Submitted:
07 October 2025
Posted:
08 October 2025
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
2.1. Participants
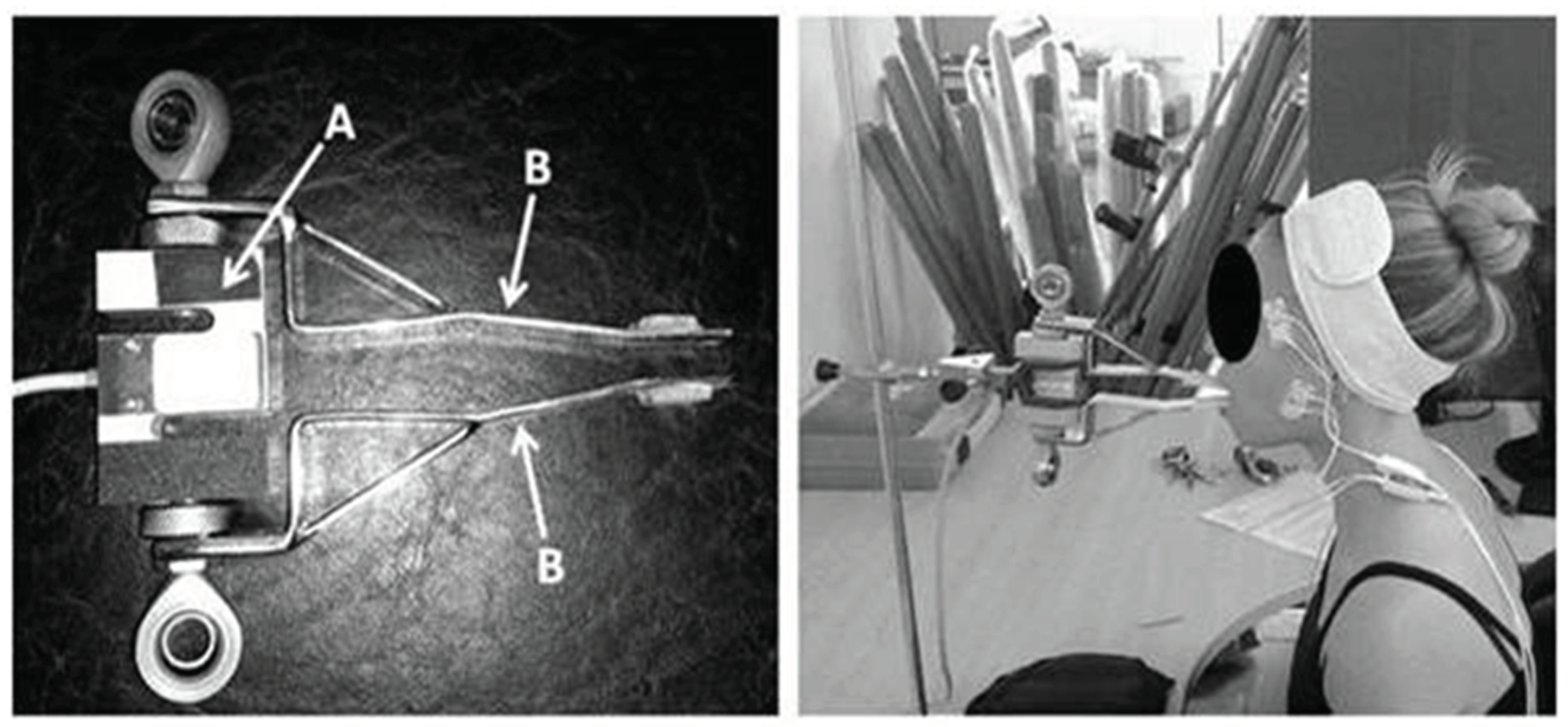
2.2. Equipment
2.3. Experimental Protocol
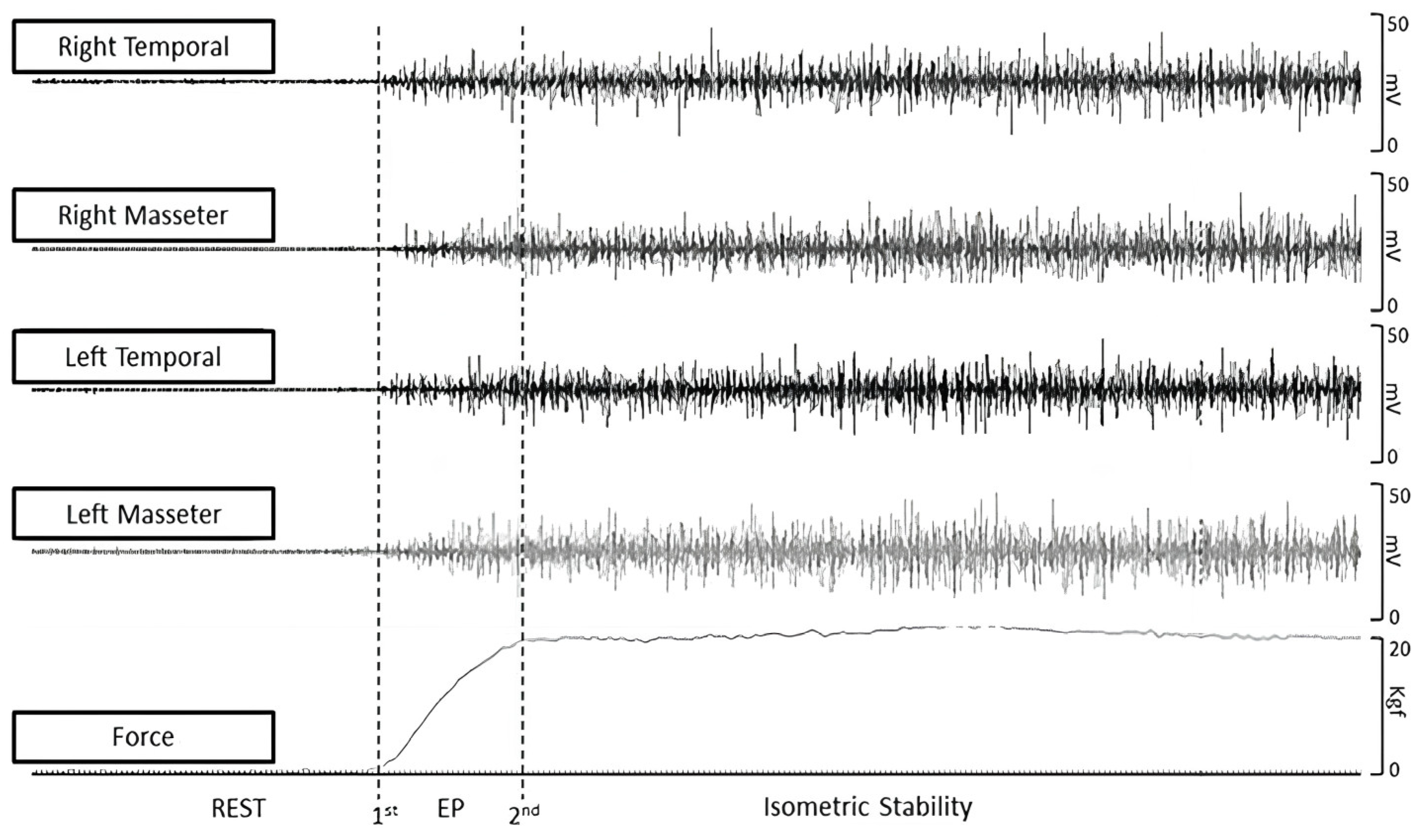
2.4. Data Extraction
2.5. Raters
2.6. Statistical Analysis
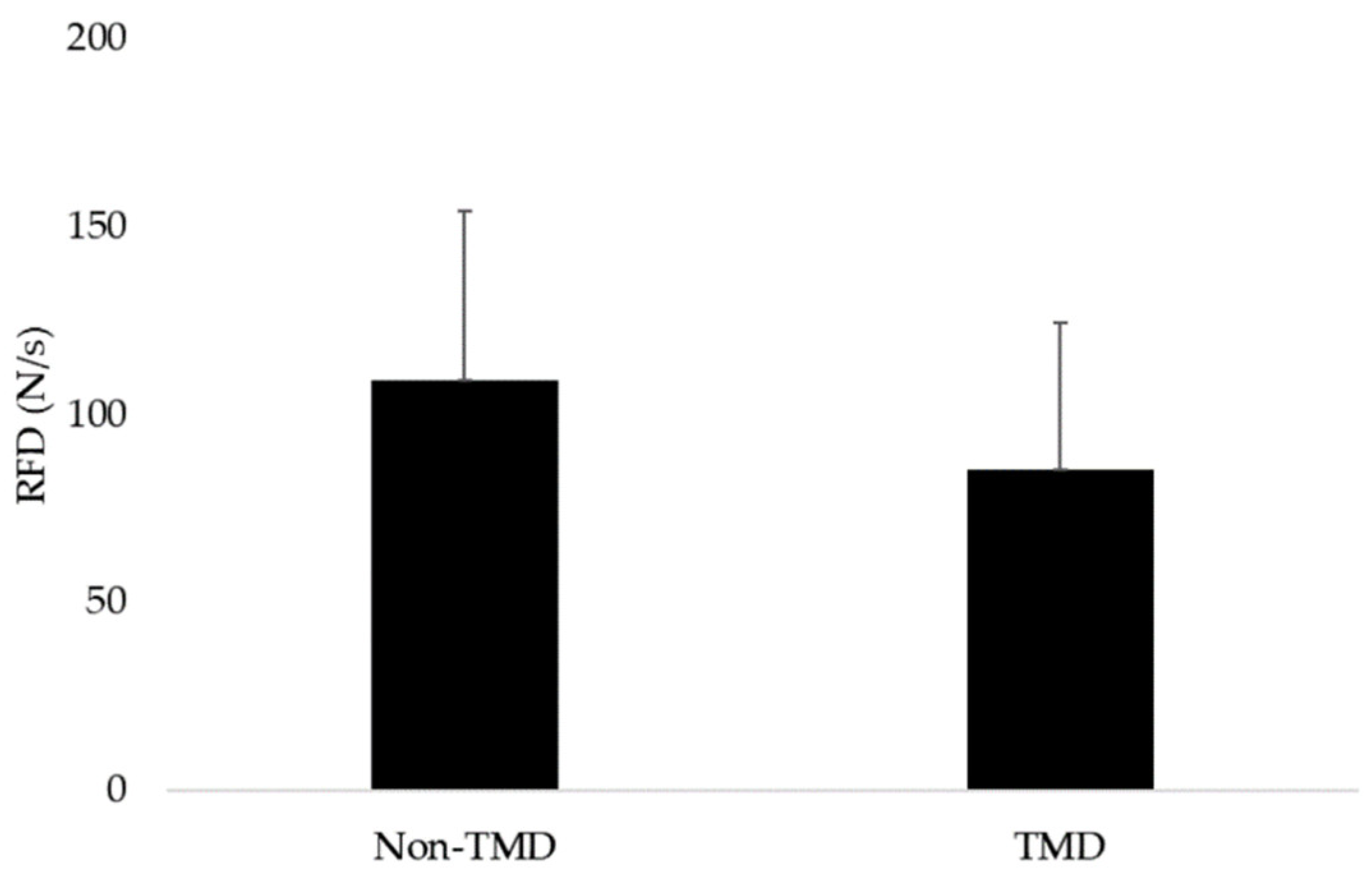
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Abbass, M.M.S.; Rady, D.; El Moshy, S.; Ahmed Radwan, I.; Wadan, A.H.S.; Dörfer, C.E.; El-Sayed, K.M.F. The Temporomandibular Joint and the Human Body: A New Perspective on Cross Talk. Dent J (Basel) 2024, 12. [Google Scholar] [CrossRef]
- Thirunavukarasu, A.J.; Ferro, A.; Sardesai, A.; Biyani, G.; Dubb, S.S.; Brassett, C.; Hamilton, D.L. Temporomandibular Joint Anatomy: Ultrasonographic Appearances and Sexual Dimorphism. Clinical Anatomy 2021, 34, 1043–1049. [Google Scholar] [CrossRef] [PubMed]
- Camacho, G.B.; Waldemarin, R. de A.; Barbin, E.L. Temporomandibular Disorder in Adults: Retrospective Study. Brazilian Journal Of Pain 2021, 4. [Google Scholar] [CrossRef]
- Herrera-Valencia, A.; Ruiz-Muñoz, M.; Martin-Martin, J.; Cuesta-Vargas, A.; González-Sánchez, M. Efficacy of Manual Therapy in Temporomandibular Joint Disorders and Its Medium-and Long-Term Effects on Pain and Maximum Mouth Opening: A Systematic Review and Meta-Analysis. J Clin Med 2020, 9, 1–14. [Google Scholar] [CrossRef]
- Whyte, A.; Phoon Nguyen, A.; Boeddinghaus, R.; Balasubramaniam, R. Imaging of Temporomandibular Disorder and Its Mimics. J Med Imaging Radiat Oncol 2021, 65, 70–78. [Google Scholar] [CrossRef]
- Vallin, S.; Liv, P.; Häggman-Henrikson, B.; Visscher, C.M.; Lobbezoo, F.; Lövgren, A. Temporomandibular Disorder Pain Is Associated with Increased Sick Leave and Reduced Health Related Quality of Life. European Journal of Pain (United Kingdom) 2024, 28. [Google Scholar] [CrossRef]
- Qamar, Z.; Alghamdi, A.M.S.; Haydarah, N.K. Bin; Balateef, A.A.; Alamoudi, A.A.; Abumismar, M.A.; Shivakumar, S.; Cicciù, M.; Minervini, G. Impact of Temporomandibular Disorders on Oral Health-Related Quality of Life: A Systematic Review and Meta-Analysis. J Oral Rehabil 2023, 50, 706–714. [Google Scholar] [CrossRef]
- Fassicollo, C.E.; Garcia, D.M.; Machado, B.C.Z.; de Felício, C.M. Changes in Jaw and Neck Muscle Coactivation and Coordination in Patients with Chronic Painful TMD Disk Displacement with Reduction during Chewing. Physiol Behav 2021, 230. [Google Scholar] [CrossRef]
- Ferrillo, M.; Migliario, M.; Marotta, N.; Fortunato, F.; Bindi, M.; Pezzotti, F.; Ammendolia, A.; Giudice, A.; Foglio Bonda, P.L.; de Sire, A. Temporomandibular Disorders and Neck Pain in Primary Headache Patients: A Retrospective Machine Learning Study. Acta Odontol Scand 2023, 81, 151–157. [Google Scholar] [CrossRef]
- Valesan, L.F.; Da-Cas, C.D.; Réus, J.C.; Denardin, A.C.S.; Garanhani, R.R.; Bonotto, D.; Januzzi, E.; de Souza, B.D.M. Prevalence of Temporomandibular Joint Disorders: A Systematic Review and Meta-Analysis. Clin Oral Investig 2021, 25, 441–453. [Google Scholar] [CrossRef]
