2023). Facial Feminization Surgery: Preoperative Planning and Surgical Technique for a Harmonious Outcome. Indian Journal of Plastic Surgery, 56(04), 298-309. | 0 | Case | Face/neck |
| Colebunders, B., Brondeel, S., D’Arpa, S., Hoebeke, P., & Monstrey, S. (2017). An update on the surgical treatment for transgender patients. Sexual medicine reviews, 5(1), 103-109. | 0 | Review | Whole body |
| MacGregor, J. L., & Chang, Y. C. (2020). Minimally invasive procedures for gender affirmation. Dermatologic clinics, 38(2), 249-260. | 0 | Review | Whole face, jaw |
| Knox, J., & Hoffman, W. Y. (2024). Facial Gender-Affirming. Gender Affirming Surgery, An Issue of Oral and Maxillofacial Surgery Clinics of North America, E-Book: Gender Affirming Surgery, An Issue of Oral and Maxillofacial Surgery Clinics of North America, E-Book, 36(2), 237. | 0 | Review | Face/neck |
| Alper, D. P., Almeida, M. N., Hu, K. G., De Baun, H. M., Hosseini, H., Williams, M. C., ... & Alperovich, M. (2023). Quantifying facial feminization surgery’s impact: focus on patient facial satisfaction. Plastic and Reconstructive Surgery–Global Open, 11(11), e5366. | 48 | Prospective, Retrospective | Face/neck |
| Fakurnejad, S., Mohan, S., Seth, R., & Knott, P. D. (2025). Functional and cosmetic considerations in gender-affirming feminization rhinoplasty. Otolaryngologic Clinics of North America, 58(2), 315-323. | 0 | Review | Middle face |
| Ihnat, J., Hu, K. G., Wood, S., Sutherland, R., Allam, O., Parikh, N., & Alperovich, M. (2025). Trends in revision facial feminization surgery. Journal of Craniofacial Surgery, 36(2), 769-772. | 327 | Retrospective | |
| Patel, V., Nolan, I. T., Card, E., Morrison, S. D., & Bared, A. (2021). Facial hair transplantation for transgender patients: a literature review and guidelines for practice. Aesthetic Surgery Journal, 41(3), NP42-NP51. | 0 | Review | Lower face |
| Setbacks in Forehead Feminization Cranioplasty: A Systematic Review of Complications and Patient-Reported Outcomes Eggerstedt et al. (2020) | 673 | Review | Upper face |
| Li, D., Xu, L., Yu, Z., Yuan, J., & Wei, M. (2021). Necessity of facial contouring in feminization surgery for Chinese transgender females. Annals of Translational Medicine, 9(7), 603. | 16 | Retrospective | Middle/lower face |
| Chaya, B. F., Berman, Z. P., Boczar, D., Siringo, N., Colon, R. R., Trilles, J., ... & Rodriguez, E. D. (2021). Current trends in facial feminization surgery: an assessment of safety and style. Journal of Craniofacial Surgery, 32(7), 2366-2369. | 77 | Retrospective | Face/neck |
| Ellis, M., Choe, J., Barnett, S. L., Chen, K., & Bradley, J. P. (2024). Facial feminization: perioperative care and surgical approaches. Plastic and reconstructive surgery, 153(1), 181e-193e. | 0 | Review | Whole face |
| Alcon, A., Badiee, R. K., Barnes, L. L., Pardo, S. T., Zevin, B., & Pomerantz, J. H. (2023). Gender-affirming facial feminization surgery at a public, safety-net hospital: a single-center early experience. Journal of Craniofacial Surgery, 34(3), 1010-1014. | 17 | Retrospective | Whole face |
| Hu, A. C., Liu, M. T., & Chan, C. H. (2023). Gender affirming surgery in nonbinary patients: a single institutional experience. Arch Plast Surg 50 (1): 63–69. | 67 | Retrospective | Whole body |
| Sharaf, B., Kuruoglu, D., Bite, U., & Morris, J. M. (2022, August). Point of care virtual surgical planning and 3D printing in facial feminization surgery. In Seminars in Plastic Surgery (Vol. 36, No. 03, pp. 164-168). Thieme Medical Publishers, Inc.. | 0 | Review | Whole face |
| Cronin, B. J., & Lee, J. C. (2024). Preoperative radiology and virtual surgical planning. Oral and Maxillofacial Surgery Clinics, 36(2), 171-182. | 0 | Review | Whole face |
| Tirrell, A. R., El Hawa, A. A. A., Bekeny, J. C., Chang, B. L., & Del Corral, G. (2022). Facial feminization surgery: a systematic review of perioperative surgical planning and outcomes. Plastic and Reconstructive Surgery–Global Open, 10(3), e4210. | 1302 | Review | Face/neck |
| Martin, S. A., Patel, V., Morrison, S. D., Kahn, D., Satterwhite, T., & Nazerali, R. (2021). Assessing gender-affirming chest surgery outcomes: does gender identity alter gaze?. Aesthetic Plastic Surgery, 45(4), 1860-1868. | 32 | Prospective | Whole face |
| Schmidt, M., Ramelli, E., Atlan, M., & Cristofari, S. (2023). FACE-Q satisfaction following upper third facial gender-affirming surgery using custom bone-section guides. International Journal of Oral and Maxillofacial Surgery, 52(6), 696-702. | 42 | Prospective | Upper face |
| Nuyen, B., Qian, Z. J., Rakkar, M., Thomas, J. P., Erickson-DiRenzo, E., & Sung, C. K. (2023). Diagnosis and management of vocal complications after chondrolaryngoplasty. The Laryngoscope, 133(9), 2301-2307. | 27 | Retrospective | Neck |
| Eble, D. J., Nguyen, A. L., Roblee, C. V., Tople, T. L., Friedrich, J. B., Skokan, A. J., ... & Morrison, S. D. (2024). Conscientious objection to gender-affirming surgery: A cross-sectional analysis of plastic surgery and urology residency programs. Journal of Surgical Education, 81(11), 1675-1682. | 0 | Review | Whole face |
| Moghadam, S., Shariati, K., Huang, K. X., Chin, M. G., LaGuardia, J. S., Bedar, M., ... & Lee, J. C. (2024). The type I+ forehead in facial feminization surgery. Aesthetic Plastic Surgery, 48(23), 4778-4783. | 123 | Retrospective | Upper Face |
| James, A. J., Assi, P. E., Torres-Guzman, R. A., Nemani, S. V., Saad, M., Kalmar, C. L., ... & Al Kassis, S. (2025). Optimizing Safety and Aesthetics in Facial Feminization: Laryngoscopic-Assisted Chondrolaryngoplasty (2019–2023). Journal of Craniofacial Surgery, 36(2), 750-753. | 32 | Retrospective | Neck |
