1. Introduction
Sport and physical activity are fundamental to maintaining health across all age groups. Their benefits are extensive, including chronic disease prevention, reduced morbidity and mortality, and improved mental well-being [
1,
2]. However, participation also carries a risk of injury. So-called ‘sports injuries’ most often involve the musculoskeletal system and typically present as tissue damage and/or pain [
3,
4]. Common examples such as muscle strains, ligament sprains, and overuse injuries frequently cause acute pain, limiting movement, reducing force generation, and impairing coordination, thereby compromising overall motor performance [
5,
6]. These symptoms are consistently observed across a wide range of sports and competition levels, from recreational to elite [
6,
7,
8].
Injuries constitute a complex challenge that extends well beyond biological processes. Athletes, especially those participating in contact, strength, or endurance disciplines, may develop an elevated tolerance to pain through repeated exposure, yet they remain susceptible to significant psychological consequences [
9,
10]. A substantial body of work highlights the adverse psychological sequelae of injury. Empirical evidence indicates that injuries are frequently associated with heightened stress, anxiety, depressive symptoms, and reduced self-esteem, all of which can compromise motivation, adherence to rehabilitation protocols, and return-to-play outcomes [
5,
11,
12]. Furthermore, retirement from sport – particularly when precipitated by injury or deselection – can exert profound and enduring effects on mental health [
13]. Thus, while athletes may present as physically resilient, the psychological repercussions of injury represent a considerable challenge, underscoring the need for holistic management approaches that address both physical and psychological dimensions [
14,
15,
16,
17,
18].
The causes, consequences, and management of sports injuries have predominantly been investigated in able-bodied athletes, with research on athletes with physical disabilities remaining scarce. In para-sport, however, pain and its implications acquire a distinct and multifaceted dimension [
19,
20]. Pain perception in disabled athletes is influenced not only by sporting exposure but also by factors such as spasticity, postural deviations, and reliance on assistive devices [
19] (19). Repeated exposure to discomfort in daily life – for instance, resulting from spasticity or altered posture – may further contribute to modified pain experiences. Although the physiological aspects of pain responses are similar to those of able-bodied athletes, reports more frequently highlight a beneficial psychological dimension of sport-related pain in disabled sportsmen. Evidence suggests that pain contributes to emotional resilience and psychological adaptation in disabled athletes through complex, multifactorial processes. In competitive athletes with spinal cord injury, resilience appears to be supported by pre-existing personality traits, social support, coping strategies, and motivation to adapt, with sport participation itself acting as a facilitator of adjustment to acquired disability [
21]. Behavioural patterns may also diverge: disabled athletes have been shown to report lower levels of antisocial behaviour and moral disengagement compared with their able-bodied colleagues [
22,
23]. Within this context, pain may assume a constructive role. While intrinsically aversive, it has the potential to foster positive changes in self-perception and self-esteem, thereby enhancing quality of life, emotional growth, and motivation to maintain physical activity. Sport- and competition-related pain – distinct from that associated with illness – may even elicit a form of ‘warrior emotionality’, conferring beneficial psychosocial effects. This phenomenon is particularly salient among individuals vulnerable to negative body perceptions arising from health conditions, aesthetic concerns, and disability.
Despite growing recognition of these adaptive mechanisms in adult para-athletes, much less is known about adolescents with disabilities. This population may not yet have fully developed strategies for managing pain, making them particularly vulnerable to maladaptive responses such as depressive symptoms, social withdrawal, or disengagement from physical activity [
2,
6,
24]. At the same time, adolescence represents a critical developmental stage in which sport participation and even mild to moderate injury-related pain could act as a form of ‘adaptive training’, shaping constructive attitudes toward pain and fostering resilience. Such experiences may help prevent the emergence of negative behavioral and emotional patterns, including depressive or antisocial tendencies, which are reported at higher rates in youth with disabilities compared to their able-bodied peers. The present study addresses this research gap by examining adolescents with lower limb disabilities engaged in sitwake. The aim of this study is to evaluate: 1) changes in quality of life among adolescents with lower limb disabilities participating in sitwake, comparing those who experienced transient injuries associated with moderate pain during trainings with those who did not; 2) changes in pain attitudes in these two groups; and 3) return to sitwake training rate in the following season. The authors hypothesise that the occurrence of injuries, despite the accompanying pain, will be associated with beneficial changes in quality of life and in attitudes towards pain, thereby increasing the likelihood of continued training.
2. Materials and Methods
2.1. Design
It was a prospective case-control study with a three-month observation period, during which the dependent variables were measured twice: once at baseline, prior to observation, and again at the end of the study period. The prevented them from continuing training for at least one week. The project was approved by the Institutional Research Ethics Committee (No. 13/2020).
2.2. Participants
The minimum required sample size was determined a sample size calculator [
25], with the following assumptions: α = 0.05, minimum effect size = 15%. The largest requirement was calculated for the cautiousness subscale of the Pain Attitudes Questionnaire (N = 19) (see below). Recruitment was concluded once the minimum required sample size in the PG had been reached (N = 20).