- Bednarczyk, V.; Proulx, F.; Paez, A. The Effectiveness of Cervical Rehabilitation Interventions for Pain in Adults with Myogenic Temporomandibular Disorders: A Systematic Review and Meta-Analysis. J Oral Rehabil 2024, 51, 1091–1107. [Google Scholar] [CrossRef]
- Silva Andresen Strini, P.J.; Silva Andresen Strini, P.J.; De Souza Barbosa, T.; Duarte Gavião, M.B. Assessment of Thickness and Function of Masticatory and Cervical Muscles in Adults with and without Temporomandibular Disorders. Arch Oral Biol 2013, 58, 1100–1108. [Google Scholar] [CrossRef] [PubMed]
- Marcelino, V.; De Rovere, S.; Paço, M.; Gonçalves, M.; Marcelino, S.; Guimarães, A.S.; Pinho, T. Masticatory Function in Individuals with Temporomandibular Disorders: A Systematic Review and Meta-Analysis. Life 2023, 13. [Google Scholar] [CrossRef]
- Liu, Z.J.; Yamagata, K.; Kasahara, Y.; Ito, G. Electromyographic Examination of Jaw Muscles in Relation to Symptoms and Occlusion of Patients with Temporomandibular Joint Disorders. J Oral Rehabil 1999, 26, 33–47. [Google Scholar] [CrossRef]
- Suzuki, S.; Castrillon, E.E.; Arima, T.; Kitagawa, Y.; Svensson, P. Blood Oxygenation of Masseter Muscle during Sustained Elevated Muscle Activity in Healthy Participants. J Oral Rehabil 2016, 43, 900–910. [Google Scholar] [CrossRef]
- Xu, L.; Fan, S.; Cai, B.; Fang, Z.; Jiang, X. Influence of Sustained Submaximal Clenching Fatigue Test on Electromyographic Activity and Maximum Voluntary Bite Forces in Healthy Subjects and Patients with Temporomandibular Disorders. J Oral Rehabil 2017, 44, 340–346. [Google Scholar] [CrossRef]
- Gay, T.; Maton, B.; Rendell, J.; Majourau, A. Characteristics of Muscle Fatigue in Patients with Myofascial Pain-Dysfunction Syndrome. Arch Oral Biol 1994, 39, 847–852. [Google Scholar] [CrossRef]
- Machado, M.B.; Nitsch, G.S.; Pitta, N.C.; Oliveira, A.S. de Tempo de Ativação Muscular Em Portadoras de Disfunção Temporomandibular Durante a Mastigação. Audiology - Communication Research 2014, 19, 202–207. [Google Scholar] [CrossRef]
- Szyszka-Sommerfeld, L.; Sycińska-Dziarnowska, M.; Spagnuolo, G.; Woźniak, K. Surface Electromyography in the Assessment of Masticatory Muscle Activity in Patients with Pain-Related Temporomandibular Disorders: A Systematic Review. Front Neurol 2023, 14. [Google Scholar] [CrossRef]
- Dorosz, T.; Mańko, A.; Ginszt, M. Use of Surface Electromyography to Evaluate Effects of Therapeutic Methods on Masticatory Muscle Activity in Patients with Temporomandibular Disorders: A Narrative Review. J Clin Med 2024, 13. [Google Scholar] [CrossRef]
- Shousha, T.; Alayat, M.; Moustafa, I. Effects of Low-Level Laser Therapy versus Soft Occlusive Splints on Mouth Opening and Surface Electromyography in Females with Temporomandibular Dysfunction: A Randomized-Controlled Study. PLoS One 2021, 16. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, M.C.; Porto de Toledo, I.; Dutra, K.L.; Stefani, F.M.; Porporatti, A.L.; Flores-Mir, C.; De Luca Canto, G. Association between Chewing Dysfunctions and Temporomandibular Disorders: A Systematic Review. J Oral Rehabil 2018, 45, 819–835. [Google Scholar] [CrossRef] [PubMed]