| Risk Factors for Postsurgical Infections in Facial Feminization Surgery Peleg et al. (2023) | 40 | Retrospective | Whole face |
| Sluiter, E. C., Lane, M., Morrison, S. D., Kuzon, W. M., & Gilman, R. H. (2024). Fat grafting for forehead contouring in facial feminization. Plastic and Reconstructive Surgery–Global Open, 12(8), e6073. | 6 | Case series | Face/neck |
| Sayegh, F., Ludwig, D. C., Ascha, M., Vyas, K., Shakir, A., Kwong, J. W., ... & Morrison, S. D. (2019). Facial masculinization surgery and its role in the treatment of gender dysphoria. Journal of Craniofacial Surgery, 30(5), 1339-1346. | 7 | Systematic Review | Upper/middle face |
| Luong, H. N., Liu, A. S., Sharaf, B. A., Bite, U., & Wagner, L. H. (2025). Effect of Facial Feminization Surgery (FFS) on Eyelid Anatomic Features. Facial Plastic Surgery, 41(03), 307-312. | 34 | Retrospective | Upper face |
| Chou, D. W., Tejani, N., Kleinberger, A., & Shih, C. (2020). Initial facial feminization surgery experience in a multicenter integrated health care system. Otolaryngology–Head and Neck Surgery, 163(4), 737-742. | 121 | Retrospective cohort | Face/neck |
| Morrison, S. D., Vyas, K. S., Motakef, S., Gast, K. M., Chung, M. T., Rashidi, V., ... & Cederna, P. S. (2016). Facial feminization: systematic review of the literature. Plastic and reconstructive surgery, 137(6), 1759-1770. | 1121 | Systematic review | Whole face |
| Ziltzer, R. S., Bellamkonda, N., Smith, A., Lee, J. C., & Mendelsohn, A. H. (2023). Morphometric Analysis and Observer Perceptions Following Transvestibular Chondrolaryngoplasty. Annals of Otology, Rhinology & Laryngology, 132(12), 1557-1563. | 10 | Prospective | Neck |
| Chen, K., Lu, S. M., Cheng, R., Fisher, M., Zhang, B. H., Di Maggio, M., & Bradley, J. P. (2020). Facial recognition neural networks confirm success of facial feminization surgery. Plastic and reconstructive surgery, 145(1), 203-209. | 20 | Retrospective | Whole face |
| Regan, A., Kent, S., & Morrison, R. (2021). Facial feminisation surgery in NHS Scotland. British Journal of Oral and Maxillofacial Surgery, 59(10), 1209-1213. | 60 | Retrospective | Face/neck |
| Khetpal, S., Dahoud, F., Elias, A., Sasson, D. C., Wolfe, E. M., & Lee, J. C. (2024). Feminization of the forehead: a scoping literature review and cohort study of transfeminine patients. Aesthetic Plastic Surgery, 48(18), 3577-3588. | 85 | Lit review and retrospective | Upper face |
| Altman, K. (2012). Facial feminization surgery: current state of the art. International journal of oral and maxillofacial surgery, 41(8), 885-894. | 0 | Narrative review | Face/neck |
| Shoffel-Havakuk, H., Cohen, O., Lahav, Y., & Khafif, A. (2023). Scarless neck feminization by transoral endoscopic vestibular approach chondrolaryngoplasty: a prospective cohort. Otolaryngology–Head and Neck Surgery, 169(1), 31-40. | 12 | Prospective | Neck |
| Dubov, A., & Fraenkel, L. (2018). Facial feminization surgery: the ethics of gatekeeping in transgender health. The American Journal of Bioethics, 18(12), 3-9. | 0 | Narrative review | Whole face |
| Capitán, L., Simon, D., Meyer, T., Alcaide, A., Wells, A., Bailón, C., ... & Capitán-Cañadas, F. (2017). Facial feminization surgery: simultaneous hair transplant during forehead reconstruction. Plastic and reconstructive surgery, 139(3), 573-584. | 65 | Retrospective | Upper face |
| Beaufils, T., Berkane, Y., Luca-Pozner, V., Watier, É., Bertheuil, N., & Qassemyar, Q. (2025). The Nasoorbitofrontal Complex in Facial Feminization Surgery. Plastic and Reconstructive Surgery, 155(2), 341-351. | 155 | Retrospective | Whole face |
| Fakurnejad, S., Park, A. M., Seth, R., & Knott, P. D. (2025). Impact of Gender-Affirming Rhinoplasty Techniques on Objective Facial Appearance. The Laryngoscope, 135(5), 1691-1696. | 33 | Retrospective | Middle face |
| Kalavacherla, S., Kalavacherla, S., Cordero, J., Becker, M., Straus, S., Sheahan, L., & Gosman, A. (2024). Maximizing patient satisfaction in facial feminizing rhinoplasty. Eplasty, 24, e26. | 25 | Retrospective | Middle face |
| Nguyen, N. H., Doan, L., Chu, M. W., Francis, S. H., Liu, Y., & Lee, J. C. (2024). The evolution of a large-scale facial gender affirmation program: A comparative outcomes analysis. Journal of Plastic, Reconstructive & Aesthetic Surgery, 99, 416-419. | 242 | Retrospective | Whole face |
| Selvaggi, G., & Bellringer, J. (2011). Gender reassignment surgery: an overview. Nature Reviews Urology, 8(5), 274-282. | 0 | Review | Face/neck |
| Cronin, B. J., Fadich, S., & Lee, J. C. (2024). Assessing preferences of facial appearance in transgender and gender nonbinary patients. Aesthetic Plastic Surgery, 48(4), 621-632. | 58 | Cross sectional survey | Whole face |
| Balaji, S. M. (2016). Facial feminization-Surgical modification for Indian, European and African faces. Annals of maxillofacial surgery, 6(2), 210-213. | 7 | Retrospective | Whole face |
| Telang, P. S. (2020). Facial feminization surgery: a review of 220 consecutive patients. Indian Journal of Plastic Surgery, 53(02), 244-253. | 220 | Retrospective | Face/neck |
| Pokrowiecki, R., Šufliarsky, B., & Jagielak, M. (2024). Feminization Surgery of the Upper Face as the Crucial Factor in Gender Confirmation—Pearls and Pitfalls. Medicina, 60(1), 120. | 20 | Retrospective | Upper face |
| Ziltzer, R. S., Lett, E., Su-Genyk, P., Chambers, T., & Moayer, R. (2023). Needs assessment of gender-affirming face, neck, and voice procedures and the role of gender dysphoria. Otolaryngology–Head and Neck Surgery, 169(4), 906-916. | 234 | Cross sectional survey | Whole face |