Participant recruitment took place during the enrolment of young people with physical disabilities who expressed interest in sitwake training at a local wakeboarding club, across three consecutive seasons (2021-2024). In each of these seasons, the procedures for recruitment, training, and, where applicable, therapeutic management of injuries remained identical. The training offer was targeted at adolescents with physical disabilities aged 10-18 years.
Compliance with the inclusion criteria was verified during an introductory meeting and examination conducted jointly by a medical doctor, a physiotherapist, and a sitwake instructor. The inclusion criteria were as follows: age between 12 and 18 years; first contact with sitwake; lower limb disability precluding independent walking (with only supported upright posture possible); full upper limb function; full intellectual capacity; absence of comorbidities precluding physical activity (e.g. cardiologic or pulmonary diagnoses); absence of psychological disorders; and ≥70% adherence to the training programme (including pauses due to injury).
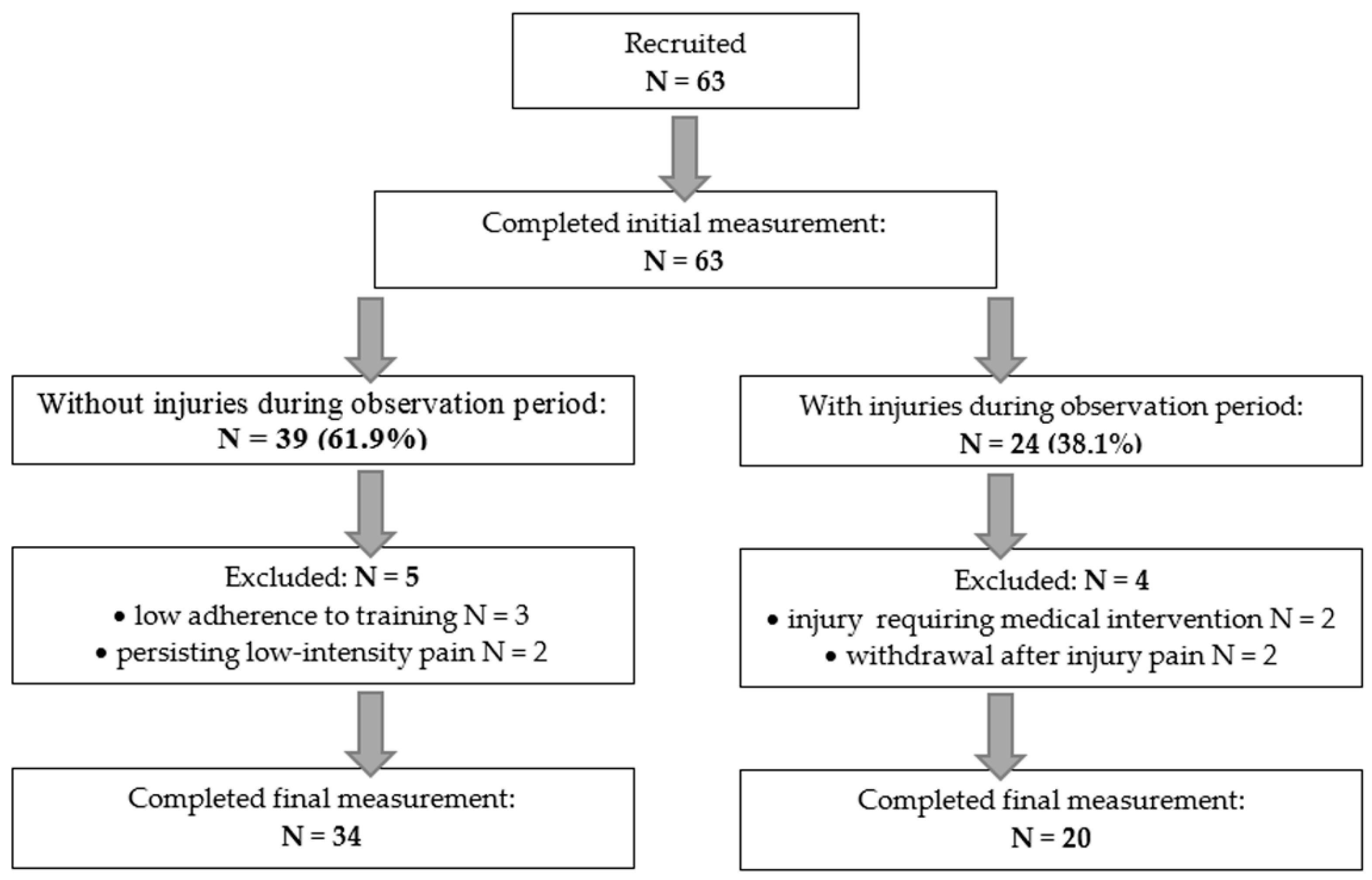
Of the 69 individuals meeting the selection criteria, 63 consented to participate in the study (informed consent form legal guardians was obtained in each case). All these participants completed the baseline assessment of the dependent variables. During the 3-month observation period (June-August in each of the three seasons), a subgroup was identified in whom sitwake-related musculo-skeletal injuries occurred accompanied by pain and functional impairment (the pain group – PG). The inclusion criteria for the PG group were: a sitwake-related mild to moderate injury with pain intensity between 50% and 80% on the Visual Analogue Scale (VAS; 0-100%), pain severe enough to preclude participation in training sessions for at least one week, and subsequent reduction of pain to 0-10% on the VAS following the applied therapy. Exclusion criteria comprised severe injuries associated with pain preventing training for more than three weeks, as well as injuries requiring medical interventions (orthopaedic or surgical) beyond physiotherapy, physical modalities (e.g. electrotherapy, magnetic field therapy, ultrasound, cryotherapy), and local anti-inflammatory or analgesic medication. The remaining participants constituted the no-pain group (no-PG).