- Moxley, B.; Stevens, W.; Sneed, J.; Pearl, C. Novel Diagnostic and Therapeutic Approaches to Temporomandibular Dysfunction: A Narrative Review. Life 2023, 13. [Google Scholar] [CrossRef]
- Dinsdale, A.; Liang, Z.; Thomas, L.; Treleaven, J. Are Jaw Range of Motion, Muscle Function and Proprioception Impaired in Adults with Persistent Temporomandibular Disorders? A Systematic Review and Meta-Analysis. J Oral Rehabil 2020, 47, 1448–1478. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, C.L.P.; Machado, B.C.Z.; Borges, C.G.P.; Rodrigues Da Silva, M.A.M.; Sforza, C.; De Felício, C.M. Impaired Orofacial Motor Functions on Chronic Temporomandibular Disorders. Journal of Electromyography and Kinesiology 2014, 24, 565–571. [Google Scholar] [CrossRef]
- Avivi-Arber, L.; Martin, R.; Lee, J.C.; Sessle, B.J. Face Sensorimotor Cortex and Its Neuroplasticity Related to Orofacial Sensorimotor Functions. Arch Oral Biol 2011, 56, 1440–1465. [Google Scholar] [CrossRef]
- Minami, I.; Akhter, R.; Albersen, I.; Burger, C.; Whittle, T.; Lobbezoo, F.; Peck, C.C.; Murray, G.M. Masseter Motor Unit Recruitment Is Altered in Experimental Jaw Muscle Pain. J Dent Res 2013, 92, 143–148. [Google Scholar] [CrossRef]
- Tartaglia, G.M.; Lodetti, G.; Paiva, G.; Felicio, C.M. De; Sforza, C. Surface Electromyographic Assessment of Patients with Long Lasting Temporomandibular Joint Disorder Pain. Journal of Electromyography and Kinesiology 2011, 21, 659–664. [Google Scholar] [CrossRef]
- Zwiri, A.; Al-Hatamleh, M.A.I.; Ahmad, W.M.A.W.; Asif, J.A.; Khoo, S.P.; Husein, A.; Ab-Ghani, Z.; Kassim, N.K. Biomarkers for Temporomandibular Disorders: Current Status and Future Directions. Diagnostics 2020, 10. [Google Scholar] [CrossRef]
- Pitta, N.C.; Nitsch, G.S.; Machado, M.B.; de Oliveira, A.S. Activation Time Analysis and Electromyographic Fatigue in Patients with Temporomandibular Disorders during Clenching. Journal of Electromyography and Kinesiology 2015, 25, 653–657. [Google Scholar] [CrossRef]
- Rodríguez-Rosell, D.; Pareja-Blanco, F.; Aagaard, P.; González-Badillo, J.J. Physiological and Methodological Aspects of Rate of Force Development Assessment in Human Skeletal Muscle. Clin Physiol Funct Imaging 2018, 38, 743–762. [Google Scholar] [CrossRef] [PubMed]
- Khawaja, S.N.; Mccall, W.; Dunford, R.; Nickel, J.C.; Iwasaki, L.R.; Crow, H.C.; Gonzalez, Y. Infield Masticatory Muscle Activity in Subjects with Pain-Related Temporomandibular Disorders Diagnoses. Orthod Craniofac Res 2015, 18, 137–145. [Google Scholar] [CrossRef] [PubMed]
