Submitted:
01 October 2025
Posted:
02 October 2025
You are already at the latest version
Abstract
Keywords:
1. Introduction
- To systematically review the literature on terminology used for fractures associated with implants.
- To quantify the heterogeneity of terminology across anatomical sites and time.
- To propose and critically appraise a unifying descriptor—“artificial fracture”—as a potential bridge term.
2. Materials and Methods
- “periprosthetic fracture”
- “peri-implant fracture”
- “implant-related fracture”
- “hardware-related fracture”
- Inclusion: clinical studies, reviews, registry analyses, consensus papers using or explicitly discussing fracture terminology related to implants.
- Exclusion: basic science, animal studies, biomechanical models without clinical context, case reports < 5 patients.
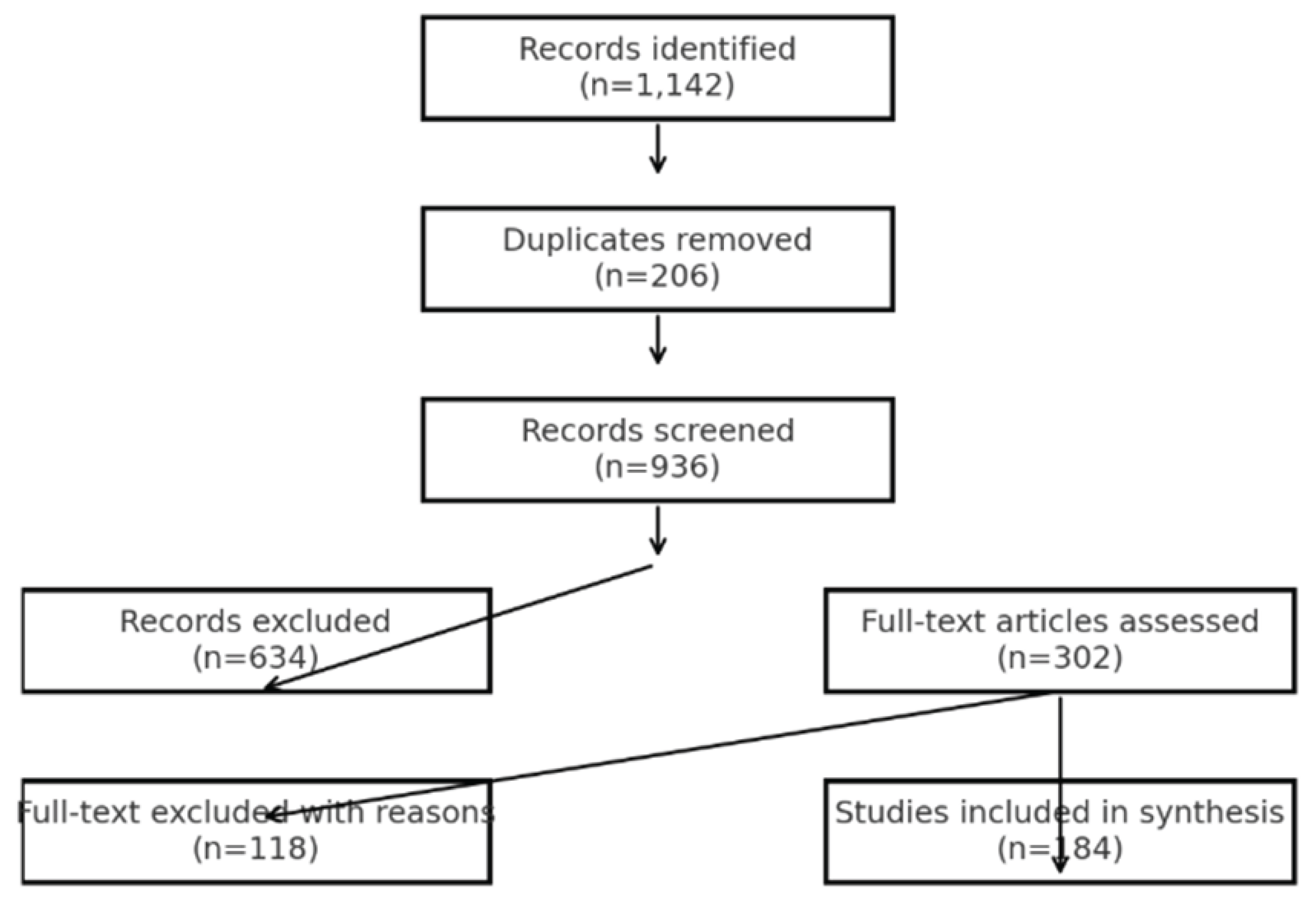
- Records identified: 1142
- After duplicates removed: 936
- Full-text screened: 302
- Excluded with reasons: 118
- Studies included: 184
3. Results
This PRISMA Flow
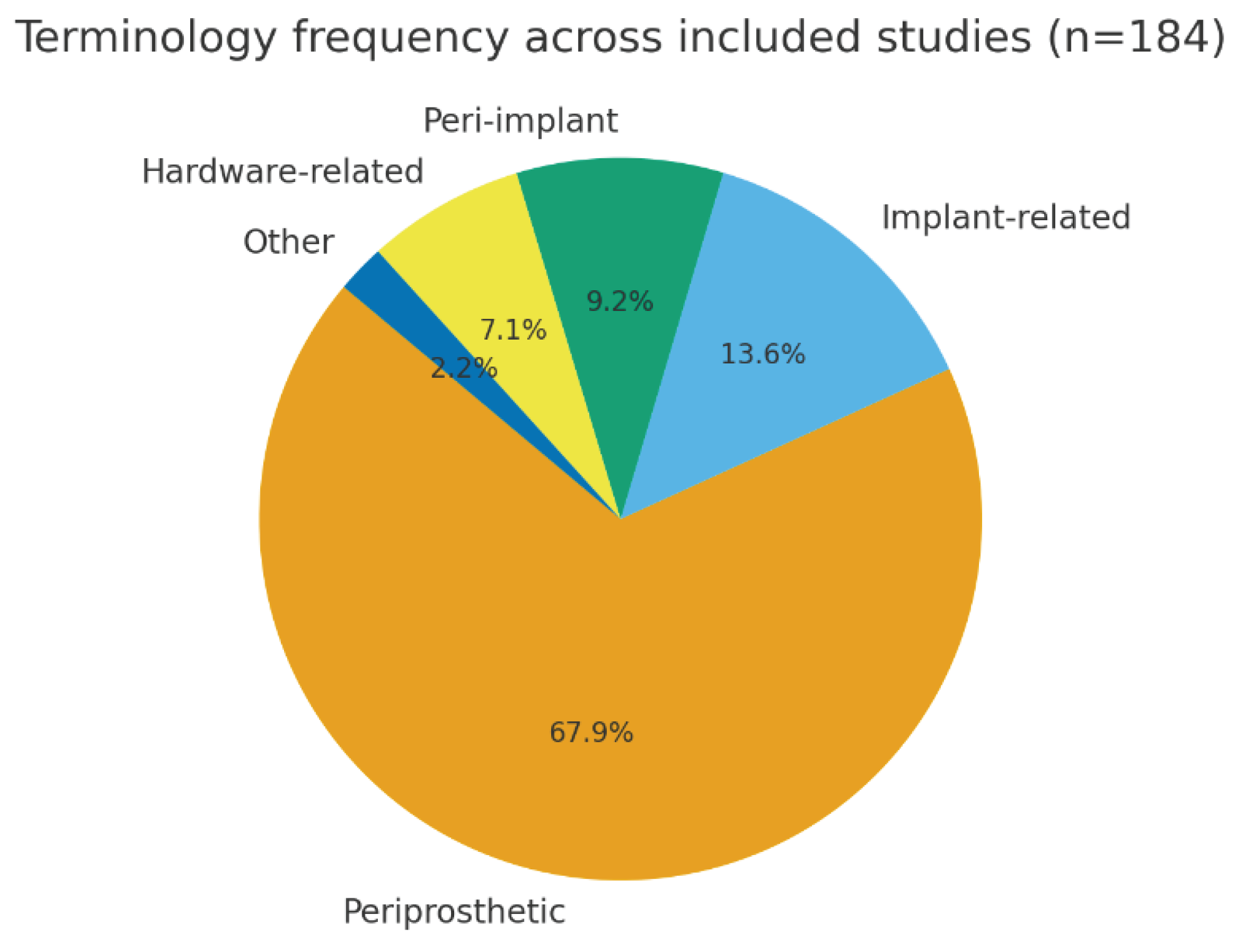
Terminology Frequency
- Implant-related fracture: 25 studies (14%)
- Peri-implant fracture: 17 studies (9%)
- Hardware-related fracture: 13 studies (7%)
- Other descriptors: 4 studies (2%)
