Submitted:
15 October 2025
Posted:
16 October 2025
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
2.1. Nature, Scope, and Study Period
2.2. Patient Selection
2.3. Parameters of Interest
2.4. Operational Definitions and Concepts
2.5. Ethical Considerations
2.6. Statistics
3. Results
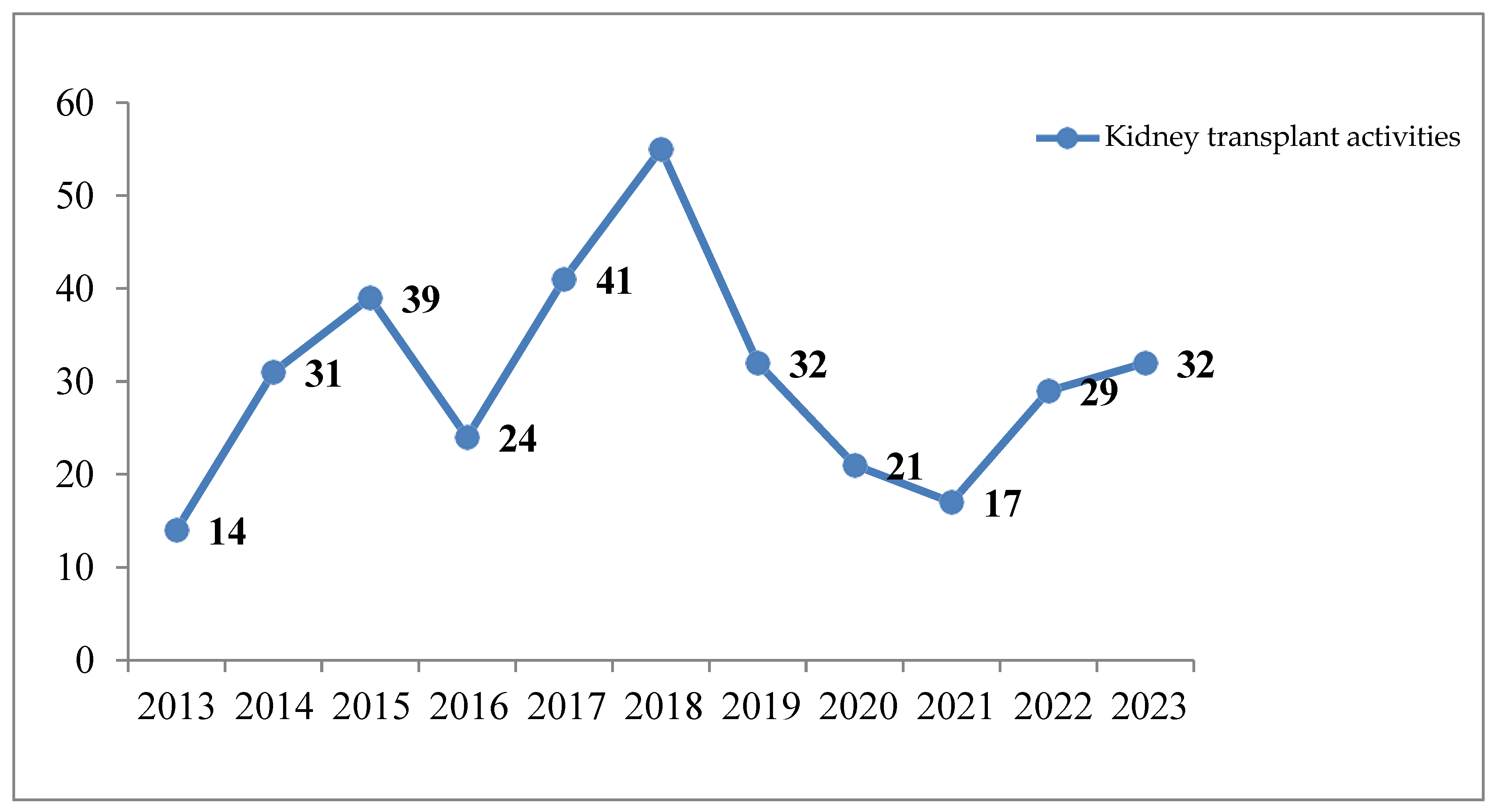
3.1. Kidney Transplant Recipients
3.2. Kidney Transplant Donors
3.3. Modalities of Renal Transplantation
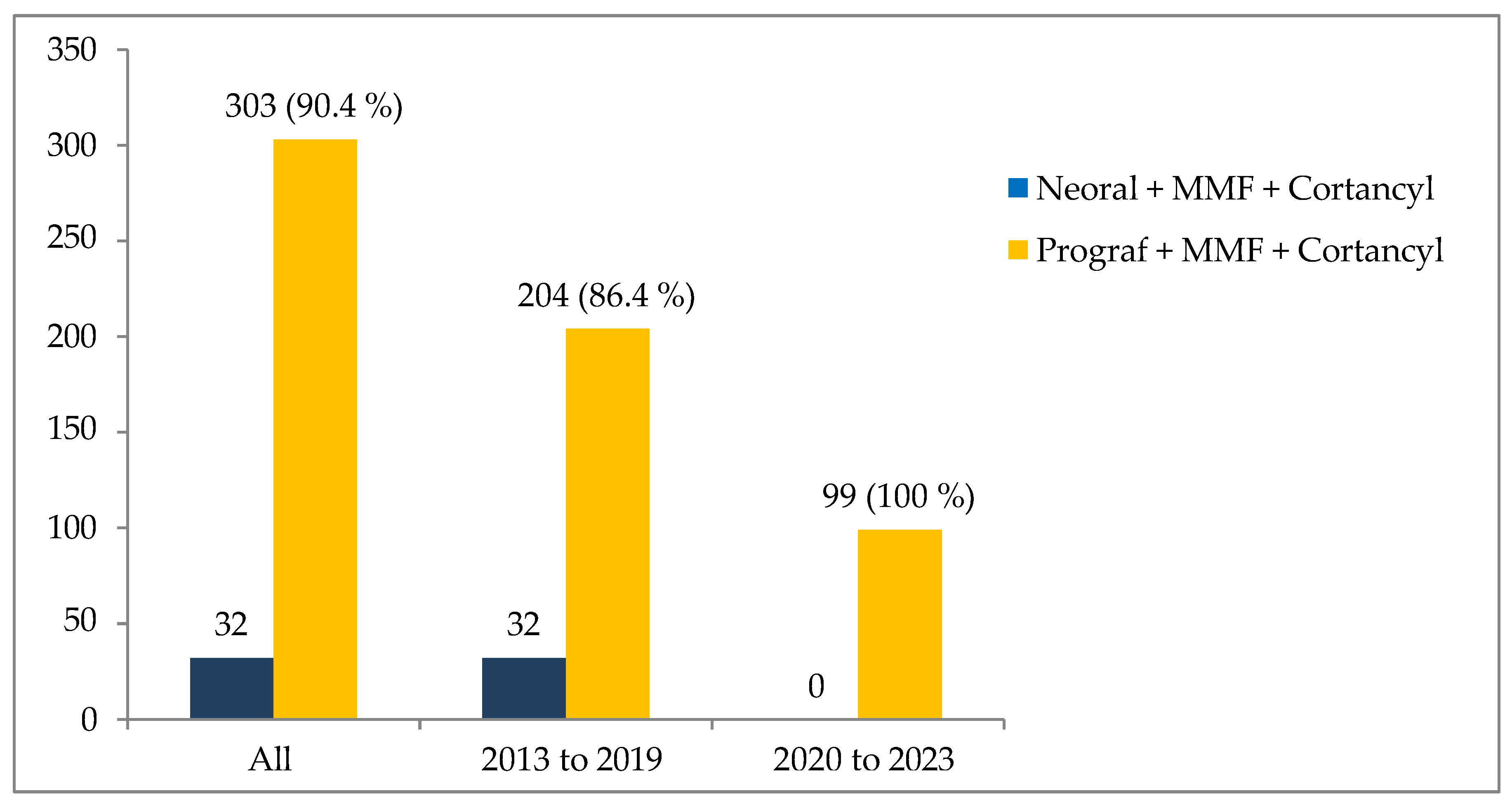
3.4. Anti-Rejection Immunosuppressive Therapy
3.5. Post-Transplant Complications
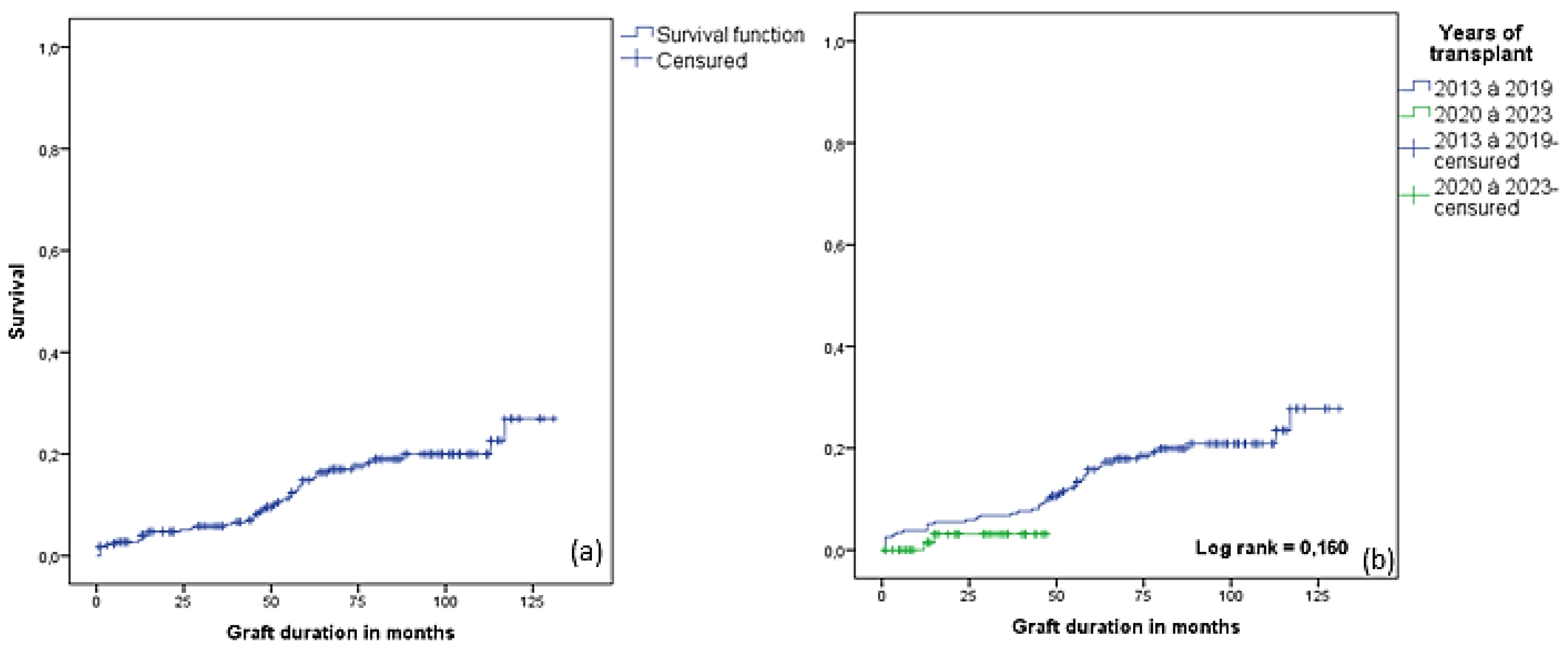
3.6. Graft Survival and Factors Associated with RGF
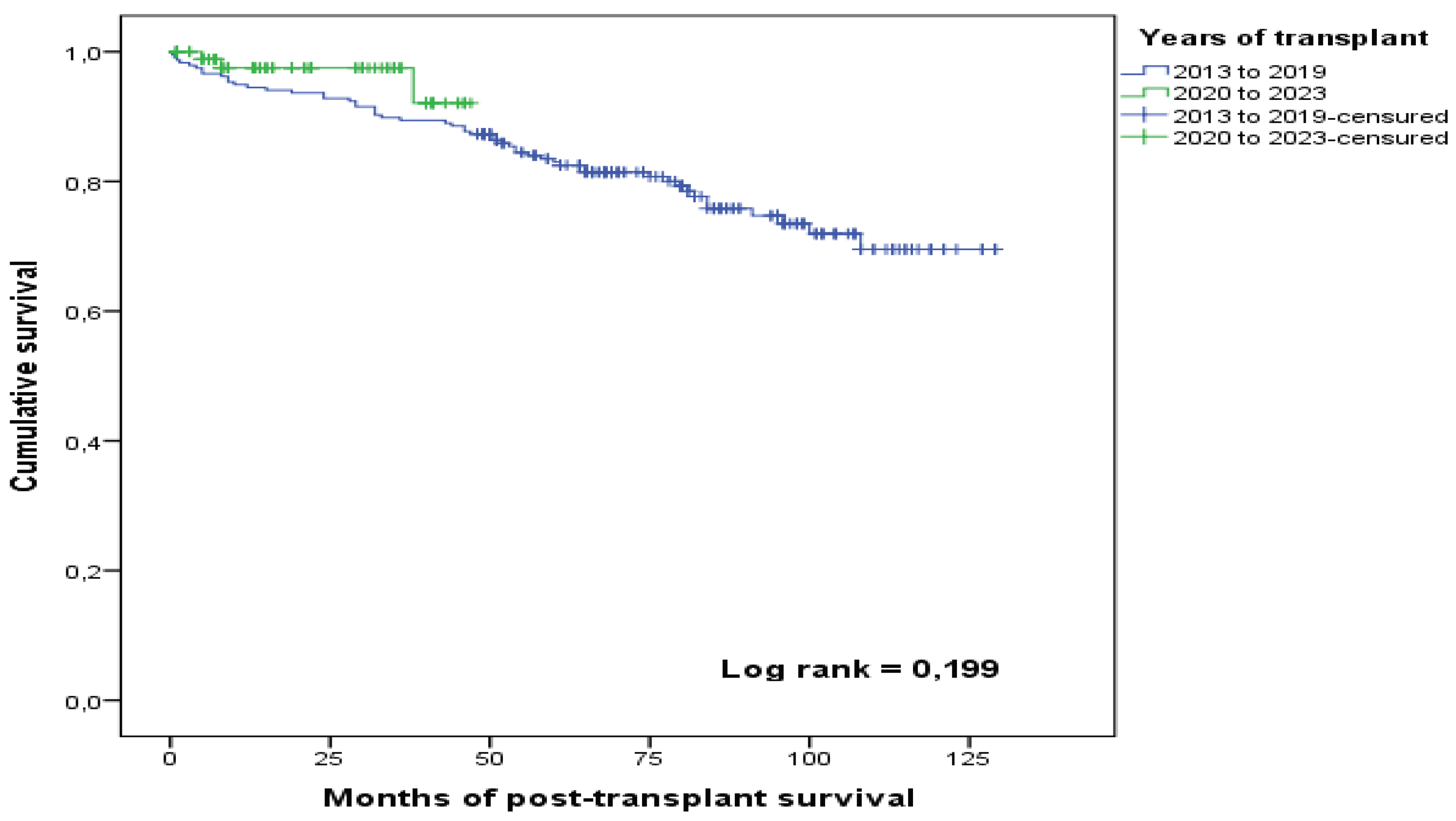
3.7. Patient Survival and Factors Associated with Death
3.8. Causes of Death