- Alam, M.K.; Zaman, M.U.; Alqhtani, N.R.; Alqahtani, A.S.; Alqahtani, F.; Cicciù, M.; Minervini, G. Salivary Biomarkers and Temporomandibular Disorders: A Systematic Review Conducted According to PRISMA Guidelines and the Cochrane Handbook for Systematic Reviews of Interventions. J Oral Rehabil 2024, 51, 416–426. [Google Scholar] [CrossRef] [PubMed]
- Ernberg, M. The Role of Molecular Pain Biomarkers in Temporomandibular Joint Internal Derangement. J Oral Rehabil 2017, 44, 481–491. [Google Scholar] [CrossRef]
- Soares, J.M.; Carneiro, B.D.; Pozza, D.H. The Role of Biomarkers in Temporomandibular Disorders: A Systematic Review. International Journal of Molecular Sciences 2025, Vol. 26, Page 5971 2025, 26, 5971. [Google Scholar] [CrossRef]
- Ginszt, M.; Zieliński, G. Novel Functional Indices of Masticatory Muscle Activity. J Clin Med 2021, 10. [Google Scholar] [CrossRef]
- Nickel, J.C.; Gonzalez, Y.M.; Liu, Y.; Liu, H.; Gallo, L.M.; Iwasaki, L.R. Mechanics- and Behavior-Related Temporomandibular Joint Differences. J Dent Res 2024, 103, 1083–1090. [Google Scholar] [CrossRef]
- Carvalho, C.R.; Fernández, J.M.; del-Ama, A.J.; Oliveira Barroso, F.; Moreno, J.C. Review of Electromyography Onset Detection Methods for Real-Time Control of Robotic Exoskeletons. J Neuroeng Rehabil 2023, 20. [Google Scholar] [CrossRef]
- Farinelli, V.; Bolzoni, F.; Marchese, S.M.; Esposti, R.; Cavallari, P. A Novel Viewpoint on the Anticipatory Postural Adjustments During Gait Initiation. Front Hum Neurosci 2021, 15. [Google Scholar] [CrossRef]
- Pereira, S.; Silva, C.C.; Ferreira, S.; Silva, C.; Oliveira, N.; Santos, R.; Vilas-Boas, J.P.; Correia, M. V. Anticipatory Postural Adjustments during Sitting Reach Movement in Post-Stroke Subjects. Journal of Electromyography and Kinesiology 2014, 24, 165–171. [Google Scholar] [CrossRef]
- Kuntamukkula, S.; Sinha, R.; Tiwari, P.K.; Paul, D. Dynamic Stability Assessment of the Temporomandibular Joint as a Sequela of Open Reduction and Internal Fixation of Unilateral Condylar Fracture. Journal of Oral and Maxillofacial Surgery 2018, 76, 2598–2609. [Google Scholar] [CrossRef]
- Basit, H.; Eovaldi, B.J.; Siccardi, M.A. Anatomy, Head and Neck, Mastication Muscles. StatPearls 2023. [Google Scholar]
- Dinsdale, A.; Liang, Z.; Thomas, L.; Treleaven, J. Is Jaw Muscle Activity Impaired in Adults with Persistent Temporomandibular Disorders? A Systematic Review and Meta-Analysis. J Oral Rehabil 2021, 48, 487–516. [Google Scholar] [CrossRef] [PubMed]
- Panhan, A.C.; Gonçalves, M.; Eltz, G.D.; Villalba, M.M.; Cardozo, A.C.; Bérzin, F. Neuromuscular Efficiency of the Multifidus Muscle in Pilates Practitioners and Non-Practitioners. Complement Ther Med 2018, 40, 61–63. [Google Scholar] [CrossRef] [PubMed]
- Paula, J.P. de; Navega, M.T.; Spinoso, D.H. Neuromuscular Efficiency of the Quadriceps in Women with and without Patellofemoral Pain. Fisioterapia e Pesquisa 2023, 30. [Google Scholar] [CrossRef]
- Aragão, F.A.; Schäfer, G.S.; De Albuquerque, C.E.; Fonseca Vituri, R.; Mícolis De Azevedo, F.; Ricardo, G.; Bertolini, F. Neuromuscular Efficiency of the Vastus Lateralis and Biceps Femoris Muscles in Individuals with Anterior Cruciate Ligament Injuries. Rev Bras Ortop (Sao Paulo) 2015, 50, 180–185. [Google Scholar] [CrossRef]
