Submitted:
09 October 2025
Posted:
11 October 2025
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
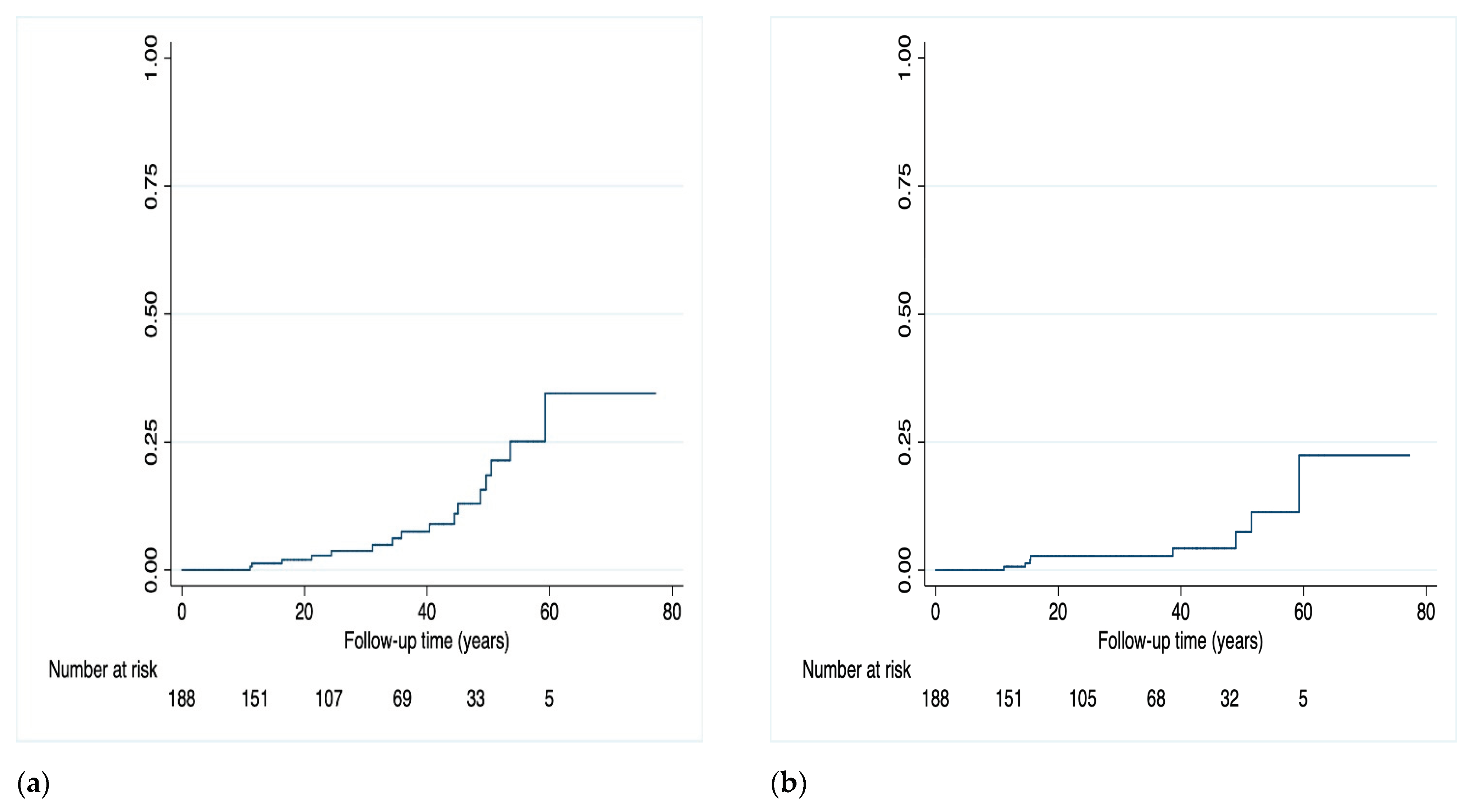
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
Abbreviations
| MDPI | Multidisciplinary Digital Publishing Institute |
| HIV | Human Immunodeficiency Virus |
| HBV | Hepatitis B Virus |
| 3TC | Lamivudine |
| 3TC/DTG | Lamivudine/Dolutegravir |
| PWH | People Living with HIV |
| ART | Antiretroviral Therapy |
| VF | Virological Failure |
| RAMs | Resistance Associated Mutations |
| OBI | Occult HBV Infection |
| TD | Treatment Discontinuation |
| PYFU | Patient Year of Follow-Up |
| HR | Hazard Ratio |
| CI | Confidence Interval |
| GSS | Genotypic Susceptibility Score |
| PrEP | Pre-Exposure Prophylaxis |
| MSM | Males who have Sex with Males |
| HCV | Hepatitis C Virus |
| IDU | Intravenous Drug Users |
| NRTI | Nucleoside Reverse Transcriptase Inhibitor |
| INSTI | Integrase Strand Transfer Inhibitor. |
References
- EACS Guidelines version 12.1, November 2024. Available at https://eacs.sanfordguide.com/. Last accessed 20/04/2025. 20 November.
- Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the Use of Antiretroviral Agents in Adults and Adolescents with HIV. Department of Health and Human Services. Year. Available at https://clinicalinfo.hiv.gov/en/guidelines/adult-and-adolescent-arv. Last accessed 20/04/2025.
- Sarmati, Loredana, and Vincenzo Malagnino. “HBV Infection in HIV-Driven Immune Suppression.” Viruses vol. 11,11 1077. 19 Nov. 2019. [CrossRef]
- Malagnino, Vincenzo et al. “Association between markers of hepatitis B virus infection and risk of virological rebound in people with HIV receiving antiretroviral therapy.” HIV medicine vol. 25,10 (2024): 1101-1111. [CrossRef]
- Thornton, Alicia C et al. “Hepatitis B, hepatitis C, and mortality among HIV-positive individuals.” AIDS (London, England) vol. 31,18 (2017): 2525-2532. [CrossRef]
- Rajbhandari R, Jun T, Khalili H, Chung RT, Ananthakrishnan AN. HBV/HIV coinfection is associated with poorer outcomes in hospitalized patients with HBV or HIV. J Viral Hepat. 2016 Oct;23(10):820-9. Epub 2016 Jun 13. PMCID: PMC5028254. [CrossRef] [PubMed]
- Soo-Yon Rhee, Matthew J. Gonzales, Rami Kantor, Bradley J. Betts, Jaideep Ravela, and Robert W. Shafer (2003) Human immunodeficiency virus reverse transcriptase and protease sequence database. Nucleic Acids Research, 31(1), 298-303.
- Osiyemi, Olayemi et al. Efficacy and Safety of Switching to Dolutegravir/Lamivudine Versus Continuing a Tenofovir Alafenamide-Based 3- or 4-Drug Regimen for Maintenance of Virologic Suppression in Adults Living With Human Immunodeficiency Virus Type 1: Results Through Week 144 From the Phase 3, Noninferiority TANGO Randomized Trial. Clinical infectious diseases: an official publication of the Infectious Diseases Society of America vol. 75,6 (2022): 975-986. [CrossRef]
- Underwood M, et al. Archived resistance and response to <40 c/mL & TND – DTG/3TC FDC at week 48 in SALSA. Presented at the 29th Conference on Retroviruses and Opportunistic Infections (CROI), February 12-16, 2022, Virtual Event. Poster.
- SOLAR-3D: Wk 144 Results of Switching to DTG/3TC in Virologically Suppressed Heavily Treatment–Experienced People With HIV. Presented at CCO Official Conference Coverage of AIDS 2024, the 25th International AIDS Conference; July 22-26, 2024; Munich, Germany.
- Kabra M, Barber TJ, Allavena C, Marcelin AG, Di Giambenedetto S, Pasquau J, Gianotti N, Llibre JM, Rial-Crestelo D, De Miguel-Buckley R, Blick G, Turner M, Harrison C, Wynne T, Verdier G, Parry CM, Jones B, Okoli C, Donovan C, Priest J, Letang E. Virologic Response to Dolutegravir Plus Lamivudine in People With Suppressed Human Immunodeficiency Virus Type 1 and Historical M184V/I: A Systematic Literature Review and Meta-analysis. Open Forum Infect Dis. 2023 Oct 27;10(11):ofad526. PMCID: PMC10686367. [CrossRef] [PubMed]
- Borghetti, Alberto et al. “Efficacy of Lamivudine Plus Dolutegravir vs Dolutegravir-Based 3-Drug Regimens in People With HIV Who Are Virologically Suppressed.” Open forum infectious diseases vol. 11,5 ofae198. 10 Apr. 2024. [CrossRef]
- Gagliardini, Roberta et al. “Impact of resistance mutations on efficacy of dolutegravir plus rilpivirine or plus lamivudine as maintenance regimens: a cohort study.” Journal of global antimicrobial resistance vol. 28 (2022): 274-281. [CrossRef]
- Borghetti, A et al. “Virological outcomes with dolutegravir plus either lamivudine or two NRTIs as switch strategies: a multi-cohort study.” The Journal of antimicrobial chemotherapy vol. 77,3 (2022): 740-746. [CrossRef]