| Gupta, N., White, H., Trott, S., & Spiegel, J. H. (2022). Observer gaze patterns of patient photographs before and after facial feminization. Aesthetic Surgery Journal, 42(7), 725-732. | 10 | Observational experimental | Whole face |
| Altman, K. (2018). Forehead reduction and orbital contouring in facial feminisation surgery for transgender females. British Journal of Oral and Maxillofacial Surgery, 56(3), 192-197. | 64 | Case series/descriptive Study | Upper face |
| Shams, M. G., & Motamedi, M. H. K. (2009). Case report: feminizing the male face. Eplasty, 9, e2. | 10 | Retrospective | Face/neck |
| Bannister, J. J., Juszczak, H., Aponte, J. D., Katz, D. C., Knott, P. D., Weinberg, S. M., ... & Seth, R. (2022). Sex differences in adult facial three-dimensional morphology: application to gender-affirming facial surgery. Facial Plastic Surgery & Aesthetic Medicine, 24(S2), S-24. | 1573 | Retrospective | Middle/lower face |
| La Padula, S., Coiante, E., Beneduce, N., Valentini, V., D’andrea, L., Giudice, G. L., ... & Meningaud, J. P. (2023). Assessment of deep plane facelift in facial feminization surgery: a prospective pilot study. Journal of Plastic, Reconstructive & Aesthetic Surgery, 85, 425-435. | 36 | Prospective | Face/neck |
| Eggerstedt, M., Lee, J. C., & Mendelsohn, A. H. (2024). Transoral feminizing chondrolaryngoplasty: development and deployment of a novel approach in 77 patients. Facial Plastic Surgery & Aesthetic Medicine, 26(5), 618-625. | 77 | Neck | |
| Chaya, B. F., Boczar, D., Colon, R. R., Berman, Z. P., Siringo, N., Diep, G. K., ... & Rodriguez, E. D. (2021). Comparative outcomes of partial and full facial feminization surgery: a retrospective cohort study. Journal of Craniofacial Surgery, 32(7), 2397-2400. | 77 | Retrospective cohort | Whole face |
| Huynh, P. P., Kleinberger, A., Brandstetter, K., Chou, D. W., Pressman, A. R., & Shih, C. (2025). Facial Feminization Surgery and Mental Health Resource Utilization: A Retrospective Institutional Review. Otolaryngology–Head and Neck Surgery, 172(5), 1585-1593. | 478 | Retrospective longitudinal cohort | Whole face |
| Khafif, A., Shoffel-Havakuk, H., Yaish, I., Tordjman, K., & Assadi, N. (2020). Scarless neck feminization: transoral transvestibular approach chondrolaryngoplasty. Facial Plastic Surgery & Aesthetic Medicine, 22(3), 172-180. | 4 | Prospective | Neck |
| Becking, A. G., Tuinzing, D. B., Hage, J. J., & Gooren, L. J. (2007). Transgender feminization of the facial skeleton. Clinics in plastic surgery, 34(3), 557-564. | 35 | Retrospective case series | Whole face |
| Mookerjee, V. G., Alper, D. P., Almeida, M. N., Hu, K. G., Parikh, N., Ihnat, J., ... & Alperovich, M. (2023). Quantitative analysis of morphometric changes in feminization rhinoplasty utilizing a standardized forehead-rhinoplasty technique. In Aesthetic Surgery Journal Open Forum (Vol. 5, p. ojad095). US: Oxford University Press. | 20 | Prospective | Middle face |
| Hu, K. G., Ihnat, J., Parikh, N., Vassallo, M., Almeida, M., Alper, D. P., ... & Alperovich, M. (2024). Finesse in Gender Affirming Frontal Contouring With Corrugator Resection. In Aesthetic Surgery Journal Open Forum (Vol. 6, p. ojae108). US: Oxford University Press. | 12 | Retrospective | Upper face |
| Capitán, L., Simon, D., Kaye, K., & Tenorio, T. (2014). Facial feminization surgery: the forehead. Surgical techniques and analysis of results. Plastic and reconstructive surgery, 134(4), 609-619. | 172 | Retrospective | Upper/lower face |
| Haddad, R., Giovanni, A., & Frandjian, H. (2025). Scarless chondrolaryngoplasty combined with a surgical reshaping of the lower face through a single transoral approach for transgender patients. European Archives of Oto-Rhino-Laryngology, 1-4. | 15 | Retrospective | Lower face |
| Siringo, N. V., Berman, Z. P., Boczar, D., Chaya, B. F., Diep, G. K., Trilles, J., ... & Rodriguez, E. D. (2022). Techniques and trends of facial feminization surgery: a systematic review and representative case report. Annals of Plastic Surgery, 88(6), 704-711. | 3554 | Review | Whole face |
| Dang, B. N., Hu, A. C., Bertrand, A. A., Chan, C. H., Jain, N. S., Pfaff, M. J., ... & Lee, J. C. (2021). Evaluation and treatment of facial feminization surgery: part I. forehead, orbits, eyebrows, eyes, and nose. Archives of Plastic Surgery, 48(05), 503-510. | 0 | Review | Whole face |
| Price, R., Debryn, D., Mukerji, S., Nozari, A., Spiegel, J. H., & Kim, E. (2023). No thromboembolic complications after facial feminization surgery in transgender patients utilizing estrogen therapy: a retrospective cohort study. Transgender Health, 8(4), 344-351. | 282 | Retrospective cohort | Whole face |
| Mukerji, S., Uppalapati, A., Lee, R., Price, R., Debryn, D., Nozari, A., ... & Kim, E. (2023). High incidence of postoperative nausea and vomiting in transgender women undergoing facial feminization procedures. Plastic and Reconstructive Surgery–Global Open, 11(11), e5360. | 282 | Retrospective | Whole face |
| Louis, M., Travieso, R., Oles, N., & Coon, D. (2021). Narrative review of facial gender surgery: approaches and techniques for the frontal sinus and upper third of the face. Annals of Translational Medicine, 9(7), 606. | 0 | Narrative review | Upper face |
| Block-Wheeler, N. R., Chou, D. W., Brandstetter, K., Kleinberger, A., & Shih, C. (2021). Psychological Effect of the COVID-19 Pandemic Among Facial Feminization Surgery Patients. The Permanente Journal, 26(1), 80. | 30 | Retrospective cohort | Whole face |
| Colon, R. R., Chaya, B. F., Berman, Z. P., Diep, G. K., Boczar, D., Trilles, J., & Rodriguez, E. D. (2021). Consideration of human immunodeficiency status in patients seeking facial feminization surgery. Journal of Craniofacial Surgery, 32(7), 2384-2387. | 77 | Retrospective | Middle face |