- Tesch, P.A.; Dudley, G.A.; Duvoisin, M.R.; Hather, B.M.; Harris, R.T. Force and EMG Signal Patterns during Repeated Bouts of Concentric or Eccentric Muscle Actions. Acta Physiol Scand 1990, 138, 263–271. [Google Scholar] [CrossRef]
- Del Vecchio, A. Neuromechanics of the Rate of Force Development. Exerc Sport Sci Rev 2023, 51, 34–42. [Google Scholar] [CrossRef]
- D’Emanuele, S.; Maffiuletti, N.A.; Tarperi, C.; Rainoldi, A.; Schena, F.; Boccia, G. Rate of Force Development as an Indicator of Neuromuscular Fatigue: A Scoping Review. Front Hum Neurosci 2021, 15. [Google Scholar] [CrossRef]
- Del Vecchio, A.; Negro, F.; Holobar, A.; Casolo, A.; Folland, J.P.; Felici, F.; Farina, D. You Are as Fast as Your Motor Neurons: Speed of Recruitment and Maximal Discharge of Motor Neurons Determine the Maximal Rate of Force Development in Humans. Journal of Physiology 2019, 597, 2445–2456. [Google Scholar] [CrossRef]
- Maffiuletti, N.A.; Aagaard, P.; Blazevich, A.J.; Folland, J.; Tillin, N.; Duchateau, J. Rate of Force Development: Physiological and Methodological Considerations. Eur J Appl Physiol 2016, 116, 1091–1116. [Google Scholar] [CrossRef]
- Lis, D.M.; Jordan, M.; Lipuma, T.; Smith, T.; Schaal, K.; Baar, K. Collagen and Vitamin C Supplementation Increases Lower Limb Rate of Force Development. Int J Sport Nutr Exerc Metab 2022, 32, 65–73. [Google Scholar] [CrossRef] [PubMed]
- Kozinc, Ž.; Smajla, D.; Šarabon, N. The Rate of Force Development Scaling Factor: A Review of Underlying Factors, Assessment Methods and Potential for Practical Applications. Eur J Appl Physiol 2022, 122, 861–873. [Google Scholar] [CrossRef] [PubMed]
- Del Vecchio, X.A.; Negro, X.F.; Falla, D.; Bazzucchi, I.; Farina, X.D.; Felici, F.; Vecchio, D.A. Higher Muscle Fiber Conduction Velocity and Early Rate of Torque Development in Chronically Strength-Trained Individuals. J Appl Physiol 2018, 125, 1218–1226. [Google Scholar] [CrossRef]
- Barbosa, M.A.; Tahara, A.K.; Ferreira, I.C.; Intelangelo, L.; Barbosa, A.C. Effects of 8 Weeks of Masticatory Muscles Focused Endurance Exercises on Women with Oro-Facial Pain and Temporomandibular Disorders: A Placebo Randomised Controlled Trial. J Oral Rehabil 2019, 46, 885–894. [Google Scholar] [CrossRef]
- Berni, K.C. dos S.; Dibai-Filho, A.V.; Pires, P.F.; Rodrigues-Bigaton, D. Accuracy of the Surface Electromyography RMS Processing for the Diagnosis of Myogenous Temporomandibular Disorder. Journal of Electromyography and Kinesiology 2015, 25, 596–602. [Google Scholar] [CrossRef]
- Rice, D.A.; Mannion, J.; Lewis, G.N.; McNair, P.J.; Fort, L. Experimental Knee Pain Impairs Joint Torque and Rate of Force Development in Isometric and Isokinetic Muscle Activation. Eur J Appl Physiol 2019, 119, 2065–2073. [Google Scholar] [CrossRef]