Across the three seasons, sitwake-related injuries occurred in 24 participants. Two of these were not classified into the PG owing to the severity of their injuries, which required orthopaedic intervention. A further two participants, although meeting the criteria for inclusion in the PG, withdrew from training after the injury. Ultimately, 20 participants were assigned to the PG. Three of them sustained injuries fulfilling the inclusion criteria on two separate occasions. All 20 individuals in the PG completed the final assessment of the dependent variables.
Of the remaining 39 individuals initially designated for the no-PG, two reported post-exercise pain (VAS 30-40%) without clinical signs of tissue damage. As this pain prevented their participation in training for one week, they were excluded from data analysis to avoid bias. Three further participants demonstrated adherence to the training programme of <70%. Consequently, the final no-PG comprised 34 participants, all of whom completed the final assessment of the dependent variables.
The flow of participants through the successive phases of the study is shown in
Figure 1. Basic demographic characteristics of both groups are presented in
Table 1.
Injuries recorded in the PG were predominantly soft tissue bruises and muscle strains, as well as joint sprains and non-sprain joint disorders (such as cartilage irritation and capsular stress) particularly affecting the shoulder girdle, upper arm, neck, and upper torso, resulting mainly from falls, transfers, pushing motions, or collisions. Occasional injuries were also reported in the lower extremities. The mean initial pain intensity was 63.45% (±7.74; 52-79) on the VAS scale, decreasing to 5.30 (±3.88; 0-10) at final assessment. The mean training absence due to injury was 12.35 days (±3.34; 8-19). The type and location of injuries recorded in the PG are detailed in
Table 2.
2.3. Measurements
In order to investigate 2 standardised questionnaires were selected. They were: the 37-item DISABKIDS Chronic Generic Module (DCGM-37) [
26,
27] and 27-item Pain Attitudes Questionnaire (PAQ-27) [
28,
29].
The DCGM-37 items are grouped into six subscales reflecting factors related to the health-related quality of life relevant to children and adolescents: independence, physical limitations, emotions, social exclusion, social inclusion, and treatment impact [
30]. Items are rated on a five-point Likert scale reflecting the frequency of behaviours or feelings experienced over the preceding four weeks, with response options ranging from 1 (never) to 5 (always). For scoring, responses within each subscale are converted to a 0-100 scale, with 1 = 100, 2 = 75, 3 = 50, 4 = 25, and 5 = 0, before summation. The DCGM-37 has shown satisfactory internal consistency with Cronbach’s alpha from 0.70 to 0.87 for specific factors, as well as good test-retest reliability with intraclass correlation coefficients from 0.71 to 0.83 [
26]. For each subscale the following interpretation applies: higher scores indicate a greater influence of the respective factor on health-related quality of life. For the independence and social inclusion subscales, the greater influence may be regarded as positive, whereas for physical limitations, emotions, social exclusion, and treatment impact, it should be considered negative.
For the PAQ-27, a two-factor model was employed [
31], comprising subscales of stoicism (14 of the 27 items) and cautiousness (13 of the 27 items). Within this framework, stoicism is conceptualized as a construct encompassing behaviours such as reluctance to express pain and/or perceiving oneself as having superior control over pain, while cautiousness reflects uncertainty regarding whether a given sensation should be identified as pain and/or a reluctance to label a sensation as painful. Each item was rated on a five-point Likert scale, ranging from 1 (strongly disagree) to 5 (strongly agree). The mean score of all items within each subscale was used as the outcome measure. In an adult Australian population, Yong et al. [2001] reported good to excellent internal consistency for the PAQ-27, with Cronbach’s alpha coefficients ranging from 0.78 to 0.86 for the stoicism subscale and from 0.75 to 0.81 for the cautiousness subscale [
29]. Test-retest reliability was also demonstrated, with Pearson’s correlation coefficients ranging from 0.86 to 0.87 for stoicism and from 0.91 to 0.92 for cautiousness. For each subscale the interpretation applies: the higher the score, the higher level of the examined attitude towards pain.
Return to sitwake training rate was recorded at the start of the season subsequent to the one in which the aforementioned measurements were obtained.