| Stallworth, J. Y., Hoffman, W. Y., Vagefi, M. R., & Indaram, M. (2023). Superior oblique palsy after facial feminization surgery. Journal of American Association for Pediatric Ophthalmology and Strabismus, 27(3), 165-166. | 2 | Case study | Upper face |
| Patrocinio, L. G., & Patrocinio, J. A. (2024). Secondary forehead lift in transgender women. Facial Plastic Surgery, 38. | 0 | Narrative review | Upper face |
| Neiderman, N. N. C., Arbel, S., Diamant, N., Wolfman, K., Yanko, R., Lior, Y., ... & Oestreicher-Kedem, Y. (2024). Direct Transvestibular Feminization Thyroid Laryngochondroplasty. Plastic and Reconstructive Surgery, 153(2), 467-476. | 9 | Retrospective cohort | Lower face |
| Perrillat, A., Coiante, E., SidAhmed, M., Graillon, N., Hersant, B., & Meningaud, J. P. (2023). Conservative approach to facial upper third feminisation: a retrospective study. Journal of Cranio-Maxillofacial Surgery, 51(2), 98-106. | 48 | Retrospective | Upper face |
| Eisemann, B. S., Wilson, S. C., Ramly, E. P., Kantar, R. S., Alfonso, A. R., Frey, J. D., ... & Rodriguez, E. D. (2020). Technical pearls in frontal and periorbital bone contouring in gender-affirmation surgery. Plastic and Reconstructive Surgery, 146(3), 326e-329e. | 0 | Narrative review | Upper face |
| Kuruoglu, D., Yan, M., Bustos, S. S., Morris, J. M., Alexander, A. E., & Sharaf, B. (2021). Point of care virtual surgical planning and 3D printing in facial gender confirmation surgery: a narrative review. Annals of Translational Medicine, 9(7), 614. | 0 | Narrative review | Upper face |
| Almeida, M. N., Long, A. S., Junn, A. H., Rivera, J. C., Hauc, S. C., Alper, D. P., ... & Alperovich, M. (2024). FACE-Q satisfaction ratings are higher after facial feminization surgery than hormone replacement therapy alone. Transgender Health, 9(5), 436-443. | 23 | Retrospective | Whole face |
| Raffaini, M., Perello, R., Tremolada, C., & Agostini, T. (2019). Evolution of full facial feminization surgery: creating the gendered face with an all-in-one procedure. Journal of Craniofacial Surgery, 30(5), 1419-1424. | 49 | retrospective | Face/neck |
| Kiessling, P., Balakrishnan, K., Fauer, A., Sanan, A., McDonald, D., Thomas, J., ... & Nuyen, B. (2023). Social Perception of External Laryngeal Anatomy Related to Gender Expression in a Web-based Survey. The Laryngoscope, 133(9), 2292-2300. | 16 | Cross sectional survey | Lower face |
| Daurade, M., Brosset, S., Chauvel-Picard, J., Sigaux, N., Mojallal, A., & Boucher, F. (2022). Trans-oral versus cervico-facial lift approach for mandibular angle resection in facial feminization: A retrospective study. Journal of Stomatology, Oral and Maxillofacial Surgery, 123(2), 257-261. | 21 | Retrospective | Lower face |
| Perez, P. I., Hendershot, K., Teixeira, J. C., Hohman, M. H., Adidharma, L., Moody, M., ... & Nuara, M. J. (2023). Analysis of cephalometric points in male and female mandibles: an application to gender-affirming facial surgery. Journal of Craniofacial Surgery, 34(4), 1278-1282. | 113 | Retrospective | Lower face |
| Bellinga, R. J., Capitán, L., Simon, D., & Tenório, T. (2017). Technical and clinical considerations for facial feminization surgery with rhinoplasty and related procedures. JAMA facial plastic surgery, 19(3), 175-181. | 200 | retrospective | Whole face |
| Oles, N., Darrach, H., Landford, W., Garza, M., Twose, C., Park, C. S., ... & Coon, D. (2022). Gender affirming surgery: a comprehensive, systematic review of all peer-reviewed literature and methods of assessing patient-centered outcomes (part 1: breast/chest, face, and voice). Annals of surgery, 275(1), e52-e66. | 52 | Systematic review | Whole face |
| Hoffman, A. F., Laspro, M., Chinta, S., Tran, D. L., & Rodriguez, E. D. (2025). From Selfies to Surgery: Unveiling Trends and Ethical Considerations in Facial Feminization on Instagram. Journal of Craniofacial Surgery, 36(2), 397-401. | 500 | Retrospective | Any |
| La Padula, S., Hersant, B., Chatel, H., Aguilar, P., Bosc, R., Roccaro, G., ... & Meningaud, J. P. (2019). One-step facial feminization surgery: the importance of a custom-made preoperative planning and patient satisfaction assessment. Journal of Plastic, Reconstructive & Aesthetic Surgery, 72(10), 1694-1699. | 25 | Retrospective cohort | Face/neck |
| Gursky, A. K., Chinta, S. R., Wyatt, H. P., Belisario, M. N., Shah, A. R., Kantar, R. S., & Rodriguez, E. D. (2024). A comprehensive analysis of genioplasty in facial feminization surgery: a systematic review and institutional cohort study. Journal of Clinical Medicine, 14(1), 182. | 351 | Retrospective cohort, Review | Lower face |
| Spiegel, J. H. (2011). Facial determinants of female gender and feminizing forehead cranioplasty. The Laryngoscope, 121(2), 250-261. | 168 | Prospective visual perception, retrospective | Whole face |
| Li, K. R., Lava, C. X., Neughebauer, M. L. B., Hassan, B., Berger, L. E., Ford, A. D., ... & Del Corral, G. A. (2024). Surgical techniques and outcomes of thyroid chondroplasty in transfeminine individuals: A systematic review. Journal of Plastic, Reconstructive & Aesthetic Surgery, 91, 56-66. | 369 | Review | Lower face |
| Gunther, S., Carboy, J., Jedrzejewski, B., & Berli, J. (2024). Flattening the Curve and Cutting Corners—Pearls and Pitfalls Facial Gender Affirming Surgery. Craniomaxillofacial Trauma & Reconstruction, 17(2), 146-159. | Experiential narrative | Whole face | |
| Taylor, J. M., Nguyen, N. H., Huang, K. X., Pfaff, M. J., Ranganathan, K., Rada, R. C., ... & Lee, J. C. Patient-Reported Preoperative Depression as a Predictor of Psychosocial Outcomes After Gender-Affirming Facial Feminization Surgery. Annals of Surgery, 10-1097. | 127 | Prospective | Whole face |