- Peñailillo, L.; Blazevich, A.; Numazawa, H.; Nosaka, K. Rate of Force Development as a Measure of Muscle Damage. Scand J Med Sci Sports 2015, 25, 417–427. [Google Scholar] [CrossRef]
- Maffiuletti, N.A.; Bizzini, M.; Widler, K.; Munzinger, U. Asymmetry in Quadriceps Rate of Force Development as a Functional Outcome Measure in TKA. Clin Orthop Relat Res 2009, 468, 191. [Google Scholar] [CrossRef]
- Asquini, G.; Pisacane, G.; Maselli, F.; Galeoto, G.; Mourad, F.; Bizzarri, P.; Balli, E.; Bagnoli, C.; Manzari, A.; Pernici, M.; et al. Effectiveness of Resistance Training of Masticatory Muscles for Patients with Temporomandibular Disorders: Protocol for a Systematic Review. BMJ Open 2024, 14, e083133. [Google Scholar] [CrossRef]
- Mapelli, A.; Zanandréa Machado, B.C.; Giglio, L.D.; Sforza, C.; De Felício, C.M. Reorganization of Muscle Activity in Patients with Chronic Temporomandibular Disorders. Arch Oral Biol 2016, 72, 164–171. [Google Scholar] [CrossRef]
- Folland, J.P.; Buckthorpe, M.W.; Hannah, R. Human Capacity for Explosive Force Production: Neural and Contractile Determinants. Scand J Med Sci Sports 2014, 24, 894–906. [Google Scholar] [CrossRef] [PubMed]
- Nunes, G.S.; Barton, C.J.; Serrão, F.V. Hip Rate of Force Development and Strength Are Impaired in Females with Patellofemoral Pain without Signs of Altered Gluteus Medius and Maximus Morphology. J Sci Med Sport 2018, 21, 123–128. [Google Scholar] [CrossRef] [PubMed]
- Balshaw, T.G.; Massey, G.J.; Maden-Wilkinson, T.M.; Lanza, M.B.; Folland, J.P. Effect of Long-Term Maximum Strength Training on Explosive Strength, Neural, and Contractile Properties. Scand J Med Sci Sports 2022, 32, 685–697. [Google Scholar] [CrossRef] [PubMed]
- Isola, G.; Anastasi, G.P.; Matarese, G.; Williams, R.C.; Cutroneo, G.; Bracco, P.; Piancino, M.G. Functional and Molecular Outcomes of the Human Masticatory Muscles. Oral Dis 2018, 24, 1428–1441. [Google Scholar] [CrossRef]
- Korfage, J.A.M.; Brugman, P.; Van Eijden, T.M.G.J. Intermuscular and Intramuscular Differences in Myosin Heavy Chain Composition of the Human Masticatory Muscles. J Neurol Sci 2000, 178, 95–106. [Google Scholar] [CrossRef]
- Desai, A.P.; Roy, S.K.; Semi, R.S.; Balasundaram, T. Efficacy of Low-Level Laser Therapy in Management of Temporomandibular Joint Pain: A Double Blind and Placebo Controlled Trial. J Maxillofac Oral Surg 2022, 21, 948–956. [Google Scholar] [CrossRef]
- Zieliński, G.; Byś, A.; Szkutnik, J.; Majcher, P.; Ginszt, M. Electromyographic Patterns of Masticatory Muscles in Relation to Active Myofascial Trigger Points of the Upper Trapezius and Temporomandibular Disorders. Diagnostics 2021, 11. [Google Scholar] [CrossRef]
- Lund, J.P.; Donga, R.; Widmer, C.G.; Stohler, C.S. The Pain-Adaptation Model: A Discussion of the Relationship between Chronic Musculoskeletal Pain and Motor Activity. Can J Physiol Pharmacol 1991, 69, 683–694. [Google Scholar] [CrossRef]
- Peck, C.C.; Murray, G.M.; Gerzina, T.M. How Does Pain Affect Jaw Muscle Activity? The Integrated Pain Adaptation Model. Aust Dent J 2008, 53, 201–207. [Google Scholar] [CrossRef]