- Santoro, Maria Mercedes et al. “Virological efficacy of switch to DTG plus 3TC in a retrospective observational cohort of suppressed HIV-1 patients with or without past M184V: the LAMRES study.” Journal of global antimicrobial resistance vol. 31 (2022): 52-62. [CrossRef]
- Malagnino, Vincenzo et al. “HbcAb Positivity as a Risk Factor for Missing HIV RNA Undetectability after the 3TC+DTG Switch.” Viruses vol. 16,3 348. 23 Feb. 2024. [CrossRef]
- Fu J, Biao R, Liu Y, Chen J, Zhao H. 24-month outcomes after switching to Dolutegravir/Lamivudine in people living with HIV and HbcAb positivity at the Beijing Ditan Hospital in China. Ann Med. 2025 Dec;57(1):2470957. Epub 2025 Feb 24. PMCID: PMC11852214. [CrossRef] [PubMed]
- Salvo PF, Ciccullo A, Visconti E, Lombardi F, Torti C, Di Giambenedetto S, Baldin G. Impact of HBV serological status on HIV virological efficacy of two-drug antiretroviral regimens: A retrospective observational study on virologically suppressed people with HIV switching to lamivudine/dolutegravir. HIV Med. 2025 Feb 5. Epub ahead of print. [CrossRef] [PubMed]
- Salpini, Romina et al. “Kinetics of hepatitis B virus replication in anti-HBc positive/HbsAg-negative people with HIV switching to tenofovir sparing therapy.” International journal of infectious diseases: IJID: official publication of the International Society for Infectious Diseases vol. 150 (2025): 107294. [CrossRef]
- Gómez-Gonzalo, M et al. “The hepatitis B virus X protein induces HIV-1 replication and transcription in synergy with T-cell activation signals: functional roles of NF-kappaB/NF-AT and SP1-binding sites in the HIV-1 long terminal repeat promoter.” The Journal of biological chemistry vol. 276,38 (2001): 35435-43. [CrossRef]
- De Miguel Buckley R, Rial-Crestelo D, Montejano R, Pinto A, Jimenez-Gonzalez M, Lagarde M, Esteban-Cantos A, Aranguren-Rivas P, Cadiñanos J, Bisbal O, Castro JM, Santacreu-Guerrero M, Bermejo-Plaza L, Moreno V, Hernando A, Martín-Carbonero L, Rubio R, Delgado R, Arribas JR, Pulido F; Antiretroviral Treatment Guided by Proviral Genotype (ART-PRO) Study Group. Long-term Evaluation of Residual Viremia in a Clinical Trial of Dolutegravir Plus Lamivudine as Maintenance Treatment for Participants With and Without Prior Lamivudine Resistance. Open Forum Infect Dis. 2022 Nov 8;9(11):ofac610. PMCID: PMC9697602. [CrossRef] [PubMed]
- Blick G, Cerreta-Dial E, Mancini G, Cosenza A, Fang L. No confirmed virological failures (CVF) for 144 weeks when switching 2-/3-/4-drug ART to DTG/3TC in heavily treatment-experienced PLWHA with prior M184V/I and multiple virological failures in the prospective SOLAR-3D study. Slides presented at: International AIDS Conference; July 22–26, 2024; Munich, Germany. 22 July.
- Borghetti A, Giacomelli A, Borghi V, Ciccullo A, Dusina A, Fabbiani M, Rusconi S, Zazzi M, Mussini C, Di Giambenedetto S. Nucleoside Reverse-Transcriptase Inhibitor Resistance Mutations Predict Virological Failure in Human Immunodeficiency Virus-Positive Patients During Lamivudine Plus Dolutegravir Maintenance Therapy in Clinical Practice. Open Forum Infect Dis. 2021 Mar 6;8(7):ofab103. PMCID: PMC8314943. [CrossRef] [PubMed]
- Borghetti A, Ciccullo A, Lombardi F, Giannarelli D, Passerotto RA, Lamanna F, Carcagnì A, Farinacci D, Dusina A, Baldin G, Zazzi M, Di Giambenedetto S. Efficacy of Lamivudine Plus Dolutegravir vs Dolutegravir-Based 3-Drug Regimens in People With HIV Who Are Virologically Suppressed. Open Forum Infect Dis. 2024 Apr 10;11(5):ofae198. PMCID: PMC11055392. [CrossRef] [PubMed]