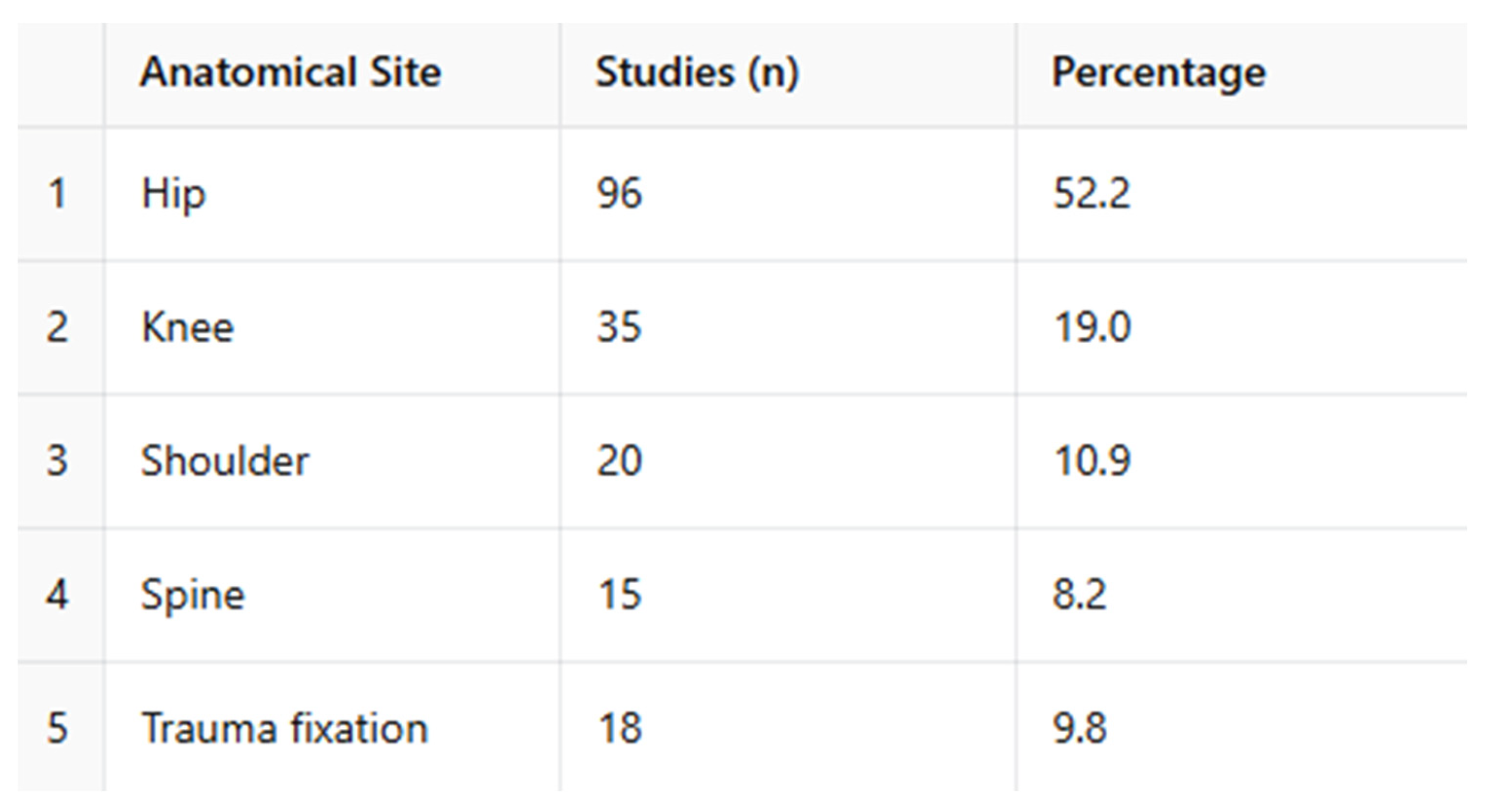
Anatomical Distribution
Comparative Analysis of Terminology by Anatomical Site [8,9,10]
- The term “periprosthetic fracture” was used almost exclusively in the hip and knee literature, accounting for the majority of studies in these regions.
- In contrast, the terms “peri-implant” and “implant-related fracture” appeared more frequently in studies of the shoulder and spine, where implant types are more heterogeneous and not always prosthetic.
- “Hardware-related fracture” was most often applied in the context of trauma fixation devices, particularly plates, screws, and intramedullary nails.
