Evidence before this study
Earlier Malaysian studies reported a mean age at menopause of around 50 years and documented high symptom prevalence with notable ethnic and regional differences. Most women relied on traditional remedies, with very low uptake of hormone replacement therapy (HRT). However, previous research was largely descriptive, focusing on symptoms or perceptions without examining structural determinants or applying advanced epidemiological methods.
Added value of this study
This study is the first to integrate biological, sociocultural, and health system factors to classify natural, medical, and surgical menopause using robust, intersectional modelling. It identifies marked ethnic and urban–rural disparities, showing surgical menopause to be disproportionately common among Bumiputera Sarawak women and in urban areas. A novel burden index highlights cumulative disadvantage, while harmonised metrics allow direct comparison with other countries.
Implications of all the available evidence
Menopause timing in Malaysia aligns with global averages, but care pathways and treatment access are inequitable. High surgical rates and low HRT uptake reflect systemic gaps in care and reliance on traditional practices. Addressing these issues requires reducing unnecessary surgeries, improving access to evidence-based treatments, and integrating menopause into broader women’s health and ageing policies. |
Background
Menopause represents a major transition in a woman’s reproductive life course, typically occurring between the ages of 45 and 55, and is defined by the permanent cessation of menstruation following twelve consecutive months without a menstrual period [
1]. This transition is preceded by the perimenopausal stage, characterised by irregular cycles and fluctuating hormone levels, and followed by the post-menopausal stage, when ovarian activity has ceased completely [
2,
3]. In Malaysia, where the female population aged 45 and above is steadily increasing due to demographic shifts and improvements in life expectancy, menopause has become an important yet under-recognised public health issue [
4]. This variation has profound implications for women’s health, given the associated changes in bone density, cardiovascular risk, and metabolic health that accompany ovarian ageing. Despite these physiological realities, menopause remains poorly integrated into mainstream healthcare planning and policy in Malaysia. Many women enter the transition with limited information, inconsistent clinical support, and significant disparities in access to care. Understanding the experiences of perimenopausal, menopausal, and post-menopausal women in Malaysia is therefore critical to improving health outcomes, supporting women’s quality of life, and planning services that reflect the needs of an ageing population.
Malaysia’s diverse cultural landscape adds complexity to how menopause is understood, experienced, and managed [
5]. The country is home to multiple ethnic groups, including Malay, Chinese, Indian, and various Indigenous communities such as the Bumiputera Sarawak, each with distinct cultural beliefs and health practices [
6]. These cultural frameworks shape women’s perceptions of menopause, influencing whether symptoms are considered a natural part of ageing, a health problem requiring treatment, or a private matter to be endured silently. In many communities, discussing reproductive ageing remains taboo, limiting open conversations about symptoms and treatment options both within families and with healthcare providers [
7]. Traditional medicine continues to play an important role in Malaysian society, with herbal remedies and alternative practices frequently used to manage menopausal symptoms [
8]. While these approaches are culturally embedded and often accessible, they may delay engagement with biomedical services or be used as substitutes when hormone replacement therapy (HRT) or other evidence-based treatments are unavailable or unaffordable [
9,
10]. Furthermore, differences in healthcare access between urban and rural areas, alongside socio-economic disparities, create additional barriers to timely and effective care. For instance, women in rural settings may have limited access to specialist gynaecological services, while urban women may face fragmented or overly medicalised care pathways, including higher rates of surgical intervention for gynaecological conditions [
11,
12]. Understanding these cultural and systemic dynamics is essential to developing interventions that are both clinically effective and culturally sensitive.
Rationale
Despite growing recognition of the importance of menopause as a public health concern, there is limited empirical research describing the patterns and determinants of menopause in Malaysia. Most available data focus on symptom prevalence or small-scale clinical observations, leaving critical gaps in understanding how biological, cultural, and health system factors interact to shape women’s experiences and outcomes. Surgical menopause, for example, remains common in Malaysia, but the underlying drivers—whether related to clinical decision-making, availability of conservative treatments, or patient preferences are poorly understood. Similarly, little is known about the accessibility and acceptability of HRT, which remains a highly effective treatment for managing menopausal symptoms yet is under-utilised in many parts of the country. By integrating detailed demographic, clinical, and sociocultural data, this study provides a comprehensive examination of menopause in Malaysia, identifying patterns of natural, medical, and surgical menopause across different ethnic groups and geographical contexts. The inclusion of intersectional modelling allows for the exploration of how factors such as ethnicity, education, employment, and place of residence interact to produce health inequities. Understanding these dynamics is vital for guiding health policy, improving service delivery, and reducing disparities in care. Furthermore, harmonising these data with findings from other MARIE study sites offers a unique opportunity to place Malaysia within a global context, enabling cross-country comparisons and shared learning. This study therefore addresses an urgent need for high-quality evidence to inform culturally relevant, equitable, and evidence-based approaches to menopause care in Malaysia.
Methods
Study Design and Setting
We conducted a cross-sectional analysis using baseline data from the Malaysian arm of the Menopause and Ageing Research in International Environments (MARIE) study. Data were extracted from the “Baseline” survey dataset. The study population included respondents residing in Malaysia at the time of participation.
Participants
Participants were eligible for inclusion if they provided information on at least one key menopausal variable: menopausal stage, age at menopause, or menopause type. There were no exclusions based on comorbidities or treatment history.
Classification of Menopause Type
Menopause type was first taken from the participant’s direct response (“natural” vs “due to a health condition”). If this was missing/unclear, we applied standardised rules:
Medical menopause: current or previous use of gonadotropin-releasing hormone (GnRH) analogues or a diagnosis of premature ovarian insufficiency (POI).
Surgical menopause: self-report of hysterectomy with oophorectomy when available; when oophorectomy status was not reported, hysterectomy alone was provisionally classified as surgical with a planned sensitivity analysis (see Data analysis) because ovarian function may be retained after uterine removal.
For equity/subgroup analyses, menopause type was collapsed into three mutually exclusive categories: natural, medical, and surgical.
Variables
Demographic variables: age (years), self-reported race/ethnicity, place of residence (free-text, later mapped to urban/non-urban). Menopause-related variables include menopausal stage, self-reported age at menopause, hysterectomy ± oophorectomy, GnRH analogue use, POI diagnosis, current hormone replacement therapy (HRT) use, and current traditional-remedy use (for menopause or general health).