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ATG | anti-thymocyte globulin |
| ATP | adenosine triphosphate |
| CHU | centre hospitalier universitaire |
| CI | confidence interval |
| CIT | cold ischemia time |
| CKD | chronic kidney disease |
| COVID-19 | coronavirus disease 2019 |
| DBD | deceased brain-dead donor |
| DCAD | deceased cardiac arrest donor |
| DSA | donor specific antidodies |
| ESRD | end stage renal disease |
| GPN | graft pyeloniphritis |
| HLA | human leukocyte antigen |
| IFTA | interstitial fibrosis and tubular atrophy |
| KT | kidney transplant |
| LVD | living-related donor |
| MFI | mean fluorescence intensity |
| MMF | mycophenolate mofetil |
| OR | odds ratio |
| RGF | renal graft failure |
| SCD | standard criteria donor |
| WIT | warm ischemia time |
References
- Jager KJ, Kovesdy C, Langham R, Rosenberg M, Jha V, Zoccali C. A single number for advocacy and communication—worldwide more than 850 million individuals have kidney diseases. Kidney Int. 1 nov 2019;96(5):1048-50.
- GBD 2016 Causes of Death Collaborators. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Lond Engl. 16 sept 2017;390(10100):1151-210. [CrossRef]
- Foreman KJ, Marquez N, Dolgert A, Fukutaki K, Fullman N, McGaughey M, et al. Forecasting life expectancy, years of life lost, and all-cause and cause-specific mortality for 250 causes of death: reference and alternative scenarios for 2016-40 for 195 countries and territories. Lancet Lond Engl. 10 nov 2018;392(10159):2052-90. [CrossRef]
- Hilde V, Knotek O. Question parlementaire | Approche systématique européenne face à l’insuffisance rénale chronique | O-000005/2022 | Parlement européen [Internet]. [cité 1 juin 2025]. Available online: https://www.europarl.europa.eu/doceo/document/O-9-2022-000005_FR.html.
- Agence de la biomédecine. Journée mondiale du rein - le 10 mars 2022 : Le Réseau Épidémiologie et Information en Néphrologie (R.E.I.N) tenu par l’Agence de la biomédecine fête ses 20 ans [Internet]. [cité 1 juin 2025]. Available online: https://www.agence-biomedecine.fr/fr/observatoire-de-la-maladie-renale-chronique/journee-mondiale-du-rein-le-10-mars-2022-le-reseau-epidemiologie-et-information-en-nephrologie-(r-e-i-n)-tenu-par-l-agence-de-la-biomedecine-fete-ses-20-ans.