Consensus Group Statements
4. Discussion
Proposal of a Transversal Descriptor
- Comparability across anatomical regions, enabling more inclusive meta-analyses and systematic reviews.
- Integration within registries and administrative datasets, where a unifying descriptor may reduce coding variability.
- Clarity in multidisciplinary settings, allowing surgeons, radiologists, and researchers to communicate with a common baseline terminology.
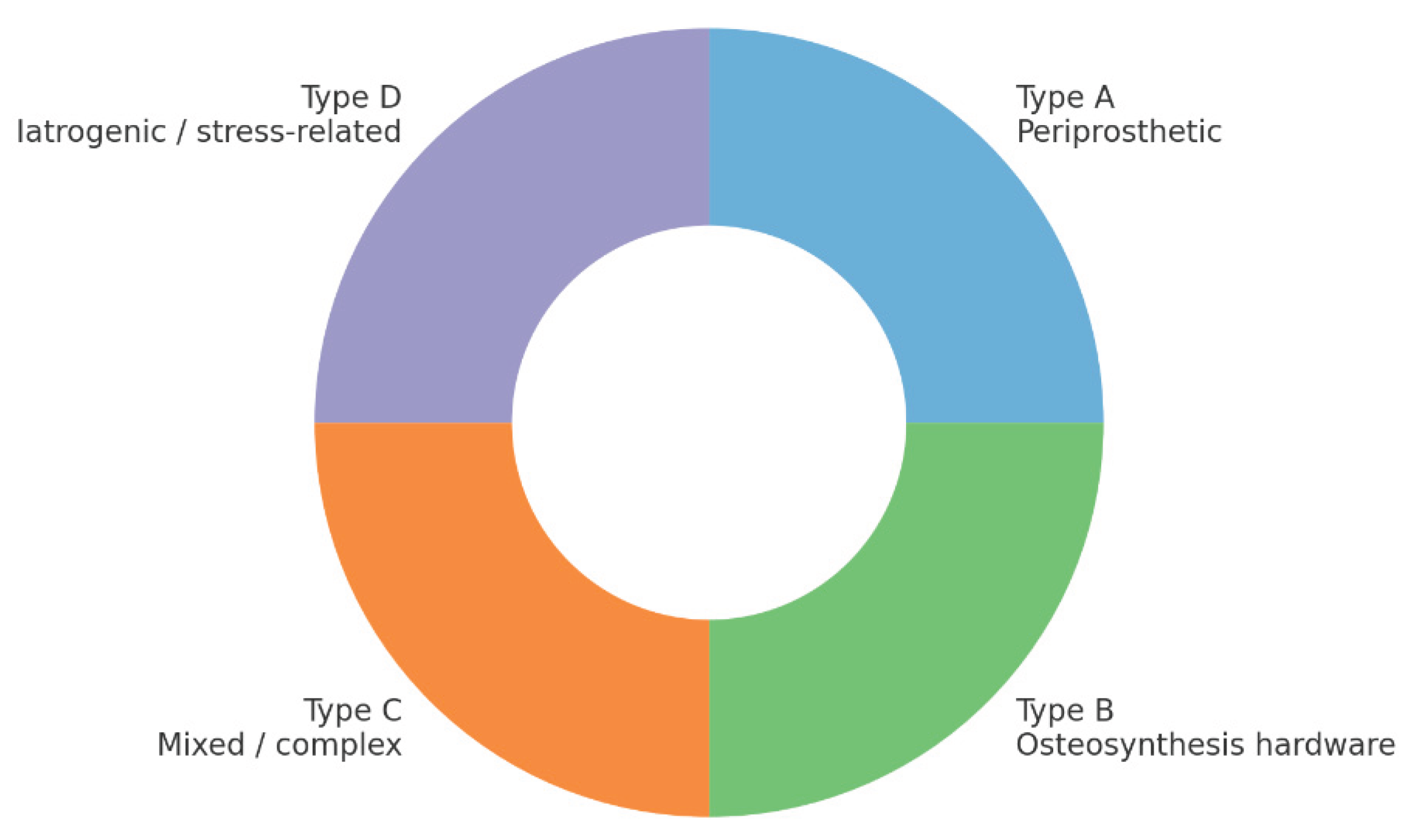
Exploratory Functional Classification
- Type A: Periprosthetic fractures (around arthroplasties)
- Type B: Fractures involving osteosynthesis hardware (plates, nails, screws)
- Type C: Mixed or complex fractures involving both prostheses and fixation devices
- Type D: Iatrogenic or stress-related fractures induced during surgery or implant loading
Addressing Potential Objections
- Ambiguity: The proposed definition of “artificial” is deliberately broad yet precise, referring to any fracture influenced by the presence of an orthopedic implant, and remains distinct from purely iatrogenic injuries.