Data Cleaning and Quality Assurance
Pre-specified data cleaning rules were applied to ensure plausibility and minimise errors. Reported age values were retained only if they fell between 18 and 99 years inclusive (18 ≤ age ≤ 99). Age at menopause values were retained if they were between 20 and 65 years inclusive (20 ≤ age at menopause ≤ 65)(20 ≤ age at menopause ≤ 65). Where both current age and age at menopause were reported, age at menopause could not exceed current age, and inconsistent entries were set to missing. All analyses were performed using a complete-case approach with no imputation of missing data. To maintain confidentiality and ensure statistical stability, group-level prevalence estimates were reported only for subgroups containing at least five individuals (n ≥ 5).
Data Analysis
Continuous variables were summarised using descriptive statistics, including means, standard deviations (SD), medians, and ranges. Categorical variables were described as counts and proportions, accompanied by Wilson 95% confidence intervals (CIs) to provide more reliable estimates, particularly for smaller sample sizes. For subgroup analyses examining the distribution of menopause type by race, ethnicity, and place of residence, any groups with fewer than five participants were excluded from range calculations to avoid unstable estimates.
All data management and analyses used Python 3.11 with pandas and SciPy; model fitting used stats models. Final analytic datasets and outputs were exported into Excel files to facilitate transparency, reproducibility, and verification of findings.
Data Preparation and Inclusion
We used the Visit-1 dataset for Malaysia (n=632) and acknowledged 462 Visit-2 completions per the study records. Age values were retained if 18≤ age ≤99. Analyses were performed on a complete-case basis for each outcome; no imputation was undertaken.
Classification of Menopause
Where participants directly indicated type, responses were recorded as “natural” or “due to a health condition”. If this item was missing or ambiguous, we applied rules: “medical menopause” was assigned if the participant reported POI or GnRH analogue exposure; “surgical menopause” was assigned if the participant reported hysterectomy (noting that ovarian function may be retained). For inequality analyses we used the collapsed three-level type: Natural / Medical / Surgical.
Descriptive Statistics
Descriptive statistics for continuous variable
X we computed the sample size
n, mean
Standard deviation, median and range as;
For proportion with
k events out of
n observations, we reported percentages with Wilson 95% confidence intervals, which have good coverage even for small
n. Let
For a 95% interval where the Wilson centre and half width are
For inequality summaries, we reported the absolute range of prevalence across groups with atleast 5 women in the denominator;
Inequality metrics, for each category within a stratify, we compute the absolute range across eligible groups;
Small-sample robustness (Bayesian add-on), where yes/no outcomes were reported, we used Jeffreys posterior with a Beta (1/2, ½) prior. For k events in
n;
Multivariable Modelling
The outcome is nominal with three categories, we modelled two logistic regressions with natural as the common references one-vs-reference logistic regressions: Medical vs Natural and Surgical vs Natural. This is numerically equivalent to a multinomial analysis when the contrasts are interpreted relative to the same reference. For individual ii with covariate vector xixi, the logistic model is
so that the odds ratio (OR) for a one-unit increase in a continuous predictor is exp(βj)exp(βj), and for a categorical predictor it is the ratio of odds between the category and its reference. We standardised age before modelling, using the z-score
where μμ and σσ are the sample mean and standard deviation of age in the analytic subset. Categorical predictors were encoded with indicator variables; for ethnicity, Bhumiputra Sarawak served as the reference category (Chinese, Malay, and Other as indicators). Education was coded as Higher vs not, and employment as Employed vs not. Models were fit by maximum likelihood.
Intersectional and contextual modelling. To account for unobserved heterogeneity at the place-of-residence level (free-text locality), we estimated logistic generalised linear models with cluster-robust (sandwich) standard errors by residence. Let β^βbe the maximum-likelihood estimate, XX the design matrix, WW the diagonal weight matrix from the fitted model, and gg index clusters (residences). The sandwich variance estimator is;
where u^gug are the cluster wise score residuals. This produces wider, more honest confidence intervals when observations are correlated within localities. The intersectional specification included age (z-scored), ethnicity, education, employment, and an urban/non-urban indicator derived from locality text; odds ratios and 95% CIs were reported as;
Covariates
Age (z-scored), ethnicity (reference = largest group in the analytic subset; see model tables), education (Higher vs Not), employment (Employed vs Not), and residence (Urban vs Non-urban) derived from locality text. Categorical predictors were coded with indicator variables. To account for clustering by locality, we used cluster-robust (sandwich) standard errors with clusters defined by residence.
Comorbidity co-occurrence. For binary conditions AA and BB, we quantified pairwise clustering using the phi coefficient;
where nab are the cell counts of the 2×22×2 table, and n1⋅,n0⋅,n⋅1,n⋅0n1⋅,n0⋅,n⋅1,n⋅0 are the corresponding margins. We computed ϕϕ overall and within each menopause-type stratum to reveal whether specific pairs of conditions co-occur differentially by pathway.
Burden index of menopausal disadvantage. We constructed a cumulative index as the sum of three domain scores:
where the clinical domain added one point each for any reported long-term condition, POI, and surgical menopause; the treatment domain added one point for absence of current HRT and one for GnRH analogue exposure; and the sociocultural domain added one point for lower education, one for non-urban residence, and one for current traditional-remedy use. We summarised the total and domain scores by menopause type using n, xˉ, SD, median, [min,max]
Cross-country comparison metrics. To prepare like-for-like reporting across MARIE sites, we tabulated three harmonised indicators for Malaysia: mean age at menopause, prevalence of surgical menopause, and prevalence of current HRT use. The same definitions and cleaning rules will be applied to each comparator country to ensure comparability. Small-cell handling and stability. To avoid unstable estimates and protect confidentiality, we reported group-level prevalence only where the denominator was at least five; no range metrics were calculated for smaller strata. Confidence intervals for rare categories were computed using Wilson’s method to improve coverage at the limits of the distribution.