| Ferrero, L., Atlan, M., & Cristofari, S. (2024). Sinocutaneous Fistula: A Long-term Complication After Surgical Feminization of the Forehead. Journal of Craniofacial Surgery, 35(6), e586-e588. | 1 | Case study | Upper face |
| Uranbey, O., Kaygisiz, O. F., Ayrancı, F., & Yanik, S. (2024). Exploring the evolution of facial feminization and masculinization surgery: a bibliometric analysis and visualization study. Maxillofacial Plastic and Reconstructive Surgery, 46(1), 19. | 0 | Review | |
| Raner, G. A., Jaszkul, K. M., Bonapace-Potvin, M., Al-Ghanim, K., Bouhadana, G., Roy, A. A., & Bensimon, É. (2024). Quality of life outcomes in patients undergoing facial gender affirming surgery: A systematic review and meta-analysis. International Journal of Transgender Health, 25(4), 653-662. | 1837 | Review | Whole face |
| Bachelet, J. T., Souchere, B., Mojallal, A., Gleizal, A., & Boucher, F. (2016, August). Facial feminization surgery-upper third. In Annales de Chirurgie Plastique et Esthetique (Vol. 61, No. 6, pp. 877-881). | 12 | Case series | Upper face |
| Alper, D. P., Almeida, M. N., Hosseini, H., De Baun, H. M., Moscarelli, J., Hu, K. G., ... & Alperovich, M. (2024). Perceived age and gender perception using facial recognition software following facial feminization surgery. Journal of Craniofacial Surgery, 35(1), 39-42. | 27 | Prospective | Whole face |
| Lundgren, T. K., & Farnebo, F. (2017). Midface osteotomies for feminization of the facial skeleton. Plastic and Reconstructive Surgery–Global Open, 5(1), e1210. | 6 | Prospective | Upper/middle face |
| Wolfort, F. G., Dejerine, E. S., Ramos, D. J., & Parry, R. G. (1990). Chondrolaryngoplasty for appearance. Plastic and Reconstructive Surgery, 86(3), 464-469. | 31 | Retrospective | Lower face |
| Strickland, L., Sussman, K. A., & Madden, L. L. (2025). Vocal quality complication following chondrolaryngoplasty: a reported case. Journal of Voice, 39(3), 856-e9. | 1 | Case study | Lower face |
| Lee, A., Piraquive, J., & Spiegel, J. H. (2022). Frontal bone cranioplasty for facial feminization in gender-affirming surgery: can fewer screws fixate bone and avoid nonunion?. Facial Plastic Surgery & Aesthetic Medicine, 24(S2), S-33. | 483 | Retrospective | Upper face |
| Kotha, V. S., Kanuri, A., Mandelbaum, M., Lakhiani, C., Hung, R. W., Wang, J., ... & Chao, J. W. (2022). Simultaneous Zygomatic Osteotomies With Reduction Mandibuloplasty–An Approach to Mid-and Lower-Facial Feminization in the Transfeminine Patient. Journal of Craniofacial Surgery, 33(5), 1569-1573. | 17 | Retrospective | Middle/lower face |
| Bedar, M., Dejam, D., Caprini, R. M., Huang, K. X., Cronin, B. J., Khetpal, S., ... & Lee, J. C. (2023). An enhanced recovery after surgery protocol for facial feminization surgery reduces perioperative opioid usage, pain, and hospital stay. Journal of Plastic, Reconstructive & Aesthetic Surgery, 85, 393-400. | 79 | Retrospective | Whole face |
| Raffaini, M., Magri, A. S., & Agostini, T. (2016). Full facial feminization surgery: patient satisfaction assessment based on 180 procedures involving 33 consecutive patients. Plastic and reconstructive surgery, 137(2), 438-448. | 33 | Retrospective | Whole face |
| Chaya, B. F., Laspro, M., Trilles, J., Brydges, H., Tran, D., Rochlin, D. H., ... & Rodriguez, E. D. (2024). Technical Pearls and Pitfalls of Facial Feminization Surgery: A Review of Techniques from a Single Institutional Practice. Annals of Plastic Surgery, 93(2), 208-214. | 231 | Retrospective | Whole face |
| Porcheray, M., Bachelet, J. T., Brosset, S., Daurade, M., Mojallal, A., & Boucher, F. (2020). Mandibular angle resection using cervicofacial lifting surgical approach. Journal of Stomatology, Oral and Maxillofacial Surgery, 121(4), 434-438. | 3 | Retrospective | Middle/lower face |
| Ihnat, J. M., Hu, K. G., Parikh, N., Almeida, M. N., Williams, M., Hauc, S. C., & Alperovich, M. (2025). Quantification of cephalometric changes in gonial angle morphology following facial feminization surgery. Journal of Craniofacial Surgery, 36(2), 743-746. | 13 | Cohort | Lower face |
| de Almeida, R. B., Costa, C. C., Ramos, H. V., e Silva Duarte, P. L., Velasco, L. C., & Cervantes, O. (2025). Surgical techniques in chondrolaryngoplasty: a narrative review. Sexual Medicine Reviews, 13(2), 237-245. | 366 | Literature review | Neck |
| Schmidt, M., Ramelli, E., Atlan, M., & Cristofari, S. (2023, January). Frontal sinus anatomical scanographic study of transgender patients for feminization frontoorbitoplasty surgery. In Annales de Chirurgie Plastique et Esthetique (Vol. 68, No. 2, pp. 93-98). | prospective | ||
| David, A. P., House, A. E., Targ, S., Park, A. M., Seth, R., & Knott, P. D. (2024). Objective outcomes of trichophytic brow lift and hairline advancement in facial feminization surgery. Facial Plastic Surgery & Aesthetic Medicine, 26(6), e807-e812. | 46 | Retrospective | Upper face |
| Pokrowiecki, R., Šufliarsky, B., & Jagielak, M. (2024). Esthetic surgery of the chin in cis-and transgender patients—application of T-genioplasty vs. single-piece segment lateralization. Medicina, 60(1), 139. | 31 | Retrospective | Lower face |
| van Rossem, A. P., Meijer, B. A., & Rinkel, R. N. (2021). Recommended maximum laryngeal prominence size in adult females: a cross-sectional study proposing a laryngeal prominence size standard for chondrolaryngoplasty in male-to-female transgender individuals. Plastic and reconstructive surgery, 147(4), 935-945. | 90 | crosssectional | Neck |