- Redundancy: The descriptor does not replace established systems but rather functions as a meta-category that links them under a coherent umbrella.
- Consensus: Successful adoption would require active engagement from professional societies, registry bodies, and coders, ensuring alignment with existing classification frameworks.
Future Directions
- Formal validation in clinical and research contexts.
- Consensus-building initiatives involving international groups (AO/OTA, ISFR, ICS).
- Integration into digital health systems (electronic records, registries, coding standards).
5. Conclusions
- Enhance terminological clarity across specialties.
- Facilitate comparative research and meta-analyses.
- Improve coding reliability within registries and electronic health systems.
- Support multidisciplinary communication among orthopedic surgeons, trauma specialists, radiologists, and researchers.
Next Steps
- Conducting Delphi surveys among international experts to evaluate acceptance, clarity, and applicability.
- Implementing registry-based pilot testing to assess feasibility in real-world data environments.
- Pursuing endorsement by orthopedic societies and classification groups (e.g., AO/OTA, ISFR, ICS), which will be essential for broad adoption and integration into future guidelines.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Duncan CP, Haddad FS. The Unified Classification System (UCS): improving our understanding of periprosthetic fractures. Bone & Joint Journal (2014). [CrossRef]
- Van der Merwe JM, Haddad FS, Duncan CP. Field testing the Unified Classification System… knee replacement. Bone & Joint Journal (2014). [CrossRef]
- Schopper C, et al. The race for the classification of proximal PFFs: Vancouver vs UCS—systematic review. BMC Musculoskeletal Disorders (2022). [CrossRef]
- Mondanelli N, et al. Treatment Algorithm of Periprosthetic Femoral Fractures. Geriatric Orthopaedic Surgery & Rehabilitation. [CrossRef]
- Patsiogiannis N, Kanakaris NK, Giannoudis PV. Periprosthetic hip fractures: an update… EFORT Open Reviews (2021). [CrossRef]
- Gausden EB, et al. What’s New in Periprosthetic Femur Fractures? Journal of Arthroplasty (2024). [CrossRef]
- Lucenti L, et al. A Novel Comprehensive Classification for Non-Prosthetic Peri-Implant Fractures. Surgeries (MDPI) (2023). [CrossRef]
- Bernstein BP, et al. How resources affect management of periprosthetic fractures of the distal femur… OTA International (2023). [CrossRef]
- Castelli A, et al. Treatment of periprosthetic hip fractures Vancouver B1 and C… bicortical fixation… Orthopedic Reviews (2024). DOI nel PDF: 10.24294/or.v16i1.117203. orthopedicreviews.openmedicalpublishing.org.
- Baba T, et al. Therapeutic strategies for periprosthetic femoral fractures (Vancouver/AO-OTA/Baba). Journal of Orthopaedic Science (2025). (titolo sintetico nella tua lista; DOI da Springer/Elsevier) SpringerLink. [CrossRef]
- Santolini E, Giordano V, Giannoudis PV. Effect of mechanical stability of osteosynthesis on infection rates… Injury (2024). [CrossRef]
- Puls L, et al. Reducing femoral peri-implant fracture risk… biomechanical study. Journal of Orthopaedic Surgery and Research (2025). [CrossRef]
- Poroh M, et al. A Retrospective analysis of peri-implant fractures… International Orthopaedics (2023). [CrossRef]
- Prieto Meré JA, et al. Non-prosthetic peri-implant fracture of both forearm bones (case report). Journal of Surgical Case Reports (2023). [CrossRef]
- Castillón P, et al. Consensus review on peri-implant femur fracture treatment (PIFF). J Orthop Traumatol Rehabil (2024). [CrossRef]
- Ebraheim NA, et al. Periprosthetic distal femur fracture after TKA. Orthop Surg 2015;7(4):331-339. [CrossRef]
- Fakler JKM, et al. A new classification of TKA periprosthetic femur fractures. BMC Musculoskelet Disord 2017;18:490. [CrossRef]
- Rhee SJ, et al. Femoral PPF after TKA. Knee Surg Relat Res 2018;30(4):243-250. [CrossRef]
- Scolaro JA, et al. Management of interprosthetic femur fractures. JAAOS 2017;25(4):e63-e73. [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).