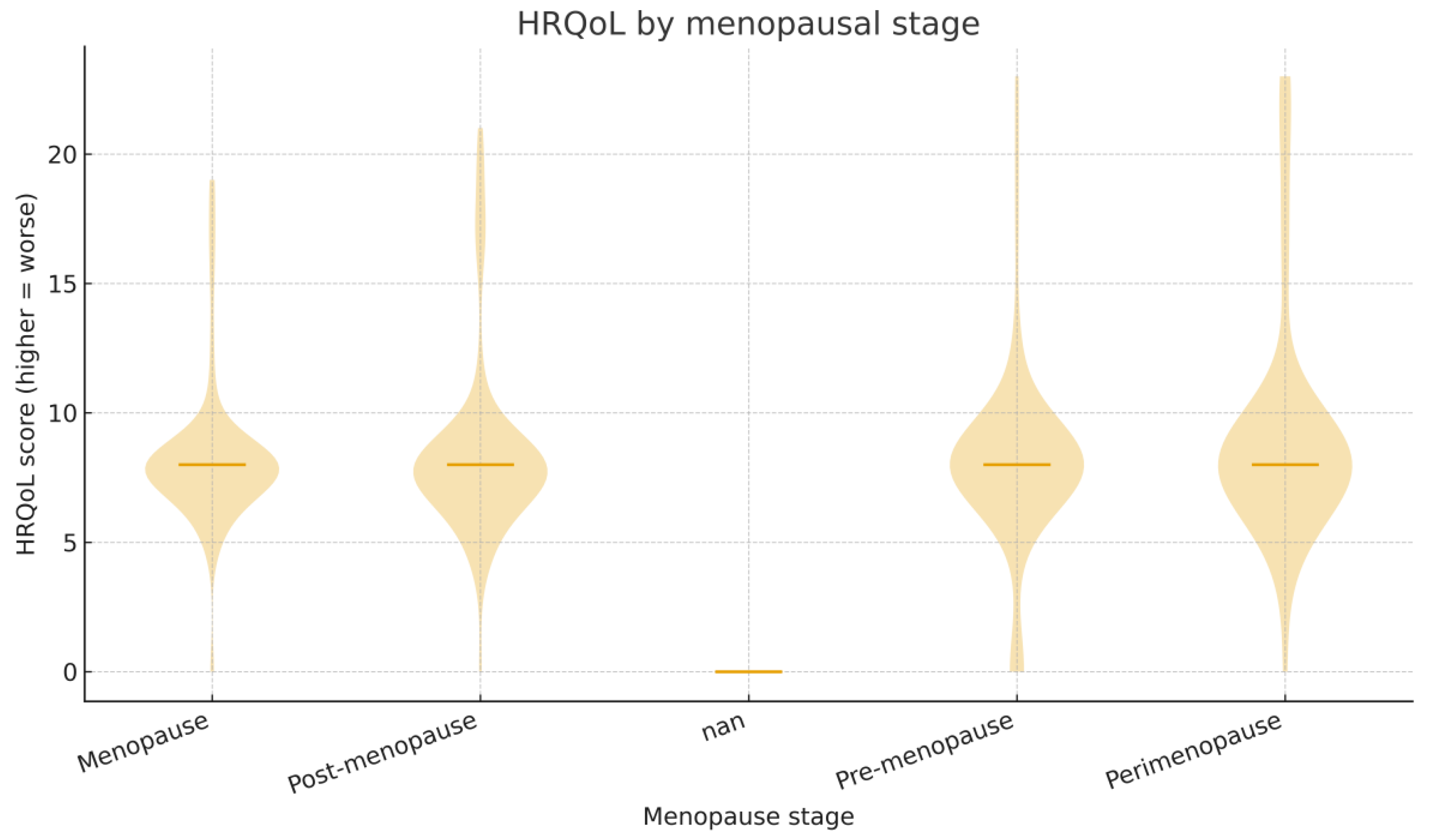
Health-related quality of life (HRQoL) was assessed using a composite score ranging from 0 to 23, where higher scores indicate greater impairment. Data cleaning and preparation were performed using Python (pandas, numpy) to ensure consistency across variables and to standardise categorical responses such as menopausal stage, menopause type, medication use, and endometriosis diagnosis.
Descriptive statistics were first generated to summarise HRQoL distribution, including the mean, median, interquartile range (IQR), and range of scores. Group-level summaries for menopausal stage, menopause type, medication use, and endometriosis diagnosis were calculated, reporting median (IQR), mean (SD), and minimum/maximum values.
Given the non-normal distribution of HRQoL scores, confirmed visually by histograms and violin plots, non-parametric statistical tests were used for group comparisons. For comparisons involving more than two groups, such as menopausal stage and menopause type, the Kruskal–Wallis test was applied to assess overall differences. For binary comparisons (e.g., medication use, endometriosis diagnosis), the Mann–Whitney U test was used.
Results
Participant Flow and Overall Cohort Characteristics
A total of 632 women completed the baseline (Visit-1) survey, representing the full Malaysian cohort recruited to the MARIE study. Follow-up data were available for 461 participants (72.9%), closely matching the 462 completions recorded in study logs, indicating minimal loss to follow-up. Analyses presented here focus on Visit-1 data.
Data quality checks were applied to ensure plausible and internally consistent values. Current age was retained for 486 women (76.9%) and age at menopause for 411 (65.0%). Implausible values outside predefined ranges (18–99 years for current age; 20–65 years for age at menopause) were excluded, and cases where age at menopause exceeded current age were set to missing. Among valid records, the mean current age was 56.7 years (SD 8.1, range 28–88), and the mean age at menopause was 50.1 years (SD 4.5, range 23–60). These distributions indicate a typical menopausal onset around 50 years, consistent with global norms, but with considerable individual variation that may reflect differences in genetics, health status, and sociocultural factors.
Menopausal Stage at Baseline
At the time of baseline assessment, most women were at or beyond the menopausal transition. Of the 632 women, 236 (37.3%) reported being in menopause and 164 (25.9%) reported post-menopause. Smaller numbers were pre-menopausal (65 women, 10.3%) or perimenopausal (49 women, 7.8%). This stage distribution provided a strong basis for examining both transition-related symptoms and longer-term post-menopausal outcomes while capturing a minority of women in earlier reproductive phases for prevention and early-intervention insights.
Classification of Menopause Type
Menopause type was determined for 275 women (43.5% of the full cohort) using direct self-report, supplemented by rule-based derivation from hysterectomy, premature ovarian insufficiency (POI), and gonadotrophin-releasing hormone (GnRH) analogue use. Natural menopause was most common, reported by 200 women (72.7%, Wilson 95% CI 67.2–77.7), while surgical menopause was reported by 44 women (16.0%, 12.1–20.8) and medical menopause by 31 women (11.3%, 8.1–15.6). Thus, almost one in four women had a non-natural pathway to menopause.