- Kazes I, Solignac J, Lassalle M, Mercadal L, Couchoud C. Twenty years of the French Renal Epidemiology and Information Network. Clin Kidney J. 13 nov 2023;17(1):sfad240. [CrossRef]
- Francis A, Harhay MN, Ong ACM, Tummalapalli SL, Ortiz A, Fogo AB, et al. Chronic kidney disease and the global public health agenda: an international consensus. Nat Rev Nephrol. juill 2024;20(7):473-85.
- Kovesdy CP. Epidemiology of chronic kidney disease: an update 2022. Kidney Int Suppl. avr 2022;12(1):7-11. [CrossRef]
- Vestergaard AHS, Jensen SK, Heide-Jørgensen U, Frederiksen LE, Birn H, Jarbøl DE, et al. Risk factor analysis for a rapid progression of chronic kidney disease. Nephrol Dial Transplant Off Publ Eur Dial Transpl Assoc - Eur Ren Assoc. 28 juin 2024;39(7):1150-8. [CrossRef]
- Losbar O. RCI. [cité 21 mai 2025]. Les guadeloupéens encore très réticents au don d’organes. Available online: https://rci.fm/guadeloupe/infos/Sante/Les-guadeloupeens-encore-tres-reticents-au-don-dorganes.
- Agence de la biomédecine. Recommandations de l’Agence de la biomédecine relatives à la poursuite des activités de prélèvement et de greffe en cas de rebond de l’épidémie de COVID-19 [Internet]. 2020 [cité 21 mai 2025]. Available online: https://www.agence-biomedecine.fr/Recommandations-de-l-Agence-de-la-biomedecine-relatives-a-la-poursuite-des.
- Agence de la biomédecine. Activité de prélèvement et de greffe d’organes en 2023 et baromètre d’opinion 2024 [Internet]. Agence de la biomédecine. 2024 [cité 1 juin 2025]. Available online: https://presse.agence-biomedecine.fr/?p=3744.
- Currie IS, Henderson LK. ABO-incompatible renal transplantation. Lancet Lond Engl. 18 mai 2019;393(10185):2014-6. [CrossRef]
- Argani H. Expanded Criteria Donors. Exp Clin Transplant Off J Middle East Soc Organ Transplant. août 2022;20(Suppl 4):13-9. [CrossRef]
- Kidney Disease: Improving Global Outcomes (KDIGO) Transplant Work Group. KDIGO clinical practice guideline for the care of kidney transplant recipients. Am J Transplant Off J Am Soc Transplant Am Soc Transpl Surg. nov 2009;9 Suppl 3:S1-155. [CrossRef]
- Agence de la biomédecine. Greffe d’organes : données générales et méthodes. Rapport annuel 2023 [Internet]. 2024 [cité 16 mai 2025]. Available online: https://rams.agence-biomedecine.fr/greffe-dorganes-donnees-generales-et-methodes.
- Cozzi E, Álvarez M, Carmona M, Mahíllo B, Forsythe J, Lomero M, et al. An Analysis by the European Committee on Organ Transplantation of the Council of Europe Outlining the International Landscape of Donors and Recipients Sex in Solid Organ Transplantation. Transpl Int Off J Eur Soc Organ Transplant. 2022;35:10322. [CrossRef]
- Katz-Greenberg G, Shah S. Sex and Gender Differences in Kidney Transplantation. Semin Nephrol. mars 2022;42(2):219-29. [CrossRef]
- Lassalle M, Fezeu L, Couchoud C, Hannedouche T, Massy ZA, Czernichow S. Obésité et accès à la greffe rénale parmi des patients démarrant une dialyse : une étude de cohorte prospective. Néphrologie Thérapeutique. 1 sept 2016;12(5):281.
- Betjes MGH, Sablik KS, Otten HG, Roelen DL, Claas FH, de Weerd A. Pretransplant Donor-Specific Anti-HLA Antibodies and the Risk for Rejection-Related Graft Failure of Kidney Allografts. J Transplant. 2020;2020:5694670. [CrossRef]
- Bonventre JV, Weinberg JM. Recent advances in the pathophysiology of ischemic acute renal failure. J Am Soc Nephrol JASN. août 2003;14(8):2199-210. [CrossRef]
- Echterdiek F, Latus J, Döhler B, Schwenger V, Süsal C. Influence of Cold Ischemia Time on the Outcome of Kidney Transplants from Donors Aged 70 Years and Above—A Collaborative Transplant Study Report. Transplantation. nov 2021;105(11):2461-9. [CrossRef]
- Jassem W, Fuggle SV, Rela M, Koo DDH, Heaton ND. The role of mitochondria in ischemia/reperfusion injury. Transplantation. 27 févr 2002;73(4):493-9.