- Tucker, K.J.; Hodges, P.W. Changes in Motor Unit Recruitment Strategy during Pain Alters Force Direction. European Journal of Pain 2010, 14, 932–938. [Google Scholar] [CrossRef] [PubMed]
- Kyun Sohn, M.; Graven-Nielsen, T.; Arendt-Nielsen, L.; Svensson, P. INHIBITION OF MOTOR UNIT FIRING DURING EXPERIMENTAL MUSCLE PAIN IN HUMANS; 2000; Vol. 23;
- Martinez-Valdes, E.; Negro, F.; Farina, D.; Falla, D. Divergent Response of Low- versus High-Threshold Motor Units to Experimental Muscle Pain. Journal of Physiology 2020, 598, 2093–2108. [Google Scholar] [CrossRef] [PubMed]
- Dubner, R.; Slade, G.D.; Ohrbach, R.; Greenspan, J.D.; Fillingim, R.B.; Bair, E.; Sanders, A.E.; Diatchenko, L.; Meloto, C.B.; Smith, S.; et al. Painful Temporomandibular Disorder: Decade of Discovery from OPPERA Studies. J Dent Res 2016, 95, 1084–1092. [Google Scholar] [CrossRef]
- Öçal, M.Ç.; Baybars, S.C.; Talu, M.H. The Relationship Between Anxiety and Masseter Muscle in Temporomandibular Disorders: An Ultrasonographic Assessment. Journal of Clinical Ultrasound 2025. [Google Scholar] [CrossRef]
- Fillingim, R.B.; Slade, G.D.; Greenspan, J.D.; Dubner, R.; Maixner, W.; Bair, E.; Ohrbach, R. Long-Term Changes in Biopsychosocial Characteristics Related to Temporomandibular Disorder: Findings from the OPPERA Study. Pain 2018, 159, 2403. [Google Scholar] [CrossRef]
- Pereira, Y.C.L.; Nascimento, G.C.; Iyomasa, D.M.; Fernández, R.A.R.; Calzzani, R.A.; Leite-Panissi, C.R.A.; Novaes, P.D.; Iyomasa, M.M. Exodontia-Induced Muscular Hypofunction by Itself or Associated to Chronic Stress Impairs Masseter Muscle Morphology and Its Mitochondrial Function. Microsc Res Tech 2019, 82, 530–537. [Google Scholar] [CrossRef]
- Ispir, N.G.; Toraman, M. The Relationship of Masseter Muscle Thickness with Face Morphology and Parafunctional Habits: An Ultrasound Study. Dentomaxillofacial Radiology 2022, 51. [Google Scholar] [CrossRef]
- Akkoca, F.; Ozyurek, S.; Ilhan, G.; Koyuncu, E.; Ozdede, M. Role of the Masseter, Anterior Temporalis, and Sternocleidomastoid Muscles in Myofascial Temporomandibular Disorder Pain: Evaluation of Thickness and Stiffness by Ultrasonography. Oral Radiol 2025, 41, 363–371. [Google Scholar] [CrossRef]
- Andersen, L.L.; Andersen, J.L.; Zebis, M.K.; Aagaard, P. Early and Late Rate of Force Development: Differential Adaptive Responses to Resistance Training? Scand J Med Sci Sports 2010, 20, e162–e169. [Google Scholar] [CrossRef]
- Ferreira, C.L.P.; Bellistri, G.; Montagna, S.; de Felício, C.M.; Sforza, C. Patients with Myogenic Temporomandibular Disorders Have Reduced Oxygen Extraction in the Masseter Muscle. Clin Oral Investig 2017, 21, 1509–1518. [Google Scholar] [CrossRef]
- Niszezak, C.M.; Sonza, A.; Garrett, A.; Santos, G.M. Muscle Oxygenation and Pain in Different Types of Temporomandibular Disorders. Clin Oral Investig 2024, 28. [Google Scholar] [CrossRef] [PubMed]