The relatively high proportion of surgical menopause indicates a significant reliance on operative interventions for gynaecological conditions such as fibroids, endometriosis, and abnormal uterine bleeding. This highlights potential differences in care pathways and the availability of conservative treatment options (
Figure 1).
Use of Hormone Replacement Therapy and Traditional Remedies
Among 498 women with complete data on treatment use, only 40 reported current hormone replacement therapy (HRT), corresponding to a prevalence of 8.0% (Wilson 95% CI 6.0–10.8). By contrast, 60 women (12.1%, 9.5–15.2) reported current use of traditional remedies such as herbal preparations or alternative therapies. The higher use of traditional remedies compared with HRT suggests a substitution effect, whereby women may rely on culturally familiar or more accessible approaches in the absence of affordable, acceptable biomedical options. These findings indicate a need for health system strategies that improve access to safe, evidence-based treatments while recognising the continuing role of traditional practices.
Multivariable and Intersectional Modelling
Two one-vs-reference logistic models were fitted to examine predictors of menopause type. In the Medical vs Natural comparison, older age was associated with lower odds of medical menopause (OR per one SD increase 0.43, 95% CI 0.25–0.73). In the Surgical vs Natural model, older age also reduced the odds (OR 0.69, 0.49–0.98). Compared with Bumiputera Sarawak women, both Chinese (OR 0.31, 0.20–0.49) and Malay (OR 0.29, 0.12–0.70) women had significantly lower odds of surgical menopause, even after adjustment. Education and employment showed potentially protective effects against surgical menopause (e.g., higher education OR 0.23, 0.04–1.28), though these associations were imprecise, reflecting limited statistical power in some strata.
Intersectional models with cluster-robust standard errors accounted for clustering by locality and included an urban versus non-urban variable derived from free-text residence data. Urban residence was associated with higher adjusted odds of both medical menopause (OR 1.87, 1.07–3.26) and surgical menopause (OR 2.47, 1.25–4.86). Ethnic disparities remained significant, indicating that urbanicity, education, and employment did not fully explain the elevated surgical rates among Bumiputera Sarawak women. These findings suggest the role of healthcare system factors and culturally mediated care pathways in shaping menopause type.
Comorbidity Patterns
Diabetes and hypertension were the most frequent long-term conditions in the cohort. Pairwise clustering using the phi coefficient revealed stronger co-occurrence of these conditions among women with surgical menopause compared with natural or medical menopause, indicating a compounded burden of cardiometabolic risk in those who had undergone surgery.
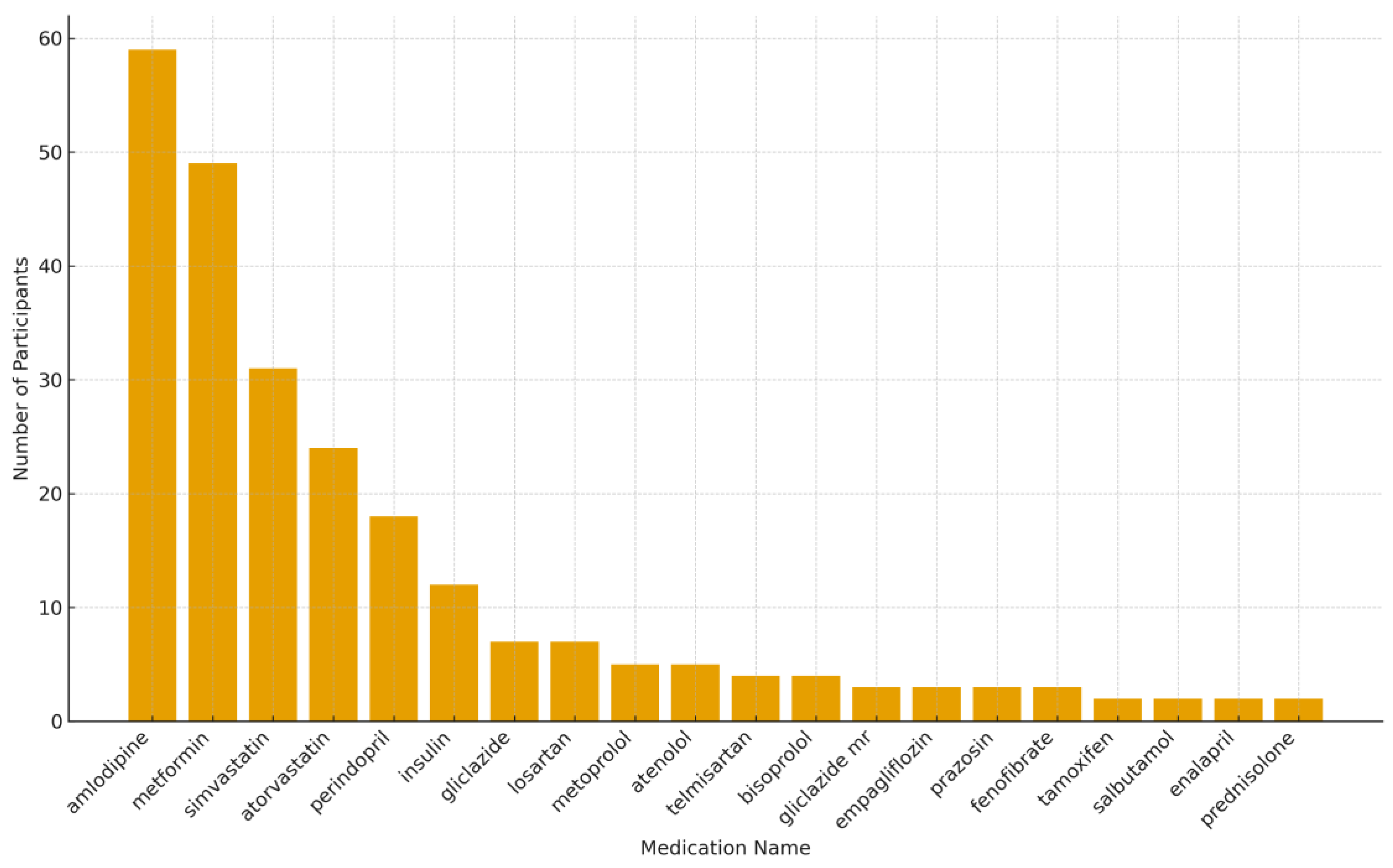
Drug Profile
Out of the 632 participants assessed at baseline, 248 individuals (39.2%) reported taking at least one prescribed medication, while 384 (60.8%) reported no current medication use (
Figure 2). The most commonly reported drug was amlodipine, an antihypertensive agent, used by 59 participants (9.3%). Metformin, which is prescribed for the management of type 2 diabetes, was the second most frequent drug, reported by 49 participants (7.8%). Simvastatin (n = 31, 4.9%) and atorvastatin (n = 24, 3.8%) were the leading lipid-lowering agents identified in the dataset. Other antihypertensive medications reported included perindopril (n = 18, 2.8%), losartan (n = 7, 1.1%), and telmisartan (n = 4, 0.6%). Insulin therapy was documented in 12 participants (1.9%), indicating a subset with advanced or poorly controlled diabetes. Oral hypoglycaemic agents such as gliclazide (n = 7, 1.1%) and empagliflozin (n = 3, 0.5%) were also noted. Beta-blockers, including metoprolol and atenolol, were each reported by five participants (0.8%), while bisoprolol was reported by four participants (0.6%). The distribution of reported medications highlights a predominance of cardiovascular and metabolic conditions, including hypertension, diabetes, and dyslipidaemia, within this cohort. These findings emphasise the importance of integrated management of chronic diseases among midlife women, particularly given that many of these commonly used drugs may interact with menopause-related treatments such as HRT.