| Chaya, B. F., Colon, R. R., Diep, G. K., Brydges, H., Tran, D., Laspro, M., ... & Rodriguez, E. D. (2023). Comparative outcomes of malar implants versus fat transfer to cheeks among transfeminine individuals undergoing malar augmentation. Annals of Plastic Surgery, 90(6S), S457-S461. | 231 | retrospective | Middle face |
| Parikh, N., Hu, K. G., Ihnat, J. M., Allam, O., Diatta, F., Rancu, A. L., ... & Alperovich, M. (2025). The Most Socially Vulnerable Patients Benefit the Most Following Gender Affirming Facial Surgery. Journal of Craniofacial Surgery, 36(2), 772-776. | 20 | prospective survey | Whole face |
| Ives, G. C., Martin, A., Munabi, N. C., Lee, J. C., Ames, J. A., Chu, M. W., ... & Francis, S. H. (2025). Temporal rotation flaps for gender-affirming hairline feminization: Taking the “M” shape out of masculine hairlines. Journal of Plastic, Reconstructive & Aesthetic Surgery, 102, 404-411. | 86 | Cohort | Upper/middle face |
| Salgado, C. J., AlQattan, H., Nugent, A., Gerth, D., Kassira, W., McGee, C. S., & Wo, L. (2018). Feminizing the face: combination of frontal bone reduction and reduction rhinoplasty. Case Reports in Surgery, 2018(1), 1947807. | 0 | Retrospective | Upper/middle face |
| Younis, H., Zhou, Z., Sun, X., Ge, H., Wang, Y., & Li, J. (2025). Middle and lower-facial feminization surgery in East Asian transgender and cisgender women: Surgical techniques and outcomes. Journal of Plastic, Reconstructive & Aesthetic Surgery, 104, 215-224. | 73 | Retrospective | Middle/lower face |
| Li, A. Y., Park, M. J., Fick, J., Ousterhout, D. K., & Deschamps-Braly, J. C. (2024). Perioperative estrogen hormonal therapy does not increase venous thromboembolism risk in facial feminization surgery. Plastic and Reconstructive Surgery, 154(6), 1309-1315. | 1715 | Retrospective | Whole face |
| Deschamps-Braly, J. C., Sacher, C. L., Fick, J., & Ousterhout, D. K. (2017). First female-to-male facial confirmation surgery with description of a new procedure for masculinization of the thyroid cartilage (Adam’s apple). Plastic and reconstructive surgery, 139(4), 883e-887e. | 1 | Case | Whole face |
| Stevenson, L. A., Song, P. C., Franco, R. A., & Naunheim, M. R. (2025). Instrumentation Considerations for Calcified Thyroid Cartilage during Chondrolaryngoplasty. The Laryngoscope, 135(2), 748-751. | 52 | Retrospective | Neck |
| Garcia-Rodriguez, L., Thain, L. M., & Spiegel, J. H. (2020). Scalp advancement for transgender women: closing the gap. The Laryngoscope, 130(6), 1431-1435. | 29 | Retrospective | Upper face |
| Mahmoud, R., Arbel, S., Shuster, A., Ianculovici, C., Peleg, O., & Kleinman, S. (2023). Intraoperative blood loss and the need for preoperative blood preparations in transgender women undergoing facial feminization surgeries: implications for surgeons. International Journal of Oral and Maxillofacial Surgery, 52(1), 72-78. | 20 | Retrospective | Whole face |
| Becking, A. G., Tuinzing, D. B., Hage, J. J., & Gooren, L. J. (1996). Facial corrections in male to female transsexuals: a preliminary report on 16 patients. Journal of Oral and Maxillofacial Surgery, 54(4), 413-418. | 16 | Retrospective case series | Middle/lower face |
| Nguyen, N. H., Taylor, J. M., Huang, K. X., Shariati, K., Chevalier, J. M., Miller, M. N., ... & Lee, J. C. (2024). Ethnic variation in lower face anthropometry on facial computed tomography scans for patients seeking facial feminization surgery. Journal of Plastic, Reconstructive & Aesthetic Surgery, 93, 222-231. | 204 | Retrospective | Whole face |
| Kaur, M. N., Morrison, S. D., Kennedy, S. L., van de Grift, T. C., Højgaard, A., Jacobsen, A. L., ... & Klassen, A. F. (2024). International study to develop a patient-reported outcome measure to evaluate outcomes of gender-affirming care-the GENDER-Q. Journal of patient-reported outcomes, 8(1), 134. | 601 | Instrument development study | Whole body |
| Kass, N. M., Cheng, L. G., Irgebay, Z., Moroni, E., Dvoracek, L., Canton, S. P., ... & Goldstein, J. A. (2024). Mixed Reality in the Operating Room: An Initial Use in Frontal Sinus Setback in Gender-affirming Facial Surgery. Plastic and Reconstructive Surgery–Global Open, 12(6), e5896. | 1 | Case reports/proof of concept | Upper face |
| Di Maggio, M. R., Anchorena, J. N., & Dobarro, J. C. (2019). Surgical management of the nose in relation with the fronto-orbital area to change and feminize the eyes’ expression. Journal of Craniofacial Surgery, 30(5), 1376-1379. | Case series | Whole face | |
| Nouraei, S. R., Randhawa, P., Andrews, P. J., & Saleh, H. A. (2007). The role of nasal feminization rhinoplasty in male-to-female gender reassignment. Archives of facial plastic surgery. | 12 | Retrospective case series | Middle face |
| Oestriecher-Kedem, Y., Neiderman, N. N. C., Levenberg, G., Lior, Y., Kidron, A., Ianculovici, C., ... & Arbel, S. (2024). Outcome of isolated and combined direct feminization laryngochondroplasty: Our first 20 cases. Journal of Cranio-Maxillofacial Surgery, 52(11), 1206-1210. | 20 | retrospective | Neck |
| Kannan, A., Chakranarayan, A., Pisharody, R. R., Kumari, P., Gadad, R., & Nagori, S. A. (2022). Atypical Orthognathic Surgical Protocol for Facial Feminisation as an Adjunct to Gender Affirmation Therapy: a Case Report. Journal of Maxillofacial and Oral Surgery, 21(4), 1296-1303. | 1 | Case study | Lower face |
| Paltura, C., & Yelken, K. (2019). An examination of vocal tract acoustics following Wendler’s glottoplasty. Folia Phoniatrica et Logopaedica, 71(1), 24-28. | 40 | ||
| Sanz, D., Ângelo, D. F., Marques, R., Maffia, F., & Cardoso, H. J. (2024). F-Chin/feminizing the chin: A genioplasty technique with virtual planning for male-to-female transgender patients. Aesthetic Plastic Surgery, 48(10), 1899-1905. | 3 | Technique discussion | Lower face |