The DCGM-37 and PAQ-27 are established questionnaires that has been described in earlier [
26,
28,
29,
30]. Their Polish adaptations, including translation and linguistic validation, was thoroughly conducted in accordance with the following protocol. Initially, two bilingual medical professionals, both native speakers of Polish, independently translated the English versions into Polish. These translations were subsequently reviewed by a panel comprising four specialists in paediatrics and psychology, who reconciled differences and produced a single consensus versions of each questionnaire. This drafts was then subjected to back-translation by an independent bilingual medical expert, with the resulting texts further examined by the panel. Following minor adjustments, a pilot test was carried out with 10 adolescents. After completing the questionnaires, participants were interviewed individually by one of the authors to verify whether the items were understandable, whether any important aspects were missing, and whether the response options were appropriate.
2.4. Research Team
The authors assumed supervisory and coordinating roles within the project. They participated in the recruitment process, were responsible for preparing the online questionnaires, and provided instructions and clarifications to participants during data collection. Subsequently, they prepared and curated the databases and conducted data analyses. They were not directly involved in the training or therapeutic procedures.
The research team included two physiotherapists with comparable levels of education (Master of Science in rehabilitation, supplemented with additional training in physiotherapy, manual therapy, and massage), each affiliated with a wakeboarding club for approximately five years, and with 10-11 years of overall professional practical experience. The physiotherapists were responsible for assessing candidates for training, monitoring the occurrence of injuries within the observed group, recording the intensity of pain symptoms, monitoring participants’ condition following pain episodes, and making decisions regarding return to training or referral for medical consultation. Once given participant was assigned to the PG group, the physiotherapists implemented the therapeutic plan established in consultation with a physician (see below).
A medical doctor specialising in orthopaedics conducted the initial screening of training candidates and carried out examinations of participants assigned to the PG group in course of the observation. Together with the physiotherapists, he contributed to the development of the therapeutic plan for each participant and, following its completion, assessed the individual’s readiness to return to training.
Two wakeboarding instructors, each with ten years of experience in conducting sit-board sessions for individuals with disabilities and applying a standardized training protocol, were involved in participant recruitment. Notably, both instructors are active athletes and serve as leaders of the Paralympic Wake Camp. They were subsequently responsible for delivering all training sessions (see below) and for recording participant attendance.
In addition, all previously mentioned team members participated in the final debriefing meetings conducted at the end of each of the three training seasons.
In addition, the supportive role of the club manager should be acknowledged, who was responsible for logistics, technical and organisational issues, as well as the contribution of the cable system operators.
2.5. Sitwake Training
Sitwake, or sit-down wakeboarding, is an adaptive water sport tailored for individuals with lower-limb impairments. Athletes utilise a specially designed wakeboard equipped with a seated bucket and harness, providing stability while being towed by a cable system. The sport encompasses a wide range of on-water activities analogous to those in traditional wakeboarding, modified for the seated position. In the present study, participants acquired the fundamental skills required for sitwake, including controlled carving, turns, and directional changes, and progressed to basic acrobatic manoeuvres, such as simple jumps, spins, and grabs.
Over each of the three 13-week training seasons, a total of 39 sitwake sessions were conducted. The sessions were delivered alternately by two instructors, depending on their individual availability. This arrangement did not cause major disruptions, as both possessed comparable skills and experience, and followed a standardised training programme. The proportion of sessions conducted by each instructor was similar, i.e. 46% and 54%.
Training sessions were held three times per week, each lasting 1.5 hours. The structure comprised: (1) introduction (10-15 min): equipment checks and adjustment, preparatory warm-up including mobility drills, core activation, and balance exercises, supported by mental rehearsal and visualisation; (2) main component (60-75 min): on-water training aligned with the weekly thematic focus; (3) conclusion (10-15 min): structured stretching, relaxation, feedback, and systematic review of recorded performance. The training scheme remained uniform (
Table 3) owing to the participants’ low skill level and the practical difficulty of forming subgroups of differing proficiency. Individual differences related to the relatively comparable degree of disability were addressed through small, ad hoc modifications to the planned exercises.
2.6. Therapy
Within the PG, therapeutic sessions with a physiotherapist were conducted every second day, excluding weekends, each lasting approximately 1.5 hours. Sessions were delivered alternately by two physiotherapists, depending on availability. This arrangement did not cause disruption, as both possessed comparable expertise and adhered to the standardised PEACE & LOVE protocol [
32], integrating acute and subacute treatment strategies. The distribution of sessions was slightly unbalanced, i.e. 39% and 61%. After each session, participants received specific recommendations for the intervening days and were required to follow these therapeutic instructions in the home setting.
All participants allocated to the PG initially reported pain intensity ≥50% on the VAS. At this stage, the PEACE phase was applied. Protection (P) involved limiting aggravating movements and, where required, using temporary supports such as slings or taping to allow tissues to settle. Protection did not equate to strict immobilisation; short, pain-free movements were encouraged to prevent stiffness. Elevation (E) was recommended where feasible, positioning the upper limb above heart level to promote venous return and minimise swelling. Avoidance of anti-inflammatory agents (A) was emphasised unless strictly necessary, with advice to minimise their use. Compression (C) with elastic bandages was applied in cases of visible swelling, providing mechanical support and oedema control. Structured Education (E) was delivered during the first therapy session, covering injury mechanisms, expected recovery timelines, and the importance of active engagement in rehabilitation to promote adherence and self-efficacy.