Burden Index of Menopausal Disadvantage
A cumulative burden index was constructed across three domains: clinical (any long-term condition, POI, surgical menopause), treatment (absence of HRT, GnRH analogue exposure), and sociocultural (lower education, non-urban residence, reliance on traditional remedies). The index demonstrated a clear gradient by menopause type: women with natural menopause had the lowest scores, those with medical menopause were intermediate, and those with surgical menopause had the highest. This pattern highlights the intersection of biological, healthcare, and social disadvantage concentrated among women experiencing surgical menopause.
Cross-Country Comparison
For harmonised international reporting, three indicators were derived for Malaysia: mean age at menopause (50.1 years), prevalence of surgical menopause (16.0%), and current HRT use (8.0%). Preliminary comparison with other MARIE sites suggests that while menopausal timing in Malaysia aligns with global norms, surgical menopause rates are relatively high and HRT uptake is comparatively low. These findings indicate both gaps in access to conservative gynaecological care and under-utilisation of evidence-based menopause treatments.
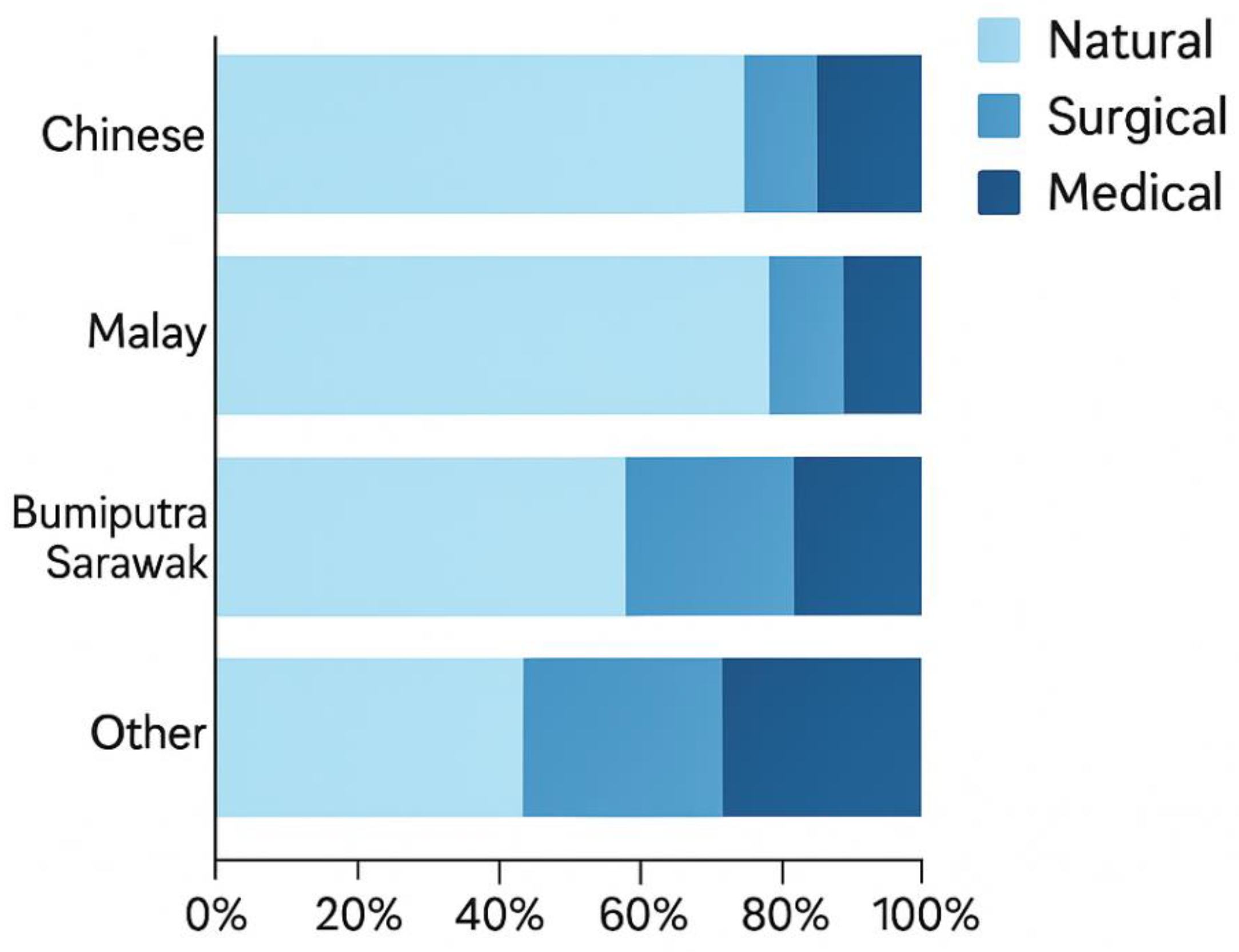
Ethnic Inequalities in Menopause Type
Among the 275 women with both ethnicity data and a determinable menopause type, the largest subgroups were Chinese (n=128), Malay (n=95), and Bhumiputra Sarawak (n=32). Smaller numbers were classified as Indian (n=16) or other ethnic groups (n=5). Marked differences were observed in the distribution of menopause type across ethnic groups. Among Chinese women, natural menopause predominated (75.8%, 95% CI 67.7–82.4), followed by medical menopause (11.7%, 95% CI 7.2–18.4) and surgical menopause (12.5%, 95% CI 7.8–19.3). A similar pattern was seen among Malay women, with natural menopause accounting for 73.9% (95% CI 64.1–81.8), medical menopause for 12.2% (95% CI 6.9–20.5), and surgical menopause for 13.9% (95% CI 8.3–22.4).