| Villepelet, A., Jafari, A., & Baujat, B. (2018). Fronto-orbital feminization technique. A surgical strategy using fronto-orbital burring with or without eggshell technique to optimize the risk/benefit ratio. European Annals of Otorhinolaryngology, Head and Neck Diseases, 135(5), 353-356. | 8 | Retrospective | Upper face |
| Natghian, H., Farnebo, F., & Lundgren, K. C. (2019). Management of the midface in the transgender patient. Journal of Craniofacial Surgery, 30(5), 1383-1386. | 9 | Commentary | Whole face |
| Ainsworth, T. A., & Spiegel, J. H. (2010). Quality of life of individuals with and without facial feminization surgery or gender reassignment surgery. Quality of Life Research, 19(7), 1019-1024. | 100 | Cross- sectional study | Whole face |
| Lam, K., Ho, T., & Yao, W. C. (2017). Sinocutaneous fistula formation after forehead recontouring surgery for transgender patients. Journal of Craniofacial Surgery, 28(3), e274-e277. | 1 | Case study | Upper face |
| Gutiérrez-Santamaría, J., Simon, D., Capitán, L., Bailón, C., Bellinga, R. J., Tenório, T., ... & Capitán-Cañadas, F. (2024). Shaping the lower jaw border with customized cutting guides: development, validation, and application in facial gender-affirming surgery. Facial Plastic Surgery & Aesthetic Medicine, 26(6), e818-e824. | 260 | Prospective case series | Lower face |
| Mundinger, G. S. (2025). Facial Augmentation in Transmasculine and Transfeminine Patients: Customization of Facial Implants and Increase in Facial Masculinization Surgery. Journal of Craniofacial Surgery, 36(2), 756-760. | 212 | Retrospective | Middle face |
| Pokrowiecki, R. (2025). Novel Plating System Designed Specifically for Chin Narrowing Surgery. Journal of Craniofacial Surgery, 36(2), 700-701. | - | Surgical feasibility | Lower face |
| Hohman, M. H., Jastrzembski, M. E., Choe, N., Nuara, M. J., Teixeira, J. C., & Vincent, A. G. (2021). 3D-printed custom cutting guides facilitate frontal cranioplasty in gender affirmation surgery. Journal of Craniofacial Surgery, 32(7), e668-e670. | 5 | Case series | Upper face |
| Gupta, N., Wulu, J., & Spiegel, J. H. (2019). Safety of combined facial plastic procedures affecting multiple planes in a single setting in facial feminization for transgender patients. Aesthetic Plastic Surgery, 43(4), 993-999. | 25 | Retrospective | Whole face |
| Dempf, R., & Eckert, A. W. (2010). Contouring the forehead and rhinoplasty in the feminization of the face in male-to-female transsexuals. Journal of Cranio-Maxillofacial Surgery, 38(6), 416-422. | 1 | Case | Upper/middle face |
| Brown, A. E., Shrout, M. A., & Howard, B. E. (2024). Frontal Osteomyelitis and Sinusitis Complication After Type III Frontal Bone Cranioplasty for Facial Feminization. Facial Plastic Surgery & Aesthetic Medicine, 26(1), 79-82. | 1 | Case | Upper face |
| Laspro, M., Hoffman, A., Chinta, S., Abdalla, J., Tran, D., Oh, C., ... & Rodriguez, E. D. (2025). The Effects of Perioperative Gender-affirming Hormone Therapy on Facial Feminization Surgery Adverse Events, Facial Features Addressed, and Esthetic Satisfaction: A Multimodal Analysis. Journal of Craniofacial Surgery, 36(2), 600-604. | 1582 | Review | Whole face |
| Soledade, V. S., Sena, L. S., & Patrocínio, L. G. (2024). Validation of the Brazilian Portuguese language version of the facial feminization surgery outcomes evaluation the Brazilian Portuguese language version of the FFSOE. Brazilian Journal of Otorhinolaryngology, 90(6), 101483. | 21 | Validation | |
| Hage, J. J., Vossen, M., & Becking, A. G. (1997). Rhinoplasty as part of gender-confirming surgery in male transsexuals: basic considerations and clinical experience. Annals of plastic surgery, 39(3), 266-271. | 22 | Mid face | |
| Nguyen, N. H., Doan, L., Chu, M. W., Francis, S. H., Liu, Y., & Lee, J. C. (2024). The evolution of a large-scale facial gender affirmation program: A comparative outcomes analysis. Journal of Plastic, Reconstructive & Aesthetic Surgery, 99, 416-419. | 191 | Retrospective | Whole face |
| Nguyen, N., Lee, J., & Liu, Y. (2024). A Case Report of Craniofacial Intraosseous Xanthoma in a Patient Seeking Facial Feminization Surgery. Annals of Plastic Surgery, 92(5), 537-539. | 1 | Case report | Whole face |
| Cho, S. W., & Jin, H. R. (2012). Feminization of the forehead in a transgender: frontal sinus reshaping combined with brow lift and hairline lowering. Aesthetic plastic surgery, 36(5), 1207-1210. | 1 | Case report | Upper face |
| Spiegel, J. H. (2008). Challenges in care of the transgender patient seeking facial feminization surgery. Facial Plastic Surgery Clinics of North America, 16(2), 233-238. | 3 | Discussion | Whole face |
| Bhethanabotla, R. M., Callander, J. K., Wulu, J. A., & Knott, P. D. (2025). Minimally invasive sternocleidomastoid muscle thinning for cervical feminization. Facial Plastic Surgery & Aesthetic Medicine, 27(1), 91-97. | 1 | Surgical feasibilty | Neck |
| Palamenghi, A., Franceschetti, L., Tambuzzi, S., D’Apuzzo, A., Mazzarelli, D., & Cattaneo, C. (2024). Transcending time: the forensic anthropological case study of three unidentified transgender women in Italy in the early 1990s. International journal of legal medicine, 138(3), 1079-1084. | 3 | Retrospective | Mid face |
| Nesiba, J. R., Caplin, C., & Nuveen, E. J. (2019). A contemporary and novel use of thyroid cartilage for structural grafting in esthetic rhinoplasty: a case report. Journal of Oral and Maxillofacial Surgery, 77(3), 639-e1. | 1 | Case report | Mid face |
References
- Caprini, R.M.; Oberoi, M.K.; Dejam, D.; et al. Effect of Gender-Affirming Facial Feminization Surgery on Psychosocial Outcomes. Ann. Surg. 2023, 277, e1184–e1190. [Google Scholar] [CrossRef]