Progression to the LOVE phase was initiated once pain intensity decreased to approximately 20-30% on the VAS. Loading (L) was introduced through pain-free, individualised exercises, starting with assisted movements and advancing to active strengthening. The optimism (O) component was deliberately omitted to avoid external influence on participants’ emotional state and thereby minimise therapist-induced bias. Vascularisation (V) was promoted via light aerobic activity adapted to the seated position (e.g. arm ergometry, rhythmic upper-limb movements) to enhance circulation and support metabolic repair. Exercise (E) was tailored to restore joint mobility, proprioception, and sport-specific function, progressing to higher-intensity drills only once baseline control and confidence were regained. By the end of the therapeutic process, pain reduction to 0-10% on the VAS was achieved.
2.7. Procedure
Prior to the first training session, all participants were asked to arrive one hour earlier to complete baseline measurements of the dependent variables. They first received detailed instructions regarding the DCGM-37, after which they read the questionnaire on a computer screen and entered their responses. To maintain adequate concentration, a 20-minute break was scheduled, including a 10-minute period of light rest, followed by instructions for the PAQ-27. Again, participants then completed the PAQ-27 on the computer. The entire procedure lasted approximately 40-50 minutes.
The next stage comprised a 13-week sitwake training period (see above). During this period, participants were instructed to report any occurrence of pain and/or dysfunction directly to the physiotherapists and to rate its intensity using the VAS. All participants with pain intensity exceeding 50% were immediately referred to the medical doctor for consultation. Those reporting pain intensity <50% were monitored by physiotherapists, including follow-up by telephone. If pain intensity increased, the participant was referred to the medical doctor; if it decreased, continuation of training was recommended. For participants meeting the criteria for the PG group, injuries were managed by the physiotherapy team as outlined above.
Within one week after the final training session, the dependent variables were reassessed during a summary visit at the wakeboarding club. During this visit, the entire team (authors, medical doctor, physiotherapists, and sitwake instructors) provided their concluding opinions, recommendations, and suggestions for the future to the participants and their legal guardians. The procedure of this follow-up data collection was identical to that employed during the initial assessment. A three-month interval was considered sufficient for participants to have forgotten their previous responses and to allow for a measurable change in the dependent variables [
33].
2.8. Data Management
All responses were stored in a computerised database. The authors did not have access to the database until data collection was completed, in order to minimise potential bias. Scale scores were calculated strictly according to the original scoring instructions. Both baseline and follow-up scores, as well as change scores (calculated as follow-up minus baseline), were subjected to statistical analysis.
2.9. Statistical Analysis
To assess the internal consistency of the data Cronbach's alpha coefficient was used. Deviations from normal distribution were analysed using the Shapiro-Wilk test. Intra-group differences were assessed using the dependent data Student's t-test or non-parametric Wilcoxon (dependent on data distribution), inter-group differences – using the independent data Student's t-test or non-parametric Mann-Whitney test. Difference in return to training rates was evaluated using the statistical test for two fractions. The Statistica 13.0 software (StatSoft, Tulsa, US) was used.
4. Discussion
The aim of this study was to examine whether transient injuries associated with moderate pain during sitwake training could influence adolescents with lower-limb disabilities in ways that go beyond the immediate biological function of pain. Specifically, we evaluated whether such experiences would be linked with changes in quality of life, shifts in pain attitudes, and subsequent likelihood of returning to the sport. In formulating this objective, we anticipated that pain – although inherently aversive – might under certain conditions serve as a stimulus for beneficial psychosocial adaptation and reinforce continued participation.
Our study deliberately does not dispute the fundamental biological role of pain as tissue-damage signal. Acute pain in the context of sport fulfilled this uncontroversial function in our sample by alerting participants to ongoing or recent tissue injury [
34,
35]. Rather, the novel and clinically relevant question addressed here concerns what follows the nociceptive signal – the psychosocial cascade that shapes interpretation, behavior and long-term participation.
Pain is not a unitary experience, it triggers highly variable psychological responses that are filtered through cognitive, emotional and social processes [
36]. Our findings align with literature showing that, beyond raw nociception, meaning-making, prior exposure, social support, self-efficacy and coping repertoire largely determine whether pain becomes disabling or, conversely, an opportunity for growth [
37,
38]. In this sense, sport provides a specific context in which pain can be reappraised: when experienced in a framework of instrumental training and group belonging, transient sport-related pain may be interpreted as evidence of effort, progress and resilience rather than as solely catastrophic threat.
This mechanism helps explain our central observation – that moderate, transient training injuries were associated with favorable shifts in quality of life among adolescents with disabilities.