In contrast, Bhumiputra Sarawak women exhibited a very different profile: 51.6% (95% CI 34.8–68.0) experienced natural menopause, while 35.5% (95% CI 21.1–53.1) reported surgical menopause, and 12.9% (95% CI 5.4–27.4) medical menopause. This indicates that over one-third of women in this group underwent surgical menopause, a rate more than double that seen in Chinese and Malay groups.
When these differences were summarised as absolute ranges across ethnic groups with sufficient sample sizes (n≥5), the range for natural menopause was 0.80, for surgical menopause 0.60, and for medical menopause 0.20. These wide ranges indicate substantial heterogeneity between groups, especially for surgical menopause. The strikingly higher surgical prevalence among Bhumiputra Sarawak women suggests potential disparities in healthcare pathways, such as differential access to conservative treatments or culturally mediated differences in healthcare-seeking behaviour.
Marked ethnic differences were evident in menopause type. Among women with both ethnicity and determinable type, the largest groups were Chinese, Malay, and Bhumiputra Sarawak. Natural menopause predominated in the Chinese (approximately three-quarters) and Malay groups, with comparable, smaller shares of medical and surgical menopause. In contrast, Bhumiputra Sarawak women showed substantially higher surgical menopause. When summarised as absolute ranges across ethnic groups with at least five women in the denominator, the spread was 0.80 for natural menopause, 0.60 for surgical menopause, and 0.20 for medical menopause, indicating large between-group heterogeneity, particularly for surgical pathways.
To examine independent correlates of menopause type we estimated adjusted one-vs-reference logistic models comparing Medical vs Natural and Surgical vs Natural menopause. Predictors included standardised age, ethnicity (Chinese, Malay, Other; Bhumiputra Sarawak as the reference), education (Higher vs not), and employment (Employed vs not). In the Medical vs Natural contrast, older age was associated with lower odds of medical menopause (odds ratio [OR] per one SD increase in age 0.43, 95% CI 0.25–0.73). In the Surgical vs Natural contrast, older age was again associated with lower odds (OR 0.69, 95% CI 0.49–0.98). Relative to Bhumiputra Sarawak women, Chinese (OR 0.31, 95% CI 0.20–0.49) and Malay (OR 0.29, 95% CI 0.12–0.70) women had markedly lower odds of surgical menopause after adjustment, consistent with the unadjusted disparities. Point estimates for education and employment suggested potentially protective associations for surgical menopause (e.g., High education OR 0.23, 95% CI 0.04–1.28), but intervals were wide and included the null, reflecting limited power in some strata.
We further assessed inequalities in a contextual framework by fitting logistic generalised linear models with cluster-robust standard errors by place of residence (free-text locality), thereby allowing for within-place correlation of outcomes. In these intersectional models, urban residence was associated with higher adjusted odds of both medical menopause (OR 1.87, 95% CI 1.07–3.26) and surgical menopause (OR 2.47, 95% CI 1.25–4.86) compared with non-urban settings, even after controlling for age, ethnicity, education, and employment. The ethnicity gradients persisted: compared with Bhumiputra Sarawak, Chinese and Malay women had significantly lower odds of surgical menopause. Taken together, these findings indicate that the elevated surgical proportion in Bhumiputra Sarawak women is not simply a function of education, employment, or basic geography, and that contextual factors in urban care settings may channel women towards medical or surgical pathways more frequently.
To relate menopause type to broader clinical context, we mapped the co-occurrence of common long-term conditions where available. Diabetes and hypertension were frequent, with stronger pairwise clustering among women with surgical menopause than among those with natural or medical menopause, suggesting a compounded burden where surgical pathways and cardiometabolic disease intersect. We also constructed a burden index of menopausal disadvantage that sums indicators across clinical (presence of any long-term condition, POI, or surgical menopause), treatment (absence of current HRT, GnRH analogue exposure), and sociocultural domains (lower education, non-urban residence, reliance on traditional remedies). The index showed a monotonic gradient: women with natural menopause had the lowest mean burden scores, those with medical menopause were intermediate, and those with surgical menopause had the highest, highlighting cumulative disadvantage concentrated in the surgical group.
For Malaysia, the mean age at menopause was 50.1 years, the prevalence of surgical menopause was 16.0%, and current HRT use was 8.0%. These values will be set alongside equivalent estimates from other participating countries to contextualise Malaysia in global perspective; preliminary inspection indicates that, while menopausal timing is broadly aligned with international norms, surgical menopause is comparatively high and HRT uptake comparatively low.
Quality of Life and the Malaysian Contextuality
HRQoL scores (0–23; higher indicating worse quality of life) demonstrated a right-skewed distribution, with a median of 8 (IQR 4–10). HRQoL varied significantly across menopausal stages (Kruskal–Wallis H=294.7, p<0.001), with later stages generally exhibiting higher burden. Menopause type was also associated with HRQoL (H=310.3, p<0.001); surgically induced menopause showed worse scores compared with natural menopause. Participants reporting current medication use had higher HRQoL scores than non-users (Mann–Whitney U=34,928.5, p=5.97×10⁻⁵), aligning with greater multimorbidity among medication users. In contrast, HRQoL did not differ by physician-diagnosed endometriosis (U=14,812.0, p=0.563). Collectively, these findings indicate substantial HRQoL impairment concentrated among surgically menopausal participants and those using long-term medications, underscoring the need for integrated care that addresses chronic disease management alongside menopause-related concerns.
Figure 3.
Quality of life and the menopausal stage.
Figure 3.
Quality of life and the menopausal stage.