- Habran M, De Beule J, Jochmans I. IGL-1 preservation solution in kidney and pancreas transplantation: A systematic review. PloS One. 2020;15(4):e0231019. [CrossRef]
- Maathuis MHJ, Ottens PJ, van Goor H, Zwaagstra JJ, Wiersema-Buist J, Schuurs TA, et al. Static cold storage preservation of ischemically damaged kidneys. a comparison between IGL-1 and UW solution. Transpl Int Off J Eur Soc Organ Transplant. mai 2008;21(5):473-82. [CrossRef]
- Jackson KR, Motter JD, Kernodle A, Desai N, Thomas AG, Massie AB, et al. How do highly sensitized patients get kidney transplants in the United States? Trends over the last decade. Am J Transplant Off J Am Soc Transplant Am Soc Transpl Surg. août 2020;20(8):2101-12. [CrossRef]
- Langewisch E, Mannon RB. Chronic Allograft Injury. Clin J Am Soc Nephrol. nov 2021;16(11):1723. [CrossRef]
- Burton SA, Amir N, Asbury A, Lange A, Hardinger KL. Treatment of antibody-mediated rejection in renal transplant patients: a clinical practice survey. Clin Transplant. févr 2015;29(2):118-23. [CrossRef]
- Bouquegneau A, Loheac C, Aubert O, Bouatou Y, Viglietti D, Empana J, et al. Complement-activating donor-specific anti-HLA antibodies and solid organ transplant survival: A systematic review and meta-analysis. PLoS Med. 2018;15(5):e1002572. [CrossRef]
- Agence de la biomédecine. Rapport annuel médical et scienti- fique. Saint-Denis La Plaine. 2014. Available online: http://www.agence- biomedecine.fr/annexes/bilan2014/donnees/organes/ 06-rein/synthese.htm.
- Racusen LC, Regele H. The pathology of chronic allograft dysfunction. Kidney Int. 1 déc 2010;78:S27-32. [CrossRef]
- Ouellet G, Houde I, Riopel J, Latulippe E, Douville P, Lesage J, et al. The Progression of Interstitial Fibrosis and Tubular Atrophy at 6 Months Is an Independent Predictor of Poor Graft Outcomes in Kidney Transplant Recipients. Transplant Direct. 4 nov 2022;8(12):e1375. [CrossRef]
| Variables | All n=335 |
2013-2019 n=236 |
2020-2023 n=99 |
P |
|---|---|---|---|---|
| Age, years | 52.5 ±11.9 | 52.3±11.6 | 53.2±12.7 | 0.553 |
| Age ≥ 70 years | 13 (3.9) | 5 (2.1) | 8 (8.1) | 0.024 |
| Gender | 0.040 | |||
| Men | 214 (63.9) | 159 (67.4) | 55 (55.6) | |
| Women | 121(36.1) | 77(32.6) | 44 (44.4) | |
| Blood types | 0.381 | |||
| O | 167 (49.9) | 115(48.7) | 52(52.5) | |
| A | 107 (31.9) | 74(31.4) | 33(33.3) | |
| B | 54 (16.1) | 43(18.1) | 11(11.1) | |
| AB | 7(2.1) | 4(1.7) | 3(3.0) | |
| HBP | 327 (97.6) | 232 (98.3) | 95 (96.0) | 0.242 |
| Diabetes mellitus | 85 (25.4) | 63 (26.7) | 22 (22.2) | 0.391 |
| Obesity | 59 (17.6) | 34 (14.4) | 25 (25.3) | 0.017 |
| Heterozygous sickle cell disease | 8 (2.4) | 2 (0.8) | 6 (6.1) | 0.010 |
| SLE | 13 (3,9) | 9 (3.8) | 4 (4,0) | 1.000 |
| ADPKD | 29 (8,7) | 15 (6,4) | 14 (14,1) | 0.021 |
| Ab HLA I positive | 145 (43,3) | 92 (39,0) | 53 (53,5) | 0.014 |
| Ab HLA II positive | 105 (31,3) | 61(25,8) | 44 (44,4) | <0.001 |