It is difficult to interpret recorded mean values for both DCGM-37 and PAQ-27 subscales, as no established normative data are currently available in the literature. In general, baseline results from our study indicated that scores for both scales were approximately at the midpoint of their respective possible ranges (25-100 for all subscales of the DCGM-37 and 1-5 points for the PAQ-27 subscales). Direct comparisons with other studies are limited due to differences in study populations; however, it is noteworthy that relatively similar results were reported by several authors [
27,
39,
40].
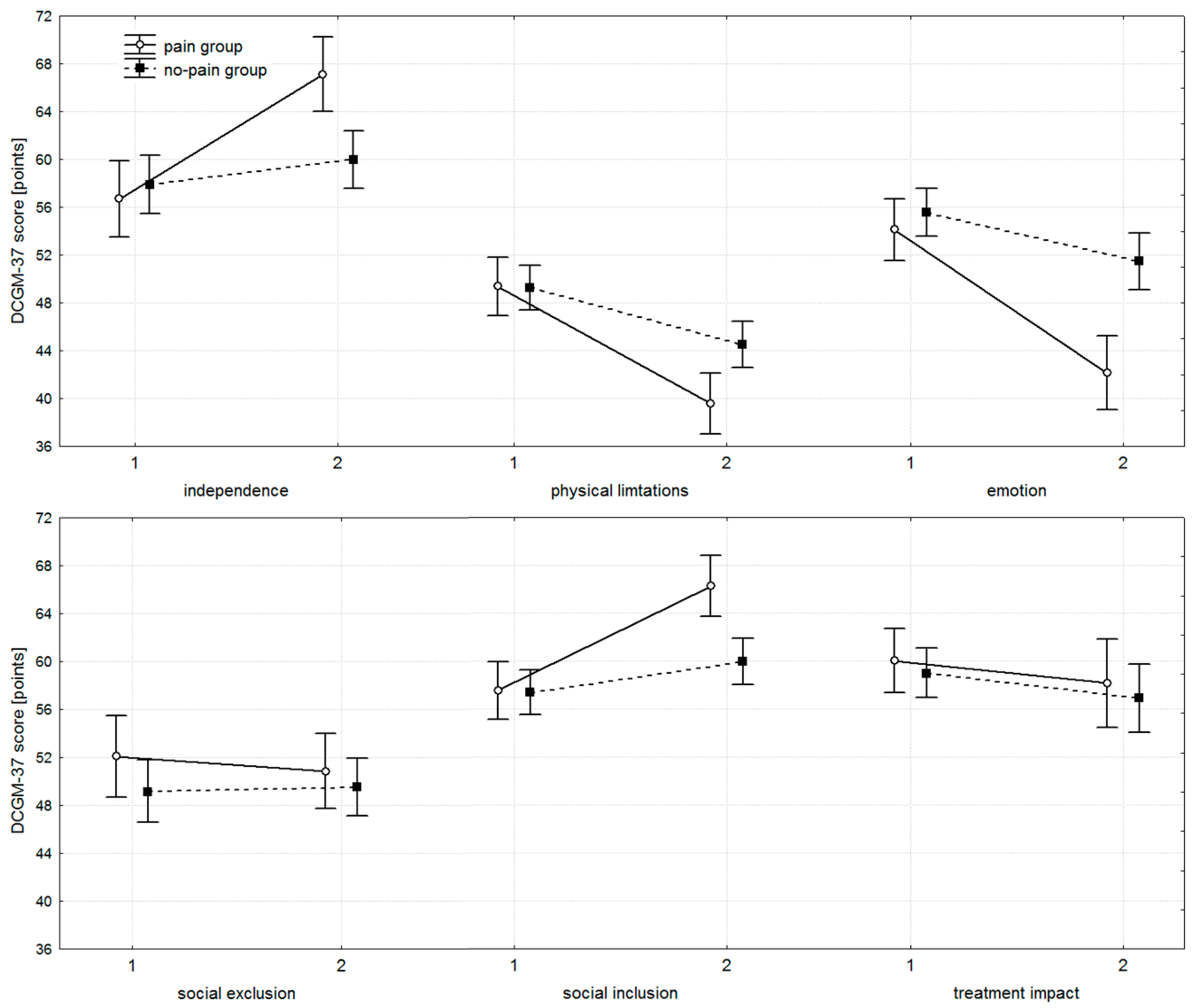
The DCGM-37 subscales for independence, physical limitations, emotion, and social inclusion clearly favored the PG group. Both groups began at comparable baseline levels; however, by the end of the study, the PG group demonstrated significantly better outcomes, reporting greater independence, fewer physical limitations, fewer negative emotions related to disability, and higher levels of social inclusion. Within-group improvements were observed in both groups, but these changes were markedly larger in the PG group. Although statistically significant progress was noted in the no-PG group, the clinical relevance of these changes is questionable. For no-PG, the mean changes on the aforementioned DCGM-37 subscales were 2.10, -4.78, -4.10, and 2.58 points, respectively, suggesting that statistical significance does not necessarily reflect meaningful clinical improvement. In contrast, the PG group exhibited substantially larger changes – 10.41, -9.81, -11.99, and 8.72 points, respectively – representing improvements two to five times greater than those observed in no-PG and more likely to be clinically relevant. No statistically or clinically important differences were observed for the social exclusion and treatment impact subscales of the DCGM-37.