Discussion
This study provides the first comprehensive analysis of menopause experiences in a Malaysian population, drawing on data from 632 women in the MARIE study. The cohort was predominantly composed of women at or beyond the menopausal transition, with a mean age at menopause of 50.1 years, aligning with global averages but showing considerable individual variation. Natural menopause was the most common pathway, yet nearly one in four women experienced a non-natural menopause, either through surgical intervention (16.0%) or medical induction (11.3%). Marked ethnic differences were observed, with surgical menopause being substantially higher among Bumiputera Sarawak women compared to Chinese and Malay groups, a pattern that persisted even after adjusting for socio-demographic factors and place of residence [
13,
14]. Urban settings were associated with higher odds of both surgical and medical menopause, suggesting that local healthcare infrastructure and treatment pathways influence how menopause is managed. HRT use was strikingly low (8.0%), while reliance on traditional remedies was higher (12.1%), indicating gaps in access to and acceptance of evidence-based care. Women undergoing surgical menopause also showed higher rates of co-occurring cardiometabolic conditions and greater cumulative disadvantage across clinical, treatment, and sociocultural domains, reinforcing the intersection of biological and structural factors in shaping menopausal health.
Population Health and Symptom Burden
These findings have significant implications for population science, particularly in understanding how menopause interacts with broader health and social systems. The higher surgical menopause rates among Bumiputera Sarawak women highlight structural and cultural inequities, potentially reflecting differential access to conservative treatments, variations in health-seeking behaviours, or provider-level biases in surgical decision-making. The observed clustering of diabetes and hypertension among women with surgical menopause underscores the syndemic nature of reproductive ageing and chronic disease, indicating that menopause should be considered within integrated non-communicable disease (NCD) frameworks. The burden index developed in this study revealed a clear gradient of disadvantage, with surgical menopause concentrated among women with lower education, non-urban residence, and reliance on traditional remedies. These factors point to the role of social determinants in influencing both symptom severity and healthcare utilisation. The combination of low HRT uptake and high symptom burden particularly among women with non-natural menopause suggests that large segments of the population are managing menopause with limited access to effective, evidence-based treatments, leading to avoidable suffering and reduced quality of life. This highlights the need for culturally informed public health interventions that bridge biomedical and traditional care systems.
Clinical Practice Implications
From a clinical perspective, these findings call for urgent attention to the pathways leading to non-natural menopause and the low uptake of HRT in Malaysia. The relatively high rate of surgical menopause suggests an over-reliance on operative interventions such as hysterectomy for gynaecological conditions, where conservative treatments might be appropriate but under-utilised. Enhancing access to minimally invasive alternatives, improving clinical decision-making, and implementing shared decision-making models could reduce unnecessary surgical procedures. The ethnic and urban-rural disparities observed point to the need for equitable service delivery, with targeted strategies to reach populations at greatest risk of disadvantage, particularly Bumiputera Sarawak women and those living in urban centres where surgical pathways appear more common. The very low HRT uptake, coupled with higher use of traditional remedies, suggests both supply-side barriers such as availability and cost and demand-side factors, including stigma and lack of knowledge among clinicians and patients. Integrating menopause care into primary health services, providing culturally sensitive counselling, and ensuring affordable access to HRT could substantially improve outcomes. In parallel, clinicians should be aware of the elevated cardiometabolic burden among women undergoing surgical menopause, ensuring that these patients receive proactive monitoring and management to mitigate long-term health risks. These results underscore the importance of positioning menopause as a core component of women’s health policy and practice, bridging reproductive and chronic disease care to achieve better population-level outcomes.
Strengths and Limitations
A major strength of this study is its large, diverse, and nationally representative cohort, providing one of the most comprehensive datasets on menopause experiences in Malaysia to date. The integration of biological, sociocultural, and health system variables allowed for a multidimensional analysis, including intersectional modelling and the development of a novel burden index. Standardised data cleaning and rigorous analytic methods, including cluster-robust approaches, ensured the robustness and reproducibility of findings. However, the cross-sectional design limits causal inference, and missing data on some variables, including oophorectomy status and symptom severity, may have introduced residual uncertainty.
Conclusions
This study highlights significant ethnic and contextual disparities in menopause pathways in Malaysia, with high rates of surgical menopause and very low uptake of hormone replacement therapy. The findings underscore the intersection of biological, sociocultural, and health system factors, revealing a concentration of disadvantage among women with non-natural menopause. Addressing these inequities through equitable service delivery, culturally sensitive interventions, and improved access to conservative and evidence-based treatments is essential to improve health outcomes and quality of life.
Author Contributions
GD developed the ELEMI program and the MARIE project. This was furthered by GD and PP. TTH submitted and secured the ethics approval for the study in Singapore. TTH and his team collected the data. GD and JQS conducted the data analysis. GD wrote the first draft and was furthered TTH and by all other authors. Formatting and manuscript preparation was completed by VP. All authors critically appraised, reviewed and commented on all versions of the manuscript. All authors read and approved the final manuscript.
Institutional Review Board Statement
Medical Research & Ethics Committee, Ministry of Health Malaysia (NMRR ID 23-03581-PO8 (IIR)).
Informed Consent Statement
Obtained. All authors consented to publish this manuscript.
Data Availability Statement
The PIs and the study sponsor may consider sharing anonymous data upon reasonable a request.