| Positive historical DSA | 88 (26,3) | 57 (24,2) | 31(31,3) | 0.174 |
| Pre-transplant transfusion | 114 (34,0) | 69 (29,2) | 45 (45,5) | 0.004 |
| Variables | All n=335 |
2013-2019 n=236 |
2020-2023 n=99 |
P |
|---|---|---|---|---|
| Average age, years | 51.5 ±16,1 | 50.6±16,7 | 53.5±14.4 | 0.007 |
| Gender | 0.001 | |||
| Men | 263(78.5) | 201 (85.2) | 62(62.6) | |
| Women | 72(21.5) | 35 (14,8) | 37(37.3) | |
| Type of donor | 0.109 | |||
| DBD | 329(98.2) | 230(97.5) | 99(100.0) | |
| LRD | 6(1.8) | 6(2.5) | 0(0.0) | |
| Blood types | 0.236 | |||
| O | 163(48.7) | 114(48.3) | 49(49.5) | |
| A | 100(29.9) | 65(27.5) | 35(35.4) | |
| B | 56(16.7) | 45(19.1) | 11(11,1) | |
| AB | 16(4.8) | 12(5.1) | 4 (4.0) |
| Variables | All | 2013-2019 | 2020-2023 | p |
|---|---|---|---|---|
| n=335 | n=236 | n=99 | ||
| CIT, min | 1090±389.7 | 1126.6±392.3 | 1002.9±402.5 | 0.009 |
| CIT >1200 min | 136 (40.6) | 101(42.8) | 35 (35.4) | 0.206 |
| WIT, min | 60.4±19.4 | 57.7±17.8 | 66.9±21.5 | <0.001 |
| WIT > 60 min | 149 (44.5) | 92 (39,0) | 57 (57.6) | 0.002 |
| Cardiac arrest | 319 (95.2) | 222 (94.1) | 97 (98.0) |
| Complications | All | 2013-2019 | 2020-2023 | P |
|---|---|---|---|---|
| n=335 | n=236 | n=99 | ||
| Delayed recovery of graft function | 4(1.2) | 4(1.7) | 0 | 0.193 |
| Acute tubular necrosis | 1(0.3) | 1(0.4) | 0 | 0.517 |
| Active humoral rejection M3 | 9(2.7) | 8(3.4) | 1(1.0) | 0.219 |
| Chronic humoral rejection M12 | 2(0.6) | 2(0.8) | 0 | 0.358 |
| Acute cellular rejection M3 | 8(2.4) | 8(3.4) | 0 | 0.064 |
| Chronic cell rejection M12 | 2(0.6) | 2(0,8) | 0 | 0.358 |
| Post-operative cardiac arrest | 2(0.6) | 2(0.8) | 0 | 0.358 |
| Graft artery thrombosis | 1(0.3) | 1(0.4) | 0 | 0.517 |
| Urological complications | ||||
| Acute urinary retention | 1(0.3) | 1(0.4) | 0 | 0.517 |
| Graft artery stenosis | 1(0.3) | 1(0.4) | 0 | 0.517 |
| External iliac artery stenosis | 2(0.6) | 2(0.8) | 0 | 0.358 |
| Plicature of the graft artery | 1(0.3) | 1(0.4) | 0 | 0.517 |
| Ureterotomy | 1(0.3) | 1(0.4) | 0 | 0.517 |
| Ureteral breach | 1(0,3) | 0 | 1(1.0) | 0.517 |
| Surgical complications | ||||
| Transplantectomy | 1(0,3) | 1(0,4) | 0 | 0.517 |
| Section of the inferior polar artery | 2(0,6) | 2(0.8) | 0 | 0.358 |
| Infectious complications | ||||
| COVID-19 | 9(2.7) | 8(3.4) | 1(1.0) | 0.219 |
| BK virus infection | 13(3.9) | 10(4.2) | 3(3.3) | 0.602 |
| Graft preservation fluid infection | 3(0.9) | 2(0.8) | 1(1.0) | 0.885 |
| Acute graft pyelonephritis | 23(6.9) | 15(6.4) | 8(8.1) | 0.569 |
| Other complications | ||||
| Cortisonic diabetes | 3(0,9) | 3(1.3) | 0 | 0.260 |
| Native nephropaty disease | 12(3,6) | 9(3.8) | 3(3.0) | 0.725 |
| Chronic allograft nephropathy | 21(6,3) | 17(7.2) | 4(4.0) | 0.276 |
| IFTA grade 1 M3 | 26(7,8) | 9(3.8) | 17(17.2) | < 0.001 |
| IFTA grade 2 M3 | 22(6,6) | 8(3.4) | 14(14.1) | <0.001 |
| IFTA grade 3 M3 | 9(2.7) | 4(1.7) | 5(5.1) | 0.083 |