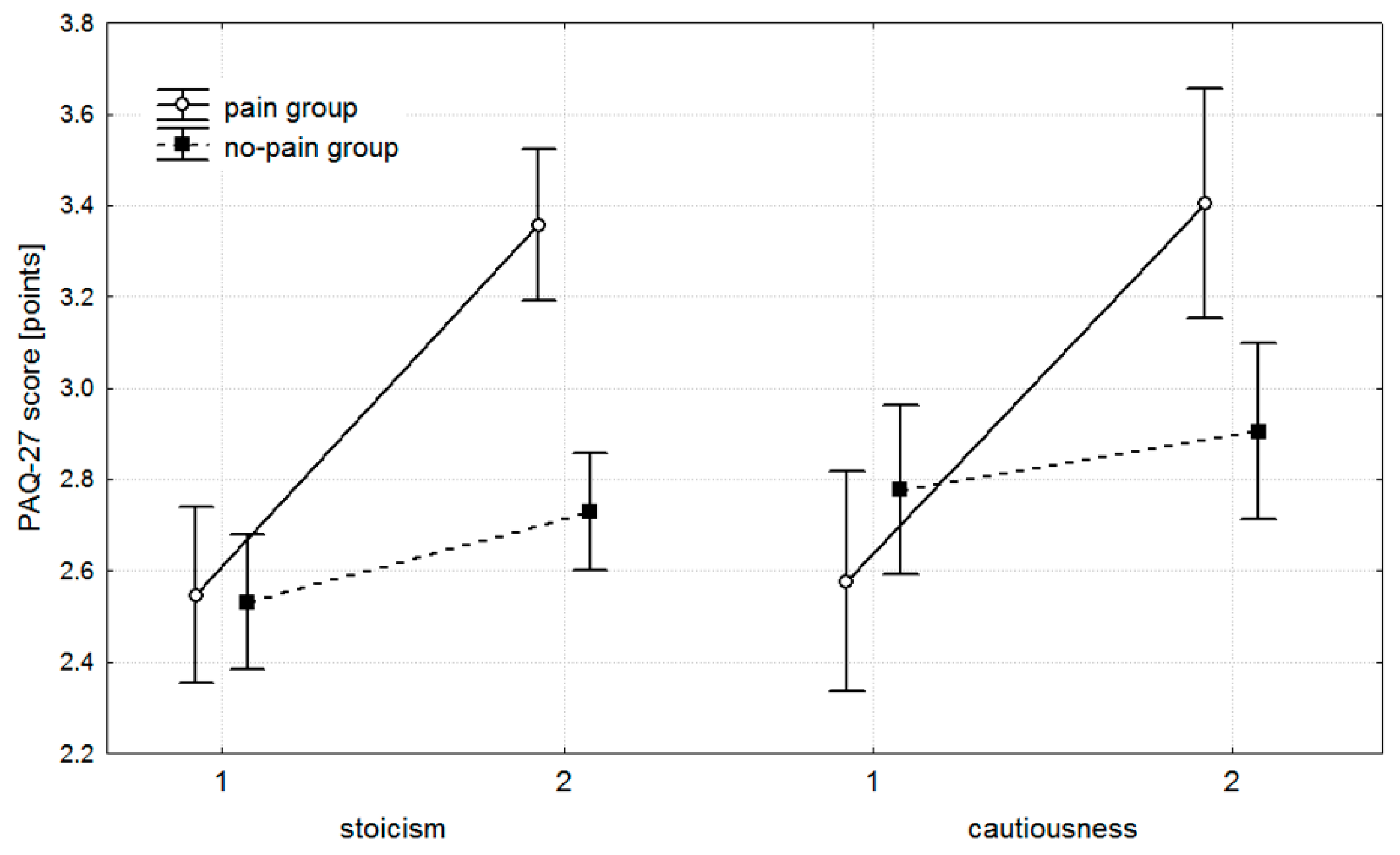
Turning to pain attitudes, as assessed by the PAQ, we observed a pattern broadly consistent with that seen in the responsive DCGM-37 subscales. It is worth noting that the stoicism subscale of the PAQ-27 reflects an attitude characterized by downplaying pain, refraining from expressing it, and maintaining a belief in one’s superior ability to control it. The cautiousness subscale, in turn, captures uncertainty in judging whether a given unpleasant sensation truly constitutes pain. At baseline, both groups exhibited comparable scores; however, by the end of the intervention, the PG group achieved significantly higher values across both PAQ subscales. Between-group comparisons of change scores further confirmed the greater progress observed in PG. Within-group analyses showed statistically significant improvements in both PG and no-PG; however, the clinical relevance of these changes in the no-PG group is debatable. Here, the magnitude of change was modest, with mean increases of 0.20 points for stoicism and 0.13 points for cautiousness, whereas in the PG group, these shifts were substantially larger – 0.80 and 0.83 points, respectively – representing four- to sevenfold greater improvements.