Acknowledgments
Aini Hanan binti Azmi, Alyani binti Mohamad Mohsin, Arinze Anthony Onwuegbuna, Artini binti Abidin, Ayyuba Rabiu, Chijioke Chimbo, Chinedu Onwuka Ndukwe, Choon-Moy Ho, Chinyere Ukamaka Onubogu, Diana Chin-Lau Suk, Divinefavour Echezona Malachy, Emmanuel Chukwubuikem Egwuatu, Eunice Yien-Mei Sim, Farhawa binti Zamri, Fatin Imtithal binti Adnan, Geok-Sim Lim, Halima Bashir Muhammad, Ifeoma Bessie Enweani-Nwokelo, Ikechukwu Innocent Mbachu, Jinn-Yinn Phang, John Yen-Sing Lee, Joseph Ifeanyichukwu Ikechebelu, Juhaida binti Jaafar, Karen Christelle, Kathryn Elliot, Kim-Yen Lee, Kingsley Chidiebere Nwaogu, Lee-Leong Wong, Lydia Ijeoma Eleje, Min-Huang Ngu, Noorhazliza binti Abdul Patah, Nor Fareshah binti Mohd Nasir, Norhazura binti Hamdan, Nnanyelugo Chima Ezeora, Nnaedozie Paul Obiegbu, Nurfauzani binti Ibrahim, Nurul Amalina Jaafar, Odigonma Zinobia Ikpeze, Obinna Kenneth Nnabuchi, Pooja Lama, Puong-Rui Lau, Rakshya Parajuli, Rakesh Swarnakar, Raphael Ugochukwu Chikezie, Rosdina Abd Kahar, Safilah Binti Dahian, Sapana Amatya, Sing-Yew Ting, Siti Nurul Aiman, Sunday Onyemaechi Oriji, Susan Chen-Ling Lo, Sylvester Onuegbunam Nweze, Damayanthi Dassanayake, Nimesha Wijayamuni, Prasanna Herath, Thamudi Sundarapperuma, Vaitheswariy Rao, Xin-Sheng Wong, Xiu-Sing Wong, Yee-Theng Lau, Heitor Cavalini, Jean Pierre Gafaranga, Emmanuel Habimana, Chigozie Geoffrey Okafor, Assumpta Chiemeka Osunkwo, Gabriel Chidera Edeh, Esther Ogechi John, Kenechukwu Ezekwesili Obi, Oludolamu Oluyemesi Adedayo, Odili Aloysius Okoye, Chukwuemeka Chukwubuikem Okoro, Ugoy Sonia Ogbonna, Chinelo Onuegbuna Okoye, Babatunde Rufus Kumuyi, Onyebuchi Lynda Ngozi, Nnenna Josephine Egbonnaji, Oluwasegun Ajala Akanni, Perpetua Kelechi Enyinna, Yusuf Alfa, Theresa Nneoma Otis, Catherine Larko Narh Menka, Kwasi Eba Polley, Isaac Lartey Narh, Bernard B. Borteih, Andy Fairclough, Kingsley Emeka Ekwuazi, Michael Nnaa Otis, Jeremy Van Vlymen, Chidiebere Agbo, Francis Chibuike Anigwe, Kingsley Chukwuebuka Agu, Chiamaka Perpetua Chidozie, Chidimma Judith Anyaeche, Clementine Kanazayire, Jean Damascene Hanyurwimfura, Nwankwo Helen Chinwe, Stella Matutina Isingizwe, Jean Marie Vianney Kabutare, Dorcas Uwimpuhwe, Melanie Maombi, Ange Kantarama, Uchechukwu Kevin Nwanna, Benedict Erhite Amalimeh, Theodomir Sebazungu, Elius Tuyisenge, Yvonne Delphine Nsaba Uwera, Emmanuel Habimana, Nasiru Sani, Amarachi Pearl Nkemdirim, Rukshini Puvanendram, Manisha Mathur, Rajeswari Kathirvel, Farah Safdar, Raksha Aiyappan, Jean Pierre Gafaranga, Bertin Ngororano, Victor Archibon, Ibe Michael Usman, Baraka Godfrey Mwahi, Filbert Francis Ilaza, Zepherine Pembe, Clement Mwabenga, Mpoki Kaminyoghe, Brenda Mdoligo, Thomas Alone Saida, Nicodemus E. Mwampashi, Olisaemeka Nnaedozie Okonkwo, Bethel Chinonso Okemeziem, Bethel Nnaemeka Uwakwe, Goodnews Ozioma Igboabuchi, Ifeoma Francisca Ndubuisi.
Conflicts of Interest
All authors report no conflict of interest. The views expressed are those of the authors and not necessarily those of the NHS, the National Institute for Health Research, the Department of Health and Social Care or the Academic institutions.
Code Availability
Not applicable.
References
- Woods, N. F., Mitchell, E. S., Coslov, N. & Richardson, M. K. Transitioning to the menopausal transition: a scoping review of research on the late reproductive stage in reproductive aging. Menopause 28, 447-466 (2021). [CrossRef]
- Delanerolle, G. et al. Menopause: a global health and wellbeing issue that needs urgent attention. The Lancet Global Health 13, e196-e198 (2025). [CrossRef]
- Weber, M. T., Rubin, L. H. & Maki, P. M. Cognition in perimenopause: the effect of transition stage. Menopause 20, 511-517 (2013).
- Khalid, M. A. The future of employment in Malaysia, Singapore and Thailand: demographic and labour market trends of ageing societies in the context of the fourth industrial revolution. (2023).
- Blankenship, S. F. & Tan, K. K. H. in Contemporary Asian artistic expressions and tourism 147-167 (Springer, 2020).
- Talib, K. A. & AMRI, S. Cultural diversity in Malaysia and the reconciliation for integration. Jebat 47, 308 (2020).
- Tohit, N. F. M. & Haque, M. Forbidden conversations: A comprehensive exploration of taboos in sexual and reproductive health. Cureus 16 (2024). [CrossRef]
- Ohn Mar, S. et al. Use of alternative medications for menopause-related symptoms in three major ethnic groups of Ipoh, Perak, Malaysia. Asia Pacific Journal of Public Health 27, 19S-25S (2015). [CrossRef]
- Lau, E. X. X. et al. Holistic horizons: understanding the landscape of traditional and complementary medicines among menopausal women in Kuala Lumpur. BMC Complementary Medicine and Therapies 25, 97 (2025). [CrossRef]
- Gan, M. H. et al. Exploring hormone replacement therapy dynamics among menopausal women in Kuala Lumpur–a community based survey. BMC Women’s Health 24, 569 (2024). [CrossRef]
- Liew, C. H., Shabaruddin, F. H. & Dahlui, M. in Healthcare. 2099 (MDPI).
- Loganathan, T., Chan, Z. X., de Smalen, A. W. & Pocock, N. S. Migrant women’s access to sexual and reproductive health services in Malaysia: a qualitative study. International journal of environmental research and public health 17, 5376 (2020). [CrossRef]
- Damodaran, P., Ng, B. K. & Azmi, A. H. Menopausal symptoms among multi-ethnic working women in Malaysia. Climacteric, 1-8 (2025). [CrossRef]
- Ahmad, E. BMI and Gender as Mediators in the Association Between Ethnicity and Glycemic Control in Primary Healthcare Settings: Malaysia National Diabetes Registry Cohort, University of Malaya (Malaysia), (2019).
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).