- Marcelin AG, Soulie C, Wirden M, Barriere G, Durand F, Charpentier C, Descamps D, Calvez V. Emergent resistance-associated mutations at first- or second-line HIV-1 virologic failure with second-generation InSTIs in two- and three-drug regimens: the Virostar-1 study. J Antimicrob Chemother. 2025 Jan 3;80(1):95-101. PMCID: PMC11695916. [CrossRef] [PubMed]
| Population | N=188 (% or IQR) |
|---|---|
| Male gender (%) | 141 (75.0) |
| Age, years (IQR) | 54 (44-61) |
|
Ethnicity (%) Caucasians Africa-Sub-Saharan South America Asians |
174 (92.5) 4 (2.1) 7 (3.7) 3 (1.6) |
|
HIV acquisition, risk factor (%) Heterosexual men and women MSM People who inject drugs (PWID) Other/unknown |
70 (37.2) 84 (44.7) 14 (7.5) 20 (10.6) |
| Time since HIV diagnosis, years (IQR) | 11 (5-17) |
| Time since ART initiation, years (IQR) | 9 (5-16) |
| Years of virological suppression (IQR) | 5 (3-9) |
| Previous AIDS event, at least one (%) | 35 (18.6) |
| Nadir CD4+ count (cells/μL), (IQR) | 270 (144-385) |
| Baseline CD4+ count (cells/μL), (IQR) | 716 (538-920) |
|
Zenith HIV-RNA (%) <100.000 copies/mL 100,000-499.999 copies/mL ≥500.000 copies/mL |
86 (47.2) 54 (29.7) 42 (23.1) |
|
Baseline HIV-RNA (%) Target not detected Target detected <20 copies/mL 20-49 copies/mL |
110 (58.5) 62 (33.0) 16 (8.5) |
| Positive HCV-Ab serostatus (%) | 19 (10.1) |
| Number of previous therapeutic lines (IQR) | 4 (3-6) |
| HR (95% CI) | p-value | aHR (95% CI) | p-value | |
|---|---|---|---|---|
| Age (per 10 years more) | 1.02 (0.54-1.91) | 0.953 | - | - |
| Sex (female vs male) | 0.44 (0.05-3.60) | 0.440 | - | - |
| Nadir CD4 count | 0.99 (0.99-1.00) | 0.110 | - | - |
| Zenith HIV-RNA | 0.99 (0.99-1.00) | 0.607 | - | - |
| Years with HIV | 1.00 (0.92-1.08) | 0.919 | - | - |
| Years of virological suppression | 0.88 (0.72-1.07) | 0.205 | - | - |
| Baseline HIV-RNA 20-49 copies/ml (versus <20 copies/mL) | 5.67 (1.10- 9.39) | 0.039 | 9.11 (1.05-79.40) | 0.046 |
| GSS*-3TC** (per 10 points more) | 1.74 (1.23-2.48) | 0.002 | 1.57 (1.07-2.29) | 0.023 |
| Pre-switch tenofovir exposure | 1.87 (0.44-7.84) | 0.395 | - | - |
| Anti-HBcAg + (vs negative) | 5.76 (1.26-26.24) | 0.024 | 8.88 (0.89-88.45) | 0.062 |
|
HBV serology: - AntiHBcAg-/AntiHBsAg- - AntiHBcAg-/AntiHBsAg+ - AntiHBcAg+/AntiHBsAg+ - AntiHBcAg+/Anti HBsAg- |
- 1.43 (0.41-5.02) 1.71 (0.41-7.23) 2.69 (0.31-3.30) |
- 0.574 0.466 0.368 |
- - - - |
- - - - |
| Anti-HBcAg + n=45 (%) | Anti-HBcAg - n=135 (%) | p-value | |
|---|---|---|---|
| Sex (male) | 41 (91.1) | 95 (70.3) | 0.005 |
| Age (years, IQR) | 58 (55-61) | 52 (50-54) | 0.002 |
|
Risk factor Hetero MSM IDU Other/Unknown |
11 (24.4) 23 (28.1) 3 (6.6) 8 (1.7) |
55 (40.7) 59 (43.7) 10 (7.4) 11 (8.1) |
0.120 |
| Years with HIV (IQR) | 14.43 (11.64-17.23) | 11.74 (10.31-13.18) | 0.072 |
| Years of suppression (IQR) | 7.27 (5.37-9.18) | 5.85 (5.09-6.62) | 0.101 |
| CD4 baseline (IQR) | 644 (493-857) | 734 (548-947) | 0.109 |
| HIV-RNA detectable (20-49 copies/mL) | 4 (8.8) | 11 (8.1) | 0.987 |
| Tenofovir exposure pre-switch | 15 (33.3) | 72 (53.3) | 0.020 |
| Previous virological failure | 13 (28.8) | 32 (23.7) | 0.651 |
| 3TC* resistance associated mutations | 2 (4.4) | 3 (2.2) | 0.695 |
| aHR (95% CI) | p-value | |
|---|---|---|
|
Previous tenofovir use and occult infection: - No prior tenofovir plus anti-HBcAg– - Prior tenofovir plus anti-HBcAg – - No prior tenofovir plus anti-HBcAg+ - Prior tenofovir plus anti-HBcAg+ |
Reference 1.51 (0.13-16.92) 2.62 (0.14-47.41) 15.06 (1.40-161.38) |
Reference 0.738 0.513 0.025 |
| Age (per 10 years more) | 0.93 (0.43-2.04) | 0.859 |
| Sex (female vs. male) | NA | NA |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