| IFTA grade 1 M12 | 9(2,7) | 7(3.0) | 2(2.0) | 0.625 |
| IFTA grade 2 M12 | 3(0.9) | 3(1.3) | 0(0.0) | 0.260 |
| IFTA grade 3 M12 | 4(1.2) | 3(1.3) | 1(1.0) | 0.841 |
| Arteriolar hyalinosis M12 | 21(6,3) | 12(5.1) | 9(9.1) | 0.168 |
| Graft failure | 48(14.3) | 44 (18.6) | 4(4.0) | <0.001 |
| Time | All | 2013-2019 | 2020-2023 | p |
|---|---|---|---|---|
| n=335 | n=236 | n=99 | ||
| 6 months | 97.3 | 97.5 | 100 | 0.160 |
| 1 year | 97.0 | 94.9 | 98.5 | |
| 4 years | 90.9 | 89.8 | 96.9 | |
| 5 years | 85.1 | 84.2 | - | |
| 10 years | 73.1 | 72.2 | - |
| Risk factors | Univariate analysis | Multivariate analysis | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | P | ORa | 95% CI | p | |
| Transplantation 2013-2019 vs 2020-2023 | 7.53 | 2.28-24.88 | ˂0.001 | 6.24 | 1.84 – 21.14 | 0.003 |
| Male vs. female donors | 3.42 | 1.18-9.85 | 0.014 | - | - | - |
| Surgical complications vs no | 4.56 | 1.41-15.31 | 0.018 | 6.01 | 1.61-22.40 | 0.080 |
| Ab HLA1+ | 2.04 | 1.05-3.96 | 0.033 | - | - | - |
| Postoperative cardiac arrest vs no | 7.24 | 5.52-9.43 | 0.020 | - | - | - |
| IFTA grade 1 M3 vs no | 1.18 | 1.12-1.24 | 0.035 | - | - | - |
| Allograft nephropathy vs. no | 3.33 | 1.26-8.77 | 0.019 | 3.21 | 1.14-9.00 | 0.027 |
| Time | All | 2013-2019 | 2020-2023 | p |
|---|---|---|---|---|
| n=335 | n=236 | n=99 | ||
| 6 months | 97.3 | 96.6 | 98.9 | 0.199 |
| 1 year | 95.3 | 94.5 | 97.6 | |
| 4 years | 87.5 | 87.3 | 95.9 | |
| 5 years | 83.2 | 83.0 | - | |
| 10 years | 72.3 | 72.0 | - |
| Risk factors | Univariate analysis | Multivariate analysis | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p | Ora | 95% CI | P | |
| Age ≥ 60 years vs. no | 2.87 | 1.60-24.88 | ˂0.001 | 2,96 | 1.39–5.62 | 0.004 |
| Graft failure vs no | 2.87 | 1,60-5.13 | ˂0.001 | 10.31 | 4.76–22.22 | ˂0.001 |
| Transplantation 2013 - 2019 vs 2020-2023 |
5.43 | 2.11-14.08 | 0.001 | 4.48 | 1.52–13.33 | 0.007 |
| Diabetes mellitus vs no | 2.50 | 1.38-4.53 | 0.004 | 3.26 | 1.57-6.75 | 0.002 |
| CIT ≥1200 min vs no |
1.88 | 1.06-3.32 | 0.039 | 2.28 | 1.15-4.54 | 0.019 |
| Post-operative cardiac arrest | 5.95 | 4.67-7.58 | 0.030 | - | - | - |
| Graft pyelonephritis vs no | 2.80 | 1.13-6.94 | 0.040 | 3.51 | 1.17-10.49 | 0.025 |
| Variables | All | 2013-2019 | 2020-2023 | P |
|---|---|---|---|---|
| n=335 | n=236 | n=99 | ||
| Death at home | 17(5,1) | 16(6,8) | 1(1,0) | 0,028 |
| Multivisceral failure due to sepsis | 18(5,4) | 17(7,2) | 1(1,0) | 0,022 |
| COVID-19 | 9(2,7) | 8(3,4) | 1(1,0) | 0,219 |
| Hemorrhagic shock | 2(0,6) | 2(0,8) | 0(0,0) | 0,358 |
| Hemorrhagic stroke | 3(0,9) | 3(0,9) | 0(0,0) | 0,260 |
| Cranioencephalic trauma | 1(0,3) | 1(0,4) | 0(0,0) | 0,517 |
| Clostridial colitis | 1(0,3) | 1(0,4) | 0(0,0) | 0,517 |
| Suicide | 1(0,3) | 1(0,4) | 0(0,0) | 0,122 |
| Cancer | 3 (0,9) | 2 (0,8) | 1(1,0) | 0,925 |
| Unknown | 1(0,3) | 1(0,4) | 0(0,0) | 0,517 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