- Puel, A.N.; da Silva Paes, A.G.; Macedo, C.; Miranda, L.S.; Graciosa, M.; Sonza, A. Peripheral Muscle Oxygenation and Symptoms of Stress in Adolescents with and without Temporomandibular Disorder. Clin Oral Investig 2023, 27, 1509–1517. [Google Scholar] [CrossRef]
- Anthierens, A.; Thevenon, A.; Olivier, N.; Mucci, P. Paraspinal Muscle Oxygenation and Mechanical Efficiency Are Reduced in Individuals with Chronic Low Back Pain. Sci Rep 2024, 14, 4943. [Google Scholar] [CrossRef]
- Hughes, D.C.; Ellefsen, S.; Baar, K. Adaptations to Endurance and Strength Training. Cold Spring Harb Perspect Med 2018, 8, a029769. [Google Scholar] [CrossRef]
- Testa, M.; Geri, T.; Pitance, L.; Lentz, P.; Gizzi, L.; Erlenwein, J.; Petkze, F.; Falla, D. Alterations in Jaw Clenching Force Control in People with Myogenic Temporomandibular Disorders. Journal of Electromyography and Kinesiology 2018, 43, 111–117. [Google Scholar] [CrossRef]
- Iturriaga, V.; Bornhardt, T.; Velasquez, N. Temporomandibular Joint: Review of Anatomy and Clinical Implications. Dent Clin North Am 2023, 67, 199–209. [Google Scholar] [CrossRef]
- Dieterich, A. V.; Botter, A.; Vieira, T.M.; Peolsson, A.; Petzke, F.; Davey, P.; Falla, D. Spatial Variation and Inconsistency between Estimates of Onset of Muscle Activation from EMG and Ultrasound. Sci Rep 2017, 7, 1–11. [Google Scholar] [CrossRef]
- Frost, L.R.; Brown, S.H.M. Muscle Activation Timing and Balance Response in Chronic Lower Back Pain Patients with Associated Radiculopathy. Clinical Biomechanics 2016, 32, 124–130. [Google Scholar] [CrossRef]
- Hodges, P.W.; Moseley, G.L.; Gabrielsson, A.; Gandevia, S.C. Experimental Muscle Pain Changes Feedforward Postural Responses of the Trunk Muscles. Exp Brain Res 2003, 151, 262–271. [Google Scholar] [CrossRef]
- López-González, L.; Falla, D.; Lázaro-Navas, I.; Lorenzo-Sánchez-aguilera, C.; Rodríguez-Costa, I.; Pecos-Martín, D.; Gallego-Izquierdo, T. Effects of Dry Needling on Neuromuscular Control of Ankle Stabilizer Muscles and Center of Pressure Displacement in Basketball Players with Chronic Ankle Instability: A Single-Blinded Randomized Controlled Trial. International Journal of Environmental Research and Public Health 2021, Vol. 18, Page 2092 2021, 18, 2092. [Google Scholar] [CrossRef]
| Muscle | Group | Pre-activation n (%) |
Post-Activation n (%) |
Normal Activation n (%) |
p | Cramér’s V |
|---|---|---|---|---|---|---|
| LM | With TMD | 7 (58.3%) | 16 (59.3%) | 18 (78.3%) | 0.30 | 0.19 |
| Without TMD | 5 (41.7%) | 11 (40.7%) | 5 (21.7%) | |||
| RM | With TMD | 8 (61.5%) | 17 (65.4%) | 15 (68.2%) | 0.92 | 0.05 |
| Without TMD | 5 (38.5%) | 9 (34.6%) | 7 (31.8%) | |||
| LT | With TMD | 10 (76.9%) | 15 (65.2%) | 16 (61.5%) | 0.62 | 0.12 |
| Without TMD | 3 (23.1%) | 8 (34.8%) | 10 (38.5%) | |||
| RT | With TMD | 8 (80.0%) | 14 (58.3%) | 17 (65.4%) | 0.48 | 0.15 |
| Without TMD | 2 (20.0%) | 10 (41.7%) | 9 (34.6%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