Taken together, the consistent pattern across both quality-of-life outcomes and pain attitudes suggests that transient injuries and their associated pain were not merely tolerated but may have initiated positive psychosocial change. Adolescents in the PG group develop – or began to develop – a more resilient and self-reliant approach to discomfort, while also learning to calibrate their appraisal of bodily signals. In other words, sport-related pain, when experienced within a supportive and supervised environment, appears to foster adaptive forms of toughness without tipping into maladaptive denial [
41,
42,
43]. Notably, the benefits observed in the DCGM-37 were concentrated in subscales that assess domains of quality of life – namely, independence, perception of physical limitations, emotions linked to disability, and sense of social inclusion – that reside ‘within the individual’, and are largely independent of external influences. This pattern suggests that responses to sport-related pain may first emerge in the internal world of the individual, initiating the development of the ‘warrior mentality’ mentioned in the Introduction. Importantly, our findings provide the first evidence that such transformation can be induced in young people whose life attitudes and emotional frameworks are still forming. Exposure to manageable adversity during this sensitive developmental window may have lasting consequences, shaping resilience and commitment that extend beyond sport. This observation directly addresses the knowledge gap highlighted in the Introduction, a topic that has received limited attention in the existing literature.
No differences were observed for the social exclusion and treatment impact DCGM-37 subscales, and several explanations may account for this finding. First, sport participation, injuries, and associated pain may primarily exert effects within the individual, without substantially influencing aspects of quality of life that are shaped by the external environment. Regarding social exclusion, it is notable that most training sessions occurred during school holidays, whereas children with disabilities are most at risk of experiencing social exclusion within the school setting. Consequently, these effects may have been attenuated in our study, and conducting the research during the academic year might have revealed different outcomes. With respect to treatment impact, children with disabilities are often exposed to frequent therapeutic interventions and may perceive therapy negatively, regardless of its specific purpose. In our study, the therapy provided was aimed at alleviating sport-related pain rather than addressing the underlying disability, yet participants may have regarded it as ‘just another therapy’, diminishing its perceived benefit.
Although inherently positive, the changes observed in the PAQ-27, which favored the PG, may carry potential risks. Increased stoicism, as captured by the PAQ-27, or a ‘can-do’ mindset can sometimes lead to elevated risk-taking and neglect of injury-prevention behaviors, particularly in the absence of adequate monitoring and education. Instruments assessing the relationship between risk, pain, and injury (e.g., the Risk–Pain–Injury Questionnaire) and empirical studies have identified associations between permissive pain attitudes and unsafe escalation of training load or premature return-to-play decisions [
44]. To mitigate such hazards, structured injury-education and safe-practice programs for athletes, coaches, and support staff are essential. Concussion education programs and targeted return-to-sport interventions provide a precedent for effective knowledge translation in youth sport [
45,
46]. In our program, we have introduced brief modules on symptom recognition, graded training, and help-seeking. These represent practical translational steps that can curb maladaptive risk-taking while preserving the psychosocial benefits observed in participants.
Finally, the practical significance of the documented changes in health-related quality of life and pain attitudes is underscored by follow-up data. In the subsequent season, twice as many adolescents from the PG group returned to sitwake compared with the no-PG group (65% vs. 29%). This finding suggests that experiencing and overcoming pain did not deter participants; on the contrary, it appears to have reinforced their motivation to re-engage with sport.
4.1. Limitations
Several limitations of our study should be acknowledged. First, our findings pertain to small- and moderate-intensity pain, and it remains unclear how participants would respond to more severe injuries. Indeed, among study dropouts, two participants withdrew even after minor injuries, suggesting that higher-intensity injuries might result in greater attrition.
Second, the study was limited to sitwake, which constrains generalization to other sports. Nonetheless, it is reasonable to assume that the experience of sport-related pain and minor injury would evoke similar internal responses across disciplines, as the key factor is the experience of injury in the context of performance rather than the specific sport. Limitations regarding generalizability are also relevant with respect to age and type of disability: our sample included predominantly young participants with mild impairments, and responses may differ in older athletes or those with more severe disabilities.
Third, this study employed a case–control design. Although prospective in nature, it provides only Level 3 evidence, as classified by the Oxford Centre for Evidence-Based Medicine Levels of Evidence.
Finally, the sample size was relatively small. However, given the three-year duration of the study and the niche nature of the sport, this represents a substantial achievement. Furthermore, the sample met the pre-specified criteria for statistical power, supporting the reliability of the results obtained.
Author Contributions
Conceptualization, A.G., M.B., and R.G.; methodology, A.G., M.B., and R.G.; software, M.B., and R.G.; validation, A.G., M.B., and R.G.; formal analysis, R.G.; investigation, A.G., M.B., and R.G.; resources, A.G.; data curation, R.G.; writing – original draft preparation, A.G., M.B., and R.G.; writing – review and editing, A.G., M.B., and R.G.; visualization, R.G.; supervision, A.G.; project administration, A.G.; funding acquisition, A.G. All authors have read and agreed to the published version of the manuscript.