- Bedar, M.; Dejam, D.; Caprini, R.M.; et al. An Enhanced Recovery After Surgery Protocol for Facial Feminization Surgery Reduces Perioperative Opioid Usage, Pain, and Hospital Stay. J. Plast. Reconstr. Aesthet. Surg. 2023, 85, 393–400. [Google Scholar] [CrossRef]
- Taylor, J.M.; Nguyen, N.; Huang, K.X.; et al. Patient-Reported Preoperative Depression as a Predictor of Psychosocial Outcomes After Gender-Affirming Facial Feminization Surgery. Ann. Surg. 2024. [Google Scholar] [CrossRef] [PubMed]
- Chin, M.G.; LaGuardia, J.S.; Ngo, H.; et al. United States Health Policies on Gender-Affirming Care in 2022. Plast. Reconstr. Surg. 2024, 153, 462e–473e. [Google Scholar] [CrossRef] [PubMed]
- LaGuardia, J.S.; Chin, M.G.; Fadich, S.; et al. Medicaid Coverage for Gender-Affirming Surgery for Transgender Patients: A State-by-State Review. Health Serv. Res. 2024. [Google Scholar] [CrossRef]
- Hu, A.C.; Dang, B.N.; Bertrand, A.A.; Jain, N.S.; Chan, C.H.; Lee, J.C. Facial Feminization Surgery Under Insurance: The UCLA Experience. Plast. Reconstr. Surg. Glob. Open. 2021, 9, e3572. [Google Scholar] [CrossRef]
- Ousterhout, D.K. Facial Feminization Surgery: The Forehead. Surgical Techniques and Analysis of Results. Plast. Reconstr. Surg. 2015, 136, 560e–561e. [Google Scholar] [CrossRef]
- Ousterhout, D.K. Feminization of the Forehead: Contour Changing to Improve Female Aesthetics. Plast. Reconstr. Surg. 1987, 79, 701–713. [Google Scholar] [CrossRef] [PubMed]
- Dang, B.N.; Hu, A.C.; Bertrand, A.A.; et al. Evaluation and Treatment of Facial Feminization Surgery: Part I. Forehead, Orbits, Eyebrows, Eyes, and Nose. Arch. Plast. Surg. 2021, 48, 503–510. [Google Scholar] [CrossRef]
- Moghadam, S.; Shariati, K.; Huang, K.X.; et al. The Type 1+ Forehead: A Novel Method to Forehead Reconstruction in Facial Feminization Surgery. Aesthet. Plast. Surg in press. 2024. [Google Scholar] [CrossRef]
- Khetpal, S.; Dejam, D.; Baker, N.F.; Morgan, K.B.J.; Lee, J.C. Feminizing Rhinoplasty: A Review of Techniques and Outcomes. Face 2023, 4, 198–206. [Google Scholar] [CrossRef]
- Nguyen, N.H.; Taylor, J.M.; Huang, K.X.; et al. Ethnic Variation in Lower Face Anthropometry on Facial CT Scans for Patients Seeking Facial Feminization Surgery. J. Plast. Reconstr. Aesthet. Surg. 2024, 93, 222–231. [Google Scholar] [CrossRef] [PubMed]
- Khetpal, S.; Baker, N.F.; Hu, V.; et al. Feminizing Genioplasty: A Review of Techniques and Outcomes. Face 2023, 4, 207–217. [Google Scholar] [CrossRef]
- Ousterhout, D.K. Facial Feminization Surgery: A Guide for the Transgendered Woman; Addicus Books: Omaha, NE, USA, 2010. [Google Scholar]
- Moghadam, S.; Roca, Y.; LaGuardia, J.S.; et al. Effect of Duration of Feminizing Hormone Therapy on Facial Fat Volumes. Plast. Reconstr. Surg. 2024, 154, 1081–1088. [Google Scholar] [CrossRef]
- Deschamps-Braly, J.C. Approach to Feminization Surgery and Facial Masculinization Surgery: Aesthetic Goals and Principles of Management. J. Craniofac. Surg. 2019, 30, 1352–1358. [Google Scholar] [CrossRef]
- Moghadam, S.; LaGuardia, J.S.; Chin, M.G.; et al. Virtual Modeling in Gender-Affirming Facial Masculinization Surgery. Plast. Reconstr. Surg. 2024, 154, 1229e–1232e. [Google Scholar] [CrossRef]
- Dang, B.N.; Hu, A.C.; Bertrand, A.A.; et al. Evaluation and Treatment of Facial Feminization Surgery: Part II. Arch. Plast. Surg. 2022, 49, 5–11. [Google Scholar] [CrossRef] [PubMed]
- Hoang, H.; Bertrand, A.A.; Hu, A.C.; Lee, J.C. Simplifying Facial Feminization Surgery Using Virtual Modeling on the Female Skull. Plast. Reconstr. Surg. Glob. Open. 2020, 8, e3268. [Google Scholar] [CrossRef]
- Cronin, B.J.; Lee, J.C. Preoperative Radiology and Virtual Surgical Planning. Oral Maxillofac. Surg. Clin. N. Am. 2024, 36, 171–182. [Google Scholar] [CrossRef]
- Miroshnychenko, A.; Rae, C.; Wong Riff, K.; et al. Psychometric Validation of the CLEFT-Q Patient Reported Outcome Measure. Cleft Palate Craniofac. J. 2023, 60, 327–335. [Google Scholar] [CrossRef]
- Thoma, A.; Sprague, S.; Veltri, K.; Duku, E.; Furlong, W. Methodology and Measurement Properties of Health-Related Quality of Life Instruments in Breast Reduction Surgery. Health Qual. Life Outcomes 2005, 3, 44. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; et al. The PRISMA 2020 Statement. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Hall, A.E.; Nguyen, N.H.; Cascavita, C.T.; et al. The Impact of Psychological Prehabilitation on Surgical Outcomes: A Meta-Analysis and Meta-Regression. Ann. Surg. in press. 2025. [Google Scholar] [CrossRef] [PubMed]
- Hall, A.E.; Perrotta, A.T.; Argame, A.A.; et al. Mind Over Scalpel: Effectiveness of Preoperative Surgical Education. J. Am. Coll. Surg in press. 2025. [Google Scholar] [CrossRef]
- Hall, A.E.; Perrotta, A.T.; Shariati, K.; Patel, A.K.; Lee, J.C. Artificial Intelligence Chatbots in Surgical Care: A Systematic Review of Clinical Applications. J. Artif. Intell. Med. Sci. in press. 2025. [Google Scholar] [CrossRef]
- Williamson, P.R.; Altman, D.G.; Blazeby, J.M.; et al. Developing Core Outcome Sets for Clinical Trials: Issues to Consider. Trials 2012, 13, 132. [Google Scholar] [CrossRef] [PubMed]
- Barnett, S.L.; Miller, M.N.; Appel, J.M.; et al. Ethical Issues Surrounding Facial Feminization Surgery: Five Major Considerations. Aesthet. Surg. J. 2024, 44, 347–353. [Google Scholar] [CrossRef] [PubMed]
- Roijer, P.J.; Vallinga, M.S.; Pidgeon, T.E.; et al. The GENDER-COS Project: Study Protocol for the Development of Two International Core Outcome Sets for Genital Gender-Affirming Surgery. Int. J. Transgend. Health 2025, 26, 78–87. [Google Scholar] [CrossRef]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





